Abstract
Objective
Behavioral intervention technologies (BITs) stand as a promising delivery mechanism that overcomes multiple condition-specific and access barriers for self-management interventions for adolescents and young adults with spina bifida (AYA-SB). The purpose of the current review was to synthesize the behavioral and self-management intervention literature in conditions that have overlapping symptoms with youth with SB and to develop a model of likely user needs for AYA-SB that promotes self-management.
Method
The search strategy was conducted by a medical research librarian in the following databases: MEDLINE (Ovid), EMBASE (Elsevier), PsycINFO (EbscoHost), the Cochrane Library (Wiley), and Web of Science (Thomson Reuters) databases. The review was based on a systematic narrative synthesis framework and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (registration number CRD42018092342).
Results
In total, 18 articles were included in the current BIT review. The majority of included studies (1) targeted the management of chronic health conditions, (2) were informed by evidence-based approaches, (3) relied on content delivery, (4) were Web-based, (5) used linear or user-driven workflows, (6) included professional human support, and (7) included a control condition.
Conclusions
Many of the evaluated BITs resulted in acceptable usage and maintained or improved targeted symptoms. A user needs model for AYA-SB is proposed with the intention that future research will promote further refinement and ultimate deployment of a BIT for AYA-SB to promote self-management.
Keywords: AYA, behavioral intervention technologies, chronic health, intellectual disability, physical disability, self-management, spina bifida
Resulting from a neural tube defect during early pregnancy, spina bifida (SB) is the most common congenital birth defect affecting the central nervous system (Copp et al., 2015). Though medical advances have improved survival rates into adulthood (Dicianno & Wilson, 2010), SB remains a significant public health concern owing to its prevalence and the substantial economic resources required to support youth with SB (Copp et al., 2015). SB poses unique challenges, as youth must manage both a complex medical treatment regimen and a variety of cognitive and psychosocial comorbidities (e.g., surgeries, bladder and bowel control, motor and sensory neurological deficits, psychosocial difficulties, and pain; Copp et al., 2015). Notably, a decline in medical adherence is often seen in late adolescence and early adulthood (Modi, Marciel, Slater, Drotar, & Quittner, 2008); such nonadherence in SB can be life-threatening, a threat often due to preventable complications such as pressure sores, urinary tract infections, or shunt malfunctions (Dicianno & Wilson, 2010). Therefore, the combination of increased survival into adulthood and high levels of nonadherence necessitates (1) research that promotes success during the complex developmental period from childhood to adulthood (a period including adolescents and young adults with SB, hereafter referred to as AYA-SB), and (2) delivery mechanisms that can overcome the unique barriers that often interfere with condition self-management for youth with SB (e.g., mobility; Boudos & Mukherjee, 2008).
Behavioral intervention technologies (BITs), the use of technology (e.g., mobile apps and Web sites) as a method of delivery for behavioral health interventions, have been identified as a promising delivery mechanism to overcome access barriers across a variety of behavioral health conditions (Mohr, Burns, Schueller, Clarke, & Klinkman, 2013). The BIT model, a framework for designing and deploying BITs, includes levels that are conceptual (“why” the BIT exists and “how” it will achieve its aims) and levels focused on the technical aspects of a BIT (“what” is delivered to users, “how” this delivery occurs, and “when”; Mohr, Schueller, Montague, Burns, & Rashidi, 2014). BITs appear to be a promising strategy for reaching AYA-SB. Indeed, 92% of adolescents with SB report consistent Internet use (Betz, Smith, Macias, & Bui, 2014), thus supporting the use of BITs with this population.
Although a mobile (mHealth) system to support self-management in chronic health conditions, iMHere, has been designed, piloted, and evaluated with adults primarily with SB (Dicianno et al., 2016; Dicianno, Henderson, & Parmanto, 2017; Fairman et al., 2013; Parmanto et al., 2013; Yu, Parmanto, Dicianno, & Pramana, 2015), this program does not appear optimal for AYA-SB. First, the app was designed for adults, who are likely already self-managing their condition. Second, during a randomized controlled trial, benefits of iMHere were only observed among high users of the system (Dicianno et al., 2016). Research on digital interface design indicates that adolescents and young adults (AYAs) not only exhibit distinct preferences in interface design and are typically more difficult to engage with new programs than older adults but are also quick to dismiss tools that do not meet their expectations (Loranger & Nielsen, 2013; Moran, 2016a, 2016b). The risks of BIT rejection/nonuse are greater among AYAs and can likely be prevented with appropriate design established through the identification of specific user needs.
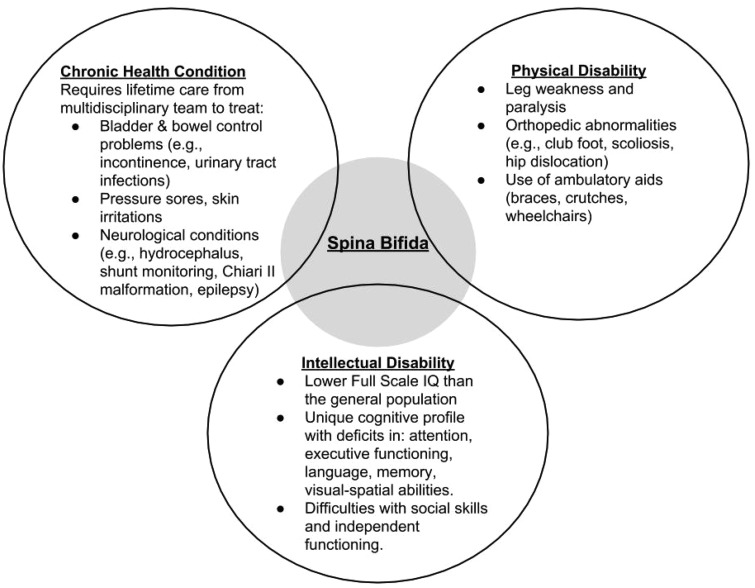
The specific needs of AYA-SB as users are likely unique, given the complex and distinct nature of this condition (Copp et al., 2015). SB is associated with considerable variability in motor, cognitive, and social functioning across individuals (Dennis, Landry, Barnes, & Fletcher, 2006). Indeed, self-management in SB focuses on several health-related tasks (e.g., medication, bowel regimen, and skin checks), which vary across individuals according to their symptom profile and needs. Given this variability in symptoms, work with AYA-SB may be informed by data from populations with (1) chronic health conditions, (2) physical and/or motor disabilities, and/or (3) intellectual disabilities, as SB comprises all three domains (see Figure 1 for a depiction of how SB overlaps with these three domains). Although a focus group for AYAs with brain and spinal cord anomalies revealed some initial user-reported needs for BITs (e.g., ease of use, provision of education, motivation, and ability to personalize; Bendixen, Fairman, Karavolis, Sullivan, & Parmanto, 2017), a comprehensive framework for BITs specific to self-management in SB has yet to be developed (Parmanto et al., 2013). Before designing and evaluating BITs to support self-management in AYA-SB, existing literature from similar populations must be synthesized to capture the user needs associated with the management of SB.
Figure 1.
Overlap of spina bifida with chronic health conditions, physical disabilities, and intellectual disabilities.
Note. IQ = intelligence quotient.
To achieve this aim, this study systematically reviewed the literature on interventions delivered via BITs designed to target AYAs with (1) chronic health conditions, (2) physical and/or motor disabilities, and (3) intellectual disabilities. The synthesis of these findings was used to propose a user needs model specific to promoting self-management in AYA-SB. A user needs model identifies what a BIT must be able to do for a specific group of users to have success (Kuniavsky, 2003). To ground the narrative of the proposed user needs model, the framework of the BIT model (Mohr et al., 2014) was used. Therefore, the purpose of the current review was to develop a model of likely user needs for AYA-SB that (1) promotes self-management during this time of transition and (2) is framed within the BIT model and informed from the synthesis of the behavioral and self-management intervention literature in conditions that have overlapping symptoms with youth with SB.
Method
Search Strategy
The search strategy was developed in collaboration with the lead author (C.S.S.) and a medical research librarian (Q.E.W.). The search strategy was adapted to the following databases: MEDLINE (Ovid), EMBASE (Elsevier), PsycINFO (EbscoHost), the Cochrane Library (Wiley), and Web of Science (Thomson Reuters). Each database was searched from the date of inception to April 2018 (See Supplementary Appendix). Non-peer-reviewed articles were excluded. In addition, the Cochrane Database of Systematic Reviews (Wiley) was searched for existing systematic reviews and protocols. Finally, reference lists of included studies were also reviewed to identify relevant citations. The review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher, Liberati, Tetzlaff, Altman, & PRISMA Group, 2009) and was registered before data extraction on the international prospective register of systematic reviews PROSPERO Web site (registration number CRD42018092342).
Inclusion and Exclusion Criteria
For inclusion in the review, studies had to (1) examine interventions aimed to target chronic health conditions, physical disabilities, or intellectual disabilities; (2) deliver the interventions via a BIT, including apps, short message service/text (SMS), Web site, and offline computer programs; (3) include participants between the ages of 12 and 25, as these ages would encompass AYAs (studies that were just outside of these age ranges, but were aimed at “adolescents” and/or “young adults,” were also included); (4) report outcomes relating to pediatric health or the management of a chronic condition, physical disability, or intellectual disability; and (5) be written in English. Conference abstracts, technical validation papers, and studies with samples fewer than 20 (to minimize pilot data) were excluded.
Study Selection
Literature search results were uploaded into Rayyan, an online software program that allows for reviewer collaboration during the study selection process (Ouzzani, Hammady, Fedorowicz, & Elmagarmid, 2016). Members of reviewer teams, comprising two reviewers out of six total reviewers, each independently screened the titles and abstracts from the initial search results against the inclusion criteria. Full-text articles were then also screened independently by two reviewers. Any discrepancies about inclusion were resolved through consensus.
Data Extraction
Reviewer teams extracted data (e.g., sample size and primary outcomes) independently and in duplicate from each eligible study using an online extraction form that was piloted with reviewers before formal data extraction. Discrepancies were again resolved through consensus.
Quality Assessment
The risk of bias was assessed using the Cochrane Collaboration’s tool for assessing risk of bias in randomized trials (Higgins et al., 2011). Risk of bias was evaluated for selection bias, performance bias, detection bias, attrition bias, and reporting bias.
Data Synthesis
A meta-analytic approach was not appropriate for this review owing to the variability in outcome measures, methodologies, and age ranges. Therefore, a systematic narrative synthesis framework was used. Three classifications were used to categorize and synthesize the data: chronic pediatric condition, physical disability, and intellectual disability. Each classification was framed under the BIT model. Specifically: (1) “Why” the BIT was created was identified through the specific aims of each intervention (e.g., target weight loss in youth with intellectual disabilities), (2) the “How” of achieving these clinical aims of the BITs was defined through the identification of behavioral change strategies (e.g., skill building and monitoring), (3) the “What” of instantiating the behavioral change strategies (i.e., transferring the theoretical aims into a technological product) was defined through identifying the technological elements of the BITs used in the studies (e.g., information delivery and passive data collection), (4) “How” the elements are displayed to a user was defined through the identification of technological characteristics (e.g., delivery platform and medium), and (5) “When” elements are delivered to a user was defined through workflows (i.e., the order in which elements are presented to users; Mohr et al., 2014). To capture as many relevant aspects of user needs for AYA-SB as possible, the systematic narrative synthesis also included support strategies, primary intervention outcomes, and usage and acceptability outcomes.
Results
Included Studies
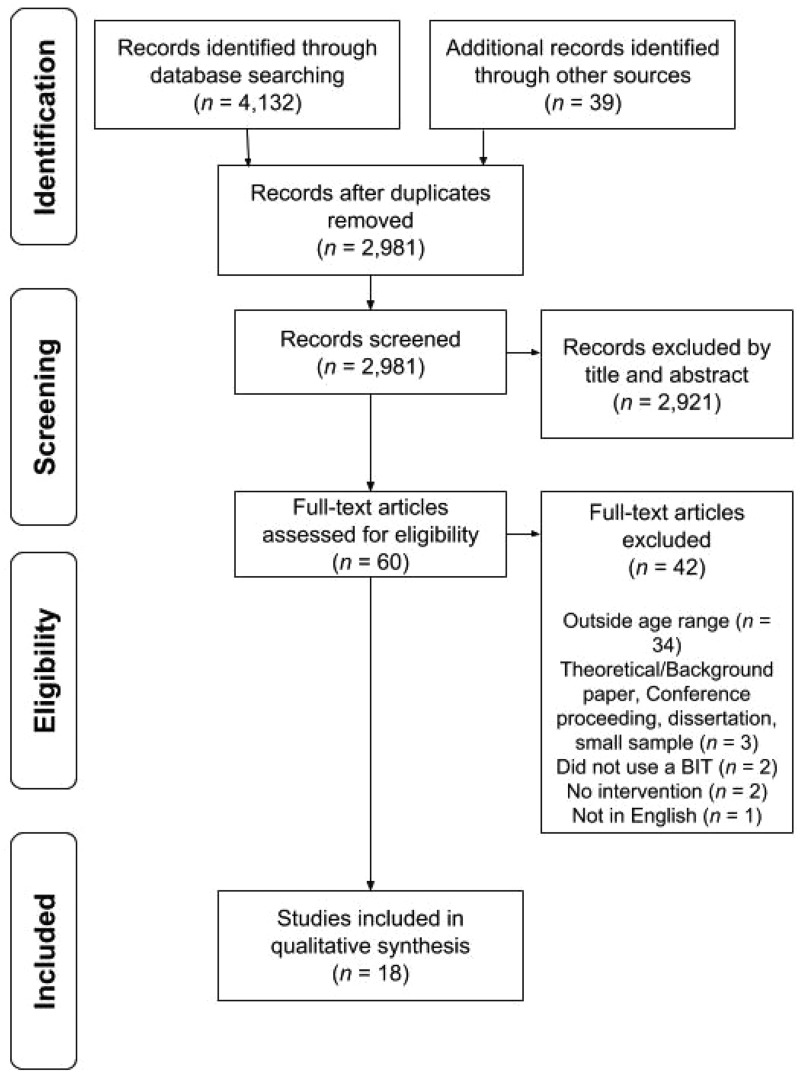
Two-thousand, nine-hundred and eighty-one article titles and abstracts were reviewed independently and in duplicate by two reviewers. Sixty full-text articles were reviewed for inclusion, with 18 included in the review for data extraction. See Figure 2 for the PRISMA flow diagram.
Figure 2.
PRISMA flow diagram for study inclusion.
Note. Adapted from “Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement,” by Moher et al. (2009).
Chronic Pediatric Conditions
Twelve studies targeted improvements in chronic pediatric conditions. Sample sizes ranged from 20 to 273, with the majority of participants being female and ranging in age from 11 to 18. All studies reported on primary and novel findings, with the exception of three reports of follow-up and secondary data analyses regarding an Internet-based cognitive behavioral therapy (I-CBT) intervention for chronic pain (Fisher et al., 2017; Law et al., 2017; Palermo et al., 2016).
Aims
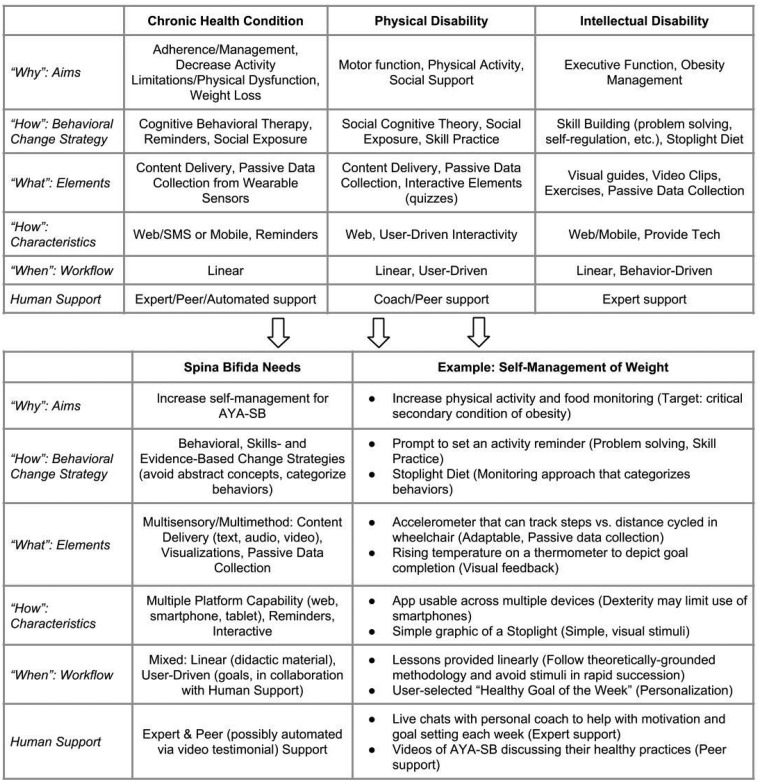
Figure 3 depicts the summary of findings framed within the BIT model. The aims of the chronic pediatric condition interventions included (1) delivering individualized treatment instructions and prompts for daily and acute asthma management (Mobile Asthma Action Plan [AAP]; Burbank et al., 2015), (2) decreased activity limitations and pain intensity in chronic pain (I-CBT; Fisher et al., 2017; Law et al., 2017; Palermo et al. 2015, 2016; Voerman et al., 2015), (3) reduction in physical dysfunction and school absence in chronic fatigue syndrome (Fatigue in Teenagers on the Internet [FITNET]; Nijhof et al., 2012), (4) increased adherence in diabetes (SuperEgo; Mulvaney et al., 2012; Newton et al., 2009), (5) improved sleep in insomnia (guided Internet therapy for insomnia [IT]; de Bruin et al., 2015), (6) self-management in juvenile idiopathic arthritis (iPeer2Peer; Stinson et al., 2016), and (7) weight loss in obesity (Loozit plus additional therapeutic contact [ATC]; Nguyen et al., 2013).
Figure 3.
User needs model for adherence in spina bifida informed by synthesized existing literature.
Note. SMS = short message service/text message. Adapted from “The behavioral intervention technology model: An integrated conceptual and technological framework for eHealth and mHealth interventions,” by Mohr et al. (2014).
Behavioral Change Strategies
The BITs were informed by the theoretical principles of CBT (58% of chronic pediatric condition BITs reviewed; see Table I); adherence reminders (25%), including messages tailored to overcome specific adherence barriers; disease-specific clinical practice/physician-informed guidelines (17%) for personalized asthma action plans; and peer mentorship and social exposure with AYAs with well-managed juvenile idiopathic arthritis (8%).
Table I.
Study Characteristics
| Authors, Year | Target Condition | BIT Name | Type of BIT | Human Support | Control Condition(s) | N | Age, % Female | Intervention, Follow-Up Durations |
|---|---|---|---|---|---|---|---|---|
| Chronic pediatric condition | ||||||||
| Burbank et al., 2015 | Asthma | AAP | Mobile app | No (A) | NR | 20 | 12–17, NR | 8 weeks, FU NR |
| de Bruin et al., 2015 | Insomnia | IT | Web-based | Yes | Waitlist and in-person group therapy | 116 | 12–19, 75% | 6 weeks, 2-month FU |
| Fisher et al., 2017a | Chronic pain | I-CBT | Web-based | Yes | Excluded from analyses | 138 dyads | 11–17, 78% | 8–10 weeks, 6- and 12-month FUs |
| Law et al., 2017a | Chronic pain | I-CBT | Web-based | Yes | Excluded from analyses | 138 dyads | 11–17, 78% | 8–10 weeks, 6- and 12-month FUs |
| Mulvaney et al., 2012 | Diabetes | SuperEgo | SMS, Web | No (A) | Age, sex, A1C matched subjects, Treatment as usual | 46 | 13–17, 53% | 3 months, FU NR |
| Newton et al., 2009 | Diabetes | NR | SMS | No (A) | Treatment as usual | 78 | 11–18, 53% | 12 weeks, FU NR |
| Nguyen et al., 2013 | Obesity | Loozit + ATC | SMS/ e-mail | Yes | In-person group sessions without SMS/e-mail ATC | 151 | 13–16, NR | Group sessions: 7 weeks; ATC: 24 months, FU NR |
| Nijhof et al., 2012 | Chronic fatigue syndrome | FITNET | Web-based | Yes | Treatment as usual | 135 dyads | 12–18, 82% | 6 months, 6- and 12-month FUs |
| Palermo et al., 2015 | Chronic pain | I-CBT | Web-based | Yes | Excluded from analyses | 135 | 11–17, 78% | 8–10 weeks, FU NR |
| Palermo et al., 2016a | Chronic pain | I-CBT | Web-based | Yes | Internet-delivered educational control | 273 dyads | 11–17, 75% | 8–10 weeks, 6-month FU |
| Stinson et al., 2016 | Juvenile idiopathic arthritis | iPeer2 Peer Program | Skype Video | Yes | Waitlist | 30 | 12–17, 97% | 8 weeks, FU NR |
| Voerman et al., 2015 | Chronic pain | Move It Now | Web-based | Yes | Excluded from analyses | 69 | 12–17, 77% | 7 weeks, 3-month FU |
| Physical disability | ||||||||
| de Mello Monteiro et al., 2014 | Cerebral palsy | NR | Virtual reality | No | Age, gender matched typically developing subjects | 64 | 11–28, 25% | 1 day, FU NR |
| Maher et al., 2010 | Cerebral palsy | Get Set | Web-based | Yes | Treatment as usual | 41 | 11––16, 37% | 8 weeks, 10- and 20-week post-baseline FU |
| Stewart et al., 2011 | Cerebral palsy and spina bifida | Ability Online | Web-based | Yes | None | 22 | 12–18, 45% | 6 months, 3-month FU |
| Intellectual disability | ||||||||
| Kurowski et al., 2013 | Traumatic brain injury | CAPS | Web-based | Yes | Internet resource comparison | 132 | 12–17, 35% (46) | 6 months, FU NR |
| Kurowski et al., 2014a | Traumatic brain injury | CAPS | Web-based | Yes | Internet resource comparison | 132 | 12–17, 35% (46) | 6, 12, and 18 months post-baseline FU |
| Ptomey et al., 2015 | Intellectual and developmental disabilities | Lose It! | Mobile app (tablet) | Yes | Conventional diet | 20 | 11–18, 45% | 8 weeks, FU NR |
Note. A = Automated Support; AAP = Mobile Asthma Action Plan; ATC = Additional Therapeutic Contact; BIT = Behavioral Intervention Technology; CAPS = Web-Based Counselor-Assisted Problem Solving; FU = Follow-Up; I-CBT = Internet Cognitive Behavioral Therapy; IT = Guided Internet Therapy; FITNET = Fatigue in Teenagers on the Internet; NR = Not Reported; SMART = Self-Management and Research Technology; SMS = Short Message Service (text message).
Follow-up or secondary data analyses.
Elements
The majority of studies used content delivery elements, such as electronically delivered lesson modules on a disease-related topic. Two studies (17%) reported the use of passive data collection to achieve aims.
Characteristics and Workflows
All interventions were delivered on a Web-based platform with a linear workflow (i.e., proceeded in a specific, uniform manner), with the exception of (1) AAP, which used a mobile app platform; (2) SuperEgo, which used SMS (text messaging) and a Web-based platform to edit alert options; (3) an unnamed SMS diabetes intervention, which used SMS-based delivery; (4) Loozit + ATC, which involved coaching via e-mail and SMS; and (5) the iPeer2Peer Program, which used Skype video.
Support Strategies
Nine studies (75%) included human support, including e-mail/electronic messages (see Table I), phone or video calls, and/or human-generated SMS messaging. All human support was conducted by professionals (i.e., pediatric therapist and dietician), with the exception of the iPeer2Peer Program, which connected peer mentors with juvenile idiopathic arthritis to participants via Skype video chat. AAP, SuperEgo, and an unnamed diabetes SMS intervention used automated support via SMS or the mobile app platform.
Primary Intervention Outcomes
Please see Supplementary Table S1 for study outcomes. The majority of studies used a control comparison group in reporting their findings, with the exception of five studies (42%): the AAP study did not enroll a control condition, three reports from the larger I-CBT study analyzed the treatment group only, and the Move It Now study dropped control comparisons owing to high attrition in the treatment group. Participants in 62.5% of the reviewed studies had significant changes in primary outcomes compared with control participants.
Usage and Acceptability Outcomes
Five studies (42%) did not report usage outcomes (e.g., number of launches and time used) of their evaluated BITs beyond reports of study attrition. The remaining studies varied considerably in their report of BIT usage, including module completion, logins to app/Web-page, duration of video calls, and number of messages sent or received. User acceptability was reported in some way by only half of the studies. Of these, SuperEgo was described as being evaluated with formal usability interviews and an unnamed usability and satisfaction measure, and the I-CBT program for chronic pain was described as being evaluated by an adapted version of the Treatment Evaluation Inventory Short Form. The remaining studies reported percentages of satisfaction without mention of formal evaluative processes.
Physical Disability
Three studies aimed to improve functioning in AYA populations with physical disabilities. Sample sizes ranged from 22 to 64, with the majority of participants being male and ranging in age from 11 to 28. All studies reported on primary and novel findings.
Aims
The three studies aimed to target (1) motor functioning in cerebral palsy (unnamed; de Mello Monteiro et al., 2014), (2) physical activity in cerebral palsy (Get Set; Maher et al., 2010), and (3) social support in cerebral palsy and SB (Ability Online; Stewart et al., 2011).
Behavioral Change Strategies
The BITs were theoretically informed by the principles of social cognitive theory (33%), peer mentorship and exposure (33%), and motor skill practice in a virtual environment (33%).
Elements
Get Set and Ability online used content delivery elements (66%), with Get Set also using quizzes, goal-setting, self-reflection, and positive role-modeling. The Get Set study also used passive data collection (i.e., distance walked). The motor functioning intervention for cerebral palsy relied on virtual reality.
Characteristics and Workflows
Get Set and Ability Online were designed to be delivered on a Web-based platform with a weekly, linear workflow (66%), whereas the motor functioning intervention for cerebral palsy was designed to be delivered during a single virtual reality session. Get Set also relied on interactive characteristics for its elements, which were user-driven in terms of workflow.
Support Strategies
Human support was included via coaching (i.e., one-on-one tour of the site and weekly e-mails/texts to promote adherence; level of training for the coaches was not reported) in Get Set and peer mentoring (mentors with cerebral palsy or SB participated in weekly chat room sessions) in Ability Online. No human support was provided in the virtual reality intervention.
Primary Intervention Outcomes
Ability Online was the only study to not use a control comparison (33%). Only the virtual reality intervention for motor functioning reported significant group differences following the intervention, with participants with cerebral palsy performing with less accuracy in timing compared with typically developing control participants, particularly when training tasks were abstract.
Usage and Acceptability Outcomes
Usage reports were again varied. Get Set use was described via median completed modules, whereas Ability Online use was described via mean group attendance (use of message boards and mail options were not reported). Use of the virtual reality program was not reported, but it is assumed that all participants completed all sessions. User acceptability was not reported by any study.
Intellectual Disability
Three studies describing two interventions (one follow-up article) were aimed at improving functioning in AYA populations with intellectual disabilities. Sample sizes ranged from 20 to 132, with the majority of participants being male and ranging in age from 11 to 18.
Aims
The targets of the included studies were executive functioning following traumatic brain injury (Web-based Counselor-Assisted Problem Solving [CAPS]; Kurowski et al., 2013, 2014) and obesity management in individuals with intellectual and developmental disabilities (Lose It!; Ptomey et al., 2015).
Behavioral Change Strategies
The BITs were theoretically informed by behavioral skill building (i.e., problem-solving, communication, and self-regulation skills) and the enhanced stoplight diet.
Elements
The CAPS study relied on educational materials via self-directed didactic content, with video clips (to model skills) and exercises to practice. The Lose It! study reported the use of visual guides (i.e., the stoplight diet) and passive physical activity data collection.
Characteristics and Workflows
The CAPS study (primary outcome and follow-up study) was designed to be deployed via a linear, Web-based platform. Lose It! was designed for mobile app deployment and was accessed by participants via a study-provided tablet device, and photo-assisted diet records were used to measure caloric intake. The Lose It! study was designed to have a repetitive workflow, which was driven by data entry (i.e., behavior-driven).
Support Strategies
Human support via a professional (i.e., psychologist for CAPS and registered dietician nutritionists for Lose It!) was provided for both interventions. Coaches in the CAPS intervention provided an initial face-to-face, in-home session to complete an assessment and guide the family in the use of the app. Subsequent coaching involved reviewing online didactic materials and engaging the family in problem-solving skills. Coaches in Lose It! provided weekly education sessions via Facetime.
Primary Intervention Outcomes
Control conditions were used in both interventions: an Internet resource comparison group for CAPS and a conventional diet group for Lose It! No group differences emerged in the CAPS study. However, older teens randomized to CAPS showed significant improvement compared with their older peers in the control condition. In the Lose It! study, intervention and control groups significantly improved in primary outcome targets without differences between groups, with one exception: energy intake reduced for those who used the Lose It! BIT.
Usage and Acceptability Outcomes
BIT use was depicted differently across the two interventions. The CAPS study described the average number of completed sessions without mention of the duration of sessions. The Lose It! study reported the average percentage of days with food and physical activity data tracked and the average percentage of completed coaching sessions. No reports of user acceptability were made in any of the studies.
Quality of Studies
As multiple study designs were eligible for inclusion, those studies that did not include randomization were labeled as having a high risk of selection bias (see Supplementary Table S2; Higgins et al., 2011). However, the majority had a low risk of selection bias (67%). Further, by nature of the interventions being delivered via BITs, blinding of allocation was difficult to maintain. This resulted in a good proportion of studies being at high or unclear risk of bias regarding performance (83%) and detection (61%). Although the majority of studies established a low attrition bias (67%), some studies reported difficulties with attrition, which likely impacted results. Finally, all studies were rated as having a low reporting bias.
Discussion
The current study aimed to synthesize the literature of BITs designed to target AYAs with chronic health conditions, physical and/or motor disabilities, and intellectual disabilities, and to propose a user needs model specific to AYA-SB. Studies meeting inclusion criteria were internationally representative (emanating from six different countries) and were primarily targeted at pediatric populations as opposed to AYAs or young adults, as the age ranges of excluded studies that included young adult populations tended to extend well into middle or late adulthood. The majority of included studies: (1) targeted the management of chronic health conditions (“Why”), (2) were informed by evidence-based treatments (“How”), (3) relied on content delivery (“What”), (4) were Web-based (“How”), (5) used linear or user-driven workflows (“When”), (6) included professional human support, and (7) were analyzed in comparison with a control condition. Unfortunately, BIT usage was inconsistently reported and was difficult to generalize. User acceptability of the evaluated BITs was reported by only one third of studies and typically did not involve validated usability interviews or questionnaires to assess this metric. Finally, given the nature of delivering an intervention via a BIT, risk of bias to elements of blinding were generally high.
Owing to the variability in outcome measures, methodologies, and reporting practices of the included studies, a meta-analytic approach was deemed inappropriate for this review. The systematic narrative synthesis approach indicated that the design, deployment, and engagement with most evaluated BITs resulted in acceptable usage and maintained or improved targeted symptoms during the intervention period. However, we are cautious to overinterpret the current findings without a meta-analytic approach to best understand the effect and strength of these interventions. Therefore, the remainder of the discussion focuses on the proposal of a user needs model for self-management in AYA-SB.
A Proposed User Needs Model for Adherence in AYA-SB
Figure 3 presents the synthesis of the current literature on BITs for chronic pediatric conditions, physical disability, and intellectual disability and the resultant summary of user needs for AYA-SB grounded within the BIT model (Mohr et al., 2014).
Aims
The aims of the included studies varied from executive function to weight loss, but all of these foci relate to issues that arise for AYA-SB and their self-management concerns. For example, activity limitations and decreased physical activity (Polfuss, Bandini, & Sawin, 2017), obesity (Polfuss et al., 2017), motor function difficulties (Copp et al., 2015), limited social support (Holmbeck et al., 2003), and executive functioning difficulties (Dennis et al., 2006) have all been noted for AYA-SB and are therefore directly related to their self-management (Psihogios, Murray, Zebracki, Acevedo, & Holmbeck, 2017). Thus, the included studies covered multiple domains that may impact self-management for AYA-SB and should therefore be considered for user needs in a BIT designed to improve self-management.
Behavioral Change Strategies
The synthesized literature used evidence-based theoretical approaches, clinical practice guidelines, or skills-based approaches to inform their designs. For youth with SB, the behavioral, skills-based approaches to target planning and problem-solving around self-management barriers highlighted particularly in the intellectual disability literature are indicated. Moreover, skills that are taught and reinforced through a BIT would need to be explicit and avoid abstract concepts that would require users to form meanings independently (owing to difficulties with assembled processing [learning to construct and digest information]; Dennis et al., 2006). For example, in problem-solving and planning for daily medication adherence, a BIT may engage an AYA-SB user with: “Your afternoon medication will be due when you are at school, would you like to set an alarm to remind you to get it from the nurse?”. Further, focusing on the associative processing (procedural learning) strength of perceiving categories (Copp et al., 2015), evidence-based education and monitoring approaches that can categorize behaviors (e.g., the use of the stoplight diet for obesity management in identifying green, yellow, and red food choices; Ptomey et al., 2015), would promote success in self-management of specific behaviors (e.g., diet monitoring). The use of evidence and skills-based strategies identified in the literature falls in line with typical cognitive processing in SB and with previous work calling for theoretically informed and longitudinal, evidence-based assessment and interventions to support individuals with SB (Holmbeck & Devine, 2010).
Elements
Given the frequent use of content delivery elements (e.g., electronically delivered lesson modules), passive data collection elements, interactive elements (e.g., quizzes), and visualizations, it is likely that users with AYA-SB would require a variety of elements to cover multiple treatment goals in the context of their varied symptom profile. Indeed, variable levels of impairment in hearing, vision, coordination, visuospatial processing, and motor dexterity in AYA-SB implicate a high number of possible BIT elements and a multisensory, multimethod approach (Pitchford, Kamchedzera, Hubber, & Chigeda, 2018). However, using a “kitchen sink” approach to element selection in response to these needs would be inappropriate. The reviewed studies used specific elements based on their intended population and targeted self-management behavior. Owing to posterior attention difficulties that impact the ability to focus and shift attention, AYA-SB would require a BIT that avoids high levels of stimuli in rapid succession (Dennis et al., 2006). This need makes the interaction of element selection and workflow particularly important for this population. Therefore, element needs are dependent on the behavioral change strategy (e.g., symptom monitoring).
The following is a series of possible elements for improving AYA-SB self-management. Owing to executive functioning problems, multistep instructions on how to use the technology, using simple visual stimuli, would be beneficial (e.g., “go through these steps to enter your catheterization schedule into the app”). Self-management psychoeducation, such as the specific disease-related topics highlighted in the literature, could be provided via electronic lessons with options for text (with large font for those with hearing difficulties), audio (for those with visual impairments), or video, promoting flexibility across intellectual functioning and visuospatial capacities. Lessons would also ideally be available in English and Spanish, given the higher prevalence of SB in Latino populations (Copp et al., 2015). Goal setting would be visual, with simple and large graphics indicating practical goals for users to set (e.g., choosing “green foods” to eat from the stoplight diet; Ptomey et al., 2015). Data collection relating to such goals would ideally be collected passively and with novel technologies (i.e., a pedometer was not highly used compared with an accelerometer in the reviewed literature) that allow for flexible recording capabilities (e.g., measuring activity by steps walked vs. distance cycled via wheelchair). Active data collection via data entry would ideally have dictation capabilities for those with issues of dexterity. Reminders for self-management behaviors and/or monitoring could be visual or auditory, based on user selection (e.g., text or spoken word stating: “Remember to drink water!”). Results of the data collection would also be visual, intuitively providing feedback on how well they achieved those goals over time (e.g., a rising temperature on a thermometer).
Characteristics
Although the majority of BITs described were Web-based, the complexity of these platforms was not well depicted; however, interactivity in design was highlighted (e.g., individual goal-setting capabilities). When users did not have access to the selected delivery platform, some studies provided the technology (i.e., tablet or smartphone; Burbank et al., 2015; Ptomey et al., 2015). Although Web-based platforms are indicated from the review, BITs capable of delivery via multiple platforms (e.g., an intervention portal that is accessible via the Web or a mobile device; notifications or reminders that users might select to have texted or appear in their notification tray on their smartphone) are likely required. This flexibility in characteristics would enable AYA-SB to use what best aligns with their functioning (e.g., motor dexterity might require some AYA-SB to use an app on a tablet device or computer, as opposed to a smartphone) and specific self-management needs (Psihogios, Kolbuck, & Holmbeck, 2015). Finally, the aesthetics of the characteristics will require formative and summative usability testing with AYA-SB users to ensure that these hypothesized characteristics are, in fact, in line with the user needs of this population (Mohr et al., 2014; Stiles-Shields & Montague, 2017).
Workflow
The mixed findings in the literature likely indicates that AYA-SB may benefit from a mixed workflow approach. For example, didactic materials might be offered linearly to follow a theoretically grounded methodology (Holmbeck & Devine, 2010), but also to limit high levels of stimuli in rapid succession (which would conflict with AYA-SB posterior attention difficulties; Dennis et al., 2006). Interactive or goal-setting elements could be ordered at the discretion of the user (e.g., selecting consistent skin checks as a primary goal for the week over other self-management behaviors), thus enabling personalization and engagement across the varied trajectories of development in AYA-SB (Psihogios, Kolbuck, & Holmbeck, 2015; Holmbeck et al., 2003). Flexible workflows could also be involved with human support, as indicated in the literature and discussed below.
Human Support Strategies
Although human support is not a specific part of the BIT model, support is associated with increased BIT adherence (Schueller, Tomasino, & Mohr, 2017) and warrants discussion in the context of AYA-SB user needs. Indeed, all but four studies included human support with their BITs, and three of these four studies still included automated support (which user may have assumed to be human-driven). Although automated or lay-person support in the use of BITs would likely be more efficient and cost-effective, the current studies overwhelmingly used professionals (e.g., psychologists and nutritionists). As AYA-SB have a complex, variable symptom profile requiring the management of multiple medical responsibilities, expert human support could help direct AYA-SB users to set specific goals related to their BIT use based on their unique symptomology. Further, expert human support could promote the use of scaffolding for users and further support those who may have cognitive impairments that impact learning. Of note, exposure to peer mentors with the same condition (i.e., arthritis, cerebral palsy, or SB) was also rated favorably in studies. AYA-SB are likely to have limited social exposure, generally and with other AYA-SB (Holmbeck & Devine, 2010); thus, they would benefit from this form of mentoring. However, enrolling and maintaining a staff of individuals with the same conditions as users likely has many barriers. Thus, a more feasible option to provide peer exposure for AYA-SB might involve the inclusion of video testimonials from other AYA-SB who have had success using the BITs. This practice has been well received in health apps for adults (Gilliam, Martins, Bartlett, Mistretta, & Holl, 2014; Schnall et al., 2015). Collectively, AYA-SB users would likely benefit from professional, human support in their use of BITs, coupled with some type of exposure to peer mentors.
Limitations
The current review and proposed model should be considered in the light of several limitations. First, the variability in methodologies and reporting strategies of the included studies precluded a meta-analytic approach to data synthesis. Second, the included studies had limited samples with young adults and limited racial and ethnic diversity, limiting the generalizability of the findings and conclusions to a broad, diverse AYA population. Although the cutoff of age 25 often excluded findings related to the larger literature of BITs for adult populations, this was done intentionally, as AYAs typically exhibit technology preferences distinct from older adult populations (Loranger & Nielsen, 2013; Moran, 2016a, 2016b). Third, the designs of the evaluated BITs were often not described in detail, and usability testing was seldomly reported. The user needs model is therefore lacking user requirements that would reflect multiple aesthetic and usability aspects (e.g., colors and readability) and is built upon the assumption that the participants found the evaluated BITs to be satisfactory and usable. Without knowing these metrics, it is unclear how accepted and used these BITs might be in open deployment (Stiles-Shields & Holmbeck, 2018). BITs designed from the currently proposed user needs for AYA-SB will require (1) formative usability testing, following an iterative design process (i.e., design, test, and design; Stiles-Shields & Montague, 2017), and (2) ongoing, summative usability testing (i.e., evaluation of a finished product) with validated measures (e.g., System Usability Scale; Brooke, 1996) during deployment. Finally, the proposed model is based on findings from literature bases that overlap with the symptom profile of AYA-SB. This proxy-based approach is merited, given the current gaps in the literature; however, user needs assessments, iterative usability testing, and evaluations of BITs specific to AYA-SB are needed.
Conclusion
BITs provide a unique opportunity to reach and promote self-management for AYA-SB, overcoming many noted access barriers unique to this population. Given the lack of evidence base around BITs for youth and young adults with SB, this review synthesized the current literature for AYAs with conditions that overlap with the complex symptom profile of SB. This information was then used to inform a proposed model of user needs for AYA-SB, under the framework of an established BIT model. However, additional research is needed to address the unique self-management needs of AYA-SB. From this, future iterations of BITs may therefore be designed, evaluated, and deployed.
Funding
This research was supported in part by grants from the National Institute of Nursing Research and the Office of Behavioral and Social Sciences Research (R01 NR016235), National Institute of Child Health and Human Development (R01 HD048629), and the March of Dimes Birth Defects Foundation (12-FY13-271). Dr. Emily Lattie is supported by a research grant from the National Institute of Mental Health (K08 MH112878).
Supplementary Material
Acknowledgments
The second through seventh authors contributed equally and are listed in alphabetical order.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Conflicts of interest: None declared.
References
- Bendixen R. M., Fairman A. D., Karavolis M., Sullivan C., Parmanto B. (2017). A user-centered approach: Understanding client and caregiver needs and preferences in the development of mHealth apps for self-management. JMIR Mhealth Uhealth, 5, e141.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz C. L., Smith K. A., Macias K., Bui K. (2014). Exploration of internet use: profile and preferences of transition-aged adolescents with spina bifida. Pediatric Nursing, 40, 173–178. [PubMed] [Google Scholar]
- Boudos R. M., Mukherjee S. (2008). Barriers to community participation: Teens and young adults with spina bifida. Journal of Pediatric Rehabilitation and Medicine, 1, 303–310. [PubMed] [Google Scholar]
- Brooke J. (1996). SUS: A “quick and dirty” usability scale In Jordan P. W., Thomas B., Weerdmeester B. A. (Eds.), Usability evaluation in industry (pp. 189–194). London, UK: Taylor & Francis. [Google Scholar]
- Burbank A. J., Lewis S. D., Hewes M., Schellhase D. E., Rettiganti M., Hall-Barrow J., Bylander L. A., Brown R. H., Perry T. T. (2015). Mobile-based asthma action plans for adolescents. Journal of Asthma, 52, 583–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copp A. J., Adzick N. S., Chitty L. S., Fletcher J. M., Holmbeck G. N., Shaw G. M. (2015). Spina bifida. Nature Reviews Disease Primers, 1, 15007.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin E. J., Bögels S. M., Oort F. J., Meijer A. M. (2015). Efficacy of cognitive behavioral therapy for insomnia in adolescents: A randomized controlled trial with internet therapy, group therapy and a waiting list condition. Sleep, 38, 1913–1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Mello Monteiro C. B., Massetti T., da Silva T. D., van der Kamp J., de Abreu L. C., Leone C., Savelsbergh G. J. (2014). Transfer of motor learning from virtual to natural environments in individuals with cerebral palsy. Research in Developmental Disabilities, 35, 2430–2437. [DOI] [PubMed] [Google Scholar]
- Dennis M., Landry S. H., Barnes M., Fletcher J. M. (2006). A model of neurocognitive function in spina bifida over the life span. Journal of the International Neuropsychological Society, 12, 285–296. [DOI] [PubMed] [Google Scholar]
- Dicianno B. E., Fairman A. D., McCue M., Parmanto B., Yih E., McCoy A., Pramana G., Yu D. X., McClelland J., Collins D. M., Brienza D. M. (2016). Feasibility of using mobile health to promote self-management in spina bifida. American Journal of Physical Medicine and Rehabilitation, 95, 425–437. [DOI] [PubMed] [Google Scholar]
- Dicianno B. E., Henderson G., Parmanto B. (2017). Design of mobile health tools to promote goal achievement in self-management tasks. JMIR Mhealth Uhealth, 5, e103.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dicianno B. E., Wilson R. (2010). Hospitalizations of adults with spina bifida and congenital spinal cord anomalies. Archives of Physical Medicine and Rehabilitation, 91, 529–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairman A. D., Dicianno B. E., Datt N., Garver A., Parmanto B., McCue M. (2013). Outcomes of clinicians, caregivers, family members and adults with spina bifida regarding receptivity to use of the iMHere mHealth solution to promote wellness. International Journal of Telerehabilitation, 5, 3–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher E., Bromberg M. H., Tai G., Palermo T. M. (2017). Adolescent and parent treatment goals in an internet-delivered chronic pain self-management program: Does agreement of treatment goals matter? Journal of Pediatric Psychology, 42, 657–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilliam M. L., Martins S. L., Bartlett E., Mistretta S. Q., Holl J. L. (2014). Development and testing of an iOS waiting room “app” for contraceptive counseling in a Title X family planning clinic. American Journal of Obstetrics and Gynecology, 211, 481e481. [DOI] [PubMed] [Google Scholar]
- Higgins J. P. T., Altman D. G., Gøtzsche P. C., Jüni P., Moher D., Oxman A. D., Savovic J., Schulz K. F., Weeks L., Sterne J. A.; Cochrane Bias Methods Group, Cochrane Statistical Methods Group. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343, d5928.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck G. N., Devine K. A. (2010). Psychosocial and family functioning in spina bifida. Developmental Disabilities Research, 16, 40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck G. N., Westhoven V. C., Phillips W. S., Bowers R., Gruse C., Nikolopoulos T., Totura C. M., Davison K. (2003). A multimethod, multi-informant, and multidimensional perspective on psychosocial adjustment in preadolescents with spina bifida. Journal of Consulting and Clinical Psychology, 71, 782–796. [DOI] [PubMed] [Google Scholar]
- Kuniavsky M. (2003). Observing the user experience: A practitioner's guide to user research. San Francisco, CA: Elsevier Science. [Google Scholar]
- Kurowski B. G., Wade S. L., Kirkwood M. W., Brown T. M., Stancin T., Taylor H. G. (2013). Online problem-solving therapy for executive dysfunction after child traumatic brain injury. Pediatrics, 132, e158–e166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurowski B. G., Wade S. L., Kirkwood M. W., Brown T. M., Stancin T., Taylor H. G. (2014). Long-term benefits of an early online problem-solving intervention for executive dysfunction after traumatic brain injury in children: A randomized clinical trial. JAMA Pediatrics, 168, 523–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law E. F., Fisher E., Howard W. J., Levy R., Ritterband L., Palermo T. M. (2017). Longitudinal change in parent and child functioning after internet-delivered cognitive-behavioral therapy for chronic pain. Pain, 158, 1992–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loranger H., Nielsen J. (2013). Teenage usability: Designing teen-targeted websites. Retrieved from https://www.nngroup.com/articles/usability-of-websites-for-teenagers/
- Maher C. A., Williams M. T., Olds T., Lane A. E. (2010). An internet-based physical activity intervention for adolescents with cerebral palsy: A randomized controlled trial. Developmental Medicine & Child Neurology, 52, 448–455. [DOI] [PubMed] [Google Scholar]
- Modi A. C., Marciel K. K., Slater S. K., Drotar D., Quittner A. L. (2008). The influence of parental supervision on medical adherence in adolescents with cystic fibrosis: Developmental shifts from pre to late adolescence. Children's Health Care, 37, 78–92. [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G.; PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLOS Medicine, 6, e1000097.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D. C., Burns M. N., Schueller S. M., Clarke G., Klinkman M. (2013). Behavioral intervention technologies: Evidence review and recommendations for future research in mental health. General Hospital Psychiatry, 35, 332–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D. C., Schueller S. M., Montague E., Burns M. N., Rashidi P. (2014). The behavioral intervention technology model: An integrated conceptual and technological framework for eHealth and mHealth interventions. Journal of Medical Internet Research, 16, e146.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran K. (2016a). Young adults appreciate flat design more than their parents do. Retrieved from https://www.nngroup.com/articles/young-adults-flat-design/
- Moran K. (2016b). Young adults/Millennials as web users (ages 18–25). Retrieved from https://www.nngroup.com/articles/young-adults-ux/
- Mulvaney S. A., Anders S., Smith A. K., Pittel E. J., Johnson K. B. (2012). A pilot test of a tailored mobile and web-based diabetes messaging system for adolescents. Journal of Telemedicine and Telecare, 18, 115–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton K. H., Wiltshire E. J., Elley C. R. (2009). Pedometers and text messaging to increase physical activity: Randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care, 32, 813–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen B., Shrewsbury V. A., O'Connor J., Steinbeck K. S., Hill A. J., Shah S., Kohn M. R., Torvaldsen S., Baur L. A. (2013). Two-year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight-loss maintenance: The Loozit randomized controlled trial. International Journal of Obesity, 37, 468–472. [DOI] [PubMed] [Google Scholar]
- Nijhof S. L., Bleijenberg G., Uiterwaal C. S., Kimpen J. L., van de Putte E. M. (2012). Effectiveness of internet-based cognitive behavioural treatment for adolescents with chronic fatigue syndrome (FITNET): A randomised controlled trial. Lancet, 379, 1412–1418. [DOI] [PubMed] [Google Scholar]
- Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. (2016). Rayyan—a web and mobile app for systematic reviews. Systematic Reviews, 5, 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T. M., Law E. F., Fales J., Bromberg M. H., Jessen-Fiddick T., Tai G. (2016). Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: A randomized controlled multicenter trial. Pain, 157, 174–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T. M., Law E. F., Zhou C., Holley A. L., Logan D., Tai G. (2015). Trajectories of change during a randomized controlled trial of internet-delivered psychological treatment for adolescent chronic pain: How does change in pain and function relate? Pain, 156, 626–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmanto B., Pramana G., Yu D. X., Fairman A. D., Dicianno B. E., McCue M. P. (2013). iMHere: A novel mHealth system for supporting self-care in management of complex and chronic conditions. JMIR Mhealth Uhealth, 1, e10.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitchford N. J., Kamchedzera E., Hubber P. J., Chigeda A. L. (2018). Interactive apps promote learning of basic mathematics in children with special educational needs and disabilities. Frontiers in Psychology, 9, 262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polfuss M., Bandini L. G., Sawin K. J. (2017). Obesity prevention for individuals with spina bifida. Current Obesity Reports, 6, 116–126. [DOI] [PubMed] [Google Scholar]
- Psihogios A. M., Kolbuck V., Holmbeck G. N. (2015). Condition self-management in pediatric spina bifida: A longitudinal investigation of medical adherence, responsibility-sharing, and independence skills. Journal of Pediatric Psychology, 40, 790–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psihogios A. M., Murray C., Zebracki K., Acevedo L., Holmbeck G. N. (2017). Testing the utility of a bio-neuropsychosocial model for predicting medical adherence and responsibility during early adolescence in youth with spina bifida. Journal of Pediatric Psychology, 42, 910–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ptomey L. T., Sullivan D. K., Lee J., Goetz J. R., Gibson C., Donnelly J. E. (2015). The use of technology for delivering a weight loss program for adolescents with intellectual and developmental disabilities. Journal of the Academy of Nutrition and Dietetics, 115, 112–118. [DOI] [PubMed] [Google Scholar]
- Schnall R., Mosley J. P., Iribarren S. J., Bakken S., Carballo-Diéguez A., Brown W. (2015). Comparison of a user-centered design, self-management app to existing mHealth apps for persons living with HIV. JMIR Mhealth Uhealth, 3, e91.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schueller S. M., Tomasino K. N., Mohr D. C. (2017). Integrating human support into behavioral intervention technologies: The efficiency model of support. Clinical Psychology: Science and Practice, 24, 27–45. [Google Scholar]
- Stewart M., Barnfather A., Magill-Evans J., Ray L., Letourneau N. (2011). Brief report: An online support intervention: Perceptions of adolescents with physical disabilities. Journal of Adolescence, 34, 795–800. [DOI] [PubMed] [Google Scholar]
- Stiles-Shields C., Holmbeck G. N. (2018). JPP student journal club commentary: Smartphone-delivered interventions for pediatric populations: Improving methodologies to address concerns of feasibility and efficacy. Journal of Pediatric Psychology, 43, 485–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles-Shields C., Montague E. (2017). Usability testing In Gellman M., Turner J. R. (Eds.), Encyclopedia of behavioral medicine. New York, NY: Springer. [Google Scholar]
- Stinson J., Ahola Kohut S., Forgeron P., Amaria K., Bell M., Kaufman M., Luca N., Luca S., Harris L., Victor C., Spiegel L. (2016). The iPeer2Peer program: A pilot randomized controlled trial in adolescents with Juvenile idiopathic arthritis. Pediatric Rheumatology, 14, 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voerman J. S., Remerie S., Westendorp T., Timman R., Busschbach J. J., Passchier J., de Klerk C. (2015). Effects of a guided internet-delivered self-help intervention for adolescents with chronic pain. Journal of Pain, 16, 1115–1126. [DOI] [PubMed] [Google Scholar]
- Yu D. X., Parmanto B., Dicianno B. E., Pramana G. (2015). Accessibility of mHealth self-care apps for individuals with spina bifida. Perspectives in Health Information Management, 12, 1h. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.