Abstract
Objective:
Sexual and gender minority (SGM) individuals are more likely to smoke than non-SGM individuals. It is unclear whether smoking cessation interventions for young adults are effective in the SGM population. The purpose of this study was to compare smoking cessation, other health risk behaviors, and intervention usability between SGM and non-SGM young adult smokers participating in a digital smoking cessation intervention trial.
Methods:
Young adult smokers (N = 500; 135 SGM) were assigned to a 90-day Facebook smoking cessation intervention (treatment) or referred to Smokefree.gov (control). Intervention participants were assigned to private Facebook groups tailored to their readiness to quit smoking. Participants reported their smoking status and other health risk behaviors at baseline, 3, 6, and 12 months. Usability of the intervention (i.e., perceptions of the intervention and treatment engagement) was assessed in the intervention group at 3 months.
Results:
Smoking cessation and intervention usability did not significantly differ between SGM participants and non-SGM participants. A greater proportion of SGM participants were at high risk for physical inactivity over the 12-month follow-up period (OR = 1.55, p = .005).
Conclusion:
SGM and non-SGM young adult smokers did not differ in their smoking cessation rates, perceptions of, or engagement in a digital intervention. Health risk behavior patterns were mostly similar; however, the disparity in physical activity between SGM and non-SGM smokers widened over time. Tailored interventions for SGM young adult smokers could increase focus on SGM experiences that can underlie multiple health risk behaviors, such as discrimination and the normativity of smoking.
Keywords: smoking cessation, young adults, Facebook, social media, sexual minorities
Despite advances in anti-smoking legislation and shifting social norms in the general population, tobacco use remains a major public health concern among sexual and gender minority identified (SGM) young adults (Centers for Disease Control and Prevention, 2017). Compared to non-SGM young adults, SGM individuals generally exhibit significantly higher rates of smoking (Lee, Griffin, & Melvin, 2009). Recent U.S. national estimates place rates of current smoking at 28.9% for gay men, 36.6% for bisexuals (of any gender), 27.4% for lesbian women, and 21– 35.5% for transgender people, compared to 14.6 – 20.2% for non-SGM individuals (Buchting, Emory, Scout, Kim, Fagan, Vera, & Emery, 2017; Emory, Kim, Buchting, Vera, Huang, & Emery, 2016; Hoffman, Delahanty, Johnson, & Zhao, 2018). Relatedly, SGM individuals are at elevated risk for serious health consequences that cannot be fully explained by higher smoking rates, such as respiratory illness (Blosnich, Jarrett, & Horn, 2010), asthma (Heck & Jacobson, 2006), and a weakened immune system (Fredriksen-Goldsen, Kim, Shui, & Bryan, 2017). In addition to smoking, SGM individuals are at greater risk for multiple health risk behaviors, such as poor diet, physical inactivity, poor sleep hygiene, unprotected sex, and substance abuse (Dai & Hao, 2017; Laska et al., 2015; Rosario et al., 2014; Smalley et al., 2016). There remains a need for interventions and resources that are effective for and well-received by SGM smokers.
There are several likely reasons for the ubiquity of smoking in the SGM community. First, smoking may be considered more normative and socially acceptable in SGM spaces. SGM social life often revolves around bars and clubs, which have traditionally served as safe spaces for socializing (Blosnich, Lee, & Horn, 2013), and smoking is common in SGM bars and nightclubs. Attending these venues is associated with higher odds of smoking (Holloway et al., 2012) and greater exposure to secondhand smoke (Fallin, Neilands, Jordan, & Ling, 2014). This may be partly due to the tobacco industry’s targeted advertising toward the SGM community in SGM bars and other social spaces (Dilley, Spigner, Boysun, Dent, & Pizacani, 2008). Although smoking has become less normative in many public and private spaces, largely due to social policies such as smokefree air laws (Cheng, Okechukwu, McMillen, & Glantz, 2015; Dinno & Glantz, 2009; Levy & Friend, 2003; McMullen, Brownson, Luke, & Chriqui, 2005), the tobacco industry’s targeted advertising is largely accepted in the SGM community and smoking is still considered normative (Smith, Thomson, Offen, & Malone, 2008).
Second, SGM individuals may experience chronic stressors, such as prejudice and discrimination, that are known to increase substance abuse risk. Specifically, the minority stress model posits that SGM individuals face chronic social stressors, both internal (e.g., internalized stigma, hypervigilance in social situations) and external (e.g., prejudice, discrimination) due to being members of a stigmatized group (Meyer, 2003). The connection between these stressors and smoking behavior has been well-supported by research involving both sexual minority (Blosnich & Horn, 2011) and gender minority (Gamarel et al., 2016) individuals. Specifically, experiencing chronic stressors as a member of a marginalized group is associated with increased likelihood of smoking. Minority stress also places SGM individuals at risk for other maladaptive health behaviors, such as substance abuse and unprotected sex, especially when they lack coping strategies and social support (Gonzales, Przedworski, & Henning-Smith, 2016; Shilo & Mor, 2014). Therefore, SGM smokers who want to improve their health may have a myriad of behaviors to confront in addition to their smoking.
If SGM individuals smoke for different reasons than their non-SGM counterparts and exhibit different patterns of multiple health risks, they may require different cessation interventions and resources. For instance, SGM-tailored interventions and resources could aim to provide coping strategies and social support for dealing with minority stress, and could address multiple health risk behaviors. Moreover, SGM smokers may perceive unique barriers to using existing interventions (Schwappach, 2008). For example, they may feel uncomfortable discussing triggers related to minority stress in a group setting, as such discussion would require disclosing their SGM status. Depending on general attitudes toward SGM individuals in their community, such disclosure may even be unsafe. Social media can be used to create a sense of community with other SGM individuals and is often viewed as a safe place to share personal experiences (Cannon et al., 2017; Chong, Zhang, Mak, & Pang, 2015). Indeed, SGM adults in the United States are more likely than non-SGM adults to have social media accounts, use Facebook daily, and use the Internet frequently (Harris Interactive, 2010; Pew Research Center, 2013; Seidenberg et al., 2017). Therefore, a social media-based intervention may be more accessible to SGM smokers than traditional face-to-face interventions.
Evidence suggests that SGM smokers prefer tailored interventions (e.g., Schwappach, 2008; Walls & Wisneski, 2010). Moreover, tailored interventions may be crucial to preventing the widening of health disparities that can occur from the widespread use of non-tailored interventions (Lee, Matthews, McCullen, & Melvin, 2014). Although such interventions are limited, the few that have been tested have demonstrated positive results. First, The Last Drag program consists of seven group sessions aimed at building social support and giving participants skills to quit smoking. A test of this program yielded a quit rate of 36–65% (depending on data imputation strategy), though these estimates should be interpreted with caution due to high attrition (52% lost to follow-up at 6 months; Eliason, Dibble, Gordon, & Soliz, 2012). Second, Matthews and colleagues reviewed a series of programs tailored to SGM smokers, all of which consisted of smoking cessation classes aimed at behavioral change and building social support. Approximately 32% of participants in these programs reported being smoke-free at the end of their program (Matthews, Li, Kuhns, Tasker, & Cesario, 2013). Importantly, neither study compared treatment outcomes between SGM and non-SGM participants.
Despite the success of these programs, tailoring interventions to specific groups of smokers may be unnecessarily inefficient, as SGM young adults may respond to non-tailored smoking cessation interventions equally as well as non-SGM young adults. To date, little research has examined the outcomes of non-tailored smoking cessation interventions among SGM smokers. Notably, Covey and colleagues found similar quit rates between gay/bisexual and heterosexual men involved in an 8-week smoking cessation intervention in New York City (Covey, Weissman, LoDuca, & Duan, 2009). Moreover, Grady and colleagues found similar quit rates between SGM and non-SGM smokers in two clinical trials in the San Francisco Bay Area (Grady, Humfleet, Delucchi, Reus, Muñoz, & Hall, 2014). However, these results may not generalize to: 1) interventions conducted online instead of in-person, 2) SGM smokers outside of coastal metropolitan areas, or 3) young adults.
First, online interventions and resources may be more beneficial for SGM than non-SGM smokers. Even in a non-tailored intervention, SGM smokers—especially young adults, who are accustomed to communicating online—may feel safer discussing their experiences online than face-to-face (Duggan, Ellison, Lampe, Lenhart, & Madden, 2015). Second, there may be a greater difference between SGM and non-SGM smokers outside of coastal metropolitan areas. Acceptance of SGM individuals in the United States is typically higher in major, coastal cities such as New York and San Francisco, where the aforementioned studies were conducted (Walther, Poston, & Gu, 2011). In other regions of the US, SGM smokers may feel less comfortable in non-tailored interventions, leading to lower treatment engagement and lower quit rates. Third, Grady and colleagues primarily studied middle-aged adults (M age for SGM participants = 45.77). Because young adults are generally less receptive to smoking cessation treatment (Curry, Sporer, Pugach, Campbell, & Emery, 2007), tailoring may be more important for young adults if it facilitates treatment engagement. Moreover, the aforementioned studies did not measure multiple health risk behaviors. Former smokers often turn to other negative coping mechanisms, such as overeating, to deal with stress (Chao, White, Grilo, & Sinha, 2016; Koopmann et al., 2011). In general, smokers are more likely than non-smokers to engage in other health risk behaviors (Zhang, Brook, Leukefeld, De La Rosa, & Brook, 2017); however, SGM smokers may have even higher risk due to minority stress.
In sum, it is unclear whether SGM and non-SGM individuals differ in their long-term patterns of smoking and other health risk behaviors, as well as their perceptions of a non-tailored smoking cessation intervention conducted entirely on social media. To date, nearly all smoking cessation interventions are conducted through in-person groups (see Baskerville et al., 2017 and Lee et al., 2014 for reviews). The efficacy of a non-tailored online group format needs to be assessed. Although SGM smokers prefer tailored interventions, the relative anonymity of the online environment may be sufficient to assuage privacy concerns and make the intervention content more accessible and effective. On the other hand, SGM smokers face serious obstacles to smoking cessation, such as minority stress and the presence of other health risk behaviors. Therefore, they may have poorer smoking outcomes and other health risk behaviors than non-SGM smokers. The purpose of the present investigation is to compare smoking cessation rates, other health risk behavior profiles, and usability of a Facebook-based digital intervention among SGM and non-SGM young adults from across the United States.
Method
Participants, Design, and Procedure
Participants were young adults (N=500) enrolled in a randomized controlled trial (RCT) of the Tobacco Status Project (TSP), a smoking cessation intervention for young adults delivered on Facebook with details of the intervention reported previously (Ramo et al., 2018; Ramo et al., 2015b). Participants were recruited from Facebook, using a paid ad campaign conducted between October 2014 and July 2015 with details reported previously (Ramo, Rodriguez, Chavez, Sommer, & Prochaska, 2014). Clicking on an ad redirected potential participants to a secure, confidential eligibility survey. Eligibility criteria included age (18–25 years old), ability to read and comprehend English, lifetime use of at least 100 cigarettes, current smoking (3+ days per week), and current Facebook use (4+ days per week). Eligible, consented participants verified their identity through email (i.e., sending a copy of a photo ID with their birth date to study staff) or Facebook (i.e., adding the study’s Facebook account as a “friend”). Participants were randomly assigned to the intervention or given a referral to smokefree.gov (control condition) using a blocked random assignment sequence generated by the study biostatistician (K.L.D.) and held by the senior author (D.E.R.). Randomization was stratified by daily smoking status (yes/no) and stage of change for quitting smoking (precontemplation, contemplation, preparation; DiClemente et al., 1991; Ramo et al., 2015a; Ramo et al., 2018).
Verified participants in the intervention conditions were assigned to “secret” (private) Facebook groups tailored to readiness to quit smoking (precontemplation, contemplation, preparation). Facebook posts were designed based on US Clinical Practice Guidelines and the Transtheoretical Model skills for smoking cessation (DiClemente et al., 1991; Fiore et al., 2008) and were posted to each group by study staff (1 post per day for 90 days). Participants also had the opportunity to participate in live, online counseling sessions. To promote engagement with the posts (i.e., commenting regularly), Facebook groups were randomly assigned to receive a monetary incentive for commenting on all 90 Facebook posts (daily, weekly, monthly, or no incentive, for a maximum of $90). All participants were compensated with a $20 gift card for completing each survey (baseline, 3 months, 6 months, 12 months). This research was approved by the University of California, San Francisco Institutional Review Board.
Measures
At baseline, 3 months, 6 months, and 12 months, participants completed an online survey using Qualtrics software. Relevant measures for the present study are described below.
Sexuality and gender identity.
Participants were classified as SGM or non-SGM at baseline using a two-item measure. The sexual orientation item asked, “Do you identify as: straight (heterosexual), lesbian/gay (homosexual), bisexual, or not listed (please specify)”. The gender identity item asked, “Are you: male, female, transgender”. Participants who reported identifying as straight and male or female were classified as non-SGM. Participants who identified as a sexual minority (i.e., lesbian/gay, bisexual, or other) and/or gender minority (i.e., transgender) were classified as SGM.
Abstinence from smoking.
Seven-day point-prevalence abstinence from smoking was assessed at 3 months, 6 months, and 12 months. Participants answered, “How many cigarettes have you smoked in the past 7 days?”. Those who reported having smoked zero cigarettes were considered abstinent.
Health risk behaviors.
At each timepoint, participants reported their risk level for 9 behaviors, derived from the Staging Health Risk Assessment (S-HRA, developed by Pro-Change Behavior Systems, South Kingstown, RI): physical inactivity, high-fat diet, low fruit and vegetable intake, poor stress management, heavy alcohol use, marijuana use, illicit drug use, unprotected sex, and poor sleep hygiene. Sample items include, “Do you eat at least 4.5 cups of fruits and vegetables per day?”, “Do you effectively practice stress management in your daily life?”, and “Do you eat a diet that is low in fat?”. Terminology was defined for each question. Response options were written based on the Transtheoretical Model to reflect participants’ stages of change (i.e., “No, and I do not intend to [change] in the next 6 months”, “No, but I intend to [change] in the next 6 months”, “No, but I intend to [change] in the next 30 days”, “Yes, I have been [engaging in the behavior], but for less than 6 months”, and “Yes, I have been [engaging in the behavior] for more than 6 months”). Response options were adapted to fit each question. Responses were recoded into high-risk (i.e., currently engaging in a risky behavior or not currently engaging in a healthy behavior) and low-risk.
Usability of the intervention.
As part of the 3-month survey, participants in the intervention group reported whether the intervention was easy to understand, gave sound advice, gave them something to think about, and helped them to be healthier, as well as whether they used the information, thought about the information, and would recommend the intervention (1 = strongly disagree, 4 = strongly agree; Ramo et al., 2015a). Sample items include, “The posts were easy to understand”, “I would recommend this program to others”, and “The posts gave me something new to think about”. Responses were dichotomized into disagreement (1–2) or agreement (3–4). Although participants in the control group answered analogous questions about smokefree.gov, only the treatment group was used in analyses. Engagement was measured by the number of comments participants in the treatment group posted on Facebook during the 90-day intervention, including comments on the daily posts, user-generated posts, live counseling sessions, and live CBT sessions.
Analyses
Analyses compared smoking abstinence, other health risk behaviors, and usability of the intervention between SGM and non-SGM participants. All analyses included experimental condition (treatment or control) in the analytic model, with the exception of analyses conducted only on the treatment group (i.e., usability). Because SGM and non-SGM participants did not significantly differ in proportions assigned to each monetary incentive condition (χ2 (3) = .62, p = .89), analyses did not control for this group-level variable. Generalized estimating equations with binary distributions and logit link functions were used to compare both 7-day reported abstinence from smoking and the 9 other health risk behaviors between SGM and non-SGM participants at 3, 6, and 12 months.
At baseline, SGM and non-SGM participants were compared on number of cigarettes smoked per day, daily smoking, years of smoking, and past year quit attempts using chi-square tests of independence. SGM and non-SGM participants were also compared on the nine health risk behaviors at baseline using logistic regression analyses. Variables on which SGM and non-SGM participants differed at baseline were entered as covariates in relevant analyses.
Two sets of analyses were conducted on the treatment group only. First, an independent samples t-test was used to compare engagement in the intervention, as measured by the number of comments, between SGM and non-SGM participants. Second, a series of logistic regression analyses compared SGM- and non-SGM participants’ perceptions of the intervention. Endorsement of each statement (agree/strongly agree or disagree/strongly disagree) was regressed on SGM status.
Results
Baseline Characteristics
There were 251 participants in the intervention condition and 249 in the control condition. The gender makeup of the sample was 54.6% female, 44.8% male, and 0.6% transgender. The racial makeup was 73.8% non-Hispanic White, 6.9% Hispanic, 2.6% Black, 1.0% American Indian or Alaskan Native, 1.2% Asian or Pacific Islander, and 14.5% multiple races. Participants were distributed throughout the United States (32.4% located in the South, 29.2% in the Midwest, 15.4% in the Northeast, and 22.7% in the West). The sample was 27.0% SGM (n = 135) and 73.0% non-SGM (n = 365). There were no significant differences on smoking characteristics between SGM and non-SGM participants (Table 1). SGM participants were more likely to be at high risk for poor sleep hygiene (OR = 1.84, 95% CI [1.14, 2.96], p = .01), and less likely to be at high risk for a high-fat diet (OR = .54, 95% CI [.32, .90], p = .02). The proportions of participants in the intervention and control conditions did not significantly differ between SGM (55.6%, n = 75) and non-SGM participants (48.2%, n = 176; χ2 (1) = 2.28, p = .13).
Table 1.
Baseline smoking characteristics of SGM and non-SGM participants
| SGM % (N) n = 135 | Non-SGM % (N) n = 365 | |
|---|---|---|
| Cigarettes per day | ||
| 10 or less | 54.1% (73) | 45.8% (167) |
| 11–20 | 40.0% (54) | 49.0% (179) |
| 21–30 | 4.4% (6) | 3.8% (14) |
| 30 or more | 1.5% (2) | 1.4% (5) |
| Daily smoking (% daily smokers) | 84.4% (114) | 87.4% (319) |
| Years of smoking | ||
| Less than 1 year | 8.9% (12) | 9.0% (33) |
| 1 year | 3.7% (5) | 3.8% (14) |
| More than 1 year | 87.4% (118) | 87.1% (318) |
| Past year quit attempt (% yes) | 65.9% (89) | 60.8% (222) |
Abstinence from Smoking
Reported abstinence rates were 8.6% for SGMs and 11.2% for non-SGMs at 3 months, 18.8% for SGMs and 15.4% for non-SGMs at 6 months, and 20.0% for SGMs and 21.6% for non-SGMs at 12 months. SGMs and non-SGMs did not significantly differ in abstinence from smoking over the 12-month follow-up period (OR = 0.95, 95% CI [.59, 1.52], p = .83). See Figure 1a.
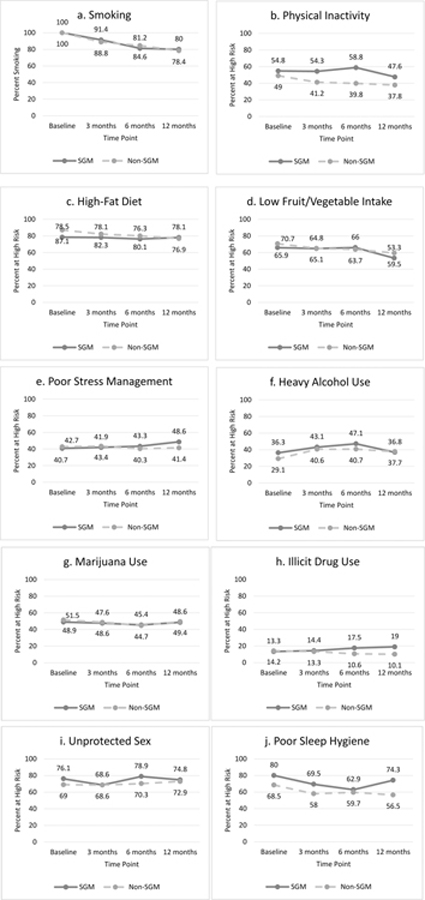
Figure 1.
Change in health risk behaviors over time for SGM and non-SGM participants.
Health Risk Behaviors over 12 Months
SGM participants were more likely to be at high risk for physical inactivity than non-SGM participants (OR = 1.55, 95% CI [1.14, 2.10], p = .005). They were more likely to be at high risk for poor sleep hygiene (OR = 1.67, 95% CI [1.22, 2.27], p = .001) than non-SGM participants, but the relationship became nonsignificant when adjusting for baseline risk (p = .075). The likelihood of being at high risk for the other 6 behaviors measured (high-fat diet, low fruit and vegetable consumption, poor stress management, heavy alcohol use, marijuana use, and illegal drug use) did not differ between SGMs and non-SGMs over the 12-month period (p’s > .05, see Figure 1b–1j).
Post-Treatment Usability of the Intervention
Results showed that SGM (M = 42.85, SD = 45.31) and non-SGM (M = 32.66, SD = 41.20) participants did not significantly differ in number of comments posted (t[249] = −1.74, p = .08, d = .24). SGM and non-SGM participants did not differ in their perceptions of the intervention (p’s > .05, see Table 2).
Table 2.
SGM and non-SGM participants’ perceptions of the intervention (treatment condition)
| SGM % agree or strongly agree (n = 105) | Non-SGM % agree or strongly agree (n = 250) | |
|---|---|---|
| Easy to understand | 85.7 | 81.2 |
| Gave sound advice | 81.9 | 78.4 |
| Helped me be healthier | 53.3 | 50.4 |
| Used the information | 61.9 | 61.2 |
| Would recommend intervention | 76.2 | 76.8 |
| Gave me something to think about | 72.4 | 72.0 |
| Thought about the information | 78.1 | 74.8 |
Note: Percentages are of participants who completed the usability measures
Discussion
This study was among the first to directly compare quit rates between SGM and non-SGM smokers in a non-tailored smoking cessation intervention. It expanded upon prior work (Baskerville et al., 2017, and Lee et al., 2014 for reviews) by recruiting a geographically diverse sample of young adult smokers in the United States, delivering a theory-driven intervention entirely on Facebook, and examining multiple health risk behaviors. SGM and non-SGM participants were compared on three outcomes of interest: abstinence from smoking, other health risk behaviors, and usability of the intervention.
First, consistent with prior research (Covey et al., 2009; Grady et al., 2014), results revealed no significant differences in smoking abstinence between SGM and non-SGM smokers. For both groups, abstinence rates increased over time, culminating in 20% abstinence for SGM participants (21.6% for non-SGM participants) 12 months after the start of the intervention. This suggests that the intervention was equally effective for SGM young adults, despite the fact that it was not tailored. This may have been partly due to the medium through which the intervention was delivered. Young adults (both SGM and non-SGM) may feel comfortable discussing their experiences and meeting new people online, as most young adults regularly use social media to communicate (Duggan et al., 2015). It is important to note that quit rates in follow-up surveys were higher in two tailored interventions (Eliason et al., 2012; Matthews et al., 2013) than in the present study. However, smokers in these studies were older (M age = 40.48 and 44.5) and greater proportions were ready to quit. The quit rates found in this study are comparable to those of other smoking cessation intervention trials targeting young smokers varying in readiness to quit (e.g., Prochaska et al., 2015; Redding et al., 2015). It is unclear whether an intervention tailored to SGM young adults, many of whom are not ready to quit smoking, would have produced higher quit rates.
Second, SGM and non-SGM participants had mostly similar health behavioral risk profiles over the 12-month follow-up period. This is encouraging, as it suggests that SGM-tailored smoking cessation interventions may not need to specifically address a wide variety of behaviors. Spreading the focus on an intervention too thinly may have hampered the delivery of information in a programmatic, comprehensible way. A tailored smoking cessation intervention, however, may still be a useful outlet for addressing some common underlying causes of smoking and other health risk behaviors. Prior research has suggested that a lack of social support and lack of healthy coping strategies influence SGM individuals’ higher rates of multiple health risk behaviors (Gonzales et al., 2016; Shilo & Mor, 2014). A tailored intervention, even one that does not explicitly focus on changing multiple health risk behaviors, may provide SGM smokers with a community of individuals who can support one another in quitting smoking, as well as coping strategies for dealing with minority stress. Although the intervention content did address a variety of coping strategies for common issues associated with smoking cessation, such as weight gain and feeling stressed, these coping strategies were not specific to issues such as prejudice and discrimination. Compared to their non-SGM peers, SGM young adult smokers may need more support and/or targeted coping strategies to substantially reduce other health risks. Indeed, SGM participants were more likely than non-SGM participants to be at high risk for physical inactivity over the 12-month follow-up period, despite a lack of significant baseline differences. This finding is consistent with research comparing heterosexual to non-heterosexual college students’ physical activity (Laska et al., 2015; VanKim, Erickson, Eisenberg, Lust, Rosser, & Laska, 2015), and it suggests that similar patterns may be found in the general population of young adults. In addition to presenting physical activity as a strategy for reducing the likelihood of weight gain after quitting smoking, a tailored intervention could focus more specifically on the underlying causes of a multitude of health risk behaviors in the SGM community.
Third, the present intervention was equally well-received by SGM and non-SGM smokers. Moreover, they had similar engagement in the intervention (as measured by their comments on the study’s Facebook posts). This suggests that SGM smokers found the study’s Facebook posts relevant and felt comfortable commenting on them, regardless of the sexual orientation and/or gender identity of their other group members. The online environment may have facilitated a high level of comfort in this sample of young adults (Duggan et al., 2015). However, perceptions of and engagement in the intervention may be further improved by tailoring, as past research has shown that SGM smokers generally prefer tailored interventions (Schwappach, 2008; Walls & Wisneski, 2010).
Overall, the results of this study suggest that Facebook is a promising medium for delivering a smoking cessation intervention to both SGM and non-SGM young adults. Digital interventions address many of the issues that may have traditionally made smoking cessation treatment less accessible to SGM smokers. First, social media is already an integral part of the daily lives of SGM individuals, with 80% of SGM people reporting having at least one social media account (compared to 58% of the general public; Pew Research Center, 2013). Digital interventions are delivered in a way that is familiar, comfortable, and convenient to many SGM smokers. Second, digital interventions may assuage privacy concerns that could prevent SGM smokers from participating in face-to-face groups. Third, digital interventions can reach smokers from underserved areas. Smokers in rural areas who want to quit smoking face multiple obstacles, including communal smoking norms and a lack of health services (Carlson et al., 2012; Hutcheson et al., 2008). Due to relatively lower acceptance of SGMs in many rural areas of the United States (Walther et al., 2011), rural SGM smokers may be less likely to engage in treatment even when it is available. Digital interventions connect these individuals to both the intervention content and to other SGM smokers who can provide social support. Although the increased disparity in physical inactivity over time is a concern that could be addressed in a tailored intervention, a Facebook-based intervention appears to be equally well-received, engaging, and effective for SGM and non-SGM young adult smokers.
Limitations and Future Directions
The present work had a few notable limitations. First, the efficacy of this digital intervention was not directly compared to that of an offline intervention. Although results suggest that the non-tailored digital intervention was equally effective for SGM and non-SGM smokers, it is unclear whether this pattern of results is specific to digital interventions. Grady and colleagues (2014) found similar results with offline interventions; however, young adults may be more willing to engage in digital compared to offline interventions. In addition to counting comments, a content analysis of participants’ comment content and how it may differ between SGM and non-SGM participants would be informative. Second, the present research did not address potential differences in reasons for smoking (e.g., minority stress, different social norms) between SGM and non-SGM smokers. These differences, if identified in future research, could inform tailored interventions to further improve quit rates among SGM smokers. Third, results may not generalize to age groups other than young adults. Young adults are among the heaviest users of social media (Duggan et al., 2015), making Facebook an ideal platform for delivering interventions to young adults. Non-digital interventions may or may not be better suited for older smokers. Moreover, identifying as SGM is now more common and more accepted among young adults than older adults (Gates & Newport, 2012), which may increase SGM smokers’ level of comfort with non-tailored interventions.
Implications and Conclusions
Results of this study showed that a non-tailored Facebook-based smoking cessation intervention for young adults, the Tobacco Status Project, was equally effective for and well-received by SGM and non-SGM smokers. However, SGM smokers were more likely to be at high risk for physical inactivity during the follow-up period. Interventions tailored to the SGM community may produce higher quit rates and could further improve SGM health by addressing physical inactivity and other health risk behaviors. Social media appear to be a promising tool for delivering smoking cessation interventions to young SGM smokers across the United States.
Acknowledgements
This study and preparation of this manuscript were supported by the National Institute on Drug Abuse (K23 DA032578, P50 DA09253, and T32 DA007250). The funding source did not have any further role in study design, in the collection, analysis, and interpretation of data, in the writing of the report, or in the decision to submit the paper for publication. DR has provided consultation to Carrot Inc., which makes a tobacco cessation device. All other authors have no financial disclosures.
References
- Baskerville NB, Cash D, Shuh A, Wong K, Abramowicz A, Yessis J, & Kennedy RD (2017). Tobacco use cessation interventions for lesbian, gay, bisexual, transgender and queer youth and young adults: A scoping review. Preventive Medicine Reports, 16, 53–62. doi: 10.1016/j.pmedr.2017.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blosnich JR, & Horn K (2011). Associations of discrimination and violence with smoking among emerging adults: Differences by gender and sexual orientation. Nicotine & Tobacco Research, 13, 1284–1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blosnich J, Jarrett T, & Horn K (2010). Disparities in smoking and acute respiratory illnesses among sexual minority young adults. Lung, 188, 401–407. [DOI] [PubMed] [Google Scholar]
- Blosnich J, Lee JGL, & Horn K (2013). A systematic review of the aetiology of tobacco disparities for sexual minorities. Tobacco Control, 22, 66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchting FO, Emory KT, Scout, Kim Y, Fagan P, Vera LE, & Emery S (2017). Transgender use of cigarettes, cigars, and e-cigarettes in a national study. American Journal of Preventive Medicine, 53, e1–e7. doi: 10.1016/j.amepre.2016.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson LE, Lounsberry JJ, Maciejewski O, Wright K, Collacutt V, & Taenzer P (2012). Telehealth-delivered group smoking cessation for rural and urban participants: Feasibility and cessation rates. Addictive Behaviors, 37, 108–114. [DOI] [PubMed] [Google Scholar]
- Cannon Y, Speedlin S, Avera J, Robertson D, Ingram M, & Prado S (2017). Transition, connection, disconnection, and social media: Examining the digital lived experiences of transgender individuals. Journal of LGBT Issues in Counseling, 11, 68–87. [Google Scholar]
- Centers for Disease Control and Prevention (2017, February 28). Tobacco-Related Disparities: LGBT and Tobacco Use Retrieved from https://www.cdc.gov/tobacco/disparities/lgbt/index.htm
- Chao AM, White MA, Grilo CM, & Sinha R (2017). Examining the effects of cigarette smoking on food cravings and intake, depressive symptoms, and stress. Eating Behavior, 24, 61–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng KW, Okechukwu CA, McMillen R, & Glantz SA (2015). Association between clean indoor air laws and voluntary smokefree rules in homes and cars. Tobacco Control, 24, 168–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong ES, Zhang Y, Mak WW, & Pang IH (2015). Social media as social capital of LGB individuals in Hong Kong: its relations with group membership, stigma, and mental well-being. American Journal of Community Psychology, 55, 228–238. [DOI] [PubMed] [Google Scholar]
- Covey LS, Weissman J, LoDuca C, & Duan N (2009). A comparison of abstinence outcomes among gay/bisexual and heterosexual male smokers in an intensive, non-tailored smoking cessation study. Nicotine & Tobacco Research, 11, 1374–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry SJ, Sporer AK, Pugach O, Campbell RT, & Emery S (2007). Use of tobacco cessation treatments among young adult smokers: 2005 National Health Interview Survey. American Journal of Public Health, 97, 1464–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H, & Hao J (2017). Sleep deprivation and chronic health conditions among sexual minority adults. Behavioral Sleep Medicine Advance online publication. [DOI] [PubMed]
- DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, & Rossi JS (1991). The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. Journal of Consulting and Clinical Psychology, 59, 295–304. [DOI] [PubMed] [Google Scholar]
- Dilley JA, Spigner C, Boysun MJ, Dent CW, & Pizacani BA (2008). Does tobacco industry marketing excessively impact lesbian, gay, and bisexual communities? Tobacco Control, 17, 385–390. [DOI] [PubMed] [Google Scholar]
- Dinno A, & Glantz S (2009). Tobacco control policies are egalitarian: a vulnerabilities perspective on clean indoor air laws, cigarette prices, and tobacco use disparities. Social Science & Medicine, 68, 1439–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan M, Ellison NB, Lampe C, Lenhart A, & Madden M (2015, January 9). Social media update 2014. Pew Research Center Retrieved from: http://www.pewinternet.org/2015/01/09/social-media-update-2014/
- Eliason MJ, Dibble SL, Gordon R, & Soliz GB (2012). The Last Drag: An evaluation of an LGBT-specific smoking intervention. Journal of Homosexuality, 59, 864–878. [DOI] [PubMed] [Google Scholar]
- Emory K, Kim Y, Buchting F, Vera L, Huang J, & Emery LS (2016). Intergroup variance in lesbian, gay, and bisexual tobacco use behaviors: Evidence that subgroups matter, notably bisexual women. Nicotine & Tobacco Research, 18, 1494–1501. 10.1093/ntr/ntv208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallin A, Neilands TB, Jordan JW, & Ling PM (2014). Secondhand smoke exposure among young adult sexual minority bar and nightclub patrons. American Journal of Public Health, 104, e148–e153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, …& Wewers ME (2008). Treating tobacco use and dependence: 2008 update, clinical practice guideline Rockville, MD: U. S. Department of Health and Human Services Public Health Service. [Google Scholar]
- Fredriksen-Goldsen KI, Kim H, Shui C, & Bryan AEB (2017). Chronic health conditions and key health indicators among lesbian, gay, and bisexual older US adults, 2013–2014. American Journal of Public Health, 107, 1332–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamarel KE, Mereish EH, Manning D, Iwamoto M, Operario D, & Nemoto T (2016). Minority stress, smoking patterns, and cessation attempts: Findings from a community-sample of transgender women in the San Francisco Bay Area. Nicotine & Tobacco Research, 18, 306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates GJ, & Newport F (2012, October 18). Special report: 3.4% of U.S. adults identify as LGBT. Gallup News Retrieved from: http://news.gallup.com/poll/158066/special-report-adults-identify-lgbt.aspx
- Gonzales G, Przedworksi J, & Henning-Smith C (2016). Comparison of health and health risk factors between lesbian, gay, and bisexual adults and heterosexual adults in the United States: Results from the National Health Interview Survey. JAMA Internal Medicine, 176, 1344–1351. [DOI] [PubMed] [Google Scholar]
- Grady ES, Humfleet GL, Delucchi KL, Reus VI, Muñoz RF, & Hall SM (2014). Smoking cessation outcomes among sexual and gender minority and nonminority smokers in extended smoking treatments. Nicotine & Tobacco Research, 16, 1207–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Interactive Harris (2010, July 13). Gay and lesbian young adults are more likely and more frequent blog readers. PR Newswire Retrieved from http://www.prnewswire.com/news-releases/gay-and-lesbian-adults-are-more-likely-and-more-frequent-blog-readers-98317299.html
- Heck JE, & Jacobson JS (2006). Asthma diagnosis among individuals in same-sex relationships. Journal of Asthma, 43, 579–584. [DOI] [PubMed] [Google Scholar]
- Hoffman L, Delahanty J, Johnson SE, & Zhao X (2018). Sexual and gender minority cigarette smoking disparities: An analysis of 2016 Behavioral Risk Factor Surveillance System Data. Preventive Medicine, 113, 109–115. [DOI] [PubMed] [Google Scholar]
- Holloway IW, Traube DE, Rice E, Schrager SM, Palinkas LA, Richardson J, & Kipke MD (2012). Community and individual factors associated with cigarette smoking among young men who have sex with men. Journal of Research on Adolescence, 22, 199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutcheson TD, Greiner KA, Ellerbeck EF, Jeffries SK, Mussulman LM, & Casey GN (2008). Understanding smoking in rural communities. The Journal of Rural Health, 24, 116–124. [DOI] [PubMed] [Google Scholar]
- Koopmann A, Dinter C, Grosshans M, von der Goltz C, Hentschel R, Dahmen N, …& Kiefer F (2011). Psychological and hormonal features of smokers at risk to gain weight after smoking cessation – Results of a multicenter study. Hormones and Behavior, 60, 58–64. [DOI] [PubMed] [Google Scholar]
- Laska MN, VanKim NA, Erickson DJ, Lust K, Eisenberg ME, & Rosser BR (2015). Disparities in weight and weight behaviors by sexual orientation in college students. American Journal of Public Health, 105, 111–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JG, Griffin GK, & Melvin CL (2009). Tobacco use among sexual minorities in the USA, 1987 to May 2007: A systematic review. Tobacco Control, 18, 275–282. [DOI] [PubMed] [Google Scholar]
- Lee JG, Matthews AK, McCullen CA, & Melvin CL (2014). Promotion of tobacco use cessation for lesbian, gay, bisexual, and transgender people: a systematic review. American Journal of Preventive Medicine, 47, 823–831. doi: 10.1016/j.amepre.2014.07.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DT, & Friend KB (2003). The effects of clean indoor air laws: what do we know and what do we need to know? Health Education Research, 18, 592–609. [DOI] [PubMed] [Google Scholar]
- Matthews AK, Li C, Kuhns LM, Tasker TB, & Cesario JA (2013). Results from a community-based smoking cessation treatment program for LGBT smokers. Journal of Environmental and Public Health, 2013, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMullen KM, Brownson RC, Luke D, & Chriqui J (2005). Strength of clean indoor air laws and smoking related outcomes in the USA. Tobacco Control, 14, 43–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center (2013, July 13). A survey of LGBT Americans: Attitudes, experiences, and values in changing times. Pew Social Trends Retrieved from http://www.pewsocialtrends.org/files/2013/06/SDT_LGBT-Americans_06-2013.pdf
- Prochaska JJ, Fromont SC, Ramo DE, Young-Wolff KC, Delucchi K, Brown RA, & Hall SM (2015). Gender differences in a randomized controlled trial treating tobacco use among adolescents and young adults with mental health concerns. Nicotine & Tobacco Research, 17, 479–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Rodriguez TMS, Chavez K, Sommer MJ, & Prochaska JJ (2014). Facebook recruitment of young adult smokers for a cessation trial: Methods, metrics, and lessons learned. Internet Interventions, 1, 58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Thrul J, Chavez K, Delucchi KL, & Prochaska JJ (2015a). Feasibility and quit rates of the Tobacco Status Project: A Facebook smoking cessation intervention for young adults. Journal of Medical Internet Research, 17, e291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Thrul J, Delucchi KL, Hall S, Ling PM, Belohlavek A, Prochaska JJ (2018). A randomized controlled evaluation of the Tobacco Status Project, a Facebook intervention for young adults. Addiction doi: 10.1111/add.14245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Thrul J, Delucchi KL, Ling PM, Hall SM, & Prochaska JJ (2015b). The Tobacco Status Project (TSP): Study protocol for a randomized controlled trial of a Facebook smoking cessation intervention for young adults. BMC Public Health, 15, 897–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redding CA, Prochaska JO, Armstrong K, Rossi JS, Hoeppner BB, Sun X, …& Velicer WF (2015). Randomized trial outcomes of a TTM-tailored condom use and smoking intervention in urban adolescent females. Health Education Research, 30, 162–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario M, Corliss HL, Everett BG, Reisner SL, Austin SB, Buchting FO, & Birkett M (2014). Sexual orientation disparities in cancer-related risk behaviors of tobacco, alcohol, sexual behaviors, and diet and physical activity: Pooled Youth Risk Behavior Surveys. American Journal of Public Health, 104, 245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwappach DL (2008). Smoking behavior, intention to quit, and preferences toward cessation programs among gay men in Zurich, Switzerland. Nicotine & Tobacco Research, 10, 1783–1787. [DOI] [PubMed] [Google Scholar]
- Seidenberg AB, Jo CL, Ribisl KM, Lee JGL, Buchting FO, Kim Y, & Emery SL (2017). A national study of social media, television, radio, and internet usage of adults by sexual orientation and smoking status: Implications for campaign design. International Journal of Environmental Research and Public Health, 2017, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shilo G, & Mor Z (2014). The impact of minority stressors on the mental and physical health of lesbian, gay, and bisexual youths and young adults. Health & Social Work, 39, 161–171. [DOI] [PubMed] [Google Scholar]
- Smalley KB, Warren JC, & Barefoot KN (2016). Differences in health risk behaviors across understudied LGBT subgroups. Health Psychology, 35, 103–114. [DOI] [PubMed] [Google Scholar]
- Smith EA, Thomson K, Offen N, & Malone RE (2008).”If you know you exist, it’s just marketing poison”: meanings of tobacco industry targeting in the lesbian, gay, bisexual, and transgender community. American Journal of Public Health, 98, 996–1003. doi: 10.2105/AJPH.2007.118174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanKim NA, Erickson DJ, Eisenberg ME, Lust K, Rosser BRS, & Laska MN (2015). College women’s weight-related behavior profiles differ by sexual identity. American Journal of Health Behavior, 39, 461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls NE, & Wisneski H (2010). Evaluation of smoking cessation classes for the lesbian, gay, bisexual, and transgender community. Journal of Social Service Research, 37, 99–111. [Google Scholar]
- Walther CS, Poston DL, & Gu Y (2011). Ecological analyses of gay male and lesbian partnering in the metropolitan United States in 2000. Population Research and Policy Review, 30, 419–448. [Google Scholar]
- Zhang C, Brook JS, Leukefeld CG, De La Rosa M, & Brook DW (2017). Lack of preventive health behaviors in the early forties: The role of earlier trajectories of cigarette smoking from adolescence to adulthood. Substance Use and Misuse, 52, 1527–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]