Abstract
OBJECTIVE
To assess proportionate mortality ratios (PMRs) for suicide among male and female US veterinarians from 1979 through 2015.
DESIGN
PMR study.
SAMPLE
Death records for 11,620 veterinarians.
PROCEDURES
Information for veterinarians who died during 1979 through 2015 was obtained from AVMA obituary and life insurance databases and submitted to a centralized database of US death records to obtain underlying causes of death. Decedent data that met records-matching criteria were imported into a software program for calculation of PMRs for suicide stratified by sex and indirectly standardized for age, race, and 5-year calendar period with 95% confidence intervals.
RESULTS
398 deaths resulted from suicide; 326 (82%) decedents were male, 72 (18%) were female, and most (298 [75%]) were ≤ 65 years of age. The PMRs for suicide for all veterinarian decedents (2.1 and 3.5 for males and females, respectively), those in clinical positions (2.2 and 3.4 for males and females, respectively), and those in nonclinical positions (1.8 and 5.0 for males and females, respectively) were significantly higher than for the general US population. Among female veterinarians, the percentage of deaths by suicide was stable from 2000 until the end of the study, but the number of such deaths subjectively increased with each 5-year period.
CONCLUSIONS AND CLINICAL RELEVANCE
Results of the study indicated that PMRs for suicide of female as well as male veterinarians were higher than for the general population. These data may help to inform stakeholders in the creation and implementation of suicide prevention strategies designed for veterinarians. (J Am Vet Med Assoc 2019;254:104–112)
A higher-than-expected number of deaths from suicide among veterinarians has been described in multiple studies1–8 from Australia, Norway, and the United Kingdom. In 1982, investigations of deaths due to any cause for US veterinarians who died during the years 1947 through 1977 found that the PMR for suicide among white male veterinarians was 1.7 times that of the general US population.9,10 Another study11 of male and female veterinarians in California who died during 1960 through 1992 determined the PMR for suicide among California veterinarians was 2.6 times that of the general population.
Evidence from surveys of veterinarians also suggests veterinarians have a higher risk of suicide, compared with the general population. In 2014, a survey of 11,627 US veterinarians found 9% had current serious psychological distress, 31% had experienced depressive episodes, and 17% had experienced suicidal ideation since leaving veterinary school12; each of these is a risk factor for suicide13,14 and each was more prevalent than in the general population.15,16 Other regional surveys supported these findings by describing higher levels of anxiety, depression, and compassion fatigue among veterinarians, compared with US regional populations.17–23 Furthermore, a study24 of veterinary surgeons from the United Kingdom found higher levels of anxiety, depression, and suicidal thoughts, compared with the general population.
The 1982 study10 of deaths among US veterinarians included only males, and most of those veterinarians practiced food animal medicine. However, the demographics in the veterinary profession have changed substantially over the past 3 decades. Beginning in the late 1980s, the number of female veterinary students began exceeding the number of male veterinary students.25 In 2017, over 60% of 110,531 US veterinarians were female, and in 2016, approximately 80% of students enrolled at US veterinary medical colleges were female.25,26 Additionally, in the past 50 years, society has moved away from an agriculture-based culture, and companion animals have become increasingly popular.27,28 Since 2007, the number of companion animal practitioners has steadily increased.26 In 2017, > 75% of US veterinarians practicing clinical medicine worked exclusively or predominantly in companion animal medicine.26
Understanding the PMRs for suicide among male and female US veterinarians in the context of the changing demographics and species specialization in the veterinary profession could help inform suicide prevention activities as part of a profession-wide and comprehensive suicide prevention strategy. The purpose of the study reported here was to conduct an updated assessment of PMRs for suicide among male US veterinarians and, for the first time to the authors’ knowledge, to investigate PMRs for suicide among female US veterinarians.
Materials and Methods
Data sources
The AVMA maintains records of deceased US veterinarians with data obtained through obituary information submitted to the JAVMA, settlements on life insurance policies obtained through AVMA membership, and computerized (internet) searches for veterinarian obituary information. By use of these resources, > 13,000 US veterinarians who died during 1979 through 2015 were identified. For most veterinarian decedents, available AVMA data included first, middle, and last names; date of birth; state of birth; date of death; state of death; sex; race; membership status (eg, member or nonmember); name of veterinary school and graduation date; primary employment facility type (eg, general practice, academic, industry, or government); primary function performed (eg, clinical medicine, teaching, research, or regulatory work); and primary species treated. These decedents were classified as having a clinical occupational position type if the AVMA listed their employment facility type as general practice or their primary function performed as clinical medicine. The species specialization for decedents was determined according to AVMA market research statistics definitions for primary species treated as follows: companion animal (exclusive [≥ 90% of contact is with canine, feline, nonpoultry avian, and exotic species] or predominant [≥ 50% contact is with the aforementioned species]), food animal (exclusive [≥ 90% of contact is with bovine, porcine, ovine, caprine, camelid, cervid, and poultry species] or predominant [≥ 50% of contact is with the aforementioned species]), mixed animal (varied species contact, with ≥ 25% from companion animal and 25% from either food animal species or equids), and equine (combination of equine predominant and exclusive where ≥ 50% of contact is with equine patients).26 Species specialization was not limited to veterinarians in clinical practice.
The NDI is a centralized database administered by the US CDC National Center for Health Statistics that includes all death records maintained by individual state vital statistics centers since 1979. Information on decedents from all states are added to the NDI each year following a 12-month delay. This database is considered the most complete death-records resource in the United States, and it is designed to assist with obtaining death records for epidemiological research.29 Decedent information was submitted to the NDI to retrieve each decedent’s underlying cause of death.
Case selection
Records were reviewed by 3 authors (SET, EDFL, and RJN) to identify US veterinarians who died between January 1, 1979, and December 31, 2015, and had minimum data available to meet NDI search requirements (full name and birth month and year). Decedents were excluded if the inclusion criteria were not met (eg, non-veterinarians, those who died before or after the study period, or those for which missing information such as date of birth could not be located through public resources). An additional subset of decedents (< 2%) was excluded through a simple random selection process (survey selection procedure)a to meet project financial restrictions, and the remaining dataset was prepared according to NDI specifications through use of a standard statistical software programa and submitted to the NDI. Final decedent matches were selected by evaluation of the NDI’s probabilistic score, which is a number calculated through a 2-step process to determine the amount of agreement between user-submitted data and the NDI record.29 The goal of the NDI probabilistic scoring technique is to determine which matches have the highest probability of being true matches.29
The LTASb program developed by the National Institute for Occupational Safety and Health was used to compare causes of death among veterinarians with the general US population.30 The LTAS requires underlying cause of death and exposure start date (assumed in this study to be the year of veterinary school graduation) for all decedents, and records not meeting these criteria were excluded. Decedent age categories were assigned by the LTAS software for calculation of PMRs and comparison with the general population. Deaths caused by suicide were identified according to the World Health Organization’s ICD coding system.31,32 The ICD codes from the ninth (E950 through E959)31 and tenth (U03 and X60 through X84)32 revisions were used for deaths that occurred during 1979 through 1998 and 1999 through 2015, respectively.
Statistical analysis
Because information on nondecedent veterinarian populations from 1979 through 2015 (the total population at-risk for dying from suicide) was unknown, PMRs were calculated instead of standardized mortality ratios. Results were calculated and stratified by sex by use of the LTAS, which indirectly standardizes for age, race, and 5-year calendar period on the basis of National Center for Health Statistics data from the general US population.30,33 The LTAS calculates PMRs by dividing the observed number of deaths from a specific cause in the decedent population by the expected number of deaths from a specific cause. For PMRs, the expected number of deaths from a specific cause is calculated by multiplying the total decedent population by the proportion of US deaths from a specific cause.30,34 Therefore, PMR calculations relate a specific cause of death to all other causes within the decedent population. A PMR value > 1.00 indicates that the proportion of deaths from the specific cause (suicide in the present study) is greater than expected.34 The LTAS calculates P values (< 0.05 or < 0.01) and 95% CIs on the basis of an assumed Poisson distribution; values of P < 0.05 were considered significant.30 Cell sizes of < 5 were suppressed to comply with NDI data presentation requirements. Odds ratios with 95% CIs were calculated to assess the association between reported method of suicide as indicated by ICD codes and occupational position type by sex. Comparisons among calendar periods were descriptive.
Results
Case selection and demographics
The initial records search identified 13,469 US veterinarians who died during the study period (Figure 1). After exclusions were applied, data for 12,501 decedents were submitted to the NDI, and of these, 11,648 were matched to a single NDI record and selected. Of 11,620 decedents with sufficient data for LTAS analysis, 398 (3%) had death certificates that reported the underlying cause of death as suicide; 326 (82%) were male and 72 (18%) were female, and 298 (75%) died at ≤ 65 years of age (working age). The median age at death by suicide was 57 years (range, 26 to 96 years) for males and 42 years (range, 26 to 81 years) for females; most female decedents (45/72 [63%]) were 25 to 44 years of age, whereas the greatest proportion of male decedents (148/326 [45%]) was 45 to 64 years of age (Table 1).
Figure 1—
Flow diagram depicting selection, inclusion, and exclusion of records for use in a study to assess PMRs for suicide among male and female veterinarians in the United States from 1979 through 2015. The initial dataset for deceased US veterinarians was collected by examination of records for obituary information submitted to the JAVMA, terminated life insurance policies obtained through AVMA membership, and computerized searches for obituaries of veterinarians. For study purposes, the date of graduation from veterinary school was considered the exposure start date.
Table 1—
Characteristics of 398 veterinarians who died by suicide during the years 1979 through 2015.
| Variable | Males (n = 326) | Females (n = 72) | Total (n = 398) |
|---|---|---|---|
| Age at death (y) | |||
| 25–14 | 74 (23) | 45 (63) | 119 (30) |
| 45–64 | 148 (45) | ≥ 5 (—) | ≥ 148 (—) |
| ≥ 65 | 104 (32) | < 5 (—) | ≥ 104 (—) |
| Position type* | |||
| Clinical | 261 (80) | 52 (72) | 313 (79) |
| Nonclinical | 56 (17) | 11 (15) | 67 (17) |
| Species specialization† | |||
| Companion animal | 174 (53) | 52 (72) | 226 (57) |
| Food animal | ≥ 5 (—) | < 5 (—) | 44 (11) |
| Mixed animal | ≥ 5 (—) | < 5 (—) | 19 (5) |
| Equine | ≥ 5 (—) | < 5 (—) | 9 (2) |
| Other | < 5 (—) | < 5 (—) | < 5 (—) |
| None–not listed | 86 (26) | 12 (17) | 98 (25) |
Data are shown as number (%). Data for cell sizes < 5 and data reported as minimum rather than exact values were suppressed to comply with the NDI data reporting requirements.
Occupational positions for 18 decedents (9 male and 9 female veterinarians) were classified as unknown.
Species specialization was classified according to AVMA market research statistics definitions26; not all individuals with species specialization were in clinical practice.
— = Percentages not calculated for compliance with NDI data reporting rules.
See Figure 1 for information on dataset selection.
Of the 398 veterinarians who died by suicide, 313 (79%) had an occupational position classified as clinical. Sixty-seven (17%) positions were classified as nonclinical, and 18 (5%) were classified as unknown (Table 1). Three hundred decedents (240 male and 60 female) had a known species specialization, and 226 of 300 (75%) worked exclusively or predominantly with companion animals. Forty-two of 60 (70%) female decedents with known species specialization were classified as clinical practitioners and worked exclusively or predominantly with companion animals.
Comparison with general US population
Veterinarians had a higher PMR for suicide, compared with the general US population (Table 2). Male veterinarians were 2.1 (95% CI, 1.87 to 2.32) times and female veterinarians were 3.5 (95% CI, 2.73 to 4.39) times as likely as the general US population to die by suicide. The PMRs for all occupational characteristics were > 1.0, although not all were significant. Both male and female veterinarians who worked in any clinical position or specialized in companion animals were significantly (P < 0.01 for both comparisons) more likely to die by suicide than was the general US population. Male and female veterinarians who specialized in food animals (P < 0.05) or worked in nonclinical positions (P < 0.01) were also significantly more likely to die by suicide than was the general US population; however, the observed numbers of female deaths in food animal specialization and nonclinical positions were low, resulting in wide CIs and less precise estimates.
Table 2—
Proportionate mortality ratios for suicide for the 398 decedents in Table 1.
| Position type | Males (n = 326) | Females (n = 72) | ||||
|---|---|---|---|---|---|---|
| No. observed | No. expected | PMR (95%CI) | No. observed | No. expected | PMR (95%CI) | |
| All | 326 | 156.3 | 2.1* (1.87–2.32) | 72 | 20.7 | 3.5* (2.73–1.39) |
| Clinical | 261 | 117.5 | 2.2* (1.96–2.51) | 52 | 15.4 | 3.4* (2.52–1.42) |
| Companion animal | 167 | 61.6 | 2.7* (2.32–3.16) | 42 | 12.3 | 3.4* (2.46–1.61) |
| Food animal | 32 | 18.8 | 1.7* (1.16–2.40) | < 5 | < 5 | 4.9† (1.00–14.19) |
| Mixed animal | 16 | 9.7 | 1.7 (0.94–2.68) | < 5 | < 5 | 3.6 (0.75–10.61) |
| Equine | < 5 | < 5 | 1.2 (0.49–2.50) | < 5 | < 5 | 1.2 (0.03–6.61) |
| Other | < 5 | < 5 | 4.0 (0.48–14.42) | < 5 | < 5 | 0 (—) |
| Not specified | 37 | 21.1 | l.8† (1.24–2.42) | < 5 | < 5 | 3.6 (0.75–10.57) |
| Nonclinical | 56 | 31.2 | 1.8* (1.36–2.33) | 11 | 2.2 | 5.0* (2.50–8.98) |
| Unknown | 9 | 7.7 | 1.2 (0.54–2.23) | 9 | 3.0 | 3.0* (1.36–5.65) |
The PMRs were generated by LTAS software with 95% CIs and 2-sided P values on the basis of an assumed Poisson distribution; values > 1.0 indicate that the proportion of deaths by suicide is greater than that for the general US population during the study period, with values of P < 0.05 considered significant.
P < 0.01.
P < 0.05.
See Table 1 for remainder of key.
Suicide deaths over time among veterinarians
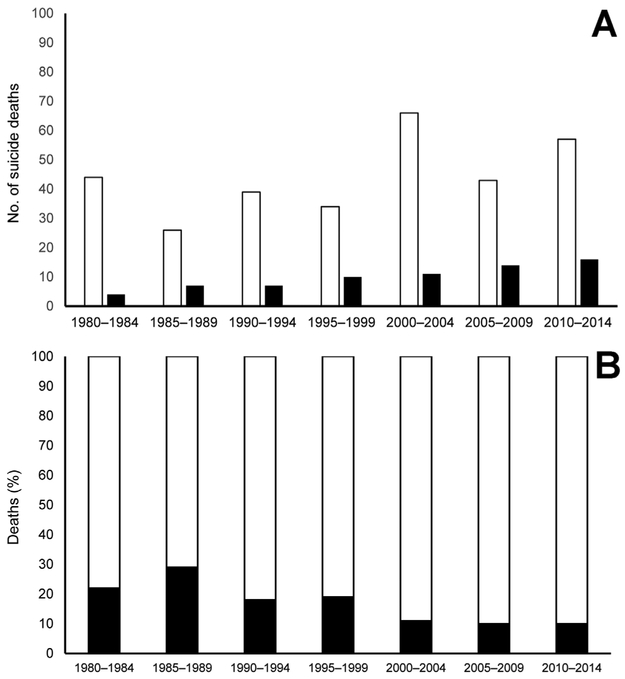
During the study period, the number of deaths by suicide per 5-year calendar period subjectively increased over time (Figure 2). The number of these deaths among males varied among calendar periods; however, the number among females appeared to consistently increase with each calendar period. Since 2000, the proportion of deaths by suicide among female decedents was approximately 10% of the total for each 5-year period. Although the study included only 1 year during the 2015 through 2019 calendar period, the proportion of deaths by suicide among female decedents for 2015 remained consistent with those in previous periods (data not shown). The PMRs for suicide were > 1.0 and significant (P < 0.05) for both male and female decedents across most calendar periods (the PMR for male decedents in the 1985 through 1989 calendar period was not statistically significant at the P < 0.05 level), indicating that veterinarians were consistently more likely than the general US population to die by suicide during the study period (Figure 3). Subjective comparison revealed that over all 7 calendar periods, the PMRs for females decreased and those for males were more variable but slightly increased.
Figure 2—
Graphic depictions of the number of deaths by suicide among male and female veterinarians (A) and the percentage of deaths by suicide among female veterinarians (B) in the seven 5-year calendar periods of the study. Calendar periods were standardized by LTASb software into 5-year periods; data for 2015 are not shown because data for only 1 year were available for the 5-year calendar period. In panel A, white and black bars represent suicide deaths of males and females, respectively. In panel B, stacked black and white bars represent the percentage deaths among females that resulted from suicide and from all other causes, respectively.
Figure 3—
Proportionate mortality ratios for suicide of male (solid line) and female (dashed line) veterinarians by calendar period during the study. The PMRs were calculated by use of LTASb software; values > 1.0 indicate that the proportion of deaths by suicide is greater than that for the general US population during the same 5-year period. All PMRs were significant (P < 0.05) except those for males in the 1985–1989 calendar period.
Methods of suicide
Among all decedents, the most common methods of suicide were the use of firearms (180/398 [45%]) and pharmaceuticals (154 [39%]; Figure 4). Other methods of suicide were reported on death certificates for the remaining 64 decedents; these included hanging or suffocation, inhalation of gases or vapors, and drowning. Of 313 decedents classified as having clinical positions, 137 (44%) died from self-inflicted firearm wounds and 130 (42%) died from pharmaceutical poisonings. Most male decedents (167/326 [51%]) died from firearm wounds, whereas most female decedents (46/72 [64%]) died from pharmaceutical poisonings. Females were more likely than males to die by use of pharmaceuticals (OR, 3.6; 95% CI, 2.10 to 6.09; P < 0.001), and males were more likely than females to die by use of firearms (OR, 4.8; 95% CI, 2.52 to 9.03; P < 0.001). Decedents in clinical positions were more likely to die from pharmaceutical poisonings than were those in nonclinical positions (OR, 2.3; 95% CI, 1.24 to 4.15; P = 0.003).
Figure 4—
Percentages of suicides among male (A) and female (B) veterinarians classified by occupational position type and means of death during 1979 through 2015. Black, white, and gray stacked bars indicate deaths incurred by pharmaceutical poisoning, firearm injury, and other methods, respectively. Occupational positions were classified as clinical if decedents had general practice listed as their employment facility type or their primary function was listed as clinical medicine. The category of all included clinical (261 males and 52 females), nonclinical (56 males and 11 females), and unknown (9 males and 9 females) position types.
Discussion
From 1979 through 2015, male and female US veterinarians had higher than expected PMRs for suicide, compared with the general US population. Female veterinarians in clinical and nonclinical roles were 3.4 and 5.0 times as likely to die by suicide as the general population, respectively. Additionally, 154 of 398 (39%) deaths by suicide among veterinarians over the 36-year study period were the result of pharmaceutical poisoning, a rate nearly 2.5 times that for individuals among the general US population who died by suicide in 2016.35,36 These findings warrant further investigation.
In the general US population, females are more likely than males to consider suicide, whereas males are more likely than females to die by suicide.35,37 A 2014 survey of US veterinarians found that, like the general population, female veterinarians had considered suicide more often than males since leaving veterinary school; however, both male and female veterinarians had considered suicide more often than the general population.12 An unusual paradigm seemingly exists within the veterinary profession, in which female veterinarians have a higher prevalence of risk factors for suicide12 and likely have a higher PMR for suicide than do male veterinarians.8,24,38–41 Additionally, research has indicated specific characteristics of the profession likely contribute to a greater than expected number of deaths from suicide among veterinarians, including long work hours, work overload, practice management responsibilities, client expectations and complaints, euthanasia procedures, and poor work-life balance.1,12,39,42–44
Female veterinarians were approximately 3.5 times as likely as the general US population to die by suicide. During the study period, the PMR for suicide remained > 3 times that of the general US population until the 2000 through 2004 calendar period. From that time through the period ending in 2014, an apparent decrease was noted in the PMR for female veterinarians. Because the number of suicides among female veterinarians increased each calendar period, the decrease in PMR was most likely because of an increase in suicide rates for the general US population.45 Although the US suicide rate increased 30% between 1999 and 2016,45 female veterinarians were still > 2.5 times as likely as the general US population to die from suicide during this part of the study period. Additionally, US veterinary school enrollment has steadily increased over the past few decades, increasing the number of practicing veterinarians in the population each year.25 Since the late 1980s, the percentage of females in the veterinary student population has surpassed the percentage of males.25 Currently, female veterinarians comprise > 60% of veterinarians in the United States.26 The number and proportion of US female veterinarians will continue to grow, as > 80% of US veterinary students enrolled in 2016 were female.25 Therefore, if the high PMRs for suicide among female veterinarians endure as the number of females in the veterinary profession continues to grow, the number of suicide deaths among female veterinarians could continue to increase.
Male and female veterinarians who worked in clinical positions had higher than expected PMRs for suicide. One potential contributing factor associated with this finding is exposure to occupational stressors. Veterinarians working in clinical medicine, particularly companion animal medicine, are exposed to high levels of occupational stress related to long working hours, client expectations, unexpected outcomes, communicating bad news, poor work-life balance, high workloads, rising veterinary care costs, professional isolation, student debt, and lack of senior support.12–14,38,39,43,46 Increased and unmanaged occupational stressors can be associated with known risk factors for suicide including burnout, psychological distress, and depression.12,47,48 In addition to the aforementioned 2014 survey of > 11,000 US veterinarians that revealed a high prevalence of risk factors for suicide,12 a 2012 survey of 394 Minnesota veterinarians reported that 22% had sought medical care for depression, 10% had physician-diagnosed anxiety, and 10% had physician-diagnosed depression.17 A 2012 survey of 701 Alabama veterinarians indicated that 66% had self-reported clinical depression and 24% had considered suicide since starting veterinary school.19 In a 1992 survey of 572 US female veterinarians, 87% of respondents considered their job stressful and 67% were experiencing signs of burnout or compassion fatigue.18 The findings of high PMRs for suicide among male and female veterinarians who worked in clinical positions were consistent with the information described in these reports, and taken together, the data suggest veterinarians who work in clinical roles are likely at increased risk for suicide. Incorporating healthy work design and well-being concepts in the clinical environment to address compassion fatigue and occupational stress and offering continuing education on managing occupational stressors might help to reduce the number of suicides among veterinarians.
In the present study, the use of firearms was the most common method of suicide. However, 154 of 398 (39%) decedents used poisoning with pharmaceuticals as a method of suicide, a proportion more than twice that for suicide decedents in the general US population as reported by other sources.16,34,49 A higher percentage of suicide deaths by poisoning, compared with the general population, is consistent with findings in several international studies4,8,10 of suicide among veterinarians. Veterinarians have access to pharmaceutical products such as injectable barbiturates, narcotics, sedatives, and tranquilizers, and they receive extensive training on the pharmacokinetics and pharmacodynamics of these products.14 Multiple studies have found that persons at risk for suicide usually choose methods that are accessible and familiar.4,8,50 Furthermore, a New Zealand study51 of suicides by occupation indicated that decedents in some health-care professions (nurses, doctors, and pharmacists) with access to pharmaceutical products were more likely to use poisoning methods than were other occupational groups. Research has indicated a potential association between suicide deaths among veterinarians and access to and knowledge of lethal pharmaceutical products.38,42 Applying administrative controls to limit and control access to potentially lethal pharmaceutical products might reduce the number of veterinarian suicides caused by pharmaceutical poisoning.
The relationships among work, personality, mental health, and suicide in other health-care professions are well-described.38,50,52 One potential factor associated with an increased risk of suicide among veterinarians is the selection of veterinary students with certain personality traits.42 The veterinary school application process commonly selects for perfectionism to meet the rigorous veterinary school academic requirements.1,42 However, perfectionism has been associated with higher risk for developing mental illnesses, including anxiety and depression.53 Veterinarians with certain personality traits who are exposed to unmanaged occupational stressors might be at risk for developing serious psychological distress, depression, and suicidal ideations.1,42 Other factors likely include financial debt and knowledge and acceptance of euthanasia procedures as well as access to potentially lethal pharmaceutical products.1,44 Additionally, veterinarians are trained to view euthanasia as an acceptable method to relieve suffering in animals, which can affect the way veterinarians view human life, including a reduced fear about death, especially among those experiencing suicidal ideation.1,43 The high PMR for suicide among veterinarians is likely attributable to a combination of factors1,54 and highlights the need for comprehensive suicide prevention strategies targeted toward this unique population.55
Recently, the CDC released a collection of the best-available evidence strategies to prevent or reduce suicides.55 The CDC listed 7 strategies and approaches to target suicide risk and protective factors at multiple levels of social ecology. The strategies range from those most likely to have a broad population impact to those focused on individuals and include the following: strengthen economic supports; strengthen access and delivery of suicide care; create protective environments; promote connectedness; teach coping and problem-solving skills; identify and support people at risk; and lessen harms and prevent future risk.55 Several prevention strategies might be more directly relevant to at-risk male or female veterinarians, including creating protective environments, teaching coping and problem-solving skills, and identifying and supporting people at risk.
The present study had several limitations. First, PMRs are useful in studies where the denominator is unknown; however, lack of denominator data prevents the calculation of standardized mortality ratios, which are statistically stronger and allow for comparisons between populations. Cause-specific PMRs are mutually dependent, meaning a higher PMR for one cause results in a lower PMR for another cause. In this study, the high PMR for suicide could have been caused by a high number of deaths by suicide in the cohort of veterinarians or by a low number of deaths from other causes.34,56 Additionally, the data for decedents not included in the study (eg, veterinarian decedents without information available through AVMA resources or those excluded because of missing data or other reasons) might differ from those of individuals who were included, and such information could potentially affect PMR calculations. However, similar findings related to death from suicide were reported in previous studies9–11,39 of causes of death in veterinarians, supporting the findings in the present study. Second, an assumption of the present study was that all decedents were correctly matched to an NDI cause-of-death record. Because social security numbers were not available, all NDI matches were made on the basis of full name, birth date, birth state, death date, death state, race, and sex, and selection of record matches was performed on the basis of the NDI-recommended scoring system, which maximizes the proportion of records correctly classified.29
Third, death by suicide was identified by the use of ICD codes listed in the NDI system as recorded from the death certificate. Finally, the possibility exists for a misclassification of death on death certificates.8,57,58 Death certificates for veterinarians might be less likely to list suicide as the cause of death because of high social standing within the community or because some intentional deaths (eg, the result of pharmaceutical poisoning) could be ruled as accidental, both of which would result in an underestimation of the PMR for suicide in this population.8,39,57
The findings of the present study and publications such as the aforementioned CDC package aimed at suicide prevention55 may provide useful information for the creation and promotion of evidence-based wellness resources. Partnerships among the AVMA, state veterinary medical associations, other veterinary professional associations, veterinary schools, and experts in suicide prevention could be used to improve veterinarian awareness of available suicide prevention programs and contribute to implementation of an effective and comprehensive suicide prevention strategy. Further studies could include periodic analyses of AVMA obituary and life insurance policy data for estimation and monitoring of PMRs for suicide among US veterinarians as a means of assessing the effectiveness of suicide prevention interventions.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
The authors thank Drs. James Yiin, Mary Schubauer-Berigan, and John Beard from the CDC National Institute for Occupational Safety and Health for their intellectual contributions with LTAS and PMR analysis, and Diane Fagen and Dana Johnson from the AVMA for their assistance with data collection.
ABBREVIATIONS
- CI
Confidence interval
- ICD
International classification of diseases
- LTAS
Life Table Analysis System
- NDI
National Death Index
- PMR
Proportionate mortality ratio
Footnotes
SAS, version 9.4, SAS Institute Inc, Cary, NC.
LTAS, version 4.0, National Institute for Occupational Safety and Health, CDC, Cincinnati, Ohio.
References
- 1.Bartram DJ, Baldwin DS. Veterinary surgeons and suicide: a structured review of possible influences on increased risk. Vet Rec 2010;166:388–397. [DOI] [PubMed] [Google Scholar]
- 2.Faragher T Suicide in Australian veterinarians. Aust Vet J 2008;86:249. [DOI] [PubMed] [Google Scholar]
- 3.Hem E, Haldorsen T, Aasland OG, et al. Suicide rates according to education with a particular focus on physicians in Norway 1960–2000. Psychol Med 2005;35:873–880. [DOI] [PubMed] [Google Scholar]
- 4.Jones-Fairnie H, Ferroni P, Silburn S, et al. Suicide in Australian veterinarians. Aust Vet J 2008;86:114–116. [DOI] [PubMed] [Google Scholar]
- 5.Kelly S, Bunting J. Trends in suicide in England and Wales, 1982–96. Popul Trends 1998;92:29–41. [PubMed] [Google Scholar]
- 6.Kelly S, Charlton J, Jenkins R. Suicide deaths in England and Wales, 1982–92: the contribution of occupation and geography. Popul Trends 1995;80:16–25. [PubMed] [Google Scholar]
- 7.Kinlen LJ. Mortality among British veterinary surgeons. Br Med J (Clin Res Ed) 1983;287:1017–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mellanby RJ. Incidence of suicide in the veterinary profession in England and Wales. Vet Rec 2005;157:415–417. [DOI] [PubMed] [Google Scholar]
- 9.Blair A, Hayes HM Jr. Cancer and other causes of death among US veterinarians, 1966–1977. Int J Cancer 1980;25:181–185. [DOI] [PubMed] [Google Scholar]
- 10.Blair A, Hayes HM Jr. Mortality patterns among US veterinarians, 1947–1977: an expanded study. Int J Epidemiol 1982;11:391–397. [DOI] [PubMed] [Google Scholar]
- 11.Miller JM, Beaumont JJ. Suicide, cancer, and other causes of death among California veterinarians, 1960–1992. Am J Ind Med 1995;27:37–49. [DOI] [PubMed] [Google Scholar]
- 12.Nett RJ, Witte TK, Holzbauer SM, et al. Risk factors for suicide, attitudes toward mental illness, and practice-related stressors among US veterinarians. J Am Vet Med Assoc 2015;247:945–955. [DOI] [PubMed] [Google Scholar]
- 13.Hawton K, Malmberg A, Simkin S. Suicide in doctors. A psychological autopsy study. J Psychosom Res 2004;57:1–4. [DOI] [PubMed] [Google Scholar]
- 14.Platt B, Hawton K, Simkin S, et al. Suicidal behaviour and psychosocial problems in veterinary surgeons: a systematic review. Soc Psychiatry Psychiatr Epidemiol 2012;47:223–240. [DOI] [PubMed] [Google Scholar]
- 15.Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. Am J Prev Med 2014;47:S176–S180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loprinzi PD, Cain DS. Updated trends in suicidal ideation among US adults, 2005–2012. Prev Med 2015;78:14–16. [DOI] [PubMed] [Google Scholar]
- 17.Fowler HN, Holzbauer SM, Smith KE, et al. Survey of occupational hazards in Minnesota veterinary practices in 2012. J Am Vet Med Assoc 2016;248:207–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elkins AD, Kearney M. Professional burnout among female veterinarians in the United States. J Am Vet Med Assoc 1992;200:604–608. [PubMed] [Google Scholar]
- 19.Skipper GE, Williams JB. Failure to acknowledge high suicide risk among veterinarians. J Vet Med Educ 2012;39:79–82. [DOI] [PubMed] [Google Scholar]
- 20.Han B, Crosby AE, Ortega LA, et al. Suicidal ideation, suicide attempt, and occupations among employed adults aged 18–64 years in the United States. Compr Psychiatry 2016;66:176–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McIntosh WL, Spies E, Stone DM, et al. Suicide rates by occupational group—17 states, 2012. MMWR Morb Mortal Wkly Rep 2016;65:641–645. [DOI] [PubMed] [Google Scholar]
- 22.Stallones L, Doenges T, Dik BJ, et al. Occupation and suicide: Colorado, 2004–2006. Am J Ind Med 2013;56:1290–1295. [DOI] [PubMed] [Google Scholar]
- 23.Milner A, Spittal MJ, Pirkis J, et al. Suicide by occupation: systematic review and meta-analysis. Br J Psychiatry 2013;203:409–416. [DOI] [PubMed] [Google Scholar]
- 24.Bartram DJ, Yadegarfar G, Baldwin DS. A cross-sectional study of mental health and well-being and their associations in the UK veterinary profession. Soc Psychiatry Psychiatr Epidemiol 2009;44:1075–1085. [DOI] [PubMed] [Google Scholar]
- 25.Association of American Veterinary Medical Colleges. Annual data report 2016–2017. Available at: www.aavmc.org/data/files/data/2017%20aavmc%20public%20data-%20final.pdf. Accessed Jul 18, 2017.
- 26.AVMA. Market research statistics—US veterinarians, 2017. Available at: www.avma.org/KB/Resources/Statistics/Pages/Market-research-statistics-US-veterinarians.aspx. Accessed Feb 20, 2018.
- 27.Hoblet KN, Maccabe AT, Heider LE. Veterinarians in population health and public practice: meeting critical national needs. J Vet Med Educ 2003;30:287–294. [DOI] [PubMed] [Google Scholar]
- 28.Maccabe AT, Matchett KE, Hueston WD. The need for public health veterinarians as seen by future employers. J Vet Med Educ 2008;35:269–274. [DOI] [PubMed] [Google Scholar]
- 29.CDC National Center for Health Statistics. National Death Index user’s guide. Hayttsville, Md: CDC National Center for Health Statitistics, 2013. Available at: www.cdc.gov/nchs/data/ndi/ndi_users_guide.pdf. Accessed Feb 20, 2018. [Google Scholar]
- 30.National Institute for Occupational Safety and Health. Life Table Analysis System (LTAS) user’s guide. Atlanta, Ga: CDC National Institute for Occupational Safety and Health; Available at: https://www.cdc.gov/niosh/ltas/pdf/LTAS-manual-2014.pdf. Accessed Jul 28, 2017. [Google Scholar]
- 31.World Health Organization. International classification of diseases: 9th revision. Geneva: World Health Organization, 2014. [Google Scholar]
- 32.World Health Organization. International statistical classification of diseases and related health problems: 10th revision. Geneva: World Health Organization, 2014. [Google Scholar]
- 33.Robinson CF, Schnorr TM, Cassinelli RT, et al. Tenth revision US mortality rates for use with NIOSH Life Table Analysis System. J Occup Environ Med 2006;48:662–667. [DOI] [PubMed] [Google Scholar]
- 34.Roman E, Beral V, Inskip H, et al. A comparison of standardized and proportional mortality ratios. Stat Med 1984;3:7–14. [DOI] [PubMed] [Google Scholar]
- 35.American Foundation for Suicide Prevention. Understanding and preventing suicide through research, education, and advocacy, 2018. Available at: afsp.org/about-suicide/suicide-statistics/. Accessed Apr 30, 2018.
- 36.CDC National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS), 2015. Available at: webappa.cdc.gov/sasweb/ncipc/mortrate.html. Accessed May 1, 2018.
- 37.Baca-Garcia E, Perez-Rodriguez MM, Keyes KM, et al. Suicidal ideation and suicide attempts in the United States: 1991–1992 and 2001–2002. Mol Psychiatry 2010;15:250–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bartram DJ, Baldwin DS. Veterinary surgeons and suicide: influences, opportunities and research directions. Vet Rec 2008;162:36–40. [DOI] [PubMed] [Google Scholar]
- 39.Platt B, Hawton K, Simkin S, et al. Systematic review of the prevalence of suicide in veterinary surgeons. Occup Med (Lond) 2010;60:436–446. [DOI] [PubMed] [Google Scholar]
- 40.Roberts SE, Jaremin B, Lloyd K. High-risk occupations for suicide. Psychol Med 2013;43:1231–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alexopoulos EC, Kavalidou K, Messolora F. Suicide mortality across broad occupational groups in Greece: a descriptive study. Saf Health Work 2016;7:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dawson BF, Thompson NJ. The effect of personality on occupational stress in veterinary surgeons. J Vet Med Educ 2017;44:72–83. [DOI] [PubMed] [Google Scholar]
- 43.Scotney RL, McLaughlin D, Keates HL. A systematic review of the effects of euthanasia and occupational stress in personnel working with animals in animal shelters, veterinary clinics, and biomedical research facilities. J Am Vet Med Assoc 2015;247:1121–1130. [DOI] [PubMed] [Google Scholar]
- 44.Volk JO, Schimmack U, Strand EB, et al. Executive summary of the Merck Animal Health Veterinary Wellbeing Study. J Am Vet Med Assoc 2018;252:1231–1238. [DOI] [PubMed] [Google Scholar]
- 45.Stone DM, Simon TR, Fowler KA, et al. Vital signs: trends in state suicide rates—United States, 1999–2016 and circumstances contributing to suicide—27 states, 2015. MMWR Morb Mortal Wkly Rep 2018;67:617–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oxley JA, Montrose VT, Kogan L. E-mental health and the veterinary profession. J Am Vet Med Assoc 2017;250:1226–1227. [DOI] [PubMed] [Google Scholar]
- 47.Chigerwe M, Boudreaux KA, Ilkiw JE. Assessment of burn-out in veterinary medical students using the Maslach Burn-out Inventory-Educational Survey: a survey during two semesters. BMC Med Educ 2014;14:255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Allison SO, Eggleston-Ahearn AM, Courtney CJ, et al. Implementing wellness in the veterinary workplace. J Am Vet Med Assoc 2016;249:879–881. [DOI] [PubMed] [Google Scholar]
- 49.Milner A, Witt K, Maheen H, et al. Access to means of suicide, occupation and the risk of suicide: a national study over 12 years of coronial data. BMC Psychiatry 2017;17:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hawton K, Clements A, Simkin S, et al. Doctors who kill themselves: a study of the methods used for suicide. QJM 2000;93:351–357. [DOI] [PubMed] [Google Scholar]
- 51.Skegg K, Firth H, Gray A, et al. Suicide by occupation: does access to means increase the risk? Aust N Z J Psychiatry 2010;44:429–434. [DOI] [PubMed] [Google Scholar]
- 52.Work Stansfeld S., personality and mental health. Br J Psychiatry 2002;181:96–98. [DOI] [PubMed] [Google Scholar]
- 53.Hewitt PL, Flett GL. Dimensions of perfectionism, daily stress, and depression: a test of the specific vulnerability hypothesis. J Abnorm Psychol 1993;102:58–65. [DOI] [PubMed] [Google Scholar]
- 54.Halliwell RE, Hoskin BD. Reducing the suicide rate among veterinary surgeons: how the profession can help. Vet Rec 2005;157:397–398. [DOI] [PubMed] [Google Scholar]
- 55.Stone DM, Holland KM, Bartholow B, et al. Preventing suicide: a technical package of policies, programs, and practices. Atlanta, Ga: CDC National Center for Injury Prevention and Control, 2017. [Google Scholar]
- 56.Breslow NE, Day NE. Statistical methods in cancer research. IARC Workshop 25–27 May 1983. IARC Sci Publ 1987:1–406. [PubMed] [Google Scholar]
- 57.Mohler B, Earls F. Trends in adolescent suicide: misclassification bias? Am J Public Health 2001;91:150–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mieno MN, Tanaka N, Arai T, et al. Accuracy of death certificates and assessment of factors for misclassification of underlying cause of death. J Epidemiol 2016;26:191–198. [DOI] [PMC free article] [PubMed] [Google Scholar]