Abstract
Background
The Mediterranean Diet (MD) is a model of healthy eating contributing to a favorable health status, but its clinical usefulness is still debated. The aim of this study was to relate the adherence to MD with the incidence of cardio/cerebro-vascular events (VEs) in north and south European participants of the IMPROVE study.
Methods
IMPROVE is an observational, longitudinal, prospective cohort study involving 3703 individuals from five European countries (Finland, Sweden, Netherlands, France and Italy). The study end-point was the incidence of the first combined cardio/cerebro-vascular event occurring during 36-months follow-up. At baseline, a dietary questionnaire about the usual intake during the year preceding enrollment was administered. Based on 7 nutritional items, a MD Score was constructed in which minimal adherence was 0 and maximal adherence was 7.
Results
Latitude was the strongest determinant of MD score (p < 0.001). VEs occurred in 215 participants. The incidence of VEs was the highest in subjects with MD score 0–1, lower in those with score 2–3 and the lowest in those with score ≥ 4. MD score remained significantly associated with subsequent VEs after adjustment for confounders (hazard ratio for one-point increment of the score = 0.75, p < 0.001) and the association was stronger in northern than in southern countries (p = 0.04 for MD Score × latitude interaction).
Conclusions
The MD adherence score based on a simple dietary questionnaire detects changes of risk of VEs. According to our findings north Europeans appear to benefit most from VE-prevention when their diet is altered to the MD diet.
Abbreviations: MD, Mediterranean Diet; CAD, Coronary artery disease; cIMT, carotid intima media thickness; VEs, Vascular Events; VRFs, vascular risk factors; TIA, transient ischemic attack; hs-CRP, high sensitive C-Reactive Protein
Keywords: Mediterranean diet score, IMPROVE study, Vascular diseases
Highlights
-
•
Mediterranean Diet score is able to detect changes of risk of vascular events.
-
•
Latitude is the strongest determinant of Mediterranean Diet score.
-
•
North Europeans are the best candidates for intervention with Mediterranean Diet.
1. Introduction
Mediterranean Diet (MD) is a model of healthy eating, known for its contribution to a favorable health status and a better quality of life [1]. MD is based on high consumption of olive oil, legumes, unrefined cereals, fruits, vegetables, moderate/high consumption of fish, moderate consumption of dairy products (mostly cheese and yogurt), wine (especially during meals), and low consumption of meat and meat products [2].
Several studies have documented a positive association between chronic diseases and single foods/nutrients not included into MD such as meat [3], and a negative association with those close to MD (fruit and vegetables [4], diet antioxidants [5]). Based on the results of the Seven Countries Study [6], Trichopoulou et al. conducted an observational prospective study in a large Greek cohort investigating the capacity of a 10-point scale MD adherence score to predict the overall and coronary artery disease (CAD) mortalities [7]. The authors showed that the adherence to MD (rather than to some of its individual components) was inversely associated with coronary death. A meta-analysis of prospective cohort studies on 4,172,412 subjects confirmed these findings and the authors proposed a nine item literature-based MD score that may predict the cardiovascular (CV) risk at the individual level [8]. In the present study, we took advantage of the large IMPROVE study, carried out in 5 European countries with major differences in dietary behavior, to investigate the association of a seven item MD adherence score with the incidence of cardio- and cerebro-vascular events (VEs) in north and south Europe.
2. Material and methods
A summary of design, objectives, eligibility criteria, methods, baseline characteristics, ultrasonographic variables and type and numbers of VEs in the IMPROVE Study have been reported [[9], [10], [11]]. Briefly, IMPROVE is an observational, longitudinal, prospective cohort study that enrolled 3703 patients (1774 men, 1929 women, aged 55–79 years) with ≥3 vascular risk factors (VRFs) free from VEs. Participants were recruited from January 2004 to May 2005 in seven centers in 5 European countries: Finland (n = 1048; 2 centers), Sweden (n = 532), the Netherlands (n = 527), France (n = 501) and Italy (n = 553 in Milan and 542 in Perugia). 36 months follow-up was attained by 93.7% of participants. The combined endpoint included angina pectoris, myocardial infarction, cardiovascular death, ischemic stroke, transient ischemic attack (TIA) and revascularizations of coronary or peripheral arteries. The criteria of diagnosis of VEs have been previously described [10,11]. The study complies with the Declaration of Helsinki. Five local ethics committee approved the research protocol. Each participant provided informed consent for general participation in the study and a separate consent for genotyping.
2.1. The IMPROVE MD score
Dietary intake maintained during the year preceding enrollment was assessed by a semi-quantitative dietary questionnaire, administered by trained personnel. Since the amount and type of vegetables, legumes, nuts and cereals consumed differ among populations [12], the items included in the questionnaire were limited to foods freely available in all the countries involved. We created a MD adherence score analogous to the Greek Mediterranean Index [7], since this index was inversely associated with the incidence of stroke in a recent Italian study [13]. Scoring was based on intake of 7 items: fruits, fish, wine, olive oil, meat, milk and eggs. For fruit or fish, high consumption (top tertile of their distributions, i.e. fruit ≥3 servings/day and fish >2 times/week) received one point, other intakes received 0 points; for meat, eggs or milk a low intake (bottom tertile of their respective distributions, i.e. meat <2 times/week, eggs ≤1 times/week, milk ≤3 dL/day) received one point. A predominant consumption of olive oil, rather than of other types of fat, and a moderate consumption of wine (1–2 glasses/day) also received one point. Based on the scale obtained, score 0 indicates minimal adherence and score 7 maximal adherence to the MD.
2.2. Statistical analysis
Quantitative variables are summarized as means ± standard deviation (SD), or median (interquartile range) when appropriate. Variables with skewed distributions were log-transformed before analysis. Baseline characteristics of subjects, stratified by MD score categories, were compared by linear regression and chi-square for trend, as appropriate. Multivariable linear regression with stepwise selection was employed to identify independent predictors of the MD score, and the interaction between latitude and each predictor was also tested. The association between MD score and VEs was assessed by three Cox models: Model-1: unadjusted; Model-2: adjusted for age, gender and stratified by latitude; Model-3: as model 2 plus lifelong exposure to cigarette smoking (pack-years), body mass index (BMI), education (as indexed by years of school), physical activity, occupation (categorized as: 1, white collars; 2, service workers and 3, manual workers), plasma concentrations of LDL and HDL cholesterol, triglycerides, glucose, high sensitive C-Reactive Protein (hs-CRP), creatinine, pulse pressure, antiplatelet and statin treatments. Kaplan-Meier curves stratified by classes of MD score were also computed. In subgroup analysis an interaction term was included in the Cox models. All tests were two-sided. Analyses were carried out by using the SAS statistical package v. 9.4 (SAS Institute Inc., Cary, NC, USA).
3. Results
3.1. Compliance with and determinants of the MD score
Patient's characteristics according to the MD adherence score are presented in Table 1. A score >1 was observed in >90% of the patients in Perugia, Milan and Paris, but only in the 46% of patients in Groningen, Stockholm and Kuopio. The lowest average MD adherence score was found in Groningen (mean ± SD, 1.3 ± 1.1) and in Kuopio (1.7 ± 1.1). Intermediate values were in Stockholm (2.1 ± 1.2) and in Paris (2.9 ± 1.3), whereas the average MD score in Milano and Perugia was >3. With univariate analysis (Table 1), the MD score was negatively and significantly associated with almost all traditional VRFs. Using multivariable analysis, latitude was the strongest independent determinant of MD score (Table 2). Social and behavioral variables, such as education, occupation, physical activity and smoking habits as well as hs-CRP, HDL-cholesterol, BMI, pulse pressure, statin and insulin treatment were also independently associated with MD score (Table 2). A significant interaction between education (a social class index) and latitude was found (p = 0.01), indicating that the dependence of MD score on social class is stronger in northern than in southern countries, the average MD score change for each year of school being 0.06 in Sweden, 0.03 in Finland and 0.016 in Italy.
Table 1.
Patient's characteristics according to classes of MD score.
| Characteristics | Missing data | MD score 0–1 (N = 1098) |
MD score 2–3 (N = 1868) |
MD score 4–7 (N = 737) |
P-trend |
|---|---|---|---|---|---|
| Latitude | |||||
| Kuopio | 0 | 472 (43.0) | 520 (27.8) | 56 (7.6) | |
| Stockholm | 0 | 177 (16.1) | 291 (15.6) | 64 (8.7) | |
| Groningen | 0 | 319 (29.1) | 191 (10.2) | 17 (2.3) | |
| Paris | 0 | 68 (6.2) | 275 (14.7) | 158 (21.4) | <0.0001 |
| Milan | 0 | 37 (3.4) | 282 (15.1) | 234 (31.8) | |
| Perugia | 0 | 25 (2.3) | 309 (16.5) | 208 (28.2) | |
| Vascular risk factors | |||||
| Framingham risk score | 0 | 27 (19, 41) | 22 (14, 33) | 18 (11, 28) | <0.0001 |
| European score | 0 | 5.4 (3.2, 9.0) | 3.8 (2.3, 6.7) | 2.9 (1.8, 5.1) | <0.0001 |
| Male | 0 | 580 (52.8) | 919 (49.2) | 275 (37.3) | <0.0001 |
| Age | 0 | 64.8 ± 5.4 | 63.9 ± 5.31 | 63.9 ± 5.7 | 0.0001 |
| BMI (kg/m2) | 3 | 28.4 ± 4.43 | 27.18 ± 4.22 | 25.83 ± 3.64 | <0.0001 |
| Waist/hip ratio | 11 | 0.93 ± 0.09 | 0.92 ± 0.09 | 0.9 ± 0.09 | <0.0001 |
| Diastolic BP (mmHg) | 5 | 84 ± 10 | 82 ± 10 | 79 ± 9 | <0.0001 |
| Systolic BP (mmHg) | 5 | 147 ± 18 | 142 ± 18 | 135 ± 18 | <0.0001 |
| Hypertension | 2 | 844 (76.9) | 1288 (69.0) | 420 (57.0) | <0.0001 |
| Diabetes mellitus | 0 | 375 (34.2) | 425 (22.8) | 113 (15.3) | <0.0001 |
| Hypercholesterolemia | 4 | 610(55.7) | 1338(71.7) | 633(85.9) | <0.0001 |
| Hypertriglyceridemia | 2 | 236(21.5) | 483(25.9) | 235(31.9) | <0.0001 |
| Hypoalphalipoproteinemia | 2 | 160 (14.6) | 248 (13.3) | 80 (10.9) | 0.024 |
| Smoking habits | 72 | ||||
| Never smokers | 498 (45.4) | 878 (47.0) | 407 (55.2) | ||
| Former smokers | 398 (36.2) | 727 (38.9) | 246 (33.4) | <0.0001 | |
| Current smokers | 202 (18.4) | 263 (14.1) | 84 (11.4) | ||
| Pack-years | 72 | 20 (9.0, 33.2) | 17 (7.8, 28.1) | 16.3 (7.5, 30.0) | 0.03 |
| Family history of: | |||||
| Coronary artery disease | 3 | 738 (70.7) | 1170 (64.7) | 407 (57.8) | <0.0001 |
| Cerebrovascular disease | 3 | 374 (34.1) | 689 (36.9) | 259 (35.1) | 0.49 |
| Peripheral vascular disease | 3 | 118 (10.7) | 236 (12.6) | 89 (12.1) | 0.3 |
| Social class | 307 | ||||
| White collars | 322 (32.0) | 743 (42.9) | 314 (47.7) | ||
| Service workers | 374 (37.2) | 562 (32.4) | 202 (30.7) | <0.0001 | |
| Manual workers | 309 (30.7) | 428 (24.7) | 142 (21.6) | ||
| Study years | 10.0 ± 3.4 | 10.6 ± 4.1 | 10.5 ± 4.2 | 0.002 | |
| Biochemical variables | |||||
| Total cholesterol, mmol/L | 16 | 5.32 ± 1.11 | 5.47 ± 1.12 | 5.8 ± 1.12 | <0.0001 |
| HDL cholesterol, mmol/L | 16 | 1.23 ± 0.36 | 1.26 ± 0.36 | 1.32 ± 0.37 | <0.0001 |
| Triglycerides, mmol/L | 16 | 1.31 (0.94, 1.91) | 1.31 (0.94, 1.91) | 1.28 (0.9, 1.8) | 0.09 |
| LDL cholesterol, mmol/L | 81 | 3.39 ± 0.96 | 3.52 ± 1.02 | 3.83 ± 0.97 | <0.0001 |
| Uric acid, μmol/L | 16 | 320 (273, 369) | 310 (263, 357) | 298 (253, 352) | <0.0001 |
| hs-CRP, mg/L | 11 | 2.1 (0.9, 3.9) | 1.8 (0.8, 3.5) | 1.6 (0.6, 3.1) | <0.0001 |
| Blood glucose, mmol/L | 12 | 6.26 ± 1.82 | 5.9 ± 1.64 | 5.43 ± 1.15 | <0.0001 |
| Creatinine, μmol/L | 17 | 82 (71, 93) | 79 (69, 90) | 75 (65, 88) | <0.0001 |
| Food items | |||||
| Fish (portions/week) | 13 | 1.3 ± 0.8 | 1.8 ± 1.1 | 2.6 ± 1.4 | – |
| Wine (dl/day) | 9 | 0.6 ± 1.6 | 1.2 ± 2 | 1.5 ± 2 | – |
| Meat (portions/week) | 14 | 4.4 ± 1.6 | 3.6 ± 1.8 | 2.7 ± 1.6 | – |
| Fruits (portions/day) | 5 | 1.7 ± 0.9 | 2.2 ± 1.3 | 3.2 ± 1.7 | – |
| Milk (dl/day) | 12 | 3.9 ± 2.8 | 2.4 ± 2.3 | 1.6 ± 2.1 | – |
| Eggs (Number/week) | 14 | 2.2 ± 1.7 | 1.2 ± 1.1 | 0.8 ± 0.7 | – |
| Mostly used fat | |||||
| Olive oil | 5 | 109 (9.93) | 942 (50.43) | 663 (89.96) | – |
| Margarine | 5 | 595 (54.19) | 479 (25.64) | 34 (4.61) | – |
| Seed oil | 5 | 235 (21.40) | 299 (16.01) | 26 (3.53) | – |
| Other fat | 5 | 159 (14.48) | 148 (7.92) | 14 (1.90) | – |
Values are mean ± SD, or median (interquartile range) or n (%). p Values were calculated by linear regression or by chi square for trend.
Table 2.
Variables independently associated with MD score by multivariable linear regression with stepwise selection.
| Variables | Betaa | SE | p Value |
|---|---|---|---|
| Latitude (degrees) | −0.09 | 0.003 | <0.0001 |
| Education (study years) | 0.03 | 0.01 | <0.0001 |
| Physical activity (1 step) | 0.11 | 0.03 | 0.0003 |
| Use of antiplatelet agents | 0.19 | 0.06 | 0.0007 |
| Log hs-CRP (mg/L) | −0.14 | 0.04 | 0.0009 |
| HDL-cholesterol (mmol/L) | 0.20 | 0.06 | 0.002 |
| Body mass index (Kg/m2) | −0.02 | 0.01 | 0.002 |
| Statin treatment | 0.12 | 0.04 | 0.006 |
| Pack-years of cigarette smoking | −0.003 | 0.001 | 0.009 |
| Creatinine (μmol/L) | −0.003 | 0.001 | 0.02 |
| Pulse pressure (mmHg) | −0.004 | 0.002 | 0.02 |
| Insulin treatment | −0.25 | 0.11 | 0.03 |
| Occupation (white collars) | 0.10 | 0.05 | 0.03 |
Beta values indicate change in MD score associated with a unit increment of the predictor. Variables not significantly associated were: sex, age, blood glucose, triglycerides, uric acid, WBC count, family history of CHD, CVD and PVD and other pharmacological treatments (Beta blockers, calcium antagonists, ACE inhibitors, sartans, diuretics, insulin, estrogens, statin, fibrates and fish-oil).
3.2. MD score and vascular events
Among the 3703 subjects enrolled in the IMPROVE Study, 215 (7.96%) developed a first VE within the 36 months follow-up (see Table 1 in Ref [14]. Among these, 125 were cardio-VEs; 73 were cerebro-VEs and 17 were peripheral-VEs.
Fig. 1 of Ref [14] shows the Kaplan-Meier incidence curves of the combined endpoint, and of cardio- and cerebro-VEs, stratified by MD adherence score classes. Regardless of the endpoint considered, the rate of events was the highest in subjects with score 0–1; lower in those with score 2–3 and the lowest in those with score 4–7. The MD score remained significantly associated with the combined endpoint also after stratification by latitude and adjustment for potential confounders (Table 3, Model 2 and 3). Similar results were obtained when cardio- and cerebro-VEs were analyzed separately (Table 3).
Fig. 1.
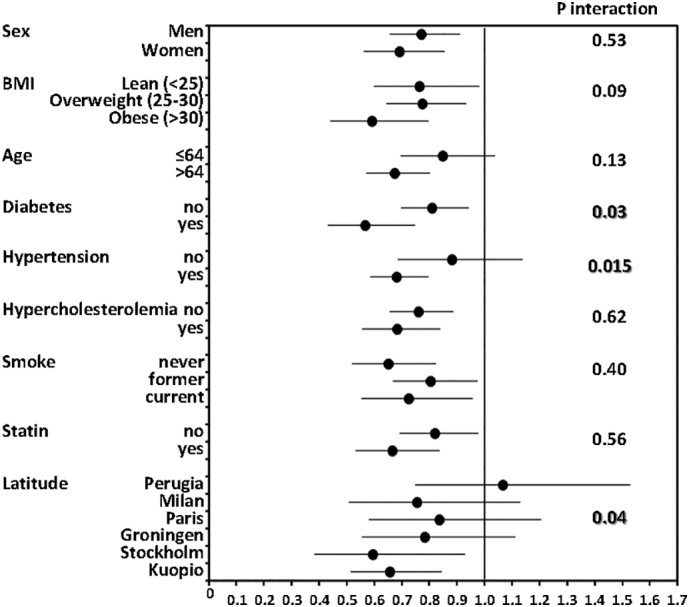
Hazard ratios for combined cardiovascular events associated with one point increase of MD score: subgroups analysis.
Horizontal lines represents 95%CI, adjusted for covariates in Model 3 (see Methods), excluding the respective stratification variables.
Table 3.
Association between MD score and vascular events: multivariable adjusted Cox models.
| MD-score | Combined events (n = 215) |
Cardiovascular events (n = 125) |
Cerebrovascular events (n = 73) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Events/subjects | HR (95% CI) | p-Value | Events/subjects | HR (95% CI) | p-Value | Events/subjects | HR (95% CI) | p-Value | ||
| Model 1 | 0–1 | 101/1098 | 1 | 58/1098 | 1 | 32/1098 | 1 | |||
| 2–3 | 94/1868 | 0.55 (0.41, 0.73) | <0.0001 | 56/1868 | 0.58 (0.40, 0.84) | 0.004 | 33/1868 | 0.59 (0.36, 0.96) | 0.03 | |
| 4–7 | 20/737 | 0.29 (0.18, 0.47) | <0.0001 | 11/737 | 0.28 (0.15, 0.53) | 0.0001 | 8/737 | 0.35 (0.16, 0.75) | 0.007 | |
| Trend | 0.74 (0.67, 0.82) | <0.0001 | 0.76 (0.66, 0.87) | <0.0001 | 0.72 (0.61, 0.87) | 0.0004 | ||||
| Model 2 | 0–1 | 101/1098 | 1 | 58/1098 | 1 | 32/1098 | 1 | |||
| 2–3 | 94/1868 | 0.62 (0.46, 0.84) | 0.0023 | 56/1868 | 0.65 (0.44, 0.97) | 0.04 | 33/1868 | 0.66 (0.39, 1.13) | 0.13 | |
| 4–7 | 20/737 | 0.36 (0.21, 0.62) | 0.0002 | 11/737 | 0.35 (0.17, 0.73) | 0.005 | 8/737 | 0.43 (0.18, 1.04) | 0.06 | |
| Trend | 0.79 (0.70, 0.89) | 0.0002 | 0.81 (0.69, 0.96) | 0.012 | 0.75 (0.61, 0.93) | 0.009 | ||||
| Model 3 | 0–1 | 101/1098 | 1 | 58/1098 | 1 | 32/1098 | 1 | |||
| 2–3 | 94/1868 | 0.53 (0.38, 0.74) | 0.0002 | 56/1868 | 0.51 (0.33, 0.80) | 0.003 | 33/1868 | 0.65 (0.37, 1.15) | 0.14 | |
| 4–7 | 20/737 | 0.31 (0.17, 0.56) | 0.0001 | 11/737 | 0.27 (0.12, 0.63) | 0.002 | 8/737 | 0.41 (0.16, 1.1) | 0.065 | |
| Trend | 0.75 (0.67, 0.87) | <0.0001 | 0.75 (0.62, 0.90) | 0.002 | 0.76 (0.61, 0.96) | 0.021 | ||||
Model 1: unadjusted; Model 2: adjusted for age, sex and stratified by latitude; Model 3: as model 2 plus smoking, body mass index, education, physical activity, occupation, LDL and HDL cholesterol, triglycerides, hs-CRP, creatinine, plasma glucose, pulse pressure, antiplatelet and statin treatments.
Subgroups analysis (Fig. 1) showed that the hazard ratios (HRs) associated with one-point increase of MD score were comparable in men and women, and tended to be lower in high-risk subjects (e.g. obese, diabetics etc.) as well as in north European countries. Of note, the MD effect was comparable and statistically significant regardless of the use of statins.
4. Discussion
The high impact of MD on VEs has been previously documented [7,8,15,16] and our data are in line with these findings. We show here, for the first time, that the association of MD with VEs is more apparent in the north than in the south of Europe and is stronger in some high-risk categories, independent of statin treatments.
To the best of our knowledge, most of the studies addressing the relation between MD scores and VEs were single nation studies (Greece [7], USA [17], Italy [13], north Sweden [18]) and only one [12] was carried out in European countries at different latitudes. Our study, which includes nations with a north to south distribution, shows that latitude is the strongest predictor of the MD score. Another important observation is that MD score is associated with a high social class, as indexed by education level, and that this association is stronger in northern than in southern countries. This latter finding is not easy to explain; one of the possible explanation is that the items of MD are easily available and relatively cheap in southern Europe, whereas they are available only to higher socio-economic classes in northern countries, due to their higher cost [9,19].
Multiple complex mechanism(s) are likely to be responsible for the protective effects of MD. Indeed, MD influences both atherosclerosis and thrombosis through an effect on low-grade inflammation. In addition, several authors have reported an association between inflammatory processes and the composition of gut microbiota [20] which, in turn, has been related to dietary habits, and specifically to MD [21]. Accordingly, hs-CRP, a widely accepted marker of low-grade inflammation, has been shown to be an important mediator of the effect of MD on VEs [22].
The results of the present study are relevant in terms of public health, and fit well with current guidelines and recommendations that strongly encourage people to consume a MD-like diet for primary and secondary prevention of major chronic diseases [23]. Unfortunately, a progressive shift toward non-MD patterns is developing even in countries bordering the Mediterranean Sea [24] and this emphasizes the need for continuing the search of dietary-based preventive programs to counteract this detrimental tendency.
An important point that needs to be stressed is that our dietary assessment was based on a relatively simple dietary questionnaire, if compared with other studies [7,25], an aspect that, theoretically, could have limited our ability to detect the relevant associations. Nevertheless, the strength and consistency of our data suggest that a MD pattern can be easily extrapolated using a limited number of food items, and that its association with VEs is so strong to be detectable even in the presence of a certain degree of misclassification.
Our study has several strengths: 1) it is based on a large cohort of 3703 participants followed for more than three years by specialized clinical centers; 2) it was conducted across five European countries, with a strong gradient in latitude and incidence of VEs.
The study has also some limitations: 1) being an observational study, a causal relation between MD and VEs cannot be demonstrated; 2) as the IMPROVE participants were selected for carrying at least three VRFs, the findings can only be extrapolated cautiously to the general European population or to patients with fewer than 3 VRFs; 3) diet was assessed only at the beginning of the study and dietary changes occurring later may have led to non-differential misclassification and underestimation of the true associations.
5. Conclusions
We found that a MD score based on a simple dietary questionnaire is able to detect changes of risk of VEs; as the protective effect of MD tend to become stronger with increasing latitude. According to our findings north Europeans appear to benefit most from VE-prevention when their diet is altered to the MD diet.
Author contributions
Elena Tremoli, Damiano Baldassarre, Fabrizio Veglia, Alessandro Di Minno, Steve E. Humphries, Rainer Rauramaa, Ulf de Faire, Andries J. Smit, Philippe Giral, Sudhir Kurl and Elmo Mannarino designed research; Mauro Amato, Beatrice Frigerio, Samuela Castelnuovo, Alessio Ravani, Daniela Sansaro and Daniela Coggi conducted research; Fabrizio Veglia and Calogero C. Tedesco performed statistical analysis; Fabrizio Veglia, Damiano Baldassarre wrote the paper; Anders Hamsten, Steve E. Humphries, Rainer Rauramaa, Ulf de Faire, Andries J. Smit, Philippe Giral, Sudhir Kurl and Elmo Mannarino performed a critical revision of the manuscript for important intellectual content; Damiano Baldassarre, Fabrizio Veglia and Elena Tremoli had primary responsibility for final content. All authors read and approved the final manuscript.
Acknowledgement of grant support
This study was supported by the European Commission (Contract number: QLG1- CT- 2002- 00896) (to Elena Tremoli, Damiano Baldassarre, Anders Hamsten, Steve E. Humphries, Rainer Rauramaa, Ulf de Faire, Andries J. Smit, Philippe Giral, Sudhir Kurl, Elmo Mannarino), Ministero della Salute Ricerca Corrente, Italy (to Damiano Baldassarre), the Swedish Heart-Lung Foundation, the Swedish Research Council - project 8691(to Anders Hamsten) and 0593, (to Ulf de Faire), the Swedish Foundation for Strategic Research, the Stockholm County Council - project 562183, (to Anders Hamsten) and the British Heart Foundation - RG2008/008, (to Steve E. Humphries). None of the aforementioned funding organizations or sponsors has had a specific role in design or conduct of the study, collection, management, analysis, or interpretation of the data, or preparation, review, or approval of the manuscript.
Role of the funding source
The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
Declaration of interest
None.
Acknowledgements
The authors wish to express their deep and sincere appreciation to all members of the IMPROVE group for their time and extraordinary commitment and Prof. S. Panico and Prof. G. Di Minno for their valuable suggestions.
Footnotes
Clinical trial registry number:
Contract number: QLG1- CT- 2002- 00896; http://cordis.europa.eu/project/rcn/68775_it.html.
Appendix A. The IMPROVE study group
-
•
Dipartimento di Scienze Farmacologiche e Biomolecolari, Università di Milano, Milan, Italy: E. Tremoli, Laura Calabresi, C.R. Sirtori.
-
•
Department of Medical Biotechnology and Translational Medicine, Università di Milano, Milan, Italy: D. Baldassarre.
-
•
Centro Dislipidemie E. Grossi Paoletti, Ospedale Ca' Granda di Niguarda. S. Castelnuovo.
-
•
Centro Cardiologico Monzino, IRCCS, Milan Italy: E. Tremoli, D. Baldassarre, M. Amato, B. Frigerio, A. Ravani, D. Sansaro, D. Coggi, F. Veglia, C. Tedesco, A. Bonomi.
-
•
Atherosclerosis Research Unit, Departments of Medicine and Cardiology, Karolinska University Hospital Solna, & Division of Cardiovascular Epidemiology, Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden: M. Ahl, G. Blomgren, M.J. Eriksson, P. Fahlstadius, M. Heinonen, L. Nilson.
-
•
University College of London, Department of Medicine, Rayne Institute, London, United Kingdom: J. Cooper, J. Acharya.
-
•
Foundation for Research in Health Exercise and Nutrition, Kuopio Research Institute of Exercise Medicine, Kuopio, Finland: K. Huttunen, E. Rauramaa, H Pekkarinen, I.M. Penttila, J. Törrönen.
-
•
Department of Medicine, University Medical Center Groningen, Groningen &Isala Clinics Zwolle, Department of Medicine; the Netherlands: A.I. van Gessel, A.M van Roon, G.C. Teune, W.D. Kuipers, M. Bruin, A. Nicolai, P. Haarsma-Jorritsma, D.J. Mulder, H.J.G. Bilo, G.H. Smeets,
-
•
Assistance Publique - Hôpitaux de Paris; Service Endocrinologie-Metabolisme, Groupe Hôpitalier Pitié-Salpetriere, Unités de Prévention Cardiovasculaire, Paris, France: J.L. Beaudeux, J.F. Kahn, V. Carreau, A. Kontush.
-
•
Institute of Public Health and Clinical Nutrition, University of Eastern Finland, Kuopio Campus: J. Karppi, T. Nurmi, K. Nyyssönen, R. Salonen, T.P. Tuomainen, J.Tuomainen, J. Kauhanen.
-
•
Internal Medicine, Angiology and Arteriosclerosis Diseases, Department of Clinical and Experimental Medicine, University of Perugia, Perugia, Italy: G. Vaudo, A. Alaeddin, D. Siepi, G. Lupattelli.
References
- 1.Panico S., Mattiello A., Panico C., Chiodini P. Mediterranean dietary pattern and chronic diseases. Cancer Treat. Res. 2014;159:69–81. doi: 10.1007/978-3-642-38007-5_5. [DOI] [PubMed] [Google Scholar]
- 2.Willett W.C. The Mediterranean diet: science and practice. Public Health Nutr. 2006;9:105–110. doi: 10.1079/phn2005931. [DOI] [PubMed] [Google Scholar]
- 3.Rohrmann S., Overvad K., Bueno-de-Mesquita H.B., Jakobsen M.U., Egeberg R., Tjonneland A. Meat consumption and mortality–results from the European prospective investigation into cancer and nutrition. BMC Med. 2013;11:63. doi: 10.1186/1741-7015-11-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bendinelli B., Masala G., Saieva C., Salvini S., Calonico C., Sacerdote C. Fruit, vegetables, and olive oil and risk of coronary heart disease in Italian women: the EPICOR study. Am. J. Clin. Nutr. 2011;93:275–283. doi: 10.3945/ajcn.110.000521. [DOI] [PubMed] [Google Scholar]
- 5.Del Rio D., Agnoli C., Pellegrini N., Krogh V., Brighenti F., Mazzeo T. Total antioxidant capacity of the diet is associated with lower risk of ischemic stroke in a large Italian cohort. J. Nutr. 2011;141:118–123. doi: 10.3945/jn.110.125120. [DOI] [PubMed] [Google Scholar]
- 6.Keys A. Harvard University Press; Cambridge, MA: 1980. Seven Countries: A Multivariate Analysis of Death and Coronary Heart Disease. [Google Scholar]
- 7.Trichopoulou A., Costacou T., Bamia C., Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003;348:2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 8.Sofi F., Macchi C., Abbate R., Gensini G.F., Casini A. Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014;17:2769–2782. doi: 10.1017/S1368980013003169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baldassarre D., Nyyssonen K., Rauramaa R., de Faire U., Hamsten A., Smit A.J. Cross-sectional analysis of baseline data to identify the major determinants of carotid intima-media thickness in a European population: the IMPROVE study. Eur. Heart J. 2010;31:614–622. doi: 10.1093/eurheartj/ehp496. [DOI] [PubMed] [Google Scholar]
- 10.Baldassarre D., Hamsten A., Veglia F., de Faire U., Humphries S.E., Smit A.J. Measurements of carotid intima-media thickness and of interadventitia common carotid diameter improve prediction of cardiovascular events: results of the IMPROVE (carotid intima media thickness [IMT] and IMT-progression as predictors of vascular events in a high risk European population) study. J. Am. Coll. Cardiol. 2012;60:1489–1499. doi: 10.1016/j.jacc.2012.06.034. [DOI] [PubMed] [Google Scholar]
- 11.Baldassarre D., Veglia F., Hamsten A., Humphries S.E., Rauramaa R., de Faire U. Progression of carotid intima-media thickness as predictor of vascular events: results from the IMPROVE study. Arterioscler. Thromb. Vasc. Biol. 2013;33:2273–2279. doi: 10.1161/ATVBAHA.113.301844. [DOI] [PubMed] [Google Scholar]
- 12.Knoops K.T., de Groot L.C., Kromhout D., Perrin A.E., Moreiras-Varela O., Menotti A. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292:1433–1439. doi: 10.1001/jama.292.12.1433. [DOI] [PubMed] [Google Scholar]
- 13.Agnoli C., Krogh V., Grioni S., Sieri S., Palli D., Masala G. A priori-defined dietary patterns are associated with reduced risk of stroke in a large Italian cohort. J. Nutr. 2011;141:1552–1558. doi: 10.3945/jn.111.140061. [DOI] [PubMed] [Google Scholar]
- 14.Veglia F., Baldassarre D., de Faire U., Kurl S., Smit A.J., Rauramaa R. 2018. Incidence of Combined, Cardio and Cerebro Vascular Events According to a Priori-defined Mediterranean Diet Score. Data in Brief. (submitted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Lorgeril M., Renaud S., Mamelle N., Salen P., Martin J.L., Monjaud I. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343:1454–1459. doi: 10.1016/s0140-6736(94)92580-1. [DOI] [PubMed] [Google Scholar]
- 16.Estruch R., Ros E., Salas-Salvado J., Covas M.I., Corella D., Aros F. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013;368:1279–1290. doi: 10.1056/NEJMoa1200303. [DOI] [PubMed] [Google Scholar]
- 17.Mitrou P.N., Kipnis V., Thiebaut A.C., Reedy J., Subar A.F., Wirfalt E. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP diet and health study. Arch. Intern. Med. 2007;167:2461–2468. doi: 10.1001/archinte.167.22.2461. [DOI] [PubMed] [Google Scholar]
- 18.Tognon G., Nilsson L.M., Lissner L., Johansson I., Hallmans G., Lindahl B. The Mediterranean diet score and mortality are inversely associated in adults living in the subarctic region. J. Nutr. 2012;142:1547–1553. doi: 10.3945/jn.112.160499. [DOI] [PubMed] [Google Scholar]
- 19.Trichopoulou A., Naska A., Costacou T. Disparities in food habits across Europe. Proc. Nutr. Soc. 2002;61:553–558. doi: 10.1079/pns2002188. [DOI] [PubMed] [Google Scholar]
- 20.Bifulco M. Mediterranean diet: the missing link between gut microbiota and inflammatory diseases. Eur. J. Clin. Nutr. 2015;69:1078. doi: 10.1038/ejcn.2015.81. PMID: 26014263. [DOI] [PubMed] [Google Scholar]
- 21.David L.A., Maurice C.F., Carmody R.N., Gootenberg D.B., Button J.E., Wolfe B.E. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Panagiotakos D.B., Georgousopoulou E.N., Pitsavos C., Chrysohoou C., Skoumas I., Pitaraki E. Exploring the path of Mediterranean diet on 10-year incidence of cardiovascular disease: The ATTICA study (2002–2012) Nutr Metab Cardiovasc Dis. 2015;25:327–335. doi: 10.1016/j.numecd.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Lichtenstein A.H., Appel L.J., Brands M., Carnethon M., Daniels S., Franch H.A. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 24.Sofi F., Vecchio S., Giuliani G., Martinelli F., Marcucci R., Gori A.M. Dietary habits, lifestyle and cardiovascular risk factors in a clinically healthy Italian population: the 'Florence' diet is not Mediterranean. Eur. J. Clin. Nutr. 2005;59:584–591. doi: 10.1038/sj.ejcn.1602112. [DOI] [PubMed] [Google Scholar]
- 25.Gardener H., Wright C.B., Cabral D., Scarmeas N., Gu Y., Cheung K. Mediterranean diet and carotid atherosclerosis in the Northern Manhattan Study. Atherosclerosis. 2014;234:303–310. doi: 10.1016/j.atherosclerosis.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


