Short abstract
Obstetric medicine as a speciality is yet to be developed in South Africa. South Africa is regarded as a developing country. The burden of HIV and metabolic syndrome creates a need for advanced maternal care. An increase has been noted in hypertension and gestational diabetes due to increasing maternal age and increasing prevalence of obesity. The South African National Committee on Confidential Enquiry into Maternal Deaths’ 2015 Saving Mothers Report identified non-pregnancy-related infections as the leading cause of maternal deaths. Obstetric medicine care includes pre-conception, antepartum and postpartum care. This article aims to highlight the importance of obstetric medicine, even in a resource-poor setting. The current internal medicine and obstetrics and gynaecology training is discussed and emphasis is placed on the opportunity to create an obstetric medicine programme.
Keywords: General medicine, high-risk pregnancy, maternal–fetal medicine
Introduction
Obstetric medicine is the management and care of medically complicated pregnancies during the pre-, intra- or postpartum period. These complications can be caused by pre-existing medical conditions or conditions presenting during pregnancy for the first time. Obstetric medicine is a relatively well-established sub-specialty in a number of developed countries such as Australia or the United Kingdom. South Africa currently has no structured obstetric medicine training programme.
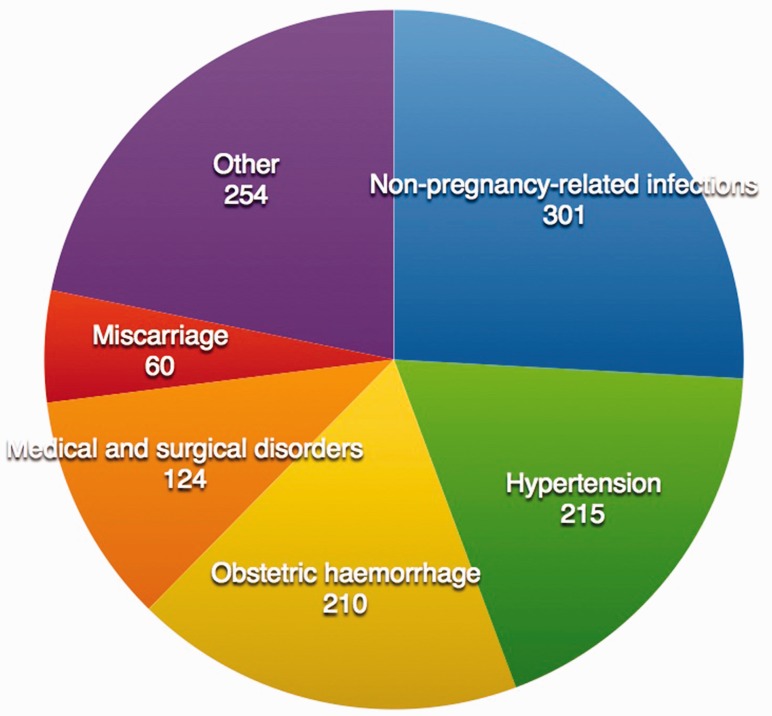
The South African National Committee on Confidential Enquiry into Maternal Deaths’ 2015 Saving Mothers Report identified non-pregnancy-related infections, complications of hypertension during pregnancy and obstetric haemorrhage as the three leading causes of maternal deaths1 as shown in Figure 1. Cardiac disease is the most common medical condition, and cardiomyopathy is the leading cardiac disease.
Figure 1.
Underlying causes of maternal deaths 2015 (adapted from Saving Mothers report1).
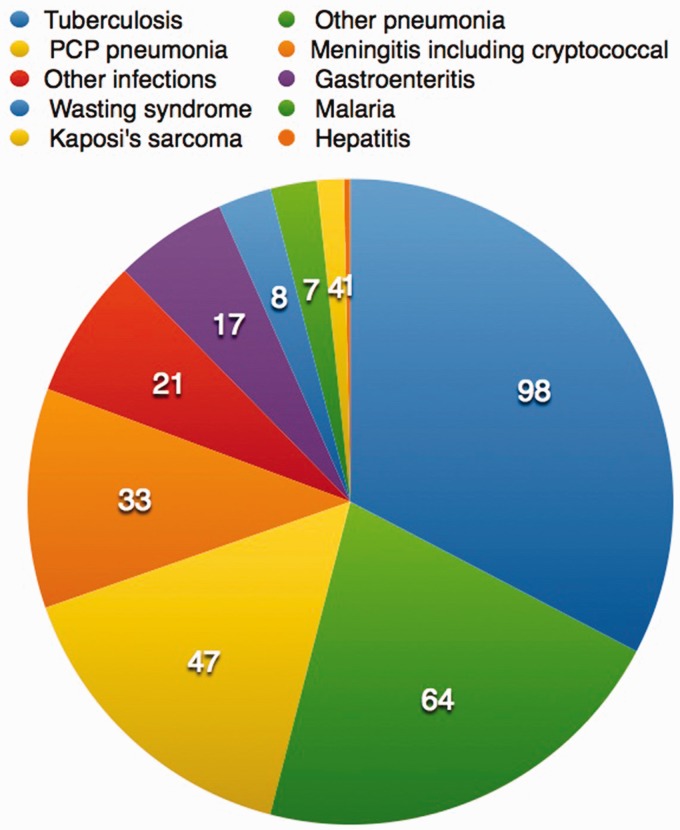
The 2015 Saving Mothers report found that 24% of maternal deaths were due to non-pregnancy-related infections, of which tuberculosis, pneumonia and Pneumocystis jirovecii (as complications of HIV) were the most common infections as shown in Figure 2. Ninety-one per cent of these patients were HIV positive.
Figure 2.
Non-pregnancy-related infections leading to Maternal Deaths in 2015 (adapted from Saving Mothers report1).
An estimated 6.19 million people in South Africa were living with HIV in 2015. The most recent publicly known estimate of HIV in antenatal women was a national prevalence 29.7% in 2013. HIV is seen as a multi-systemic disease affecting most organ systems, which could potentially lead to end organ damage in the form of nephropathies, cardiomyopathies, neuropathies and bone marrow suppression. These women are also more exposed to opportunistic infections such as, but not limited to, tuberculosis, P. jirovecii, cryptococcus, viral hepatitis and cytomegalovirus. HIV has an increased association with malignancies such as non-Hodgkin’s lymphoma, carcinoma of the cervix and Kaposi sarcoma. The drugs used in the treatment of HIV are known to have numerous side effects. Nine pregnant women died in South Africa in 2015 due to side effects of antiretroviral drugs (ARVs).1 These conditions and complications require early diagnosis and treatment.
The Saving Mothers report found that complications of hypertension in pregnancy were responsible for 19.5% of deaths. Other medical-related subcategories included medical and surgical causes (13%); puerperal sepsis (5.2%); adverse drug reactions (1.7%), mostly due to antiretroviral therapy and pulmonary embolism (2.7%). According to the South African Demographic and Health Survey (SADHS), almost half of women in South Africa (46%) are hypertensive.2
The prevalence of gestational diabetes is currently not reported in South Africa. However, the increase of westernised lifestyles predicts a rapid increase in complications and deaths associated with this disease, during and beyond pregnancy. The SADHS reports that 40–50% of women are obese. The International Diabetes Foundation estimates that 16.2% of all pregnancies resulting in live births are affected by some form of hyperglycaemia during pregnancy. Of these pregnancies, an estimated 85.1% are due to gestational diabetes with the remaining 15% split equally between other types of diabetes detected during pregnancy, or prior to pregnancy.3
The abovementioned data reflect the need for the input from specialist physicians in the care of complex obstetric patients with underlying medical problems. The majority of women only require primary healthcare from midwives or obstetricians during their pregnancy. Even though diabetes, HIV, hypertension and obesity are primarily managed by primary healthcare facilities, medical conditions in pregnancy contribute to more than 50% of morbidity and mortality during pregnancy and the puerperium.4 This demonstrates room for obstetric physicians or physicians with a special interest in obstetrics to manage the complicated cases of these diseases.
Maternal care in South Africa
The South African medical system is divided into private and public medical care. There are approximately 1.2 million births in SA of which more than 80% take place in the public sector. Ninety-four per cent of women attend antenatal care and 96% deliver in healthcare facilities.5 Government-subsidised medical care is currently available to all South Africans. Private institutions are mostly attended by those with private healthcare insurance as they offer personalised care, often with a greater range of diagnostic and therapeutic options. The majority of patients without private healthcare insurance attend the government model of healthcare. This model of healthcare is free but is associated with long waiting periods and limited resources. In the 2011 General Household survey conducted by Statistics South Africa,6 it was found that 16% of the South African population was covered by a private healthcare insurance.
South Africa aims to implement a national healthcare insurance act. Once the national health insurance act is implemented, the care structure is expected to change. All residents will have a right to access comprehensive healthcare services free of charge,7 thereby amalgamating private and public healthcare. These services will be delivered closest to where the patient lives or works. Funding for the national health insurance act will primarily come from general taxes.
The majority of public sector obstetric medical care in South Africa is provided by midwives at primary care facilities.8 Of all births, 60% take place at primary level Community Health Centres and District Hospitals, 25% at regional hospitals and 15% at tertiary hospitals. Complicated or predicted high-risk patients are referred to secondary or tertiary hospitals for specialised care by trained obstetricians. Secondary hospitals have specialist obstetricians but also medical officers with an interest in obstetric care. Academic hospitals have a Maternal and Fetal Medicine Unit (MAFU), staffed by MAFU sub-specialists and those still in a training position. MAFU sub-specialists have received additional training in procedural and ultrasonographic diagnostic skills, management of high-risk pregnancies and obstetric critical care.
The majority of private sector obstetric care is provided by obstetricians or general practitioners with an interest in obstetrics. Rising medical insurance costs and an increase in litigation are resulting in fewer doctors choosing to care for pregnant women in the private sector. Many obstetrician–gynaecologists are opting to only practise as gynaecologists.
Internal medicine offers consultative services to the maternity wards or clinics through general physicians or sub-specialists. Patients are primarily managed by the obstetric team with the physicians acting as a support service. Complicated pregnancies are mostly managed primarily by the obstetric team, even though some complications are not directly due to the pregnancy.
General medicine training
All medical graduates complete two years of internship at a Health Professions Council of South Africa (HPCSA) accredited secondary or tertiary hospital. They work under the supervision of qualified and training specialists, where they rotate in two to four-month blocks through all major specialities of clinical medicine. Once full registration is obtained from the HPCSA, all medical practitioners complete a year of community service, mostly at district hospitals and smaller or rural healthcare facilities. Practitioners may often choose to spend six months in a department of their interest; this may include internal medicine or obstetrics and gynaecology.
Internal medicine and obstetric medicine training
There are a number of internal medicine specialists (hereafter called physicians) with an interest in the care of obstetric patients. The authors are not aware of any formally trained, practising obstetric physicians. The physicians with an interest in obstetric medicine have broadened their knowledge by extensive reading, attending short courses and conferences in the field of obstetric medicine. Internal medicine registrars are trained in the care of obstetric patients by general physicians, and sub-specialists including cardiologists, nephrologists, rheumatologists and endocrinologists.
The College of Medicine of South Africa has recently introduced expected outcomes on medical problems in pregnancy for graduates as a separate section in the final exam to register as a fellow of the College of Physicians.9
Obstetric and gynaecology and maternal medicine training
Every medical student is trained in Essential Steps in the Management of Obstetric Emergencies (ESMOE). ESMOE is taught to all interns by an accredited trainer and this must be signed off prior to registration as a medical practitioner. All obstetrics and gynaecology, and paediatrics registrars are trained in ESMOE. Topics covered include amongst other obstetric and fetal emergencies: maternal and neonatal resuscitation, eclampsia and pre-eclampsia, management of sepsis, postpartum haemorrhage, cord prolapse, shoulder dystocia and management of HIV in pregnancy.10
Doctors who choose to specialise in obstetrics and gynaecology may work as a medical officer in their department of interest or as private general practitioners while waiting for a registrar post in obstetrics and gynaecology.
Once accepted to a registrar training programme the doctors write a part one exam for the college of medicine South Africa within their first year of training and a part two, or exit exam after at least 36 months in a registrar post. A registrar has to spend 48 months in a training position before registering with the HPCSA as a specialist obstetrician and gynaecologist.
During their four-year training programme, registrars are exposed to maternal and fetal medicine where they are trained to manage obstetric emergencies such as hypertensive disorders in pregnancy. Registrars are often exposed to medical emergencies in obstetric patients such as diabetic keto acidosis. Medical complications mostly lead to co-management between internal medicine and the obstetric department.
The certificate in maternal and fetal medicine is an 18 to 36-month training programme focusing on maternal and fetal health. The maternal medicine half of the programme focuses on: medical complications in pregnancy; surgical complications of pregnancy; infectious diseases; complicated obstetrics; operative procedures and the intra-partum management of high-risk pregnancies. The fetal medicine half of the programme focuses on: structural fetal anomalies; teratogens including infections, smoking, alcohol; genetic conditions including aneuploidy, rearrangements, single gene, multifactorial; multifetal pregnancies; functional fetal impairment; ultrasound and invasive procedures.11
Interdepartmental care
Good co-operation between maternal–fetal specialists and physician sub-specialists has been established in the different units across the country. This provides a high standard of care for the pregnant patient with established disease. In units such as Groote Schuur, Tygerberg, Steve Biko and Charlotte Maxeke hospitals, interdepartmental clinics and/or ward rounds with departments such as cardiology and/or endocrinology have been established. Some of these units also have joined clinics between obstetrics and anaesthesiology.
None of the centres providing tertiary care to the obstetric population have dedicated physicians committed to the care of acute or chronic medical conditions in pregnancy. Maternal–fetal specialists run high-risk medical conditions clinics and regularly consult medical sub-specialities such as nephrology, rheumatology, haematology.
There is limited to no access to pre-pregnancy counselling clinics for patients with known chronic diseases such as chronic renal failure, autoimmune disease or congenital heart disease.
When obstetric patients are admitted to the tertiary unit for care of a medical condition, general physicians are consulted to assist in the diagnosis and management of the acute complication. Pregnant patients have markedly different physiology to non-pregnant patients. Not all physicians have an interest or experience in treating obstetric patients. This creates a need for obstetric physicians.
Interdepartmental meetings aimed at discussing complicated cases between internal medicine and obstetrics are at most on an ad hoc basis.
Job opportunities
First-world countries estimate for one obstetric physician to remain employed in a full-time position one has to practise at a centre that has between 5000 and 10,000 deliveries per annum.12–14 With the high incidence of HIV, obesity and metabolic syndrome in South Africa, the authors expect this number to be lower.
An estimated 29.7% of antenatal woman are infected with HIV.1 HIV is seen as a multi-system disease with a potential for developing multi-organ involvement. Complications of the disease as well as the treatment often require specialist consultation. Physicians in South Africa are well trained in the diagnosis and management of these conditions.
A recent review of trends in obesity and diabetes across Africa from 1980 to 2014 showed that the prevalence of obesity amongst women in Africa increased from 4.1% to 8.9% over two decades. Similarly, diabetes has a higher prevalence in Southern African women in comparison with the rest of the world.15 Obesity and diabetes are known as independent risk factors for complicated pregnancies.
In a resource-limited setting such as South Africa, it is vital that patients attend antenatal follow-up at the appropriate level of care. The majority of HIV and metabolic syndrome can be managed at a primary or secondary healthcare level. Potential complications should be identified early and referred to specialist care. If complicated patients are screened and referred appropriately, the authors expect an increased demand for physicians with an interest in obstetric patients.
Maternal medicine specialists are trained in the management of medical complications in pregnancy. Physicians are trained to have a broad knowledge of diagnosis and management of chronic medical conditions and their acute exacerbations. Maternal medicine specialists and obstetric physicians have overlapping skills that can complement each other in the care of pregnant women. This includes the management of medical conditions due to pregnancy as well as chronic medical conditions in pregnancy.
The future in South Africa
South Africa has a significantly higher rate of maternal morbidity and mortality when compared to high-income countries. In 2015, there were 138 maternal deaths per 100,000 live births, in comparison to the 9 maternal deaths per 100,000 in the United Kingdom in the same year.16
Possible explanations include:
A high burden of disease, including HIV, hypertension, diabetes and obesity.
Access to pre-pregnancy counselling is limited or non-existent for the majority of women with medical conditions
General practitioners and midwives care for women with complicated pregnancies when referral systems fail.
Private gynaecologists are withdrawing obstetric care due to the fear of increasing litigation and increasing medical malpractice insurance costs.
Maternal–fetal sub-specialists are lacking in numbers.
Sub-specialists in obstetric medicine are non-existent, with limited availability of physicians with a specialist interest in pregnancy.
Obstetric physicians can play a vital part in the management of complicated pregnancies. South Africa has most of the infrastructure ready for developing an obstetric medicine programme and sub-speciality. With an increased focus on maternal health, babies and children will be nurtured into stronger, healthier adults. The HPCSA and College of Medicine do not yet recognise obstetric medicine as a sub-speciality.
Proposed solutions include:
Obstetric physician input to work closely with Maternal and fetal medicine sub-specialists in the tertiary academic centres where their skills can be complemented with each other. The highest risk women are triage effectively into these tertiary academic centres.
Recruitment into obstetric medicine or driving interest in pregnancy amongst internal medicine trainees by rotation in obstetrics.
Ensuring adequate coverage of maternal medicine problems in the general obstetric and gynaecology syllabus. This will include joined lectures between the obstetric and internal medicine departments.
Supporting continued professional development in primary care amongst general practitioners and midwives as the system is very much dependent on identification of high-risk women to be referred into secondary and tertiary level care.
In summary, medically complicated pregnancies may be challenging and difficult to manage. South Africa has a great need for physicians with an interest in obstetric care partly but not completely due to our high prevalence of HIV/AIDS, obesity, diabetes and hypertensive disease.
Maternal deaths have seen a steady decline since 2009, as care of obstetric complications has been identified and boldly improved. Medical complications now account for an even greater part of maternal morbidity and mortality. In a resource-limited country, maternal care requires healthcare professionals who are passionate about their goals and driven to improve the multitude of disease seen in our developing country.
Acknowledgements
The authors would like to thank Prof. RC Pattinson and Prof. JA Ker for their inspiration, review and encouragement in the writing of this article.
Declaration of conflicting interests
The author(s) declared no potential conflict of interest with respect to the research, authorship and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
Ethical approval
None required.
Guarantor
LW.
Contributorship
All authors contributed equally.
References
- 1.National Committee on Confidential Enquiry into Maternal Deaths. Saving Mothers, sixth (2011–2013) and seventh (2014-2015) report of the National Committee for Confidential Enquiry into Maternal Deaths in South Africa. Pretoria: DOH.
- 2.National Department of Health. Demographic and health survey 2016 Key indicators report Pretoria, South Africa: Statistics South Africa, 2017. pp.45–48.
- 3.International Diabetes Federation – Gestational diabetes, www.idf.org/our-activities/care-prevention/gdm?language=ru (accessed 30 May 2017).
- 4.Acquah L, Burton R. Obstetric medicine. Interlinking obstetrics and internal medicine. SAMJ 2014; 104: 9. [DOI] [PubMed] [Google Scholar]
- 5.National Department of Health. Demographic and health survey 2016 key indicators report Pretoria: Statistics South Africa, 2017, p.19.
- 6.Statistics South Africa. Use of health facilities and levels of selected health conditions in South Africa: findings from the general household survey. Pretoria: Statistics South Africa, 2011. [Google Scholar]
- 7.Department of Health, Republic of South Africa. National health insurance for South Africa towards universal health coverage. Pretoria: Government Gazette, 2015, pp.9–10. [Google Scholar]
- 8.Department of Health. Guidelines for maternity care in South Africa. A manual for clinics, community health centres and district hospitals. 4th ed Pretoria: National department of Health, 2015, p.19. [Google Scholar]
- 9.The Colleges of Medicine of South Africa. Fellowship of the College of Physicians of South A. 2018. Available at: https://www.cmsa.co.za/view_exam.aspx?QualificationID=28
- 10.Frank K, Lombard H, Pattinson R. Does completion of the essential steps in managing obstetric emergencies (ESMOE) training package result in improved knowledge and skills in managing obstetric emergencies? SAJOG 2009; 15: 94–99. [Google Scholar]
- 11.The Colleges of Medicine of South Africa. Sub-specialty certificate in maternal and fetal medicine of the College of Obstetricians and Gynaecologists of South Africa: Cert Maternal and Fetal Medicine (SA). 2018. Available at: https://www.cmsa.co.za/view_exam.aspx?QualificationID=90
- 12.Magee L, Cote A, Joseph G, et al. Obstetric medical care in Canada. Obstet Med 2016; 9: 117–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carson M, Chen K, Miller M. Obstetric medical care in the United States of America. Obstet Med 2017; 10: 36–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jakes A, Watt-Coote I, Coleman M, et al. Obstetric medical care and training in the United Kingdom. Obstet Med 2017; 10: 40–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kengwe A, Bentham J, Zhou B, et al. Trends in obesity and diabetes across Africa from 1980 to 2014: an analysis of pooled population-based studies. Int J Epidemiol 2017; 46: 1421–1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maternal mortality ratio (modeled estimate, per 100,000 live births) | Data, https://data.worldbank.org/indicator/SH.STA.MMRT (2015, accessed 8 March 2018).