Summary:
Orbital roof fracture is a relatively rare trauma. In most cases, surgical intervention is not needed since the fracture is slight. However, invasive surgical procedures are inevitable once pulsatile exophthalmos occurs if vision impairment is to be avoided. We report our rare experience of orbital roof fracture in a child with pulsatile exophthalmos. Good reconstruction of the anterior cranial base was achieved using a custom-made titanium mesh and a minimally invasive approach. A 3-year-old girl who had been diagnosed with subdural hematoma, brain contusion, and fracture of the right orbital roof caused by facial bruising underwent emergent external decompression by coronal skin incision and a transcranial approach on the same day as the trauma. Cranioplasty using autologous frozen bone in the same approach was performed 103 days posttrauma, but this was followed by pulsatile exophthalmos. After recovering from critical stage, the girl was brought to our department for reconstruction of the anterior base. Risk of vision impairment was also one reason for reconstruction, but the neurosurgeon hesitated to approach the region using a coronal approach considering the possibility of infection in the frozen autologous bone. Through cross-team discussion, reconstruction using a subeyebrow incision was performed with a custom-made titanium mesh plate. Pulsatile exophthalmos completely disappeared. Pulsatile exophthalmos is a very rare but serious complication that carries a risk of vision impairment. By applying a custom-made titanium mesh plate, precise reconstruction was enabled with minimal invasiveness and low risk.
INTRODUCTION
Orbital roof fractures due to craniofacial trauma are not common. An estimated 1–9% of facial bone fractures involve the orbital roof.1 Physical signs and symptoms may include diplopia, enophthalmos, exophthalmos, hyperglobus, and hypoglobus. Little bony displacement is seen in most cases involving children, and surgical intervention is not required in most cases (53–93%).2,3 However, serious complications such as pulsatile exophthalmos arise once the bone is severely displaced. Such severe displacement is very rare (seen in 5% of orbital roof fractures),4 but early surgical intervention is essential to avoid or address visual disturbance.
Here, we present the case of a child who underwent reconstruction of the anterior cranial base in a minimally invasive approach using custom-made titanium mesh.
CASE
A 3-year-old girl presented with a history of contusion to the right fronto-orbital region after being accidentally struck by an umbrella. As subdural hematoma and brain contusion were diagnosed, emergent external decompression was performed by neurosurgeons. Three months after the trauma, cranioplasty was performed using cryostored autologous skull bone. Pulsatile exophthalmos appeared gradually from 1-month postcranioplasty since right roof fracture remained. The patient attended our department to address concerns of progressive visual disturbance. Local examination revealed hypoglobus and pulsatile exophthalmos (see video, Supplemental Digital Content 1, which displays markable hypoglobus and pulsatile exophthalmos of the right eye, http://links.lww.com/PRSGO/A935).
Video Graphic 1.

See video, Supplemental Digital Content 1, which displays markable hypoglobus and pulsatile exophthalmos of the right, http://links.lww.com/PRSGO/A935.
Computed tomography (CT) revealed a large, 4-cm2 defect in the right orbital roof with frontal lobe herniation into the orbit (Fig. 1A). A custom-made titanium mesh plate (thickness, 0.6 mm) was made before operation using a 3D model of the orbit (Fig. 1B). Since exploration of the cryostored autologous skull bone through a coronal incision included a risk of infection, a subeyebrow incision was selected, and the periorbita was carefully separated from the skull base, where the dura had previously been reconstructed with fascia. The custom-made titanium mesh was fixed at the orbital rim with titanium screws (Fig. 2A). Pulsatile exophthalmos was completely resolved just after this surgery. CT showed that the titanium mesh completely separated the intracranial contents and orbit and had not been displaced (Fig. 2B). Slight pulsation of the forehead was evident 9 months after surgery, but no recurrence of hypoglobus or pulsatile exophthalmos was seen (see video, Supplemental Digital Content 2, which displays the postoperative view 9 months after surgery. No recurrence of hypoglobus or pulsatile exophthalmos is seen, http://links.lww.com/PRSGO/A936).
Fig. 1.
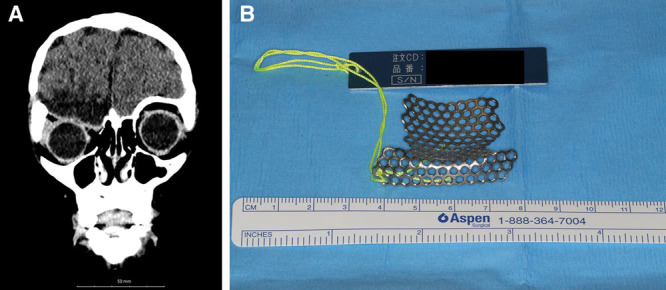
A, CT reveals large defect of the right orbital roof with frontal lobe herniation into the orbit. B, A custom-made titanium mesh plate was created before the operation using a 3D model of the orbit.
Fig. 2.
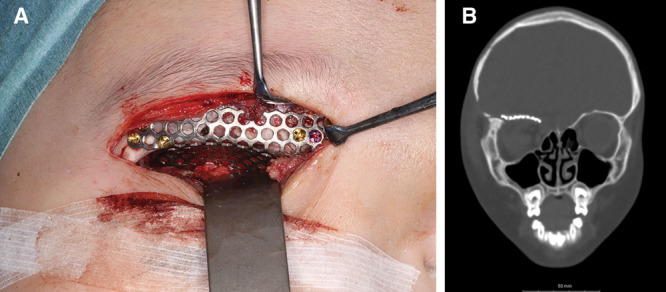
A, With subeyebrow incision, the periorbita is carefully separated from the skull base. Custom-made titanium mesh is fixed at the orbital rim with titanium screws. B, CT shows that the titanium mesh has completely separated the intracranial contents and orbit without displacement.
Video Graphic 2.

See video, Supplemental Digital Content 2, which displays the postoperative view 9 months after surgery. No recurrence of hypoglobus or pulsatile exophthalmos is seen, http://links.lww.com/PRSGO/A936.
DISCUSSION
Orbital roof fracture with traumatic encephalocele is very rare, but may lead to pulsatile exophthalmos. Only 28 cases have been reported in the literature.5–7 Among children, only 8 cases have been reported, and none of those showed total defect of the anterior cranial base.6–8 Almost all cases needed a transcranial approach with coronal incision. Our case is unique in that we created a precise reconstruction of the anterior cranial base in a child with pulsatile exophthalmos using a minimally invasive extracranial approach and a custom-made titanium mesh plate.
With regard to the etiology of pulsatile exophthalmos, orbital roof fracture with orbital encephalocele could conceivably cause an increase in intraorbital pressure, leading to exophthalmos. In addition, the optic nerve is continuously extended and compressed because of intracranial arterial pulsation, which results in progressive visual disturbance. Early surgical intervention is thus mandatory.
Two approaches to the orbital roof can be used: trans cranial and extracranial.1,5 The transcranial approach is usually selected through a bicoronal incision for frontal craniotomy. This method is suitable when a large defect is present or the injury reaches the dura mater or frontal lobe, because it allows a good surgical field and combination with other flaps such as temporalis muscle flap or pericranial flap. In our case, as a total defect of the anterior cranial base and a bicoronal scar from the previous cranioplasty were present, a bicoronal approach was considered. On the other hand, the bicoronal approach would have led to exposure of the cryostored autologous skull bone, which might have carried a high risk of infection. A previous report described the rate of autogenous bone infection without re-exposure as 25.9%.9 Another report has shown that the rate of microbial contamination in cryostored bone graft is significant, at 27.8%.10 Since that situation of infection had to be avoided, we chose an extracranial approach through the subeyebrow incision. The chief advantage of this approach was the minimal invasiveness without exposure of cryostored autologous bone graft. In contrast, the disadvantages included the increased technical difficulty of surgical procedures because of the deep, narrow surgical field. Regarding this situation, we created an orbital model using a 3-dimensional printer, and ordered a custom-made titanium mesh plate based on that model. The titanium mesh plate was large, at 4-cm2, but we could insert the mesh into the region precisely without any complications. Without the custom-made titanium mesh plate, reconstruction of the narrow, deep defect would not have held sufficiently.
Several materials are available for reconstructing the orbital roof, such as autologous bone, titanium mesh, absorbable plates, and ceramics. Autologous bone offers the best biocompatibility, but shows difficulties with contouring, especially for reconstructions demanding precise shaping. A risk of pulsatile exophthalmos due to unexpected absorption remains, and an additional donor site is also needed. We considered it does not have indication for this case since the patient was still 3 years old, and if absorption occurs, the donor sacrifice would become unacceptable. Advantage of absorbable plates would be their biocompatibility, but they were considered inadequate for this case to avoid recurrence of pulsatile exophthalmos. Ceramics also offer good biocompatibility and stability, but show difficulties with contouring and screw fixation. For these reasons, we chose the titanium mesh to provide good biocompatibility and a reduced risk of infection, while requiring no additional donor site and allowing easy preformation. Regarding the possibility of replacing the plate, we considered titanium mesh as the most easily removed option. Indications for custom-made titanium mesh plates remain limited due to the high cost (7,000 USD), but the method is reliable when anatomically precise reconstruction is achieved under a minimally invasive approach.
DECLARATION OF HELSINKI
The study was conducted in keeping with the principles outlined in the Declaration of Helsinki.
Footnotes
Published online 11 February 2019.
Presented at the 23rd meeting of Japan Society for Innovative Techniques in Plastic Surgery, February 10, 2018, Amagasaki-City, Japan.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Haug RH, Van Sickels JE, Jenkins WS. Demographics and treatment options for orbital roof fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:238–246. [DOI] [PubMed] [Google Scholar]
- 2.Messinger A, Radkowski MA, Greenwald MJ, et al. Orbital roof fractures in the pediatric population. Plast Reconstr Surg. 1989;84:213–216; discussion 217. [PubMed] [Google Scholar]
- 3.Koltai PJ, Amjad I, Meyer D, et al. Orbital fractures in children. Arch Otolaryngol Head Neck Surg. 1995;121:1375–1379. [DOI] [PubMed] [Google Scholar]
- 4.Martello JY, Vasconez HC. Supraorbital roof fractures: a formidable entity with which to contend. Ann Plast Surg. 1997;38:223–227. [PubMed] [Google Scholar]
- 5.Mokal NJ, Desai MF. Titanium mesh reconstruction of orbital roof fracture with traumatic encephalocele: a case report and review of literature. Craniomaxillofac Trauma Reconstr. 2012;5:11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenwald MJ, Lissner GS, Tomita T, et al. Isolated orbital roof fracture with traumatic encephalocele. J Pediatr Ophthalmol Strabismus. 1987;24:141–144. [DOI] [PubMed] [Google Scholar]
- 7.Cayli SR, Kocak A, Alkan A, et al. Intraorbital encephalocele: an important complication of orbital roof fractures in pediatric patients. Pediatr Neurosurg. 2003;39:240–245. [DOI] [PubMed] [Google Scholar]
- 8.Antonelli V, Cremonini AM, Campobassi A, et al. Traumatic encephalocele related to orbital roof fractures: report of six cases and literature review. Surg Neurol. 2002;57:117–125. [DOI] [PubMed] [Google Scholar]
- 9.Matsuno A, Tanaka H, Iwamuro H, et al. Analyses of the factors influencing bone graft infection after delayed cranioplasty. Acta Neurochir (Wien). 2006;148:535–540; discussion 540. [DOI] [PubMed] [Google Scholar]
- 10.Chan DYC, Mok YT, Lam PK, et al. Cryostored autologous skull bone for cranioplasty? A study on cranial bone flaps’ viability and microbial contamination after deep-frozen storage at -80°C. J Clin Neurosci. 2017;42:81–83. [DOI] [PubMed] [Google Scholar]


