Abstract
Rationale:
Penetrating brain injury caused by a welding electrode is a rare occurrence. This type of injury requires careful preoperative assessment and timely treatment measures to avoid secondary damage.
Patient concerns:
A 55-year-old male patient fell from a height of approximately 5 m during when a welding electrode in his left hand was inadvertently inserted into his brain. The patient had a GCS score of 15 and complaints of dizziness and headache. CT showed an object of metallic density penetrating the skull and entering the brain parenchyma in the frontotemporal region.
Diagnosis:
According to the clinical findings and preoperative imaging examination, the diagnosis was open craniocerebral injury with intracranial foreign body and left orbital wall fracture.
Intervention:
After definite diagnosis and sufficient preoperative preparation, active surgical treatment was carried out to remove intracranial foreign body. Anti-infection and other symptomatic treatment were given after operation. The signs of infection and changes of vital signs were closely observed.
Outcomes:
After treatment, no obvious adverse reactions were found and the patient was discharged. No complications such as infection occurred during the follow-up period of 6 months.
Lessons:
In treating patient with a welding electrode penetrating the brain, assessments need to be made preoperatively, the welding electrode needs to be removed in a timely manner, complete hemostasis needs to be achieved during surgery with total repair of the damaged area, and anti-inflammatory treatment needs to be administered postoperatively to achieve good results.
Keywords: intracranial foreign body, open brain injury, surgery, welding electrode
1. Introduction
Penetrating brain injury is common in modern life.[1–3] However, penetrating brain injury caused by a welding electrode is rare and has obvious characteristics. The welding electrode consists of a metal core (Fig. 1A, blue line) and a fuel coating (Fig. 1A, red line) (Fig. 1B, C). It is also caused by low-energy motion.[4,5] In recent years, the incidence of this type of injury has escalated;[6] thus, it is important for clinicians to understand this type of injury and address it in a timely manner.[7] Generally, a welding electrode can be successfully removed by surgery. However, if the preoperative examination shows that an important blood vessel or nerve is injured, the electrode should not be blindly removed. Careful preoperative preparations should be made because the risk of secondary brain injury is unacceptable.[4,8] Therefore, this injury requires reasonable and timely treatment measures that avoid secondary damage. After we contacted the ethics committee of The First Hospital of Jilin University, ethical approval was not required for this case report article. Informed consent was obtained from the patient for the publication of this case report.
Figure 1.
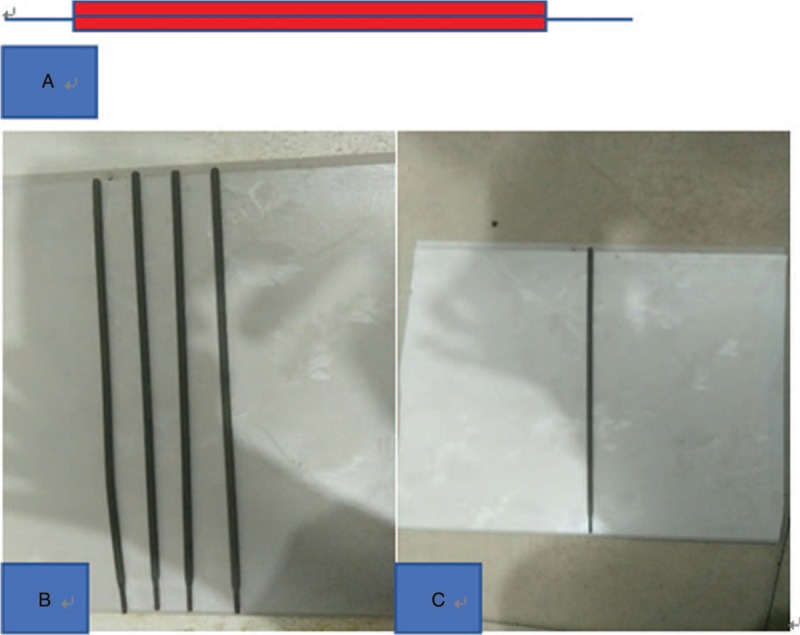
A, Hand-drawn schematic of a welding electrode. B, C, Photographs of welding electrodes.
2. Case report
A 55-year-old male patient fell from a height of approximately 5 m on November 26, 2016. During the fall, due to other objects, the welding electrode in his left hand was inadvertently inserted into his brain. After the injury, there was bleeding at the location of foreign-body penetration. The patient reported dizziness and headache but no nausea, vomiting, bleeding from the ears or nose, poor physical activity or convulsions. The patient was admitted to the hospital 3 hours after the injury. The patient exhibited a normal body temperature, a Glasgow coma scale score of 15 points, clear consciousness and speech, and cooperation during the physical examination. The welding electrode was penetrating the brain from the outer sidewall of the left eye socket (Fig. 2A). Both pupils were equal and round, with a diameter of 3.0 mm, with direct and indirect light reflex intact. The muscle strength and muscular tension of the limbs were normal. Bilateral Babinski signs were not induced. The patient was given a preoperative test immediately after admission, as well as an intramuscular injection of tetanus antitoxin and an intravenous infusion of antibiotics. CT was performed and showed an object of metallic density penetrating the skull and entering the brain parenchyma in the frontotemporal region. The sagittal reconstruction of intracranial nerves and vessels was carried out according to the CT images of the head before operation, and whether the electrodes injured the intracranial nerves and vessels was determined. The results showed that there was no neurovascular injury. Accurate preoperative assessment. (Fig. 2B, C). Surgical treatment was performed about 45 hours after injury due to family economic reasons. During the surgery, the metal (electrode) was observed to have passed through the skull wall from the bottom of the anterior cranial fossa, and the surrounding brain tissue was necrotic with hemorrhage (Fig. 3A). Fully exposing the metal foreign body after achieving hemostasis showed that it was slanted upward, reaching beneath the cerebral falx. After the welding electrode was cleared from the surrounding blood vessels, it was slowly pulled out from the outer corner of the eye, and no bleeding was observed (Fig. 3B). The total length of the electrode is about 17 cm and the intracranial segment is about 7.2 cm (Fig. 3C, D). The cranial wall was ruptured, and the cavity was repeatedly irrigated with 3% hydrogen chloride solution to completely stop the bleeding. Then, dura mater was closed tightly with tension-reduced sutures. The surgery was continued from this point by the ophthalmology department to complete the eye treatment. Postoperative head CT scans were reviewed (Fig. 4A, B), anti-inflammatory treatment was administered, and the patient was closely monitored for cerebrospinal fluid leakage (no colorless fluid flowed through the nostril and external auditory canal) and fever. There were no complications during surgery, and the patient was administered broad-spectrum antibiotics and prophylaxis for seizures and tetanus. Postoperatively, the surgical site showed no signs of infection (Fig. 4C). The patient was followed for 2 months, no significant complications, such as cerebrospinal fluid leakage or fever, were observed during the patient's review (Fig. 4D) or follow-up.
Figure 2.
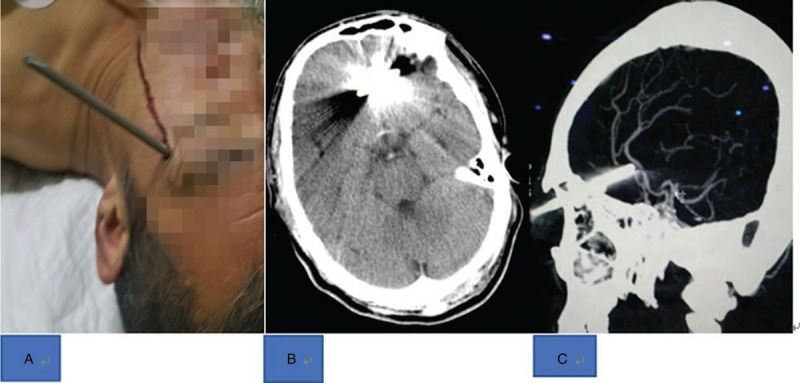
A, Preoperative CT (computed tomography) scan of the patient's head. Small intraventricular hemorrhage on axial head CT scan showing 1 radiopaque welding electrode penetrating both skull plates and entering the brain parenchyma. B, Welding electrode penetrating the brain from the outer sidewall of the left eye socket. C, CT (computed tomography) sagittal reconstruction, no significant damage to important nerves and vessels was observed.
Figure 3.
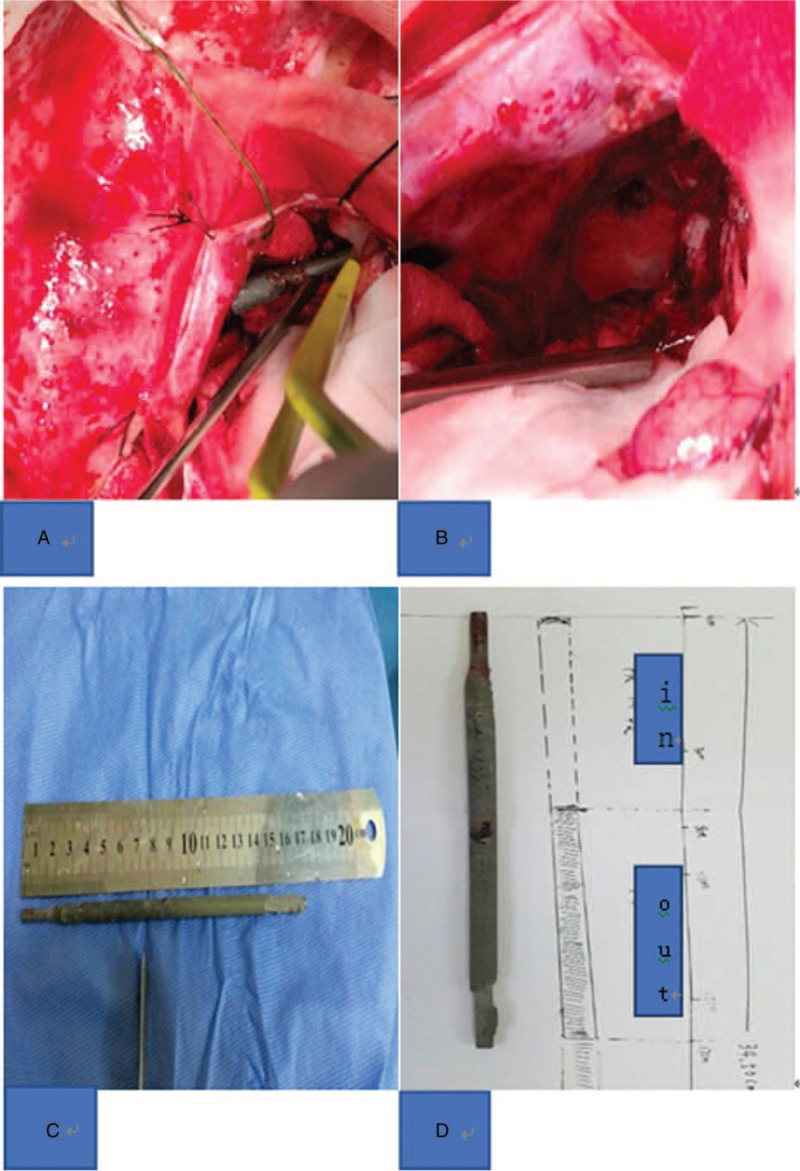
A, Some visible parts of the intracranial welding electrode during surgery. B, Surgical field after the welding electrode was removed and hemostasis was achieved. C, The welding electrode removed during surgery was approximately 17 cm in length. D, The intracranial segment of the welding electrode removed during surgery was approximately 7.2 cm in length.
Figure 4.
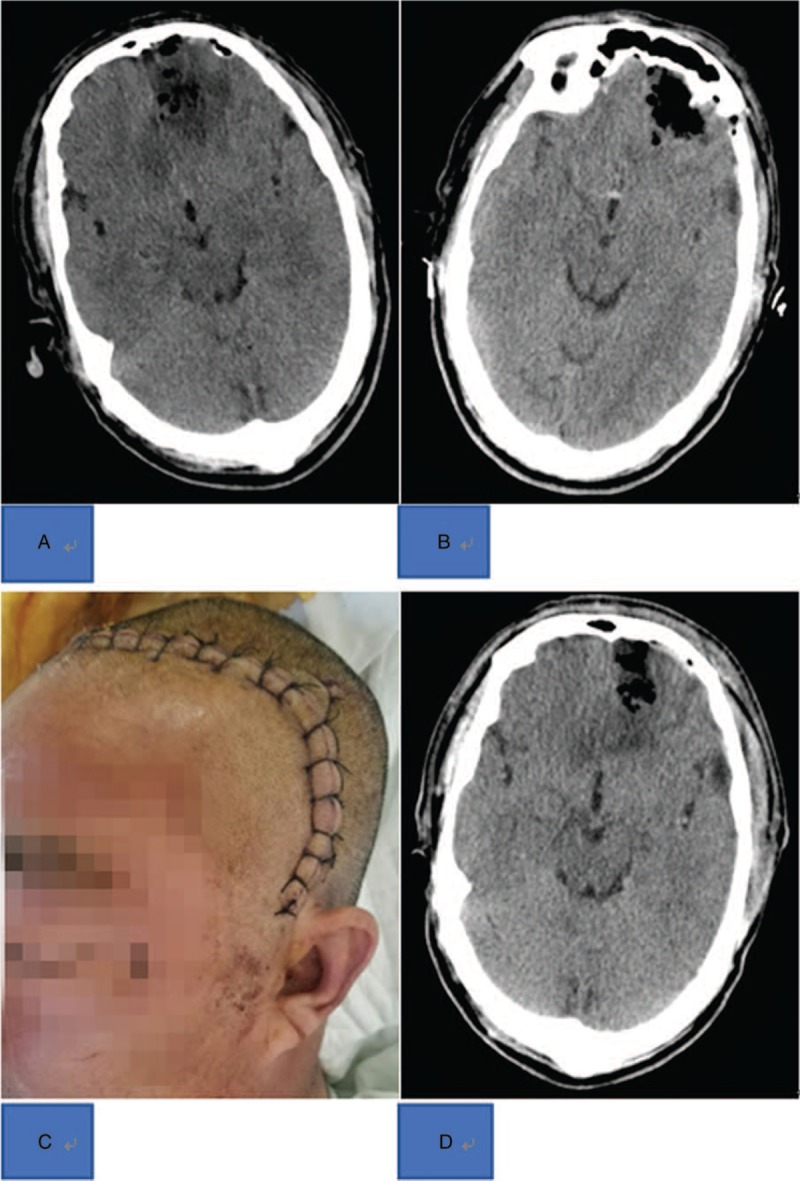
A, On the first day after surgery, the head CT (computed tomography) scan was reviewed and showed a small hematoma in the left frontal lobe and edema that was more serious. The gas shadow was observed on the plate of the skull adjacent to the left frontal parietal bone and in the intracranial area. B, On the third day after surgery, the head CT scan was reviewed and showed a small hematoma remaining in the left frontal lobe accompanied by edema. The gas shadow was increased compared with the first day after surgery at the skull plate adjacent to the left frontal parietal bone and in the intracranial area. C, The postoperative surgical scar was 20 cm in length. No redness, swelling and exudation. D, A follow-up head CT scan was obtained after the patient was discharged from the hospital. The small hematoma in the left frontal lobe was basically absorbed, and the edema was obviously relieved. While the gas shadow at the skull plate adjacent to the left frontal parietal bone and in the intracranial area was still present, it was partially absorbed.
3. Discussion
With the use of welding materials in the construction industry, penetrating brain injury caused by welding electrodes is inevitable, and most of these injuries are industrial accidents.[9–11] However, in clinical practice, such cases are extremely rare. In this case, the patient had a penetrating brain injury caused by a welding electrode. Before treatment, the author believes that the following considerations are particularly noteworthy: the time the foreign body stays in the brain; the potential for infection by anaerobic or other bacteria carried by the foreign body; and most importantly, whether the foreign body has caused irreversible damage to important functional areas of the brain or vascular nerves. Therefore, it is important to perform an early imaging examination of the brain. In this case, the time from injury to treatment at our hospital was short, and the imaging examination was performed promptly to confirm the anatomical positional relationship of the electrode with the brain parenchyma and other important structures, which provided information for the treatment. Head CT scans clearly showed that no important functional areas or structures were damaged; neuroimaging is crucial in any penetrating head injury.[12]
If available, intraoperative CT can be performed to reduce or even avoid secondary surgery due to surgical complications. Due to limited conditions, intraoperative CT was not used in this case. Intraoperative CT can display intracranial changes in real time that may not be apparent from the surface anatomy.[13] As such, some authors have suggested that if there is no active bleeding or the patient has clear consciousness at the time, removal of the object penetrating the brain can be delayed, thus allowing a stable clot to form around the object and achieving a certain level of hemostasis.[14] However, in this case, the foreign body was removed as early as possible because a delay would have increased the possibility of infection or formation of a wrapped membranous structure, which would have in turn increased the difficulty of surgical removal.
Therefore, timely surgical removal is a necessary means to reduce mortality. However, in the clinic, the mortality rate is 33% in cases of timely surgical treatment, and this rate increases to 53% in cases of delayed surgery.[15] These mortality rates might be due to clinicians only focusing on removing foreign bodies or harmful substances while ignoring damage caused by foreign bodies to the surrounding brain tissue or skull;[11,16,17] clinicians may neglect to thoroughly sterilize the area after removal of the foreign body, such as by flushing with hydrogen peroxide or broad-spectrum antibiotics, or not repair minor dural damage, resulting in cerebrospinal fluid leakage. In this case, as much as possible of the flammable fuel coating remaining in the skull was removed during the surgery. Even if the intraoperative temperature does not reach the ignition point of the fuel coating, it can cause secondary damage due to heat conduction or by promoting infection. Tissue with contusion around the foreign body or possible contamination was removed, as well as the skull fragments. The wound was flushed to eliminate possible pathogens, and the dura mater was closed tightly with tension-reduced sutures. The patient was monitored closely for postoperative fever and cerebrospinal fluid leakage, among other signs.
The complications of penetrating brain injury include local wound infection, meningitis, brain abscess formation, and an increased risk of infection by cerebrospinal fluid leakage.[18] Prophylactic antibiotics can reduce the incidence of postoperative complications and are recommended. However, in the clinic, the administration of antibiotics has come to require the consensus of clinicians. In this patient, vancomycin was used after surgery, and no signs of infection were observed. In addition, the incidence of epilepsy in patient with penetrating brain injury is approximately 30% to 50%.[18] Therefore, prophylactic antiepileptic drugs should be administered in the early stage of the injury to reduce the incidence of posttraumatic epilepsy. The postoperative prophylactic use of sodium valproate is effective for preventing epilepsy.
The dressing of the head wound was changed regularly, and the stitches were removed on time. The patient had clear consciousness and speech when he was discharged, and there was no increase in body temperature or neurological dysfunction. Head CT scans were reviewed regularly after discharge, and no obvious discomfort was observed. The patient was followed for 2 months and showed no cerebrospinal fluid leakage or convulsions. Although open head injuries are prone to serious complications, with timely examinations and foreign body removal, the patient can achieve a good quality of life after surgery. Although penetrating brain injury has a high mortality rate, it can be treated promptly, and neurological deficits can be avoided, with full patient recovery.
Author contributions
Conceptualization: Hongfa Yang.
Data curation: Lin Shi, Yue Sun, Hongfa Yang.
Funding acquisition: Hongfa Yang.
Investigation: Yue Sun, Limin Chen, Hang Xue.
Resources: Yue Sun, Weitao Zhang, Hongfa Yang.
Software: Limin Chen.
Visualization: Limin Chen.
Writing – original draft: Lin Shi.
Writing – review & editing: Lin Shi.
Footnotes
Abbreviation: CT = Computed tomography.
The authors have no conflicts of interest to disclose.
References
- [1].Harvey HH. Reducing traumatic brain injuries in youth sports: youth sports traumatic brain injury state laws, January 2009-December 2012. Am J Public Health 2013;103:1249–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Chan RK, Siller-Jackson A, Verrett AJ, et al. Ten years of war: a characterization of craniomaxillofacial injuries incurred during operations Enduring Freedom and Iraqi Freedom. J Trauma Acute Care Surg 2012;736 suppl 5:S453–458. [DOI] [PubMed] [Google Scholar]
- [3].Kittle CP, Verrett AJ, Wu J, et al. Characterization of midface fractures incurred in recent wars. J Craniofac Surg 2012;23:1587–91. [DOI] [PubMed] [Google Scholar]
- [4].Agu CT, Orjiaku ME. Management of a nail impalement injury to the brain in a non-neurosurgical centre: a case report and review of the literature. Int J Surg Case Rep 2016;19:115–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Chen PC, Tsai SH, Chen YL, et al. Post-traumatic cerebral infarction following low-energy penetrating craniocerebral injury caused by a nail. J Korean Neurosurg Soc 2014;55:293–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Englot DJ, Laurans MS, Abbed K, et al. Removal of nail penetrating the basilar artery. Neurosurg Rev 2010;33:501–4. [DOI] [PubMed] [Google Scholar]
- [7].Isaacs AM, Yuh SJ, Hurlbert RJ, et al. Penetrating intracranial nail-gun injury to the middle cerebral artery: a successful primary repair. Surg Neurol Int 2015;6:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sweeney JM, Lebovitz JJ, Eller JL, et al. Management of nonmissile penetrating brain injuries: a description of three cases and review of the literature. Skull Base Rep 2011;1:39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Litvack ZN, Hunt MA, Weinstein JS, et al. Self-inflicted nail-gun injury with 12 cranial penetrations and associated cerebral trauma. Case report and review of the literature. J Neurosurg 2006;104:828–34. [DOI] [PubMed] [Google Scholar]
- [10].Selvanathan S, Goldschlager T, McMillen J, et al. Penetrating craniocerebral injuries from nail-gun use. J Clin Neurosci 2007;14:678–83. [DOI] [PubMed] [Google Scholar]
- [11].Son S, Kang DH, Kim BH, et al. Incidentally discovered a self-inflicted a nail in the brain of schizophrenia patient. Psychiatry Investig 2011;8:272–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ferraz VR, Aguiar GB, Vitorino-Araujo JL, et al. Management of a low-energy penetrating brain injury caused by a nail. Case Rep Neurol Med 2016;2016:4371367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Carnevale JA, Morrison JF, Choi DB, et al. Self-inflicted nail-gun injury with cranial penetration and use of intraoperative computed tomography. Surg Neurol Int 2016;7suppl 10:S259–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Williams JR, Aghion DM, Doberstein CE, et al. Penetrating brain injury after suicide attempt with speargun: case study and review of literature. Front Neurol 2014;5:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Miller CF, Brodkey JS, Colombi BJ. The danger of intracranial wood. Surg Neurol 1977;7:95–103. [PubMed] [Google Scholar]
- [16].Strub WM, Weiss KL. Self-inflicted transorbital and intracranial injury from eyeglasses. Emergency radiology 2003;10:109–11. [DOI] [PubMed] [Google Scholar]
- [17].James G, Blakeley CJ, Hashemi K, et al. A case of self-inflicted craniocerebral penetrating injury. Emerg Med J 2006;23:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Cemil B, Tun K, Yigenoglu O, et al. Attempted suicide with screw penetration into the cranium. Ulus Travma Acil Cerrahi Derg 2009;15:624–7. [PubMed] [Google Scholar]


