Abstract
Purpose of review:
This review summarizes the recent epidemiologic literature examining health outcomes in communities living close to unconventional natural gas development (UNGD) and identifies areas requiring further study.
Recent findings:
To date, these studies have been primarily retrospective in design and used self-report of health symptoms or electronic health databases to obtain outcome information. Proximity to UNGD is often used as a surrogate for exposure. There is preliminary evidence linking respiratory outcomes, including asthma exacerbations, and birth outcomes, such as reduced fetal growth and preterm birth, to UNGD; however, results differ across study populations and regions.
Summary:
Although small, the current body of literature suggests that living near UNGD may have negative health consequences for surrounding communities, but additional work using more granular estimates of exposure or personalized monitoring is urgently needed.
Keywords: unconventional natural gas development, fracking, geographic information system, health effects, birth outcomes, asthma
Introduction
Unconventional natural gas development (UNGD) uses novel gas extraction methods to tap natural gas reserves tightly bound in shale formations at depths previously unattainable using conventional techniques. These methods include horizontal drilling through shale layers at levels thousands of feet below ground as well as high volume hydraulic fracturing, commonly referred to as “fracking,” a process that involves pumping millions of gallons of water, mixed with a proppant (usually sand) and other chemicals, to fracture the shale around the well and enhance the release and flow of the gas. In the United States, rapid UNGD expansion began in the early 21st century in areas like the Barnett Shale in Texas, the Denver-Julesberg Basin in Colorado, and the Marcellus Shale in Pennsylvania [1]. Hydraulic fracturing remains a controversial issue in affected areas, particularly with regard to health concerns raised in popular media, such as in Josh Fox’s 2010 documentary Gasland. However, this exponential growth of UNGD has outpaced environmental and human health effects studies, although a small but growing body of literature, reviewed presently, suggests that UNGD may have adverse health consequences for nearby communities.
Epidemiologic studies exploring the potential human health impacts of UNGD have started to emerge only within the last decade. In general, the two categories of health endpoints most often investigated in these studies are respiratory symptoms/conditions and adverse birth outcomes, such as low birth weight and preterm birth, although dermal, neurological, and other conditions have also been considered (see Table 1). Much of the work regarding UNGD and public health has been conducted in Colorado and Pennsylvania, and some metric of proximity to these activities is typically used as a surrogate for exposure. The following review summarizes this recent, peer-reviewed literature and recommends next steps to improve exposure assessment and advance research in this field.
Table 1.
Summary of peer-reviewed studies examining human health effects of unconventional natural gas development. (Abbreviations: CHDs=congenital heart defects, NTDs=neural tube defects, SGA=small for gestational age, WIC=Women, Infants and Children, BMI=Body Mass Index, NMR=nearest major road)
| Authors | Year | Study Region | Total Sample Size | Exposure Metric | Outcomes Assessed | Covariates |
|---|---|---|---|---|---|---|
| Fryzek et al. | 2013 | Pennsylvania | 1,874 cancers before drilling; 1,996 after | before versus after drilling | all childhood cancers, childhood leukemia, central nervous system tumors | age, sex, race |
| McKenzie et al. | 2014 | Rural Colorado | 124,842 births | inverse distance weighted well count | birth defects (CHDs, NTDs, oral cleft), preterm birth, term low birth weight | maternal age, education, tobacco use, ethnicity, alcohol use, parity, infant sex, gestational age, elevation |
| Rabinowitz et al. | 2015 | Southwest Pennsylvania | 180 households (492 people) | distance from nearest well (<1 km, 1–2 km, and >2 km) | skin, upper respiratory, lower respiratory, cardiac, gastrointestinal, and neurological symptoms | age, household education, sex, smokers in household, job type, animals in household, awareness of environmental risk |
| Stacy et al. | 2015 | Southwest Pennsylvania | 15,451 births | inverse distance weighted well count | birth weight, SGA, preterm birth | maternal age, education, pre-pregnancy weight, smoking during pregnancy, gestational diabetes, prenatal care, WIC assistance, race, parity, gestational age, infant sex |
| Casey et al. | 2016 | Central/northeast Pennsylvania | 10,946 births | inverse-distance squared | term birth weight, preterm birth, low 5-minute APGAR score, SGA | infant sex, gestational age, season of birth, maternal age, race, primary care patient status, smoking status, prepregnancy BMI, parity, antibiotic orders, medical assistance, delivery hospital, drinking water source, distance to NMR, residential greenness, community socioeconomic deprivation, year of birth |
| Rasmussen et al. | 2016 | Central/northeast Pennsylvania | 27,401 asthma exacerbations | inverse-distance squared | asthma hospitalizations, asthma emergency department visits, oral corticosteroid orders | age, sex, race, family history of asthma, smoking status, season, medical assistance, overweight/obesity status, type 2 diabetes, community socioeconomic deprivation, distance to NMR, temperature day prior to event |
| Tustin et al. | 2016 | Central/northeast Pennsylvania | 7,785 adults | inverse-distance squared | chronic rhinosinusitis, fatigue, migraine headache | age, sex, race, medical assistance, smoking status |
Exposure Assessment
Many of the activities associated with UNGD emit pollutants with known or hypothesized negative impacts on human health. Exposure may occur primarily through inhalation of air pollutants emitted during various phases of development or through ingestion of contaminated drinking water [1]. Diesel-powered drill rigs, hydraulic fracturing pumps, and trucks transporting materials to and from drilling sites are sources of harmful air contaminants such as nitrous oxides, particulate matter, and volatile organic compounds (e.g. benzene, xylene) [2]. Exposure to particulate matter and other air pollutants has been linked to a variety of adverse health outcomes, including respiratory and cardiovascular conditions as well as low birth weight and preterm birth in infants [3,4]. A human health risk assessment of air emissions from UNGD in Garfield County, Colorado found that residents living within 0.5-mile of UNGD activities had greater total subchronic, non-cancer hazard indices than those living >0.5-mile away, driven mostly by exposures to trimethylbenzenes, aliphatic hydrocarbons, and xylenes [5]. Residents living close to UNGD also had greater cumulative cancer risks, due in large part to exposure to benzene [5].
Spills or leaks occurring during the storage, treatment, and disposal of wastewater (also known as flowback or produced water) may lead to additional opportunities for human exposure. When the pressure in the gas well is released, allowing the natural gas to flow freely back up the well, it brings with it flowback fluids containing a mixture of hydrocarbon products, the chemical additives used to fracture the shale, and naturally-occurring contaminants from the shale layer itself (e.g., metals and radionuclides). This wastewater may be stored in surface pits or sealed tanks before reuse or disposal [1]. In the western US, wastewater is typically disposed of through deep underground injection, a practice which is less common in Pennsylvania, where disposal wells are not readily available and may be costly to implement [6]. In Pennsylvania, disposal practices have included transportation of wastewaters to Ohio for deep-well injection or treatment at municipal sewage treatment plants, followed by surface water discharge. However, a moratorium was placed on the latter when concentrations of bromine and other contaminants elevated above water quality criteria were measured in drinking water obtained from affected rivers [7,8]. Another study found that workers dealing with UNGD wastewaters could be exposed to levels of benzene above allowable occupational health levels [9]. Other investigations have reported that several air and water contaminants associated with UNGD, including some of the chemical additives used in the hydraulic fracturing process, are potential endocrine disruptors [10,11] or carcinogens [12].
To date, epidemiologic studies have not had the resources to link human health outcomes directly with environmental concentrations of pollutants associated with UNGD. Instead, investigators have used proximity metrics, such as distance to the nearest well or inverse distance weighting, as a surrogate for exposure to UNGD. In these studies, a geographic information system (GIS) is used to link residential locations of participants to locations of gas wells for proximity analysis. Inverse distance weighting is a common approach for estimating individual pollutant exposures from multiple fixed point sources [13–15]. Although a useful starting point for preliminary studies, proximity analyses are primarily hypothesis-generating. They do not take into account geological, meteorological, or other factors that affect the movement of pollutants through water, soil, or air and, therefore, what concentrations actually reach human populations. Thus, even if we observe an association between proximity to a pollution source and a health outcome, we can only speculate as to the specific agent or agents that might be responsible. The remainder of this review summarizes the recent UNGD epidemiologic literature, identifies current research gaps, and makes recommendations for improved exposure assessment beyond proximity.
Cancer
To date, one study has been published exploring cancer outcomes and unconventional gas development [16]. Fryzek et al. compared incidences of the two most common childhood cancers, leukemia and central nervous system (CNS) tumors, in Pennsylvania counties before and after UNGD [16]. The authors defined “before” as the period from 1990 to the year before the first unconventional well was drilled in a county and “after” starting the year the first well was drilled in a county through 2009. They identified 1,874 total cases of childhood cancer before drilling and 1,996 cases after, and compared observed to expected numbers of cancers using standardized incidence ratios (SIRs). Except for a slightly elevated SIR for CNS tumors (SIR: 1.1, 95% CI: 1.0, 1.3) after drilling, observed numbers of all childhood cancers and of childhood leukemia were close to expected both before and after UNGD. However, others have noted that the lag period between drilling activities, which started in Pennsylvania in the mid-2000s, and the development of a clinically observable cancer was too short in this study [17]. UNGD has continued to flourish in the Marcellus Shale region since Fryzek et al. conducted their study, and, now that gas development has been occurring for about ten years in Pennsylvania, its potential impact on childhood cancer rates there and near other shale formations is one area deserving of further research.
Respiratory Outcomes
Several studies, also conducted in Pennsylvania, have found associations between proximity to UNGD and increases in certain respiratory conditions and symptoms, including nasal and sinus irritation as well as asthma exacerbations [18–20]. The earliest study characterized groups of exposure to UNGD using distance thresholds [18], while later studies used a more complex inverse distance-squared metric taking into account distance from residence to well, well characteristics, and the dates and durations of well development phases [19,20]. Rabinowitz et al. conducted a health symptom survey of 180 households with ground-fed water wells in Washington County, Pennsylvania, an area of active natural gas development [18]. The authors administered a community environmental health assessment questionnaire to participating households in 2012, asking respondents if they or any household members had experienced specific respiratory, skin, cardiac, gastrointestinal, or neurological symptoms in the past year. They used distance from the nearest gas well to classify households into three “exposure” groups and compared those living <1 km and 1–2 km from the closest well to those living >2 km. After adjustment for covariates, which included sociodemographic factors and awareness of environmental hazard, individuals living <1 km of UNGD were more likely to report upper respiratory symptoms (e.g. sinus problems, cough, sore throat, stuffy nose) compared to those living >2 km (OR=3.1, 95% CI=1.5, 6.7). Reports of lower respiratory symptoms such as asthma/COPD, chronic bronchitis, and wheezing were also somewhat more common in the most versus least exposed groups, although the odds ratio was not statistically significant (OR=1.5, 95% CI=0.7, 3.1).
Two very recent studies have investigated proximity to drilling and respiratory conditions in central and northeast Pennsylvania, another active region of UNGD. In these investigations, participants were identified from the Geisinger Clinic population and assigned inverse distance-squared metrics for well pad activities (e.g., preparation, start of drilling, and production phases) [19,20]. Rasmussen et al. used a nested case-control study design to explore associations between these UNGD activity metrics and several measures of asthma exacerbation, including asthma hospital visits, emergency department visits, and new oral corticosteroid (OCS) medication orders from 2005 to 2012 [19]. Controls were asthma patients without exacerbations. Adjusted results were similar across UNGD activity metrics, with the patients most exposed to these activities having greater odds for hospitalizations, emergency department visits, and OCS orders compared to the least exposed patients for 11 of 12 UNGD-outcome pairs.
In a cross-sectional study in Pennsylvania, Tustin et al. investigated associations between chronic rhinosinusitis (CRS) and several other symptom groups with proximity to UNGD [20]. The authors gathered symptom information via surveys administered to 7,785 Geisinger Clinic patients in 2014. Similar to previous studies from this group [19,21], they assigned patients UNGD activity metrics for four time-varying phases of well development. After adjustment for potential confounding factors, the highest quartile of UNGD activity was not associated with current CRS (OR=1.1, 95% CI=0.8, 1.7) compared to the lowest quartile. However, for the most compared to least exposed patients, associations were statistically significant for combinations of two or more outcomes, including CRS and fatigue, and CRS, fatigue, and migraine.
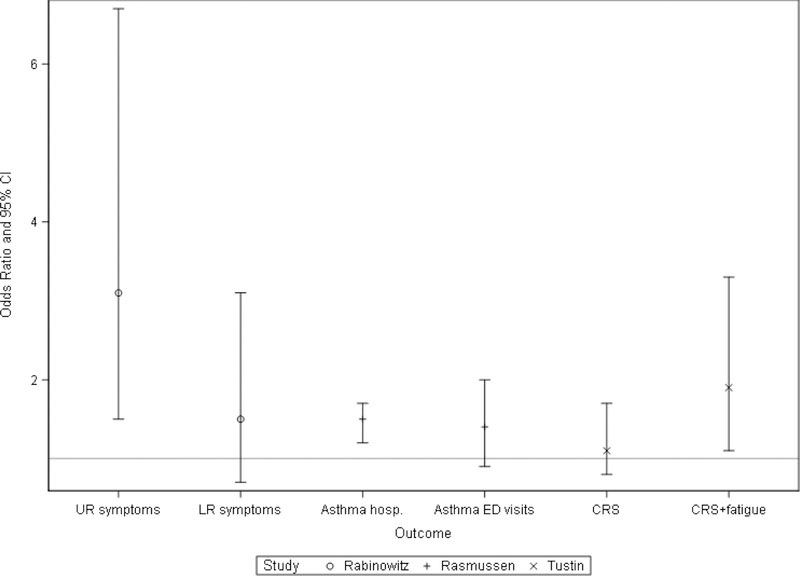
The few studies that have explored respiratory health and UNGD thus far have differed in design, exposure metrics used, outcomes assessed, and confounding factors considered, making direct comparisons challenging. Two of these studies relied on self-reported symptoms [18,20], while the third used electronic health data to identify possible asthma exacerbations [19]. Figure 1 summarizes some of the major results from each of these studies. For concision, odds ratios and confidence intervals are shown only for the most (compared to least) exposed groups from each study. Considered together, these results suggest that living close to UNGD activities in the Marcellus Shale may have an adverse impact on respiratory health. Lower respiratory symptoms, including asthma, had an elevated if not statistically significant association with UNGD in the first published study, while proximity to these activities was associated with several objective asthma outcomes in Rasmussen et al. [19]. Associations with upper respiratory symptoms, including nasal and sinus symptoms, are suggestive but somewhat inconsistent. In Tustin et al., CRS was associated with UNGD only when considered in conjunction with other conditions [20]. Additional investigations in the Marcellus Shale and other regions affected by unconventional gas development that utilize electronic health records or sources of more objective health outcome data (as opposed to self-reported symptoms) are needed to corroborate these findings.
Figure 1.
Select adjusted odds ratios (OR) and 95% confidence intervals (CI) from studies examining respiratory symptoms or outcomes and proximity to unconventional natural gas development. ORs reported for the most vs. least exposed groups from each study. (Abbreviations: UR=upper respiratory, LR=lower respiratory, hosp.=hospitalizations, ED=emergency department, CRS=chronic rhinosinusitis)
Birth Outcomes
Perhaps the most active area of research regarding the human health effects of UNGD has been on infant health outcomes, including birth defects, low birth weight, and preterm birth [14,21,22]. One practical reason for this is the availability of vital records maintained by state health departments. Using this data, we can conduct preliminary studies of the health effects of UNGD relatively quickly, considering health endpoints we can observe months, rather than years after exposure to UNGD activities. The fetus, infant, and child are also sensitive populations. There are windows of vulnerability during pregnancy and early childhood when the fetus or child may have heightened susceptibility to the adverse health effects of chemical exposures [23]. Reduced fetal growth has been associated with a number of chronic health outcomes later in life [24], so eliminating these early life exposures can improve health across the lifespan. In addition, children born preterm are at risk for long-term neurobehavioral impairments [25,26].
Similar to the studies discussed so far, investigations of UNGD and birth outcomes have also used proximity metrics as a proxy for exposure. There is more consistency in the health endpoints analyzed, although only one study was able to consider several classes of birth defects [14]. McKenzie et al. conducted a retrospective cohort study of 124,842 singleton live births in rural areas of Colorado between 1996 and 2009, a time period encompassing the start of UNGD expansion in Colorado in the year 2000 [14]. They assigned each mother an inverse distance weighted (IDW) well count, a measure summing the inverse distances between the birth residence and each well within 10 miles of the residence. Comparing categories of low, medium, and high IDW well counts to a referent group with no exposure to UNGD (i.e., no wells within 10 miles of the residence), the authors explored associations between UNGD well proximity and congenital heart defects, neural tube defects, oral clefts, preterm birth, and term low birth weight. After adjustment for sociodemographic and behavioral factors, McKenzie and colleagues found that infants born to the most exposed mothers had 30% greater prevalence of congenital heart defects than those born to mothers with no wells within a 10-mile radius (OR=1.3, 95% CI=1.2–1.5). There was a monotonic increase in the prevalence of congenital heart defects with increasing exposure to UNGD in both unadjusted and adjusted models (p<0.0001). Prevalence of neural tube defects was also positively associated with proximity in the most exposed group compared to the referent (OR=2.0, 95% CI=1.0–3.9), while no statistically significant associations were found for oral clefts. In contrast, risks for preterm birth and term low birth weight decreased with increasing exposure to UNGD in this study (p<0.0001).
Stacy et al. also used the IDW well count approach to assign exposure groups to UNGD and examine associations with continuous birth weight, small for gestational age (SGA), and preterm birth in southwest Pennsylvania [22]. Their study included 15,451 singleton live births born in three rural counties from 2007 to 2010, the period of the most rapid UNGD expansion in this area at the time they conducted the study. All participants lived within 10 miles of unconventional gas wells; mothers in the top three quartiles of exposure were compared to the bottom quartile of IDW well counts. For the topmost compared to the bottom quartile, Stacy et al. found a small but statistically significant decrease in birth weight with increasing exposure to UNGD (β=−22, SE=9, p=0.02). Similarly, odds for being born SGA increased across increasing quartiles of exposure and reached statistical significance for the most exposed quartile (OR=1.3, 95% CI=1.1, 1.6). However, no similar trend was observed for risk of preterm birth, while infants born to mothers in the second quartile of exposure had a slightly reduced risk for being born preterm.
The most recent study of birth outcomes and UNGD was conducted in central and northeast Pennsylvania using data from the Geisinger Health System [21]. Casey et al. had a sample of 10,496 neonates born to 9,384 mothers between 2006 and January 2013. They assigned exposure using an inverse distance-squared metric, taking into account distance to the mother’s residence, dates and durations of various phases of well development, and production volume. After adjustment for infant and maternal characteristics, mothers in the fourth quartile of the UNGD activity index had infants with lower term birth weight compared to mothers in the first quartile (difference= −31, 95% CI= −57, −5), although further adjustment for year of birth attenuated this association. Odds of preterm birth increased across quartiles of exposure, with the strongest association in the fourth quartile after adjustment for year of birth and other factors (OR=1.9, 95% CI=1.2, 2.9). The authors did not find associations between the UNGD activity index and 5-minute Apgar score or SGA.
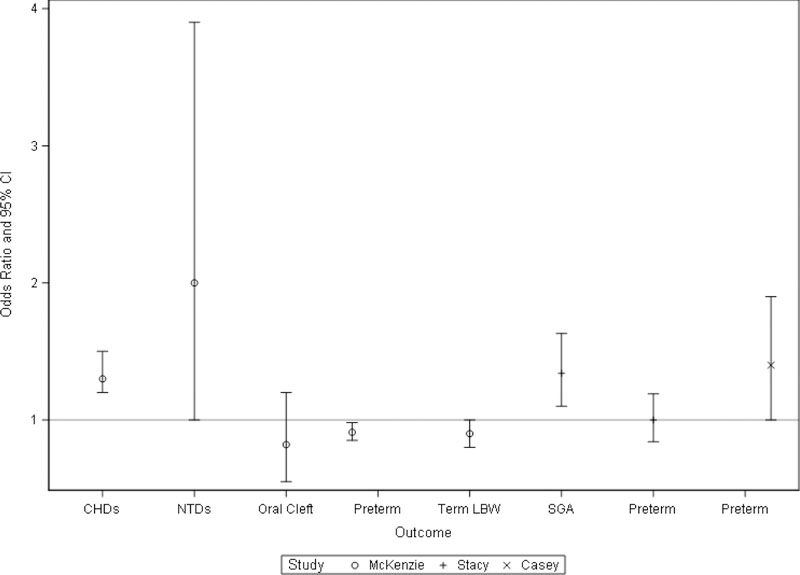
In all three studies, authors identified at-risk infants and assigned exposure to UNGD retrospectively. The use of data from birth certificates or electronic health record files enabled these studies to have large sample sizes. Notably, the McKenzie study had almost 125,000 births, which allowed them to examine three classes of birth defects as well as specific clinical diagnostic groups of congenital heart defects [14]. For ease of comparison, binary outcomes considered and adjusted odds ratios of the most exposed group from each study are shown in Figure 2. Results for continuous outcomes are not displayed. Each study examined preterm birth and measures of reduced birth weight (term low birth weight and SGA), although results are somewhat conflicting. Considering the most exposed groups, McKenzie et al. found reduced risk for preterm and term low birth weight, whereas Stacy et al. observed an increased risk for SGA and no association between preterm birth and exposure to UNGD. Casey et al. observed an association between increased exposure to UNGD and lower term birth weights, but this result was attenuated after further adjustment for year of birth. Contrary to the previous two studies, Casey et al. found an association between increasing exposure to UNGD and increased risk for preterm birth. Together, these investigations suggest that exposure to UNGD, as represented using proximity metrics, may be associated with certain infant health outcomes, but additional studies are needed to confirm the direction and strength of these associations. We need large sample sizes to obtain enough statistical power to examine birth defects, which are relatively rare events in a study population.
Figure 2.
Adjusted odds ratios (OR) and 95% confidence intervals (CI) from studies examining birth outcomes and proximity to unconventional natural gas development. ORs reported for the most vs. least exposed groups from each study. (Abbreviations: CHDs=congenital heart defects, NTDs=neural tube defects, LBW=low birth weight, SGA=small for gestational age)
Other Health Outcomes
In addition to upper respiratory symptoms, Rabinowitz et al. also found increased reporting of skin conditions, such as rashes and dermatitis, for participants living <1 mile of UNGD [18]. Reports of neurological symptoms, including but not limited to severe headache, migraine, and dizziness, were elevated but not statistically significant in their most exposed group (OR: 1.53, 95% CI: 0.89, 2.63) [18]. Tustin et al. found an elevated odds for migraine headache among participants in their highest quartile of exposure to UNGD [20]. As described previously, risks for adverse outcomes in their study were significantly increased in participants with both CRS and fatigue, migraine headache and fatigue, and for those with all three outcomes [20]. Finally, in a symptom survey of a convenience sample of 53 participants living close to UNGD, stress was the most frequently reported symptom [27]. Although outside the scope of this review, persistent stress can have a negative impact on both mental and physical health [28]. The impact of stress, due to nearby natural gas development, on the health of surrounding communities is another area of future research.
Conclusion
A small but growing body of literature suggests that communities living close to unconventional natural gas development may be at greater risk for certain health outcomes. Studies to date have primarily relied on proximity metrics as a proxy for exposure to UNGD and have collected outcome data using surveys administered to study participants or electronic health databases. In studies using self-reported health symptoms, participants with greater awareness of UNGD activities close to their home may be more likely to report adverse symptoms or more likely to choose to participate in the study, both sources of potential bias [18]. We need additional studies using electronic health records, medically confirmed diagnoses, or other less biased methods for health outcome assessment to further confirm some of the links found between UNGD and particular health effects, including skin, respiratory, and neurological conditions. From the three major birth outcome studies, there is evidence that proximity to these activities is associated with increased risk for several birth defects, preterm birth, and certain measures of reduced fetal growth, but results differ somewhat by region and study population. Although more resource and time intensive, the recruitment and follow-up of large, prospective birth cohorts in drilling areas would aid in confirming the associations found in these preliminary studies. As 20 unique water and air pollutants associated with UNGD have evidence of increased risk for childhood leukemia [12], further epidemiologic studies on childhood cancer risk in drilling areas appears warranted.
The epidemiologic studies reviewed presently are primarily hypothesis generating, and the use of proximity and density metrics of UNGD cannot identify specific exposures that could explain observed associations. Future studies of the health effects of UNGD would greatly benefit from using more granular estimates of exposure or conducting more individualized exposure assessments. This could include the use of portable sampling equipment [29] as well as the measurement of biomarkers of exposure in biospecimens collected from study participants (e.g., measuring PAH- or benzene-DNA adducts in blood). These methods would allow us to develop a more complete picture of what types and concentrations of contaminants affected communities are actually exposed to and enable us to link health outcomes with specific agents. GIS methods can also aid in estimating personal exposures to UNGD, such as the use of global positioning system technology to integrate study population activity data with measured concentrations of environmental contaminants [29,30].
In conclusion, the current body of literature examining the health effects of unconventional natural gas development suggests that proximity to these activities may have adverse implications for the health of nearby communities. Future epidemiologic studies should implement personal exposure assessments to examine associations between individual contaminants and relevant health outcomes, particularly to explain associations seen with respiratory and birth outcomes.
Footnotes
Conflict of Interest
The author declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.Adgate JL, Goldstein BD, McKenzie LM: Potential public health hazards, exposures and health effects from unconventional natural gas development. Environmental Science & Technology 2014; 48: 8307–8320. [DOI] [PubMed] [Google Scholar]
- 2.Roy AA, Adams PJ, Robinson AL: Air pollutant emissions from the development, production, and processing of Marcellus Shale natural gas. Journal of the Air & Waste Management Association 2014; 64: 19–37. [DOI] [PubMed] [Google Scholar]
- 3.Kelly FJ, Fussell JC: Air pollution and public health: emerging hazards and improved understanding of risk. Environ Geochem Health 2015; 37: 631–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nieuwenhuijsen MJ, Dadvand P, Grellier J, et al. : Environmental risk factors of pregnancy outcomes: A summary of recent meta-analyses of epidemiologic studies. Environmental Health 2013; 12: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McKenzie LM, Witter RZ, Newman LS, et al. : Human health risk assessment of air emissions from development of unconventional natural gas resources. Science of the Total Environment 2012; 424: 79–87. [DOI] [PubMed] [Google Scholar]
- 6.Vidic RD, Brantley SL, Vandenbossche JM, et al. : Impact of shale gas development on regional water quality. Science 2013; 340: 1235009-1–9. [DOI] [PubMed] [Google Scholar]
- 7.Wilson JM, VanBriesen JM: Oil and gas produced water management and surface drinking water sources in Pennsylvania. Environmental Practice 2012; 14: 288–300. [Google Scholar]
- 8.Ferrar KJ, Michanowicz DR, Christen CL, et al. : Assessment of effluent contaminants from three facilities discharging Marcellus Shale wastewater to surface waters in Pennsylvania. Environmental Science & Technology 2013; 47: 3472–3481. [DOI] [PubMed] [Google Scholar]
- 9.Esswein EJ, Breitenstein M, Snawder J: NIOSH field effort to assess chemical exposures in oil and gas workers: Health hazards in hydraulic fracturing. In: Health Impact Assessment of Shale Gas Extraction: Workshop Summary The National Academies Press, Washington, D.C. 2013. [Google Scholar]
- 10.Kassotis CD, Tillitt DE, Hormann AM, et al. : Estrogen and androgen receptor activities of hydraulic fracturing chemicals and surface and ground water in a drilling-dense region. Endocrinology 2013; 155: 897–907. [DOI] [PubMed] [Google Scholar]
- 11.Kassotis CD, Klemp KC, Vu DC, et al. : Endocrine-disrupting activity of hydraulic fracturing chemicals and adverse health outcomes after prenatal exposure in male mice. Endocrinology 2015; 156: 4458–4473. [DOI] [PubMed] [Google Scholar]
- 12.Elliott EG, Trinh P, Ma X, et al. : Unconventional oil and gas development and risk of childhood leukemia: Assessing the evidence. Science of The Total Environment 2017; 576: 138–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghosh JKC, Wilhelm M, Su J, et al. : Assessing the influence of traffic-related air pollution on risk of term low birth weight on the basis of land-use-based regression models and measures of air toxics. American Journal of Epidemiology 2012; 175: 1262–1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.• McKenzie LM, Guo R, Witter RZ, et al. Birth outcomes and maternal residential proximity to natural gas development in rural Colorado. Environmental Health Perspectives 2014; 122: 412–417.This was the first study to examine birth outcomes and proximity to unconventional gas development. The authors found an increased risk for congenital heart defects and neural tube defects with increased exposure to UNGD.
- 15.Brauer M, Lencar C, Tamburic L, et al. : A cohort study of traffic-related air pollution impacts on birth outcomes: University of British Columbia. Environmental Health Perspectives 2008; 116: 680–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fryzek J, Pastula S, Jiang X, et al. : Childhood cancer incidence in Pennsylvania counties in relation to living in counties with hydraulic fracturing sites. Journal of Occupational and Environmental Medicine 2013; 55: 796–801. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein BD, Malone S. Obfuscation does not provide comfort: Response to the article by Fryzek et al on hydraulic fracturing and childhood cancer. Journal of Occupational and Environmental Medicine 2013; 55: 1376–1378. [DOI] [PubMed] [Google Scholar]
- 18.Rabinowitz PM, Slizovskiy IB, Lamers V, et al. : Proximity to natural gas wells and reported health status: Results of a household survey in Washington County, Pennsylvania. Environmental Health Perspectives 2015; 123: 21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.• Rasmussen SG, Ogburn EL, McCormack M, et al. : Association Between Unconventional Natural Gas Development in the Marcellus Shale and Asthma Exacerbations. JAMA Internal Medicine 2016.In this study, the authors used electronic health records from the Geisinger Clinic to identify asthma exacerbations, including hospitalizations, emergency department visits, and OCS orders. The participants most exposed to unconventional gas development had greater odds for these outcomes.
- 20.• Tustin AW, Hirsch AG, Rasmussen SG, et al. : Associations between Unconventional Natural Gas Development and Nasal and Sinus, Migraine Headache, and Fatigue Symptoms in Pennsylvania. Environmental Health Perspectives 2016. [Epub ahead of print].This study used self-reported health symptoms from the Geisinger Clinic population and found associations between increased exposure to UNGD and increased reports for two or more health outcomes, including chronic rhinosinusitis (CRS) plus migraine and CRS, migraine, plus fatigue.
- 21.• JA Casey, DA Savitz, SG Rasmussen, et al. : Unconventional natural gas development and birth outcomes in Pennsylvania, USA. Epidemiology 2016; 27: 163–172.In central and northeastern Pennsylvania, increased risk for preterm birth was associated with more exposure to UNGD, using an activity index that accounted for distance to the mother’s residence, dates and durations of various phases of well development, and production volume.
- 22.• Stacy SL, Brink LL, Larkin JC, et al. : Perinatal outcomes and unconventional natural gas operations in Southwest Pennsylvania. PloS one 2015; doi 10: e0126425.This study was the first UNGD and birth outcomes study in Pennsylvania and, similar to McKenzie et al., used an inverse distance weighted well count to represent exposure to UNGD. In three southwestern PA counties, infants in the most exposed group were at greater risk for being born small for gestational age.
- 23.Landrigan PJ, Miodovnik A: Children’s health and the environment: an overview. Mount Sinai Journal of Medicine 2011; 78: 1–10. [DOI] [PubMed] [Google Scholar]
- 24.Barker DJ. The origins of the developmental origins theory. Journal of Internal Medicine 2007; 261: 412–417. [DOI] [PubMed] [Google Scholar]
- 25.Salmaso N, Jablonska B, Scafidi J, et al. : Neurobiology of premature brain injury. Nat Neurosci 2014; 17: 341–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sutton PS, Darmstadt GL. Preterm birth and neurodevelopment: a review of outcomes and recommendations for early identification and cost-effective interventions. J Trop Pediatr 2013; 59: 258–265. [DOI] [PubMed] [Google Scholar]
- 27.Ferrar KJ, Kriesky J, Christen CL, et al. : Assessment and longitudinal analysis of health impacts and stressors perceived to result from unconventional shale gas development in the Marcellus Shale region. International Journal of Occupational and Environmental Health 2013; 19: 104–112. [DOI] [PubMed] [Google Scholar]
- 28.Schneiderman N, Ironson G, Siegel SD: Stress and health: psychological, behavioral, and biological determinants. Annual Review of Clinical Psychology 2005; 1: 607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rohlman D, Syron L, Hobbie K, et al. : A Community-Based Approach to Developing a Mobile Device for Measuring Ambient Air Exposure, Location, and Respiratory Health. Environmental Justice 2015; 8: 126–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nuckols JR, Ward MH, Jarup L: Using geographic information systems for exposure assessment in environmental epidemiology studies. Environmental Health Perspectives 2004; 112: 1007–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]