Abstract
Background
This study investigated the effects of progressive stabilization exercise program carried out with respiratory resistance in patients with lumbar instability.
Material/Methods
Forty-three patients with lumbar instability were randomly assigned to experimental (n=20) and control groups (n=23). The experimental group performed progressive lumbar stabilization exercises along with respiratory resistance, and the control group only performed progressive lumbar stabilization exercises, for 40 min per session, 3 sessions a week, for 4 weeks. Numeric rating scale (NRS), Korean-Oswestry disability index (K-ODI), static balance ability, Fear-Avoidance Beliefs Questionnaire (FABQ), and pulmonary function test (PFT) were performed before and after the intervention program for comparison.
Results
The 2 groups showed significant differences in NRS, K-ODI, balance ability, and FABQ after the interventions (p<0.05), but greater improvements were shown by the experimental group in balance ability and FABQ values. PFT results in the experimental group showed a significant increase (p<0.05) in forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and maximum voluntary ventilation (MVV). The experimental group showed a greater improvement (p<0.05) in FVC and MVV compared to the control group.
Conclusions
Progressive stabilization exercise program with respiratory resistance is an effective method with clinical significance in pain reduction, psychosocial stability, and enhancement of motor and respiratory functions.
MeSH Keywords: Back Pain, Breathing Exercises, Exercise Therapy, Joint Instability, Progressive Patient Care, Respiratory Therapy
Background
Longer times are spent in a seated position due to industrialization and the development of transportation methods, and it has led to lower-extremity and trunk muscle weakness, causing chronic low back pain [1]. Early stages of low back pain can progress to chronic pain depending on the frequency of the pain attacks, and this leads to muscle imbalances and motor dysfunctions [2,3]. Instability may also result from weakening of lumbar muscles [4,5], and increase psychosocial problems such as depression, and low quality of life may arise along with anxiety, depression, and feeling of helplessness in people with chronic low back pain [6,7]. Considering that the primary cause of low back pain is lumbar instability and muscle imbalances, maintaining proper posture and exercise programs for enhancing balance abilities are essential for low back pain management [8,9].
Patients with low back pain are prescribed exercises with various intensity and form for muscle strengthening and balance control [10–12]. The effects of stabilization exercise program methods that enhance muscle activation through trunk muscle contraction for pain decrease and functional recovery have been reported [11,13]. Stabilization of the deep muscles plays a critical role in anatomical structures of patients with low back pain. Particularly, erector spinae, multifidus, quadratus lumborum, iliopsoas, and abdominals play an important role in stabilizing the spine, and exercise methods that progressively activate these muscles are recently being recommended [14,15]. These exercise methods treat and prevent low back pain, and also has the advantage of stabilizing and progressively approaching the lumbo-pelvic area [15–17].
To provide stabilization through the lumbar segment, contraction of the deep muscles is a critical factor [18]. Respiration techniques that induce transversus abdominis and diaphragm contraction are implemented to enhance the effects of spinal stabilization for patients with low back pain [19]. The implementation of respiration techniques such as abdominal hollowing, diaphragm, and respiratory resistance assists harmonious muscle activations with other muscles [20], and it affects posture and spinal stabilization greatly by co-contracting deep muscles such as internal oblique abdominals, multifidus, and pelvic floor muscles [21].
There are many studies on various exercise methods on patients with low back pain, but it is only recent when the importance of respiration has been emphasized. Therefore, this study aimed to investigate the effects of progressive stabilization exercise with respiration resistance on pain, motor function, pulmonary function, and psychosocial factors. The hypothesis of this study is that the activation of deep muscles during accurate forced respiratory training will reduce pain and increase motor and pulmonary functions to provide psychosocial stability.
Material and Methods
Participants
Sixty-nine patients admitted for treatment for low back pain were recruited. The inclusion criteria were: (1) persons between 18–65 years of age and having had low back pain within the last 6 weeks, (2) a score of 3 or higher on the numeric rating scale (NRS), (3) positive in 3 or more out of the 5 items in the lumbar instability test (Hicks et al., 2003), (4) and persons who are able to stand on 1 leg for 30 s. Patients who had compression fracture, diagnosed with systemic diseases such as cancer, difficulties in participating in the study due to neurological conditions, and persons who had participation rate lower than 80% of the program schedule were excluded.
The purpose and the process of the study were explained to all participants, and they all signed the written consent that their participation is fully voluntary. This study was approved by the Ethics Committee, and is registered in the WHO International Clinical Trials Registry Platform: KCT0003107.
Study design and process
This was randomized control trial, in which the recruited participants went through lumbar instability testing for selection screening. Lumbar instability testing consisted of: (1) lumbar instability test in prone position (pain occurring while applying pressure on the vertebral segments by raising both legs up in prone position is indicated as positive), (2) lumbar posterior-anterior mobility test (excessive or abnormal movements while pressure is applied on the vertebral segments prone position is indicated as positive), (3) straight leg raising test (mean angle exceeding 90 degrees during hip flexion with knee flexed on both sides is indicated as positive), (4) passive lumbar extension test (pain occurring when both legs are lifted in prone position and pain relieved when the legs are returned to the starting position is indicated as positive), and (5) under 40 years of age. If there were more than 3 items that were positive, the person was categorized as having lumbar instability [22]. To calculate the sample size, G-power 3.19 software was used. Moderate effect size (effect size=0.5) was set based on Cohen’s d, significance level was set to α=0.05, and power (1-β)=0.8, resulting in a minimum 17 of participants. However, a drop-out rate of 15% was considered, thereby setting the minimum number of participants to 20.
Twenty-three among 69 participants were excluded by the screening test (lumbar instability test). Pre-intervention assessment was made to compare the effects pre- and post-intervention. Random number allocation was used to assign the 46 participants to either experimental (n=23) or control (n=23) groups. The experimental group performed a lumbar stabilization exercise program using respiratory resistance training, and the control group performed only a lumbar stabilization exercise program. The participants were trained by a therapist until they were familiar with the program by the different stages, and afterwards they performed exercises independently. All of the participants performed the intervention without knowing which group they belonged to. Due to refusal and early discharge, 3 participants dropped out from the experimental group, resulting in 20 participants in the experimental group and 23 participants in the control group. Their data were recorded and analyzed (Figure 1).
Figure 1.
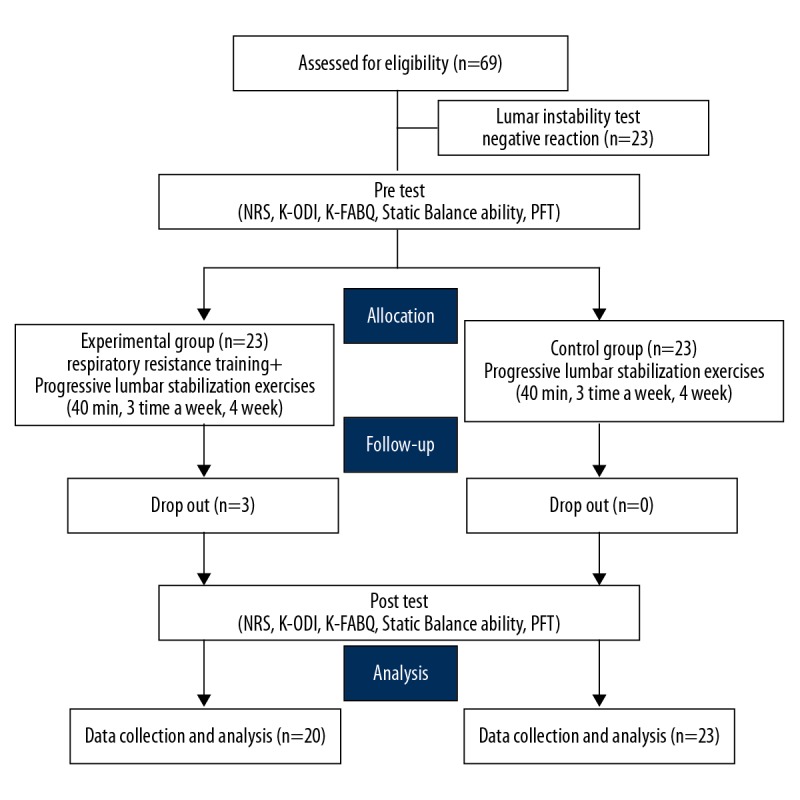
CONSORT flow chart.
Intervention
Progressive stabilization exercise
The progressive stabilization exercise program provided to patients with lumbar instability was modified from the intervention method of Lee et al. (2016) [15]. The progressive stabilization exercise program, which is a method developed to help stabilization of anterior, posterior, and lateral trunk muscles, consists of Curl up, Dead Bug, Superman, Bird Dog, and Side Flank with knee flexion (Figure 2). Pain and motor function levels of the participants were considered to provide easy movements to more difficult movements as the weeks progressed. Stretching for 5 min was performed to warm up and cool down before and after the sessions. Each movement was made for 3 sets consisting of 5 repetitions and 20 s each repetition, with a 1-min break between each set. The intervention was implemented for 4 weeks, 3 times a week, and 40 min per session, where the participant progressed to the next level of movements when the program movements were successful by 80%. Each weekly program consisted of 5 movements and the participants should be able to perform at least 4 of the 5 movements in order to perform the next week’s level of movements.
Figure 2.
Progressive stabilization exercise program.
Respiratory resistance training
The experimental group performed breathing resistance training simultaneously with the progressive stabilization exercise program. The experimental group performed the exercise program using a respiration-resisting device (Expand-a-Lung, USA), which is composed of a silicon mouth piece and a valve that controls ventilation. The respiration-resisting device controls the ventilation amount during inhalation and exhalation, and results in resistance of air flow for respiratory muscle strengthening. With the use of the respiration-resisting device, the resistance level was set to a stage where the participants could stay below 14 in Borg’s rating of perceived exertion [23]. The participants were notified about potential dizziness, nausea, vomiting, and shortness of breath during use of the respiration-resisting device, and were given an explanation regarding immediate termination of the intervention.
Assessment tools
To identify the pain levels of the participants following the intervention program, the NRS was used [24]. To quantify physical inconveniences in daily life due to low back pain, the Korean version of the Oswestry Disability Index (K-ODI) was used, and the total score was converted to percentage (%) for recording [25]. Balance ability was measured to identify the level of physical functions between the groups depending on the intervention methods. The participants stepped on top of the platform Wii balance board (Nintendo, Kyoto, Japan) to track the sway of center of pressure (CoP) to derive path length, velocity, and area 95%. The participants maintained a relaxed position with both arms placed by the side and both feet on the Wii balance board. Then, the participant stood on the dominant leg when instructed by the therapist. To control postural disturbance coming from vision, the participants were asked to focus on a dot 15 cm in diameter and 3 m away. The mean of measure values from 3 trials were used for analysis. The inter-rater reliability of the Wii Balance Board is ICC=.92–.98 [26], and the Balancia program is a helpful assessment tool that has standardized inter-rater reliability (r=.79–.96) and validity (r=.85–.96) [27]. The Korean version of the Fear-Avoidance Beliefs Questionnaire (K-FABQ) is a self-reported questionnaire that assesses relationships of fear-avoidance response, low back pain, and dysfunction [28]. Five items related to physical activities in FABQ-PA and 11 items related to work in FABQ-W are given in a 7-point scale (0=Totally disagree, 6=Perfectly agree) for self-assessment. The score range of FABQ is 0–66, and higher score means stronger degree. The Korean version of the FABQ Joo et al. (2009) was used, and the reliability of this test is.95 [25]. Pulmonary function testing was conducted using Microquark® (COSMED, Italy). The total amount of emitted air after maximal inhalation and forced exhalation is assigned as forced vital capacity (FVC), and forced expiratory volume (FEV) for 1 s is set as FEV1. The 2 values were then used to derive the FEV1/FEV ratio (FEV1%), and the amount of ventilated air for 15 s at the fastest speed was converted to the amount in 1 min to determine maximal voluntary ventilation (MVV). A physiotherapist with substantial experience in pulmonary function testing assessed 3 trials, and the values were used for analysis. There was a 10-min break between each test.
Statistical analysis
Data analysis was performed using SPSS version 21.0 (IBM, Chicago, IL, USA). General characteristics of the participants were provided using mean and standard deviation values through descriptive statistics, and the Shapiro-Wilk test was used for normality testing. Normal distribution of all variables from the results was identified. General characteristics between groups and homogeneity test of pre-intervention values were analyzed through chi-squared test and t test. The independent-samples t test and chi-squared test were used to compare the intervention results between the groups, and the paired t test was used to compare the dependent variables within the groups. Statistical significance was set at p<0.05.
Results
General characteristics and dependent variables of the participants between the groups were homogeneous before the intervention (Table 1).
Table 1.
General characteristics of participants.
| Variables | Experimental group (n=20) | Control group (n=23) | t/χ2 | p |
|---|---|---|---|---|
| Gender (Male/Female) | 12/8 | 12/11 | −0.505 | 0.616 |
| Age (years) | 30.9±4.53 | 30.70±6.32 | 0.12 | 0.905 |
| Height (cm) | 169.60±9.06 | 168.87±8.60 | 0.271 | 0.788 |
| Weight (kg) | 69.74±17.35 | 70.30±18.55 | −0.101 | 0.92 |
The 2 groups both showed statistically significant differences in NRS, K-ODI, balance abilities, and K-FABQ for pre- and post-interventions (p<0.05). However, there were significant differences between groups only in CoP path length, velocity of balance ability, and FABQ-PA for physical activities (Table 2). As for pulmonary function, FVC, FEV1, and MVV showed significant increase (p<0.05) in the experimental group, but the control group only had a significant increase in MVV (p<0.05). There were no differences between the 2 groups except for FVC and MVV (Table 3).
Table 2.
Comparison of pain, motor function, psychosocial level between groups.
| Variables | Experimental group (n=20) | Control group (n=23) | t(p) | |
|---|---|---|---|---|
| NRS (score) | Pre | 6.85±1.23 | 6.91±1.24 | −0.167 (.868) |
| Post | 3.60±1.14 | 3.65±1.27 | ||
| Post-pre | −3.25±1.164 | −3.26±1.51 | 0.026 (.979) | |
| t(p) | −12.485 (.000) | −10.329 (.000) | ||
| K-ODI (score) | Pre | 16.30±6.68 | 16.04±4.15 | 0.149 (.883) |
| Post | 9.85±4.81 | 11.08±4.30 | ||
| Post-pre | −6.45±3.15 | −4.96±3.27 | −1.519 (.136) | |
| t(p) | −9.147 (.000) | −7.274 (.000) | ||
| CoP velocity (cm/s) | Pre | 4.59±0.66 | 4.80±0.66 | −1.288 (.205) |
| Post | 3.54±0.56 | 4.30±0.85 | ||
| Post-pre | −1.05±0.67 | −0.50±0.54 | −2.957 (.005) | |
| t(p) | −6.992 (.000) | −4.456 (.000) | ||
| CoP length (cm) | Pre | 137.84±19.70 | 145.15±19.12 | −1.264 (.213) |
| Post | 110.21±19.40 | 129.63±20.78 | ||
| Post-pre | −27.63±22.51 | −15.53±15.02 | −2.098 (.042) | |
| t(p) | −5.490 (.000) | −4.956 (.000) | ||
| CoP area 95% (cm2) | Pre | 9.09±3.40 | 8.38±2.70 | 0.419 (.677) |
| Post | 5.93±2.52 | 6.37±2.32 | ||
| Post-pre | −3.16±3.09 | −2.01±2.54 | −1.343 (.187) | |
| t(p) | −4.566 (.000) | −3.793 (.001) | ||
| K-FABQ-PA (score) | Pre | 23.00±3.88 | 20.35±6.62 | 1.626 (.113) |
| Post | 15.20±3.55 | 16.22±6.78 | ||
| Post-pre | −7.80±2.89 | −4.13±4.07 | −3.358 (.002) | |
| t(p) | −12.05 (.000) | −4.866 (.000) | ||
| K-FABQ-W (score) | Pre | 44.15±7.66 | 40.70±10.95 | 1.181 (.244) |
| Post | 33.10±6.59 | 33.65±9.27 | ||
| Post-pre | −11.05±5.81 | −7.04±7.81 | −1.884 (.067) | |
| t(p) | −8.508 (.000) | −4.323 (.000) |
Values are presented as mean ±SD. NRS – numeric rating scale; K-ODI – Korean version of Oswestry Disability Index; CoP – center of pressure; K-FABQ – Korean version of Fear-Avoidance Beliefs Questionnaire; PA – physical activity; W – work.
Table 3.
Comparison of pulmonary function levels between groups.
| Variables | Experimental group (n=20) | Control group (n=23) | t(p) | ||||
|---|---|---|---|---|---|---|---|
| Pulmonary function test | |||||||
| FVC (L) | Pre | 3.87±0.98 | 3.75±0.81 | 0.590 (.558) | |||
| Post | 4.10±1.00 | 3.81±0.82 | |||||
| Post-pre | 0.23±.180 | 0.61±0.17 | 3.053 (.004) | ||||
| t(p) | 5.644 (.000) | 1.682 (.107) | |||||
| FEV1 (L) | Pre | 3.41±0.93 | 3.20±0.83 | 0.742 (.462) | |||
| Post | 3.63±0.97 | 3.28±0.77 | |||||
| Post-pre | 0.22±0.23 | 0.08±0.34 | 1.471 (.149) | ||||
| t(p) | 4.114 (.001) | 1.115 (.277) | |||||
| FEV1/FVC (%) | Pre | 88.15±8.02 | 88.80±7.86 | −0.270 (.789) | |||
| Post | 88.25±8.71 | 85.86±8.98 | |||||
| Post-pre | 0.10±5.87 | −2.94±9.69 | 1.222 (.229) | ||||
| t(p) | 0.076 (.940) | −1.457 (.159) | |||||
| MVV (L/min) | Pre | 99.92±24.75 | 102.60±26.86 | −0.255 (.800) | |||
| Post | 124.14±29.77 | 111.24±29.84 | |||||
| Post-pre | 24.21±21.70 | 8.64±10.83 | 2.910 (.007) | ||||
| t(p) | 4.990 (.000) | 3.826 (.001) | |||||
Values are presented as mean ±SD. FVC – forced vital capacity; FEV1 – forced expiratory volume in one second; FEV1/FVC – forced expiratory volume in one second/forced vital capacity; MVV – maximum voluntary ventilation.
Discussion
The purpose of this study was to compare the effects of progressive stabilization exercise program with and without respiration resistance on patients with lumbar instability. All participants had decreased pain, anxiety towards motor performance, and psychosocial anxiety, whereas balance ability has increased. In addition, the progressive stabilization exercise program using respiratory resistance resulted in significant improvements in balance, anxiety towards physical activities, and lung capacity in the experimental group compared to the control group. Progressive stabilization exercise enhances stabilization of the spine and has the advantage of suggesting exercise methods to patients appropriate to their levels; therefore, the clinical usability of this method is good. Moon et al. (2013) [29] reported significant levels of pain reduction in non-specified chronic low back pain patients after 8 weeks of implementing a stabilization exercise program (p<0.05, effect size d=1.50), and Hwangbo et al. (2015) [30] reported significant decrease in pain after applying trunk stabilization exercise to chronic low back pain patients for 6 weeks (p<0.05, effect size d=3.61). In addition, Lee et al. (2016) reported that 3 weeks of progressive stabilization exercise in chronic low back pain patients showed a significant decrease in pain compared to conventional physical therapy (p<0.05, effect size d=1.46). The present study showed that both the control group (effect size d=2.60) and the experimental group (effect size d=2.74) had significant decreases in pain. Although there were no statistically significant differences between the 2 groups, both interventions showed significant effects on pain relief. Lumbar stabilization exercises suggested by the exercise program activates the muscles around the lumbar, pelvis, and abdominals, contributing to the improvement of trunk stabilization [31]. Particularly for the experimental group, strong abdominal contractions from forced exhalation muscles during respiratory resistance may have contributed to greater stabilization in the trunk. The progressive lumbar stabilization exercise program not only decreased low back pain, but also decreased the unease during physical activities in everyday life and enhanced motor functions. ODI is the most commonly recommended condition-specific outcome measurement method in spinal dysfunctions [32,33].
This study used the Korean Version of the Oswestry Disability Index to investigate the level of motor dysfunction in the lumbar area [34]. Excluding the items related to sexual activities, a percentage was derived from 45 points total. The experimental group showed decrease in dysfunction level from 36.22% to 21.82% and 35.65% to 24.63% in the control group. Although the pre- and post-intervention differences are not significant between the groups, progressive lumbar stabilization exercise effects were demonstrated in both groups.
In patients with low back pain, there is a report that stability during while standing on 1 leg on the dominant side is relatively decreased in patients with low back pain when compared to healthy adults [35]. Hungerford et al. (2004) [36] demonstrated that mobilization pattern and muscle activation of deep trunk muscles such as internal oblique abdominals and multifidus, and muscles related to pelvic extension, such as gluteus maximus and tensor fascia latae, are different in low back pain patients during one-leg standing compared to healthy adults. These muscles are reported to contribute to chronic pain when unstable due to dysfunction and motor control injuries. Therefore, one-leg standing may be a qualitative and quantitative test of stabilization muscles in low back pain patients [37]. Also, in this study, a static one-leg standing test was conducted to assess motor performance in lumbar instability. The participants performed one-leg stand for 30 s on their dominant leg, and the variables for CoP, length, velocity, and area were measured for comparison. The 2 groups both showed significant increase in all variables before and after the interventions, and the path length and velocity of CoP resulted in a significant decrease in the experimental group. To prevent and reduce spinal dysfunction, trunk muscles that maintain optimal alignment of the spine and pelvis must be established and the patient should avoid unnecessary exercises [38]. Progressive stabilization exercise using respiratory resistance increased co-contraction of core muscles that determine trunk stabilization, and this may have led to the increase of balance ability.
When one is afflicted with an injury or disease, the fear-avoidance response disturbs normal sensations and it may lead to severe disability. One avoids physical and vocational activities due to fear-avoidance response, and this may potentially lead to fibrosis and atrophy [28]. Additionally, fear-avoidance response due to pain from physical and vocational activities may lower self-efficacy, worsen the health condition, and cause a disability [39]. Therefore, the assessment on fear-avoidance response related to lumbar dysfunction is considered to be important in examining the prognosis of returning to everyday living and psychosocial changes [28,40]. This study used the Korean Version of the Fear-Avoidance Beliefs Questionnaire to investigate fear-avoidance responses before and after the interventions. The results demonstrated that decrease in lumbar pain and the improvement of motor functions are associated with decrease of anxiety. FABQ-PA results showed that both groups showed significant decreases in psychological anxiety towards physical activities before and after the interventions, and these effects were greater in the experimental group (effect size=2.10) than in the control group (effect size=0.62). FABQ-W is the result of measuring psychological stability regarding vocational performance, and the differences pre- and post-intervention within each group were statistically significant. However, the differences between the 2 groups did not show any significant difference and this may have been due to not being able to consider vocational characteristics of the participants when randomizing.
Serratus posterior inferior, levatores costarum, sternocleidomastoid, latissimus dorsi, pectoralis major, and quadratus lumborum muscles are contracted in forced inspiration during respiratory resistance, and rectus abdominis, external oblique abdominals, internal oblique abdominals, transversus abdominis, transversus thoracis, and internal intercostals are contracted [41]. The co-contraction of muscles not only provides lumbar stabilization, but also forced respiration. The progressive stabilization exercise program with respiratory resistance showed significant increases in FVC and MVV in the experimental group. The progressive stabilization exercise program with respiratory resistance requires co-contraction of stabilization muscles such as diaphragm, multifidus, and transversus abdominis, and provides integrity of each lumbar segment from a functionally interdependent compensation system. This exercise program also decreases pain, increases motor function, provides psychosocial stability, and improves lung functions.
The progressive stabilization exercise program using respiratory resistance requires a relatively long time for the participants to adjust. The participants had saliva pooling in the mouth-piece or expressed feeling nausea. The weekly exercise program was easily administered after the participants were sufficiently adjusted to the respiratory resistance device. This study has some limitations. First, the intervention period was only 4 weeks, and continuous effects after the interventions could not be compared and analyzed. Secondly, the age range of the participants was limited; therefore, making generalizations about chronic low back pain patients of all age groups could be difficult. It is questionable whether older chronic low back pain patients could use of the tolerate respiratory resistance device. The application of respiration must be considered for lumbar stabilization. Future studies may need to consider these limitations to modify lumbar stabilization exercise programs using respiration.
Conclusions
This study investigated the effects of a progressive stabilization exercise program using respiratory resistance for low back pain patients with unstable lumbar spine. The results showed decreased pain, as well as increased motor function and psychosocial stability, leading to significant improvement in respiratory function. These results show that progressive stabilization exercise using respiratory resistance is beneficial to patients with lumbar instability.
Footnotes
Source of support: This work was supported by the National Research Foundation of Korea (NRF) through a grant from the Korean Government (MSIP; Ministry of Science, ICT & Future Planning) (No. 20180066)
References
- 1.Morrow LJ, Smith S. The management of lower back pain. J R Nav Med Serv. 2014;100:282–87. [PubMed] [Google Scholar]
- 2.Skoffer B. Low back pain in 15- to 16-year-old children in relation to school furniture and carrying of the school bag. Spine (Phila Pa 1976) 2007;32:E713–17. doi: 10.1097/BRS.0b013e31815a5a44. [DOI] [PubMed] [Google Scholar]
- 3.Burton AK, Balague F, Cardon G, et al. Chapter 2. European guidelines for prevention in low back pain: November 2004. Eur Spine J. 2006;15(Suppl 2):S136–68. doi: 10.1007/s00586-006-1070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’sullivan PB, Burnett A, Floyd AN, et al. Lumbar repositioning deficit in a specific low back pain population. Spine (Phila Pa 1976) 2003;28:1074–79. doi: 10.1097/01.BRS.0000061990.56113.6F. [DOI] [PubMed] [Google Scholar]
- 5.Adams MA, Roughley PJ. What is intervertebral disc degeneration, and what causes it? Spine (Phila Pa 1976) 2006;31:2151–61. doi: 10.1097/01.brs.0000231761.73859.2c. [DOI] [PubMed] [Google Scholar]
- 6.Gatchel RJ, Bernstein D, Stowell AW, Pransky G. Psychosocial differences between high-risk acute vs. chronic low back pain patients. Pain Pract. 2008;8:91–97. doi: 10.1111/j.1533-2500.2008.00176.x. [DOI] [PubMed] [Google Scholar]
- 7.Kovacs FM, Abraira V, Zamora J, et al. Correlation between pain, disability, and quality of life in patients with common low back pain. Spine (Phila Pa 1976) 2004;29:206–10. doi: 10.1097/01.BRS.0000107235.47465.08. [DOI] [PubMed] [Google Scholar]
- 8.Teyhen DS, Rieger JL, Westrick RB, et al. Changes in deep abdominal muscle thickness during common trunk-strengthening exercises using ultrasound imaging. J Orthop Sports Phys Ther. 2008;38:596–605. doi: 10.2519/jospt.2008.2897. [DOI] [PubMed] [Google Scholar]
- 9.Lim NY, Yi YJ. [The effects of Koryo Hand-Acupuncture on the patients with chronic low back pain]. Taehan Kanho Hakhoe Chi. 2003;33:79–86. doi: 10.4040/jkan.2003.33.1.79. [in Chinese] [DOI] [PubMed] [Google Scholar]
- 10.Cairns MC, Foster NE, Wright C. Randomized controlled trial of specific spinal stabilization exercises and conventional physiotherapy for recurrent low back pain. Spine (Phila Pa 1976) 2006;31:E670–81. doi: 10.1097/01.brs.0000232787.71938.5d. [DOI] [PubMed] [Google Scholar]
- 11.Goldby LJ, Moore AP, Doust J, Trew ME. A randomized controlled trial investigating the efficiency of musculoskeletal physiotherapy on chronic low back disorder. Spine (Phila Pa 1976) 2006;31:1083–93. doi: 10.1097/01.brs.0000216464.37504.64. [DOI] [PubMed] [Google Scholar]
- 12.Kofotolis N, Kellis E. Effects of two 4-week proprioceptive neuromuscular facilitation programs on muscle endurance, flexibility, and functional performance in women with chronic low back pain. Phys Ther. 2006;86:1001–12. [PubMed] [Google Scholar]
- 13.Kavcic N, Grenier S, Mcgill SM. Quantifying tissue loads and spine stability while performing commonly prescribed low back stabilization exercises. Spine (Phila Pa 1976) 2004;29:2319–29. doi: 10.1097/01.brs.0000142222.62203.67. [DOI] [PubMed] [Google Scholar]
- 14.Mcgill SM. Low back stability: from formal description to issues for performance and rehabilitation. Exerc Sport Sci Rev. 2001;29:26–31. doi: 10.1097/00003677-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Lee HS, Kim DJ, Oh Y, et al. The effect of individualized gradable stabilization exercises in patients with chronic low back pain: Case-control study. J Back Musculoskelet Rehabil. 2016;29:603–10. doi: 10.3233/BMR-160724. [DOI] [PubMed] [Google Scholar]
- 16.Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 2002;48:297–302. doi: 10.1016/s0004-9514(14)60169-0. [DOI] [PubMed] [Google Scholar]
- 17.Niemisto L, Lahtinen-Suopanki T, Rissanen P, et al. A randomized trial of combined manipulation, stabilizing exercises, and physician consultation compared to physician consultation alone for chronic low back pain. Spine (Phila Pa 1976) 2003;28:2185–91. doi: 10.1097/01.BRS.0000085096.62603.61. [DOI] [PubMed] [Google Scholar]
- 18.Bradley H, Esformes J. Breathing pattern disorders and functional movement. Int J Sports Phys Ther. 2014;9:28–39. [PMC free article] [PubMed] [Google Scholar]
- 19.Macedo LG, Latimer J, Maher CG, et al. Effect of motor control exercises versus graded activity in patients with chronic nonspecific low back pain: A randomized controlled trial. Phys Ther. 2012;92:363–77. doi: 10.2522/ptj.20110290. [DOI] [PubMed] [Google Scholar]
- 20.Hodges PW, Gandevia SC. Changes in intra-abdominal pressure during postural and respiratory activation of the human diaphragm. J Appl Physiol (1985) 2000;89:967–76. doi: 10.1152/jappl.2000.89.3.967. [DOI] [PubMed] [Google Scholar]
- 21.Obayashi H, Urabe Y, Yamanaka Y, Okuma R. Effects of respiratory-muscle exercise on spinal curvature. J Sport Rehabil. 2012;21:63–68. doi: 10.1123/jsr.21.1.63. [DOI] [PubMed] [Google Scholar]
- 22.Hicks GE, Fritz JM, Delitto A, Mishock J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil. 2003;84:1858–64. doi: 10.1016/s0003-9993(03)00365-4. [DOI] [PubMed] [Google Scholar]
- 23.Hollander DB, Durand RJ, Trynicki JL, et al. RPE, pain, and physiological adjustment to concentric and eccentric contractions. Med Sci Sports Exerc. 2003;35:1017–25. doi: 10.1249/01.MSS.0000069749.13258.4E. [DOI] [PubMed] [Google Scholar]
- 24.Maher CG, Latimer J, Hodges PW, et al. The effect of motor control exercise versus placebo in patients with chronic low back pain [ACTRN012605000262606] BMC Musculoskelet Disord. 2005;6:54. doi: 10.1186/1471-2474-6-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joo MK, Kim TY, Kim JT, Kim SY. Reliability and validity of the Korean version of the fear-avoidance beliefs questionnaire. Phys Ther Korea. 2009;16:24–30. [Google Scholar]
- 26.Holmes JD, Jenkins ME, Johnson AM, et al. Validity of the Nintendo Wii(R) balance board for the assessment of standing balance in Parkinson’s disease. Clin Rehabil. 2013;27:361–66. doi: 10.1177/0269215512458684. [DOI] [PubMed] [Google Scholar]
- 27.Park DS, Lee G. Validity and reliability of balance assessment software using the Nintendo Wii balance board: usability and validation. J Neuroeng Rehabil. 2014;11:99. doi: 10.1186/1743-0003-11-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Waddell G, Newton M, Henderson I, et al. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–68. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 29.Moon HJ, Choi KH, Kim DH, et al. Effect of lumbar stabilization and dynamic lumbar strengthening exercises in patients with chronic low back pain. Ann Rehabil Med. 2013;37:110–17. doi: 10.5535/arm.2013.37.1.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hwangbo G, Lee CW, Kim SG, Kim HS. The effects of trunk stability exercise and a combined exercise program on pain, flexibility, and static balance in chronic low back pain patients. J Phys Ther Sci. 2015;27:1153–55. doi: 10.1589/jpts.27.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Richardson CA, Snijders CJ, Hides JA, et al. The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine (Phila Pa 1976) 2002;27:399–405. doi: 10.1097/00007632-200202150-00015. [DOI] [PubMed] [Google Scholar]
- 32.Deyo RA, Battie M, Beurskens AJ, et al. Outcome measures for low back pain research. A proposal for standardized use. Spine (Phila Pa 1976) 1998;23:2003–13. doi: 10.1097/00007632-199809150-00018. [DOI] [PubMed] [Google Scholar]
- 33.Roland M, Fairbank J. The Roland-Morris disability questionnaire and the oswestry disability questionnaire. Spine (Phila Pa 1976) 2000;25:3115–24. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 34.Kim DY, Lee SH, Lee HY, et al. Validation of the Korean version of the oswestry disability index. Spine (Phila Pa 1976) 2005;30:E123–27. doi: 10.1097/01.brs.0000157172.00635.3a. [DOI] [PubMed] [Google Scholar]
- 35.Jo HJ, Song AY, Lee KJ, et al. A kinematic analysis of relative stability of the lower extremities between subjects with and without chronic low back pain. Eur Spine J. 2011;20:1297–303. doi: 10.1007/s00586-010-1686-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hungerford B, Gilleard W, Lee D. Altered patterns of pelvic bone motion determined in subjects with posterior pelvic pain using skin markers. Clin Biomech (Bristol, Avon) 2004;19:456–64. doi: 10.1016/j.clinbiomech.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 37.Page P, Frank C, Lardner R. Assessment and Treatment of Muscle Imbalance: The Janda Approach, 2010. Human Kinetics [Google Scholar]
- 38.Sahrmann S, Azevedo DC, Dillen LV. Diagnosis and treatment of movement system impairment syndromes. Braz J Phys Ther. 2017;21:391–99. doi: 10.1016/j.bjpt.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain. 2000;85:317–32. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 40.Pfingsten M, Kroner-Herwig B, Leibing E, et al. Validation of the German version of the Fear-Avoidance Beliefs Questionnaire (FABQ) Eur J Pain. 2000;4:259–66. doi: 10.1053/eujp.2000.0178. [DOI] [PubMed] [Google Scholar]
- 41.De Almeida IC, Clementino AC, Rocha EH, et al. Effects of hemiplegy on pulmonary function and diaphragmatic dome displacement. Respir Physiol Neurobiol. 2011;178:196–201. doi: 10.1016/j.resp.2011.05.017. [DOI] [PubMed] [Google Scholar]



