Abstract
Type 2 diabetes (T2D) with high morbidity and mortality is characterized by abnormal glucose and lipid metabolism due in part to insulin resistance in liver, which lead to elevated hyperglycemia and hyperlipidemia. This study sough to explore the effects of corosolic acid (CA) in different T2D models and explored the underlying mechanism. Separated from Eriobotrya japonica leaves, CA purity was above 95% measured by a HPLC method. Compared with cAMP and DEX induced T2D HepG2 model, CA significantly stimulated glucose consumption and improved glycogen accumulation by inhibiting PEPCK mRNA expression. And in cAMP and DEX induced T2D zebrafish model, CA reduced glycogen degradation and increased glucose consumption by regulating some key enzymes in carbon metabolism including GLUT1, GLUT2, GLUT3, LDHA, LDHB, GP, G6Pase, GYS1, and PFKFB3. In addition, insulin receptor signals were also involved in CA-regulated hypoglycemic action. Furthermore, in STZ-induced T2D rat model, compared with diabetic control groups, CA remarkably downregulated the levels of serum lipid, blood glucose, ICAM-1, malonaldehyde and insulin resistance index, while upregulated SOD activity and impaired glucose tolerance. In a conclusion, CA can regulate glucose and lipid metabolic adaptation in T2D like HepG2, zebrafish and rat models partly through reducing inflammation and oxidative stress and suppressing PEPCK.
Introduction
Type 2 diabetes(T2D) is a widely heterogeneous disorder featured by fasting and post-prandial hyperglycemia and progression of insulin resistance, which has affected increasing number of populations and become one of the most costly and burdensome diseases1. Despite great efforts have been made to normalize blood glucose level in clinic therapy, it’s still a formidable challenge2.
It is essential to maintain blood glucose levels in a normal range for the health of human body, because hyperglycemia can cause damage to protein dysfunction and oxidative stress led by nonspecific glycosylation. Excessive hepatic glucose output is the main cause of hyperglycemia in diabetic patients. Therefore, alleviating excessive hepatic gluconeogenesis is a potential target for the treatment of glucose metabolic disorders3. Phosphoenolpyruvate carboxykinase (PEPCK) is a rate-limiting enzyme in liver and kidney gluconeogenesis, which catalyzes the conversion of oxaloacetate (OAA) into phosphoenolpyruvate (PEP)4. The transcription of PEPCK can be regulated by hormones involved in glucose homeostasis, for example, glucagon (acting by the second messenger cAMP), glucocorticoid (dexamethasone(DEX)) and retinoic acid5, dominantly repressed by insulin6. The overexpression of PEPCK has been found in almost all diabetes models, therefore, PEPCK can be used as an indicator of blood glucose levels7,8.
At present, many therapeutic agents for T2D treatment, like sulphonylures and bisguanidine, are responsible for side effects like flatulence and diarrhea9. Thus, much attention has been paid to active natural products from Chinese herbal medicines, which have the functions on controlling glucose level and alleviating the risk of complications10.
It’s previously reported that terpenoids are strikingly lower-blood glucose compounds by enhancing insulin sensitivity, promoting insulin secretion, inhibiting protein tyrosine phosphatase 1B, α-glucosidase, aldose reductase (AR) and dipeptidyl peptidase-4(DPP-4) activities to further reducing liver glycogen decomposition and gluconeogenesis11. Corosolic acid (2α,3β-2,3-dihydroxy-urs-12-en-28-oic acid) is a natural pentacyclic triterpene discovered in traditional Asian medical herbs such as Lagerstroemia speciose12,13, Eriobotrta japonica14, Tiarella polyphylla15, which has attracted much attention for its antidiabetic and anti-lipid oxidative activity in some animal experiments and clinical trials, including development of glucose metabolism by declining insulin resistance in mice and reducing on post-challenge plasma glucose levels in human16–25. Although corosolic acid was reported to be a talented compound for diabetes, its underlying mechanism has not been systematically analyzed.
As a vertebrate, due to high homology with human, zebrafish has been widely used as a model organism to research on biological process of vertebrate. These studies include malignant neoplasms, cardiovascular diseases, immune system diseases, antioxidant stress and diabetes26. It’s been reported that zebrafish regulated glucose metabolism by producing insulin, glucagon and other important proteins, such as PEPCK, which identified similar regulation patterns and activity in mammalian models27,28.
In our study, we firstly separated corosolic acid from Eriobotrya japonica leaves, investigated the effect of corosolic acid on glucose and lipid metabolism and identified the molecular mechanism of corosolic acid alleviated hyperglycemia in different T2D models containing cAMP and DEX-induced HepG2 cells, cAMP and DEX-induced zebrafish and STZ-induced rats.
Results
Separation and identification of CA
After dried and powdered, Eriobotrya Japonica leaves were extracted by ethanol and concentrated to get the extract. Discard the supernatant, dissolve the residue by ethanol again, and decolor it by activated carbon repeatedly. After filtration, the supernatant could be reduced pressure concentrated and dried to prepare the crude extract. Dissolve the crude extract by methanol and filtrate it with 0.45μm membrane in order to do preparative HPLC separation. In contrast to CA standard, the corresponding peak effluent of CA was collected, combined, concentrated under reduced pressure, and finally recrystallized with methanol to get corosolic acid.
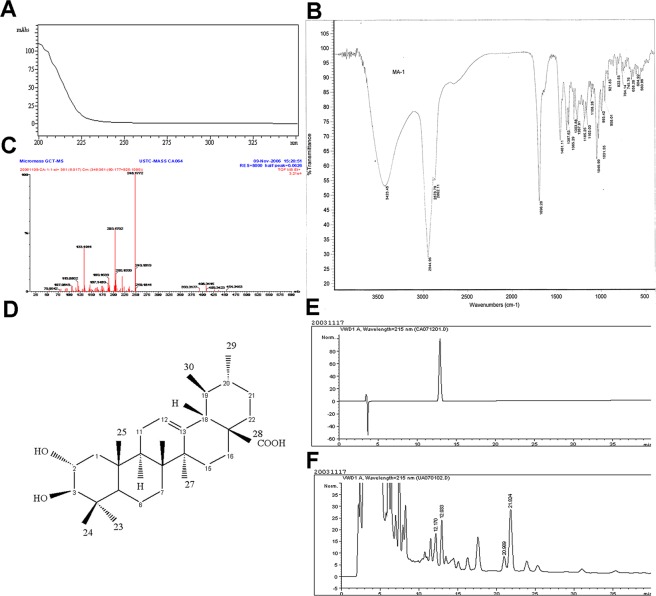
Since the target sample structure contains only chromophores such as saturated alkanes, cyclohexene, mono-carboxyl and hydroxyl groups, simultaneously the maximum absorption wavelength of these chromophores all fall within the deadline wavelength of methanol, only the terminal absorption can be seen in the UV-visible spectrum (Fig. 1A).
Figure 1.
Separation, identification and determination of CA. (A) UV analysis for products separated by preparative chromatography; (B) IR spectra of CA; (C) EI-MS spectra of CA; (D) Chemical structure of CA; (E) HPLC chromatograms of standard CA; (F) HPLC chromatograms of four triterpene acids separated from Eriobotrya Japonica leaves.
Samples were plated with KBr. The IR absorption bands at 3415, 2973, 2927, and 2872 cm−1 indicated the presence of hydroxy, carbonyl and alkene (Fig. 1B).
Corosolic acid isolated as a white powder, exhibited an EI-MS ion at m/z 454.3463[M-18]+ (calcd for C30H46O3, 454.3447) (Fig. 1C) and combined with the 13C NMR data (Table 1), displayed 30 carbon resonances, which were classified as 7 methyl, 8 methylene, 8 methine, and 7 quaternary, which suggested a molecular formula of C30H48O4 (Fig. 1D). Its 1H NMR data (Table 1) showed signals for 7 methyl groups at δ H0.71 (3 H, s, H29), 0.75(3 H, s, H30), 0.82(3 H, s, H25), 0.92(3 H, s, H24), 0.92(3 H, s, H26), 0.92 (3 H, s, H27), 1.0(3 H, s, H23), an olefinic proton at δ 5.17(1 H, t, J = 3.4 Hz, H12), and a tertiary carbon proton at δ 2.11 (1 H, t, H20).
Table 1.
13C NMR data (500 MHz, DMSO-d6).
| position | δC, type | position | δC, type |
|---|---|---|---|
| 1 | 46.8,CH2 | 16 | 23.7,CH2 |
| 2 | 67.1,CH | 17 | 46.9,C |
| 3 | 82.2,CH | 18 | 52.3,CH |
| 4 | 38.8,C | 19 | 38.4,CH |
| 5 | 54.7,CH | 20 | 38.4,CH |
| 6 | 18.0,CH2 | 21 | 30.1,CH2 |
| 7 | 32.6,CH2 | 22 | 36.2,CH2 |
| 8 | 39.0,C | 23 | 28.8,CH3 |
| 9 | 47.0,CH | 24 | 17.1,CH3 |
| 10 | 37.5,C | 25 | 16.4,CH3 |
| 11 | 22.9,CH2 | 26 | 16.9,CH3 |
| 12 | 124.4,CH | 27 | 23.2,CH3 |
| 13 | 138.2,C | 28 | 178.2,C |
| 14 | 41.6,C | 29 | 21.0,CH3 |
| 15 | 27.4,CH2 | 30 | 16.9,CH3 |
Corosolic acid
white powder; mp254–256 °C; IR (Nujol) 2973, 2927, and 2872 cm−1; 1H-NMR(DMSO-d6, 500 MHz) δ: 0.71(3 H, s, H29), 0.75(3 H, s, H30), 0.82(3 H, s, H25), 0.92(3 H, s, H24), 0.92(3 H, s, H26), 0.92(3 H, s, H27), 1.0(3 H, s, H23), 4.22(1 H, d, J = 8.7 Hz, H-2β), 4.33(1 H, dd, J = 9.0, 11.5, H-3α), 5.17 (1 H, t, J = 3.4 Hz, H12), 3.42(1 H, t, J = 9.8 H18), 2.74(1 H, t, H19), 2.11 (1 H, t, H20);13C-NMR(DMSO-d6,125 MHz)δ178.2(COOH, C-28), 138.2(C, C-13), 124.4(CH, C-12), 82.2(CH, C-3), 67.1(CH, C-2), 54.7(CH, C-5), 52.3(CH, C-18), 47(CH, C-9), 46.9(C, C-17), 46.8(CH2, C-1), 41.6(C, C-14), 39(C, C-8), 38.8(C, C-4), 38.4(CH, C-19), 38.4(CH, C-20), 37.5(C, C-10), 36.2(CH2, C-22), 32.6(CH2, C-7), 30.1(CH2, C-21), 28.8(CH3, C-23), 27.4(CH2, C-15), 23.7(CH2, C-16), 23.2(CH3, C-27), 22.9(CH2, C-11), 21(CH3, C-29), 18(CH2, C-6), 17.1(CH3, C-24), 16.9(CH3, C-26), 16.9(CH3, C-30), 16.4(CH3, C-25).
Furthermore, comparing to CA standard(Fig. 1E), a HPLC-UV method was built to detect purity of CA (Fig. 1F) by determining the peak with S/N greater than 3 as impurities (>96.1%, shown in Supporting Information, S1), which was also confirmed by melting range of 254–256 °C, the same as related references29. In addition, the average content of CA in Eriobotrya Japonica leaves is 0.814% (Table 2).
Table 2.
Determination of CA content in Eriobotrya Japonica leaves.
| Number | CA Content/(mg/g) |
|---|---|
| 110106 | 8.66 |
| 110307 | 7.88 |
| 110510 | 7.91 |
| 110804 | 8.13 |
| 111108 | 8.22 |
| average | 8.14 |
CA stimulated glucose consumption and improved glycogen accumulation by regulating PEPCK in HepG2 cells
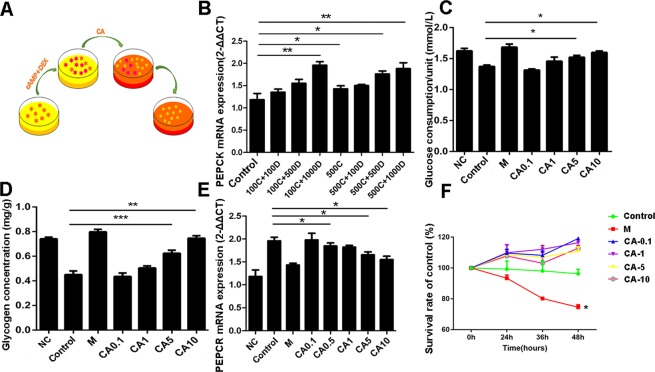
Phosphoenolpyruvate carboxykinase (PEPCK) is a key rate-limiting enzyme of gluconeogenesis in the liver30. The expression of PEPCK is regulated at transcriptional level and regulated by glucose-related hormones involved in glucose homeostasis, such as glucagon, glucocorticoid and insulin31. So far, overexpression of PEPCK has been found in many diabetes models and induction of PEPCK overexpression in rodent models can induce insulin-resistant, a kind of Type 2 diabetes (T2D) like syndrome6. In our study, we established type 2 diabetic-like model in HepG2(details in Supporting Information. S2, S3, Fig. S1, S2) stimulated by cAMP and DEX (Fig. 2A). After testing the effect and stability of insulin-resistant hepatocytes, the expression of PEPCK was further detected. The result in Fig. 2B showed that PEPCK expressions in different treatments of cAMP and DEX were higher than that in the control group. Especially, PEPCK expressions in groups of 100 μM cAMP + 1000 nM DEX, 500 μM cAMP, 500 μM cAMP + 500 nM DEX, and 500 μM cAMP + 1000 nM DEX were much higher than control with significant difference. Therefore, the expression level of PEPCK in HepG2 cells treated with 100 μM cAMP + 1000 nM DEX (P < 0.01), which was our induced condition of T2D model, was obviously higher than control in accordance with glucose consumption and glycogen accumulate.
Figure 2.
CA improved glucose consumption and glycogen stimulate led by cAMP and DEX induced T2D cell model. (A) Model building schematic diagram; (B) PEPCK mRNA expression in different cAMP and DEX treated group; After CA treatment, glucose consumption (C), glycogen stimulate (D) and PEPCK mRNA expression (E) were analyzed; (F) Antiproliferative effect of CA on HepG2 cells were analyzed by CCK8. * Indicates a significant difference from the control at P < 0.05, **P < 0.01, ***P < 0.0001. C, cAMP; D, DEX; M, metformin.
Next, we analyzed glucose consumption and glycogen stimulate after treating by CA in insulin-resistant hepatocytes. In Fig. 2C,D, the unit glucose consumption and intracellular glycogen content of CA treated groups upregulated with the increasing concentration of CA. The unit glucose consumptions of 5 μM and 10 μM CA treated group were 1.11 times and 1.16 times higher than cAMP and DEX treated group, respectively (P < 0.05). In addition, 5 μM and 10 μM CA could significantly improve the intracellular glycogen degradation induced by cAMP and DEX, and 10 μM CA regulated glycogen content change was almost no significant difference with metformin treated group (P < 0.01). To sum up, 10 μM CA can significantly improve the decrease of glucose consumption and intracellular glycogen content induced by cAMP and DEX, maintain glucose homeostasis and reduce glucose toxicity caused by excess glucose. To investigate the mechanism of hypoglycemic activity of CA in HepG2 cells, the expression of PEPCK was evaluated in mRNA level, which is a well-known enzyme involved in type 2 diabetes. As shown in Fig. 2E, the expression of PEPCK was decreased by CA treatments, and significant differences were observed at 5 μM and 10 μM concentration(P < 0.05). It was worth that the effect of 10 μM CA on reversing the overexpression of PEPCK in T2D model was nearly similar to that of metformin.
In addition, we further detected the toxicity of CA on HepG2 cell at different concentrations. The survival rate in Fig. 2F presented CA showed no significant effect on cell viability in the concentration range of hypoglycemic action, even if at maximum concentration of 10 μM.
CA reduced glycogen output by regulation of carbon metabolism and insulin receptor in zebrafish model
It has been reported that zebrafish have great potential in the study of diabetes. Exposure of zebrafish to a high concentration of glucose solution can induce metabolic changes similar to hyperinsulinemia and damage glucose metabolism in peripheral tissues. And it also been found that adult zebrafish respond to diabetes drugs by lowering blood sugar levels, which is similar to that in mammalian models.
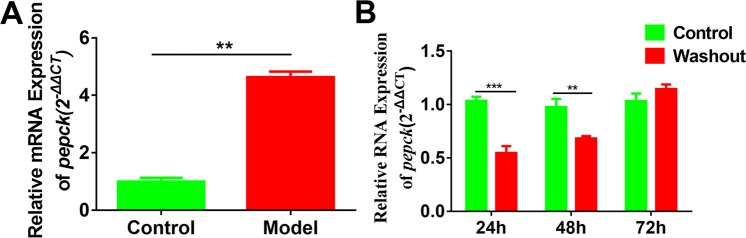
In our work, zebrafish model was introduced to study the hypoglycemic effect of CA. To establish zebrafish model with PEPCK overexpression, 3 mL of culture medium containing 100 μM cAMP and 1000 nM DEX was added to each well of the treatment group. The results in Fig. 3A indicated that the expression level of PEPCK gene was significantly increased about 4.638 times than that of the control group (P < 0.01) and glucose level was also upregulated in Fig. 4B. To further confirm the stability of our established diabetic zebrafish model, after incubating 48 h, we replaced the cAMP and DEX solution with normal culture and continued to develop for another 24 h, 48 h, and 72 h, respectively. The result of Fig. 3B presented that PEPCK gene expression was conspicuously lower than the corresponding control group at 24 h and 48 h (24 h, P < 0.001; 48 h, P < 0.01), but PEPCK gene expression was slightly higher than the control group without significant difference at 72 h. Therefore, the model’s stability is poor after removing the irritants cAMP and DEX and they are required to exist during incubation periods.
Figure 3.
Establishment and stability of diabetic zebrafish model. (A) Effect of 100 μM cAMP and 1000 nM DEX treatment for 48 h on the zebrafish fertilized 96 h. The chart showed the relative mRNA expression of PEPCK. **P <0.01; Effect of the washout of 100 μM cAMP and 1000 nM DEX treatment for 48 h on PEPCK gene expression. At least 20 zebrafish larvae were used for each group. **P < 0.01,***P < 0.001.
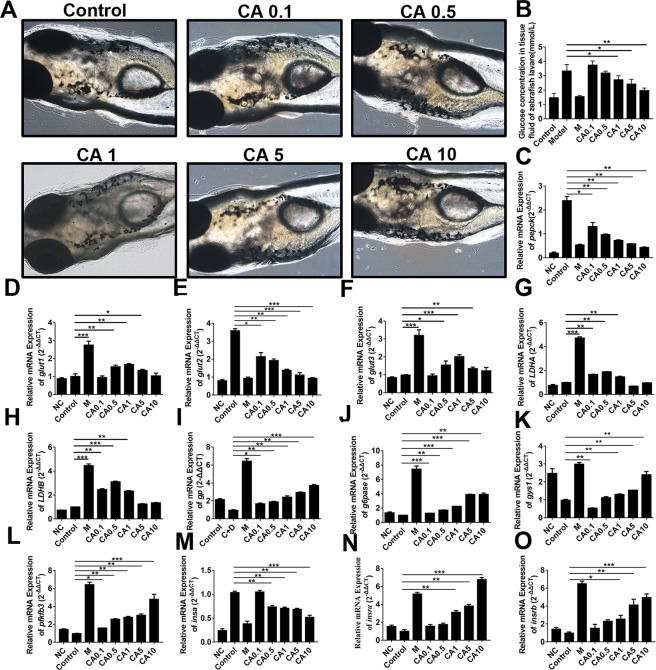
Figure 4.
CA reduced glycogen output in zebrafish model. (A) The toxicity of CA on zebrafish; (B) Glucose concentration in zebrafish tissue fluid treated by different dosages of CA; C-O, PEPCK, GLUT1, GLUT2, GLUT3, LDHA, LDHB, GP, GP6ase, GYS1, PFKFB3, INSα, INSRα and INSRβ mRNA expressions were analyzed by qPCR. P < 0.05, **P < 0.01, ***P < 0.0001. NC, negative control; Control, diabetic control; M, metformin.
After assessment of Metformin toxicity against zebrafish (Fig. S3, Table S1), the toxicity of CA on zebrafish was firstly determined by morphologic observation and survival statistics. 0.1–10 μM CA have not brought hemolysis and peritoneal hemorrhage in zebrafish larvae (Fig. 4A). After zebrafish larvae cultured in different concentrations of CA for continuous 9 days, only three groups including 10 μM CA at the 7th day, 0.1 μM CA at the 8th day and 10 μM CA at the 9th day, each of which has one zebrafish larva died respectively (Table 3). This result indicated CA within the concentration of 0.1 μM-10 μM has almost non-toxic to zebrafish larvae, which was consistent with our previous T2D HepG2 models.
Table 3.
Toxicity analysis of CA on zebrafish larvae.
| Groups | Zebrafish numbers | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1d | 2d | 3d | 4d | 5d | 6d | 7d | 8d | 9d | |
| Control | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| CA 0.1 μM | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| CA 0.5 μM | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| CA 1 μM | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| CA 5 μM | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| CA 10 μM | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
In order to detect whether CA plays a hypoglycemic role by regulating the glycol-metabolism of zebrafish, we firstly detected glucose concentration of zebrafish larvae after treated with different concentrations of corosolic acid. Because the zebrafish juveniles did not bleed, our team added the determination of the zebrafish tissue fluid glucose concentration according to reference32. The results indicated that CA reduced glucose level in zebrafish fluid in a dose-dependent manner (Fig. 4B, Table 4).
Table 4.
Glucose concentration in tissue fluid of zebrafish larvae after treated with different concentrations of corosolic acid (mmol/L).
| Group | Control | Model | M | M + CA 0.1 μM | M + CA 0.5 μM | M + CA 1 μM | M + CA 5 μM | M + CA 10 μM |
|---|---|---|---|---|---|---|---|---|
| 1 | 1.46 ± 0.30 | 3.29 ± 0.41 | 1.52 ± 0.05 | 3.40 ± 0.43 | 3.31 ± 0.29 | 2.38 ± 0.32 | 2.08 ± 0.50 | 1.96 ± 0.18 |
To further discover its underlying mechanism, we analyzed several key enzymes from carbon metabolism in mRNA level including PEPCK, GLUT1, GLUT2, GLUT3, LDHA, LDHB, GP, G6Pase, GYS1 and PFKFB3. The result indicated that CA dramatically downregulated the expression of pepck (Fig. 4C), glut1(Fig. 4D), glut2 (Fig. 4E), glut 3(Fig. 4F), LDHA (Fig. 4G) and LDHB(Fig. 4H), whereas, upregulated the expression of gp (Fig. 4I), g6pase (Fig. 4J), gys1 (Fig. 4K) and pfkfb3 (Fig. 4L) in a dose-dependent manner.
In addition, it’s reported that high stimulation of glucose induced by cAMP and DEX in cell can lead to glucose toxicity and further inhibit the secretion of β cells, the latter of which may induce β cells apoptosis and hyperinsulinemia, and stimulate insulin resistance by reducing the amount of insulin receptor33. In our study, we also analyzed the expression of INSα and two of its receptor INSRα and INSRβ. Figure 4M suggested CA significantly downregulated INSα expression in a concentration-dependent manner, which was probably led by the secretion of insulin based on glucose concentration. As shown in Fig. 4N,O, the expressions of two types of insulin receptor were upregulated by CA in a dose-dependent manner(P < 0.01).
Moreover, these results indicate cAMP and DEX treatment on zebrafish can establish an insulin resistance model. CA can significantly increase the sensitivity of insulin receptor and improve its effect. Therefore, CA can relieve hyperglycemia, insulin resistance and other symptoms of type 2 diabetes by promoting insulin power.
CA regulated glucose, lipid metabolism and insulin resistance of STZ-induced type 2 diabetic rats
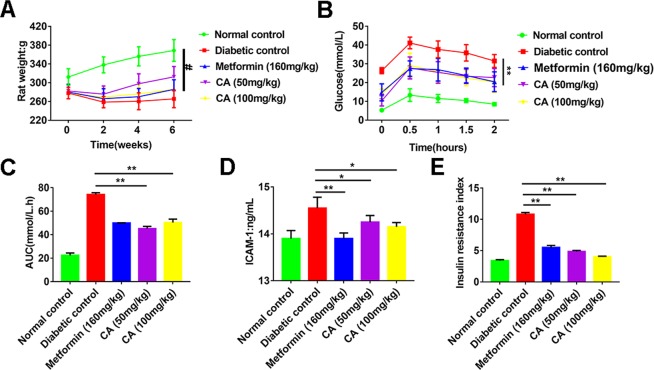
In this part, a T2D rat’s model was established by both highly fat diet and a low dose of STZ at the same time, with the purpose to discover the effect of CA on hyperglycemia, hyperlipemia and insulin resistance using glucose tolerance and IRI as well-known biomarkers of type 2 diabets34. The establishment details about STZ-induced T2D diabetic rats were provided in supporting information (S3) according to previous study35. As illustrated in Fig. 5A, with similarly initial body weights, diabetic group’s body weight was remarkably lower than that of the normal control group throughout the entire research (P < 0.01). Diabetic rats conducted by CA (50 or 100 mg/kg) showed a tendency to put on weight. CA inhibited the loss of body weight in STZ-induced diabetic rate, and 100 mg/kg CA effects were comparable to metformin group.
Figure 5.
CA regulated glucose, lipid metabolism and insulin resistance of STZ-induced T2D rats. (A) Effect of CA on body weight in diabetic rats; Effect of CA on the glucose tolerance (B) and AUC(C) in diabetic rats; Effect of CA on ICAM-1(D) and IRI (E) in diabetic rats. The rats were treated with CA (50 or 100 mg/kg) and metformin (160 mg/kg) for 6 weeks. *P < 0.05, **P < 0.01 compared to diabetic groups; #P < 0.01 compared to normal control groups.
In an attempt to measure the consequence of CA on diabetes process caused by high-fat diet and low-dose STZ, we elucidated fasting blood glucose (FBG) levels, glucose tolerance and glycated serum protein (GSP). The six-week administration of CA restrained the estimated increase in the FBG level (Fig. 5B) and augmented the impaired glucose tolerance in T2D rats (Fig. 5C). Moreover, treatment with CA (50 or 100 mg/kg) for 6 weeks declined level of FBG and GSP, and the suppression rates were 86.4%, 91.4%(FBG) and 70.6%, 71.6%(GSP), respectively (Table 5). These results confirmed the antihyperglycemic effect of CA on T2D rats.
Table 5.
Effect of coroslic acid on biochemical parameters in diabetic rats.
| Parameter | Normal control | Diabetic control | Metformin 160 mg/kg | CA 50 mg/kg | CA 100 mg/kg |
|---|---|---|---|---|---|
| FBG(mmol/L) | 5.51 ± 1.41 | 26.37 ± 7.82b | 10.47 ± 5.86d | 8.25 ± 4.67d | 7.21 ± 3.11d |
| GSP(mmol/L) | 0.61 ± 0.11 | 1.63 ± 0.44b | 0.94 ± 0.29d | 0.91 ± 0.28d | 0.90 ± 0.32d |
| TC(mmol/L) | 2.08 ± 0.41 | 6.58 ± 1.50 | 2.59 ± 1.10 | 2.46 ± 1.15 | 2.11 ± 0.53 |
| TG(mmol/L) | 0.65 ± 0.17 | 2.71 ± 0.86b | 1.09 ± 0.67 | 0.76 ± 0.23 | 0.81 ± 0.37 |
| HDL-C(mmol/L) | 1.71 ± 0.31 | 0.84 ± 0.26 | 1.56 ± 0.40 | 1.55 ± 0.31 | 1.77 ± 0.33 |
| LDL-C(mmol/L) | 0.49 ± 0.23 | 3.46 ± 0.81 | 0.66 ± 0.37 | 0.71 ± 0.29 | 1.56 ± 0.40 |
| FFA(μmol/L) | 0.51 ± 0.06 | 1.95 ± 0.21b | 0.53 ± 0.10d | 1.01 ± 0.15d | 0.78 ± 0.17d |
| SOD(U/ml) | 295.6 ± 45.8 | 188.7 ± 28.4b | 291.9 ± 52.2d | 248.6 ± 39.5c | 249.8 ± 30.8d |
| MDA(nmol/L) | 2.26 ± 0.71 | 10.83 ± 0.61b | 4.48 ± 1.78d | 5.51 ± 2.26d | 5.12 ± 1.35d |
The diabetic rats were orally ingested by coroslic acid (50 or 100 mg/kg) and metformin (100 mg/kg) once a day for 6 weeks. The rats of normal control and diabetic control were administrated with vehicle. All above indexes were analyzed after six weeks conducting. Values are recorded by mean ± S.D. for 9 rats in each group. One-way ANOVA test was applied for comparisons between different groups. bP < 0.01 compared with normal control group; cP < 0.05 compared with diabetic control group; dP < 0.01 compared with diabetic control group.
Then, we further illustrated the influences of CA on hyperlipidemia in diabetic rats on assessing the serum levels of HDL-C, LDL-C, TC, TG and FFAs. The results in Table 5 presented that the levels of TC, TG, LDL-C and FFAs were upregulated while the level of HDL-C was downregulated in diabetic rats with significant differences. Administration of CA on diabetic rats remarkably prevented these increases and decreases. These findings show that CA has potential antihyperlipidemic effect in T2D rats.
As we know, the increased level of oxidative stress is the key factor leading to diabetes and its complications. Therefore, in order to exploit the effect of CA on lipid peroxidation, inflammation, and the SOD activity, we also measured MDA and ICAM-1 levels in serum. Compared to normal control rats, MDA and ICAM-1 levels were significantly upregulated, while the SOD activity was remarkably downregulated in diabetic groups (Table 5, Fig. 5D). And rats treated with CA showed decreasing MDA and ICAM-1 levels and increasing SOD activity than diabetic control rats. These results suggest that CA possess crucial antioxidant and anti-inflammatory function in T2D rats.
Insulin resistance is associated with inflammation, which is recognized as potential factor in pathogenesis of T2D36. In our study, the IRI (insulin resistance index) in diabetic rats was observably higher than normal control rats, and rats administrated with CA strikingly declined IRI compared to the diabetic rats (Fig. 5E), which show that CA had suppressive effect of insulin resistance.
Discussion
Type 2 diabetes mellitus (T2DM) as an epidemic disease, associated with increased significant social and financial burden, is a cause of very high morbidity and mortality in the world2. It is characterized by abnormal glucose and lipid metabolism due in part to insulin resistance in skeletal muscle, liver and fat, leading to elevated hepatic glucose production, hyperglycemia and hyperlipidemia37. Patients with T2DM suffer 2–8 times more deaths than patients with cardiovascular disease38. The bioactive products derived from plants, which are with the benefits of availability of materials, affordability, relatively cheap and little or no side effects39, are being considered to be a promising source to design effective therapeutic agents for fatal disease including cancer, cardiovascular and diabetes mellitus40.
Among numbers of natural products, triterpenoids own various of therapeutic characteristics, containing a hypoglycemic activity41. Corosolic acid, a triterpenoid, has been discovered in many Chinese medicinal herbs and been considered as an anti-diabetes agent in food supplementary products42. Studies have showed that triterpenoid extract crucially decreased plasma glucose levels in diabetic rats8, and corosolic aicd had a lowering effect on post-challenge plasma glucose levels in vivo in humans18. In addition, many researchers have been trying to find out CA hypoglycemic underlying mechanism. Miura T suggested that the acute hypoglycemic effect of CA was derived, at least in part, from an increase in GLUT4 translocation in mouse muscle, and that CA improved glucose metabolism by reducing insulin resistance43. Shi. L demonstrated that CA may exert its antidiabetic effects through enhancing insulin receptor β phosphorylation by inhibiting certain PTPs20. Cheng K reported that CA represented a new class of allosteric site inhibitors of glycogen phosphorylase(GP),and their glucose-lowing activity could, at least in part, be due to modulation of glycogen metabolism44. In addition, Yamada found that CA increased glucokinase activity without affecting glucose-6-phosphatase activity, suggesting an increase in glycolysis45,46. According to the researches to date, no side effects have been reported in animals, nor have adverse events been viewed or reported in controlled human clinical studies. Consider together, it is likely that CA might implement its glucose-lowing effect through multiple targets.
In our study, CA were isolated by semi-preparative high-performance liquid-phase method from Eriobotrya japonica leaves of Santan area, the structure and purity of which were confirmed and characterized by NMR, EI-MS spectra and HPLC. Then we invited three different T2D models to systematically research on hypoglycemic effect and potential mechanism of corosolic acid. Phosphoenolpyruvate carboxy kinase (PEPCK) is the rate-limiting enzyme of gluconeogenesis. Enhanced expression of the PEPCK gene in liver is present in most diabetes models and PEPCK overexpression is thought to contribute to the increased hepatic glucose output seen in this disease47. A PEPCK gene overexpression HepG2 cell model was established. Different concentrations of CA promoted the consumption of glucose in HepG2 cells, which can improve the degradation of glycogen in cAMP and DEX-induced T2D cell models, inhibited the overexpression of PEPCK.
Zebrafish are complex vertebrates and maintain similarly elaborate mechanisms for activating or mitigating the effects of exogenous chemical substances48. It has a short generation time, are highly fertile, and cost little in terms of housing space and daily maintenance owing to their tiny size49. Therefore, zebrafish have been used extensively as a model to investigate many vertebrate biological process, including cancer, melanoma, cardiovascular disease, immune system, antioxidative stress and diabetes mellitus26. Herein, we firstly established a T2D zebrafish model to evaluate the CA effect on carbon metabolism. This model can not only induce hyperglycemia, but also induce insulin resistance. Our results showed that CA inhibited expression of PEPCK, GLUT1,GLUT2, GLUT3, LDHA, LDHB and INSα, and improve expression levels of GP, GYS1, G6Pase, PFKFB3 and INSR, suggesting the promotion of glycolysis (Fig. S5).
Additionally, T2D rats were treated by high-fat diet and a low dose of STZ. After 6 weeks of continuous gavage administration, the rats suffered from hyperglycemia with higher FBG, GSP, TC, TG, LDL-C and FFA level and lower HDL-C level. Additionally, higher glucose tolerance and insulin resistance index were also shown in diabetic rats, both of which were considered widely as type 2 diabetic markers34. Our results revealed that CA alleviated the weight loss of diabetic rats, significantly reduced biochemical parameters including FBG, GSP, TC, TG, LDL-C and FFA level of T2D rats, and improved HDL-C level. And rats treated with CA showed decreasing MDA and ICAM-1 levels and increasing SOD activity than diabetic control rats. Furthermore, rats administrated with CA pronouncedly inhibited IRI compared to the diabetic rats. Taken together, CA can inhibit blood glucose elevation, possess promising antioxidant and anti-inflammatory action, and have an insulin resistance inhibitory effect as well in STZ-induced T2D rats.
Conclusion
In summary, the results indicate CA extracted from Eriobotrya japonica leaves was with high accurate, purity and content. And CA could strongly improve impaired glucose, hyperlipidemia and insulin resistance in T2D models, which were relied on declining the expression of PEPCK and other genes involved in carbon metabolism, T2D related oxidative stress and inflammation. Hence, CA may be a promising agent in the treatment of T2D and more future investigations would be undertaken on its safety and efficacy in clinical trials.
Experimental Section
Ethics statement
All animal experiments in this study were conducted in compliance with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996) and approved by the Animal Care and Use Committee of Nanjing Normal University, China (Permit Number 2090658).
Chemicals and reagents
Dried Eriobotrya japonica leaves were collected from southern part of Anhui province named shexian county. Methanol, ethanol, acetic acid and other all HPLC solvents were bought from Sigma-Aldrich Chemical Co, Ltd. (St. Louis, MO, USA), and all other analytical grade reagents were obtained from Aladdin (Shanghai, China). Corosolic acid (CA) standards (HPLC ≥ 95%) were purchased from Jiangsu Institute for Food and Drug Control. Metformin HCL, DEPC, Dexamethasone, Adenyl-3′, 5′-cyclic phosphate, STZ, Sodium citrate, Citric acid and Glucose were purchased from Sigma Aldrich.
Dulbecco’s Modified Eagle’s Medium (DMEM) and fetal bovine serum (FBS) were purchased from Gibico (Thermo Fisher Scientific, Grand Island, USA). Cell counting kit-8(CCK-8), RNA isolaterTM Total RNA Extraction Reagent, HiScriptTM II Q RT SuperMix for qPCR and AceQ qPCR SYBR Green Master Mix (High ROX) were purchased from Vazyme Co. Ltd. (Nanjing, Jiangsu, China). Intercellular Adhesion Molecule-1 (ICAM-1) ELISA Kit and Insulin ELISA Kit were purchased from Dakewe Biotech Co., Ltd (Shanghai, China). Glucose assay kit, Muscle/liver glycogen test kit, glycated serum protein (GSP), FFAs, malondialdehyde (MDA) and superoxide dismutase (SOD) were purchased from Nanjing Jiancheng Bioengineering Institute (Nanjing, China). The kits for measurement of total cholesterol (TC), triglyceride (TG), high density lipoprotein-cholesterol (HDL-C), low density lipoprotein-cholesterol (LDL-C) were purchased from Sigma-Aldrich Chemical Co, Ltd. (St. Louis, MO, USA).
Preparation of 4 mM dexamethasone (DEX) mother liquor: Weigh 0.0167 g of DEX powder, dissolve it with appropriate amount of ultrapure water, sonicate for 20 min, dilute to 10 ml, configure into 4000 μM DEX mother liquor, store at −20 °C, and leave for use.
Preparation of 5 mM adenyl-3′,5′-cyclic phosphate (cAMP) mother liquor: Weigh 0.0165 g cAMP powder, add appropriate amount of ultrapure water to dissolve, sonicate for 20 min, dilute to 10 ml, configure into 5000 μM cAMP mother liquor, place Store at −20 °C and leave for spare.
Preparation of 10 × E3 zebrafish embryo culture solution: Weigh NaCl: 1462.5 mg, KCl: 63.325 mg, CaCl2: 242.583 mg, MgSO4: 198 mg, add appropriate amount of mono-distilled water to dissolve, sonicate for 20 min, after all dissolved, transfer to 500 mL volumetric flask Medium, constant volume, the prepared mother liquid is stored in a refrigerator at 4 °C, and diluted 10 times with single distilled water.Preparation of a molding agent: A solution having a final concentration of 100 μM (cAMP) and 1 μM (DEX) was prepared using 1 × E3.
Adult Tuebingen zebrafish were brought from Model Animal Research Center of Nanjing University and Male Sprague-Dawley rats (180–200 g) were purchased from Qing Longshan Animal Breeding Farm in Nanjing. Animal quality certificate number: SYXK (Su) 2014-0052.
Cell culture, animals and treatments
Human liver hepatocellular carcinoma cells (HepG2) were kept by our own lab and cultured in DMEM supplemented with 10% FBS in a humidified atmosphere containing 5% CO2 at 37 °C.
The wild type zebrafish was reared with filtered tap water, with a photoperiod of 14 h (daylight)/10 h (dark night) and a temperature of 28 ± 1 °C. Zebrafish are fed twice a week with dried fish and brine shrimp50. Eggs were collected from natural spawning that was induced in the morning by turning on the light. The eggs were obtained within 30 min after fertilization and incubated in double distilled water until the desired developmental age.
SD Rats were fed with normal diets (21.5% protein, 6.5% calories, 4.1% fiber, 8% ash, and 2.8% minerals) and were allowed to eat freely in the laboratory. The plastic cage was filled with tap water (four to five per cage), the temperature was controlled at (22 ± 2 °C), relative humidity (50% to 60%), and a 12 h light/dark cycle was maintained. The rats were domesticated for a week.
After continuous gavage for six weeks, rats in each group were anesthetized with sodium pentobarbital (60 mg/Kg) intraperitoneally and euthanized by cervical dislocation. Blood was taken from the femoral artery and placed in a centrifuge tube coated with EDTA. The sample was centrifuged at 3000 rpm for 10 minutes at 4 °C. The serum was collected and stored at −20 °C until use.
Cytotoxicity assay of HepG2 cells in vitro
5 × 104 cells/mL HepG2 cells were added to 96-well cell culture plates at 100 μL per well. They were incubated in a 37 °C, 5% CO2 incubator for different times. Cytotoxicity assay was measured by CCK8 kit according to the manufacturer’s protocols.
Cellular glucose consumption assay
Cells were randomly divided into different group containing low glucose DMEM medium. After 12 hours, 24 hours, or 36 hours incubation, glucose assay kit was used to measure the glucose consumption. Add 10 μL CCK8 cross-shaking 96-well plate to each well. After incubation for 1 h in a cell culture incubator, the absorbance was measured at 450 nm, and the glucose consumption per well was calculated by glucose content divided corresponding OD value of CCK8 to obtain the unit glucose consumption per well. Three replicated wells were used in each group and the experiment was repeated three times.
Cell glycogen accumulation assay
HepG2 cells were kept with serum-free high-glucose DMEM culture medium and starved for 12 hours. The cells were randomly divided into different groups and cultured in low glucose medium for another 12 hours. Then the cells were collected and washed twice with 1 mL of 1X PBS. The glycogen content of cells in each experimental treatment group was subsequently determined following a liver glycogen assay kit.
Glucose concentration detection in tissue fluid of zebrafish larvae
Whole body glucose was determined by using an Amplex Red glucose assay kit (Life Technologies) according to the instructions.
Establishment of diabetic zebrafish model
After 96 hours of fertilization, zebrafish juveniles which have fully developed organs including the liver and pancreas were sowed in six-well cell culture plates, 20 zebrafish juveniles were added to each well, and 3 mL cultures were added to the blank group. 3 mL of culture medium containing 100 μM cAMP and 1000 nM DEX was added to each well of the treatment group. After incubated for 48 h, total mRNA was extracted using the total RNA extraction kit for RT-qPCR, and the expression level of PEPCK gene was detected.
Zebrafish toxicity assay
The fertilized fish eggs were collected by plastic pipettes, sown in 24 well plates, 6 per well, and randomly divided into groups with different CA concentrations (0.1, 0.5, 1, 5, 10 μM). Toxicity test was further determined by the observation of the survival of zebrafish juveniles and the presence of hydrocele every day. Fish were not fed and dead fish were immediately removed from the wells.
Blood glucose detection assay in rats
The rats were abstained from food except water for 12 h. At 0 and 120 min, the venous plexus blood was taken for blood glucose determination. The levels of glucose in rat serum were measured according to the test methods specified in the kit’s instructions.
- The area under the blood glucose curve (AUC) is calculated as follows:
Bg0, Bg0.5, Bg1, Bg1.5, and Bg2 correspond to glucose concentrations after 0, 0.5, 1, 1.5, and 2 h glucose loading, respectively.1 -
The inhibition rate of fasting blood glucose is calculated according to the following formula:
C0: fasting blood glucose in the normal control group,2 C1: fasting blood glucose in the diabetic control group,
C2: fasting blood glucose in the administration group.
The insulin resistance index (IRI) is calculated according to the following formula:
| 3 |
FBG: fasting blood glucose; FBI: fasting blood insulin levels.
Oral glucose tolerance test in rats
The oral glucose tolerance test was performed in the fifth week. After continuous administration of corosolic acid for 5 weeks, rats fasted for 12 h. Blood was then taken from the venous plexus of the rat’s eyelid to measure the blood glucose level of fasting blood glucose for 0 min. Rats received oral glucose 2.0 g/kg. Blood samples were collected 30 min, 60 min, 90 min, and 120 min after glucose loading. Blood glucose levels were measured with a kit, and changes in OGTT before and after treatment were observed.
RNA extraction and quantitative real time PCR (qRT-PCR)
After different treatment, total RNA was extracted from cells using the RNA isolaterTM Total RNA Extraction Reagent (Vazyme Co. Ltd.). RNA concentration was determined using a nucleic acid protein assay, and cDNA was synthesized from the total RNA using the HiScriptTM II Q RT SuperMix for qPCR kit (Vazyme Co.Ltd.) according to the manufacturer’s instructions. To assess the expression of genes in each treatment group, the cDNA was used as the template for real-time PCR using AceQ qPCR SYBR Green Master Mix (High ROX) kit (Vazyme Co. Ltd.). All primers were listed in Table 6 27.
Table 6.
Danio rerio primers for RT-PCR assays.
| Name | Accession | Direction | Primer sequence (5′-3′) |
|---|---|---|---|
| Target gene | |||
| PEPCK | NM_002591.3 | Forward | AAAACGGCCTGAACCTCTCG |
| Reverse | ACACAGCTCAGCGTTATTCTC | ||
| INS | NM_131056.1 | Forward | AGTGTAAGCACTAACCCAGGCACA |
| Reverse | TGCAAAGTCAGCCACCTCAGTTTC | ||
| INSRa | NM_001142672.1 | Forward | CAACATGCCCCCTCACCACT |
| Reverse | CGACACACATGTTGTTGTG | ||
| INSRb | NM_001123229.1 | Forward | GACTGATTACTATCGCAAGGG |
| Reverse | TCCAGGTATCCTCCGTCCAT | ||
| GLUT1 | NM_001039808.1 | Forward | TCCCATGGTTCATTGTGGCA |
| Reverse | GCCGGTCAGTTCCTCAACAT | ||
| GLUT2 | NM_001042721.1 | Forward | GGGATACAGCTTGGGCGTCATC |
| Reverse | GGACAACATGCCTCCGACAGAGA | ||
| GLUT3 | NM_006931.3 | Forward | ACTTGCTGCTGAGAAGGACAT |
| Reverse | GGGTGACCTTCTGTGTCCCC | ||
| LDHA | NM_131246.1 | Forward | TTCCTCACATCACCAGTGCG |
| Reverse | GAGGCCATCTTCAACTGTGG | ||
| LDHB | NM_001174097.2 | Forward | AGCGGAGAGACTTGTTGCATT |
| Reverse | CAGCCAGAGACTTTCCCAGAA | ||
| GP | NM_001008538.1 | Forward | CTTCCCTGATAAGGTTGCCA |
| Reverse | TCCACAAATATCCGCATCAA | ||
| GYS1 | NM_201180.2 | Forward | CTCTCCTCAACTTCTCCTCTC |
| Reverse | CTCGGCTGGTGTGTATCC | ||
| G6Pase | NM_001163806.1 | Forward | CCACACCGTTCGCAAGTC |
| Reverse | CCACACCGTTCGCAAGTC | ||
| PFKFB3 | NM_213397.1 | Forward | TTCGCAGGTGCTCTTGCTA |
| Reverse | GTTCGTACGGCACATTGAGA | ||
| β-actin | NM_131031.1 | Forward | CGAGCAGGAGATGGGAACC |
| Reverse | CAACGGAAACGCTCATTGC | ||
Statistical analysis
All the experimental results were triply performed and analyzed by GraphPad Prism 7 software (GraphPad Software, Inc, La Jolla, CA, USA). The data are presented as mean ± SEM. The statistical analyses were assessed by Student’s t-test. P-value < 0.05 was considered significantly difference.
Supplementary information
Acknowledgements
We thank analysis and testing center of Nanjing Normal University for NMR, LC-MS and IR analysis and Pro.Wei from Jiangsu Branch of China Academy of Chinese Medical Science for zebrafish guidance. This work was supported by grants from Science and Technology Major Projects of Anhui Province (Grant No. 17030801026) and Nanjing Medical Science and Technique Development Foundation (No. YKK18123).
Author Contributions
Shuwen Xu contributed to study design, manuscript preparation and funds collection; Gang Wang contributed to study design, manuscript preparation and literature search; Wei Peng contributed to data collection; Yandi Xu contributed to statistical analysis; Yu Zhang and Ying Ge contributed to data interpretation; Yue Jing contributed to study design, manuscript preparation, literature search and data analysis; Zhunan Gong contributed to study design and funds collection. All authors reviewed the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shuwen Xu, Gang Wang contributed equally.
Contributor Information
Yue Jing, Email: jingyueshadow@126.com.
Zhunan Gong, Email: gongzhunan@njnu.edu.cn.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-40934-7.
References
- 1.Hartstra AV, Bouter KE, Backhed F, Nieuwdorp M. Insights into the role of the microbiome in obesity and type 2 diabetes. Diabetes care. 2015;38:159–165. doi: 10.2337/dc14-0769. [DOI] [PubMed] [Google Scholar]
- 2.Liu X, et al. Glucosidase inhibitory activity and antioxidant activity of flavonoid compound and triterpenoid compound from Agrimonia Pilosa Ledeb. BMC complementary and alternative medicine. 2014;14:12. doi: 10.1186/1472-6882-14-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee SY, et al. Rhodiola crenulata extract suppresses hepatic gluconeogenesis via activation of the AMPK pathway. Phytomedicine. 2015;22:477–486. doi: 10.1016/j.phymed.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 4.Theodoulou FL, Eastmond PJ. Seed storage oil catabolism: a story of give and take. Current opinion in plant biology. 2012;15:322–328. doi: 10.1016/j.pbi.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 5.Waltner-Law M, et al. Elements of the glucocorticoid and retinoic acid response units are involved in cAMP-mediated expression of the PEPCK gene. J Biol Chem. 2003;278:10427–10435. doi: 10.1074/jbc.M211846200. [DOI] [PubMed] [Google Scholar]
- 6.Cournarie F, et al. The inhibitory effect of glucose on phosphoenolpyruvate carboxykinase gene expression in cultured hepatocytes is transcriptional and requires glucose metabolism. FEBS letters. 1999;460:527–532. doi: 10.1016/S0014-5793(99)01407-6. [DOI] [PubMed] [Google Scholar]
- 7.Tang Y, et al. Overexpression of PCK1 Gene Antagonizes Hepatocellular Carcinoma Through the Activation of Gluconeogenesis and Suppression of Glycolysis Pathways. Cell Physiol Biochem. 2018;47:344–355. doi: 10.1159/000489811. [DOI] [PubMed] [Google Scholar]
- 8.Judy WV, et al. Antidiabetic activity of a standardized extract (Glucosol) from Lagerstroemia speciosa leaves in Type II diabetics. A dose-dependence study. Journal of ethnopharmacology. 2003;87:115–117. doi: 10.1016/S0378-8741(03)00122-3. [DOI] [PubMed] [Google Scholar]
- 9.Senat MV, et al. Effect of Glyburide vs Subcutaneous Insulin on Perinatal Complications Among Women With Gestational Diabetes: A Randomized Clinical Trial. Jama. 2018;319:1773–1780. doi: 10.1001/jama.2018.4072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abuissa H, Jones PG, Marso SP, O’Keefe JH., Jr. Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for prevention of type 2 diabetes: a meta-analysis of randomized clinical trials. Journal of the American College of Cardiology. 2005;46:821–826. doi: 10.1016/j.jacc.2005.05.051. [DOI] [PubMed] [Google Scholar]
- 11.Wu PP, Zhang K, Lu YJ, He P, Zhao SQ. In vitro and in vivo evaluation of the antidiabetic activity of ursolic acid derivatives. European journal of medicinal chemistry. 2014;80:502–508. doi: 10.1016/j.ejmech.2014.04.073. [DOI] [PubMed] [Google Scholar]
- 12.Hou W, et al. Triterpene acids isolated from Lagerstroemia speciosa leaves as alpha-glucosidase inhibitors. Phytotherapy Research. 2009;23:614–618. doi: 10.1002/ptr.2661. [DOI] [PubMed] [Google Scholar]
- 13.Liby KT, Yore MM, Sporn MB. Triterpenoids and rexinoids as multifunctional agents for the prevention and treatment of cancer. Nature reviews. Cancer. 2007;7:357–369. doi: 10.1038/nrc2129. [DOI] [PubMed] [Google Scholar]
- 14.Zong W, Zhao G. Corosolic acid isolation from the leaves of Eriobotrta japonica showing the effects on carbohydrate metabolism and differentiation of 3T3-L1 adipocytes. Asia Pacific journal of clinical nutrition. 2007;16(Suppl 1):346–352. [PubMed] [Google Scholar]
- 15.Park SH, Oh SR, Ahn KS, Kim JG, Lee HK. Structure determination of a new lupane-type triterpene, tiarellic acid, isolated from Tiarella polyphylla. Archives of pharmacal research. 2002;25:57–60. doi: 10.1007/BF02975262. [DOI] [PubMed] [Google Scholar]
- 16.Woo, S. M. et al. Corosolic Acid Induces Non-Apoptotic Cell Death through Generation of Lipid Reactive Oxygen Species Production in Human Renal Carcinoma Caki Cells. International journal of molecular sciences19, 10.3390/ijms19051309 (2018). [DOI] [PMC free article] [PubMed]
- 17.Liu Q, et al. Determination of corosolic acid, a natural potential anti-diabetes compound, in rat plasma by high-performance liquid chromatography-mass spectrometry and its application to pharmacokinetic and bioavailability studies. Planta medica. 2011;77:1707–1711. doi: 10.1055/s-0030-1270993. [DOI] [PubMed] [Google Scholar]
- 18.Fukushima M, et al. Effect of corosolic acid on postchallenge plasma glucose levels. Diabetes research and clinical practice. 2006;73:174–177. doi: 10.1016/j.diabres.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Wen X, et al. Pentacyclic triterpenes. Part 5: synthesis and SAR study of corosolic acid derivatives as inhibitors of glycogen phosphorylases. Bioorganic & medicinal chemistry letters. 2007;17:5777–5782. doi: 10.1016/j.bmcl.2007.08.057. [DOI] [PubMed] [Google Scholar]
- 20.Shi L, et al. Corosolic acid stimulates glucose uptake via enhancing insulin receptor phosphorylation. European journal of pharmacology. 2008;584:21–29. doi: 10.1016/j.ejphar.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 21.Jayakumar KS, et al. Corosolic acid content and SSR markers in Lagerstroemia speciosa (L.) Pers.: a comparative analysis among populations across the Southern Western Ghats of India. Phytochemistry. 2014;106:94–103. doi: 10.1016/j.phytochem.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Sivakumar G, Vail DR, Nair V, Medina-Bolivar F, Lay JO., Jr. Plant-based corosolic acid: future anti-diabetic drug? Biotechnol J. 2009;4:1704–1711. doi: 10.1002/biot.200900207. [DOI] [PubMed] [Google Scholar]
- 23.Tidke PS, Patil CR. Nrf2 activator corosolic acid meliorates alloxan induced diabetic nephropathy in mice. Asian Pacific Journal of Tropical Biomedicine. 2017;7:797–804. doi: 10.1016/j.apjtb.2017.08.010. [DOI] [Google Scholar]
- 24.Miura T, et al. Antidiabetic effects of corosolic acid in KK-Ay diabetic mice. Biological & pharmaceutical bulletin. 2006;29:585–587. doi: 10.1248/bpb.29.585. [DOI] [PubMed] [Google Scholar]
- 25.Miura T, Takagi S, Ishida T. Management of Diabetes and Its Complications with Banaba (Lagerstroemia speciosa L.) and Corosolic Acid. Evidence-based complementary and alternative medicine: eCAM. 2012;2012:871495. doi: 10.1155/2012/871495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kang M-C, et al. Protective effect of fucoxanthin isolated from Ishige okamurae against high-glucose induced oxidative stress in human umbilical vein endothelial cells and zebrafish model. Journal of Functional Foods. 2014;11:304–312. doi: 10.1016/j.jff.2014.09.007. [DOI] [Google Scholar]
- 27.Elo B, Villano CM, Govorko D, White LA. Larval zebrafish as a model for glucose metabolism: expression of phosphoenolpyruvate carboxykinase as a marker for exposure to anti-diabetic compounds. J Mol Endocrinol. 2007;38:433–440. doi: 10.1677/JME-06-0037. [DOI] [PubMed] [Google Scholar]
- 28.Maddison LA, Chen WB. Nutrient Excess Stimulates beta-Cell Neogenesis in Zebrafish. Diabetes. 2012;61:2517–2524. doi: 10.2337/db11-1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li, E.-N., Zhou, G.-D. & Kong, L.-Y. Chemical Constituents from the Leaves of Eriobotrya japonica. Vol. 7 (2009).
- 30.Yang J, Kalhan SC, Hanson RW. What is the metabolic role of phosphoenolpyruvate carboxykinase? J Biol Chem. 2009;284:27025–27029. doi: 10.1074/jbc.R109.040543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Montal ED, et al. PEPCK Coordinates the Regulation of Central Carbon Metabolism to Promote Cancer Cell Growth. Mol Cell. 2015;60:571–583. doi: 10.1016/j.molcel.2015.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Michel M, Page-McCaw PS, Chen W, Cone RD. Leptin signaling regulates glucose homeostasis, but not adipostasis, in the zebrafish. Proc Natl Acad Sci USA. 2016;113:3084–3089. doi: 10.1073/pnas.1513212113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gao HX, Regier EE, Close KL. International Diabetes Federation World Diabetes Congress 2015. Journal of diabetes. 2016;8:300–302. doi: 10.1111/1753-0407.12377. [DOI] [PubMed] [Google Scholar]
- 34.Lebovitz HE. Insulin resistance–a common link between type 2 diabetes and cardiovascular disease. Diabetes, obesity & metabolism. 2006;8:237–249. doi: 10.1111/j.1463-1326.2005.00521.x. [DOI] [PubMed] [Google Scholar]
- 35.Ren B, et al. Apigenin and naringenin regulate glucose and lipid metabolism, and ameliorate vascular dysfunction in type 2 diabetic rats. European journal of pharmacology. 2016;773:13–23. doi: 10.1016/j.ejphar.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 36.Cersosimo E, DeFronzo RA. Insulin resistance and endothelial dysfunction: the road map to cardiovascular diseases. Diabetes/metabolism research and reviews. 2006;22:423–436. doi: 10.1002/dmrr.634. [DOI] [PubMed] [Google Scholar]
- 37.Ha do T, et al. Selected compounds derived from Moutan Cortex stimulated glucose uptake and glycogen synthesis via AMPK activation in human HepG2 cells. Journal of ethnopharmacology. 2010;131:417–424. doi: 10.1016/j.jep.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 38.Penno, G. et al. Non-albuminuric renal impairment is a strong predictor of mortality in individuals with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicentre study. Diabetologia, 10.1007/s00125-018-4691-2 (2018). [DOI] [PubMed]
- 39.Engel N, Oppermann C, Falodun A, Kragl U. Proliferative effects of five traditional Nigerian medicinal plant extracts on human breast and bone cancer cell lines. Journal of ethnopharmacology. 2011;137:1003–1010. doi: 10.1016/j.jep.2011.07.023. [DOI] [PubMed] [Google Scholar]
- 40.Kashyap D, Tuli HS, Sharma AK. Ursolic acid (UA): A metabolite with promising therapeutic potential. Life sciences. 2016;146:201–213. doi: 10.1016/j.lfs.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 41.Hamid K, et al. Tetracyclic triterpenoids in herbal medicines and their activities in diabetes and its complications. Curr Top Med Chem. 2015;15:2406–2430. doi: 10.2174/1568026615666150619141940. [DOI] [PubMed] [Google Scholar]
- 42.Stohs SJ, Miller H, Kaats GR. A review of the efficacy and safety of banaba (Lagerstroemia speciosa L.) and corosolic acid. Phytotherapy research: PTR. 2012;26:317–324. doi: 10.1002/ptr.3664. [DOI] [PubMed] [Google Scholar]
- 43.Miura T, et al. Corosolic acid induces GLUT4 translocation in genetically type 2 diabetic mice. Biological & pharmaceutical bulletin. 2004;27:1103–1105. doi: 10.1248/bpb.27.1103. [DOI] [PubMed] [Google Scholar]
- 44.Cheng K, Zhang P, Liu J, Xie J, Sun H. Practical synthesis of bredemolic acid, a natural inhibitor of glycogen phosphorylase. J Nat Prod. 2008;71:1877–1880. doi: 10.1021/np8003886. [DOI] [PubMed] [Google Scholar]
- 45.Yamada K, et al. Dietary corosolic acid ameliorates obesity and hepatic steatosis in KK-Ay mice. Biological & pharmaceutical bulletin. 2008;31:651–655. doi: 10.1248/bpb.31.651. [DOI] [PubMed] [Google Scholar]
- 46.Yamada K, et al. Effect of corosolic acid on gluconeogenesis in rat liver. Diabetes research and clinical practice. 2008;80:48–55. doi: 10.1016/j.diabres.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 47.Davies GF, Khandelwal RL, Wu L, Juurlink BH, Roesler WJ. Inhibition of phosphoenolpyruvate carboxykinase (PEPCK) gene expression by troglitazone: a peroxisome proliferator-activated receptor-gamma (PPARgamma)-independent, antioxidant-related mechanism. Biochemical pharmacology. 2001;62:1071–1079. doi: 10.1016/S0006-2952(01)00764-X. [DOI] [PubMed] [Google Scholar]
- 48.Rennekamp AJ, Peterson RT. 15 years of zebrafish chemical screening. Current opinion in chemical biology. 2015;24:58–70. doi: 10.1016/j.cbpa.2014.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Asaoka Y, Terai S, Sakaida I, Nishina H. The expanding role of fish models in understanding non-alcoholic fatty liver disease. Dis Model Mech. 2013;6:905–914. doi: 10.1242/dmm.011981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Manigandan K, Jayaraj RL, Jagatheesh K, Elangovan N. Taxifolin mitigates oxidative DNA damage in vitro and protects zebrafish (Danio rerio) embryos against cadmium toxicity. Environ Toxicol Pharmacol. 2015;39:1252–1261. doi: 10.1016/j.etap.2015.04.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.