Abstract
Background
This is an excerpt from chapter 4 of the annual registry report from the Australia and New Zealand islet and pancreas transplant registry. The full report is available at http://anziptr.org/reports/.
Methods
We report data for all allogeneic islet isolation and transplant activity from 2002 to end 2017. Solid organ pancreas transplantation activity is reported separately. New Zealand does not have an islet transplant program. Data analysis was performed using Stata software version 14 (StataCorp, College Station, TX).
Results
From 2002 to 2017, a total of 104 allogeneic islet transplants were performed in 62 recipients.
Conclusions
The number of islet transplants performed in Australia was slightly lower in 2017 but continues to increase over time.
Overview of Islet Transplantation
Islet transplants are a treatment for type 1 diabetics who have hypoglycemic unawareness and/or severe metabolic instability, are sensitive to insulin, but who have minimal or no kidney impairment. Pancreatic islets are isolated from whole donor pancreas organs and are infused into the liver of transplant recipients via the portal vein. Islet transplant recipients generally require more than 1 islet transplant to become insulin-independent.
Data for islet transplant donors and recipients in Australia are still sparse. The islet transplant program started in 2002. There are 2 islet isolation facilities in Australia; St Vincent's Hospital Melbourne in Victoria, and Westmead Hospital in New South Wales. There are 3 active islet transplant centers: the National Pancreas Transplant Unit at Westmead Hospital, St Vincent's Hospital Melbourne, and the Royal Adelaide Hospital. There is no islet transplant program in New Zealand.
We have only reported islet donors and procedures that were intended to be used for an islet transplantation and not islet isolation procedures that were undertaken for research purposes only. Some donor isolations intended for transplantation did not proceed to transplantation, generally because the pancreas processing failed to meet release criteria, with the major reason being insufficient concentrations of islet cells.
Islet Waiting List Activity
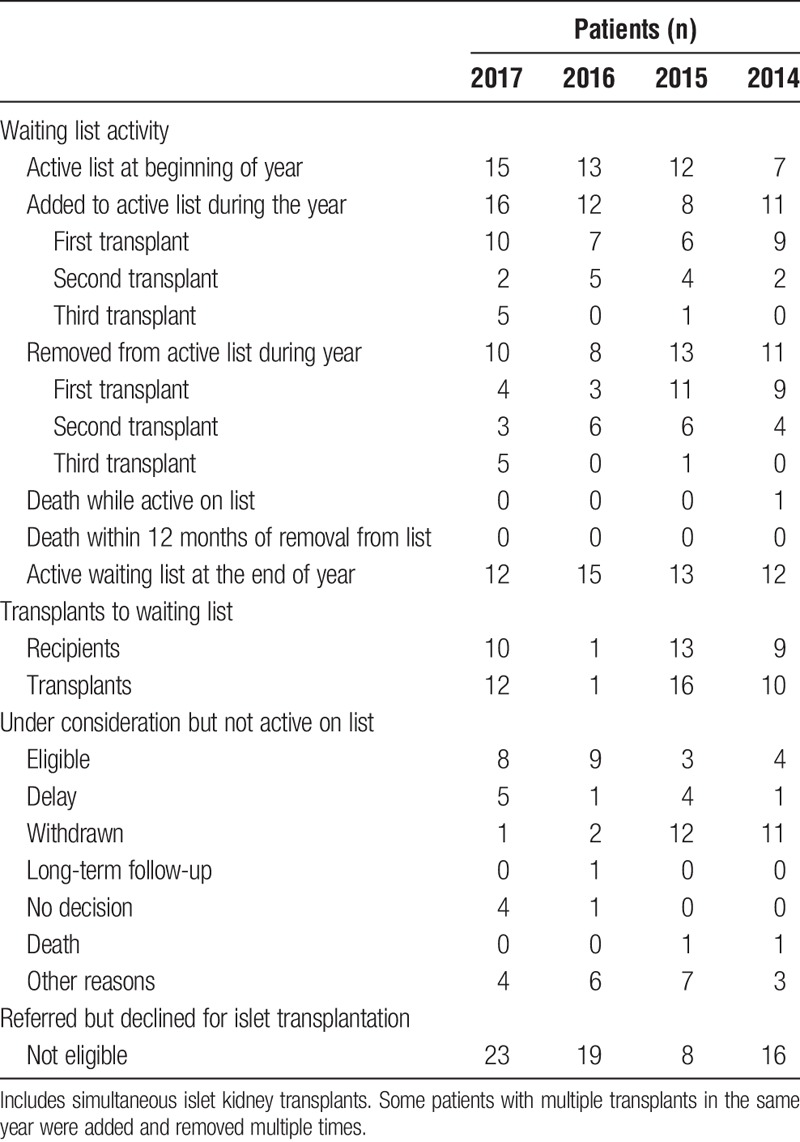
The islet program waiting list is intentionally not long. Table 1 shows the number of patients referred for an islet transplant in 2017 by state of residence and the transplant center they were referred to. Table 2 shows the number of patients accepted onto an islet waiting list during 2017, whereas Table 3 shows the islet waiting list activity over time.
TABLE 1.
Referrals for allogeneic islet transplant during 2017 by state of residence and transplant center they were referred to
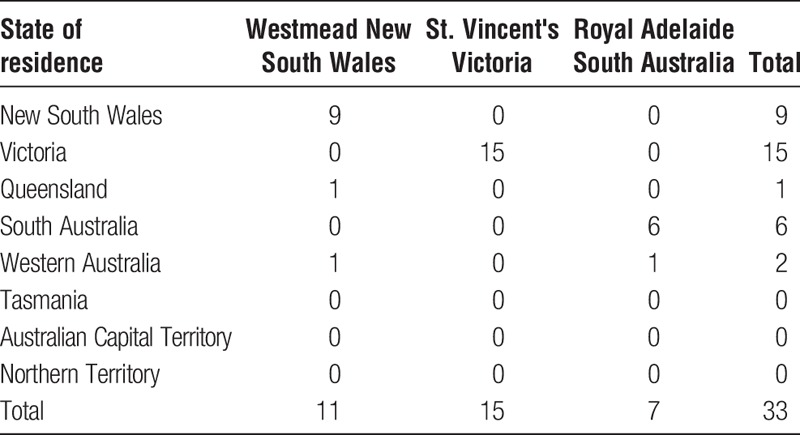
TABLE 2.
Patients accepted onto a waiting list for an allogeneic islet transplant during 2017 by state of residence and transplant center they were referred to
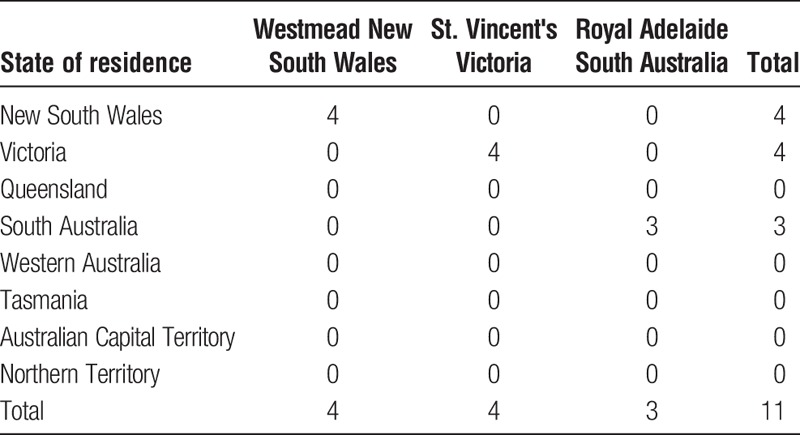
TABLE 3.
Islet waiting list status over time; Westmead Hospital (New South Wales), St Vincent's Hospital (Victoria), Royal Adelaide Hospital (South Australia)
Islet Isolations
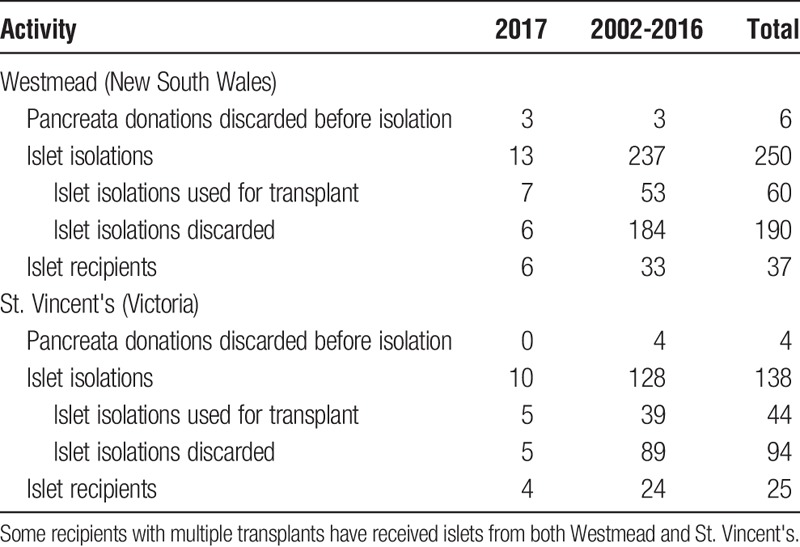
Islet isolation procedures follow good manufacturing procedure guidelines as set out by the Australian Therapeutic Goods Administration. The decision to proceed with transplantation is made once release criteria are met. Release criteria establish quality and quantity of the isolation and include absence of bacteria, absence of endotoxin, and a minimum concentration of 4000 IEQ/kg. Isolations occur at 1 of 2 dedicated isolation facilities at Westmead (Sydney) and St. Vincent's Institute (Melbourne). Islet preparations that meet release criteria may be transplanted locally or transported to 1 of the other 2 centers for transplantation, depending on patient and islet characteristics. A summary of islet cell isolation activity by center and year is presented in Table 4.
TABLE 4.
Summary of allogeneic islet cell isolation activity, for all centers in Australia
The donor characteristics of islet cell donor isolations are presented in Table 5. Donor characteristics are influenced in part by the Australian donor pancreas allocation policy which allocates pancreata for both pancreatic islet isolation and for whole pancreas transplantation. This policy is available at https://www.tsanz.com.au/organallocationguidelines/index.asp. Please note that solid organ pancreas transplant activity is also reported by the registry, and an extract is also published for 20171 and for 2018.2
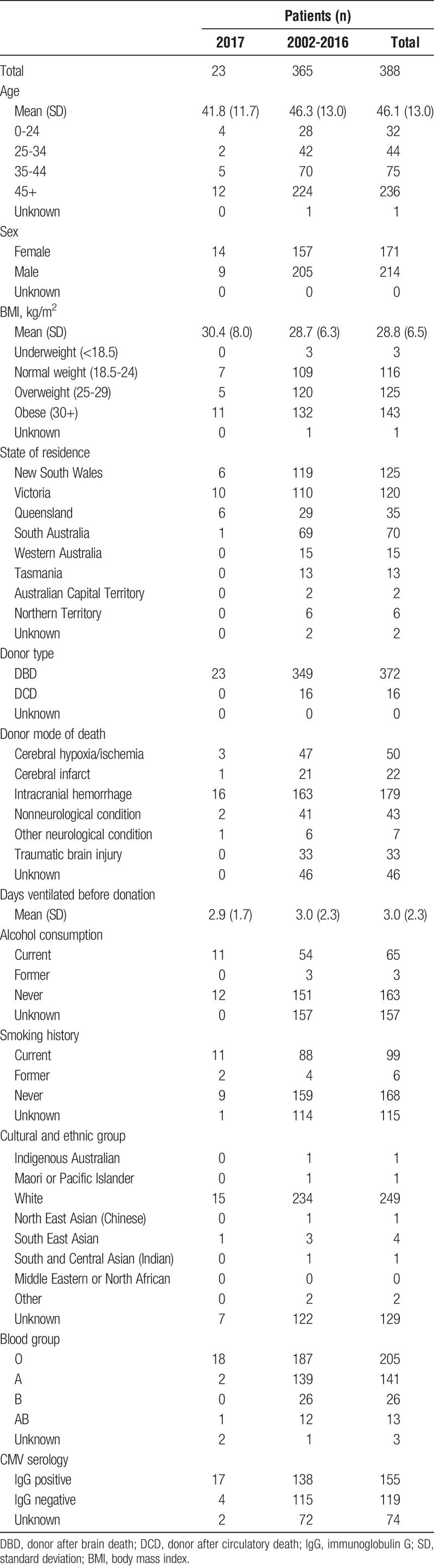
TABLE 5.
Donor characteristics for allogeneic islet isolations (all centers)
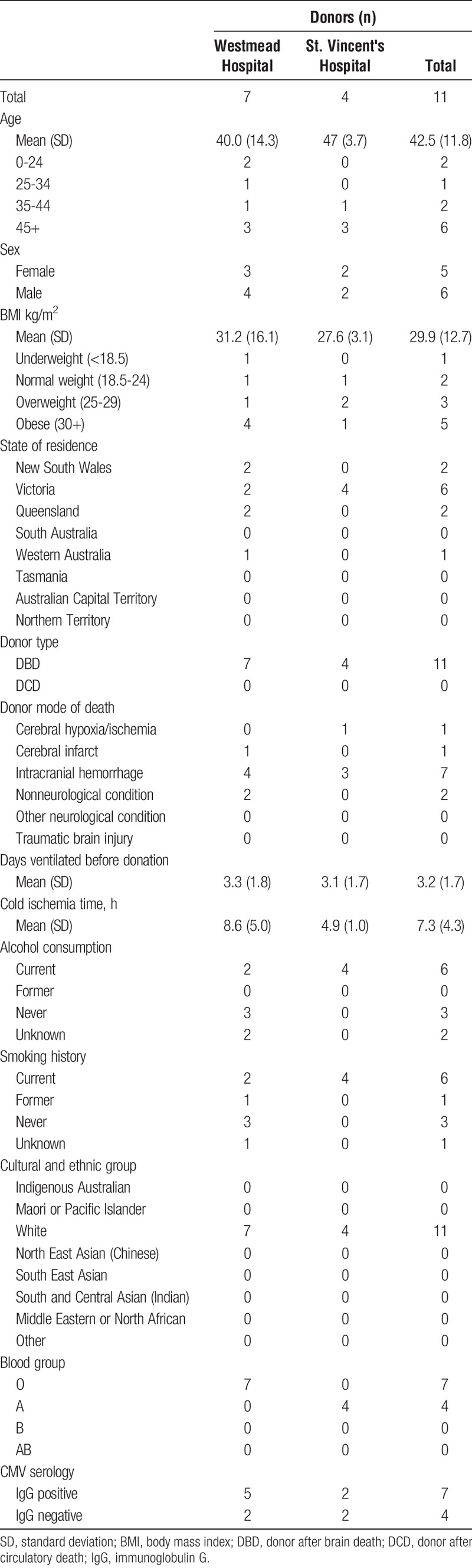
Donors who provided pancreata that resulted in islet isolations that proceeded to transplantation are summarized in Table 6.
TABLE 6.
Donor characteristics for allogeneic islet isolations which resulted in transplantation in 2017
Islet Transplant Recipients
Figure 1 illustrates the number of islet cell transplants in Australia between 2002 and 2017. The transplants were performed in Westmead (58), St Vincent's (29), and Royal Adelaide (17) Hospitals. In 2017, 7 transplants were performed at Westmead, 5 at St Vincent's and none at the Royal Adelaide.
FIGURE 1.
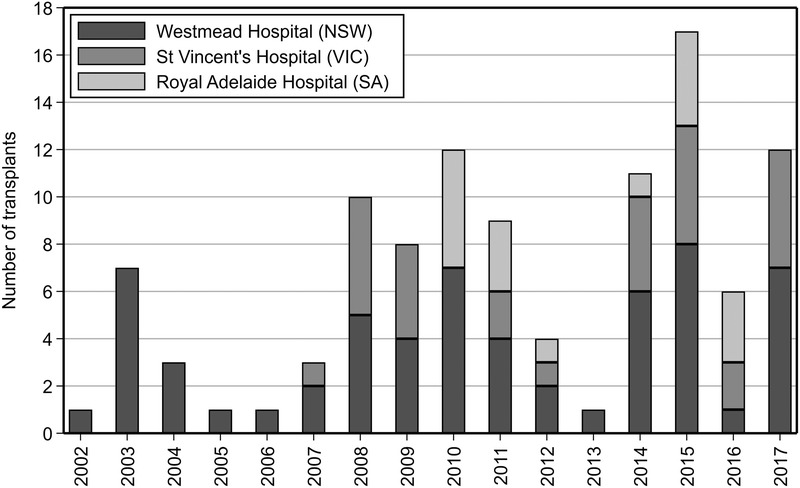
Allogeneic islet transplant activity 2002 to 2017, by transplanting center.
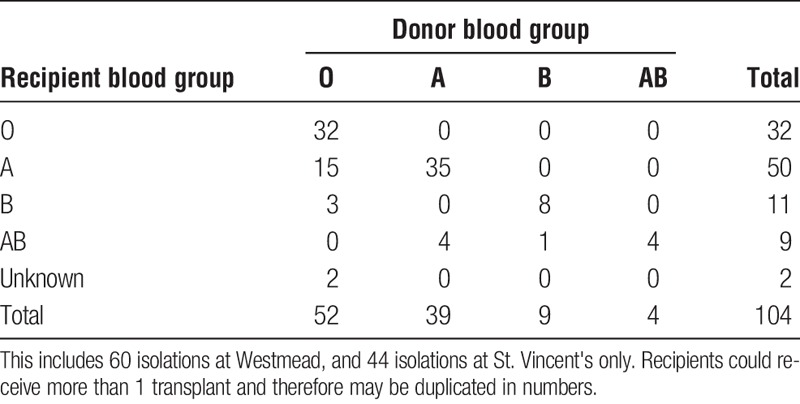
The characteristics of donor and recipient matches according to sex and blood group distributions for all centers are presented in Table 7 and Table 8.
TABLE 7.
Cross tabulation of recipient and donor sex, 2002-2017
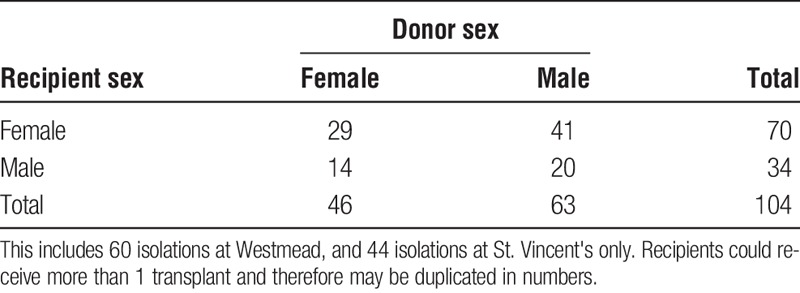
TABLE 8.
Cross tabulation of recipient and donor blood groups, 2002-2017, for allogeneic islet transplants undertaken in Australia
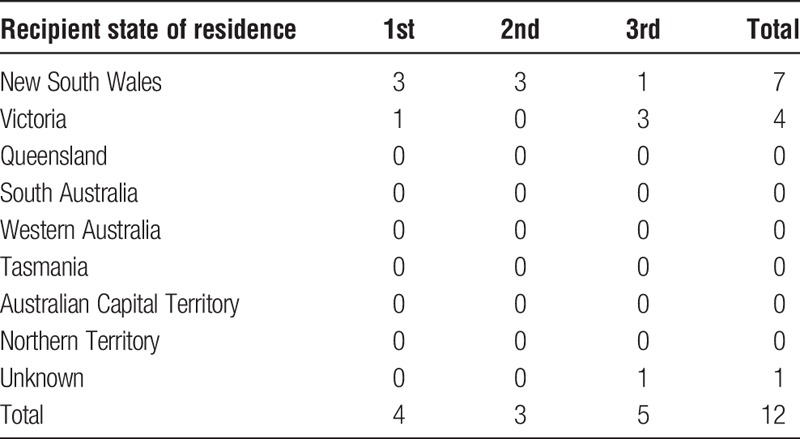
State of residence of recipients receiving an islet transplant in 2017, by the order of their transplant is presented in Table 9.
TABLE 9.
Allogeneic islet transplant recipients by state of residence and number of transplants received (all centers, 2017)
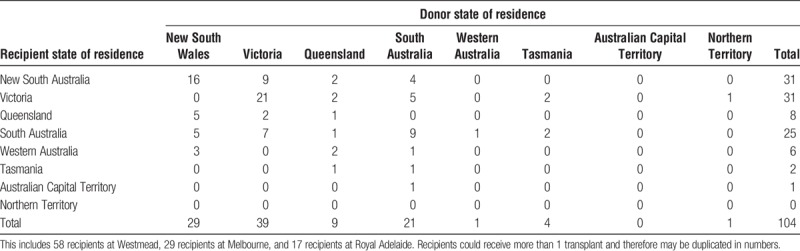
The states of residence of donors and recipients for each transplantation are shown in Table 10, stratified by the transplant center.
TABLE 10.
Cross-tabulation of allogeneic islet donor and recipient state of residence 2002-2017
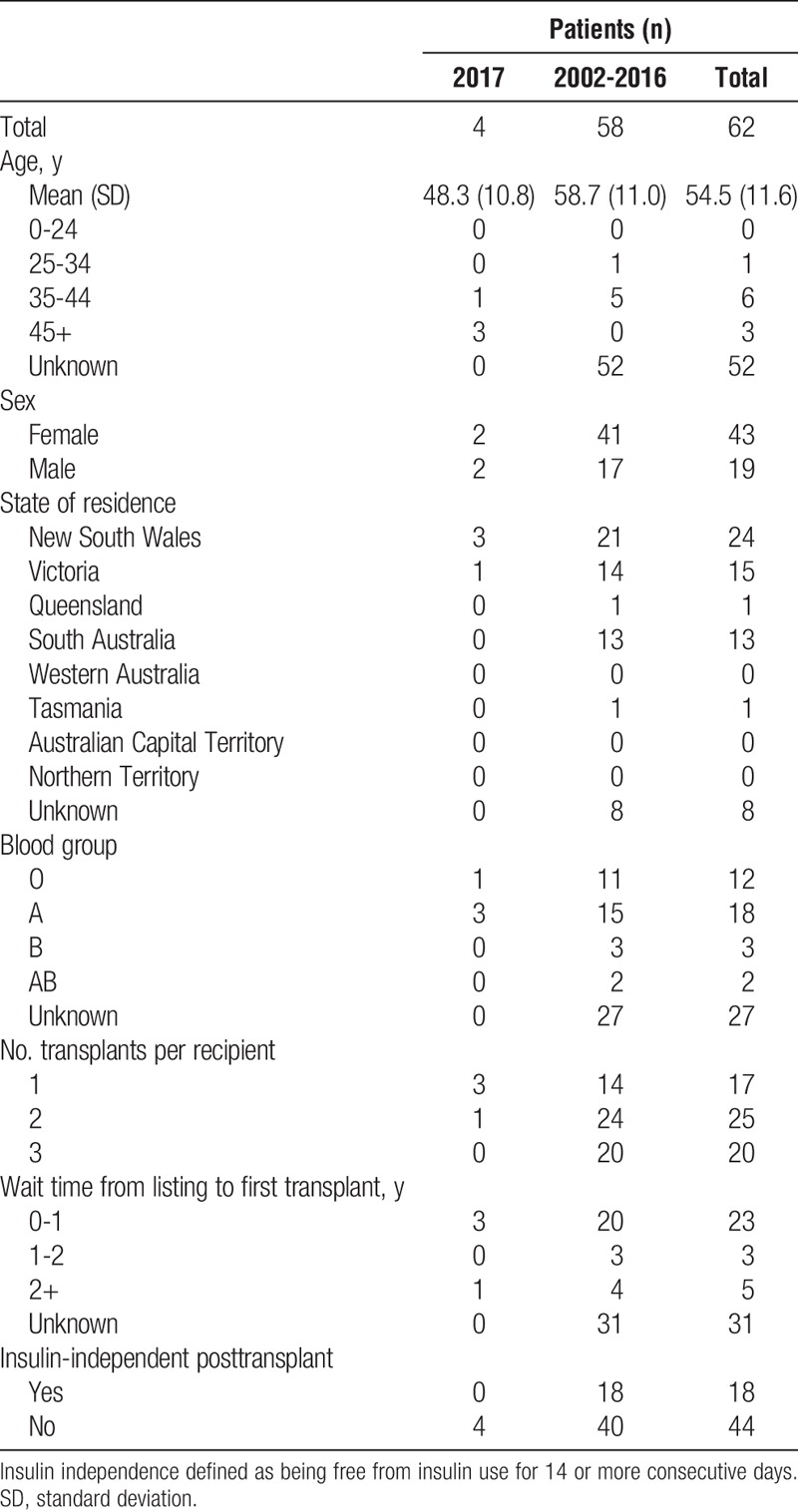
Characteristics of islet recipients over time are shown in Table 11.
TABLE 11.
Characteristics of allogeneic islet cell transplant recipients in Australia by year of first transplant
The time from activation on the waiting list to first islet transplant for 2002 to 2017 is presented in Figure 2. Data were available for 91 patients added to the waiting list before December 31, 2017, 56 of whom have received at least 1 transplant during this period. However, the date of waitlisting is complete for only 50 patients, 35 of whom received at least 1 transplant as of December 31, 2017. Recipients waited a median of 0.98 years from activation on the waiting list to receiving their first transplant (interquartile range, 0.62-2.18 years).
FIGURE 2.
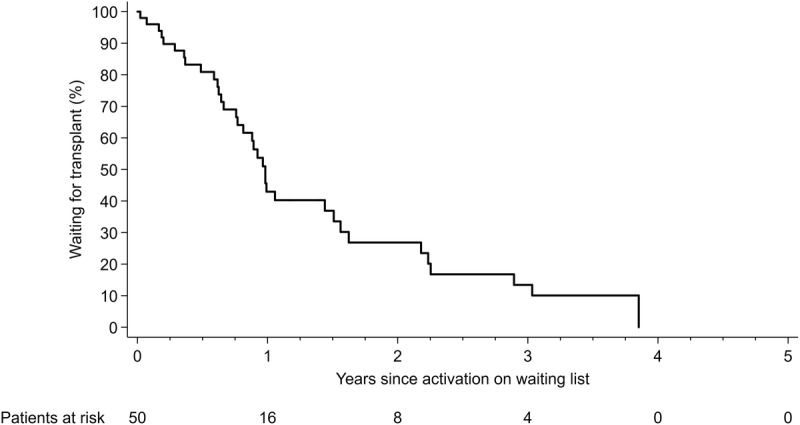
Time from activation on a waiting list to first allogeneic islet transplant.
The time from first to second islet transplant for 2002 to 2017, truncated at 5 years, is presented in Figure 3. Recipients waited a median of 0.80 years from first transplant to receiving a second transplant (interquartile range, 0.32-13.63 years).
FIGURE 3.
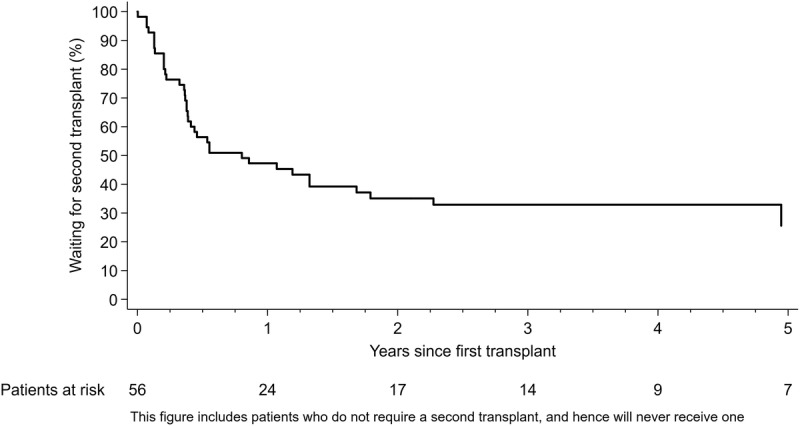
Time from first to second allogeneic islet transplant.
The time from second to third islet transplant for 2002 to 2017, truncated at 5 years, is presented in Figure 4. The median time from second transplant to third transplant has not yet been reached (25th percentile, 1.33 years), likely due to many recipients not requiring a third transplant.
FIGURE 4.
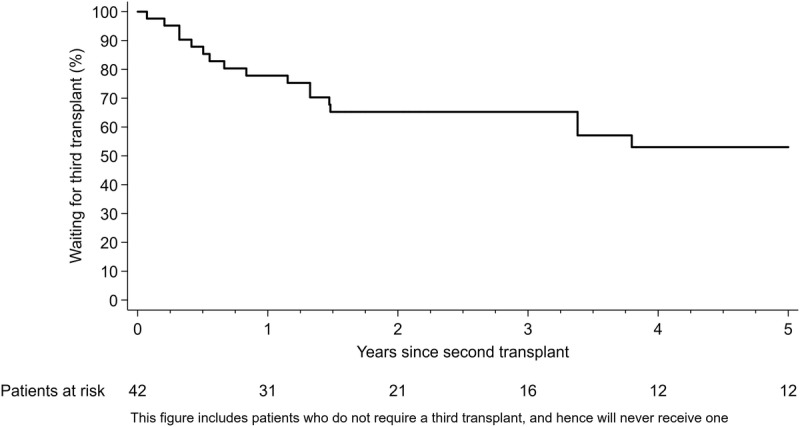
Time from second to third allogeneic islet transplant.
The distribution of C-peptide measurements over time after first islet infusion is presented in Figure 5. The normal range for a nondiabetic person in the fasting state is approximately 0.7 to 1.9 ng/mL.
FIGURE 5.
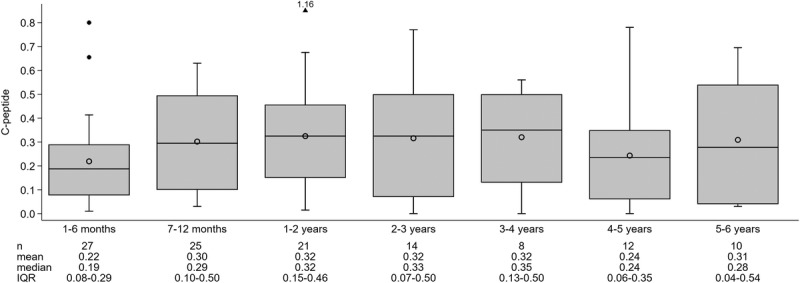
Posttransplant distribution of C-peptide over time after at least 1 allogeneic islet infusion.
The impact of hypoglycemia on an individual can be gauged by a symptom score to measure frequency, severity and degree of unawareness of hypoglycemia experienced by diabetics. The Edmonton hyposcore is a numeric score based on day to day measurements of blood glucose by an individual with diabetes over a 4-week period. The higher the HYPO score, the worse the impact of hypoglycemia for an individual. The full HYPO score scale is presented in the article by Ryan et al (Diabetes 2004;53:955-962).
The distribution of HYPO score measurements over time after first islet infusion (but before second islet infusion) is presented in Figure 6; the distribution of HYPO score measurements over time after second islet infusion (but before third islet infusion) is presented in Figure 7, and the distribution of HYPO score measurements over time after third islet infusion is presented in Figure 8.
FIGURE 6.
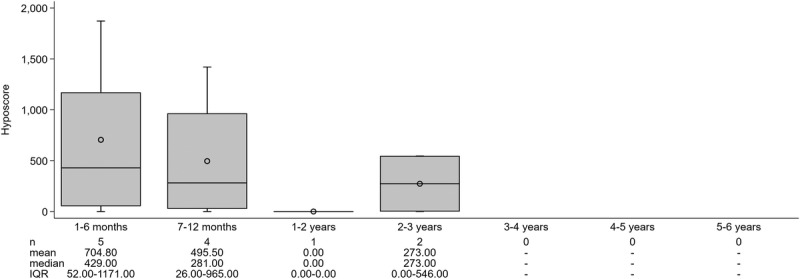
Posttransplant distribution of HYPO score over time since first allogeneic islet infusion.
FIGURE 7.
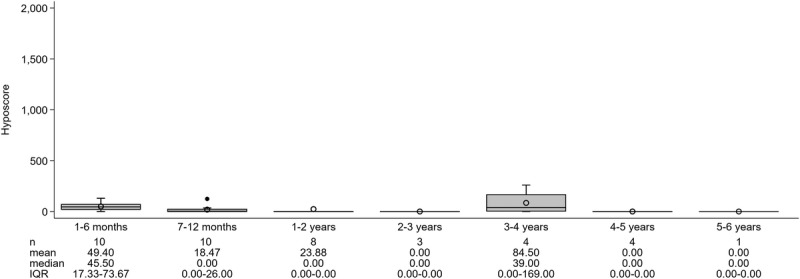
Posttransplant distribution of HYPO score over time since second allogeneic islet infusion.
FIGURE 8.
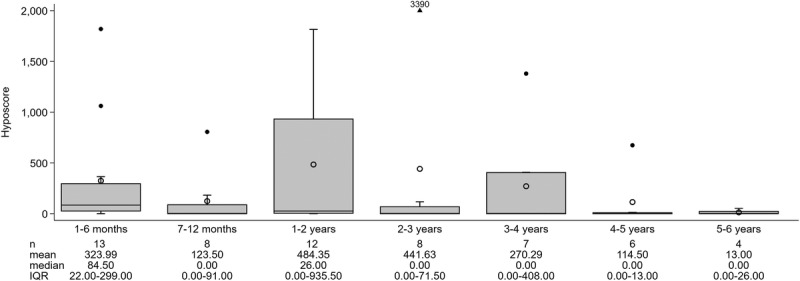
Posttransplant distribution of HYPO score over time since third allogeneic islet infusion.
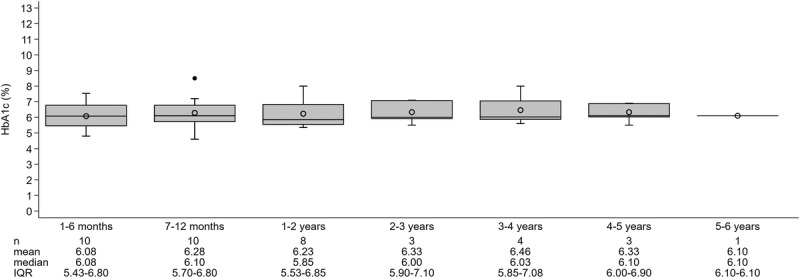
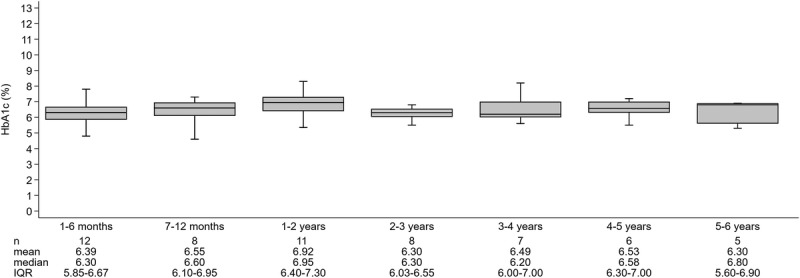
The distribution of glycosylated hemoglobin A1c (HbA1c) measurements over time after first islet infusion (but before second islet infusion) is presented in Figure 9, the distribution of HbA1c measurements over time after second islet infusion (but before third islet infusion) is presented in Figure 10, and the distribution of HbA1c measurements over time third first islet infusion is presented in Figure 11.
FIGURE 9.
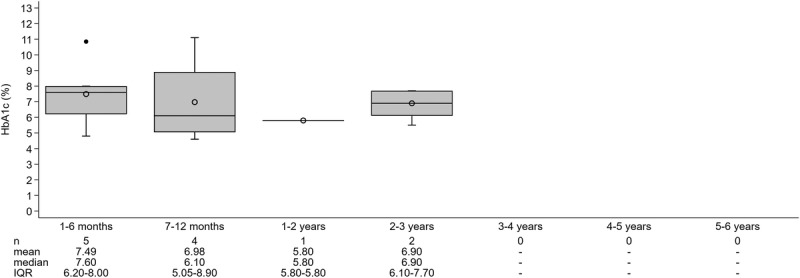
Posttransplant distribution of hemoglobin A1c (HbA1c; %) over time since first allogeneic islet infusion.
FIGURE 10.
Posttransplant distribution of hemoglobin A1c (HbA1c; %) over time since second allogeneic islet infusion.
FIGURE 11.
Posttransplant distribution of hemoglobin A1c (HbA1c; %) over time since third allogeneic islet infusion.
Insulin independence is defined as a person being free from insulin use for at least 14 days. Current registry data is incomplete, but shows there are at least 18 patients who have achieved insulin independence; 1 patient after their first transplant, 9 patients after their second transplant, and 8 patients after their third transplant. The duration of insulin independence from the time insulin was first ceased for 2002 to 2017 is presented in Figure 12.
FIGURE 12.
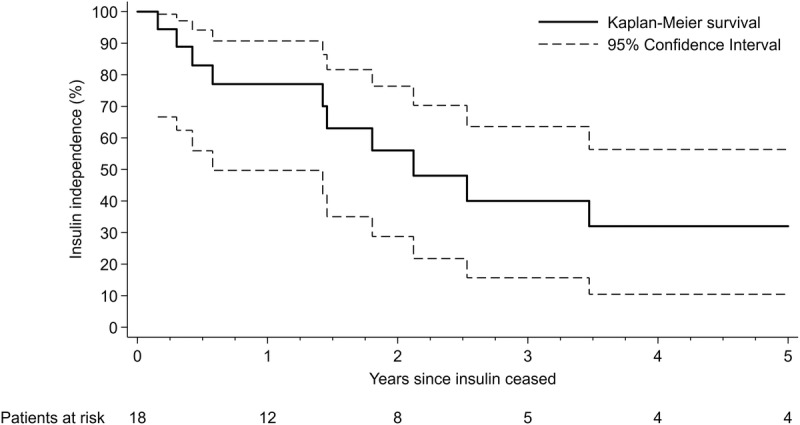
Posttransplant duration of insulin independence from time first ceased.
The Future: Reporting Islet Transplant Activity and the ANZIPTR Registry
The ANZIPTR registry is a clinical quality registry, reporting annually, on pancreas and islet transplant activity in Australia and New Zealand. To learn more about the ANZIPTR registry and to see full annual reports since 2005, please see http://anziptr.org.
It is important to note that registry data seeks to be both inclusive and population based, and that data are collected in real time. The data on which this report is based were data-locked in March 2018. However, the database is dynamic, with regular data interrogation and cleaning, as part of the reporting process, and so this report may not entirely reflect that data today. Changes and corrections are also made as the data are used, when any omissions or errors are identified, and clarification is sought from the contributing center. We constantly work to include more informative analyses and to improve data quality.
Islet transplantation in Australia is still developing, and so the numbers of recipients are small. Given the small numbers of recipients contributing data, please interpret results with caution, and in knowledge that random variability may be substantial with small sample sizes.
Future reports will endeavor to include more and longer-term outcome data and to include separate analyses on the small number of people undergoing kidney-with-islet procedures in Australia.
ACKNOWLEDGMENTS
This article is presented on behalf of the Australian Islet-cell Transplant consortium, who have all contributed to the article: Professor Philip J O'Connell, Associate Professor D. Jane Holmes-Walker, Professor Thomas W Kay, Professor Richard J MacIsaac, Associate Professor Glenn M Ward, Ms Kathy Howe, Professor P Toby Coates, Professor David Torpy, Dr Anthony Roberts, Dr Chris Russell, Dr Santosh Olakkengil.
Footnotes
Published online 7 January, 2019.
The registry is funded in part by a grant from the Commonwealth Department of Health and Ageing.
The authors declare no conflicts of interest.
The operation of this registry is legally mandated by the Australian Organ and Tissue Authority (OTA), hence institutional review board approval was not required.
A.C.W. is the registry executive officer. J.H. is the data analyst. P.F.A. is the data interpreter and article editor. W.J.H. is the data interpreter and article editor. T.R. is the data interpreter and article editor. C.D. is the data interpreter and article editor. N.R. is the data interpreter and article editor. D.G. is the data interpreter and article editor. M.L. is the data interpreter and article editor. T.L. is the data interpreter and article editor. P.J.K. is the biostatistics consultant.
Contributor Information
Collaborators: on behalf of the Australian Islet-cell Transplant consortium
REFERENCES
- 1.Webster AC, Hedley J, Patekar A, et al. Australia and New Zealand islets and pancreas transplant registry annual report 2017—pancreas waiting list, recipients, and donors. Transplant Direct. 2017;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Webster AC, Hedley J, Robertson P, et al. Australia and New Zealand islets and pancreas transplant registry annual report 2018—pancreas waiting list, recipients, and donors. Transplant Direct. 2018;4. [DOI] [PMC free article] [PubMed] [Google Scholar]


