Abstract
Background
Psychological distress including depression and anxiety are among the most serious causes of morbidity and mortality in Bangladesh. There has been no study in the rural area to report the prevalence of and risk factors for psychological distress. The aim of this study was to estimate the prevalence of and risk factors for psychological distress in a rural district in Bangladesh.
Methods
A total of 2425 adults (1249 women) aged 18–90 years were selected from the Narail upazilla using multi-level cluster random sampling for a cross-sectional study. Psychological distress was assessed using the Kessler 10 items questionnaire. Participants’ socio-demographic status, life style factors and health conditions were also collected. Odds ratios and 95% confidence intervals for binary outcomes and mean changes for continuous outcomes of psychological distress score were computed. Logistic regression and generalized linear model techniques were used for analytical purpose.
Results
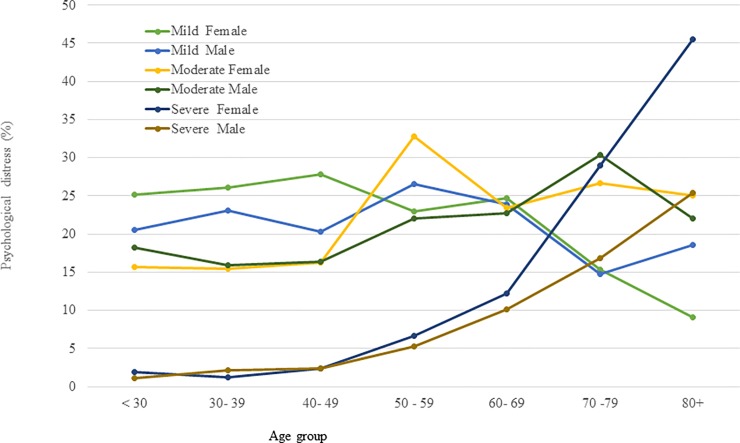
The overall prevalence of psychological distress was 52.5%. This proportion included 22.7% people rated as having mild psychological distress, 20.8% moderate and 9.0% severe. The prevalence of moderate (24.7% vs. 17.5%, p<0.001) and severe (16.2% vs. 2.5%, p<0.001) psychological distress was significantly higher in older adults of age 60–90 years than that in younger adults of age 18–59 years. The prevalence of severe psychological distress was higher in females than males and the difference increased with age (vs. (females vs males: 1.9% vs. 1.1% at age of <30 years, 12.2% vs. 10.1% at age between 60–69 years, and 45.5% vs. 25.4% at age of 80 years or older). After multivariate adjustment, compared to degree or equivalent level of education, no education (odds ratio (OR), 1.71, 95% confidence interval (CI), 1.03–2.82) was associated with higher prevalence of any psychological distress in the total sample. Compared to married, psychological distress among widowed older adults was almost five times higher prevalence (OR, 4.89, 95% CI, 2.51–9.55). Socio-economic status showed a U-shaped relationship with the prevalence of psychological distress; being very poor or wealthy was associated with higher prevalence of psychological distress compared to those of moderate socio-economic status. People living in pourashava (semi-urban areas) reported significantly higher prevalence of psychological distress compared to people living in typical rural unions.
Conclusions
In this rural Bangladeshi community, the prevalence of psychological distress was high, especially among older women. Factors including lower level of education, inability to work, and living in semi-urban areas were associated with higher prevalence of psychological distress. Public health programmes should target people in high risk groups to reduce their psychological distress in Bangladesh.
Introduction
Psychological distress is common across the world [1, 2]. There are currently over 542 million people living with depression or anxiety symptoms, which represents an increase of more than 18% from 2005 to 2015 [3–5]. It is projected that one in four individuals globally will be affected by depressive symptoms at some point in their lifetime [6, 7]. If this depression is present with chronic diseases as co-morbid conditions, it can reduce life expectancy by approximately 20 years [8]. Psychological distress is the presence of a number of depressive symptoms including lack of enthusiasm, feeling hopeless about the future, and anxiety symptoms [9].
The prevalence of psychological distress and its associated factors vary across the globe. A meta-analysis of 174 surveys across 63 countries from 1980 to 2013 comprising 665,433comprised 665433 individuals reported a pooled prevalence of 17.6% (14.7% in men and 19.7% in women) with common mental disorder during 12-months preceding assessments. In addition, 29.2% of respondents had experienced a common mental disorder at some time during their lifetime [10]. A study among South African adults reported 28.4% prevalence of lifetime psychological distress with varying proportions of intensity, such as 10.3% prevalence of moderate levels of distress, 6.4% prevalence of high or very high levels of distress[9]. The lifetime prevalence of psychological distress was 31% among Australian adults with two-thirds reporting moderate and one-third reporting high level of psychological distress [11]. Bangladesh is one of the most densely populated countries in the world, with a population of approximately 163 million people [12]. Depression and anxiety are among the most serious causes of morbidity and mortality in Bangladesh [13–16]. An urban tertiary hospital based study reported 47% of patients with stroke and 54% of patients with cancer had severe depression in Bangladesh [17]. Despite the adverse impacts of such mental health conditions, they receive little attention in most of the low and middle-income countries, including Bangladesh, and hence, treatment of such conditions is not considered a national health priority [18, 19]. In terms of service delivery, mental health services are almost non-existent at primary care level throughout the country and the referral to hospital is mostly a long delay. A study conducted in a rural area reported that 65% of patients with the mental health condition were referred to the hospital 3 months to several years after onset of the disorder [20, 21]. In several studies, the prevalence of and risk factors for psychological distress both in urban and rural areas, both at community and facility based settings in Bangladesh, was found to vary between 6.5 and 31.0% [20].
All studies of psychological distress or depression and anxiety and their associated risk factors were conducted over a decade ago, despite significant changes in socio-demographic factors and life expectancy. For example, life expectancy in Bangladesh was 44.9 years in 1975, 58.1 years in 2000 [22] and currently 72 years in 2018 [23]. Therefore, there is a need to accurately investigate the current prevalence of and risk factors for psychological distress. It is also important to identify the groups at most risk of psychological distress at a population level in order to develop appropriate intervention and prevention strategies. The need was also highlighted by Hossain et al. in their systematic review [20]. The current study aims to estimate the prevalence of psychological distress, its severity and the associated factors, by conducting across-sectional study in people with a wide age distribution in a rural district in Bangladesh.
Materials and methods
Study location
Data were collected from the Narail upazila, which is considered to be reflective of typical rural demography in Bangladesh. Bangladesh is divided into 8 administrative divisions, each of which is divided into a number of districts and thus there are 64 districts, or zila, in total. For the purposes of local government, each district/zila is divided into a number of upazila. There are 493 upazila in total in Bangladesh with 163 million people [24]. Narail district is located approximately 150 km south-west of Dhaka, the capital city of Bangladesh, with a population of 272,872. Narail has an estimated population density of 722 people per km2, which is comparable to the national rural population density of 873 people per km2[24].
Sample size and statistical power
The sample size was calculated based on severe depression in adults of age 18 to 59 years and older adults of age 60 to 90 years. Prior prevalence of severe depression was 6.5% in adults and 21% in older adults [20]. With the assumption of margin of error of 3% in prevalence for adults, and of 5% in older adults, with a significance level of 0.05 and statistical power above 80% a required sample size of 1283 was needed for adults and 1128 for the older adults. In the current study, we ended up recruiting 1278 adults and 1147 older adults, i.e. 2425 total participants. Since the sample size is large enough to detect a minimum prevalence of 6.5%, the estimated sample size is large enough for any prevalence larger than 6.5%, as well as both in adults and older adults group, and by gender. Exclusion criteria were age <18 years or >90 years, and any severe illness preventing participants from participating in the study.
Sampling frame and recruitment
Narail upazilla consists of 13 rural unions, and an urban city known as Narail paurashova, which consists of 9 wards. Each union consists of 15–20 villages and a ward consists of 8–12 mahallas or para and each village or mahalla consists of 200 to 500 households depending on the size of the villages/mahallas. Three from 13 rural unions and one from 9 urban wards were randomly selected at cluster level 1. Two to three villages or mahallas from each selected union or ward were randomly selected at level 2. The participants from the village or mahalla were not selected at random but prioritisation was given in recruiting older adults first. The recruitment started from a corner of a village and continued until the recruitment of a maximum of 250 participants was reached for a large village where the number of eligible participants were greater than 250. In case of fewer than 250 households in a village, the recruitment continued to the adjacent village to reach the number to 250. Data were collected by three teams, each of which had 3 members. The team members participated in an intensive 2-day training programme in Narail before the commencement of data collection. The interviewers were instructed to interview an older adult first. If none were available in this subgroup, the interviewers approached an adult person of that household. Again, if there was more than one male or female adult in the same household, one individual was selected, based on who was born closer to January. However, to maintain an approximately equal number of males and female participants, one female was interview immediately after a male participant. The K10 was translated into Bengali independently by two bilingual translators including a medical practitioner with experience in public health. The K10 questionnaire was translated using back-translation techniques [25]. We have reported the study sample, recruitment strategy, and data collection previously [26].
Outcome variables
The Kessler 10 items questionnaire [27] was used for measuring psychological distress, which is the main outcome variable for this study. The Kessler 10 (K10) items is based on 10 items that measure the frequency of non-specific psychological distress symptoms during the past four weeks. Respondents were asked, “During the past four weeks, how often did you feel: 1) tired out for no good reason; 2) nervous; 3) so nervous that nothing could calm you down; 4) hopeless; 5) restless or fidgety; 6) so restless you could not sit still; 7) sad or depressed; 8) so depressed that nothing could cheer you up; 9) everything was an effort; 10) worthless.” Items were rated on a five-point ordinal scale― none of the time (score 1), a little of the time (score 2), some of the time (score 3), most of the time (score 4), and all of the time (score 5). The total K10 score for each respondent was calculated by summing all 10 items, which then ranged from a minimum of 10 to a maximum of 50. The total scores were then categorised into: no psychological distress (10 to 19), mild (20 to 24), moderate (25 to 29) and severe psychological distress (30 to 50) as per Andrews[28] and Kessler [27]. The psychometric properties of the K10 questionnaire were investigated using a Rasch analysis and proposed to be a modified version of seven items with 1 to 4 categories [29]. The total K7 score for each respondent was calculated by summing all 7 items, which then ranged from a minimum of 7 and a maximum of 28 to investigate the robustness of the findings from the K10.
Independent variables
Socio-demographic factors including age, gender and level of education were collected. Level of education was categorised into: no schooling, primary school level of education (grade 1 to 5), secondary school level of education (grade 6 to 10) and school secondary certificate (SSC) or above. Socio-economic status (SES) was assessed according to Cheng et al.[30] asking whether "over the last twelve months, in terms of household food consumption, how would you classify your socio-economic status?" with the possible answers: (i) insufficient funds for the whole year, (ii) insufficient funds some of the time, (iii) neither deficit nor surplus (balance), and (iv) sufficient funds most of the time. Data on current occupation (e.g., student, housework, daily labour, government or non-government job, business, and unable to work or retired), marital status, current health problems (yes or no), number of health problems, and medication use were also collected during the interview.
Statistical analysis
Participant characteristics including age, gender and level of education are presented for adults and older adults using descriptive statistics. We used binary logistic regression models to estimate the odds ratio (OR) and 95% confidence intervals (CI) for any psychological distress. In this case, participants were categorised into (1) no psychological distress (scores of 19 and lower) and (2) any level of psychological distress (scores of 20 and above) from the total score of 50 in association with categorical responses of the independent variables (e.g., level of education). We used multinomial logistic regression techniques to determine the odds of increasing the severity of psychological distress (normal, mild, moderate and severe) associated with different binary, multi-category or incremental categories for ordinal cut-off of quantitative variables. We also used a generalised linear model in presenting mean difference and 95% confidence interval for psychological distress score on a continuous scale ranging from 10 to 50 units for K10 items and 7 to 28 units for modified K7 items in association with categorical responses of the independent variables. All models were adjusted for age, gender, level of education, marital status, socio-economic status, occupation, smoking status, medical condition and geographic location. Statistical software SPSS (SPSS Inc, version 24) was used for the analysis.
Ethical approval
We conducted the research following the tenets of the Declaration of Helsinki. Human Ethics Approval was received from the Swinburne University of Technology Human Ethics Committee (SHR Project 2015/065). We obtained written consent from the participants who were able to sign and a finger print was obtained from those who were unable to sign. In the case of finger print consent, the data collector provided a counter signature for the participants. Participants were informed of their right to withdraw from the study at any stage if they wished.
Results
Of 2425 participants, 51.5% were female (52.8% in adults and 50% in older adults). In comparison of socio-demographic factors between adults and older adults, 13.4% vs. 43.6% had no schooling, 9% vs. 30% had house duties, 16% vs. 7.9% were labourers, 91% vs. 68% were married, 3% vs. 32% were widowed, 26% vs. 28.6% were tobacco smokers and 11.0% vs. 37.9% consumed smokeless tobacco (SLT), respectively (Table 1).
Table 1. Sociodemographic characteristic of adults and older adults in a rural district in Bangladesh.
| Characteristic | Total, N = 2425 | Adults (18–59 years), N = 1278 (52.7%) |
Older adults (60–90 years), N = 1147 (47.3%) |
|---|---|---|---|
| Gender | Number (%) | Number (%) | Number (%) |
| Female | 1249 (51.5) | 675 (52.8) | 574 (50) |
| Male | 1176 (48.5) | 603 (47.2) | 573 (50) |
| Level of education (in years) | |||
| No education | 671 (27.7) | 171 (13.4) | 500 (43.6) |
| Primary (1–5) | 946 (39.0) | 510 (39.9) | 436 (38.0) |
| Secondary (6–9) | 327 (13.5) | 238 (18.6) | 89 (7.8) |
| SSC or HSC Pass (10–12) | 385 (15.9) | 295 (23.1) | 90 (7.8) |
| Degree or equivalent (13–16) | 96 (4.0) | 64 (5.0) | 32 (2.8) |
| Socio-economic Condition: | |||
| Insufficient funds most of the time | 367 (15.1) | 172 (13.5) | 195 (17.0) |
| Insufficient funds some of the time | 781 (32.2) | 400 (31.3) | 381 (33.2) |
| Balance | 1037 (43.0) | 582 (45.5) | 455 (39.7) |
| Sufficient funds most of the time | 240 (9.9) | 124 (9.7) | 116 (10.1) |
| Occupation | |||
| Housework | 970 (40) | 629 (49) | 341 (30) |
| Student | 45 (1.9) | 40 (3.1) | 5 (0.4) |
| Farming | 217 (8.9) | 130 (10.2) | 87 (7.6) |
| Labourers | 297 (12) | 206 (16.1) | 91 (7.9) |
| Business, government or non-government job | 359 (14.9) | 262 (20.5) | 97 (88.5) |
| Retired or unable to work | 537 (22.1) | 11 (0.9) | 526 (46) |
| Marital status | |||
| Married | 1937 (80.0) | 1163 (91.0) | 774 (68) |
| Widow | 405 (17.0) | 38 (3.0) | 367 (32) |
| Unmarried/never married | 78 (3.2) | 73 (5.7) | 5 (0.4) |
| Divorce/separation | 5 (0.2) | 4 (0.3) | 1 (0.1) |
| Smoking status | |||
| Never smoker | 1180 (49.0) | 800 (62.9) | 380 (33.5) |
| Ever of current tobacco smoker | 656 (27.3) | 331 (26.0) | 325 (28.6) |
| Smokeless tobacco consumption | 570 (23.7) | 140 (11.0) | 430 (37.9) |
| Any medical condition | |||
| No | 1063 (43.9) | 803 (62.8) | 260 (22.7) |
| Yes | 1361(56.1) | 476 (37.2) | 885 (77.3) |
| Geographic location | |||
| Urban pouroshova | 685 (28.2) | 388 (56.6) | 297 (43.4) |
| Rural Banshgram | 656 (27.1) | 381 (58.1) | 275 (41.9) |
| Rural Tularampur | 501 (20.7) | 209 (41.7) | 292 (58.3) |
| Rural Vodrobilla | 583 (24.0) | 301 (51.6) | 282 (48.4) |
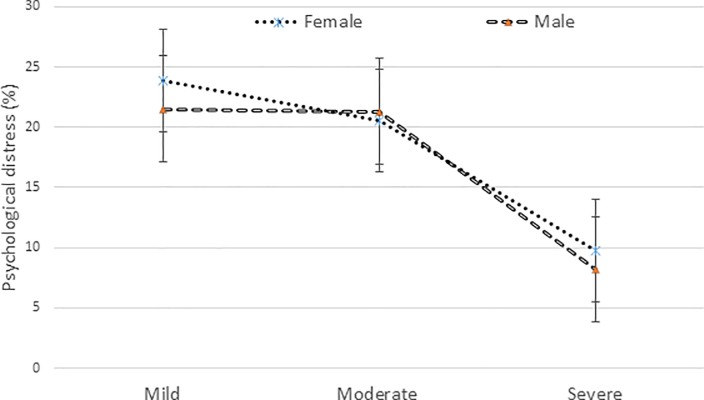
The prevalence of any level of psychological distress was 52.5% in the total sample, with a significant difference between adults and older adults (44.5% in adults vs. 61.8% in older adults, p<0.001). There was no significant difference in any psychological distress or severity of psychological distress between males and females (Fig 1). However, after the age of 60 years, the prevalence of severe psychological distress was significantly higher in females than in males; in contrast, mild psychological distress was higher in males (Fig 2). The prevalence of any psychological distress was higher in people with no education (60.1%), being widowed (70.1%), unable to work or retired (62.0%), insufficient funds most of the time (59.9%) or suffering from any health problem (58.3%) than their counterparts.
Fig 1. Different levels of psychological distress in males and females in total sample.
Fig 2. Different levels of psychological distress in males and females by age groups.
Table 2 shows individual risk factor associations for psychological distress after adjustment for age, gender, level of education, marital status, socio-economic status, occupation, smoking status, medical condition and geographic location. Compared to adults of age 18–59 years, older adults of age 60–90 years reported 50% higher prevalence of any psychological distress (odds ratio (OR) 1.50, 95% confidence interval (CI) 1.19–1.88). There was a U-shape relationship observed between the socio-economic status and any psychological distress. For example, having insufficient funds most of the time (very poor) (OR 1.65, 95% CI 1.25–2.17) or sufficient funds most of the time (wealthy) (OR 1.89, 95% CI 1.34–2.64) were associated with higher prevalence of any psychological distress compared to those with insufficient funds some of the time (poor or middle class)
Table 2. Association of socio-demographic factors with any psychological distress in the total participants using binary regression model.
| No at risk | Normal, n (%) | Any PD, n (%) | OR (95% CI)* | |
|---|---|---|---|---|
| Total | 2425 | 1149 (47.4) | 1276 (52.5) | |
| Age : Adult | 1279 | 711 (55.6) | 568 (44.4) | 1.0 |
| Elderly | 1146 | 438 (38.2) | 708 (61.8) | 1.50 (1.19, 1.88) |
| Age group: 18–29 | 247 | 144 (58.3) | 103 (41.7) | 1.0 |
| 30–39 | 423 | 245 (57.9) | 178 (42.1) | 1.05 (0.73, 1.51) |
| 40–49 | 416 | 238 (57.2) | 178 (42.8) | 1.04 (0.72, 1.52) |
| 50–59 | 193 | 84 (43.5) | 109 (56.5) | 1.58 (1.01, 2.47) |
| 60–69 | 728 | 301 (41.3) | 427 (58.7) | 1.57 (1.07, 2.31) |
| 70–79 | 315 | 108 (34.3) | 207 (65.7) | 2.88 (1.78, 4.68) |
| 80 and above | 103 | 29 (28.2) | 74 (71.8) | 3.58 (1.89, 6.78) |
| Sex: Female | 1238 | 567 (45.8) | 671 (54.2) | 1.0 |
| Male | 1187 | 582 (49.0) | 605 (51.0) | 0.94 (0.67, 1.33) |
| Education: Degree or equivalent | 96 | 48 (50.0) | 48 (50.0) | 1.0 |
| SSC or HSC pass | 385 | 212 (55.1) | 173 (44.9) | 1.09 (0.67, 1.76) |
| Secondary (6–10) | 327 | 180 (55.0) | 147 (45.0) | 1.27 (0.76, 2.12) |
| Primary (1–5) | 946 | 441 (46.6) | 505 (53.4) | 1.53 (0.95, 2.47) |
| No Education | 671 | 268 (39.9) | 403 (60.1) | 1.71 (1.03, 2.83) |
| Marital status: Married | 1937 | 975 (50.3) | 962 (49.7) | 1.0 |
| Widow | 405 | 121 (29.9) | 284 (70.1) | 1.76 (1.31, 2.36) |
| unmarired/never married | 78 | 49 (62.8) | 29 (37.2) | 0.58 (0.3, 1.11) |
| Housework | 976 | 474 (48.6) | 502 (51.4) | 1.0 |
| Occupation: Student | 45 | 20 (44.4) | 25 (55.6) | 2.69 (1.17, 6.16) |
| Farming | 217 | 105 (48.4) | 112 (51.6) | 1.22 (0.77, 1.92) |
| Labour | 220 | 115 (52.3) | 105 (47.7) | 0.94 (0.59, 1.49) |
| Business, govt. or non-govt job | 419 | 223 (53.2) | 196 (46.8) | 0.86 (0.58, 1.29) |
| unable to work or retired | 534 | 203 (38.0) | 331 (62.0) | 1.09 (0.76, 1.56) |
| SES: insufficient funds most of the time | 367 | 147 (40.1) | 220 (59.9) | 1.65 (1.25, 2.17) |
| Insufficient funds some of the time | 781 | 448 (57.4) | 333 (42.6) | 1.0 (ref) |
| Balance | 1037 | 456 (44.0) | 581 (56.0) | 1.74 (1.40, 2.15) |
| Sufficient funds most of the time | 240 | 98 (40.8) | 142 (59.2) | 1.89 (1.34, 2.64) |
| Health Problems: No | 1063 | 581 (54.7) | 482 (45.3) | 1.0 (ref) |
| Yes | 1361 | 568 (41.7) | 793 (58.3) | 1.35 (1.04, 1.74) |
| Medication use: No | 1527 | 787 (51.5) | 740 (48.5) | 1.0 |
| Yes | 898 | 362 (40.3) | 536 (59.7) | 1.14 (0.89, 1.47) |
| Smoking: Never smoker | 1180 | 617 (52.3) | 563 (47.7) | 1.0 |
| Current or past smoker | 656 | 281 (42.8) | 375 (57.2) | 1.42 (1.12, 1.81) |
| Smokeless tobacco | 570 | 236 (41.4) | 334 (58.6) | 1.11 (0.88, 1.41) |
| Geographic location: Urban pouroshova |
685 | 261 (38.1) | 424 (61.9) | 1.0 |
| Rural Banshgram | 656 | 273 (41.6) | 383 (58.4) | 0.76 (0.59, 0.97) |
| Rural Tularampur | 501 | 325 (64.9) | 176 (35.1) | 0.25 (0.19, 0.33) |
| Rural Vodrobilla | 583 | 290 (49.7) | 293 (50.3) | 0.47 (0.36, 0.6) |
OR (95% CI)* adjusted for age, gender, level of education, marital status, socio-economic condition, occupation, smoking status, medical condition and geographic location.
The association of any psychological distress in association with risk factors for adults, older adults and for males and females are shown in Table 3. Having insufficient funds most of the time was associated with higher prevalence of psychological distress both in adults and older adults. However, having sufficient funds most of the time was only associated with higher prevalence of psychological distress in older adults (OR 4.06, 95% CI 2.37–6.95). Compared to married, being widowed was significantly associated with higher prevalence of any psychological distress in older adults, especially among older males (OR 4.89, 95% CI 2.51–9.55). Compared to the urban pourashava, people living in rural unions reported lower prevalence of psychological distress. Although no education was associated with higher prevalence of any psychological distress in the total sample, it was no longer significant after stratification for adults and older adults, or for gender.
Table 3. Association of socio-demographic factors with any psychological distress for adults and older adults, and for males and females.
| Adults, N = 1278 | Older adults, N = 1147 | Females, N = 1238 | Males, N = 1187 | |||||
|---|---|---|---|---|---|---|---|---|
| Any psychological distress, N (%) | 568 (44.4) | 708 (61.8) | 671 (54.4) | 605 (51.0) | ||||
| n (%) | OR (95% CI)* | n (%) | OR (95% CI)* | n (%) | OR (95% CI)* | n (%) | OR (95% CI)* | |
| Adults | 306 (45.7) | 1.0 | 262 (43.0) | 1.0 | ||||
| Older adults | 365 (64.3) | 1.46 (1.04,2.05) | 343 (59.3) | 1.56 (1.13, 2.16) | ||||
| Sex: Female |
306 (45.7) | 1.0 | 365 (64.3) | 1.0 | ||||
| Male | 262 (43.0) | 0.72 (0.37, 1.44) | 343 (59.3) | 1.12 (0.74, 1.69) | ||||
| Education: Degree or equivalent |
33 (51.6) | 1.0 | 15 (46.9) | 1.0 | 15 (57.7) | 1.0 | 33 (47.1) | 1.0 |
| SSC or HSC pass | 131 (44.4) | 0.94 (0.51, 1.71) | 42 (46.7) | 1.10 (0.47, 2.58) | 68 (42.8) | 0.68 (0.26, 1.79) | 105 (46.5) | 1.38 (0.76, 2.48) |
| Secondary (6–10) | 97 (40.8) | 1.19 (0.62, 2.3) | 50 (56.2) | 1.64 (0.69, 3.91) | 79 (44.1) | 0.82 (0.31, 2.21) | 68 (45.9) | 1.58 (0.82, 3.03) |
| Primary (1–5) | 222 (43.4) | 1.22 (0.66, 2.29) | 283 (65.1) | 2.19 (1.0, 4.81) | 265 (53.9) | 0.96 (0.37, 2.53) | 240 (52.9) | 1.92 (1.07, 3.45) |
| No Education | 85 (49.7) | 1.67 (0.83, 3.36) | 318 (63.6) | 2.16 (0.97, 4.81) | 244 (63.9) | 1.29 (0.47, 3.5) | 159 (55) | 1.76 (0.95, 3.26) |
| Marital status: Married | 520 (44.7) | 1.0 | 442 (57.2) | 1.0 | 437 (49.8) | 1.0 | 525 (49.6) | 1.0 |
| Widow | 20 (52.6) | 1.29 (0.61, 2.73) | 264 (71.9) | 2.02 (1.44, 2.82) | 225 (67.6) | 1.32 (0.92, 1.88) | 59 (81.9) | 4.89 (2.51, 9.55) |
| unmarired/never married | 27 (37) | 0.6 (0.29, 1.23) | 2 (40) | 0.65 (0.1, 4.34) | 8 (34.8) | 0.16 (0.03, 0.86) | 21 (38.2) | 0.8 (0.39, 1.63) |
| Occupation: Homemaker |
287 (45.4) | 1.0 | 215 (62.5) | 1.0 | 496 (51.7) | 1.0 | 6 (35.3) | 1.0 |
| Student | 20 (50) | 2.16 (0.81, 5.75) | 5 (100) | — | 14 (56) | 7.56 (1.42, 40.28) | 11 (55) | 7.31 (1.48, 36.14) |
| Farmer | 54 (41.5) | 1.46 (0.66, 3.26) | 58 (66.7) | 1.47 (0.76, 2.83) | 0 | 0 | 112 (52.3) | 5.12 (1.52, 17.32) |
| Labour | 80 (48.8) | 1.57 (0.71, 3.46) | 25 (44.6) | 0.56 (0.27, 1.18) | 0 | 0 | 105 (48.2) | 3.31 (0.98, 11.21) |
| Business or any govt/non-govt job | 120 (41.1) | 0.99 (0.48, 2.04) | 76 (59.8) | 0.93 (0.53, 1.62) | 13 (56.5) | 1.05 (0.39, 2.8) | 183 (46.2) | 3.25 (0.99, 10.75) |
| unable to work or retired | 4 (36.4) | 0.86 (0.18, 4.21) | 327 (62.5) | 0.9 (0.6, 1.34) | 147 (65.9) | 1.08 (0.71, 1.66) | 184 (59.2) | 3.92 (1.17, 13.19) |
| SES: insufficient funds most of the time | 85 (49.4) | 1.51 (1.0, 2.28) | 135 (69.2) | 1.77 (1.19, 2.63) | 127 (64.8) | 1.69 (1.14, 2.50) | 93 (54.4) | 1.66 (1.10, 2.49) |
| Insufficient funds some of the time | 132 (32.9) | 1.0 (ref) | 201 (52.9) | 1.0 (ref) | 175 (43.3) | 1.0 (ref) | 158 (41.9) | 1.0 (ref) |
| Balance | 298 (51.2) | 1.58 (1.15, 2.17) | 283 (62.2) | 1.78 (1.30, 2.45) | 299 (57.9) | 1.91 (1.42, 2.58) | 282 (54.1) | 1.59 (1.17, 2.18) |
| Sufficient funds most of the time | 53 (42.7) | 0.92 (0.56, 1.51) | 89 (76.7) | 4.06 (2.37, 6.95) | 70 (57.4) | 1.63 (1.00, 2.63) | 72 (61) | 2.20 (1.35, 3.60) |
| Health Problems: No | 342 (42.6) | 1.0 | 140 (53.8) | 1.0 | 233 (45.2) | 1.0 | 249 (45.5) | 1.0 |
| Yes | 226 (47.5) | 0.98 (0.65, 1.47) | 567 (64.1) | 1.75 (1.2, 2.55) | 438 (60.7) | 1.52 (1.05, 2.18) | 355 (55.6) | 1.22 (0.84, 1.77) |
| Medication use: No | 403 (41.8) | 1.0 | 337 (59.9) | 1.0 | 383 (49.7) | 1.0 | 357 (47.2) | 1.0 |
| Yes | 165 (52.4) | 1.8 (1.15, 2.8) | 371 (63.6) | 0.86 (0.63, 1.17) | 288 (61.7) | 1.07 (0.76, 1.51) | 248 (57.5) | 1.2 (0.83, 1.73) |
| Smoking: Never smoker | 358 (44.8) | 1.0 | 205 (53.9) | 1.0 | 361 (48.1) | 1.0 | 202 (47) | 1.0 |
| Current or past smoker | 149 (45) | 1.28 (0.89, 1.82) | 226 (69.5) | 1.76 (1.23, 2.5) | 87 (77) | 1.96 (1.15, 3.35) | 288 (53) | 1.39 (1.03, 1.86) |
| Smokeless tobacco | 60 (42.9) | 0.84 (0.55, 1.29) | 274 (63.7) | 1.28 (0.94, 1.75) | 223 (59.5) | 1.06 (0.77, 1.44) | 111 (56.9) | 1.28 (0.87, 1.9) |
| Geographic Location: Urban Pourashava | 239 (61.6) | 1.0 | 185 (62.3) | 1.0 | 213 (61.6) | 1.0 | 211 (62.2) | 1.0 |
| Banshgram | 201 (52.8) | 0.62 (0.44, 0.86) | 182 (66.2) | 0.92 (0.62, 1.36) | 212 (62.9) | 0.96 (0.67, 1.36) | 171 (53.6) | 0.57 (0.4, 0.82) |
| Tularampur | 9 (4.3) | 0.02 (0.01, 0.05) | 167 (57.2) | 0.75 (0.52, 1.09) | 87 (34.5) | 0.28 (0.19, 0.42) | 89 (35.7) | 0.21 (0.14, 0.31) |
| Vodrobilla | 119 (39.5) | 0.34 (0.24, 0.48) | 174 (61.7) | 0.69 (0.47, 1.02) | 159 (52.5) | 0.59 (0.41, 0.84) | 134 (47.9) | 0.33 (0.23, 0.49) |
* OR (95% CI) adjusted for age, gender, level of education, marital status, socio-economic condition, occupation, smoking status and medical condition and geographic location.
The prevalence of mild psychological distress (adults vs. older adults: 24.4% vs. 20.9%) was higher in adults, but the prevalence of moderate (17.5% vs. 24.7%) and severe psychological distress (2.5% vs. 16.2%) was significantly higher in older adults. The prevalence of severe psychological distress was higher in older adults, especially in people with no education (21.4%), widowed (24.8%) and unable to work or retired (20.3%) compared to the overall 16.2% in the older adults (Table 4).
Table 4. Any psychological distress and it’s severity by socio-demographic factors of the total participants and by adults and older adults.
| Total | Adults | Older adults | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No at risk | Mild, n(%) | Moderate, n(%) | Severe, n(%) | No at risk | Mild, n(%) | Moderate, n(%) | Severe, n(%) | No at risk | Mild, n(%) | Moderate, n(%) | Severe, n(%) | |
| Total | 2425 | 551 (22.7) | 507 (20.9) | 218 (9.0) | 1279 | 312(24.4) | 224(17.5) | 32(2.5) | 1146 | 239(20.9) | 283(24.7) | 186(16.2) |
| Sex: Female | 1238 | 296 (23.9) | 254 (20.5) | 121 (9.8) | 670 | 175 (26.1) | 116 (17.3) | 15 (2.2) | 568 | 121 (21.3) | 138 (24.3) | 106 (18.7) |
| Male | 1187 | 255 (21.5) | 253 (21.3) | 97 (8.2) | 609 | 137 (22.5) | 108 (17.7) | 17 (2.8) | 578 | 118 (20.4) | 145 (25.1) | 80 (13.8) |
| Education: No Education | 671 | 116 (17.3) | 175 (26.1) | 112 (16.7) | 171 | 35 (20.5) | 45 (26.3) | 5 (2.9) | 500 | 81 (16.2) | 130 (26) | 107 (21.4) |
| Primary (1–5) | 946 | 255 (27) | 176 (18.6) | 74 (7.8) | 511 | 145 (28.4) | 65 (12.7) | 12 (2.3) | 435 | 110 (25.3) | 111 (25.5) | 62 (14.3) |
| Secondary (6–10) | 327 | 76 (23.2) | 58 (17.7) | 13 (4) | 238 | 53 (22.3) | 40 (16.8) | 4 (1.7) | 89 | 23 (25.8) | 18 (20.2) | 9 (10.1) |
| SSC or HSC pass | 385 | 83 (21.6) | 76 (19.7) | 14 (3.6) | 295 | 64 (21.7) | 58 (19.7) | 9 (3.1) | 90 | 19 (21.1) | 18 (20) | 5 (5.6) |
| Degree or equivalent | 96 | 21 (21.9) | 22 (22.9) | 5 (5.2) | 64 | 15 (23.4) | 16 (25) | 2 (3.1) | 32 | 6 (18.8) | 6 (18.8) | 3 (9.4) |
| Marital status: Married | 1937 | 451 (23.3) | 387 (20) | 124 (6.4) | 1164 | 284 (24.4) | 207 (17.8) | 29 (2.5) | 773 | 167 (21.6) | 180 (23.3) | 95 (12.3) |
| Widow | 405 | 83 (20.5) | 109 (26.9) | 92 (22.7) | 38 | 12 (31.6) | 7 (18.4) | 1 (2.6) | 367 | 71 (19.3) | 102 (27.8) | 91 (24.8) |
| unmarired/never married | 78 | 17 (21.8) | 10 (12.8) | 2 (2.6) | 73 | 16 (21.9) | 9 (12.3) | 2 (2.7) | 5 | 1 (20) | 1 (20) | 0 (0) |
| Occupation: Student | 45 | 14 (31.1) | 10 (22.2) | 1 (2.2) | 40 | 12 (30) | 7 (17.5) | 1 (2.5) | 5 | 2 (40) | 3 (60) | 0 (0) |
| Housewives | 976 | 249 (25.5) | 191 (19.6) | 62 (6.4) | 632 | 165 (26.1) | 108 (17.1) | 14 (2.2) | 344 | 84 (24.4) | 83 (24.1) | 48 (14) |
| land owner | 217 | 49 (22.6) | 51 (23.5) | 12 (5.5) | 130 | 23 (17.7) | 28 (21.5) | 3 (2.3) | 87 | 26 (29.9) | 23 (26.4) | 9 (10.3) |
| Labour | 220 | 47 (21.4) | 49 (22.3) | 9 (4.1) | 164 | 39 (23.8) | 35 (21.3) | 6 (3.7) | 56 | 8 (14.3) | 14 (25) | 3 (5.4) |
| Business | 282 | 74 (26.2) | 40 (14.2) | 19 (6.7) | 195 | 52 (26.7) | 25 (12.8) | 1 (0.5) | 87 | 22 (25.3) | 15 (17.2) | 18 (20.7) |
| Govt. or non-govt job | 137 | 29 (21.2) | 28 (20.4) | 6 (4.4) | 97 | 20 (20.6) | 18 (18.6) | 4 (4.1) | 40 | 9 (22.5) | 10 (25) | 2 (5) |
| unable to work or retired | 534 | 88 (16.5) | 135 (25.3) | 108 (20.2) | 11 | 1 (9.1) | 1 (9.1) | 2 (18.2) | 523 | 87 (16.6) | 134 (25.6) | 106 (20.3) |
| SES: Very poor | 367 | 111 (30.2) | 75 (20.4) | 34 (9.3) | 172 | 61 (35.5) | 20 (11.6) | 4 (2.3) | 195 | 50 (25.6) | 55 (28.2) | 30 (15.4) |
| Poor | 781 | 139 (17.8) | 121 (15.5) | 73 (9.3) | 401 | 77 (19.2) | 48 (12) | 7 (1.7) | 380 | 62 (16.3) | 73 (19.2) | 66 (17.4) |
| Middle class | 1037 | 237 (22.9) | 254 (24.5) | 90 (8.7) | 582 | 149 (25.6) | 134 (23) | 15 (2.6) | 455 | 88 (19.3) | 120 (26.4) | 75 (16.5) |
| Rich | 240 | 64 (26.7) | 57 (23.8) | 21 (8.8) | 124 | 25 (20.2) | 22 (17.7) | 6 (4.8) | 116 | 39 (33.6) | 35 (30.2) | 15 (12.9) |
| Health Problems: No | 1063 | 208 (19.6) | 232 (21.8) | 42 (4) | 803 | 165 (20.5) | 162 (20.2) | 15 (1.9) | 260 | 43 (16.5) | 70 (26.9) | 27 (10.4) |
| Yes | 1361 | 343 (25.2) | 274 (20.1) | 176 (12.9) | 476 | 147 (30.9) | 62 (13) | 17 (3.6) | 885 | 196 (22.1) | 212 (24) | 159 (18.0) |
| Medication use: No | 1527 | 312 (20.4) | 314 (20.6) | 114 (7.5) | 964 | 204 (21.2) | 179 (18.6) | 20 (2.1) | 563 | 108 (19.2) | 135 (24) | 94 (16.7) |
| Yes | 898 | 239 (26.6) | 193 (21.5) | 104 (11.6) | 315 | 108 (34.3) | 45 (14.3) | 12 (3.8) | 583 | 131 (22.5) | 148 (25.4) | 92 (15.8) |
| Smoking: Never smoker | 1180 | 277 (23.5) | 218 (18.5) | 68 (5.8) | 800 | 204 (25.5) | 139 (17.4) | 15 (1.9) | 380 | 73 (19.2) | 79 (20.8) | 53 (13.9) |
| current or past smoker | 656 | 138 (21) | 165 (25.2) | 72 (11) | 331 | 70 (21.1) | 64 (19.3) | 15 (4.5) | 325 | 68 (20.9) | 101 (31.1) | 57 (17.5) |
| Smokeless tobacco | 570 | 133 (23.3) | 123 (21.6) | 78 (13.7) | 140 | 37 (26.4) | 21 (15) | 2 (1.4) | 430 | 96 (22.3) | 102 (23.7) | 76 (17.7) |
| Geographic Location: Urban Pourashava | 685 | 144(21) | 219(32) | 61(8.9) | 388 | 100(25.8) | 118(30.4) | 21(5.4) | 297 | 44(14.8) | 101(34) | 40(13.5) |
| Banshgram | 656 | 192(29.3) | 131(20) | 60(9.1) | 381 | 122(32) | 70(18.4) | 9(2.4) | 275 | 70(25.5) | 61(22.2) | 51(18.5) |
| Tularampur | 501 | 58(11.6) | 43(8.6) | 75(15) | 209 | 7(3.3) | 0() | 2(1) | 292 | 51(17.5) | 43(14.7) | 73(25) |
| Vodrobilla | 583 | 157(26.9) | 114(19.6) | 22(3.8) | 301 | 83(27.6) | 36(12) | 0() | 282 | 74(26.2) | 78(27.7) | 22(7.8) |
Following the multivariate adjustment and using the multinomial logistic regression techniques, older age, having insufficient funds most of the time, suffering from any health problem and ever smoking were associated with the severity of psychological distress in total sample as well as in both adults and older adults. For example, among males, having insufficient funds most of the time was associated with a 153% higher prevalence of moderate psychological distress (OR 2.53, 95% CI 1.79, 3.57) and 174% higher prevalence of severe psychological distress (OR 2.74, 95% CI 1.22, 6.15) compared to people who had insufficient funds some of the time. The associations of SES with severity of psychological distress in older adults were similar to those observed in adults. Being widowed was associated with higher prevalence of moderate (OR 1.92, 95% CI 1.31, 2.80) and severe (OR 2.73, 95% CI 1.79, 4.16) psychological distress in older adults but not in adults. For older adults, smoking was associated with higher prevalence of mild (OR 1.56, 95% CI 1.11, 2.19), moderate (OR 1.71, 95% CI 1.22, 2.36) and severe (OR 1.57, 95% CI 1.07, 2.30) psychological distress but not for adults (Table 5).
Table 5. Association of socio-demographic and other characteristics with the severity of psychological distress in a multi-nominal logistic regression model by adults and older adults.
| Total | Adult | Older adult | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Normal | Mild | Moderate | Severe | Mild | Moderate | Severe | Mild | Moderate | Severe | |
| OR (95% CI) † | OR (95% CI) † | OR (95% CI) † | OR (95% CI) † | OR(95% CI) † | OR (95% CI) † | OR(95% CI) † | OR (95% CI) † | OR (95% CI) † | ||
| Older adults vs adults | 1.0 | 1.24 (1.01, 1.53) | 2.05(1.66, 2.54) | 9.44 (6.37, 14.0)** | ||||||
| Male vs. Female | 1.0 | 0.84 (0.69, 1.03) | 0.97 (0.79, 1.2) | 0.78 (0.58, 1.05) | 0.82(0.63, 1.07) | 0.98(0.72, 1.32) | 1.19(0.59, 2.42) | 0.84(0.61, 1.16) | 0.91(0.67, 1.22) | 0.65(0.46, 0.92) |
| ‡Education level | 1.0 | 1.29 (0.98, 1.69) | 0.65 (0.5, 0.84) | 0.57 (0.4, 0.8)** | 1.07(0.69, 1.64) | 0.43(0.28, 0.66) | 0.74(0.27, 2.05)** | 1.46(1.02, 2.09) | 0.83(0.6, 1.16) | 0.62(0.42, 0.91)** |
| ⁋SES | 1.0 | 1.38 (1.11, 1.72) | 2.11(1.68, 2.67) | 1.82 (1.31, 2.52)** | 1.30(0.97, 1.73) | 2.53(1.79, 3.57) | 2.74(1.22, 6.15)** | 1.41(1.0, 1.97) | 1.73(1.25, 2.39) | 1.62(1.11, 2.35)* |
| Widowed vs. married | 1.0 | 1.33 (0.94, 1.88) | 1.74 (1.25, 2.44) | 2.57 (1.73, 3.81)** | 1.34(0.63, 2.86) | 1.37(0.54, 3.42) | 1.11(0.14, 9.07) | 1.39(0.93, 2.07) | 1.92(1.31, 2.8) | 2.73(1.79, 4.16)** |
| Health problem vs. no problem | 1.0 | 1.74 (1.38, 2.19) | 0.9 (0.71, 1.15) | 1.91 (1.29, 2.83)** | 1.71(1.29, 2.27) | 0.73(0.51, 1.03) | 1.99(0.94, 4.24)** | 1.81(1.21, 2.71) | 1.12(0.79, 1.6) | 2.02(1.26, 3.24)* |
| Ever smoker vs. never smoker | 1.0 | 1.17 (0.93, 1.47) | 1.32 (1.04, 1.67) | 1.5 (1.07, 2.11)* | 0.90(0.65, 1.25) | 1.04(0.72, 1.52) | 2.45(1.05, 5.72) | 1.56(1.11, 2.19) | 1.71(1.22, 2.36) | 1.57(1.07, 2.3)* |
†Odds Ratio (95% Confidence Interval (CI)) adjusted for variables included in the model
‡Education level was not adjusted for SES and vice versa.
⁋Insufficient funds some of the time is the reference group
*indicates a significant trend with p≤0.05 and
** indicates p≤0.001.
In a generalised linear model adjusting for similar risk factors, older adults, no education, widowed, any health problem, current or past smoker and the people living in the urban pourashava were associated with higher psychological distress scores, and having insufficient funds some of the time was associated with lower psychological distress scores. The results were consistent for scores computed from the K10 items and the validated K7 items, in the total sample, and in adults and older adults as well (Table 6).
Table 6. Effect size (change in psychological distress score) in total sample, by adults and older adults for K10 and validated K7 scale.
| K10: Total | K7: Total | K10: Adults | K7: Adults | K10: Older adults | K7: Older adults | ||
|---|---|---|---|---|---|---|---|
| ΔPsychological distress score | Comparison group | Δmeans (95% CI)** |
Δmeans (95% CI)** | Δmeans (95% CI)** |
Δmeans (95% CI)** |
Δmeans (95% CI)** |
Δmeans (95% CI)** |
| Older adults | Adults | 1.53* (0.92, 2.15) | 1.06* (0.57, 1.56) | ||||
| Female | Male | 0.11 (-0.78, 1.01) | 0.004 (-0.72, 0.72) | 1.09 (-0.42, 2.6) | 0.33 (-0.87, 1.53) | 0.52 (-0.66, 1.71) | -0.38 (-1.34, 0.57) |
| No education | Degree or equivalent | 2.04* (0.66, 3.41) | 1.58* (0.48, 2.69) | 1.63* (0.09, 3.17) | 1.11 (-0.13, 2.32) | 2.54* (0.08, 4.99) | 2.12* (0.15, 4.09) |
| SSC or HSC pass | 1.88* (1.01, 2.75) | 1.16* (0.46, 1.85) | 1.42* (0.42, 2.41) | 0.76 (-0.03, 1.55) | 3.34* (1.71, 4.96) | 2.33* (1.03, 3.63) | |
| Secondary (6–10) | 1.80* (0.96, 2.65) | 1.35* (0.68, 2.03) | 1.43* (0.45, 2.42) | 1.30* (0.25, 1.81) | 1.64* (0.09, 3.18) | 1.18 (-0.06, 2.42) | |
| Primary (1–5) | .82* (0.19, 1.44) | 0.24 (-0.26, 0.74) | 0.62 (-0.23, 1.47) | 0.05 (-0.63, 0.73) | 0.76 (-0.13, 1.66) | 0.22 (-0.52, 0.92) | |
| Widowed | Married | 1.95* (1.2, 2.71) | 1.73* (1.12, 2.34) | 0.91 (-0.67, 2.49) | 0.87 (-0.39, 2.13) | 2.48* (1.52, 3.43) | 2.10* (1.33, 2.87) |
| Unmarried/ never married |
2.82* (0.98, 4.66) | 2.21* (0.74, 3.69) | 1.40 (-0.81, 3.6) | 1.27 (-0.49, 3.02) | 4.25 (-1.41, 9.92) | 2.52 (-2.03, 7.06) | |
| Student | House duties | 1.37 (-0.76, 3.5) | 0.93 (-0.78, 2.64) | -0.49 (-2.03, 1.06) | 0.04 (-1.62, 1.69) | -1.78 (-7.43, 3.87) | 2.19 (-2.35, 6.74) |
| Farmer | 0.54 (-1.69, 2.77) | 0.34 (-1.45, 2.13) | -1.4 (-3.6, 0.81) | -0.79 (-2.58, 1.00) | -4.25 (-9.92, 1.41) | 1.49 (-3.13, 6.1) | |
| Labour | 1.58 (-0.61, 3.77) | 1.26 (-0.5, 3.02) | 0.28 (-1.8, 2.36) | 0 (-1.75, 1.75) | 3.18 (-2.48, 8.84) | 2.77 (-1.96, 7.51) | |
| Business, Govt/ non-govt job |
1.92 (-0.22, 4.07) | 1.44 (-0.29, 3.16) | -1.35 (-3.6, 0.91) | 0.64 (-1.07, 2.35) | 2.3 (-3.45, 8.05) | 2.02 (-2.56, 6.6) | |
| unable to work or retired |
0.3 (-1.88, 2.47) | 0.21 (-1.55, 1.94) | -0.43 (-2.62, 1.77) | -1.94 (-4.74, 0.86) | 3.73 (-2.17, 9.63) | 1.96 (-2.55, 6.48) | |
| Insufficient funds some of the time | Insufficient fund all the time |
-0.98* (-1.7, -0.23) | -0.71* (-1.31, -0.12) | -0.29 (-1.19, 0.61) | -0.20 (-0.92, 0.51) | -1.36* (-2.51, -0.2) | -0.99* (-1.91, -0.06) |
| Medium (not good or bad) |
-1.54* (-2.1, -0.97) | -1.31* (-2.77, -0.86) | -1.05*(-1.70, -0.39) | -0.93* (-1.45, -0.4) | -1.82*(-2.76, -0.89) | -1.49* (-2.24, -0.74) | |
| Sufficient funds all the time | -2.15 (-3.04, -1.25) | -2.20 (-2.92, -1.48) | -0.95 (-2.02, 0.11) | -1.29* (-2.14, -0.44) | -3.12 (-4.55, -1.7) | -2.96* (-4.1, -1.82) | |
| Any health problem | No | 1.18* (0.49, 1.87) | .97* (0.42, 1.53) | 0.95 (-0.11, 2.02) | -0.05 (-0.72, 0.62) | 3.12* (1.7, 4.55) | 2.04* (1.15, 2.93) |
| On medication | No | 0.21 (-0.45, 0.86) | 0.42 (-0.11, 0.95) | -0.09 (-1.07, 0.88) | 1.30* (0.56, 2.04) | 1.30 (-0.05, 2.66) | -0.12 (-0.86, 0.61) |
| Current or past smoker | Never smoker | 1.02* (0.39, 1.66) | .87* (0.36, 1.38) | -0.1 (-0.95, 0.74) | 0.72* (0.11, 1.33) | 2.44* (1.33, 3.54) | 1.38* (0.56, 2.2) |
| Smokeless tobacco | 0.70 (-0.02, 1.42) | .68* (0.11, 1.26) | 1.41* (0.48, 2.34) | 0.97* (0.14, 1.81) | -0.51 (-1.42, 0.4) | .80* (0, 1.6) | |
| Pouroshoba | Bashgram | 1.36* (0.7, 2.03) | 1.44* (0.9, 1.97) | 2.18* (1.45, 2.92) | 2.04* (1.45, 2.63) | 0.4 (-0.74, 1.53) | 0.72 (-0.19, 1.63) |
| Tularampur | 4.31* (3.61, 5.02) | 3.73* (3.16, 4.29) | 7.95* (7.09, 8.8) | 6.81* (6.12, 7.49) | 1.01 (-0.1, 2.11) | 0.95* (0.07, 1.84) | |
| Vodrobila | 3.26* (2.58, 3.95) | 2.88* (2.32, 3.42) | 3.90* (3.12, 4.68) | 3.25* (2.63, 3.86) | 2.55* (1.41, 3.69) | 2.43* (1.51, 3.34) |
*Indicates significant changes compared to the reference groups
**Difference in means (95% CI) adjusted for age, gender, level of education, marital status, socio-economic condition, occupation, smoking status and medical condition and geographic location.
Discussion
Our study reported the prevalence of psychological distress, its severity and its associations with socio-demographic, lifestyle and medical conditions in a typical rural district in Bangladesh. Using the internationally validated K10 psychological distress measuring tool[27], we report that overall 52.5% of adults had any psychological distress—44% in people who were younger than 60 years of age and 62% in people who were older or equal to 60 years of age. Severe psychological distress was nine times more likely in older adults compared to younger adults. The study adds further evidence of high prevalence of psychological distress to a literature that was lacking current data for more than a decade.
The prevalence of psychological distress is higher in our study but the risk factors are found to be similar to previous studies. Results from a systematic review reported a wide variation of depressive symptoms in Bangladesh between 6.5 to 31.0% [20]. Choudhury et al. [31] reported the highest prevalence of 65% in a disaster affected area, with a higher percentage in females in Bangladesh. The prevalence of 6.5% was self-reported psychological distress for which data were collected from people of all ages from a single rural village in 1981. Prevalence of 31% was also self-reported psychological distress for which data were collected from people of age 13 years or older from a tertiary care hospital in 1975. The studies reported lower prevalence of psychological distress in rural areas, such as 6.5% to 16.5%, compared to 28% to 31.5% in urban areas [20]. Although our study suggested higher prevalence of psychological distress, the wide variation and lower prevalence in previous studies can be attributed to the use of different protocols, age ranges, assessment tools and different definitions of disease outcomes. The higher prevalence of psychological distress in urban areas is consistent with the previous studies in Bangladesh, and contradict those reported in Australian and US studies, which found higher prevalence of psychological distress in rural areas [11, 32].
Although there was no significant difference in overall prevalence of any psychological distress or severity of psychological distress between males and females, severity of psychological distress was found to be significantly higher in females after the age of 60 years, and these results are consistent with previous findings [33–37]. Higher prevalence of psychological distress multi-factorial in cause, and include lack of access to, and utilisation of, mental health services, stigma about mental health treatment, poor physical health, other medical conditions, disability and isolation [11, 38], and low SES [38, 39]. In our study, factors such as no education, being widowed, unable to work or being retired, and suffering from any medical condition were associated with higher prevalence of severe psychological distress, especially in older women. These findings are also consistent with the previous findings [34, 38]. This higher prevalence in females can also be explained by the fact that females are more susceptible to the established risk factors of psychological distress such as lower level of education and less engagement in any income generation activities in Bangladesh [40]. For example, our data showed that among people with no education, 57% were females and 43% were males, among widowed adults, 82% were females and 18% were males, among people having government or non-government jobs, 10% were females vs. 90% were males. Poor financial situation, especially in developing countries is also more frequent among females, which is reported to be associated with higher prevalence of psychological distress [41–43]. A study by the World Health Organisation reports that women who had experienced severe abuse, either physical, mental or sexual abuse, independently of the time period, also experienced more psychological distress in their older age [44]. Globally, sexual violence is experienced more by girls and women, and there is a strong association between being sexually abused in childhood and the presence of multiple mental health problems later in life [33, 44], although these findings can not be verified from the current study as these data were not collected. This indicates that being of female gender is not inherently associated with higher prevalence of psychological distress but the established risk factors are higher in females, which can be the main reason for higher prevalence of psychological distress, especially in older age women [40].
Insufficient funds most of the time (i.e. very poor) was associated with higher prevalence of psychological distress, both in males and females. Although Bangladesh has shown significant economic growth in recent years [45], 24.3% people still live under the poverty line and 12.9% live under an extreme poverty line, which is higher in rural areas than those in urban areas [46]. Gross family income not only impacts daily life, it is also associated with a low level of education, higher rate of unemployment, and poor or no medical facilities, and this leads to a severe psychological distress and poor quality of life. Interestingly, our data show a parabolic relationship between socio-economic status and psychological distress. That is, sufficient funds most of the time was also associated with higher prevalence of psychological distress compared to those with insufficient funds some of the time (poor to middle class). The causes of such an association in Bangladesh is difficult to explain. However, it is comparable to the global fact that the prevalence of depression and anxiety in some high income countries such as in France and United States is higher than that in lower-middle income countries such as in Brazil, India and China [47]. Cruza-Guet[48] reported a similar parabolic relationship between psychological distress and social support from a study of psychological distress among Hispanic elderly in USA, indicating both lower and higher level of facilities may cause more psychological distress than a medium level of facilities. Moreover, we have found that the prevalence of psychological distress was the lowest in people who are daily labourers and have claimed to have insufficient funds some of the time (poor), which indicates people with a reasonable income can lead a less distressful life than their relatively rich and very poor counterparts.
Although literature does exist on psychological distress and socio-economic condition in Bangladesh [20], the literature on smoking and psychological distress is very limited. The current study reports associations of smoking with psychological distress in older adults, both in males and females. From a cross-sectional study, Islam and Hossain [49] reported a similar association of smoking with higher prevalence of psychological distress, among the healthy adults university students Literature suggests that people with mental health problems have a higher prevalence of smoking than the general population [50]. At the same time, smoking has been reported to be linked to mental health conditions, either as a consequence or as a cause [43, 51]. Therefore, whether smoking causes psychological distress or vice versa is unknown and it cannot be explained from this cross-sectional study. Although data were collected from a rural upazila, some data were collected from the typical rural unions where no urban facilities exist and some data were collected from upazila headquarters which is an urban area. The current study shows that the prevalence of psychological distress was higher in urban pourashava compared to that in rural unions which is consistent with the previous studies [20].
The advantage of the present study is that it included a large sample with a wide age distribution and which collected data directly through a face-to-face interview from adults and older adults, with almost 50% female participants and 1147 people were 60 years of age or older. The study has reported the prevalence of and risk factors for psychological distress, both for adults and older adults separately with sufficient statistical power. The data was derived from a comprehensive questionnaire that included socio-demographic and medical factors along with smoking status reported either through smoking tobacco or use of SLT. Psychological distress was measured using the K10 questionnaire, which has been widely used. The psychometric properties were tested for the K10 questionnaire and a modified 7-item questionnaire was proposed. To check the robustness, both K10 and validated K7 were used to report the factors associated with the psychological distress score. Both K10 and K7 showed robust findings. It is also possible to report the associations of not only any psychological distress but also the severity of psychological distress with the risk factors due to the large sample size.
The study has a number of limitations. Firstly, data were collected from one district and thus the results may not be generalised at the national level. Whilst the sample was representative of the situation in Narail district, and the rural population is very homogenous in Bangladesh, the study’s results need to be extrapolated with caution to other rural parts of Bangladesh. Secondly, data on smoking and SLT use, and medical condition were based on self-report response. Reporting bias, reporting error and different perceptions about health conditions are very likely dependent on disease severity and the level of knowledge of the participants. Thirdly, the subjectivity in reporting availability of funds is not the most appropriate measure of SES. Therefore, the association of medical condition, SES and smoking with psychological distress need to be evaluated with caution. Fourthly, some key predictors such as history of mental health problems, exposure to violence, and other traumatic experiences were not included in the questionnaire.
Conclusions
The prevalence of psychological distress in a rural area in Bangladesh was considerably high. Generally, the prevalence of mild psychological distress was similar in males and females but the prevalence of moderate and severe psychological distress in females showed a sharp increase after the age of 60 years. The risk factors associated with psychological distress in this sample included older age, low SES, being widowed, being unable to work and having a medical condition. The study suggests that hypertension, diabetes and other chronic diseases are closely linked and suggest a need for management through a common strategy.
Supporting information
(SAV)
Acknowledgments
There are many people to acknowledge for this manuscript. I would like to thank Dr Minh Huynh and Shenae Calleja for their critical review of the manuscript. I am grateful to Dr Ben Bullock, Senior Lecturer of Psychological Sciences, Swinburne University of Technology, for reviewing the manuscript for language and grammar. Thanks to Mohammed Naziumuddin for his data preparation. I would like to thank Md Rafiqul Islam and Mr Arzan Hosen for their contribution to questionnaire preparation, data collection and data entry. I would like to express my gratitude to the study participants for their voluntary participation.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author received $3000 for data collection from the Swinburne University of Technology RDGS grant. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med. 2013;43(5):897–910. 10.1017/S003329171200147X . [DOI] [PubMed] [Google Scholar]
- 2.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–86. 10.1016/S0140-6736(13)61611-6 . [DOI] [PubMed] [Google Scholar]
- 3.WHO. "Depression: let’s talk" says WHO, as depression tops list of causes of ill health. 2017.
- 4.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2017. 2017. [Google Scholar]
- 5.Baxter AJ, Scott KM, Ferrari AJ, Norman RE, Vos T, Whiteford HA. Challenging the myth of an "epidemic" of common mental disorders: trends in the global prevalence of anxiety and depression between 1990 and 2010. Depress Anxiety. 2014;31(6):506–16. 10.1002/da.22230 . [DOI] [PubMed] [Google Scholar]
- 6.World health report: Mental disorders affect one in four people [Internet]. 2001. Available from: http://www.who.int/whr/2001/media_centre/press_release/en/.
- 7.Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Preventing chronic disease. 2006;3(2):A42 [PMC free article] [PubMed] [Google Scholar]
- 8.Health statistics and information systems Estimates for 2000–2012, Global summmary estimates. 2016.
- 9.Lincoln KD, Taylor RJ, Watkins DC, Chatters LM. Correlates of Psychological Distress and Major Depressive Disorder Among African American Men. Res Soc Work Pract. 2011;21(3):278–88. 10.1177/1049731510386122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. International journal of epidemiology. 2014;43(2):476–93. 10.1093/ije/dyu038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kilkkinen A, Kao-Philpot A, O'Neil A, Philpot B, Reddy P, Bunker S, et al. Prevalence of psychological distress, anxiety and depression in rural communities in Australia. Australian Journal of Rural Health. 2007;15(2):114–9. 10.1111/j.1440-1584.2007.00863.x WOS:000253902400008. [DOI] [PubMed] [Google Scholar]
- 12.Vital Statistics: Bangladesh Bureau of Statistics 2013.
- 13.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–8. 10.1016/S0140-6736(07)61415-9 . [DOI] [PubMed] [Google Scholar]
- 14.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bulletin of the World Health Organization. 2003;81(8):609–15. WOS:000185162800010. [PMC free article] [PubMed] [Google Scholar]
- 15.Lamers F, van Oppen P, Comijs HC, Smit JH, Spinhoven P, van Balkom AJLM, et al. Comorbidity Patterns of Anxiety and Depressive Disorders in a Large Cohort Study: the Netherlands Study of Depression and Anxiety (NESDA). J Clin Psychiat. 2011;72(3):341–8. 10.4088/JCP.10m06176blu WOS:000288838100010. [DOI] [PubMed] [Google Scholar]
- 16.Egede LE. Effect of comorbid chronic diseases on prevalence and odds of depression in adults with diabetes. Psychosom Med. 2005;67(1):46–51. 10.1097/01.psy.0000149260.82006.fb . [DOI] [PubMed] [Google Scholar]
- 17.Karim ME, Firoz AHM, MF A. Assessment of Depression in Parkinson’s disease, Psoriasis, Stroke, and Cancer patients. Bang J Psychiatry 2001;15(2):11–8. [Google Scholar]
- 18.Bruckner TA, Scheffler RM, Shen G, Yoon J, Chisholm D, Morris J, et al. The mental health workforce gap in low- and middle-income countries: a needs-based approach. B World Health Organ. 2011;89(3):184–94. 10.2471/Blt.10.082784 WOS:000288406200009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hock RS, Or F, Kolappa K, Burkey MD, Surkan PJ, Eaton WW. A new resolution for global mental health. Lancet. 2012;379(9824):1367–8. WOS:000302806800005. 10.1016/S0140-6736(12)60243-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hossain MD, Ahmed HU, Chowdhury WA, Niessen LW, Alam DS. Mental disorders in Bangladesh: a systematic review. BMC Psychiatry. 2014;14:216 10.1186/s12888-014-0216-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chowdhury SH, Muztaba S, A H. Referral pattern of psychiatric patients to pabna mental hospital. Ban J Psychiatry 1995;7(1):9–12. [Google Scholar]
- 22.Khan HTA, Raeside R. SOCIO-DEMOGRAPHIC CHANGES IN BANGLADESH:A STUDY ON IMPACT. BRAC University Journal. 2005;II:1–11. [Google Scholar]
- 23.WHO. Life Expectancy WHO: Bangladesh profile 2018.
- 24.Bangladesh Bureau of Statistics. Population and Housing Census. 2011.
- 25.Brislin RW. Back-Translation for Cross-Cultural Research. J Cross Cult Psychol. 1970;1(3):185–216. 10.1177/135910457000100301 WOS:A1970Y151500001. [DOI] [Google Scholar]
- 26.Uddin MN, Bhar S, Al Mahmud A, Islam FMA. Psychological distress and quality of life: Rationale and protocol of a prospective cohort study in a rural district in Bangladesh. BMJ Open. 2017. htt. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler R.C., Andrews G, al. CLJe. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002. 2002;32(6):959–76. [DOI] [PubMed] [Google Scholar]
- 28.Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust N Z J Public Health. 2001;25(6):494–7. . [DOI] [PubMed] [Google Scholar]
- 29.Uddin MN, Islam FMA, Al Mahmud A. Psychometric evaluation of an interview-administered version of the Kessler 10-item questionnaire (K10) for measuring psychological distress in rural Bangladesh. BMJ open. 2018;8(6):e022967 10.1136/bmjopen-2018-022967 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng YH, Chi I, Boey KW, Ko LS, Chou KL. Self-rated economic condition and the health of elderly persons in Hong Kong. Social science & medicine. 2002;55(8):1415–24. . [DOI] [PubMed] [Google Scholar]
- 31.Choudhury WA, Quraishi FA, Haque Z. Mental health and psychosocial aspects of disaster preparedness in Bangladesh. Int Rev Psychiatr. 2006;18(6):529–35. 10.1080/09540260601037896 WOS:000242763900007. [DOI] [PubMed] [Google Scholar]
- 32.Hoyt DR, Conger RD, Valde JG, Weihs K. Psychological distress and help seeking in rural America. Am J Community Psychol. 1997;25(4):449–70. . [DOI] [PubMed] [Google Scholar]
- 33.WHO. Gender and Mental Health World Health Organisation, Geneva, Swizerland 2002.
- 34.Arslantas D, Unsal A, Ozbabalik D. Prevalence of depression and associated risk factors among the elderly in Middle Anatolia, Turkey. Geriatr Gerontol Int. 2014;14(1):100–8. 10.1111/ggi.12065 . [DOI] [PubMed] [Google Scholar]
- 35.Assil SM, Zeidan ZA. Prevalence of depression and associated factors among elderly sudanese: a household survey in Khartoum State. East Mediterr Health J. 2013;19(5):435–40. . [PubMed] [Google Scholar]
- 36.Rajkumar AP, Thangadurai P, Senthilkumar P, Gayathri K, Prince M, Jacob KS. Nature, prevalence and factors associated with depression among the elderly in a rural south Indian community. International psychogeriatrics / IPA. 2009;21(2):372–8. 10.1017/S1041610209008527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Das J, Farzana FD, Ferdous F, Ahmed S, Tegenfeldt S, R.C. P, et al. Factors Associated with Elderly Depression among Rural Bangladeshi Individuals. American Journal of Psychiatry and Neuroscience. 2014;2(1):1–7. 10.11648/j.ajpn.20140201.11 [DOI] [Google Scholar]
- 38.Alexopoulos GS. Depression in the elderly. Lancet. 2005;365(9475):1961–70. 10.1016/S0140-6736(05)66665-2 . [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization. The world health report: 2001 Mental health: new understanding, new hope. Geneva: WHO; 2001. 2001. [Google Scholar]
- 40.Zaman MA, Kabir MS, ALI RN, Markovic MR. Gender Inequality in Bangladesh Journal of Women’s Entrepreneurship and Education 2015;3–4:54–64. [Google Scholar]
- 41.Nasreen HE, Kabir ZN, Forsell Y, Edhborg M. Prevalence and associated factors of depressive and anxiety symptoms during pregnancy: a population based study in rural Bangladesh. BMC women's health. 2011;11:22 10.1186/1472-6874-11-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tareque MI, Begum S, Saito Y. Gender differences in disability-free life expectancy at old ages in Bangladesh. J Aging Health. 2013;25(8):1299–312. 10.1177/0898264313501388 . [DOI] [PubMed] [Google Scholar]
- 43.Ballbe M, Martinez-Sanchez JM, Gual A, Martinez C, Fu M, Sureda X, et al. Association of second-hand smoke exposure at home with psychological distress in the Spanish adult population. Addict Behav. 2015;50:84–8. 10.1016/j.addbeh.2015.06.020 . [DOI] [PubMed] [Google Scholar]
- 44.WHO. WHO Multi-country Study on Women's Health and Domenstic Violence (preliminary results, 2001). Geneva, World Health Organisation (unpublished document) 2001. [Google Scholar]
- 45.Bloom DE, Williamson JG. Demographic Transisios and Economic Miracles in Emerging Asia. The World Bank Economic Review 2013;12:419–55. [Google Scholar]
- 46.ADB. Poverty in Bangladesh Asian Development Bank 2017.
- 47.Mental Health Atlas 2014. 2014.
- 48.Cruza-Guet MC, Spokane AR, Caskie GI, Brown SC, Szapocznik J. The relationship between social support and psychological distress among Hispanic elders in Miami, Florida. J Couns Psychol. 2008;55(4):427–41. 10.1037/a0013501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Islam MA, Hossin MZ. Prevalence and risk factors of problematic internet use and the associated psychological distress among graduate students of Bangladesh. Asian J Gambl Issues Public Health. 2016;6(1):11 10.1186/s40405-016-0020-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. JAMA. 2000;284(20):2606–10. . [DOI] [PubMed] [Google Scholar]
- 51.Morissette SB, Tull MT, Gulliver SB, Kamholz BW, Zimering RT. Anxiety, anxiety disorders, tobacco use, and nicotine: a critical review of interrelationships. Psychol Bull. 2007;133(2):245–72. 10.1037/0033-2909.133.2.245 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.