Abstract
Background:
The authors sought to assess the safety and early efficacy of the pCONUS Bifurcation Aneurysm Implants in a meaningful number of patients; we performed a systematic review and meta-analysis for the treatment of 203 intracranial aneurysms.
Methods:
A literature search was performed by a reference librarian, and after screening nine case series were included in this analysis. We estimated from each study the cumulative incidence (event rate) and 95% confidence interval (CI) for each outcome. Event rates were pooled in a meta-analysis across studies using the random-effects model; descriptive statistics were reported when relevant.
Results:
The pCONUS devices can be used with a technical success rate of 100% (95% CI: 0.98–1.00) and a technical complication rate of 0% (95% CI: 0.00–0.02). Perioperative morbidity and mortality rates were 7% (95% CI: 0.03–0.11) and 0% (95% CI: 0.00–0.01), respectively. Perioperative hemorrhage rate was 0% (95% CI: 0.00–0.02); rate of treatment-related long-term neurological deficit was 2% (95% CI: 0.00–0.06). The long-term complete occlusion rate was 60% (95% CI: 0.52–0.69) and retreatment rate was 14% (95% CI: 0.06–0.22).
Conclusions:
The pCONUS devices are an additional tool for the treatment of wide-necked intracranial aneurysms with high rates of technical success and sufficiently low rates of morbidity and mortality. Comparative studies with longer-term follow-up are needed to clarify the role of this device in the management of challenging aneurysms.
Keywords: Aneurysm, coiling, endovascular, pCONUS, stent, wide neck
INTRODUCTION
While coil embolization is a safe and established treatment option for intracranial aneurysms, broad-based, bifurcation aneurysms continue to represent a treatment challenge despite innovations in balloon-assistance and stent technology. To improve treatment results in these challenging situations, novel devices have been engineered to sit at the neck of the aneurysm, brace against the parent vessel wall, and prevent coil herniation. Among these devices are the pCONUS1 and pCONUS2 Bifurcation Aneurysm Implants (Phenox, Bochum, Germany) [Figure 1]. The pCONUS2 device is similar to the original device with the addition of two pedals for improved coverage of the aneurysm neck and a shorter shaft to decrease metal in the parent vessel. Since 2014, these devices have been utilized and individual centers have limited experiences. Therefore, in an attempt to assess the safety and early efficacy of this device in a meaningful number of patients, we collected the literature and performed a systematic review and meta-analysis for the treatment of 203 intracranial aneurysms with the pCONUS devices.
Figure 1.
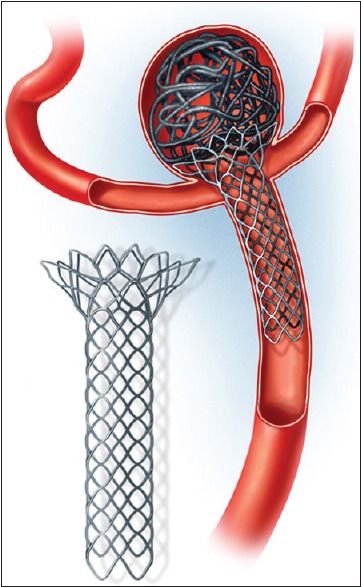
Artist rendering of the pCONUS bifurcation aneurysm implant (original)
SUBJECTS AND METHODS
This systematic review is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement (PRISMA, 2009).[11]
Literature search, study selection, and eligibility criteria
A medical reference librarian was asked to execute a comprehensive literature search of the PubMed, MEDLINE, EMBASE, Web of Science, and Scopus for case series published in English from January 1, 2000 until June 13, 2018. Searched terms were: pCONUS, pCONUS2 (its newer prototype), and aneurysm.
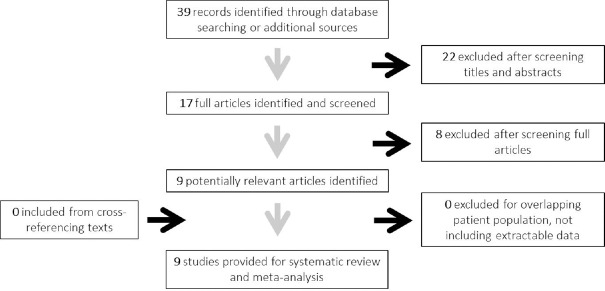
First, titles and abstracts were screened, and non-relevant and redundant articles were excluded. Full texts of the remaining studies were obtained and reviewed by two investigators (Thomas J. Sorenson and Marta Iacobucci) and only manuscripts that specifically reported data regarding the treatment of intracranial aneurysms with the pCONUS devices were included in this meta-analysis. Exclusion criteria for the full-text screen included: no relevance, not written in English, conference abstract, case reports, case series reporting fewer than five aneurysms treated, review articles, commentary or errata, withdrawn articles, and book chapters. A summary of the search strategy is presented in Figure 2.
Figure 2.
Summary of the literature screening strategy (original)
Once the final list of articles meeting inclusion criteria was compiled, the data were abstracted from each study, including but not limited to: age of patients; number, size, morphology, and status (ruptured versus unruptured) of aneurysms; treatment details (number of devices used, technical success, complications, related morbidity/mortality); incidence of perioperative complications, morbidity, and mortality; time to last follow-up; radiological status of aneurysm at last follow-up; clinical status at last follow-up. Data were abstracted by two separate authors (Thomas J. Sorenson and Marta Iacobucci) and compared. A summary of the included studies is presented in Table 1.[1,3,4,5,7,9,10,12,13]
Table 1.
Summary of included studies
| Author, Year | Study type | Patient cohort | Device | Risk of Bias |
|---|---|---|---|---|
| Aguilar Perez, 2014[2] | Retrospective | 28 | pCONUS | High |
| Gory, 2015[3]; Gory, 2017[4] | Retrospective | 40 | pCONUS | Medium |
| Fischer, 2016[9] | Retrospective | 25 | pCONUS | High |
| Lubicz, 2016[10] | Retrospective | 18 | pCONUS | High |
| Aguilar Perez, 2017[7] | Retrospective | 21 | pCONUS | Medium |
| Labeyrie, 2017[5] | Retrospective | 36 | pCONUS | Medium |
| Lylyk, 2018[6] | Retrospective | 12 | pCONUS2 | Medium |
| Ulfert, 2018[8] | Retrospective | 21 | pCONUS | Low |
Evaluation of methodological quality
A modified STROBE checklist was utilized to assess the quality of reporting in the included retrospective case series since there were no randomized controlled trials available.[14] All case series were assessed by two reviewers. Scores were ranked, and scores < 20 (out of 25) were designated as paper of having a high risk of bias [Supplemental Table 1]. If scores for an article were not in agreement, further discussion was pursued until agreement was reached.
Supplemental Table 1.
Modified strobe scores for each observational case series
| Included study | Scores | Total (/25) | |||
|---|---|---|---|---|---|
| Introduction (/2) | Methods (/12) | Results (/8) | Discussion (/3) | ||
| Author, year | |||||
| Aguilar Perez, 2014 | 2 | 11 | 7 | 3 | 23 |
| Gory, 2015; Gory, 2017 | 2 | 12 | 7 | 3 | 24 |
| Fischer, 2016 | 2 | 11 | 6 | 3 | 22 |
| Lubicz, 2016 | 2 | 10 | 7 | 3 | 22 |
| Aguilar Perez, 2017 | 2 | 11 | 8 | 3 | 24 |
| Labeyrie, 2017 | 2 | 12 | 7 | 3 | 24 |
| Lylyk, 2018 | 2 | 11 | 6 | 3 | 22 |
| Ulfert, 2018 | 2 | 12 | 6 | 3 | 23 |
Statistical analysis
All included studies were non-comparative. We estimated from each study the cumulative incidence (event rate) and 95% confidence interval (CI) for each outcome. Event rates were pooled in a meta-analysis using the random-effects model after stabilizing the variance using the Freeman-Tukey double arcsine method. We chose the random effects model a priori because it incorporates within-study variance and between-study variance.[2] Descriptive statistics (mean and range; and proportions) were reported when relevant. We quantified between-study heterogeneity using the I-squared statistic and Q test. We were not able to test for publication bias due to non-comparative nature of included studies.
RESULTS: SEARCH RESULTS
Initial library search yielded 39 articles. After screening of titles and abstracts, 17 articles were considered for full-text analysis. Of these studies, eight met exclusion criteria (conference abstracts: 5; duplication: 1; fewer than 5 aneurysms: 2), leaving nine case series that reported greater than five patients with an intracranial aneurysm treated with the pCONUS or pCONUS2 device [Figure 1]. A total of 201 patients with 203 aneurysms that were treated with the pCONUS or pCONUS2 device were reported in the literature. Of the nine included studies, eight reported results of the pCONUS device and one reported results with the newer prototype, pCONUS2 [Table 1].
Demographics
Of these 203 aneurysms, 22 (22/203; 11%) were previously treated with simple coiling and 51 (51/203; 25%) had previously ruptured. Of the 201 patients, 122 (122/201; 61%) were female. The mean age [± standard deviation (SD)] of included patients was 58.2 (±3.3) years. The mean (±SD) neck size was 5.97 (±0.63) mm, and mean (±SD) dome-to-neck ratio of the included aneurysms was 1.45 (±0.16). The most common location of treatment with the device was the middle cerebral artery (MCA) (90/203; 44%). The mean (±SD) length of clinical follow-up was 8.5 (±4.5) months, and the mean (±SD) length of imaging follow-up was 9.9 (±3.8) months. Six studies used only digital subtraction angiography (DSA) for imaging follow-up, while the remaining three used a combination of DSA and magnetic resonance angiography (MRA). Full demographic information is available in Table 2.
Table 2.
Summary of demographic information
| Values | |
|---|---|
| Patients | 201 |
| Average age (SD) (years) | 58.2 (3.31) |
| Female:male | 1.54:1 |
| Aneurysms | 203 |
| Average dome size (SD) (mm) | 8.2 (0.97) |
| Average neck size (SD) (mm) | 5.97 (0.63) |
| Average dome: neck ratio | 1.45:1 |
| Location | |
| Anterior cerebral artery (ACA) | 2 (1%) |
| Anterior communicating artery (ACOM) | 69 (34%) |
| Middle cerebral artery (MCA) | 90 (45%) |
| Internal carotid artery (ICA) bifurcation | 6 (3%) |
| Posterior communicating artery (PCOM) | 1 (0.5%) |
| Posterior cerebral artery (PCA) | 2 (1%) |
| Basilar apex | 31 (15%) |
| Basilar fenestration | 1 (0.5%) |
| Mean follow-up time (SD) (months) | |
| Clinical | 8.48 (4.53) |
| Imaging | 9.91 (3.80) |
Outcomes
The technical success rate was 100% (95% CI: 0.98–1.00) and technical complication rate was 0% (95% CI: 0.00–0.02). The rates of perioperative morbidity and mortality were 7% (95% CI: 0.03–0.11) and 0% (95% CI: 0.00–0.01), respectively. The rate of perioperative hemorrhage was 0% (95% CI: 0.00–0.02). Rate of treatment-related long-term permanent neurological deficit was 2% (95% CI: 0.00–0.06). Late-term (at last imaging follow-up) complete occlusion rate was 60% (95% CI: 0.52–0.69). Retreatment rate was 14% (95% CI: 0.06–0.22). Full outcomes are summarized in Table 3.
Table 3.
Summary of outcomes
| Outcome | Effect size (95% CI) | I2 (%) |
|---|---|---|
| Technical success | 1.00 (0.98-1.00) | 0.00 |
| Technical complication | 0.00 (0.00-0.02) | 0.00 |
| Perioperative morbidity | 0.07 (0.03-0.11) | 0.00 |
| Perioperative mortality | 0.00 (0.00-0.01) | 0.00 |
| Perioperative hemorrhage | 0.00 (0.00-0.02) | 0.00 |
| Long-term neurological deficit | 0.02 (0.00-0.06) | 0.00 |
| Mid-term complete occlusion | 0.53 (0.42-0.64) | 35.79 |
| Late-term complete occlusion | 0.60 (0.52-0.69) | 0.00 |
| Retreatment | 0.13 (0.06-0.22) | 44.72 |
DISCUSSION
Our meta-analysis of the literature found that intracranial aneurysms can be treated with a pCONUS device with a technical success rate of 100% and a technical complication rate of 0%. Perioperative morbidity and mortality rates were low (7% and 0%, respectively) and a perioperative hemorrhage rate of 0%. Rate of treatment-related long-term neurological deficit was 2%. The complete occlusion rate at last radiological follow-up (mean time: 9.9 months) was 62% and retreatment rate was 14%. The most common treatment location was the MCA (44%) and the average neck size was almost 6 mm (dome:neck ratio: 1.45:1).
The pCONUS Bifurcation Aneurysm Implant is a laser-cut electrolytically detachable stent with a distal crown and four pedals that deploy into the aneurysm and rest at the level of the aneurysm neck. The name derives from the fact that it looks like an ice cream cone and its design is a further evolution of the “waffle-cone technique,” which has been used in the past for stent-assisted coiling of challenging aneurysms.[6,8,15] There are now several devices in the market that address a similar niche.
As more experiences are gained with these devices, it is clear that limitations still exist. As we found in our analysis, though technically successful and safe in its limited use, complete occlusion rates at radiological follow-up with the pCONUS devices are only 60% with 14% of aneurysms requiring retreatment, so whether or not these devices truly represent a substantial treatment advance is yet to be fully determined. Additionally, as a neuroendovascular surgeon, it is important to feel completely comfortable and confident with tools utilized during the procedure. As more devices for the treatment of complicated aneurysms come to market, practitioner wisdom and personal experience must be increasingly relied on to ensure that the treatment strategies associated with these devices do not become more difficult than the actual procedure itself.
LIMITATIONS
Our meta-analysis is based on single-center case series with limited experiences with a new endovascular device, and the nature of these single-center case series may introduce bias into the results reported in the literature. Nevertheless, we have adhered to the highest standards recommended in reporting this type of study which represents an updated snapshot of a fairly large number of patients who were treated with this novel device.
Financial support and sponsorship
Nil.
Conflicts of interest
Thomas J. Sorenson, Marta Iacobucci, Mohammad H. Murad, and Giuseppe Lanzino have no disclosures. Laurent Spelle and Jacques Moret are consultants for Sequent/MicroVention, Medtronic, Stryker, and Balt, outside of the submitted work.
Acknowledgements
The authors would like to thank the Mayo Clinic librarian, Patricia Erwin, for performing the literature search.
Footnotes
Contributor Information
Thomas J. Sorenson, Email: soren721@umn.edu.
Marta Iacobucci, Email: marta.iacobucci@gmail.com.
Mohammad H. Murad, Email: murad.mohammad@mayo.edu.
Laurent Spelle, Email: laurent@spelle.fr.
Jacques Moret, Email: pr.j.moret@orange.fr.
Giuseppe Lanzino, Email: lanzino.giuseppe@mayo.edu.
REFERENCES
- 1.Aguilar-Perez M, Kurre W, Fischer S, Bazner H, Henkes H. Coil occlusion of wide-neck bifurcation aneurysms assisted by a novel intra- to extra-aneurysmatic neck-bridging device (pCONus): Initial experience. AJNR Am J Neuroradiol. 2014;35:965–71. doi: 10.3174/ajnr.A3807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67:974–8. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- 3.Fischer S, Weber A, Titschert A, Brenke C, Kowoll A, Weber W. Single-center experience in the endovascular treatment of wide-necked intracranial aneurysms with a bridging intra-/extra-aneurysm implant (pCONus) J Neurointerv Surg. 2016;8:1186–91. doi: 10.1136/neurintsurg-2015-012004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gory B, Aguilar-Perez M, Pomero E, Turjman F, Weber W, Fischer S, et al. One-year angiographic results after pCONus stent-assisted coiling of 40 wide-neck middle cerebral artery aneurysms. Neurosurgery. 2017;80:925–33. doi: 10.1093/neuros/nyw131. [DOI] [PubMed] [Google Scholar]
- 5.Gory B, Aguilar-Perez M, Pomero E, Turjman F, Weber W, Fischer S, et al. pCONus device for the endovascular treatment of wide-neck middle cerebral artery aneurysms. AJNR Am J Neuroradiol. 2015;36:1735–40. doi: 10.3174/ajnr.A4392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horowitz M, Levy E, Sauvageau E, Genevro J, Guterman LR, Hanel R, et al. Intra/extra-aneurysmal stent placement for management of complex and wide-necked- bifurcation aneurysms: Eight cases using the waffle cone technique. Neurosurgery. 2006;58(Suppl 2):ONS-258–62. doi: 10.1227/01.NEU.0000204713.24945.D2. discussion ONS-262. [DOI] [PubMed] [Google Scholar]
- 7.Labeyrie PE, Gory B, Aguilar-Perez M, Pomero E, Biondi A, Riva R, et al. The pCONus device for treatment of complex wide-neck anterior communicating artery aneurysms. World Neurosurg. 2017;101:498–505. doi: 10.1016/j.wneu.2017.02.045. [DOI] [PubMed] [Google Scholar]
- 8.Limbucci N, Nappini S, Renieri L, Consoli A, Rosi A, Grillea G, et al. Hybrid y stenting with the waffle-cone.A technical note. Interv Neuroradiol. 2014;20:677–85. doi: 10.15274/INR-2014-10065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lubicz B, Morais R, Alghamdi F, Mine B, Collignon L, Eker OF. The pCONus device for the endovascular treatment of wide neck bifurcation aneurysms. J Neurointerv Surg. 2016;8:940–4. doi: 10.1136/neurintsurg-2015-011898. [DOI] [PubMed] [Google Scholar]
- 10.Lylyk P, Chudyk J, Bleise C, Sahl H, Perez MA, Henkes H, et al. The pCONus2 neck-bridging device: Early clinical experience and immediate angiographic results. World Neurosurg. 2018;110:e766–75. doi: 10.1016/j.wneu.2017.11.097. [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perez MA, Bhogal P, Moreno RM, Wendl C, Bazner H, Ganslandt O, et al. Use of the pCONus as an adjunct to coil embolization of acutely ruptured aneurysms. J Neurointerv Surg. 2017;9:39–44. doi: 10.1136/neurintsurg-2016-012508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ulfert C, Pfaff J, Schonenberger S, Bosel J, Herweh C, Pham M, et al. The pCONus device in treatment of wide-necked aneurysms: Technical and midterm clinical and angiographic results. Clin Neuroradiol. 2018;28:47–54. doi: 10.1007/s00062-016-0542-z. [DOI] [PubMed] [Google Scholar]
- 14.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet. 2007;370:1453–7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 15.Yang TH, Wong HF, Yang MS, Ou CH, Ho TL. “Waffle cone” technique for intra/extra-aneurysmal stent placement for the treatment of complex and wide-necked bifurcation aneurysm. Interv Neuroradiol. 2008;14(Suppl 2):49–52. doi: 10.1177/15910199080140S210. [DOI] [PMC free article] [PubMed] [Google Scholar]