Abstract
To compare percutaneous vertebroplasty (VP) and balloon kyphoplasty (BKP) for their effectiveness and safety in the treatment of newly onset osteoporotic vertebral compression fractures (VCF).
Patients with confirmed diagnosis of newly onset osteoporotic VCF and treated in our center between January 2008 and December 2016 were retrospectively included in the study. Patients were divided into 2 groups according the surgical treatment they have received. They were followed for 12 months after surgery by outpatient visits and phone interviews. Changes in VAS and ODI scores, quantity of injected bone cement, cost of treatment, changes in the height of the vertebra, incidence of complications such as bone cement leakage, adjacent level vertebral fracture during follow up and total were compared between the 2 groups.
A total of 338 patients were included in the final analysis. Demographic characteristics were similar in 2 groups. There were no significant differences between the 2 groups concerning VAS and ODI scores after the surgery and at last follow up (P > .05). However, total cost of treatment, quantity of injected bone cement, incidence of adjacent level fracture, restored vertebral height and the loss of vertebral body height at the last follow up were significantly higher in the BKP group than the VP group (P < .05).
Considering the similar key outcome parameters such as VAS and ODI scores and significantly more cost of BKP, VP can be prioritized over BKP in the treatment of patients with newly onset osteoporotic VCF.
Keywords: BKP, minimal invasive surgery, osteoporosis, vertebral fracture, VP
1. Introduction
There are estimated 1.4 million patients with newly onset osteoporotic vertebral compression fractures (VCF) each year, and the direct annual cost exceeds 1 billion dollars in US only. Osteoporotic VCF may result in acute and chronic pain, impaired mobility, height loss, spinal deformity, reduced pulmonary function, depression and even patient mortality.[1–3] Although patients with mild conditions can be treated with bed rest and pain medication, non-surgical treatment cannot be tolerated by many patients because of the additional health problems caused by immobilization.
As the most commonly applied minimal invasive surgical methods, percutaneous vertebroplasty (VP) and percutaneous balloon kyphoplasty (BKP) have gained acceptance in the treatment of osteoporotic VCF over the last a few decades.[4,5] However, although there are some reports on the short and long term outcomes and complications of those 2 methods, there is little data comparing the safety and cost-effectiveness of those 2 methods.[6,7] Based on our clinical experience, we hypothesized that both VP and BKP can significantly alleviate pain and restore mobility, but there may be no significant differences between the two methods on their effectiveness and safety. The current research was carried out to test this hypothesis.
2. Methods
This is a retrospective study of patient materials, which did not include any experimental treatments. The current study was carried out based on the clinical materials of a total of 338 patients who were treated in Zhongshan City Torch High-tech Industrial Development Zone Hospital between January 2008 and December 2016.
Patients with confirmed diagnosis of compressive vertebral fracture with less than 6 weeks duration, and anterior wall of vertebral body was compressed by more than 30% and less than 75%, and fracture in a single vertebral body were included. Patients agreed to receive surgical treatment and follow up visits up to 1 year after the surgery were included in the study. Patients who had no ability to provide informed consent, patients with VCF for more than 6 weeks, patients with malignant tumors, patients with known allergies to bone cement or contrast agent, patients with neurological impairment due to injury, patients with history of bed rest and patients with lung or heart conditions that made them intolerant for surgical procedure were excluded from the study.
All the patients were followed up in outpatient clinics and by phone interviews for 12 months after the surgery. Diagnosis of compressive vertebral fracture secondary to osteoporosis was made by the X-ray images (General Electric Company, NY). Three dimensional CT scans were carried out by 64 - slice spiral dual-source computer tomographic scans (Siemens, Germany) to rule out burst fractures. 1.5 T magnetic resonance imaging examinations (Siemens Avonto, Germany) were carried out to rule out compression fractures that were already healed. The bone mineral density was measured in vivo at the lumbar spine by dual-energy X-ray absorptiometry using EXA 3000 equipment (HFS Ltd., Korea), and the diagnosis of osteoporosis was confirmed when T < −2.5.[8] Surgical treatment was advised if the time elapsed between injury and treatment was less than 6 weeks and the patient had failed to achieve satisfactory mobility and pain alleviation. The choice between VP and PKP was made by the patients themselves after the surgeon provided detailed information about the 2 procedures to the patients.
All the surgeries were carried out with patients in prone position. 5 ml of 1% lidocaine was used to regionally anesthetize the entry point in both VP and PKP. Patients in the BKP group were treated with balloon kyphoplasty procedure (Fig. 1). A guide pin was inserted from the entry point to locate and confirm the target vertebra and create the working tunnel. The core drill was inserted in the vertebral body, and the balloon was inserted through the working tunnel into the cancellous bone of the compressed vertebra. The contrast agent was injected in the balloon under the observation of C- arm image intensifier. After the balloon was expanded and the restoration of height of the vertebra was considered satisfactory, the contrast media and balloon were removed, the polymethylmethacrylate bone cement in semi-solid state was injected into the balloon. The working tunnel was removed after the bone cement became solid. In the VP group (Fig. 2), same amount of lidocaine was used to regionally anesthetize the entry point, from which a guide pin was inserted to confirm the target vertebra. The core drill was inserted into the vertebral body; the polymethylmethacrylate bone cement in semi-solid state was injected into vertebra under constant monitoring with a C-arm image intensifier. The working tunnel was removed after the bone cement became solid.
Figure 1.
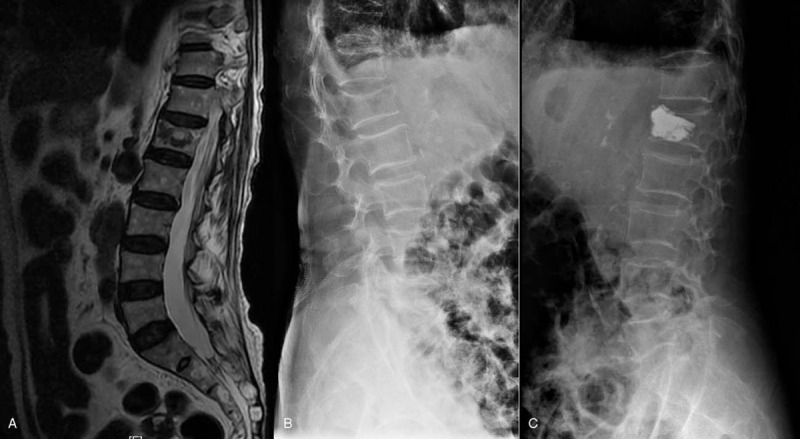
MRI (a) and X-ray (b, c) of a patient who underwent percutaneous balloon kyphoplasty.
Figure 2.
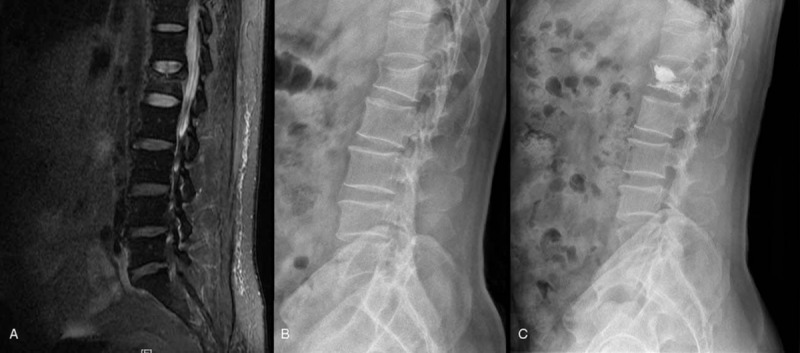
MRI (a) and X-ray (b, c) of a patient who underwent percutaneous vertebroplasty.
After the surgery, patients were allowed to ambulate after 8 hours of postoperative bed rest. Patients received systematic anti-osteoporosis treatment with drugs including calcium supplements, calcitriol and risedronate sodium.
In order avoid bias related to outcome assessment, outcome evaluations were carried out and recorded by the nursing staff and graduate students who had no knowledge of the specific surgical intervention each patient received. Before the surgery, demographic characteristics such as patient age, gender, bone mineral density (BMD), and loss of the vertebral body height were measured and recorded. The loss of vertebral body height was calculated as the estimated vertebral body height (EVH, calculated as the half of the added height of caudal and rostral neighboring vertebral bodies) - measured vertebral body height / estimated vertebral body height. Pain was evaluated by visual analogue scale (VAS)[9] before the surgery, 3 days after the surgery, and at the end of 1 year follow up. The Oswestry disability index (ODI)[10] was assessed before the surgery, 3 days after the surgery, and at the end of follow up.
Quantity of injected bone cement, restored vertebral height, incidence of leakage of bone cement and other complications were recorded during the surgery. The restored vertebral height was calculated as (vertebral body height after the surgery- vertebral body height before the surgery)/estimated vertebral body height.
After the surgery, alleviation of pain, incidence of adjacent level fracture of follow up, total cost during the treatment, and loss of vertebral body height 12 months after the surgery were recorded.
Only the data from patients who finished the 12 months follow up were included in the final statistical analysis. All the data was analyzed by IBM-SPSS22.0 (SPSS Inc. Chicago, IL) statistical software. Differences in the distribution of gender, segment of injury and incidence of adjacent level VCF were compared using Pearson X2 analysis; the other basic characteristics and outcome assessment parameters were compared between the groups using one way analysis of variance. The difference was considered significant when P < .05.
3. Results
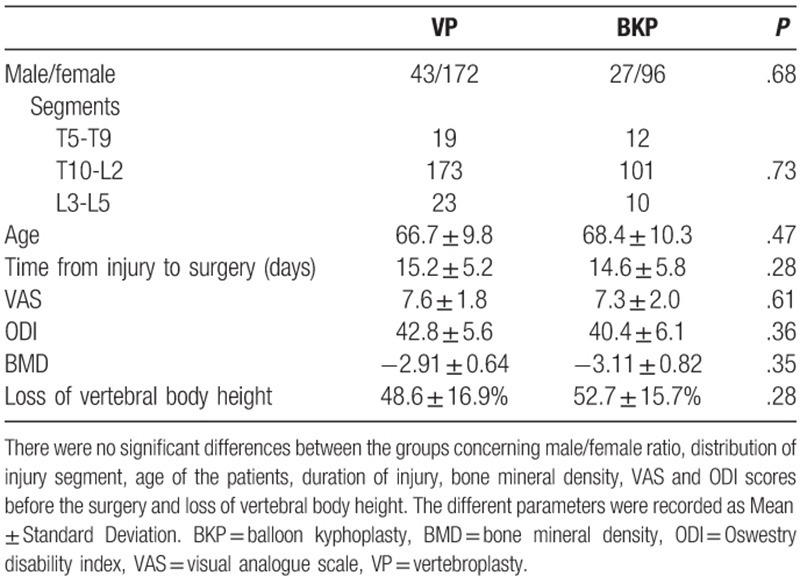
There were no significant differences between the 2 groups concerning the segments of fracture, male/female ratio, age of the patients, bone mineral density, pain before surgery and loss of vertebral body height (P > .05, Table 1). All the patients were hospitalized before surgery. Most patients received surgical treatment within 2 weeks after the injury. All patients were followed up for 12 months after surgery. There were no significant differences between the 2 groups concerning the time interval between injury and surgery and loss of vertebral body height (P > .05, Table 1).
Table 1.
Demographic characteristics of patients in the two groups before the surgery.
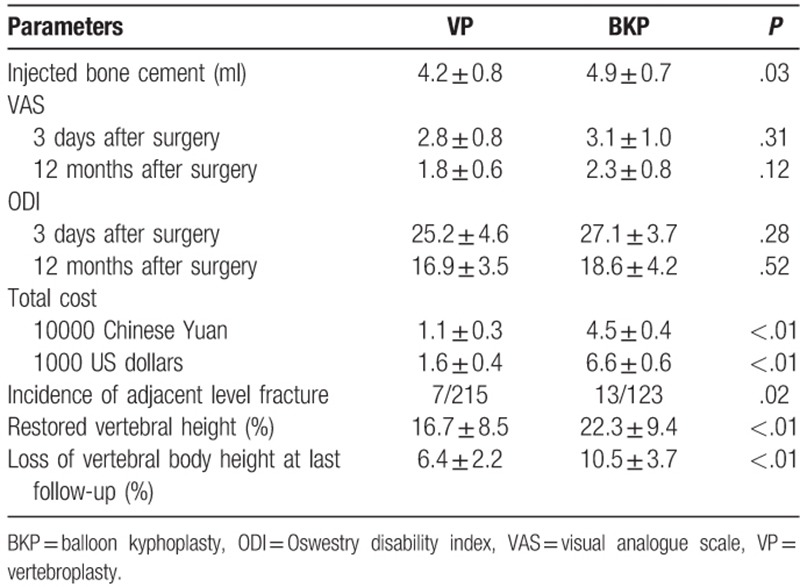
During the surgery, quantity of injected bone cement was significantly higher in the BKP group than the VP group (P < .05). Incidence of leakage of bone cement was found in 15 patients in the VP group, while none of the patients in BKP group experienced leakage of bone cement. The bone cement was leaked into the intervertebral disk in 11 cases (Fig. 3) and into the vertebral canal in 4 patients (Fig. 4). No special treatments were carried out to correct cement leakage since none of those patients reported any symptom of neural injury after surgery and there was no incidence of leak towards major vessels. VAS pain scores were significantly reduced after the surgery, and there were no significant differences between the 2 groups regarding the alleviation of VAS pain scores (P > .05). ODI scores were significantly increased after the surgery, and there were no significant differences between the 2 groups regarding the changes of ODI scores (P > .05). Total cost was significantly higher in the BKP group than the VP group (P < .01). Although the restored vertebral height was significantly more in the BKP group (P < .01), incidence of adjacent level fracture (Fig. 5) and the loss of vertebral body height at the last follow up was also significantly higher in the BKP group (P > .05, Table 2).
Figure 3.

X-ray images of a patient with bone cement leakage into intervertebral space during percutaneous vertebroplasty.
Figure 4.
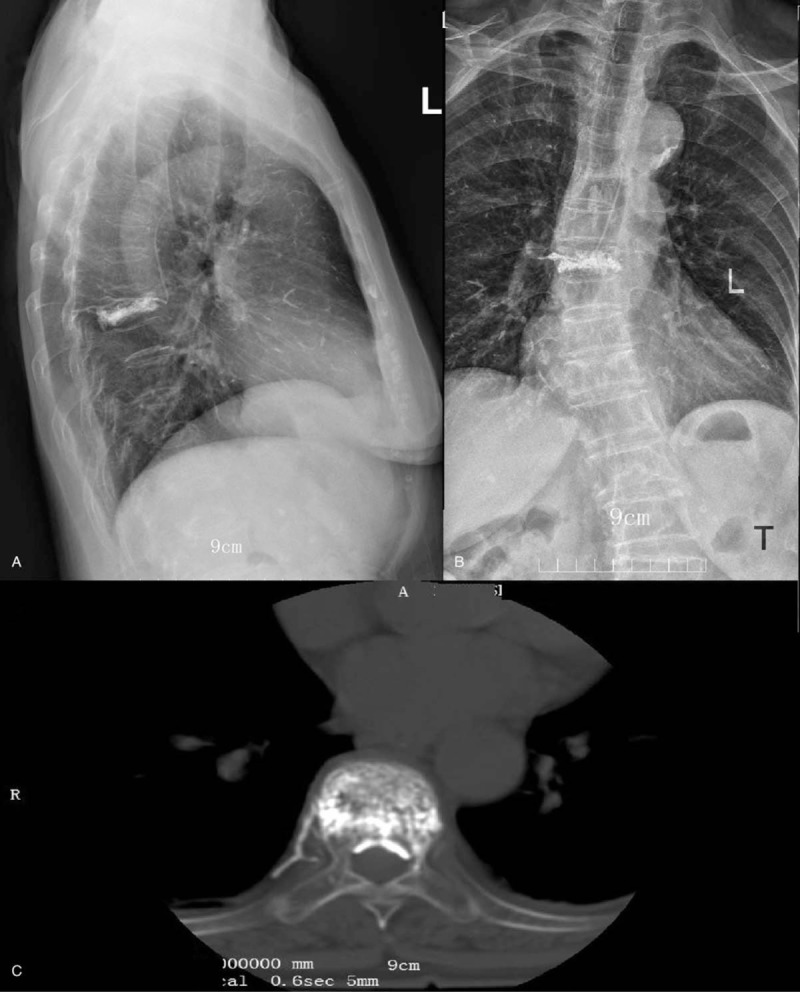
X-ray (a, b) and CT (c) images of a patient with bone cement leakage to vertebral canal during percutaneous vertebroplasty.
Figure 5.

MRI scan of a patient with compression fracture of L2 and L4 vertebra after percutaneous balloon kyphoplasty of L1 vertebra.
Table 2.
Comparison of different outcome parameters between the 2 groups; the data was recorded as mean ± standard deviation.
4. Discussion
In the current study, VAS pain score was significantly reduced (P < .01) in both groups after the surgery. However, there was no significant difference between the 2 groups concerning the decrease in VAS after the surgery, indicating that the BKP and VP are equally effective in the alleviation of pain. This adds useful value in the matter under dispute over the last decade.[11,12] Although percutaneous vertebroplasty and balloon kyphoplasty have been applied in the treatment of osteoporotic VCF for many years, studies by Kallmes et al and Buchbinder et al showed that pain alleviation with vertebroplasty was not significantly better than sham control group.[13,14] Other studies such as VAPOUR and FREE trials advocated the safety and efficacy of VP and BKP in patients with osteoporotic VCF with the onset of less than 6 weeks.[15,16] Results of the current study are in accordance with the results of VAPOUR and FREE trials.
The amount and distribution of bone cement in the surgery is the main determinant factor in the restoration of vertebral height.[17] In the current study, the total amount of injected bone cement was 3.5 ± 0.8 ml in the VP group and 4.2 ± 0.5 ml in the BKP group, which was statistically significant (P = .03). This is similar to the results of the previous studies, and it could be the reason of the significant difference between the 2 groups concerning restored vertebral height. In the current study, the vertebral height was restored significantly better (P < .01) in the BKP (22.3 ± 9.4 mm) group compared to the VP group (16.7 ± 8.5 mm). During BKP, inflatable bone tamps were carried out before the injection of bone cement, so that relatively larger amount of bone cement could be injected into the vertebral body, allowing the surgeon to restore more vertebral height compared to VP. Patients from the BKP group experience significantly (P < .01) more loss of vertebral body height at the end of the follow up than patients of VP group (10.5 ± 3.7 mm vs 6.4 ± 2.2 mm). There are several reasons that may be responsible for this complication: first, the bone cement that is unevenly distributed in the balloon at the anterior region of vertebral body could cause biomechanical imbalance leading to the concentration of pressure on a small surface of osteoporotic vertebral body; a second reason could be the damage of the expanded balloon on the microstructure and blood supply of osteoporotic vertebral bone, causing necrotic changes that may eventually lead to the collapse of the vertebral body. Third, during the VP procedure, bone cement can diffuse into the trabecular space of the osteoporotic bone, which increases its ability to withstand pressure.[18,19]
All patients were advised to undertake regular exercises and to take bone mineral supplements that may help increase BMD, and prevent a second compressive fracture of the same and adjacent vertebrae. However, there are 13 patients in the BKP group and 7 patients in the VP group suffered from vertebral fracture at the adjacent levels during the 12 month follow up. The incidence of adjacent level vertebral fracture was significantly higher in BKP group than VP group (X2 analysis, P = .02). It may be explained by the similar principles on how patients from BKP group experience significantly more loss of vertebral body height at the end of the follow up than the VP group.[20]
The study has several limitations. Since there is a huge difference between the cost of BKP and VP (P < .01), only the patients with good economic background chose to accept BKP. Moreover, the current study was carried out retrospectively, and randomization of the included patients into 2 different groups was not possible. However, there were no significant differences between the 2 groups concerning their gender, age, distribution of injury, baseline body mass index (BMI), VAS, and DOI scores. Considering that this is a study based on more than 300 patients with osteoporotic VCF, results of the current study can be valuable reference for the decision making process in the treatment of osteoporotic VCF.
5. Conclusions
In the treatment of osteoporotic VCF, there are no significant differences between VP and BKP concerning the key outcome parameters such as VAS and ODI scores. Considering the significantly less cost of VP than BKP, we recommend prioritizing VP over BKP for patients with newly onset osteoporotic VCF.
Author contributions
Junjie Cheng was responsible for patient selection and recruitment and carrying out the procedures. Xianming Zeng, Liebin Liu, Yang Liu and Yaying Chen were responsible for collecting the data; Aikeremujiang Muheremu was responsible for analyzing the data and drafting the manuscript.
Conceptualization: Junjie Cheng.
Data curation: Xianming Zeng, Liebin Liu, Yaying Chen.
Formal analysis: Aikeremujiang Muheremu.
Investigation: Junjie Cheng, Xianming Zeng, Liebin Liu, Yang Liu, Yaying Chen.
Methodology: Junjie Cheng, Aikeremujiang Muheremu.
Project administration: Yaying Chen.
Resources: Liebin Liu.
Writing – original draft: Aikeremujiang Muheremu.
Footnotes
Abbreviations: BKP = balloon kyphoplasty, BMD = bone mineral density, EVH = estimated vertebral body height, ODI = Oswestry disability index, VAS = visual analogue scale, VCF = vertebral compression fractures, VP = vertebroplasty.
The study was approved by the institutional review board of the Zhongshan City Torch High-tech Industrial Development Zone Hospital (May 8th, 2018). All the patients gave written consent for the publication of their individual research data, provided that their identity cannot be revealed by those data.
Written informed consent for publication was obtained from all patients.
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006;17:1726–33. [DOI] [PubMed] [Google Scholar]
- [2].Silverman S. The clinical consequences of vertebral compression fracture. Bone 1992;13:S27–31. [DOI] [PubMed] [Google Scholar]
- [3].Goldstein CL, Chutkan NB, Choma TJ, et al. Management of the elderly with vertebral compression fractures. Neurosurgery 2015;77suppl 4:S33–45. [DOI] [PubMed] [Google Scholar]
- [4].Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J 2006;6:479–87. [DOI] [PubMed] [Google Scholar]
- [5].Fachklinik O, Schwarzach S, Beaulieu CG, et al. Treatment of osteoporotic vertebral compression fractures: applicability of appropriateness criteria in clinical practice. Pain Phys 2016;19:E113–20. [PubMed] [Google Scholar]
- [6].Savage, Jason W, Gregory D, et al. Vertebroplasty and kyphoplasty for the treatment of osteoporotic vertebral compression fractures. J Am Acad Orthop Sur 2014;22:53–64. [DOI] [PubMed] [Google Scholar]
- [7].Chandra RV, Maingard J, Asadi H, et al. Vertebroplasty and kyphoplasty for osteoporotic vertebral fractures: what are the latest data? Am J Neuroradiol 2018;39:798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mauch JT, Carr CM, Cloft H, et al. Review of the imaging features of benign osteoporotic and malignant vertebral compression fractures. Am J Neuroradiol 2018;39:1584–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Boonstra AM, Preuper HR, Balk GA, et al. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 2014;155:2545–50. [DOI] [PubMed] [Google Scholar]
- [10].Fairbank JC, Pynsent PB. The Oswestry disability index. Spine 2000;25:2940–53. [DOI] [PubMed] [Google Scholar]
- [11].Wang H, Sribastav S, Ye F, et al. Comparison of percutaneous vertebroplasty and balloon kyphoplasty for the treatment of single level vertebral compression fractures: a meta-analysis of the literature. Pain Phys 2015;18:209–22. [PubMed] [Google Scholar]
- [12].Zhao G, Liu X, Li F. Balloon kyphoplasty versus percutaneous vertebroplasty for treatment of osteoporotic vertebral compression fractures (OVCFs). Osteoporosis Int 2016;27:2823–34. [DOI] [PubMed] [Google Scholar]
- [13].Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009;361:569–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 2009;361:557–68. [DOI] [PubMed] [Google Scholar]
- [15].Clark W, Bird P, Gonski P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 2016;388:1408–16. [DOI] [PubMed] [Google Scholar]
- [16].Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet 2009;373:1016–24. [DOI] [PubMed] [Google Scholar]
- [17].Zhang L, Wang Q, Wang L, et al. Bone cement distribution in the vertebral body affects chances of recompression after percutaneous vertebroplasty treatment in elderly patients with osteoporotic vertebral compression fractures. Clin Interv Aging 2017;12:431–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Krüger A, Oberkircher L, Figiel J, et al. Height restoration of osteoporotic vertebral compression fractures using different intravertebral reduction devices: a cadaveric study. Spine J 2015;15:1092–8. [DOI] [PubMed] [Google Scholar]
- [19].Fujimoto K, Kanchiku T, Imajo Y, et al. Reduction of vertebral height with fragility vertebral fractures can induce variety of neurological deterioration. J Orthop Surg Res 2017;12:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Li Y, Guo D, Zhang S, et al. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (VP) or percutaneous kyphoplasty (BKP). Int Orthop 2018;42:2131–9. [DOI] [PubMed] [Google Scholar]


