Abstract
Background
Diabetic retinopathy (DR) is one of the most common diseases causing blindness in the world, and most patients are already in advanced stage. Recent years, many studies reported mean platelet volume (MPV) may be associated with development of DR, but there was no consistent conclusion reached.
Methods
Literature was retrieved by formally searching PubMed, Embase, Cochrane library and Scopus and by hand searching of reference lists of related articles. Finally, a total of 14 literatures included, and Review manager 5.3 and STATA 14.0 statistical software were utilized for processing.
Results
Meta-analysis showed that MPV values in DR were significantly higher than health controls [SMD (95% CI) = 0.92 (0.60–1.24)] and type 2 diabetes mellitus without diabetic retinopathy (T2DM without DR) [SMD (95% CI) = 0.36 (0.19–0.53)]. Subgroup analysis indicated that MPV level in proliferative diabetic retinopathy (PDR) patients was higher than T2DM without DR patients [SMD (95% CI) = 0.48 (0.28, 0.68)], but this difference didn’t appear in non-proliferative diabetic retinopathy (NPDR).
Conclusions
The study demonstrated that increased MPV level was significant associated with the development of DR, and it might reflect the severity of DR, which could be provided to monitor development and progression of DR clinically.
Keywords: Mean platelet volume, Diabetic retinopathy, Meta-analysis
Background
Type 2 diabetes mellitus is a common metabolic disease with all kinds of microvascular diseases occurring. Diabetic retinopathy (DR), a kind of microvascular lesions occurring in fundus, accounts for 40 percent of diabetics over 40 years of age [1], and is the main cause of impaired vision and even blindness in diabetics [2]. The pathogenesis of diabetic retinopathy is not clear, relevant studies have shown that it may be associated with local microvascular injury and microcirculation disorders, and improving blood circulation of the retina effectively before or early in the emergence of DR may prevent it from developing [3, 4]. The diagnosis of diabetic retinopathy depends on fundus examination, but it’s not good for routine screening, and the patient’s compliance is poor. Therefore, it is especially important to find simple detection methods. Microthrombus formation caused by microcirculation changes is a pathogenic factor, in which platelet plays an important role [5, 6]. Mean platelet volume (MPV) reflects the average size and function of platelet in a person’s blood sample, of which the relationship with acute myocardial infarction and coronary artery has been shown [7, 8]. As parameters of platelet, high level MPV might be associated with increased thrombotic potential [9], which might participate in development of DR. However, conflicting data are available on MPV in DR, and there hasn’t been a systematic review to assess the relationship.
This study aims to assess and quantify differences in MPV comparing subjects with DR, type 2 diabetes mellitus without diabetic retinopathy (T2DM without DR) and control group, for exploring the relationship between MPV and DR.
Methods
Literature search
Literature was retrieved by formal search of electronic databases (PubMed, Embase, Cochrane library and Scupos) and by hand searching of reference lists of related articles. These computer searches were limited to English language articles from the beginning of building database to December 2017, and Chinese language articles must be published on medline. The following keywords were used for searching: ‘‘diabetic retinopathy’’ AND ‘‘mean platelet volume’’. The retrieval strategy of Pubmed as follow: (((((Diabetic Retinopathies [Title/Abstract] OR Retinopathies, Diabetic [Title/Abstract] OR Retinopathy, Diabetic[Title/Abstract])) OR diabetic retinopathy[Title/Abstract]) OR “Diabetic Retinopathy”[Mesh])) AND ((((Mean Platelet Volumes[Title/Abstract] OR Platelet Volume, Mean[Title/Abstract] OR Platelet Volumes, Mean[Title/Abstract] OR Volume, Mean Platelet[Title/Abstract] OR Volumes, Mean Platelet[Title/Abstract])) OR mean platelet volume[Title/Abstract]) OR “Mean Platelet Volume”[Mesh]).
Selection criteria
The inclusion criteria were as follows: (1) published literature related to the association of MPV level with DR; (2) independent case–control studies or cross-section studies using either a hospital-based or a population-based design; (3) the original studies must provide the number of each group and the mean and standard of MPV. Excluded criteria: (1) duplicated data; (2) the original data could not be extracted.
Data extraction and quality assessment
Two authors (SF Ji and XD Fan) independently extracted the original data. Disagreement was resolved by discussion. If the two authors could not reach a consensus, the result was reviewed by a third author (XN Ning). The extracted data were consisted of the follow items: the first author’s name, publication year, population (Ethnicity), methods, study design, matching criteria, sex, total number of cases and controls, and age (years). Study quality was assessed by the Newcastle–Ottawa scale (NOS), which uses a ‘‘star’’ rating system to judge the quality of all observational studies. The NOS ranges between zero (worst) up to nine stars (best) and studies with a score equal to or higher than seven were considered to be of high quality. Two investigators (SF Ji and XD Fan) independently assessed the quality of the included studies, and the results were reviewed by a third investigator (J Zhang). Disagreement was resolved by discussion.
Statistical analysis
We utilized Review manager 5.3 and Stata 14.0 software to perform the meta-analysis in the present study. Heterogeneity among studies was assessed by I2 statistic, P < 0.10 and I2 > 50% indicated evidence of heterogeneity. If heterogeneity existed among the studies, the random effects model was used to estimate the pooled standard mean difference (SMD). Otherwise, the fixed effects model was adopted. The standard mean difference (SMD) and corresponding 95% confidence interval (CI) were utilized to assess the associations. The potential publication bias was investigated using Egger’s test and Funnel plot. Egger’s test (P < 0.05) was also considered to be representative of statistically significant publication bias, which was conducted with the Stata14.0 software. Subgroup analysis about study design, location, quality and DR sub-type were performed to further explore the heterogeneity and clinical significance.
Results
Study characteristics
We retrieved a total of 98 studies. After duplicates were removed, only 42 full-text studies were evaluated. After exclusion of review and no-related articles, a total of 14 studies [10–23] were included in the final meta-analysis according to the inclusion criteria, including 2 cross-section studies [10, 14] and 11 case control studies [11–13, 15–23]. There are 1252 cases in the DR group, 1359 cases in T2DM without DR group and 1133 cases in control group. Table 1 shows the characteristics of included studies. Figure 1 shows the process of literature selection. As for the application of anticoagulation methods, ethylenediaminetetraacetic acid (ETDA) was used in 9 literature [11, 13, 15, 16, 18–22], and 5 literature reported the collection and measurement time [18–22]. One literature using citrate [23] and 4 literature have not specifically reported [10, 12, 14, 17].
Table 1.
Characteristics of included studies
| Authors | Location, year | DR | T2DM without DR | Control | -Tubes | NOS | |||
|---|---|---|---|---|---|---|---|---|---|
| N | MPV | N | MPV | N | MPV | ||||
| Yilmaz et al. | Turkey, 2016 | 174 | 8.1 ± 0.83 | 88 | 7.81 ± 0.76 | 85 | 7.42 ± 0.68 | EDTA | 9 |
| Ateş et al. | Turkey, 2009 | 90 | 7.96 ± 0.76 | 30 | 7.52 ± 1.01 | EDTA | 9 | ||
| Dindar et al. | Turkey, 2013 | 24 | 11.26 ± 1.08 | 47 | 10.68 ± 1.68 | 50 | 10.23 ± 1.01 | EDTA | 9 |
| Citirik et al. | Turkey, 2015 | 97 | 8.08 ± 0.71 | 43 | 7.94 ± 0.63 | 40 | 7.74 ± 0.78 | EDTA | 8 |
| Demirtas et al. | Turkey, 2015 | 67 | 9.54 ± 0.88 | 240 | 9.2 ± 0.92 | NR | 8 | ||
| Tetikoglu et al. | Turkey, 2016 | 136 | 8.71 ± 0.82 | 63 | 8.51 ± 1 | 76 | 8.32 ± 0.9 | NR | 7 |
| Müberra et al. | Turkey, 2016 | 120 | 9.6 ± 1 | 158 | 9.7 ± 1.2 | 107 | 9.3 ± 1 | EDTA | 8 |
| Gungor et al. | Turkey, 2016 | 52 | 9.3 ± 1 | 50 | 8.8 ± 1.1 | 50 | 8.3 ± 0.6 | EDTA | 9 |
| Zhong et al. | China, 2011 | 200 | 10.09 ± 0.92 | 100 | 9.46 ± 0.93 | NR | 7 | ||
| Li et al. | China, 2016 | 47 | 10.72 ± 1.57 | 52 | 10.39 ± 0.9 | 48 | 9.75 ± 0.89 | EDTA | 8 |
| Zhou et al. | China, 2016 | 51 | 10.4 ± 1.1 | 328 | 10 ± 1.1 | 96 | 9.1 ± 0.8 | NR | 8 |
| Radha et al. | India, 2016 | 14 | 9.2 ± 0.61 | 30 | 8.39 ± 0.68 | 100 | 8.02 ± 0.86 | EDTA | 8 |
| Buch et al. | India, 2017 | 80 | 11.4 ± 1.96 | 162 | 9.91 ± 1.97 | 200 | 8.48 ± 1.01 | EDTA | 6 |
| Papanas et al. | Greece, 2004 | 167 | 15.8 ± 1.3 | 98 | 10.9 ± 1.1 | 151 | 7.1 ± 1.2 | Citrate | 6 |
DR diabetic retinopathy, T2DM without DR type 2 diabetic mellitus without DR, N number of subjects, MPV mean platelet volume, NOS Newcastle–Ottawa scale, EDTA ethylenediaminetetraacetic acid, NR no report
Fig. 1.

Flow diagram for literature selection
Meta-analysis
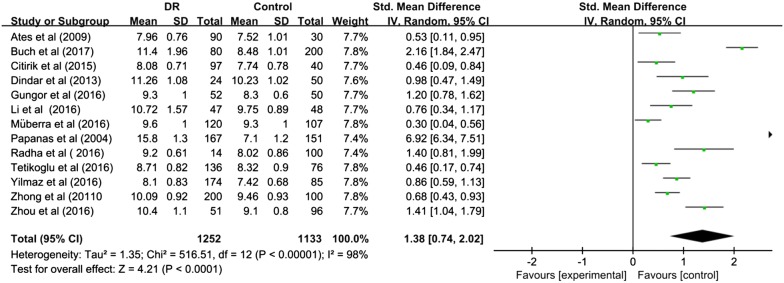
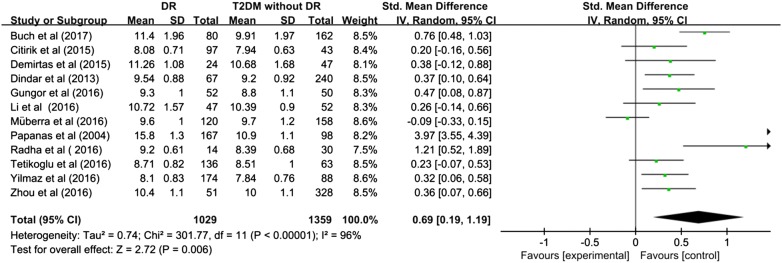
The pooled SMD estimate showed that significant higher value of MPV in DR compared to control group [SMD (95% CI) = 1.38 (0.74, 2.02)] (Fig. 2) and T2DM without DR [SMD (95% CI) = 0.69 (0.19, 1.19)] (Fig. 3). I2 test indicated that the heterogeneity was that I2 = 98% (P < 0.00001) and I2 = 96% (P < 0.00001) respectively, therefore, given the significance, the random-effects model was applied to perform meta-analysis.
Fig. 2.
Meta-analysis for mean platelet volume in DR and control
Fig. 3.
Meta-analysis for mean platelet volume in DR and T2DM without DR
Subgroup analysis
To further explore the origin of heterogeneity and the clinical significance of MPV in assessing severity of DR, subgroups analysis about study design, quality, location and DR sub-type were performed. Unfortunately, we discovered heterogeneity of subgroup was generally high in the comparison to DR and control, low-quality studies in particular, which mean that the origin of heterogeneity was unclear. In the comparison to DR and T2DM without DR, we concluded that study design and low-quality studies generated heterogeneity obviously. Finally, we further explored the association between MPV level and DR type. We found, in terms of MPV level, both NPDR and PDR were significantly higher than control group [SMD (95% CI) = 0.41 (0.16, 0.65) P = 0.81 (0.48, 1.14)], PDR was higher than T2DM without DR [SMD (95% CI) = 0.48 (0.28, 0.68), P = 0.349] and NPDR [SMD (95% CI) = 0.41 (0.17, 0.64)], while NPDR was no difference with T2DM without DR [SMD (95% CI) = 0.04 (− 0.16, 0.24)]. We take gap in time between collection and measuring MPV-60 min to divide into subgroups, and the results showed that (Table 2), when ≤ 60 min, DR vs control, SMD = [0.39 (0.20–0.58), I2 = 0%], DR vs T2DM without DR, SMD = [0.02 (− 0.25 to 0.30), I2 = 43%], obviously the latter results no statistical significance. Then, when > 60 min, DR vs control, SMD = [0.99 (0.67–1.31), I2 = 41%], DR vs T2DM without DR, SMD = [0.37 (0.15–0.58), I2 = 0%], no significant difference appeared. Therefore, study design, low-quality articles, DR type and gap in time between collection and measuring MPV were the sources of heterogeneity, and high MPV level might reflect the severity of DR.
Table 2.
Subgroup analysis of the relation between MPV and DR patients
| Subgroup | Study | No. of studies | SMD | 95% CI | Heterogeneity | |
|---|---|---|---|---|---|---|
| P value | I2 (%) | |||||
| DR vs control | ||||||
| Location | Turkey | 7 | 0.66 | 0.42–0.90 | = 0.003 | 70 |
| China | 3 | 0.94 | 0.49–1.40 | = 0.005 | 81 | |
| India | 2 | 1.82 | 1.09–2.56 | = 0.003 | 70 | |
| Study quality | High | 11 | 0.79 | 0.57–1.01 | < 0.0001 | 76 |
| Low | 2 | 4.53 | − 0.14 to 9.21 | < 0.00001 | 99 | |
| DR vs T2DM without DR | ||||||
| Location | Turkey | 7 | 0.24 | 0.09–0.40 | = 0.11 | 42 |
| China | 2 | 0.33 | 0.09–0.56 | = 0.68 | 0 | |
| India | 2 | 0.87 | 0.49–1.25 | = 0.23 | 30 | |
| Study design | Case–control | 10 | 0.76 | 0.17–1.35 | < 0.00001 | 97 |
| Cross-sectional | 2 | 0.37 | 0.11–0.62 | = 0.95 | 0 | |
| Study quality | High | 10 | 0.30 | 0.15–0.45 | = 0.03 | 51 |
| Low | 2 | 2.36 | − 0.79 to 5.51 | < 0.00001 | 99 | |
| DR sub-type | NPDR vs control | 4 | 0.41 | 0.16–0.65 | = 0.182 | 38.3 |
| PDR vs control | 4 | 0.81 | 0.48–1.14 | = 0.031 | 66.1 | |
| NPDR vs T2DM without DR | 3 | 0.04 | − 0.16 to 0.24 | = 0.642 | 0 | |
| PDR vs T2DM without DR | 3 | 0.48 | 0.28–0.68 | = 0.349 | 5.1 | |
| PDR vs NPDR | 4 | 0.41 | 0.17–0.64 | = 0.193 | 36.6 | |
| Intervalsa | ||||||
| ≤ 60 min | DR vs control | 3 | 0.39 | 0.20–0.58 | = 0.60 | 0 |
| DR vs T2DM without DR | 2 | 0.02 | − 0.25 to 0.30 | = 0.18 | 43 | |
| > 60 min | DR vs control | 2 | 0.99 | 0.67–1.31 | = 0.19 | 41 |
| DR vs T2DM without DR | 2 | 0.37 | 0.15–0.58 | = 0.53 | 0 | |
MPV mean platelet volume, DR diabetic retinopathy, T2DM without DR type 2 diabetic mellitus without diabetic retinopathy, NPDR non-proliferative diabetic retinopathy, PDR proliferative diabetic retinopathy, SMD standard mean difference, CI confidence interval
aIntervals of MPV collection and measurement
Sensitive analysis
The contribution of each study to the pooled estimate was performed in order to assess the sensitivity analysis (Table 3). It was noteworthy that Papanas et al. [23] might cause heterogeneity, which was excluded at a time and recalculated the pooled result. After that, the heterogeneity in DR compared to T2DM without DR was decreased significantly to 66%. Meanwhile, the result was also decreased [SMD (95% CI) = 0.36 (0.19, 0.53)]. Further analysis revealed that the biggest difference between the study on Papanas et al. [23]. and other included literatures lies in the different anticoagulants used in the collection of platelet sample tubes. Only Papanas et al. [23] used citrate and the results didn’t change significantly after excluding Papanas et al. [DR vs control, SMD = 0.92 (0.60–1.24), I2 = 90%, DR vs T2DM without DR, SMD = 0.36 (0.19–0.53), I2 = 66%], which were considered as final results. Finally, the results of two comparisons exhibited that our meta-analysis was reliable, without inverse changes appearing.
Table 3.
Sensitivity analysis (leave-one-out approach to) for MPV in DR
| Study | SMD | 95% CI | P value | I2 (%) |
|---|---|---|---|---|
| DR vs control | ||||
| Ates et al. | 1.45 | 0.76–2.13 | < 0.00001 | 98 |
| Buch et al. | 1.31 | 0.65–1.98 | < 0.00001 | 98 |
| Citirik et al. | 1.46 | 0.77–2.14 | < 0.00001 | 98 |
| Dindar et al. | 1.41 | 0.73–2.09 | < 0.00001 | 98 |
| Gungor et al. | 1.39 | 0.71–2.08 | < 0.00001 | 98 |
| Li et al. | 1.43 | 0.74–2.12 | < 0.00001 | 98 |
| Müberra et al. | 1.47 | 0.77–2.17 | < 0.00001 | 98 |
| Papanas et al. | 0.92 | 0.60–1.24 | < 0.00001 | 90 |
| Radha et al. | 1.38 | 0.70–2.05 | < 0.00001 | 98 |
| Tetikoglu et al. | 1.46 | 0.76–2.16 | < 0.00001 | 98 |
| Yilmaz et al. | 1.42 | 0.71–2.14 | < 0.00001 | 98 |
| Zhong et al. | 1.44 | 0.72–2.16 | < 0.00001 | 98 |
| Zhou et al. | 1.38 | 0.68–2.07 | < 0.00001 | 98 |
| DR vs T2DM without DR | ||||
| Buch et al. | 0.69 | 0.13–1.24 | < 0.00001 | 97 |
| Citirik et al. | 0.74 | 0.20–1.28 | < 0.00001 | 97 |
| Demirtas et al. | 0.72 | 0.19–1.25 | < 0.00001 | 97 |
| Dindar et al. | 0.72 | 0.17–1.28 | < 0.00001 | 97 |
| Gungor et al. | 0.71 | 0.17–1.25 | < 0.00001 | 97 |
| Li et al. | 0.73 | 0.20–1.27 | < 0.00001 | 97 |
| Müberra et al. | 0.77 | 0.23–1.31 | < 0.00001 | 96 |
| Papanas et al. | 0.36 | 0.19–0.53 | = 0.001 | 66 |
| Radha et al. | 0.65 | 0.13–1.17 | < 0.00001 | 97 |
| Tetikoglu et al. | 0.74 | 0.19–1.29 | < 0.00001 | 97 |
| Yilmaz et al. | 0.73 | 0.17–1.29 | < 0.00001 | 97 |
| Zhou et al. | 0.72 | 0.17–1.28 | < 0.00001 | 97 |
Publication bias
The publication bias was evaluated using funnel plot and egger test. There was no publication bias existing in MPV level with DR compared to control group (Egger’s P = 0.36) and T2DM without DR group (Egger’s P = 0.15). The funnel plots were shown in Figs. 4 and 5 respectively.
Fig. 4.
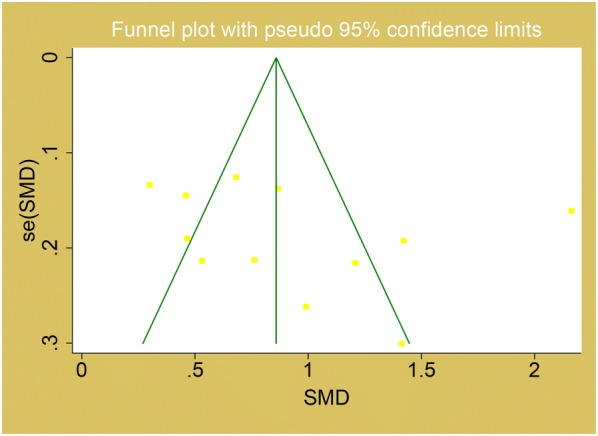
Funnel plot for MPV in the comparison of DR and control
Fig. 5.
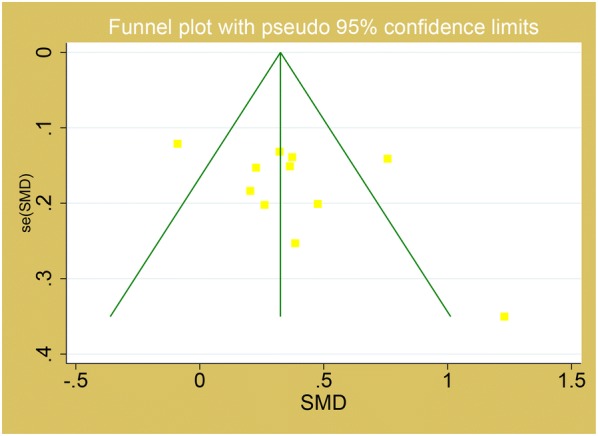
Funnel plot for MPV in the comparison of DR and T2DM without DR
Discussion
To our knowledge, this is the first study that systematically reviews and summarizes through a meta-analysis to explore the relationship between platelet parameters and DR. Our results evidenced statistically significantly higher values of MPV in DR compared with T2DM without DR and health.
Platelets were one of the causes of capillary nonperfusion in diabetes. Qualitative abnormalities and activation of platelet in DM have been reported [24], which has a close relationship with insulin resistance, hyperglycemia, and dyslipidemia [25, 26]. Larger platelets are more active because of elevated prothrombic contents, such as thromboxane A2, thromboxane B2, platelet factor 4, serotonin, and platelet-derived growth factor (PDGF) [27]. Some studies revealed that platelet participated in development of DR by thrombogenesis with microvascular lesions [12], and so far, the specific mechanisms of platelets in DR focuses on platelet-derived growth factor (PDGF), which is released from platelets. Eng et al. [28] reached a conclusion that pericyte loss caused by PDGF-B may also be a causal pathogenic event in human DR. Yokota et al. [29] found that hyperglycemia can increase PDGF-B levels in the retina, which mediated via PDGF-β receptors in part by protein kinase C (PKC) activation to upregulate expression of an essential factor endothelin-1 (ET-1) participated in pathophysiology of DR. Geraldes et al. [30] further found hyperglycemia persistently activated PKCδ and p38α MAPK to increase the expression of a novel target, Scr homology-2 domain containing phosphatase-1 (SHP-1), leading to PDGF receptor-β dephosphorylation and actions, and increased pericyte apoptosis, independent of NF-κB, and Chen et al. [31] reached the similar conclusion. Praidou et al. [32] discovered the correlation between PDGF and NPDR, and topical ketorolac tromethamine to treat PDR caused PDGF levels to decrease [33]. Therefore, platelets play an important role in formation of DR. However, clopidogrel (the selective antiplatelet drug), did not prevent neuronal apoptosis, glial reactivity, capillary cell apoptosis, or acellular capillaries in retinas of diabetic rats [34], suggesting that platelet do not initiate the pathology of early diabetic retinopathy.
MPV is positively correlated with platelet adhesion and aggregation, the higher level MPV, the higher rate and stronger function of platelets. Recent research found that MPV was strongly and independently associated with the presence and severity of diabetes [35], and there were great significance of cardio-vascular complications in diabetes mellitus [36], which may be associated with osmotic change [37]. Taurine is a key compound in osmoregulation, which plays an important role in maintaining cell volume [38, 39]. Taurine is found in high concentration in platelets [40], the level of which in platelets decreases during diabetes, and a clinical study involving oral administration of taurine to diabetes patients showed that the platelet hyperaggregation could be normalised [41, 42]. Therefore, increased MPV in patients with diabetic retinopathy may be associated with decreased taurine levels. Furthermore, a study in diabetic rats with an aldose reductase inhibitor showed that polyol pathway activity is involved in the hyperaggregability of platelets [43]. High plasma glucose could increase the intracellular glucose level, which leads to abnormal activation of aldose reductase, a key enzyme in the polyol pathway, reducing glucose to sorbitol [44, 45]. Sorbitol is a polyhydroxy alcohol, hydrophilic, not easy to penetrate the cell membrane, accumulating intracellularly with possible osmotic consequences [44]. The accumulation of sorbitol causes depletion of other osmolytes, such as taurine, causing dysfunction of cell volume regulation [46]. Retinal microvascular lesion of DR is characterized by thickening and microthrombosis of capillary base, and platelet dysfunction has an important influence on development of microvascular complications. The larger MPV, the more likely formation of thrombosis, and in other hand, vascular endothelial injury triggers platelet adhesion and aggregation to accelerate thrombosis. Subgroup analysis exhibited MPV level in NPDR was no difference with T2DM without DR, but in PDR was higher than both of them, which was consistent with theory that platelets do not initiate the pathology of early DR. We reached conclusions that DR grade resulted in the heterogeneity and MPV level was also upregulated in higher DR severity. In addition, in the pooled analysis of MPV, we discovered the heterogeneity was decreased significantly after excluding Papanas et al. [23]. What is special about this article is that only citrate is used in it, while other included articles using EDTA. Citrate is mainly used for hemostasis test and blood sedimentation test. Because its toxicity is small, also used in blood transfusion maintenance fluid. The anticoagulant mechanism is that citrate forms a soluble chelate with calcium ions in blood to prevent blood coagulation. However, the coagulation time of plasma from different sources of thrombin reagents can vary greatly for the same normal person or patient. The results did not change significantly after excluding it, so we took the results of exclusion. We hold the view that the reason why T2DM without DR patients of it might arise from other potential complications affecting real result of MPV, such as nephropathy [15]. However, the final result of MPV didn’t change, which suggested the reliability of our results. There were some articles reporting the relationship between other hematological indicators and diabetic retinopathy, such as NLR [47, 48]. A latest systematic review reported, similar to MPV, higher level NLR appears in DR compared to control and T2DM without DR [49], which may be useful for monitoring DR when combined with MPV.
Of course, there were some limits in our article. First of all, the definition and diagnosis of T2DM without DR and DR were not consistent completely. All of our included studies were case–control or cross-sectional studies, so we couldn’t suppress interference of other non-matched factors. Only English language was included in this meta-analysis, so some eligible studies, which were unpublished or reported in other languages, were likely missed. The intervals of MPV collection and measurement are not completely consistent. Some diabetes-related factors, such as glycaemic control, duration of diabetes and kidney complications, were difficult to be corrected. In addition, many studies have reported that drugs, including statins and metformin, also could affect platelets [50–54], but none of the included articles mentioned patients’ medication status. All the factors mentioned above may be sources of heterogeneity, which should be paid attention to in future research design.
Conclusions
Fortunately, higher values of MPV in DR vs T2DM without DR were exhibited, hence, we concluded that platelets have a closed relationship with DR. MPV is easily accessible platelet volume parameters and reflect function of platelet, so it will be of great significance if we can monitor the development and progression of DR with it. Given the significance of MPV in DR grade, we need to attach importance to MPV in the development of DR. Taking account of the limits in this study, more rigorous and high-quality researches need to be implemented to further confirm our conclusions.
Authors’ contributions
SJ and JZ conceived and designed the methods, extracted the original data and drafted the manuscript. SJ, XF, XW, BZ and HS performed statistical analysis. JZ and XN interpreted results. HY revised the manuscript. HY had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of data analysis. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated or analyzed during this study are included in this article.
Consent for publication
Not applicable.
Ethics approval and consent to participate
All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
Funding
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- MPV
mean platelet volume
- DR
diabetic retinopathy
- T2DM without DR
type 2 diabetes mellitus without diabetic retinopathy
- PDR
proliferative diabetic retinopathy
- NPDR
non-proliferative diabetic retinopathy
- NOS
Newcastle–Ottawa scale
- SMD
standard mean difference
- CI
confidence interval
References
- 1.Adamis AP. Is diabetic retinopathy an inflammatory disease? Brit J Ophthalmol. 2002;4:363–365. doi: 10.1136/bjo.86.4.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Higgins JPT. Cochrane handbook for systematic reviews of interventions. Chichester: Wiley-Blackwell; 2008. [Google Scholar]
- 3.Mehuys E, De Bolle L, Van Bortel L, Annemans L, Van Tongelen I, Remon JP, Giri M. Medication use and disease management of type 2 diabetes in Belgium. Pharm World Sci. 2008;30:51–56. doi: 10.1007/s11096-007-9140-0. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg RB. Cytokine and cytokine-like inflammation markers, endothelial dysfunction, and imbalanced coagulation in development of diabetes and its complications. J Clin Endocrinol Metab. 2009;9:3171–3182. doi: 10.1210/jc.2008-2534. [DOI] [PubMed] [Google Scholar]
- 5.Hekimsoy Z, Payzin B, Ornek T, Kandogan G. Mean platelet volume in Type 2 diabetic patients. J Diabetes Complicat. 2004;18:173–176. doi: 10.1016/S1056-8727(02)00282-9. [DOI] [PubMed] [Google Scholar]
- 6.Vinik AI, Erbas T, Park TS, Nolan R, Pittenger GL. Platelet dysfunction in type 2 diabetes. Diabetes Care. 2001;24:1476–1485. doi: 10.2337/diacare.24.8.1476. [DOI] [PubMed] [Google Scholar]
- 7.Kodiatte T, Rao S, Manikyam U, Reddy M, Lakshmaiah V, Jagadish T, Lingaiah HK. Mean platelet volume in type 2 diabetes mellitus. J Lab Physicians. 2012;4:5. doi: 10.4103/0974-2727.98662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abali G, Akpinar O, Soylemez N. Correlation of the coronary severity scores and mean platelet volume in diabetes mellitus. Adv Ther. 2014;31:140–148. doi: 10.1007/s12325-013-0081-9. [DOI] [PubMed] [Google Scholar]
- 9.Endler G, Klimesch A, Sunder-Plassmann H, Schillinger M, Exner M, Mannhalter C, Jordanova N, Christ G, Thalhammer R, Huber K, Sunder-Plassmann R. Mean platelet volume is an independent risk factor for myocardial infarction but not for coronary artery disease. Br J Haematol. 2002;117:399–404. doi: 10.1046/j.1365-2141.2002.03441.x. [DOI] [PubMed] [Google Scholar]
- 10.Zhou XY, Liu Q, Bai HL, Liang L. Clinical significance of mean platelet volume and neutrophil-to-lymphocyte ratio in patients with diabetic retinopathy. Int Eye Sci. 2016;16:981–983. [Google Scholar]
- 11.Li S, Cao W, Sun X. Role of platelet parameters on neovascular glaucoma, A retrospective case–control study in China. PLoS ONE. 2016;11:e166893. doi: 10.1371/journal.pone.0166893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhong ZL, Han M, Chen S. Risk factors associated with retinal neovascularization of diabetic retinopathy in type 2 diabetes mellitus. Int J Ophthalmol. 2011;4:182–185. doi: 10.3980/j.issn.2222-3959.2011.02.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buch A, Kaur S, Nair R, Jain A. Platelet volume indices as predictive biomarkers for diabetic complications in type 2 diabetic patients. J Lab Physicians. 2017;9:84–88. doi: 10.4103/0974-2727.199625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Demirtas L, Degirmenci H, Akbas EM, Ozcicek A, Timuroglu A, Gurel A, Ozcicek F. Association of hematological indicies with diabetes, impaired glucose regulation and microvascular complications of diabetes. Int J Clin Exp Med. 2015;7:11420–11427. [PMC free article] [PubMed] [Google Scholar]
- 15.Radha RK, Selvam D. MPV in uncontrolled & controlled diabetics- its role as an indicator of vascular complication. J Clin Diagn Res. 2016;10:EC22–EC26. doi: 10.1111/crj.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dindar S, Cinemre H, Sengul E, Annakkaya AN. Mean platelet volume is associated with glycaemic control and retinopathy in patients with type 2 diabetes mellitus. West Indian Med J. 2013;62:519–523. doi: 10.7727/wimj.2012.284. [DOI] [PubMed] [Google Scholar]
- 17.Tetikoglu M, Aktas S, Sagdik HM, Yigitoglu ST, Ozcura F. Mean platelet volume is associated with diabetic macular edema in patients with type-2 diabetes mellitu. Semin Ophthalmol. 2017;32:651–654. doi: 10.3109/08820538.2016.1157612. [DOI] [PubMed] [Google Scholar]
- 18.Müberra A, Yasemin UB, Kagan H. The association of hematologic inflammatory markers with atherogenic index in type 2 diabetic retinopathy patients. Clin Ophthalmol. 2016;10:1797–1801. doi: 10.2147/OPTH.S110749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Güngör AA, Gürsoy G, Güngör F, Bayram SM, Atalay E. The relationship of mean platelet volume with retinopathy in type 2 diabetes mellitus. Turk J Med Sci. 2016;46:1292–1299. doi: 10.3906/sag-1410-95. [DOI] [PubMed] [Google Scholar]
- 20.Yilmaz T, Yilmaz A. Relationship between altered platelet morphological parameters and retinopathy in patients with type 2 diabetes mellitus. J Ophthalmol. 2016;2016:1–5. doi: 10.1155/2016/9213623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Citirik M, Beyazyildiz E, Simsek M, Beyazyildiz O, Haznedaroglu IC. MPV may reflect subcinical platelet activation in diabetic patients with and without diabetic retinopathy. Eye (Lond) 2015;29:376–379. doi: 10.1038/eye.2014.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ate O, Kiki L, Bilen H, Kele M, Koçer İ, Kulaçoğlu DN, Baykal O. Association of mean platelet volume with the degree of retinopathy in patients with diabetes mellitus. Eur J Gen Med. 2009;9:99–102. [Google Scholar]
- 23.Papanas N, Symeonidis G, Maltezos E, Mavridis G, Karavageli E, Vosnakidis T, Lakasas G. Mean platelet volume in patients with type 2 diabetes mellitus. Platelets. 2009;15:475–478. doi: 10.1080/0953710042000267707. [DOI] [PubMed] [Google Scholar]
- 24.El HM, Rosado JA. Platelet signalling abnormalities in patients with type 2 diabetes mellitus: a review. Blood Cells Mol Dis. 2008;41:119–123. doi: 10.1016/j.bcmd.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 25.Kim JH, Bae HY, Kim SY. Response: clinical marker of platelet hyperreactivity in diabetes mellitus. Diabetes Metab J. 2014;38:160–161. doi: 10.4093/dmj.2014.38.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suslova TE, Sitozhevskii AV, Ogurkova ON, Kravchenko ES, Kologrivova IV, Anfinogenova Y, Karpov RS. Platelet hemostasis in patients with metabolic syndrome and type 2 diabetes mellitus: CGMP- and NO-dependent mechanisms in the insulin-mediated platelet aggregation. Front Physiol. 2015;5:501. doi: 10.3389/fphys.2014.00501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des. 2011;17:47–58. doi: 10.2174/138161211795049804. [DOI] [PubMed] [Google Scholar]
- 28.Enge M, Bjarnegard M, Gerhardt H, Gustafsson E, Kalen M, Asker N, Hammes HP, Shani M, Fassler R, Betsholtz C. Endothelium-specific platelet-derived growth factor-B ablation mimics diabetic retinopathy. EMBO J. 2002;21:4307–4316. doi: 10.1093/emboj/cdf418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yokota T, Ma RC, Park JY, Isshiki K, Sotiropoulos KB, Rauniyar RK, Bornfeldt KE, King GL. Role of protein kinase C on the expression of platelet-derived growth factor and endothelin-1 in the retina of diabetic rats and cultured retinal capillary pericytes. Diabetes. 2003;52:838–845. doi: 10.2337/diabetes.52.3.838. [DOI] [PubMed] [Google Scholar]
- 30.Geraldes P, Hiraoka-Yamamoto J, Matsumoto M, Clermont A, Leitges M, Marette A, Aiello LP, Kern TS, King GL. Activation of PKC-delta and SHP-1 by hyperglycemia causes vascular cell apoptosis and diabetic retinopathy. Nat Med. 2009;15:1298–1306. doi: 10.1038/nm.2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen Y, Wang W, Liu F, Tang L, Tang R, Li W. 9-Cis-retinoic acid improves sensitivity to platelet-derived growth factor-BB via RXRalpha and SHP-1 in diabetic retinopathy. Biochem Biophys Res Commun. 2015;465:810–816. doi: 10.1016/j.bbrc.2015.08.093. [DOI] [PubMed] [Google Scholar]
- 32.Praidou A, Papakonstantinou E, Androudi S, Georgiadis N, Karakiulakis G, Dimitrakos S. Vitreous and serum levels of vascular endothelial growth factor and platelet-derived growth factor and their correlation in patients with non-proliferative diabetic retinopathy and clinically significant macula oedema. Acta Ophthalmol. 2011;89:248–254. doi: 10.1111/j.1755-3768.2009.01661.x. [DOI] [PubMed] [Google Scholar]
- 33.Schoenberger SD, Kim SJ, Shah R, Sheng J, Cherney E. Reduction of interleukin 8 and platelet-derived growth factor levels by topical ketorolac, 0.45%, in patients with diabetic retinopathy. JAMA Ophthalmol. 2014;132:32–37. doi: 10.1001/jamaophthalmol.2013.6203. [DOI] [PubMed] [Google Scholar]
- 34.Antonetti DA, Barber AJ, Khin S, Lieth E, Tarbell JM, Gardner TW. Vascular permeability in experimental diabetes is associated with reduced endothelial occludin content: vascular endothelial growth factor decreases occludin in retinal endothelial cells. Penn State Retina Research Group. Diabetes. 1998;47:1953–1959. doi: 10.2337/diabetes.47.12.1953. [DOI] [PubMed] [Google Scholar]
- 35.Shah B, Sha D, Xie D, Mohler ER, Berger JS. The relationship between diabetes, metabolic syndrome, and platelet activity as measured by mean platelet volume: the national health and nutrition examination survey, 1999–2004. Diabetes Care. 2012;35:1074–1078. doi: 10.2337/dc11-1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Han JY, Choi DH, Choi SW, Kim BB, Ki YJ, Chung JW, Koh YY, Chang KS, Hong SP. Stroke or coronary artery disease prediction from mean platelet volume in patients with type 2 diabetes mellitus. Platelets. 2013;24:401–406. doi: 10.3109/09537104.2012.710858. [DOI] [PubMed] [Google Scholar]
- 37.Gende OA. Effect of hyperosmolarity on agonist-induced increases of intracellular calcium in human platelets. Thromb Res. 2003;110:33–37. doi: 10.1016/S0049-3848(03)00289-5. [DOI] [PubMed] [Google Scholar]
- 38.Pasentes-Morales H, Schousboe A. Role of taurine in osmoregulation in brain cells: mechanisms and functional implications. Amino Acids. 1997;12:281–292. doi: 10.1007/BF01373008. [DOI] [Google Scholar]
- 39.Lang F, Busch GL, Ritter M, Volkl H, Waldegger S, Gulbins E, Ussinger DH. Functional significance of cell volume regulatory mechanisms. Physiol Rev. 1998;78:247–306. doi: 10.1152/physrev.1998.78.1.247. [DOI] [PubMed] [Google Scholar]
- 40.Jacobsen JG, Smith LH. Biochemistry and physiology of taurine and taurine derivatives. Physiol Rev. 1968;48:424–511. doi: 10.1152/physrev.1968.48.2.424. [DOI] [PubMed] [Google Scholar]
- 41.Franconi F, Bennardini F, Mattana A, Miceli M, Ciuti M, Mian M, Gironi A, Anichini R, Seghieri G. Plasma and platelet taurine are reduced in subjects with insulin-dependent diabetes mellitus: effects of taurine supplementation. Am J Clin Nutr. 1995;61:1115–1119. doi: 10.1093/ajcn/61.5.1115. [DOI] [PubMed] [Google Scholar]
- 42.Franconi F, Miceli M, Fazzini A, Seghieri G, Caputo S, DiLeo MA, Lepore D, Ghirlanda G. Taurine and diabetes—humans and experimental models. Adv Exp Med Biol. 1996;403:579–582. doi: 10.1007/978-1-4899-0182-8_62. [DOI] [PubMed] [Google Scholar]
- 43.Hara T, Nakamura J, Koh N, et al. An aldose reductase inhibitor, TAT, prevented hyperaggregation in diabetic rats. In: Hotta N, Greene DA, Ward JD, Sima AAF, Boulton AJM, et al., editors. Diabetic neuropathy: new concepts and insights. Amsterdam: Excerpta medica; 1995. pp. 137–141. [Google Scholar]
- 44.Gabbay KH. The sorbitol pathway and the complications of diabetes. N Engl J Med. 1973;288:831–836. doi: 10.1056/NEJM197304192881609. [DOI] [PubMed] [Google Scholar]
- 45.Oates PJ. The polyol pathway and diabetic peripheral neuropathy. In: Tomlinson DR, editor. Neurobiology of diabetic neuropathy. London: International Review of Neurobiology, Academic Press; 2002. pp. 325–392. [DOI] [PubMed] [Google Scholar]
- 46.Burg MB, Kador PF. Sorbitol, osmoregulation and the complications of diabetes. J Clin Invest. 1988;81:635–640. doi: 10.1172/JCI113366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Öztürk ZA, Kuyumcu ME, Yesil Y, Savas E, Yildiz H, Kepekçi Y, Arioğul S. Is there a link between neutrophil-lymphocyte ratio and microvascular complications in geriatric diabetic patients? J Endocrinol Invest. 2013;36:593–599. doi: 10.3275/8894. [DOI] [PubMed] [Google Scholar]
- 48.Wang RT, Zhang JR, Li Y, Liu TM, Yu KJ. Neutrophil–lymphocyte ratio is associated with arterial stiffness in diabetic retinopathy in type 2 diabetes. J Diabetes Complicat. 2015;29:245–249. doi: 10.1016/j.jdiacomp.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 49.Ji SF, Ning XN, Zhang J. Neutrophil to lymphocyte ratio for diagnosis of diabetic retinopathy: a meta-analysis. Ophthalmol China. 2018;27:442–446. [Google Scholar]
- 50.Xian-Yu JB, Feng JF, Chen YC, Yang YW. Effects of simvastatin and atorvastatin on biochemical and hematological markers in patients with risk of cardiovascular diseases. Int J Clin Exp Med. 2015;8:13983–13989. [PMC free article] [PubMed] [Google Scholar]
- 51.Papanas N, Maltezos E. Rosuvastatin and mean platelet volume in diabetes. Angiology. 2016;67:113–115. doi: 10.1177/0003319715591743. [DOI] [PubMed] [Google Scholar]
- 52.Kucera M, Balaz D, Kruzliak P, Ciccocioppo R, Oravec S, Rodrigo L, Zulli A, Hirnerova E, Sabaka P, Komornikova A, Sabo J, Slezak P, Gaspar L. The effects of atorvastatin treatment on the mean platelet volume and red cell distribution width in patients with dyslipoproteinemia and comparison with plasma atherogenicity indicators—a pilot study. Clin Biochem. 2015;48:557–561. doi: 10.1016/j.clinbiochem.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 53.Sivri N, Tekin G, Yalta K, Aksoy Y, Senen K, Yetkin E. Statins decrease mean platelet volume irrespective of cholesterol lowering effect. Kardiol Pol. 2013;71:1042–1047. doi: 10.5603/KP.2013.0259. [DOI] [PubMed] [Google Scholar]
- 54.Dolasik I, Sener SY, Celebi K, Aydin ZM, Korkmaz U, Canturk Z. The effect of metformin on mean platelet volume in diabetic patients. Platelets. 2013;24:118–121. doi: 10.3109/09537104.2012.674165. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article.