Abstract
Studies of children’s functioning following exposure to a traumatic event rarely have investigated change over the weeks following the event, but studying recovery in the short aftermath of a traumatic event is important for understanding vulnerability to subsequent disorder, as well as the potential utility of preventive interventions. Data are reported from a short-term longitudinal study of 35 mother-child dyads over 14 weeks following exposure to an incident of severe intimate partner violence. Using a developmental-ecological framework, we proposed that maternal parenting practices would be associated with children’s recovery, and that mother’s mental health would be associated with her parenting practices. Consistent with hypotheses, observed parenting practices at baseline predicted the trajectory of children’s self-reported internalizing problems over the study period. Growth in maternal mental health problems was marginally associated with the trajectory of child internalizing symptoms. Parenting did not mediate the relationship between maternal mental health symptoms and child internalizing. Further studies should pay closer attention to the role of parenting in children’s adjustment in the aftermath of a traumatic event.
Keywords: parenting practices, trauma, children, domestic violence, mental health
Introduction
Intimate partner violence (IPV) is the most common source of exposure to traumatic events for children, with an estimated 15 million children yearly witnessing violence between adult partners1 (McDonald, Jouriles, & Skopp, 2006). Over the past two decades, a large body of research has documented the negative effects of exposure to IPV on children’s adjustment (for comprehensive reviews, see Kitzmann, Gaylord, Holt, & Kenny, 2003; Wolfe, Crooks, Lee, McIntyre-Smith, & Jaffe, 2003). Witnessing IPV is associated with internalizing and externalizing symptoms, cognitive and social problems, and a small but growing body of longitudinal data has demonstrated the specific impact of exposure to IPV at particular developmental stages (e.g., Yates, Dodds, Sroufe, & Egeland, 2003). Longitudinal studies, however, primarily have examined functioning over years (e.g., Ehrensaft et al., 2003), rather than in the weeks and months following exposure to violence. The goal of this study was to investigate the family correlates of child internalizing symptoms in the short-term aftermath (i.e., 2–14 weeks) of a severe IPV incident witnessed by the target child.
Children’s Short-term Adjustment Following Traumatic Events
An understanding of distress and recovery in the short-term (acute adaptation) may be important for understanding subsequent vulnerability to disorder following exposure to traumatic events (Litz, 2004; Pine & Cohen, 2002). Acute or posttraumatic distress symptoms within the month following a traumatic event may portend later posttraumatic stress disorder, or indicate vulnerability to other, related adjustment difficulties (Fein, Kassam-Adams, Vu, & Datner, 2001; Kassam-Adams & Winston, 2004). There is a clear need for further research to understand patterns and rates of recovery among children exposed to traumatic events, particularly to inform the timing and nature of interventions (Kenardy et al., 1996; Litz, 2004).
Very few studies of IPV have examined short-term adjustment trajectories, in part because recruiting families shortly after an incident of IPV is challenging (Dutton et al., 2003). Jouriles and colleagues (1998) reported decreases in internalizing symptoms among school-aged children over a six-month period following residence in a domestic violence shelter (in contrast to externalizing symptoms, which remained stable). Short-term data gathered in the wake of other traumatic incidents have demonstrated strong associations of these events with children’s internalizing symptoms (Perrin, Smith, & Yule, 2000; Pine & Cohen, 2002). Some inconsistencies in patterns of symptom expression are evident, with several studies indicating acute increases in symptoms shortly after the event, with a gradual decrease over the next year or two (Laor, Wolmer, & Cohen, 2001), and others indicating a lag in symptom expression (Shaw, Applegate, & Schorr, 1996).
Multiple early indicators may influence vulnerability to internalizing symptoms for children exposed to traumatic events, including event characteristics (degree and extent of exposure/victimization; Brown, Cohen, Johnson, & Smailes, 1999; Fergusson, Horwood, & Lynskey, 1996), child characteristics (e.g., pre-existing anxiety; LaGreca, Wasserstein, & Silverman, 1998, cognitive appraisals; Jouriles, Spiller, Stephens, McDonald, & Swank, 2000; Cummings & Davies, 1996; Grych & Fincham, 1990), and social - family and environmental - support (Smith, Perrin, Yule, & Rabe-Hesketh, 2001). In the context of war and terrorism, for example, child vulnerability to PTSD appears to be associated with degree of familial disruption and displacement (e.g., Laor et al., 2001). Interestingly enough, few studies - mainly with IPV samples - have focused specifically on the role of parenting practices in the context of child functioning following trauma exposure. The increased focus on parenting in the IPV literature is not surprising given the nature of IPV and the roles of parents as victims and/or victimizers.
Influence of Parenting Practices on Child Adjustment Following IPV
Studies across the developmental spectrum have reported associations between parenting and child externalizing problems in IPV populations (Margolin, 1998). Levendosky and colleagues (2006) reported that maternal functioning (a combination of maternal mental health and parenting) mediated the relationship between exposure to domestic violence and infants’ externalizing behaviors in 203 dyads. Observed parenting mediated the relationship between current IPV and infant adjustment, while mental health mediated the relationship between both past and current IPV and infant externalizing. In a study of 85 preschoolers who witnessed interparental violence, maternal psychopathology and mother-child relationship quality each contributed unique variance in predicting children’s behavior problems (Lieberman, Van Horn, & Ozer, 2005).
Rossman, Bingham, & Emde (1997) assessed school-aged children’s functioning across different stressful events (dog bite, domestic violence, and normative stressors). Positive maternal parenting (assessed by self-report) predicted fewer child internalizing and externalizing problems, and better school performance; maternal and child symptoms also were associated. In another study of school-aged children using observational measures of parenting, maternal warmth and authority-control in battered women were negatively associated with child behavior problems. IPV directly and indirectly (through maternal mental health) influenced parenting (Levendosky & Graham-Bermann, 2000).
In sum, maternal parenting practices appear to be good predictors of children’s externalizing problems in an IPV context, but less is known either about their role in the short-term aftermath of a violent event, or about their role in internalizing problems. This study aims to bridge the gap between the (largely longer-term) studies of parenting and IPV, and the (largely non-IPV) studies of children’s short-term functioning in the wake of a traumatic event, by examining the influence of maternal parenting on child internalizing trajectories shortly after an IPV incident. This is the first study to examine short-term longitudinal relationships among observed maternal parenting, self-reports of maternal mental health, and child self-reports of distress after IPV.
Conceptual Framework and Research Questions
Family stress models (e.g., Fauber, Forehand, Thomas, & Wierson, 1990; Forgatch & DeGarmo, 1999) have demonstrated how a variety of family transitions including marital conflict negatively affect child adjustment through parental distress and impaired parenting. Using a conceptual model adapted from Forgatch & DeGarmo (2002; and adapted for trauma contexts by Gewirtz, Forgatch, & Wieling, 2008), we propose that child internalizing is directly influenced by maternal parenting practices and maternal mental health. Family stress models have also specified direct effects of parental mental health and indirect effects through effective parenting. That is, the increased distress and sequelae of disruptive family events interfere with effective parenting, and parenting is viewed as more proximal to child adjustment. We were not able to test direct effects of IPV and family transitions; however, within such a model we focused on the unique contributions of maternal parenting practices (mother ‘as parent’) a nd mothers’ distress (mother ‘as person’) on short-term child internalizing problems for a sample of mother-child dyads recently experiencing IPV. As outcomes, we also hypothesized that maternal distress and child internalizing symptoms would decrease as time passed since the IPV acute event stressor that initially heightens distress (Forgatch & DeGarmo, 2002; Gewirtz et al., 2008); while mothers’ parenting practices would be relatively more stable over time.
Method
Sample
Participants were 35 mother-child dyads recruited from three domestic violence shelters (54%), and from a county domestic violence court (46%) in a large metropolitan area. Families were eligible to participate if mother was the victim of an incident of physical IPV within the past 1–3 weeks, and if a 6–12 year old biological child witnessed the assault. Fifty-seven percent of the abusers were current partners (40%) or spouses (17%); 43% were former partners (40%) or spouses (3%). Approximately half of the abusers (51.4%) were the target child’s biological father. The target IPV incidents all included physical assault, and in many instances, the events included threats of harm, use of weapons (knife, gun, brick), property damage, and violations of Orders of Protection. Seven mothers reported at least one additional violent incident occurring during the course of the study period.
Mothers’ ages were 24 to 46 years (M = 33.7; SD = 6.6); child mean age was 8 years, 11 months, and boys and girls were equally represented (17 boys, 18 girls). Mothers were 57% African-American, 29% Caucasian, 6% Native American, and 8% bi-racial. Annual income was measured by binned categories ranging from (1) less than $5,000 to (11) $50,000 or more. The median and modal category for the sample was $5,000-$9,999.
Procedures
University IRB approval was received for the study, which was conducted at a large domestic violence agency in a major metropolitan area. Recruitment flyers were posted in the waiting room of the civil court and in shelters. Court and shelter advocates also were contacted with information about the study; those whose clients were interested referred them to the study team, who followed up with them by phone. Participants were offered transportation, and refreshments, and childcare was provided for siblings of the target child. The informed consent process was conducted by the PI and/or interviewers; mothers signed a consent form and children an assent form. Mothers were informed about how the data were used, efforts to protect their privacy (a certificate of confidentiality was received from the National Institutes of Health) and the limits to confidentiality.
Interviewers were trained graduate students in clinical psychology and related disciplines. Assessments included concurrent, separate parent and child interviews, and a 40-minute parent- child observational task. At Time 1 baseline (T1), the average time since the violent incident was 20 days. Mothers and their children were invited back for subsequent assessments at approximately 7 weeks (Time 2) and 14 weeks (Time 3) following the violent incident. At Time 2 (T2), data were obtained for 29 mothers (82.9%) and 28 children (80%), and at Time 3 (T3), data were obtained for 30 mothers (85.7%) and 29 children (82.9%). A missing values analysis of the child adjustment measures, parenting indicators, mothers’ mental health, and control variables indicated that data was missing completely at random over time (MCAR). Little’s MCAR χ2(296) = 299.43, p =.44, meaning data from partial missing cases did not significantly differ from observed means and covariances for complete data cases and the probability of missingness was not dependent on the observed data (Shafer & Graham, 2002).
Measures
The key longitudinal study variables assessed child internalizing problems, mothers’ effective parenting, and mothers’ mental health at T1 to T3. The study design employed multimethod multi-agent assessment procedures that included child interview-based assessments of child adjustment problems, mothers’ self-reported mental health, and observational-based ratings of structured mother-child interaction tasks.
Child internalizing problems.
The focal child outcomes were three validated indicators of child depression, distress, and fears. Depression was measured by the Child Depression Inventory - Short Form (CDI-S: Kovacs, 1983), a 10-item self-report assessment of children’s cognitive, behavioral, and affective symptoms of depression. The CDI Short Form (alpha = .80) is correlated .89 with the CDI Full version. Since the CDI is designed to be sensitive to change over time, test-retest reliability for the Full version varies between .38 and .87 depending on the sample and the time interval being used. The CDI Full version has been repeatedly shown to correlate highly with similar measures of depression and to distinguish between clinical and non- clinical samples.
ChildDistress was measured by the Levonn (Richters, Martinez, & Valla, 1990), a 40- item cartoon-based interview of children’s post-traumatic distress symptoms. The measure contains several brief scripts about a boy named Levonn. Children were instructed to indicate how often they experienced each item (e.g., “Here is Levonn having a hard time going to sleep at night because he keeps remembering something scary that happened to him. How many times have you felt like Levonn?”) by responding “never (0),” “some of the time (1),” or “a lot of the time (2).” Therefore, the total index score ranged from 0 to 80. Above each response was a picture of a thermometer containing mercury, with higher levels of mercury indicating a greater frequency of each symptom. Each script corresponded with a picture of Levonn. Scores for each item were summed to produce an overall score. Test-retest reliability is reported at 0.81 and internal consistency at 0.71–0.84.
Child Fears were measured by an extension of the Children’s Fear Survey (CFS: Ramirez, Masten, & Miliotis, 1994), a 34-item checklist assessing childhood fears and worries. The original measure, developed for studies of homeless families, assesses four types of fears: common fears, deprivation fears, social rejection fears, and animal fears. For this study, two items pertinent to domestic violence were added (“my mom getting hurt” and “getting really mad and hurting someone”). Children were instructed to indicate how fearful they were of each item on an illustrated four-point Likert scale. The total summative index score ranged from 1 to 136. The measure has adequate internal consistency (.90) and test-retest reliability (0.71 with a 1- week interval between tests).
ChildInternalizing Construct was an overall composite score averaging the three child internalizing problems over time. To compute the growth score, we first rescaled the original respective indicators of child adjustment to a common metric ranging from 0 to 10. Rescaling to a common metric retains the mean information for assessing growth increases or decreases over time. Correlations among the three child adjustment measures ranged from .40 to .62 (p <.001) at T1, .57 to .72 (p <.001) at T2, and .43 to .67 at T3. In addition, principal components factor analyses obtained loadings ranged from .75 to .87 at T1, .80 to .90 at T2, and .75 to .88 at T3.
Mothers’ effective parenting.
Effective parenting was assessed using observational ratings of mother-child interaction during seven Family Interaction Tasks (FITs). The FITs provide validated measures of parenting practices demonstrating convergent validity, and external validity predictive of children’s developmental outcomes (Forgatch & DeGarmo, 1999). The FITs in the present study lasted a total of 40 minutes starting with a refreshment break and free-play task for the child using toys provided in the assessment room after which the mother was asked to direct her child to clean up the toys. In the next task, the dyad was asked to plan a fun family activity (times 1 and 3) or a birthday party (time 2). Two 5-minute problem-solving tasks followed, during which the dyad attempted to resolve current conflict issues. The issues were selected separately by mothers and children during their individual interviews, from the Issues Checklist (Prinz, Foster, Kent, & O’Leary, 1979), which lists topics of frequent family conflicts (e.g., chores, school problems, behavior). Finally, mother and child engaged in three cooperation/competition and teaching tasks: a guessing game, labyrinth game, and tangoes. The guessing game requires mother, then the child, to provide clues about the cards they hold in order for the other to guess the objects on the cards. The labyrinth game used a wooden labyrinth board, adapted so that the only open holes are those at the four corners of the board. The game required mother and child to use the control knobs to move marbles from the center of the board to one or more of the corner holes, first cooperatively, then competing with one another. The tangoes task required the mother to provide guidance to the child in order for the child to put together a series of plastic shapes in order to match designs shown on six cards.
FITs were videotaped and coded using previously validated ratings of key parenting practices predictive of children’s developmental outcomes (DeGarmo, Patterson, & Forgatch, 2004; Patterson, 2005). The four key parenting domains measured in the present study were skill encouragement, positive involvement, problem solving outcome, and inept discipline. Trained coders provided Likert-type ratings after viewing each of the interaction tasks. In addition overall global impressions were provided after viewing and scoring all of the tasks.
Skill encouragement was based on 9 items rating the mother’s ability to promote children’s skill development through contingent encouragement and scaffolding strategies observed during the game tasks. The scale included items such as breaks task into manageable steps, reinforces success, and prompts. Some items were originally on a 4-point scale and some on a 5-point scale. All items were rescaled from 1 to 5 to compute a growth construct score. Cronbach’s a was .85, .85, and .92 from T1 to T3.
Positive involvement was based on 31 items from the refreshments, clean up, problem solving, and game tasks. Items included ratings of mothers’ warmth, empathy, encouragement, affection, acceptance, respect of child, and so on. Items were rated on 4- and 5-point Likert scales and subsequently rescaled from 1 to 5. Cronbach’s a was .98, .98, and .97 over time.
Problem Solving Outcome was assessed with a 9-item scale scored for each of the problem solving discussions. Items were rated on a 5-point scale indicating the solution quality, extent of resolution, apparent satisfaction, likelihood of follow through, and so on. Cronbach’s a was .95, .95, .93 for Issue A over time and .93, .95, and .91 for Issue B over time.
Inept Discipline was a 11-item scale score rated on a 5-point scale; items included mother was... overly strict, authoritarian, erratic, inconsistent, oppressive, erratic, used nagging or nattering to get compliance, and so on. Crohbach’s α was .86, .87, and .85 over time.
Effective Parenting Construct was an overall composite score averaging the four parenting indicators above. Inept Discipline was reverse scaled at the item level to indicate good discipline. Therefore, the parenting construct score ranged from 1 to 5 indicating effective parenting behaviors. The construct obtained intra scale correlations ranging from .56 to .78 (p < .001) at T1, .57 to .82 (p < .001) at T2, and .63 to .80 (p < .001) at T3. Cronbach’s α was .89, 90, and .88 over time for the parenting construct.
Mothers’ mental health.
Mental Health was measured with the Global Severity Index (GSI) of the Brief Symptom Inventory (BSI: Derogatis & Spencer, 1982), a 53-item questionnaire that assesses distress and psychopathology. The mother was instructed to indicate how distressed she has felt by each symptom during the past 7 days, on a four-point Likert scale. The GSI, a measure of overall symptoms, was derived by summing the totals for all items then dividing by the total number of questions answered. The BSI has demonstrated good internal consistency (alpha reliability for the nine sub-scales ranged from 0.71 to 0.85), test-retest reliability (.90), and convergent and discriminate validity (Derogatis & Spencer, 1982).
Control variables.
Child Age was measured in years since birth and Child Gender was scored as “1” for boys and “2” for girls.
Analytic Strategy
Using three waves of data, the pilot study hypotheses were evaluated with linear growth curve models using a multilevel regression framework in the HLM6 program (Raudenbush & Bryk, 2002). Growth models combine individual and group levels of analysis, taking into account individual variation in growth over time used to summarize mean level growth and variance for the sample. To further specify temporal or causal ordering (Singer & Willett, 2003), change in maternal mental health and parenting practices from Time 1 to Time 2 were entered as predictors growth rates in child internalizing from Time 1 to Time 3.
The current analysis was a two-level model with repeated assessments of child outcomes modeled as the level one dependent variable. After estimating variance in individual trajectories of child adjustment, the individual growth curves and their variance then became the outcome focus of analysis. The Level 1 outcome slopes are then regressed on fixed or time-varying predictors at Level 2. In this case the Level 2 predictors are child age, child gender, maternal mental health, and effective parenting at baseline assessed shortly after the target IPV incident.
HLM growth curve models provided a key advantage for the present analyses. HLM can estimate linear slope trajectories based on each individual’s unique time line of assessment and can incorporate missing data at Level 1. In this study of IPV, variation in time since the event could be an important factor in reliably estimating change in family adjustment. Therefore, as opposed to fixing time weights at 3, 7, and 14 weeks, the time weighting for change was estimated as actual weeks for each individual family since the IPV event. For example, the mean number of weeks since the IPV event was 2.94 weeks (SD = .86) at T1, 7.61 weeks (SD = .83) at T2, and 13.59 weeks (SD = .83) at T3. Although eligible pilot families were recruited within 1 to 3 weeks of IPV and were assessed at roughly 7 and 14-week follow-ups, a family assessed within the first week of IPV may be more distressed than families in the 3rd week following the event. Because HLM does not require equal time spacing fixed for each individual the growth estimates more reliably estimate adjustment over time taking into account variance in IPV time at baseline as well as variance in spacing and duration of weeks at follow-up assessments.
The Level 1 equation was Level 1 ChildInternalizingt i where the dependent variable for child i is repeated over time t. The growth scores are a function of the baseline intercept for child i, a growth rate for child i over 14 weeks, and an error term. After summarizing the individual intercepts and growth slopes, the Level 2 model then regresses intercepts and slopes on predictors as
Level 2 Child Internalizing Intercept
Level 2 Child Internalizing Growth
where β00 is the sample intercept controlling for predictors, β01 is the effect of child age on the intercept and β04 the effect of parenting plus a random error term; and β11 represents the effect of child age and β14 the effect of parenting on growth rate plus a random error term.
Results
Means and standard deviations over time for the child adjustment measures, mothers’ effective parenting, and mothers’ mental health are provided in Table 1. The first step in the growth model analysis was to estimate the unconditional model specifying the intercepts and growth rates for the sample. Results of the unconditional model in the form of unstandardized regression coefficients are provided in Table 2. Focusing first on the intercepts, the mean intercepts in the unconditional model indicated that each of the child adjustment measures was significantly different from zero at Time 1 and that there was significant individual differences in initial status for each of the indicators and the overall adjustment construct score. Focusing on the growth rates in Table 2, each child internalizing measure showed significant mean decrease over the 14 weeks of the study. For example, on average, the sample decreased in depression symptoms at a rate of −.13 per week (p < .001), −.61 in distress per week (p < .01), and a rate of - .73 (p < .01) in fears per week. The construct score decreased by −.05 units per week (p < .01).
Table 1.
Means and Standard Deviations Over Time for Key Study Variables and Composite Growth Construct Scores for Child Internalizing and Mothers’ Parenting
| Time 1 | Time 2 | Time 3 | ||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| Child Internalizing Measures | ||||||
| Depression (CDI) | 3.26 | 3.43 | 1.34 | 2.19 | 1.61 | 2.66 |
| Distress (Levonn) | 24.37 | 16.29 | 18.29 | 18.32 | 18.07 | 18.60 |
| Fear (CFS) | 30.80 | 16.63 | 27.79 | 19.61 | 22.18 | 13.09 |
| Internalizing Problems | ||||||
| Composite Growth Score* | 2.29 | 1.38 | 1.66 | 1.39 | 1.65 | 1.49 |
| Mothers’ Observed Parenting | ||||||
| Skill Encouragement | 2.06 | .58 | 1.86 | .54 | 1.99 | .70 |
| Positive Involvement | 3.68 | 1.01 | 3.45 | .97 | 3.67 | .91 |
| Problem Solving Outcome | 2.42 | .81 | 2.46 | .88 | 2.51 | .70 |
| Inept Discipline | 4.19 | .67 | 4.05 | .78 | 4.23 | .66 |
| Effective Parenting | ||||||
| Composite Growth Score | 3.47 | .87 | 3.17 | .90 | 3.45 | .82 |
| Mothers’ Mental Health | ||||||
| Global Severity Index (GSI) | 56.14 | 37.57 | 42.03 | 36.99 | 37.80 | 38.41 |
Note:
Child Internalizing growth score construct computed from rescaling CDI, Levonn, and CFS 0 to 10.
Table 2.
Mean and Variance Components for Unconditional Growth Model of Child Indicators and Internalizing Construct
| Child Depression |
Child Distress |
Child Fears |
Adjustment Construct |
|
|---|---|---|---|---|
| Initial Status Intercept | ||||
| Mean | 3.37*** | 25.78*** | 33.13*** | 2.34*** |
| Variance | 8.83*** | 264.62*** | 274.04** | 1.52*** |
| Longitudinal Growth Rate | ||||
| Mean | −0.13*** | −0.61** | −0.73** | −0.05** |
| Variance | 0.06 | 0.55*** | 0.26† | 0.003† |
p < .001
p < .01
p < .05
p < .10
Focusing on the child outcomes, examination of the growth rate variance components indicated that the individual trajectories of child internalizing showed very similar patterns of adjustment, or decreasing problems, when comparing slopes across individual children with the exception of the Levonn measure of child distress (variance = .55, p < .001). Therefore, the data in Tables 1 and 2 indicated that the children in this sample were elevated in adjustment problems shortly following the IPV event, they exhibited significant individual differences in initial levels, but showed very similar patterns of adjustment over the 14 week assessment period. For the parenting construct and maternal distress mean scores shown in Table 1, similar growth analyses (models not shown for brevity) indicated that parenting was stable over time and did not exhibit mean growth or significant individual differences in trajectory variance. Maternal mental health symptoms, however, did show significant mean decrease and individual variance in change.
The next stage of multivariate analyses tested effects of child age, gender, mothers’ parenting and mental health on growth in child internalizing. For the initial status internalizing intercepts we entered T1 parenting and maternal mental health predictors. For estimating children’s growth rates from Time 1 to Time 3, we entered maternal parenting and maternal distress as predictors from Time 1 to Time 2. In addition, we entered the change scores for parenting and maternal distress controlling for Time 1 initial status. Specifying change scores and initial status as opposed to entering autoregressive Time 1 and Time 2 scores will result in estimates of true effects of baseline parenting and distress controlling for change and vice versa (see Kessler and Greenberg, 1981 for a discussion). Results of the prediction growth models are shown in Table 3 using HLM estimates of robust standard errors.
Table 3.
Unstandardized Beta Coefficients for Predictors of Initial Status Intercept and Growth Rate in Hierarchical Linear Growth Models
| Child Depression |
Child Distress |
Child Fears |
Internalizing Construct |
|
|---|---|---|---|---|
| T1 Initial Status Intercept as Outcome | ||||
| Intercept | 10.44** | 50.09* | 54.36** | 5.14** |
| T1 Child Age | −0.64** | −2.59* | −4.63** | −0.32** |
| T1 Child Gender (girl) | −0.46 | −5.30 | 7.81 | −0.17 |
| T1 Parenting Construct | −0.54 | 1.02 | 0.63 | −0.04 |
| T1 Maternal MH Construct | 0.32 | 0.61 | 1.27 | 0.10 |
| Longitudinal Growth Rate as Outcome | ||||
| Intercept | −0.05 | 0.83 | 0.40 | 0.04 |
| Child Age | 0.02† | 0.00 | 0.16 | 0.00 |
| Child Gender (girl) | −0.10 | 0.24 | −0.21 | 0.01 |
| T1 Parenting Construct | −0.01 | −0.65*** | −0.56* | −0.05** |
| Δ T2 Parenting | −0.00 | −0.12 | −0.03 | 0.00 |
| T1 Maternal MH Construct | −0.02 | 0.22** | 0.02 | 0.01 |
| Δ T2 Maternal Mental Health | 0.03 | 0.26* | 0.25† | 0.03† |
Note:T1 = Time 1; T2 = Time 2; Δ = Change from Time 1 to Time 2
p < .001
p < .01
p < .05
p < .10
Focusing on individual differences in initial status intercepts, holding the predictors constant, children’s internalizing problems were significantly different from zero and elevated for each of the indicators of child problems at baseline. Younger children across the board were more vulnerable to depressive symptoms (β = −.64, p <.01), distress (β = −2.59, p <.05), fears (β = −4.63, p <.01), and overall internalizing (β = −.32, p <.01). Child gender was not associated with initial levels. Neither baseline parenting nor mothers’ mental health was concurrently associated with the indicators or overall child internalizing construct.
Focusing on growth rate outcomes in Table 3, child age and gender were not associated with growth rates in child internalizing. Controlling for child gender older children exhibited marginally higher rates of growth in child depression measured by the CDI (β = .02, p < .10). Thus, while younger children were at higher risk at baseline, they did not adjust more poorly over time relative to older children.
For overall child internalizing, baseline level of parenting practices was the only significant predictor of change over time with higher levels of effective parenting predicting decreases in child internalizing problems (β = −.05, p <.01). Time 1 parenting also was associated with reductions in child distress (β = −.65, p <.001) and child fears (β = −.56, p <.01). Change in parenting from Time 1 to Time 2 was not predictive of growth, consistent with the data indicating that parenting was rather stable over the three time periods. Exploratory models (not shown) on average levels of parenting across the time period exhibited the same pattern of results. These data specifying initial status and change therefore indicate that mothers’ effective parenting shortly after the target IPV incident was the key protective factor for child adjustment.
For maternal mental health symptoms, change scores from T1 to T2 showed a more consistent pattern of prediction compared to baseline. Increases in maternal mental health symptoms were associated with growth in child distress symptoms (β = .26, p <.05), and marginally predicted growth in child fears (β =.25, p <.10) and the overall internalizing construct (β = .03,p <.10). Initial levels of maternal mental health symptoms predicted growth in child distress symptoms only (as measured by Levonn; β = .22, p <.01), not fears or depression.
As a final step we evaluated whether direct effects of maternal mental health symptoms were mediated by change in parenting to examine whether maternal distress had indirect effects through effective parenting. Examination of these models did not support findings of mediation. In summary, therefore, over time, effective parenting was the more proximal and significant protective factor associated with decreases in child adjustment problems controlling for maternal distress. To illustrate the effect of parenting on child adjustment, the fitted random effects slopes for the 25th, 50th, and 75th percentiles of effective parenting are plotted in Figure 1 controlling for covariates.
Figure 1.
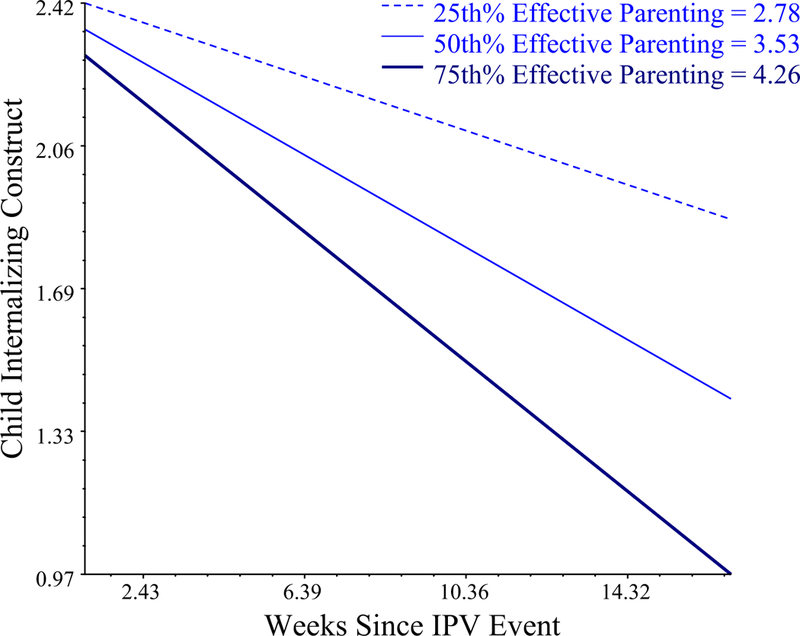
Random effects growth model plot of Time 1 Effective Parenting predicting reductions in Child Internalizing.
Discussion
In this short-term longitudinal study, mother’s parenting practices significantly influenced children’s recovery over the weeks following a severe IPV incid ent. These are the first data that we know of - with no method overlap among key variables - to describe short-term dynamic associations between observed parenting, maternal distress, and child functioning, following a violent incident. Our results provide preliminary support for the role of parenting as a key source of protection for children in the close aftermath of stressful and traumatic events, even events where the parent herself is the victim. Although we could find no other studies reporting on the association of parenting with short-term child internalizing trajectories, these findings are consistent with prior studies showing that effective parenting is protective in high-risk situations (Margolin & Gordis, 2000; Masten et al., 1999). The lack of concurrent association at baseline between parenting and child distress indicate that parenting may provide ‘banked’ protection for children (i.e., it may buffer the process of recovery, rather than a child’s distress in the immediate aftermath of a traumatic event, which may be more a function of multiple concurrent factors such as safety, coping resources, etc).
Of note, parenting and maternal distress were not related to each other, thus we did not find evidence for indirect effects of maternal distress on child internalizing through parenting. These findings are inconsistent with prior research on at-risk populations that demonstrated how maternal distress interferes with parenting, impairing child adjustment- for example, in samples of affectively ill mothers (Beardslee, Bemporad, Keller, & Klerman, 1983; Beardslee, Keller, Lavori, & Staley, 1993). However, the results are consistent with Levendosky et al.’s (2006) study of mothers and infants exposed to IPV which also yielded no associations between maternal mental health and parenting. Similar findings also were reported in a study examining relationships among parenting, child adjustment, and maternal mental health among highly stressed formerly homeless mothers (Gewirtz, DeGarmo, Plowman, August, & Realmuto, 2009).
At very high levels of parental distress, such as exhibited in this sample affected by recent violence, it appears that parenting may function somewhat ‘autonomously’ to parental distress, with both parenting and change in distress directly and uniquely influencing child internalizing. Indeed, these findings are consistent with one element of the conceptual model outlined earlier, which distinguishes the roles of mothers ‘as parent’ and ‘as person’. The model is illustrated in the anecdotal reports of individuals who describe working consciously to be effective parents in the aftermath of a traumatic event, to protect their child(ren), and to normalize daily life and routines. Such active attempts by mothers to effectively parent their children despite their own ‘mother as person’ stressors are reflected in the qualitative interviews of parenting of 95 battered women conducted by Levendosky and Graham-Bermann (2000), who noted that “some of the women appeared to be strengthening their defenses by increasing their sense of competency through parenting and focusing on parent ing” (2000, p. 257).
Baseline and growth in maternal mental health symptoms was significantly associated with growth in child distress, and in addition, growth in maternal distress was marginally associated (p<.10) with growth in fears, and overall internalizing. Relationships between maternal and child distress have been reported frequently in the trauma literature (e.g. Laor et al., 2001) but few studies have distinguished posttraumatic distress from other internalizing symptoms (i.e. depression, fears). Interestingly, child depression symptoms (unlike trauma- related distress or fears) were associated with neither parenting nor maternal distress. This may be for temporal reasons: fear and trauma-related distress symptoms may emerge more rapidly after a traumatic event compared to depression symptoms (LaGreca, Silverman, Vernberg, & Prinstein, 1996). Further research over a longer time period might shed light on the sequence of emergence of anxiety compared with depression symptoms.
In contrast to the significant decreases in child and maternal symptoms across the study period, mother’s parenting was stable across the study period. This finding is consistent with other studies suggesting that parenting practices remain fairly stable over the short term (e.g., Vuchinich, Bank, & Patterson, 1992 reported a stability coefficient of .83 for observed parental discipline over a 2 year period; Loeber, Burke, Lahey, Winters, & Zera, 2000). The finding of stability is interesting, however, in the context of a period of extreme disruption (domestic violence incident, entry into shelter and/or legal system, number of moves in this sample, etc). Longer-term data suggest that over extended time periods of family stress, parenting may be eroded (e.g. Forehand, Thomas, Wierson, Brody, & Fauber, 1990). Further research with larger, and representative samples will enable a more detailed examination of parenting over time.
Limitations
This present study had a small sample n of 35; although reliability and power is enhanced with the use of three repeated assessments, power to test indirect effects is limited and examination of moderators is precluded. Larger samples and replication are needed for further examination of relationships among maternal parenting, mental health and child adjustment in the aftermath contexts of domestic violence. In order to capture short-term changes in functioning shortly after a violent incident, data were collected from a convenience sample of women recently exposed to severe IPV, and from locations where such women were likely to receive services (i.e. courts and shelters). These data therefore do not necessarily generalize to a broader community samples of women exposed to (typically more mild) IPV, although other researchers have highlighted the value of studies more narrowly focused on specific types of violence (mild vs. severe; Jouriles et al., 2000; Kitzmann et al., 2003). Given the short-term nature of the study we did not sample characteristics of perpetrating partners, but nonetheless recognize the importance of gathering such data in the IPV context. Given these limitations, the present longitudinal inferences utilized temporal specification of predictors and employed multiple methods minimizing method overlap among predictors and outcomes (e.g., maternal report, observed parenting, and child report).
Research and Practice Implications
The results of this study contribute to the inchoate body of knowledge about the correlates of children’s short-term adjustment following a traumatic event. The separate but direct associations of parenting practices with child adjustment suggest that interventions targeting child adjustment shortly following traumatic events should focus on parenting as a protective process for child internalizing symptoms. Parenting interventions might be especially useful for those who have experienced traumatic events (e.g., violence) because of their focus on practicing and maintaining emotional regulation in family interactions (see, e.g., Gewirtz, Forgatch, & Wieling, 2008; Levendosky et al., 2006). These results also raise questions about the appropriate time to provide interventions for trauma-related distress. Data on early intervention indicate that if delivered too soon after an event, treatment may actually interfere with the individual’s natural recovery resources (e.g., Litz, 2004). In this study, much of the decrease in child internalizing occurred within about seven weeks of the violent incident (i.e., between Times 1 and 2, as noted in Table 1), which is consistent with research showing that cognitive- behavioral interventions offered at least 6 weeks after a traumatic event may improve outcomes in vulnerable populations (Shalev et al., 2008).
Acknowledgments
This work was supported in part by the University of Minnesota Graduate School, and by Grant P30 DA023920 from the Division of Epidemiology, Services and Prevention Branch, National Institute on Drug Abuse. We thank Professor Gloria Leon for her support, as well as Lisa Goldstein, and the many other students who worked on this project. In particular, we are grateful to the families who participated in this study, as well as the staff and administration at Tubman Family Alliance.
Footnotes
In this article we define IPV as acts of physical aggression between adult partners, although we of course acknowledge that IPV also includes acts of psychological aggression.
Contributor Information
Abigail H. Gewirtz, University of Minnesota.
David S. DeGarmo, Oregon Social Learning Center
Amanuel Medhanie, University of Minnesota.
References
- Beardslee WR, Bemporad J, Keller MB, & Klerman GL (1983). Children of parents with major affective disorder. American Journal of Psychiatry, 140, 825–832. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Keller MB, Lavori PW, Staley JE, & et al. (1993). The impact of parental affective disorder on depression in offspring: A longitudinal follow-up in a nonreferred sample. Journal of the American Academy of Child & Adolescent Psychiatry, 32, 723–730. [DOI] [PubMed] [Google Scholar]
- Brown J, Cohen P, Johnson JG, & Smailes EM (1999). Childhood Abuse and Neglect: Specificity ofz Effect on Adolescent and Young Depression and Suicidaliy. Journal of Amer Academy of Child & Adolescent Psychiatry, 38, 1490. [DOI] [PubMed] [Google Scholar]
- Cummings EM, & Davies P (1996). Emotional security as a regulatory process in normal development and the development of psychopathology. Development and Psychopathology, 8, 123–139. [Google Scholar]
- DeGarmo DS, Patterson GR, & Forgatch MS (2004). How do outcomes in a specified parent training Intervention maintain or wane over time? Prevention Science, 5, 73–89. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, & Spencer PM (1982). The brief symptom inventory (BSI): Administration, scoring and procedures manual: Baltimore: Johns Hopkins School of Medicine. [Google Scholar]
- Dutton MA, Holtzworth-Munroe A, Jouriles E, McDonald R, Krishnan S, McFarlane J, Sullivan C (2005). Recruitment and retention in intimate partner violence research. US Department of Justice, NCJ 201943. Downloaded on 4/01/10. [Google Scholar]
- Ehrensaft MK, Cohen P, Brown J, Smailes E, Chen H, & Johnson JG (2003).Intergenerational Transmission of Partner Violence: A 20-Year Prospective Study. Journal of Consulting and Clinical Psychology, 71, 741–753. [DOI] [PubMed] [Google Scholar]
- Fein JA, Kassam-Adams N, Vu T, & Datner EM (2001). Emergency department evaluation of acute stress disorder symptoms in violently injured youths. Annals of emergency medicine, 38, 391–396. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood L, & Lynskey MT (1996). Childhood sexual abuse and psychiatric disorder in young adulthood: II. Psychiatric outcomes of childhood sexual abuse. Journal of American Academy of Child & Adolescent Psychiatry, 35, 1365–1374. [DOI] [PubMed] [Google Scholar]
- Forehand R, Thomas AM, Wierson M, Brody G, & Fauber R (1990). Role of maternal functioning and parenting skills in adolescent functioning following parental divorce. Journal of Abnormal Psychology, 99, 278–283. [DOI] [PubMed] [Google Scholar]
- Forgatch MS, & DeGarmo D (2002). Extending and testing the social interaction learning model with divorce samples. Washington, DC: American Psychological Association. [Google Scholar]
- Forgatch MS, & DeGarmo DS (1999). Parenting Through Change: An effective prevention program for single mothers. Journal of Consulting and Clinical Psychology, 67, 711–724. [DOI] [PubMed] [Google Scholar]
- Gewirtz A, Forgatch M, & Wieling E (2008). Parenting practices as potential mechanisms for child adjustment following mass trauma. Journal Marital & Fam Therapy, 34, 177–192. [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, DeGarmo DS, Plowman EJ, August G, & Realmuto G (2009). Parenting, parental mental health, and child functioning in families residing in supportive housing. American Journal of Orthopsychiatry, 79(3), 336–347. [DOI] [PubMed] [Google Scholar]
- Grych JH, & Fincham FD (1990). Marital conflict and children’s adjustment: A cognitive- contextual framework. Psychological Bulletin, 108(2), 267–290. [DOI] [PubMed] [Google Scholar]
- Jouriles EN, McDonald R, Stephens N, Norwood W, Spiller LC, & Ware HS (1998). Breaking the cycle of violence: Helping families departing from battered women’s shelters. Washington, DC: American Psychological Association. [Google Scholar]
- Jouriles EN, Spiller LC, Stephens N, McDonald R, & Swank P (2000). Variability in adjustment of children of battered women: The role of child appraisals of interparent conflict. Cognitive Therapy and Research, 24, 233–249. [Google Scholar]
- Kassam-Adams N, & Winston FK (2004). Predicting child PTSD: the relationship between acute stress disorder and PTSD in injured children. Journal of Amer Academy of Child & Adolescent Psychiatry, 43, 403. [DOI] [PubMed] [Google Scholar]
- Kenardy JA, Webster RA, Lewin TJ, Carr VJ, Hazell PL, & Carter GL (1996). Stress debriefing and patterns of recovery following a natural disaster. Journal of Traumatic Stress, 9, 37–49. [DOI] [PubMed] [Google Scholar]
- Kessler RC, & Greenberg DF (1981). Linear panel analysis: Models of quantitative change: Academic Press. [Google Scholar]
- Kitzmann KM, Gaylord NK, Holt AR, & Kenny ED (2003). Child witnesses to domestic violence: A meta-analytic review. Journal of Consulting and Clinical Psychology, 71, 339–352. [DOI] [PubMed] [Google Scholar]
- Kovacs M (1981). Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica, 46, 305–315. [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Vernberg EM, & Prinstein MJ (1996). Symptoms of posttraumatic stress in children after Hurricane Andrew: A prospective study. Journal of Consulting and Clinical Psychology, 64, 712–723. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, & Wasserstein SB (1998). Children’s predisaster functioning as a predictor of posttraumatic stress following Hurricane Andrew. J Consult Clin Psychol, 66, 883–892. [DOI] [PubMed] [Google Scholar]
- Laor N, Wolmer L, & Cohen DJ (2001). Mothers’ functioning and children’s symptoms 5 years after a SCUD missile attack. American Journal of Psychiatry, 158, 1020. [DOI] [PubMed] [Google Scholar]
- Levendosky AA, & Graham-Bermann SA (2000). Behavioral observations of parenting in battered women. JFam Psychol, 14, 80–94. [DOI] [PubMed] [Google Scholar]
- Levendosky AA, Leahy KL, Bogat GA, Davidson WS, & von Eye A (2006). Domestic violence, maternal parenting, maternal mental health, and infant externalizing behavior. Journal of Family Psychology, 20, 544. [DOI] [PubMed] [Google Scholar]
- Lieberman AF, Van Horn P, & Ozer EJ (2005). Preschooler witnesses of marital violence: predictors and mediators of child behavior problems. DevPsychopathol, 17, 385–396. [DOI] [PubMed] [Google Scholar]
- Litz BT (2004). Early intervention for trauma and traumatic loss: The Guilford Press. [Google Scholar]
- Loeber R, Burke JD, Lahey BB, Winters A, & Zera M (2000). Oppositional defiant and conduct disorder: a review of the past 10 years, part I. Journal of Amer Academy of Child & Adolescent Psychiatry, 39, 1468. [DOI] [PubMed] [Google Scholar]
- Margolin G (1998). Effects of domestic violence on children. Violence against children in the family and the community, 57–101. [Google Scholar]
- Margolin G, & Gordis EB (2000). The effects of family and community violence on children. Annual Review of Psychology, 51, 445–479. [DOI] [PubMed] [Google Scholar]
- Masten AS, Hubbard JJ, Gest SD, Tellegen A, Garmezy N, & Ramirez M (1999). Competence in the context of adversity: pathways to resilience and maladaptation from childhood to late adolescence. Dev Psychopathol, 11, 143–169. [DOI] [PubMed] [Google Scholar]
- McCloskey LA, Figueredo AJ, & Koss MP (1995). The effects of systemic family violence on children’s mental health. Child Development, 66, 1239–1261. [PubMed] [Google Scholar]
- McDonald R, Jouriles EN, & Skopp NA (2006). Reducing conduct problems among children brought to women’s shelters: Intervention effects 24 months following termination of services. Journal of Family Psychology, 20, 127–136. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Wood JJ, & Weisz JR (2007). Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review, 27, 155–172. [DOI] [PubMed] [Google Scholar]
- Patterson GR (2005). The Next Generation of PMTO Models. Behavior Therapist, 28, 27–33. [Google Scholar]
- Perrin S, Smith P, & Yule W (2000). Practitioner review: The assessment and treatment of post-traumatic stress disorder in children and adolescents. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 41(03), 277–289. [PubMed] [Google Scholar]
- Pine DS, & Cohen JA (2002). Trauma in children and adolescents: risk and treatment of psychiatric sequelae. Biol Psychiatry, 51(7), 519–531. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Foster SL, Kent RN, & O’Leary K (1979). Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of Applied Behavior Analysis, 12(4), 691–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez M, Masten AS, & Miliotis D (1994). The fears of homeless children. University of Minnesota, Minneapolis, MN. [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods (Vol. 1). Thousand Oaks, CA: Sage. [Google Scholar]
- Richters JE, Martinez P, & Valla JP (1990). Levonn: A cartoon-based structured interview for assessing young children’s distress symptoms. Bethesda, MD: NIMH. [Google Scholar]
- Rossman BR, Bingham RD, & Emde RN (1997). Symptomatology and adaptive functioning for children exposed to normative stressors, dog attack, and parental violence. J Am Acad Child Adolesc Psychiatry, 36(8), 1089–1097. [DOI] [PubMed] [Google Scholar]
- Schafer JL, & W.Graham J (2002). Missing data: Our view of the state of the art. Psychological Methods, 7(2), 147–177. [PubMed] [Google Scholar]
- Shalev AY, Freedman S, Adesskey R, Errera Y, Peleg T, & Israeli-Shalev Y (2008, November). Prevention of PTSD by Early Treatment: A Randomized Controlled Trial. Poster presented at the International Society for Traumatic Stress Studies, Chicago, IL. [Google Scholar]
- Shaw JA, Applegate B, & Schorr C (1996). Twenty-one-month follow-up study of school-age children exposed to Hurricane Andrew. Journal of Amer Academy of Child & Adolescent Psychiatry, 35(3), 359. [DOI] [PubMed] [Google Scholar]
- Singer JD, & Willett JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press. [Google Scholar]
- Smith P, Perrin S, Yule W, & Rabe-Hesketh S (2001). War exposure and maternal reactions in the psychological adjustment of children from Bosnia-Hercegovina. Journal of Child Psychology and Psychiatry, 42(3), 395–404. [PubMed] [Google Scholar]
- Vuchinich S, Bank L, & Patterson GR (1992). Parenting, peers, and the stability of antisocial behavior in preadolescent boys. Developmental Psychology, 28(3), 510–521. [Google Scholar]
- Wolfe DA, Crooks CV, Lee V, McIntyre-Smith A, & Jaffe PG (2003). The effects of children’s exposure to domestic violence: A meta-analysis and critique. Clinical Child and Family Psychology Review, 6(3), 171–187. [DOI] [PubMed] [Google Scholar]
- Yates TM, Dodds MF, Sroufe LA, & Egeland B (2003). Exposure to partner violence and child behavior problems: A prospective study controlling for child physical abuse and neglect, child cognitive ability, socioeconomic status, and life stress. Development and Psychopathology, 15(01), 199–218. [DOI] [PubMed] [Google Scholar]


