Abstract
Traditional clinical care models focus on the measurement and normalization of individual organ systems and de-emphasize aspects of health related to the integration of physiologic systems. Measures of physical, cognitive and sensory, and psychosocial or emotional function predict important health outcomes like death and disability independently from the severity of a specific disease, cumulative co-morbidity, or disease severity measures. A growing number of clinical scientists in several subspecialties are exploring the utility of functional assessment to predict complication risk, indicate stress resistance, inform disease screening approaches and risk factor interpretation, and evaluate care. Because a substantial number of older adults in the community have some form of functional limitation, integrating functional assessment into clinical medicine could have a large impact. Although interest in functional implications for health and disease management is growing, the science underlying functional capacity, functional limitation, physical frailty, and functional metrics is often siloed among different clinicians and researchers, with fragmented concepts and methods. On August 25–26, 2016, participants at a trans-disciplinary workshop, supported by the National Institute on Aging and the John A. Hartford Foundation, explored what is known about the pathways, contributors, and correlates of physical, cognitive, and sensory functional measures across conditions and disease states; considered social determinants and health disparities; identified knowledge gaps, and suggested priorities for future research. This article summarizes those discussions.
Keywords: Cognition, Disability, Frailty, Physical performance
Function represents the integration of multiple physiologic systems against a background of specific disease manifestations, comorbidities, and age-related physiologic changes; its preservation is a top priority for older adults (1). As reported by the 2012 Medicare Current Beneficiary Survey (MCBS), limitation in activities of daily living (ADLs) or instrumental ADLs (IADLS) affect over 9 million older adults. Health care utilization and costs increase with the increasing degree and severity of limitation; thus, patients with functional limitations account for a disproportionate share of Medicare spending. Levels of physical and cognitive function inform risk prediction, disease screening strategies, and appropriate targeting and evaluation of care. Functional measures are among the patient-reported outcomes emphasized by the U.S. Food and Drug Administration. Thus, targeting functional outcomes in practice is important beyond those outcomes achievable through a strictly disease-based approach.
The traditional organ-centric model of medical care has yielded remarkable health advances, but the gains from this approach appear to be slowing. Indeed, the age-adjusted prevalence of ADL and IADL limitations has remained stable since 1997. An expanded clinical model embracing functional outcomes can exploit the power of gerontology and geriatrics, which focus on patients as integrated systems. Subspecialties such as cardiology and surgery have begun to embrace this approach, and interest in traditionally gerontological concepts such as frailty has grown rapidly in the subspecialties. Despite this interest, the science underlying function, functional limitation, and frailty is fragmented.
On August 25–26, 2016, a workshop, co-sponsored by the National Institute on Aging (NIA) and the John A. Hartford Foundation, was held in Arlington, Virginia to explore the pathways, contributors, and correlates of functional impairment across specialties. Bringing geriatricians and gerontologists together with researchers and specialists from other fields of medicine, the workshop addressed age-associated contributors, mechanisms, and correlates of functional decline. It also explored outcomes of functional limitation, including frailty, with respect to example conditions commonly seen in older adults. The workshop then addressed how functional limitation is measured, how those measures could be influenced by biologic hallmarks of aging and by environmental or sociocultural factors such as health disparities. Function is a facet of disablement models that also typically include environmental and societal factors. However, as the workshop’s primary aim was to explore ways to integrate functional limitation into basic, translational, and clinical research, environmental/societal determinants of disability were not emphasized.
Discussions, knowledge gaps, and potential priorities for future research are summarized in this article. “Function” is discussed as a domain that involves the integration of various systems. The workshop addressed four major domains of function: motor, cognitive, sensory, and emotional or psychosocial. In many disability models, “impairment” is seen to reflect deficits in specific physiologic, body, or organ system. This article focuses on “functional limitation,” to reflect diminished capacity in a functional domain.
Measuring Functional Limitation
Measures include self-report measures such as ADL scales and the 36-item Short Form Health Survey, and objective physical performance measures, which evaluate individuals’ capability as they perform specific tasks. Traditionally, measures of function have relied on participants’ report of their ability or difficulties in performing certain tasks or activities. It is important to distinguish “capability,” which refers to an individual’s ability to perform a task, from “activity,” the tasks an individual actually performs. The interpretation of what a task comprises is idiosyncratic, and answers may conflate the respondent’s capability to do a task with whether that task is something that the respondent might actually do. However, self-reported function is immediately relevant to the lived experience of the patient; it also is strongly associated with medical outcomes such as medical expenses, future disability, and mortality (2,3). A wide variety of potential scales and instruments measuring function have been poorly standardized across fields (4). The desire for more standardized measures has led to the increasing use of objective performance tests. Objective and subjective assessments have complementary roles and predict outcomes independently of each other.
Many simple measures, like gait speed, are highly reproducible, decline with age, and have been associated with multiple physiologic measures and health outcomes. For example, higher gait speed is associated with lower mortality risk: a pooled analysis across many cohorts showed that mortality risk decreases by 12% for each increase of 0.1 m/s in usual gait speed (5). Among 70-year-old patients undergoing bypass graft or valve replacement surgery, a gait speed below 0.83 m/s indicates significantly higher risk for post-operative complication (6). In the Health ABC study, the risk for mobility limitation increases log-linearly with decreasing gait speed without evidence of a threshold (7). Gait speed cut-points ranging from 0.6 to 1.0 m/s have been used to define increased risk for a variety of adverse outcomes (8,9). Gait speed has been used as an indicator of functional reserve by asking participants to walk at high speed or over long distances, as opposed to “usual” performance under conditions without stress. Other aspects of physical performance that predict adverse outcomes have also been studied (10).
The Short Physical Performance Battery (SPPB) assesses timed standing balance, timed 4 m walk at a usual pace, and time to rise from a chair five times, with a summary score ranging from 0 to 12. An SPPB score of 8–12 has been associated with shorter hospital stays among patients in a geriatric ward (11), and SPPB scores predict survival among patients receiving induction chemotherapy for acute myelogenous leukemia (12). In a cohort of injection drug users, HIV-negative users with low SPPB scores were two to three times more likely to die than those with higher SPPB scores and just as likely to die as HIV-positive users with high SPPB scores (13).
Performance measures can also be outcomes. In recent studies, SPPB scores were higher among hip fracture patients in comprehensive care programs than among those receiving usual care (14). SPPB scores correlated with measures of lower and upper extremity function in patients with multiple sclerosis (15) and with 6-m walk distance among stroke survivors (16). Thus, poor physical performance itself can be a target for intervention and a patient centered outcome of treatments for chronic conditions such as congestive heart failure and chronic obstructive pulmonary disease.
In many clinical situations, patients cannot participate in objective physical assessments or provide a self-reported assessment of function. It is common to ask caregivers or close relatives questions regarding the physical abilities of such patients. The validity of proxy responses to these questions depends on a subject’s perceptions about a task (eg, degree of difficulty) is not high (17). Validity improves when observable behaviors like using a cane are assessed (17). More work is needed to clarify which tools are most appropriate for which circumstances and to standardize tools to bridge medical subspecialties.
Frailty and Resilience
Frailty, defined as a state of reduced physiologic fitness resulting in vulnerability to stressors (18), encompasses multimorbidity, functional limitation, and geriatric syndromes, thus representing a compendium of interacting factors contributing to poorer health outcomes. Frailty often serves as a surrogate for health status and is better than chronologic age at predicting outcomes, and has been used to guide treatment and screening decisions. In a Canadian care model, an integrated plan for treatment and follow-up for a frail individual is guided by a comprehensive geriatric assessment (19) that assesses medical, psychological, and functional capacity (20). France has developed frailty referral clinics from a similar framework (21). Employment of such a model has been shown to improve mobility among home-dwelling patients older than 70 years with hip fractures (14). The Cochrane Library is conducting a systematic review of comprehensive geriatric assessments for improving outcomes in older patients admitted for surgery (22).
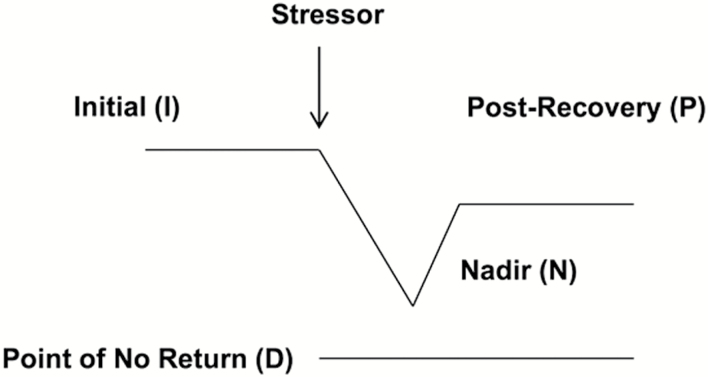
Performance measures have promise for understanding resiliency in response to stressors. As discussed at a 2015 National Institute on Aging workshop (23), a stressor such as an illness or accident causes functional decline from an initial level to a nadir, followed by some degree of recovery (Figure 1). Resilience can be considered as the degree and speed that patients regain baseline status following the stressor. Also important in this framework is the patient’s reserve, or the distance between initial status and the “point of no return,” and resistance, or how far patients fall from their initial functional state when exposed to a given stressor. The consideration of functional assessments as resilience indicators is only now receiving systematic attention.
Figure 1.
Framework for Functional Decline, Recovery, and Resilience. Following exposure to a stressor, patients decline from an initial level of function to a nadir, then recover. Resistance can be defined as the extent of functional loss to the nadir. Reserve can be defined as the distance between initial function and the point of no return. Resilience can be defined as the degree to which post-recovery function matches initial function. In some cases, patients can decline to a point of no return, leading to permanent disability or death.
Psychological resilience, or the ability to maintain positive affect regardless of a situation, has been associated with individual flexibility in neurochemical stress responses, genetic variants indirectly associated with exercise and physical function (24), and psychosocial mechanisms such as positive interpersonal relationships, stronger internal resources, and realistic expectations and achievable goals. Psychologically resilient individuals can respond to challenges by adjusting behavior, regaining equilibrium, and gaining knowledge, experience, and a stronger sense of well-being; they are less likely to succumb to mental or physical illness. However, the concept of psychological resilience has not received much attention in the medical subspecialty literature.
Subjective well-being (SWB) refers not only to generally feeling satisfied with life, but also to an experiential view in the context of an activity. The level of SWB declines later in life (25,26). Regardless of functional limitation, high life satisfaction has been associated with fewer doctor visits and higher use of preventive health care services (27), and fewer overnight hospitalizations (28). Individuals with disabilities spend less time on work and productive activities and more time on passive leisure (29), and they experience increased frustration and decreased activity-related happiness. Some aspects of emotional well-being are clearly associated with physical and emotional function (eg, depression and gait speed), but the connection between the physical, cognitive, and emotional domains remains underdeveloped (30).
Functional Decline: Age-Associated Contributors, Mechanisms, and Correlates
The Aging Brain
Age-related changes in the central nervous system contribute to poorer physical function (31). The integrity of integrated networks of brain regions that regulate walking, including the hippocampus and fronto-parietal subcortex (32), degrades with age. On neuroimaging, poorer mobility is associated with lower integrity of these networks as illustrated by more white matter hyperintensities in connecting tracts, smaller volume and lower micro-structural integrity of the gray matter, lower functional connectivity at rest, and higher pre-frontal cortex activation while patients are walking (33). These networks also regulate cognitive function, primarily information processing, memory and executive control (34,35). Several reports correlate cognitive function, primarily in executive function, verbal fluency, and memory, with impaired gait (36–38), supporting a relationship between cognition and walking in older adults without clinically overt neurologic conditions. Studies consistently report that slowing gait in community-dwelling older adults precedes and predicts cognitive decline in general (27,39–41), and mild cognitive impairment (MCI) (36,42,43), Alzheimer’s disease (36,44), and vascular dementia (36,39), in particular. Among older adults with normal cognition, physical task performance can deteriorate markedly if they are challenged by a cognitive task simultaneously. The degree of dual-task interference is related to the risk for falling (45). Critical illness is associated with cognitive impairment (46), and poorer cognitive function is a risk factor for delirium, which confers a poor prognosis for future physical and cognitive health (47). Klepin et al. (12) found that poor performance on the mini-mental status exam predicted early mortality in patients being treated for acute myelogenous leukemia, but more work is needed to understand how cognitive function relates to therapeutic responses and complication risks.
Sensory Impairment
Sensory loss across all five senses is strongly associated with older age (48). Similar to physical and cognitive functional decline, sensory impairment is often viewed as an inevitable consequence of aging, but there are strong associations with serious health outcomes such as disability, depression, falls and accidents, and cognitive impairment (49–52). Many older adults have multiple sensory impairments, and sensory loss often co-exists with other medical conditions (48,50,53,54). Comorbidity and sensory loss present a bidirectional challenge in management: comorbidities influence treatment plans and outcomes for sensory loss, while sensory loss affects patients’ ability to manage their comorbidities.
Do Biologic Hallmarks of Aging Explain the Utility of Functional Measures?
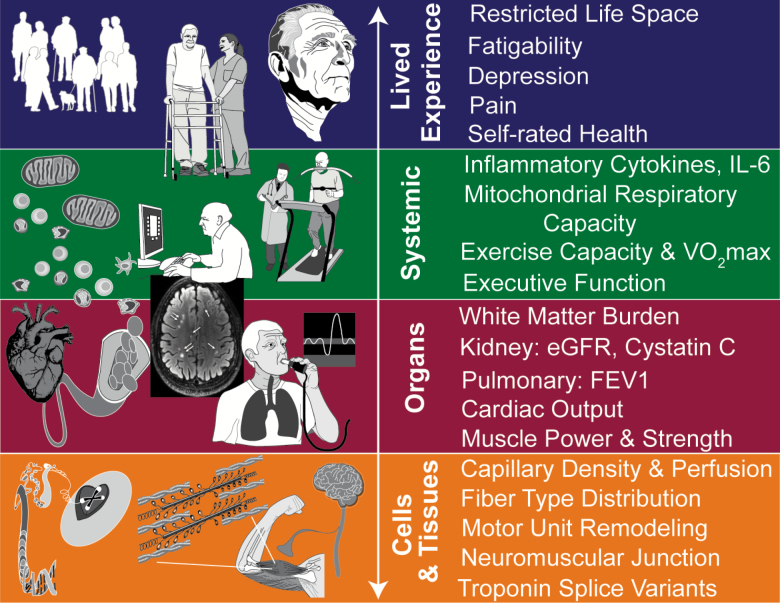
Functional measures might provide insight into the underlying biology of aging and its effect on the integration of physiologic systems. Indeed, slow gait reflects impairment at many levels of biologic organization, from the cellular level to the lived experience of older adults (Figure 2). Hence, it provides qualitatively different information about health than physiologic readouts of individual organ systems. The potential of new treatments targeting the biology of aging to improve or preserve function depends on the connection between aging biology and the integration of the systems that determine functional abilities.
Figure 2.
A functional measure like gait speed integrates information from cells to the lived patient experience.
Inflammation, Physical Limitation, and Frailty
Models suggest that clinically apparent functional decline and frailty are driven by interacting biologic changes and environmental influence, which in turn promote aging-associated changes in physiologic processes (55). Among these processes is inflammation; evidence suggests inflammation can influence physical function, frailty risk, clinical outcomes, and mortality. In a recent study, IL-6 and tumor necrosis factor alpha (TNF-α) receptor 1 levels were almost as predictive of 10-year mortality as age (56). Chronically elevated IL-6 signaling has been associated with mitochondrial dysfunction and fibrotic tissue changes through angiotensin II signaling (55). TNF-α drives further inflammatory activation and accelerates cell loss through apoptotic and necrotic signaling (57).
Senescent Cell Burden
Cell senescence increases with older age and may drive aging phenotypes such as reduced resilience and chronic disease development. Clearance of senescent cells enhances health span in older mice (58–60), and inhibitors of Jak signaling, critical to the maintenance of senescence, blunt the senescence-associated secretory phenotype and appear to be beneficial even after the onset of frailty (61). Thus, senescent cell burden may be a target for interventions to maintain function. Senolytics are drugs that reduce the accumulation of senescent cells and reverse senescence-associated upregulation of survival genes, and they appear to improve function and delay frailty in progeroid mice (58,62).
Mitochondrial Mass and Function
The effect of age on mitochondrial function, which plays a direct role in muscle function, is complex and poorly understood. The literature presents a conflicting view of age-associated changes in mitochondrial copy number, mitochondrial biogenesis, and mitophagy. Emerging evidence suggests some age-associated effects on the mitochondria. Within a single muscle fiber, mutations in the mitochondrial genome can accumulate with age (63) until they reach a phenotypic threshold leading to electron transport chain (ETC) deficiencies (64), triggering apoptosis and necrosis (65). Thus mutations in a single molecule can kill muscle fibers and contribute to sarcopenia. Stimulation of mitochondrial biogenesis dramatically increases the number of ETC-deficient muscle fibers and decreases the overall number of muscle fibers in older rats (66). Mitochondrial unfolded protein response-mediated activation of mitochondrial biogenesis propagates the accumulation of mitochondrial DNA mutations in C. elegans (67), and activation of AMPK contributes to mitochondrial dysfunction-associated senescence and the accumulation of senescent cells in Polg-mutator mice. Thus, deficits in energy production might be an important cause of declining function and relate to the high rates of adverse outcomes in persons with declining function.
Translational Animal Models
Though imperfect, animal models of functional limitation should allow for the evaluation of both decline and recovery, as the mechanisms governing these phases likely differ, and they should be used to assess function at appropriate ages. For example, the early phase of acute respiratory distress syndrome (ARDS) is associated with massive inflammation and muscle proteolysis, which can drive skeletal muscle atrophy and late-phase functional limitation (68). Almost all animal models of ARDS and sepsis use young mice, but the incidence and mortality of these syndromes increase almost exponentially with age, and there are marked differences when animals of different age are used (69–71). Development of a workable ARDS model in older mice has required a substantial reduction in lipopolysaccharide dose, versus that given to younger mice, to allow survival of a sufficient percentage of animals to study recovery (72).
A mouse model of health span, which integrates components from the motor, cognitive, vascular, inflammatory, and metabolic domains of health span (73–75), can be used in studies of late-life treatments and primary prevention. Several translatable assessments for health span are also available in other rodent models and in humans (Table 1).
Table 1.
Examples of Functional and Function-Supporting Measurements in Both Rodents and Humans
| Common Functional or Biomarker Measures |
|---|
| Aerobic exercise capacity (VO2max) |
| Autonomic nervous system (HRV; SNS activity) |
| Body composition (lean and fat mass; bone density; DXA, CT, MRI) |
| Body temperature |
| Cardiovascular (BP; pulse wave velocity; endothelial function; cardiac-echocardiography) |
| Cognitive function (executive function; memory; etc.) |
| Energy expenditure (metabolic rate); physical activity |
| Glucose tolerance; insulin sensitivity |
| Inflammation/oxidative stress (superoxide production; cytokines; antioxidants) |
| Kidney function (GFR; BUN; urinary protein) |
| Motor/physical function (strength; endurance; balance; coordination) |
| Pulmonary function |
| “Omics” (tissue biopsies; blood cells; platelets; plasma; serum; faeces; saliva; etc.) |
Functional Limitation and Outcomes across Important Conditions in Older Adults
Heart Failure
Heart failure incidence increases with age, and though early data focused on systolic heart (pump) failure, more recent data suggest the symptom complex of clinical heart failure as a composite of heart, lung, and muscle functions. Further, functional measures such as 6-min walk distance and peak VO2 on cardiopulmonary exercise testing strongly predict outcomes. Advanced understanding of physical function within the context of heart failure also illuminates mechanisms related to aging. Although cardiac disease entails key mechanisms of pathophysiology, it overlaps with age-associated changes in cellular, interstitial, vascular, and skeletal muscle physiology that exacerbate functional decrements (76). Contemporary clinical emphasis of transcatheter aortic valve replacement (TAVR) for older frail patients with aortic stenosis has placed greater focus on the interplay between aging and disease and functional metrics to delineate which cardiac patients will most likely benefit from the procedure. Gait speed stands out as a useful metric to delineate which older aortic stenosis patients will benefit from TAVR (77). Similar precepts extend to heart failure (78) and are even implicit in recent guidelines for managing heart failure patients in skilled nursing facilities (79). The best outcomes are observed in patients who can tolerate rehabilitation (ie, management contingent on functional attributes), rather than in those who achieve cardiocentric parameters (79).
Surgery
Although physical strength usually declines gradually with increasing age, it declines more precipitously after surgery and is followed by a gradual return to baseline with some rehabilitation. A return to ADLs and IADLs can take as long as 3–6 months (80). In one retrospective cohort study, almost a third of patients showed some loss of independence, as illustrated by decreased function, decreased mobility, or new care needs, following discharge (81). Interest in the surgical arena has focused primarily on frailty, or the end result of functional limitation. Among non-cardiac surgery patients, frailty increases the risk for 30-day complications by twofold, prolonged hospitalization by 1.49-fold, and discharge to an assisted care facility by 3.16-fold (82). Although the presence of frailty appears to improve the predictive power beyond traditional surgical risk measures, the value of multi-dimensional functional and frailty assessments (83) need to be demonstrated to facilitate their introduction into the pre-operative setting (83).
Single performance measures of functional status are easier to do and may be just as predictive. Among patients undergoing colorectal or cardiac surgeries, an up-and-go time of 15 s or longer is associated with increased mortality, complications, readmissions, and discharge to nursing facilities (84). Likewise, a 5-m walking speed of 6 s or longer has been associated with higher all-cause 30-day mortality, kidney injury, deep sternal wound infection, prolonged mechanical ventilation, and prolonged length of stay following cardiac surgery (77,85). Among patients who have undergone surgery for hip fracture, baseline grip strength has been associated with self-reported walking recovery (86), self-reported ADLs (87), and functional recovery and independence (88). Decreased self-reported mobility, as assessed by the video tool MAT-sf, has been associated with postoperative complications, time to discharge, and discharge to nursing facilities, even in non-frail patients (89).
Critical Care
Critical care can be viewed in two phases: phase 1, which encompasses events in the intensive care unit (ICU) itself, and phase 2, which encompasses post-discharge sequelae. While in the ICU, approximately 75% of patients develop delirium, and approximately 50–60% experience muscle-nerve “decoupling” (90,91). Arising from the critical illness itself, ICU-acquired neuromuscular dysfunction has a substantial impact on recovery (92–94) and has been associated with increased short- and long-term mortality, increased length of stay both in the ICU and the hospital overall, an inability to return to work, and increased costs.
Increased understanding of phase 1 critical care has led to the development of intense assessments within the ICU to address problems with over-sedation and immobility, and randomized controlled trials have found that phase 1 interventions reduce mortality by 15% and delirium by 25% (95,96). Despite the improved quality of care during phase 1, however, functional measures still have not been integrated into most ICU stays, and no long-term studies have combined cognitive and physical measures. In addition, the nomenclature with respect to ICU-acquired neuromuscular dysfunction has been disparate. Even the agreed-upon diagnosis, “ICU-acquired weakness,” (97) misses patients who show functional limitation but do not meet the established criteria, which do not address muscle fatigability or ICU-acquired frailty.
The events and pathophysiology that affect phase 2 recovery and care are even more poorly understood. The current concept of recovery time points is dictated more by paradigms of care than by the illness or condition. However, as illustrated by a study of hip fracture survivors, significant and meaningful differences in physical function can be evident long after rehabilitation (98). Although these later time points might represent an optimal time for recovery, they are currently ignored in clinical practice.
Health Disparities in Functional Assessment and Outcomes
As defined by the National Institute of Minority Health and Health Disparities, health disparities are unfair and avoidable (99) outcomes that adversely affect disparate populations (100) and are associated with social, economic, and environmental disadvantages. Identifying and addressing such disparities is important to both clinical practice and public health. As seen with the 2012 MCBS, the prevalence of functional limitation is higher among women, individuals older than 85 years, individuals from racial and ethnic minority groups, those with lower income, and those with less education. Black, Mexican American, Native Hawaiian, and Pacific Islander individuals are more likely to be affected by functional limitation than those who are White or Asian (101,102). Cognitive health, an important domain of overall functional status, also varies by race/ethnicity (103). These disparities can be apparent not only in the prevalence of risk factors for decline, but also in the relationship of those factors to the rate or overall severity of decline emphasizing the need diverse study populations.
Racial and ethnic cognitive disparities that appear in older age may reflect disadvantages across the entire life course (104) with differences in cognition evident at 65 years of age. However, much of the difference in overall function is also attributable to SES differences rather than race/ethnicity per se (105).
Sociocultural context impacts functional measures. The Nagi Disablement Process model suggests that disease leads to organ impairment, which in turn leads to functional limitation, defined as restrictions in basic physical and mental actions used in different situations in daily life. Functional limitation drives disability, or difficulty in performing activities associated with one’s social role in regular daily life. Thus, the disability driven by functional limitation involves an individual operating within a sociocultural and physical environment. Likewise, the International Classification of Functioning, Disability, and Health (ICF), adopted by the World Health Organization in the early 2000s, classifies health and health-related domains and includes environmental factors because an individual’s function and disability occur within a context. The San Antonio Longitudinal Study of Aging (SALSA) Disablement Process Model links variables within the disease-disability pathways and the contextual, psychosocial, and lifestyle modifiers to those variables (106). The model posits that racial and ethnic groups might differ with respect to processes underlying the same disease. Although race/ethnicity and SES interact in fundamental ways to explain observed health disparities in many of the leading causes of morbidity and mortality in the United States, little research has examined contributions to functional limitation across different diseases and conditions among older populations.
Integrating Functional Limitation into Clinical Research
Successful translation of research findings to clinical practice depends in large part on study designs that account for the baseline health and functional status of treatment groups; otherwise, studies will yield incorrect answers even with statistical adjustments. Like SES, physical and cognitive functional status is an important feature of baseline risk for adverse health outcomes, including mortality (107,108). For example, the Model for End-stage Liver Disease (MELD) score, which is based on physiologic measures, is used to determine which patients receive a liver transplant, but the SPPB strongly predicts waitlist survival, particularly among the oldest patients, over and above MELD score (109). Yet, the SPPB is not used in organ allocation or formal assessment of eligibility on a national level. Among patients initiating dialysis, the degree of mortality risk associated with non-ambulatory status is equivalent to that of four comorbidities (110). As an integrated measure of the end impact of disease, functional status cuts across diseases and can provide more information than laboratory markers or disease-specific measures. Thus, all studies that rely on prognostic inference should include measures of functional status, and failure to do so should render a study of uncertain value. Despite their importance, the integration of functional measures into research is challenged by how, what, and when to measure, as well as by constraints in time, money, and workflow.
Integration of functional measures into research also may be challenged by an under appreciation of how strongly function may influence risk for adverse outcomes. We do not often ask how high a proportion of risk is actually attributable to poor function. Attributable risk can aid in focusing interventions and characterizing the public health impact of poor function, as well as in translating functional measures into clinical and preventive practice. A librarian-assisted literature review shortly preceding the workshop found only 10 publications that had explored the fraction of adverse geriatric outcomes attributable to function-related measures, such as dementia, sarcopenia, or frailty. Attributable risk estimates assume causality. Few studies have intervened on functional limitation, however; thus, causal data are sparse and causal inferences are based on observational data. Statistical estimates of attributable risk often rely on relative risk and population estimates of prevalence for a risk factor (111). Methodologies to explicitly address causal effects on aging outcomes are needed.
NIA-supported cohort studies have collected extensive data on functional limitation measures; indeed, the commonly used frailty index was derived from one such study. In recognition of the research community’s need for common measures for many health and disease constructs, the NIH developed the NIH Toolbox (http://www.healthmeasures.net/explore-measurement-systems/nih-toolbox, Table 2), a multidimensional set of royalty-free measures to assess cognitive, motor, sensory, and emotional function in 2 h or less across various study designs and settings. Four domain-level batteries are available in English and Spanish and normed for ages 3–85 years. The NIH Toolbox has been built to be methodologically sound, diverse, dynamic, and adaptable to new technology, and minimally burdensome both to participants and investigators, and it uses state-of-the-art psychometric or computer-adaptive testing. It is not intended to substitute for individual measures investigators might use; rather, it is meant to enhance and add uniformity to their work. Frameworks within the toolbox and the overarching areas they include are listed in Table 2.
Table 2.
Domain Frameworks Within the NIH Toolbox
| Domain | Overarching Areas within the Domain Framework |
|---|---|
| Cognition | Executive function |
| Attention | |
| Episodic memory | |
| Language | |
| Processing speed | |
| Working memory | |
| Motor | Dexterity |
| Strength | |
| Balance | |
| Locomotion | |
| Endurance | |
| Sensation | Vision |
| Audition | |
| Gustation | |
| Somatosensation | |
| Vestibular | |
| Olfaction | |
| Emotion | Psychological well-being (positive affect, life satisfaction, meaning, and purpose) |
| Social relationships (social support, companionship, social distress, positive social development) | |
| Stress and self-efficacy (perceived stress, self-efficacy) | |
| Negative affect (fear, sadness, anger) |
Discussion and Future Directions
Function, which encompasses physical, cognitive, sensory, and psychosocial domains, predicts medically relevant outcomes across a wide range of disease contexts, independently of measures of disease severity and multimorbidity. Functional measures have been most commonly used in risk prediction, risk stratification, and treatment selection. However, these measures hold great promise to increase our understanding of stress resistance, biological age, and global integrated health. Functional measures tap into currently unmeasured aspects of physiology reflecting their severity and interactions. As such, they are likely to be useful in informing the management of clinical care of older adults.
The workshop identified knowledge gaps and made recommendations to accelerate our understanding in this area (Table 3). Progress in the field is slowed by the lack of agreement on which measures to use across clinical subspecialties. The lack of standardization impedes the ability to compare findings across subspecialties and slows the spread of innovation from one area of medicine to others. Activities geared at forming this consensus should be a high priority. Although workshop participants did not include representatives from the fields of rehabilitative science or rehabilitative care, efforts to form consensus should involve both these fields. Other fields, such as rheumatology, orthopedics, and neurology, are equally important and also should be included. Bridging conceptual models that guide research and care focused on function and disability, such as the Nagi, ICF, and other models, should also be an important priority in achieving consensus.
Table 3.
Research Needs to Advance Our Understanding of the Role of Functional Assessment in Clinical Care
| Research Needs | 1. Standard definitions for “impairment,” “functional limitations,” “disability,” and “dependence” to facilitate comparisons across specialties and national databases |
|
2. Purposeful study of racially, ethnically, and clinically diverse study populations incorporating standardized measures of socioeconomic status | |
| 3. Attention to functional measurements across a broader segment of the lifespan | |
| 4. Longitudinal studies to help identify physiologic impairments affecting test performance from age-related change including information relevant to elucidating underlying mechanisms at play (eg, mitochondrial function or senescent burden) | |
| 5. Incorporation of sensory and psychosocial health measures into clinical and epidemiological research | |
| 6. Standard incorporation of some kind of functional measures into primary and specialty care services and settings, clinical trials, and disease registries and other large care collaborations | |
| 7. New studies and methods to assess attributable risk associated with functional measures | |
| 8. Studies comparing the feasibility and value added of functional assessments across multiple domains in common clinical care contexts |
The biologic/physiologic basis of the function–outcome relationship is only partially understood. The workshop included several presentations on potential mechanisms that might explain the relationship, but much more work is needed to improve understanding so that these or other mechanisms might be specifically targeted for intervention development. For example, in the ICU, more studies of phase 1 interventions are needed in older adults and in conditions that represent accelerated aging, based on the potential for common biological mechanisms between ICU- and age-related loss of function.
The workshop considered many kinds of function. The existing research base rarely considers multiple functional domains at the same time. Moreover, sensory function and psychosocial function are scarcely measured at all. Research is needed to develop interventions that strengthen resilience at a time when resilience is low, to establish the impact of personality and genetics on resilience and determine how psychological resilience relates to physical resilience. In addition, research is needed to understand whether functional change across domains is independent or linked, and whether decline across different kinds of functions might reflect a more profound “latent trait” that could be studied in its own right. There are large gradients in function by race/ethnicity and economic status with functional limitations evident at earlier ages in disadvantaged groups. The basis of these differences needs to be better understood both as an end in itself, but also as a way of assessing potential drivers of functional decline. These gradients also suggest that the process of functional decline may begin early in the lifespan; these early processes also should be studied.
Work to date suggests that a performance-based measure like walking speed is valuable in predicting outcomes across several disease contexts. Indeed, several medical specialties appear to have adopted this measure. However, there are instances, for example in critical care, when performance testing is not feasible. In those cases, approaches that simulate or assess performance before the onset of critical illness are needed. It is unclear what measures beyond gait speed would also provide value in projecting clinical outcomes. Comparing the ability of measures from various domains to predict outcomes across common care settings would accelerate the uptake and understanding of the functional measures. This exercise would also allow the comparison of individual functional assessments with constructed measures like sarcopenia or frailty. One could also assess the feasibility of including several measures in each context to help balance the costs of introducing new measures against the knowledge gained. The settings examined should include acute care, routine primary care, and skilled nursing facilities.
There was consensus that any study of the current or future health of older persons should include functional measures, both as risk factors and as outcomes depending on the context in which they are used. The many options include both brief and in-depth measures across a variety of functional domains.
Functional measures can also provide a basis for patient-centered approaches to care. Patients want independence and improved quality of life; this depends primarily on functional capabilities. Evolving clinical practice paradigms should focus on medical interventions for this purpose. With that said, future research also should explore patients’ perceptions of function and be mindful of risks associated with those perceptions. For example, some individuals might resist cognitive assessments, because they fear being removed from their homes.
The integration of function into research and clinical practice across the subspecialties will require a shift from traditional medical silos to a coordinated, patient-centered approach. Standard terminology, including the term “functional limitation,” and uniform measures are needed, along with the willingness of investigators to agree upon and use these measures. Translation can be improved by: encouraging inclusion of functional measures in animal models; establishing standardized, non-proprietary methods informed by clinical colleagues; and improving the ability to perform serial longitudinal assessments with minimally or noninvasive procedures. Models should be validated as they are developed to mimic the functional decline seen in humans and to assess whether they can show meaningful changes with intervention.
This workshop identified the current lack of integration of functional assessment in the electronic health record as a major impediment to progress. Physical therapy, nursing home, and home care settings usually generate highly structured notes that include information from systematic assessments of functional status. However, function is not part of routine medical assessment in the clinic. Increased multidisciplinary collaboration, including access to existing data collections, is needed not only among mechanistic scientists, clinical scientists, and clinicians, but between these and other drivers of medicine, including patients, their families, care settings outside the clinic, and insurers.
Funding
This work was supported by a grant from the National Institute on Aging at the National Institutes of Health (grant number U13AG040938), with matching funds from the John A. Hartford Foundation (grant number 2016-0048). Dr. Schmader was supported by National Institute on Aging (NIA) P30 AG028716.
Supplementary Material
Acknowledgments
The authors, serving as the writing group for the contributors to and participants of the Workshop on Pathways, Contributors, and Correlates of Functional Impairment across Specialties, wish to thank the following speakers and moderators:
Karen Bandeen-Roche, Johns Hopkins University
Lisa Barnes, Rush University Medical Center
Kenneth Covinsky, University of California, San Francisco,
Luigi Ferrucci, National Institute on Aging
D. Clark Files, Wake Forest School of Medicine
Leanne Groban, Wake Forest School of Medicine
Helen Hazuda, University of Texas HSC at San Antonio
George Heckman, University of Waterloo
James Kirkland, Mayo Clinic, Rochester
Debra Reed-Gillette, Centers for Medicare and Medicaid Services
Barbara Resnick, University of Maryland School of Nursing
Caterina Rosano, University of Pittsburgh
Doug Seals, University of Colorado
Jacqui Smith, University of Michigan
Molly Wagster, National Institute on Aging
Jeremy Walston, Johns Hopkins University
Jonathan Wanagat, UCLA School of Medicine
Heather Whitson, Duke University Medical Center.
Conflict of interest
None declared.
References
- 1. Huang ES, Gorawara-Bhat R, Chin MH. Self-reported goals of older patients with type 2 diabetes mellitus. J Am Geriatr Soc. 2005;53: 306–311. doi:10.1111/j.1532-5415.2005.53119.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hardy SE, Kang Y, Studenski SA, Degenholtz HB. Ability to walk ¼ mile predicts subsequent disability, mortality, and health care costs. J Gen Intern Med. 2011;26:130–135. doi:10.1007/s11606-010-1543-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beauchamp MK, Schmidt CT, Pedersen MM, Bean JF, Jette AM. Psychometric properties of the late-life function and disability instrument: a systematic review. BMC Geriatr. 2014;14:12. doi:10.1186/1471-2318-14-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Guralnik JM, Patel K, Ferrucci L. Assessing functional status and disability in epidemiologic studies. In: Newman AB, Cauley JA, eds. The Epidemiology of Aging. Dordrecht: Springer; 2012:91–117. doi:10.1007/978-94-007-5061-6_7 [Google Scholar]
- 5. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi:10.1001/jama.2010.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Afilalo J, Mottillo S, Eisenberg MJ, et al. Addition of frailty and disability to cardiac surgery risk scores identifies elderly patients at high risk of mortality or major morbidity. Circ Cardiovasc Qual Outcomes. 2012;5: 222–228. doi:10.1161/CIRCOUTCOMES.111.963157 [DOI] [PubMed] [Google Scholar]
- 7. Cesari M, Kritchevsky SB, Penninx BW, et al. Prognostic value of usual gait speed in well-functioning older people–results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:1675–1680. doi:10.1111/j.1532-5415.2005.53501.x [DOI] [PubMed] [Google Scholar]
- 8. Cummings SR, Studenski S, Ferrucci L. A diagnosis of dismobility–giving mobility clinical visibility: a mobility working group recommendation. JAMA. 2014;311:2061–2062. doi:10.1001/jama.2014.3033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rolland YM, Cesari M, Miller ME, Penninx BW, Atkinson HH, Pahor M. Reliability of the 400-m usual-pace walk test as an assessment of mobility limitation in older adults. J Am Geriatr Soc. 2004;52:972–976. doi:10.1111/j.1532-5415.2004.52267.x [DOI] [PubMed] [Google Scholar]
- 10. Ward RE, Beauchamp MK, Latham NK, et al. Neuromuscular impairments contributing to persistently poor and declining lower-extremity mobility among older adults: new findings informing geriatric rehabilitation. Arch Phys Med Rehabil. 2016;97:1316–1322. doi:10.1016/j.apmr.2016.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Volpato S, Cavalieri M, Guerra G, et al. Performance-based functional assessment in older hospitalized patients: feasibility and clinical correlates. J Gerontol A Biol Sci Med Sci. 2008;63:1393–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Klepin HD, Geiger AM, Tooze JA, et al. Geriatric assessment predicts survival for older adults receiving induction chemotherapy for acute myelogenous leukemia. Blood. 2013;121:4287–4294. doi:10.1182/blood-2012-12-471680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Greene M, Covinsky K, Astemborski J, et al. The relationship of physical performance with HIV disease and mortality. AIDS. 2014;28:2711–2719. doi:10.1097/QAD.0000000000000507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Prestmo A, Hagen G, Sletvold O, et al. Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet. 2015;385:1623–1633. doi:10.1016/S0140-6736(14)62409-0 [DOI] [PubMed] [Google Scholar]
- 15. Motl RW, Learmonth YC, Wójcicki TR, et al. Preliminary validation of the short physical performance battery in older adults with multiple sclerosis: secondary data analysis. BMC Geriatr. 2015;15:157. doi:10.1186/s12877-015-0156-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stookey AD, Katzel LI, Steinbrenner G, Shaughnessy M, Ivey FM. The short physical performance battery as a predictor of functional capacity after stroke. J Stroke Cerebrovasc Dis. 2014;23:130–135. doi:10.1016/j.jstrokecerebrovasdis.2012.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gruber-Baldini AL, Shardell M, Lloyd KD, Magaziner J “Use of Proxies and Informants”. In: Newman AB, Cauley JA, eds. The Epidemiology of Aging. Dordrect: Springer; 2012:91–90. doi:10.1007/978-94-007-5061-6_6 [Google Scholar]
- 18. Bergman H, Ferrucci L, Guralnik J, et al. Frailty: an emerging research and clinical paradigm–issues and controversies. J Gerontol A Biol Sci Med Sci. 2007;62:731–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Abellan van Kan G, Rolland Y, Houles M, Gillette-Guyonnet S, Soto M, Vellas B. The assessment of frailty in older adults. Clin Geriatr Med. 2010;26:275–286. doi:10.1016/j.cger.2010.02.002 [DOI] [PubMed] [Google Scholar]
- 20. Beaulieu MD, Haggerty J, Tousignant P, et al. Characteristics of primary care practices associated with high quality of care. CMAJ. 2013;185: E590–E596. doi:10.1503/cmaj.121802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cesari M, Vellas B. Frailty in clinical practice. Nestle Nutr Inst Workshop Ser. 2015;83:93–98. doi:10.1159/000382091 [DOI] [PubMed] [Google Scholar]
- 22. Eamer G, Taheri A, Daviduck Q, Chambers T, Shi X, Khadaroo RG. Comprehensive geriatric assessment for improving outcomes in elderly patients admitted to a surgical service. Cochrane Database Syst Rev. 2018;1:1–45. doi:10.1002/14651858.CD012485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hadley E, Kuchel GA, Newman AB, et al. Report: NIA workshop on measures of physiologic resiliencies in human aging. J Gerontol A Biol Sci Med Sci. 2017;72:980–990. doi:10.1093/gerona/glx015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Resnick B, Klinedinst NJ, Yerges-Armstrong L, Choi EY, Dorsey SG. The impact of genetics on physical resilience and successful aging. J Aging Health. 2015;27:1084–1104. doi:10.1177/0898264315577586 [DOI] [PubMed] [Google Scholar]
- 25. Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385:640–648. doi:10.1016/S0140-6736(13)61489-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gerstorf D, Ram N, Mayraz G, et al. Late-life decline in well-being across adulthood in Germany, the United Kingdom, and the United States: something is seriously wrong at the end of life. Psychol Aging. 2010;25: 477–485. doi:10.1037/a0017543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kim ES, Park N, Sun JK, Smith J, Peterson C. Life satisfaction and frequency of doctor visits. Psychosom Med. 2014;76:86–93. doi:10.1097/PSY.0000000000000024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sun JK, Kim ES, Smith J. Positive self-perceptions of aging and lower rate of overnight hospitalization in the US population over age 50. Psychosom Med. 2017;79:81–90. doi:10.1097/PSY.0000000000000364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Anand P, Ben-Shalom Y. How do working-age people with disabilities spend their time? New evidence from the American Time Use Survey. Demography. 2014;51:1977–1998. doi:10.1007/s13524-014-0336-3 [DOI] [PubMed] [Google Scholar]
- 30. Smith J, Ryan LH, Queen TL, Becker S, Gonzalez R. Snapshots of mixtures of affective experiences in a day: findings from the health and retirement study. J Popul Ageing. 2014;7:55–79. doi:10.1007/s12062-014-9093-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sorond FA, Cruz-Almeida Y, Clark DJ, et al. Aging, the central nervous system, and mobility in older adults: neural mechanisms of mobility impairment. J Gerontol A Biol Sci Med Sci. 2015;70:1526–1532. doi:10.1093/gerona/glv130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Capaday C. The special nature of human walking and its neural control. Trends Neurosci. 2002;25:370–376. [DOI] [PubMed] [Google Scholar]
- 33. Holtzer R, Wang C, Verghese J. The relationship between attention and gait in aging: facts and fallacies. Motor Control. 2012;16:64–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fehr T. A hybrid model for the neural representation of complex mental processing in the human brain. Cogn Neurodyn. 2013;7:89–103. doi:10.1007/s11571-012-9220-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Vendetti MS, Bunge SA. Evolutionary and developmental changes in the lateral frontoparietal network: a little goes a long way for higher-level cognition. Neuron. 2014;84:906–917. doi:10.1016/j.neuron.2014.09.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Verghese J, Wang C, Lipton RB, Holtzer R, Xue X. Quantitative gait dysfunction and risk of cognitive decline and dementia. J Neurol Neurosurg Psychiatry. 2007;78:929–935. doi:10.1136/jnnp.2006.106914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Montero-Odasso M, Verghese J, Beauchet O, Hausdorff JM. Gait and cognition: a complementary approach to understanding brain function and the risk of falling. J Am Geriatr Soc. 2012;60:2127–2136. doi:10.1111/j.1532-5415.2012.04209.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Martin KL, Blizzard L, Wood AG, et al. Cognitive function, gait, and gait variability in older people: a population-based study. J Gerontol A Biol Sci Med Sci. 2013;68:726–732. doi:10.1093/gerona/gls224 [DOI] [PubMed] [Google Scholar]
- 39. Verghese J, Lipton RB, Hall CB, Kuslansky G, Katz MJ, Buschke H. Abnormality of gait as a predictor of non-Alzheimer’s dementia. N Engl J Med. 2002;347:1761–1768. doi:10.1056/NEJMoa020441 [DOI] [PubMed] [Google Scholar]
- 40. Verghese J, Wang C, Lipton RB, Holtzer R. Motoric cognitive risk syndrome and the risk of dementia. J Gerontol A Biol Sci Med Sci. 2013;68:412–418. doi:10.1093/gerona/gls191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Best JR, Liu-Ambrose T, Boudreau RM, et al. An Evaluation of the longitudinal, bidirectional associations between gait speed and cognition in older women and men. J Gerontol A Biol Sci Med Sci. 2016;71:1616–1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Albers MW, Gilmore GC, Kaye J, et al. At the interface of sensory and motor dysfunctions and Alzheimer’s disease. Alzheimers Dement. 2015;11:70–98. doi:10.1016/j.jalz.2014.04.514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dumurgier J, Artaud F, Touraine C, et al. Gait speed and decline in gait speed as predictors of incident dementia. J Gerontol A Biol Sci Med Sci. 2017;72:655–661. doi:10.1093/gerona/glw110 [DOI] [PubMed] [Google Scholar]
- 44. Aggarwal NT, Wilson RS, Beck TL, Bienias JL, Bennett DA. Motor dysfunction in mild cognitive impairment and the risk of incident Alzheimer disease. Arch Neurol. 2006;63:1763–1769. doi:10.1001/archneur.63.12.1763 [DOI] [PubMed] [Google Scholar]
- 45. Herman T, Mirelman A, Giladi N, Schweiger A, Hausdorff JM. Executive control deficits as a prodrome to falls in healthy older adults: a prospective study linking thinking, walking, and falling. J Gerontol A Biol Sci Med Sci. 2010;65:1086–1092. doi:10.1093/gerona/glq077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Baumbach P, Meissner W, Guenther A, Witte OW, Götz T. Perceived cognitive impairments after critical illness: a longitudinal study in survivors and family member controls. Acta Anaesthesiol Scand. 2016;60:1121–1130. doi:10.1111/aas.12755 [DOI] [PubMed] [Google Scholar]
- 47. Pendlebury ST, Lovett NG, Smith SC, et al. Observational, longitudinal study of delirium in consecutive unselected acute medical admissions: age-specific rates and associated factors, mortality and re-admission. BMJ Open. 2015;5:e007808. doi:10.1136/bmjopen-2015-007808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Correia C, Lopez KJ, Wroblewski KE, et al. Global sensory impairment in older adults in the United States. J Am Geriatr Soc. 2016;64:306–313. doi:10.1111/jgs.13955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. National Academies of Sciences, Engineering, and Medicine;. Hearing Health Care for Adults: Priorities for Improving Access and Affordability. Washington, DC: The National Academies Press; 2016. [PubMed] [Google Scholar]
- 50. National Academies of Sciences, Engineering and Medicine. Making Eye Health a Population Health Imperative: Vision for Tomorrow. Washington, DC: The National Academies Press; 2016. [PubMed] [Google Scholar]
- 51. Reuben DB, Mui S, Damesyn M, Moore AA, Greendale GA. The prognostic value of sensory impairment in older persons. J Am Geriatr Soc. 1999;47:930–935. [DOI] [PubMed] [Google Scholar]
- 52. Miwa T, Furukawa M, Tsukatani T, Costanzo RM, DiNardo LJ, Reiter ER. Impact of olfactory impairment on quality of life and disability. Arch Otolaryngol Head Neck Surg. 2001;127:497–503. [DOI] [PubMed] [Google Scholar]
- 53. Fischer ME, Cruickshanks KJ, Klein BE, Klein R, Schubert CR, Wiley TL. Multiple sensory impairment and quality of life. Ophthalmic Epidemiol. 2009;16:346–353. doi:10.3109/09286580903312236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Whitson HE, Cousins SW, Burchett BM, Hybels CF, Pieper CF, Cohen HJ. The combined effect of visual impairment and cognitive impairment on disability in older people. J Am Geriatr Soc. 2007;55:885–891. doi:10.1111/j.1532-5415.2007.01093.x [DOI] [PubMed] [Google Scholar]
- 55. Walston JD. Connecting age-related biological decline to frailty and late-life vulnerability. Nestle Nutr Inst Workshop Ser. 2015;83:1–10. doi:10.1159/000382052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Varadhan R, Yao W, Matteini A, et al. Simple biologically informed inflammatory index of two serum cytokines predicts 10 year all-cause mortality in older adults. J Gerontol A Biol Sci Med Sci. 2014;69:165–173. doi:10.1093/gerona/glt023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kearney CJ, Martin SJ. An inflammatory perspective on necroptosis. Mol Cell. 2017;65:965–973. doi:10.1016/j.molcel.2017.02.024 [DOI] [PubMed] [Google Scholar]
- 58. Zhu Y, Tchkonia T, Pirtskhalava T, et al. The Achilles’ heel of senescent cells: from transcriptome to senolytic drugs. Aging Cell. 2015;14:644–658. doi:10.1111/acel.12344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Xu M, Palmer AK, Ding H, et al. Targeting senescent cells enhances adipogenesis and metabolic function in old age. Elife. 2015;4:e12997. doi:10.7554/eLife.12997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Roos CM, Zhang B, Palmer AK, et al. Chronic senolytic treatment alleviates established vasomotor dysfunction in aged or atherosclerotic mice. Aging Cell. 2016;15:973–977. doi:10.1111/acel.12458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Xu M, Tchkonia T, Ding H, et al. JAK inhibition alleviates the cellular senescence-associated secretory phenotype and frailty in old age. Proc Natl Acad Sci U S A. 2015;112:E6301–E6310. doi:10.1073/pnas.1515386112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Zhu Y, Tchkonia T, Fuhrmann-Stroissnigg H, et al. Identification of a novel senolytic agent, navitoclax, targeting the Bcl-2 family of anti-apoptotic factors. Aging Cell. 2016;15:428–435. doi:10.1111/acel.12445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Wanagat J, Cao Z, Pathare P, Aiken JM. Mitochondrial DNA deletion mutations colocalize with segmental electron transport system abnormalities, muscle fiber atrophy, fiber splitting, and oxidative damage in sarcopenia. FASEB J. 2001;15:322–332. doi:10.1096/fj.00-0320com [DOI] [PubMed] [Google Scholar]
- 64. Herbst A, Pak JW, McKenzie D, Bua E, Bassiouni M, Aiken JM. Accumulation of mitochondrial DNA deletion mutations in aged muscle fibers: evidence for a causal role in muscle fiber loss. J Gerontol A Biol Sci Med Sci. 2007;62:235–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cheema N, Herbst A, McKenzie D, Aiken JM. Apoptosis and necrosis mediate skeletal muscle fiber loss in age-induced mitochondrial enzymatic abnormalities. Aging Cell. 2015;14:1085–1093. doi:10.1111/acel.12399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Herbst A, Wanagat J, Cheema N, Widjaja K, McKenzie D, Aiken JM. Latent mitochondrial DNA deletion mutations drive muscle fiber loss at old age. Aging Cell. 2016;15:1132–1139. doi:10.1111/acel.12520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lin YF, Schulz AM, Pellegrino MW, Lu Y, Shaham S, Haynes CM. Maintenance and propagation of a deleterious mitochondrial genome by the mitochondrial unfolded protein response. Nature. 2016;533:416–419. doi:10.1038/nature17989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Files DC, Sanchez MA, Morris PE. A conceptual framework: the early and late phases of skeletal muscle dysfunction in the acute respiratory distress syndrome. Crit Care. 2015;19:266. doi:10.1186/s13054-015-0979-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Cooke CR, Erickson SE, Watkins TR, Matthay MA, Hudson LD, Rubenfeld GD. Age-, sex-, and race-based differences among patients enrolled versus not enrolled in acute lung injury clinical trials. Crit Care Med. 2010;38:1450–1457. doi:10.1097/CCM.0b013e3181de451b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Rubenfeld GD, Caldwell E, Peabody E, et al. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353:1685–1693. doi:10.1056/NEJMoa050333 [DOI] [PubMed] [Google Scholar]
- 71. Ely EW, Wheeler AP, Thompson BT, Ancukiewicz M, Steinberg KP, Bernard GR. Recovery rate and prognosis in older persons who develop acute lung injury and the acute respiratory distress syndrome. Ann Intern Med. 2002;136:25–36. [PubMed] [Google Scholar]
- 72. Files DC, Ilaiwy A, Perry TL, et al. Lung injury-induced skeletal muscle wasting in aged mice is linked to alterations in long chain fatty acid metabolism. Metabolomics. 2016;12:134. doi:10.1007/s11306-016-1079-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Justice J, Miller JD, Newman JC, et al. Frameworks for proof-of-concept clinical trials of interventions that target fundamental aging processes. J Gerontol A Biol Sci Med Sci. 2016;71:1415–1423. doi:10.1093/gerona/glw126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Richardson A, Fischer KE, Speakman JR, et al. Measures of healthspan as indices of aging in mice-a recommendation. J Gerontol A Biol Sci Med Sci. 2016;71:427–430. doi:10.1093/gerona/glv080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Seals DR, Melov S. Translational geroscience: emphasizing function to achieve optimal longevity. Aging (Albany NY). 2014;6:718–730. doi:10.18632/aging.100694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Fleg JL, Morrell CH, Bos AG, et al. Accelerated longitudinal decline of aerobic capacity in healthy older adults. Circulation. 2005;112:674–682. doi:10.1161/CIRCULATIONAHA.105.545459 [DOI] [PubMed] [Google Scholar]
- 77. Alfredsson J, Stebbins A, Brennan JM, et al. Gait speed predicts 30-day mortality after transcatheter aortic valve replacement: results from the society of thoracic surgeons/American college of cardiology transcatheter valve therapy registry. Circulation. 2016;133:1351–1359. doi:10.1161/CIRCULATIONAHA.115.020279 [DOI] [PubMed] [Google Scholar]
- 78. Pulignano G, Del Sindaco D, Di Lenarda A, et al. Incremental value of gait speed in predicting prognosis of older adults with heart failure: insights from the IMAGE-HF study. JACC Heart Fail. 2016;4:289–298. doi:10.1016/j.jchf.2015.12.017 [DOI] [PubMed] [Google Scholar]
- 79. Jurgens CY, Goodlin S, Dolansky M, et al. Heart failure management in skilled nursing facilities: a scientific statement from the American Heart Association and the Heart Failure Society of America. Circ Heart Fail. 2015;8:655–687. doi:10.1016/j.cardfail.2015.02.007 [DOI] [PubMed] [Google Scholar]
- 80. Lawrence VA, Hazuda HP, Cornell JE, et al. Functional independence after major abdominal surgery in the elderly. J Am Coll Surg. 2004;199:762–772. doi:10.1016/j.jamcollsurg.2004.05.280 [DOI] [PubMed] [Google Scholar]
- 81. Berian JR, Mohanty S, Ko CY, Rosenthal RA, Robinson TN. Association of loss of independence with readmission and death after discharge in older patients after surgical procedures. JAMA Surg. 2016;151:e161689. doi:10.1001/jamasurg.2016.1689 [DOI] [PubMed] [Google Scholar]
- 82. Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210:901–908. doi:10.1016/j.jamcollsurg.2010.01.028 [DOI] [PubMed] [Google Scholar]
- 83. Partridge JS, Harari D, Dhesi JK. Frailty in the older surgical patient: a review. Age Ageing. 2012;41:142–147. doi:10.1093/ageing/afr182 [DOI] [PubMed] [Google Scholar]
- 84. Robinson TN, Wu DS, Sauaia A, et al. Slower walking speed forecasts increased postoperative morbidity and 1-year mortality across surgical specialties. Ann Surg. 2013;258:582–8; discussion 588. doi:10.1097/SLA.0b013e3182a4e96c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Afilalo J, Kim S, O’Brien S, et al. Gait speed and operative mortality in older adults following cardiac surgery. JAMA Cardiol. 2016;1:314–321. doi:10.1001/jamacardio.2016.0316 [DOI] [PubMed] [Google Scholar]
- 86. Savino E, Martini E, Lauretani F, et al. Handgrip strength predicts persistent walking recovery after hip fracture surgery. Am J Med. 2013;126:1068–75.e1. doi:10.1016/j.amjmed.2013.04.017 [DOI] [PubMed] [Google Scholar]
- 87. Wehren LE, Hawkes WG, Hebel JR, Orwig DL, Magaziner J. Bone mineral density, soft tissue body composition, strength, and functioning after hip fracture. J Gerontol A Biol Sci Med Sci. 2005;60:80–84. [DOI] [PubMed] [Google Scholar]
- 88. Beloosesky Y, Weiss A, Manasian M, Salai M. Handgrip strength of the elderly after hip fracture repair correlates with functional outcome. Disabil Rehabil. 2010;32:367–373. doi:10.3109/09638280903168499 [DOI] [PubMed] [Google Scholar]
- 89. Kim S, Marsh AP, Rustowicz L, et al. Self-reported mobility in older patients predicts early postoperative outcomes after elective noncardiac surgery. Anesthesiology. 2016;124:815–825. doi:10.1097/ALN.0000000000001011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Brummel NE, Bell SP, Girard TD, et al. Frailty and subsequent disability and mortality among patients with critical illness. Am J Respir Crit Care Med. 2017;196:64–72. doi:10.1164/rccm.201605-0939OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369:1306–1316. doi:10.1056/NEJMoa1301372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Hermans G, Van Mechelen H, Clerckx B, et al. Acute outcomes and 1-year mortality of intensive care unit-acquired weakness. A cohort study and propensity-matched analysis. Am J Respir Crit Care Med. 2014;190:410–420. doi:10.1164/rccm.201312-2257OC [DOI] [PubMed] [Google Scholar]
- 93. Ali NA, O’Brien JM Jr., Hoffmann SP, et al. Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med. 2008;178:261–268. doi:10.1164/rccm.200712-1829OC [DOI] [PubMed] [Google Scholar]
- 94. Cheung AM, Tansey CM, Tomlinson G, et al. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;174:538–544. doi:10.1164/rccm.200505-693OC [DOI] [PubMed] [Google Scholar]
- 95. Barnes-Daly M, Phillips G, Ely EW. Improving hospital survival and reducing brain dysfunction at seven California community hospitals: implementing PAD guidelines via the ABCDEF bundle in 6,064 patients. Crit Care Med. 2017;45:171–178. doi:10.1097/CCM0000000000002149 [DOI] [PubMed] [Google Scholar]
- 96. Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014;42:1024–1036. doi:10.1097/CCM0000000000000129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Stevens RD, Marshall SA, Cornblath DR, et al. A framework for diagnosing and classifying intensive care unit-acquired weakness. Crit Care Med. 2009;37(10 Suppl):S299–S308. doi:10.1097:CCM.0b013e3181b6ef67 [DOI] [PubMed] [Google Scholar]
- 98. Edgren J, Salpakoski A, Sihvonen SE, et al. Effects of a home-based physical rehabilitation program on physical disability after hip fracture: a randomized controlled trial. J Am Med Dir Assoc. 2015;16:350.e1–350.e7. doi:10.1016/j.jamda.2014.12.015 [DOI] [PubMed] [Google Scholar]
- 99. World Health Organization. Social Determinants of Health 2016. http://who.int/topics/social_determinants/en/. Accessed September 19, 2016.
- 100. Perez-Stable E. NIMHD Vision and Research Agenda. 2016. https://www.nimhd.nih.gov/about/legislative-info/clips/nimhd-vision.html. Accessed December 31, 2017. [Google Scholar]
- 101. Fuller-Thomson E, Brennenstuhl S, Hurd M. Comparison of disability rates among older adults in aggregated and separate Asian American/Pacific Islander subpopulations. Am J Public Health. 2011;101:94–100. doi:10.2105/AJPH.2009.176784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Louie GH, Ward MM. Socioeconomic and ethnic differences in disease burden and disparities in physical function in older adults. Am J Public Health. 2011;101:1322–1329. doi:10.2105/AJPH.2010.199455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Zahodne LB, Manly JJ, Azar M, Brickman AM, Glymour MM. Racial disparities in cognitive performance in mid- and late adulthood: analyses of two cohort studies. J Am Geriatr Soc. 2016;64:959–964. doi:10.1111/jgs.14113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31:285–293. [PubMed] [Google Scholar]
- 105. Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States. N Engl J Med. 2006;355:695–703. doi:10.1056/NEJMsa044316 [DOI] [PubMed] [Google Scholar]
- 106. Quiben MU, Hazuda HP. Factors contributing to 50-ft walking speed and observed ethnic differences in older community-dwelling Mexican Americans and European Americans. Phys Ther. 2015;95:871–883. doi:10.2522/ptj.20140152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Lee SJ, Lindquist K, Segal MR, Covinsky KE. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295:801–808. doi:10.1001/jama.295.7.801 [DOI] [PubMed] [Google Scholar]
- 108. Greysen SR, Stijacic Cenzer I, Auerbach AD, Covinsky KE. Functional impairment and hospital readmission in Medicare seniors. JAMA Intern Med. 2015;175:559–565. doi:10.1001/jamainternmed.2014.7756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Lai JC, Feng S, Terrault NA, Lizaola B, Hayssen H, Covinsky K. Frailty predicts waitlist mortality in liver transplant candidates. Am J Transplant. 2014;14:1870–1879. doi:10.1111/ajt.12762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Kurella M, Covinsky KE, Collins AJ, Chertow GM. Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med. 2007;146:177–183. [DOI] [PubMed] [Google Scholar]
- 111. Eide GE, Gefeller O. Sequential and average attributable fractions as aids in the selection of preventive strategies. J Clin Epidemiol. 1995;48: 645–655. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.