Abstract
Background:
The objective of this meta-analysis was aimed to illustrate the functional outcomes of exercise for total hip arthroplasty (THA) patients.
Methods:
In July, 2018, a systematic computer-based search was conducted in PubMed, EMBASE, Web of Science, Cochrane Database of Systematic Reviews, and Google database. Data on exercise for functional outcomes for THA patients were retrieved. The primary endpoint was walking speed. Other outcomes included physical activity scale, Harris hip score, pain scores, abduction strength, and the length of hospital stay. After testing for publication bias and heterogeneity between studies, data were aggregated for random-effects models when necessary.
Results:
Ten clinical studies with 441 patients were ultimately included in the meta-analysis. Compared with the control group, exercise was associated with an increase of the walking speed by 0.15 m/s than control group (weighted mean difference [WMD] 0.15; 95% confidence interval [CI] 0.08, 0.22; P = .000). Also, exercise group could also increase Harris hip score (WMD 8.49; 95% CI 5.19, 11.78; P = .000) and abduction strength than control group (WMD 9.75; 95% CI 5.33, 14.17; P = .000). What is more, exercise has a beneficial role in reducing the pain scores (WMD −1.32; 95% CI −2.07, −0.57; P = .001) and the length of hospital stay (WMD −0.68; 95% CI −1.07, −0.29; P = .001) than the control group. However, there was no significant difference between the physical activity scale (WMD −2.13; 95% CI −6.31, 2.05; P = .317).
Conclusions:
Compared with control group in the management of THA, postoperative exercise has a better pain relief and clinical outcomes. Considering the beneficial of the postoperative exercise, we take a positive attitude toward use exercise for patients with THA.
Keywords: exercise, meta-analysis, pain scores, total hip arthroplasty
1. Introduction
Total hip arthroplasty (THA) is a common surgical procedure for relieving pain in patients with end-stage osteoarthritis (OA) and femoral head necrosis.[1–3] However, loss of muscle strength and other long-term postoperative deficits has been reported after THA.[4,5] These deficits include walking symmetry, muscle strength, and functional performance.[6] At present, no clear evidence exists on how to improve the functional outcome after THA. Previous studies have been reported that there was an immediate muscle loss after THA.[7]
Postoperative exercise was an effective method in improving muscle strength, and it was more effective than other rehabilitation methods.[8] However, these studies were with small sample and with conflicting results.[9–12]
Thus, we conducted a systematic review and meta-analysis about exercise for clinical outcome for THA patients. The purpose of this systematic review and meta-analysis was to compare the efficacy of exercise for clinical outcome after THA.
2. Methods
The manuscript has been prepared according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement.
2.1. Search strategies
Two investigators have independently searched the following databases (inception to July, 2018): PubMed, EMBASE, the Cochrane Library, and the Google database. Search key words and Mesh terms were as follows: “total hip arthroplasty” OR “total hip replacement” OR “THA” OR “THR” OR ““Arthroplasty, Replacement, Hip”[Mesh]” AND “exercise” AND “training”. The reference lists of related meta-analysis were manually searched for any omitted studies. There was no restriction on the language or publication date.
2.2. Inclusion criteria and study selection
Patients were prepared for primary THA. Intervention included postoperative exercise after THA. The standard of care or no treatment was considered as a comparison group. The primary endpoint was walking speed. Other outcomes included physical activity scale, Harris hip score, pain scores, and abduction strength. The study design was selected as randomized controlled trials (RCTs). Two reviewers selected the potential studies according to the inclusion criteria. If there was any disagreement about the selection of the studies, consult from a senior reviewer was obtained. Cohen kappa test was used for assessing consistency between reviewers; more than 0.61 was an acceptable level.[6,7]
2.3. Data abstraction and quality assessment
A specific extraction was conducted to collect data in a pregenerated standard Microsoft Excel (Microsoft Corporation, Redmond, WA) file. The items extracted from relevant studies were as follows: first author and publication year, country, sample size of the intervention and control groups, mean age of the intervention and control groups, the protocol of intervention and comparison groups, and follow-ups. Data in other forms (ie, median, interquartile range, and mean ± 95% confidence interval [CI]) were converted to the mean ± standard deviation (SD) according to the Cochrane Handbook.[13] If the data were not reported numerically, we extracted these data using the “GetData Graph Digitizer” software from the published figures. All the data were extracted by 2 independent reviewers, and disagreements were resolved by discussion.
The quality of all included trials was independently assessed by 2 reviewers on the basis of the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 (http://handbook.cochrane.org/).[13] A total of 7 domains were used to assess the overall quality: random sequence generation, allocation concealment, blinding of participant and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. Each domain was measured as low bias, unclear bias, or high bias.
2.4. Outcome measures and statistical analysis
Continuous outcomes (walking speed, physical activity scale, Harris hip score, pain scores, abduction strength, and the length of hospital stay) were expressed as a weighted mean difference (WMD) with 95% CI. Statistical significance was set at P < .05 to summarize the findings across the trials. Variables in the meta-analysis were calculated using Stata software, version 12.0 (Stata Corp., College Station, TX). Statistical heterogeneity was evaluated using the chi-square test and the I2 statistic. When there was no statistical evidence of heterogeneity (I2 < 50%, P > .1), a fixed-effects model was adopted; otherwise, a random-effects model was chosen. Publication bias was tested using funnel plots. Publication bias was visually assessed using funnel plots and was quantitatively assessed using Begg test.
3. Results
3.1. Search results and quality assessment
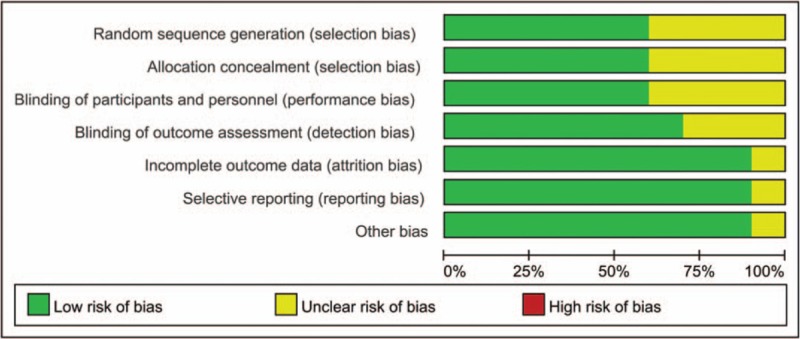
Flow of trials through the meta-analysis can be seen in Fig. 1. In the initial search, a total of 514 studies were identified from the electronic databases (PubMed 82, Embase 33, Web of Science 47, Cochrane Library 13, Google database 20). Then, all papers were input into Endnote X7 (Thomson Reuters Corp.) software for the removal of duplicate papers. A total of 151 papers were reviewed and 141 papers were removed according to the inclusion criteria at abstract and title levels. Finally, a total of 10 studies (441 THAs, exercise group 221, control group 220) were finally included in this meta-analysis.[9–11,14–20] General characteristics of the included studies can be seen in Table 1. Publication year ranged from 1995 to 2014. Mean age of the included studies ranged from 45.44 to 71. Follow-up ranged from 5 weeks to 12 months.
Figure 1.
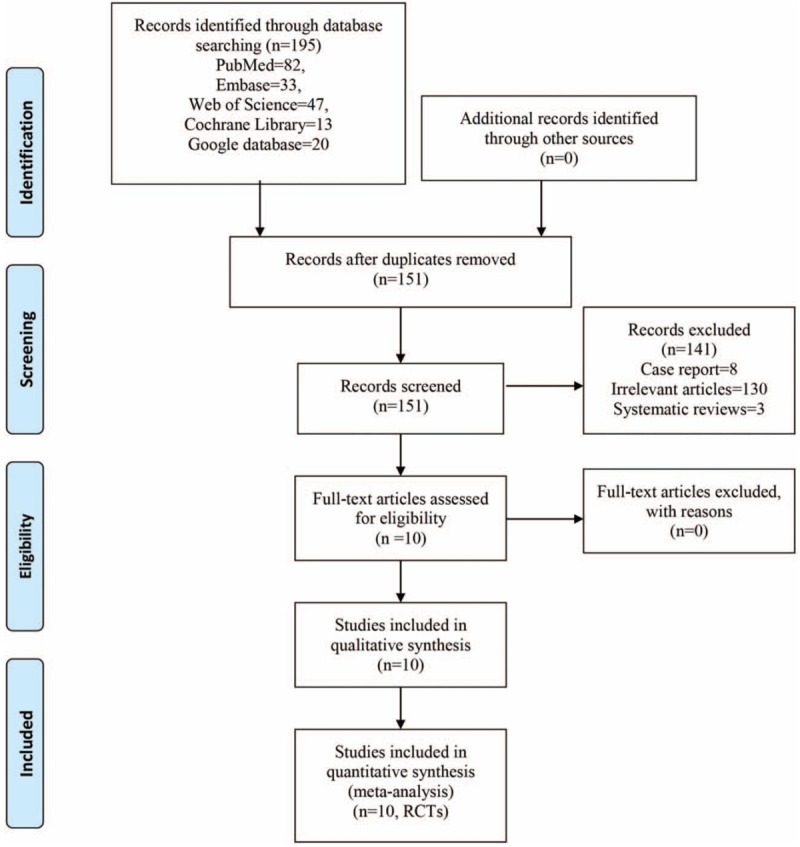
Flow of trials through the meta-analysis.
Table 1.
General characteristic of the included studies.
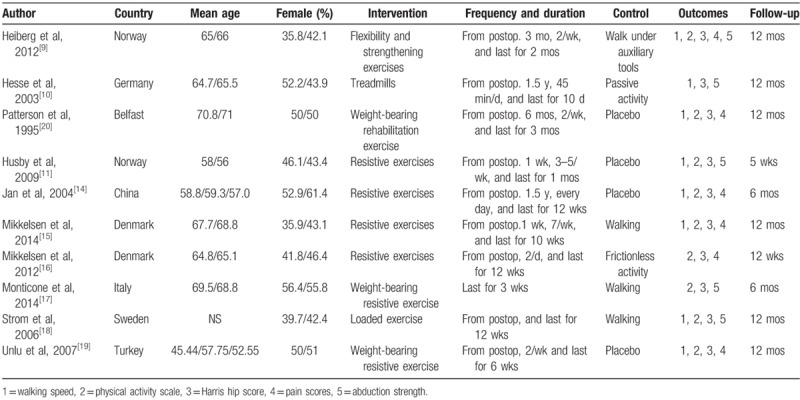
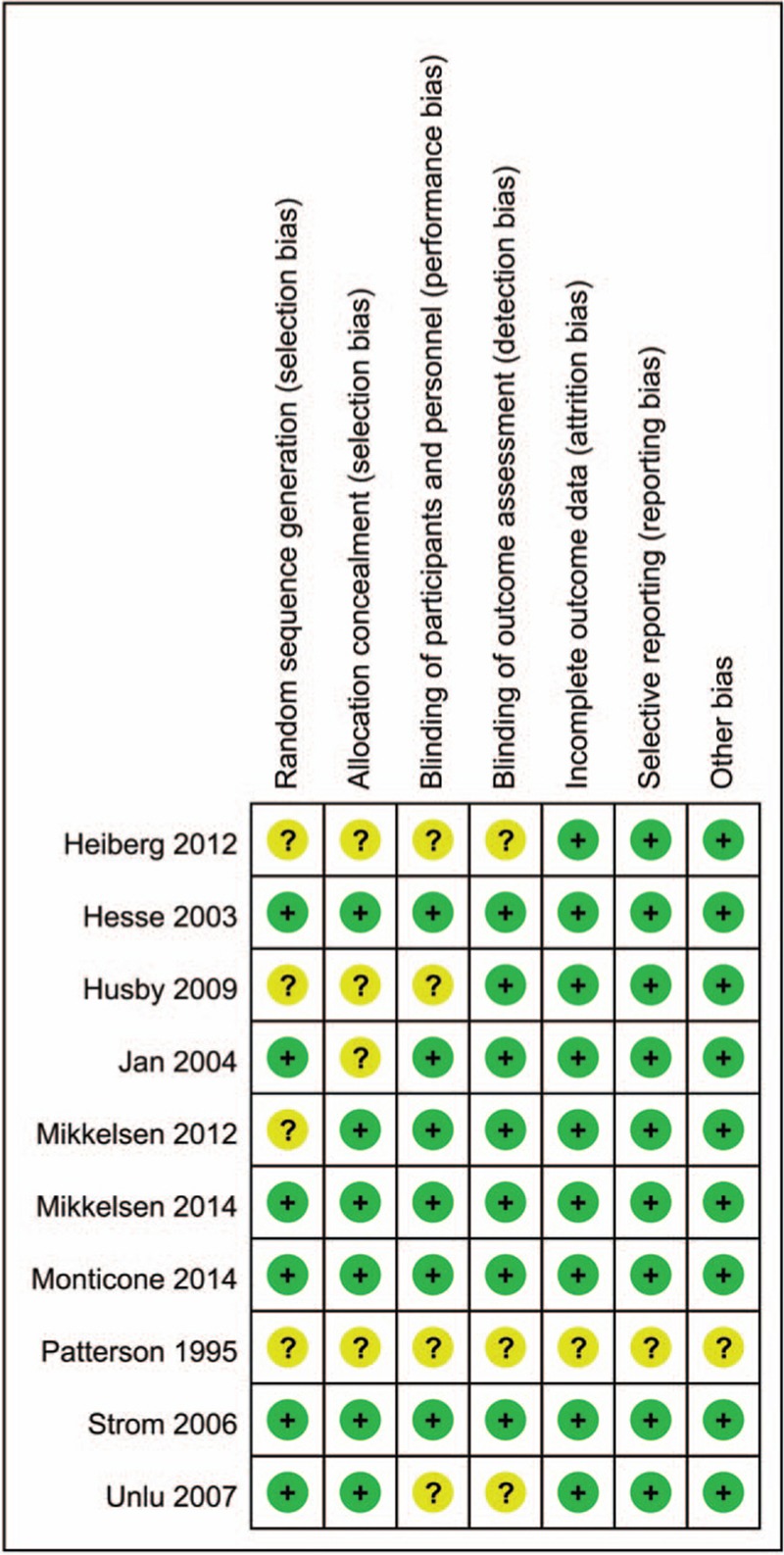
3.2. Risk of bias of the included studies
Risk of bias summary and risk of bias graph can be seen in Figs. 2 and 3, respectively. Attrition bias and allocation concealment was low in 6/10 of the included studies. Blinding of the participant and outcome assessment was low in 6/10 and 7/10, respectively. Incomplete data, selection reporting, and other bias were unclear in 1 study.
Figure 2.
The risk of bias summary. +, no bias; −, bias; ?, bias unknown.
Figure 3.
Risk of bias of summary of the included randomized controlled trials.
3.3. Walking speed
Walking speed was reported in 7 studies, and the pooled results indicated that exercise was associated with an increase of the walking speed by 0.15 m/s compared with the control group (WMD 0.15; 95% CI 0.08, 0.22; P = .000; Fig. 4).
Figure 4.
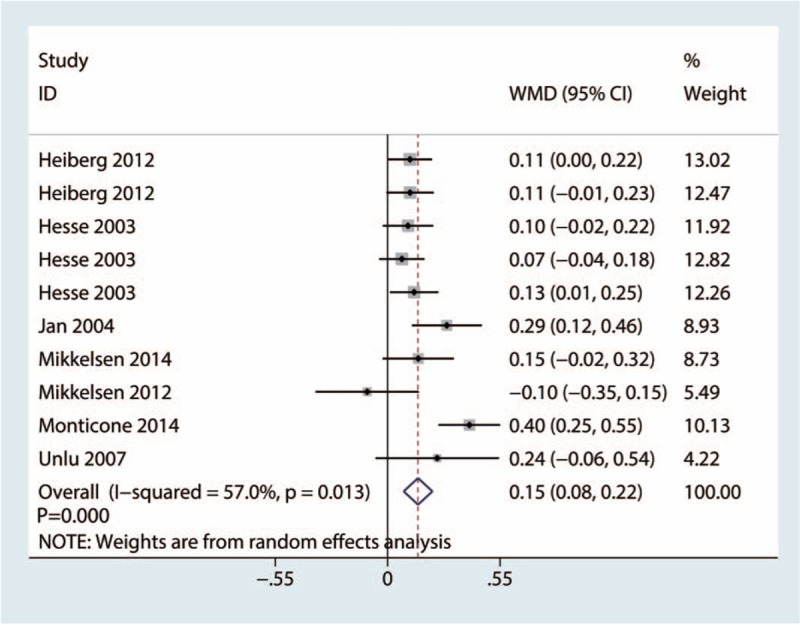
Forest plots of the included studies comparing the walking speed.
3.4. Physical activity scale
Physical activity scale was reported in 5 studies, and the pooled results indicated that there was no significant difference between the exercise group and control group in terms of the physical activity scale (WMD −2.13; 95% CI −6.31, 2.05; P = .317; Fig. 5).
Figure 5.
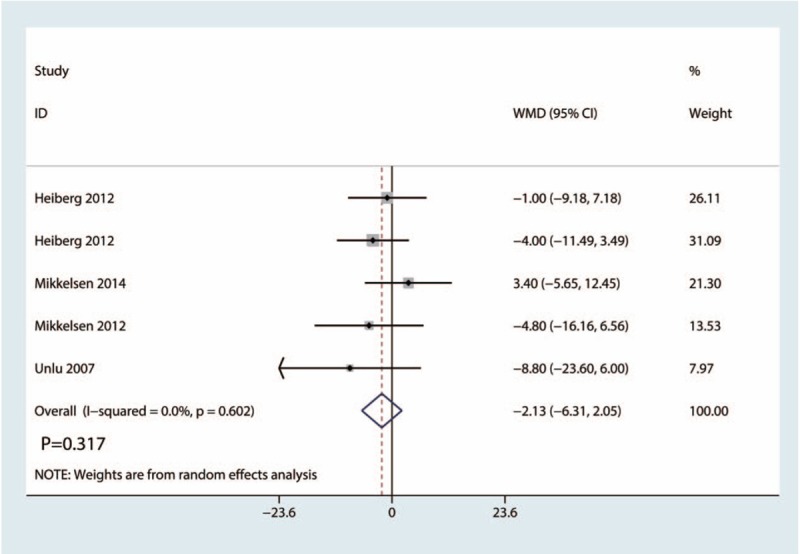
Forest plots of the included studies comparing the physical activity scale.
3.5. Harris hip score
Harris hip score was reported in 6 studies, and the pooled results indicated that exercise group was associated with an increase of the Harris hip scores compared with the control group (WMD 8.49; 95% CI 5.19, 11.78; P = .000; Fig. 6).
Figure 6.
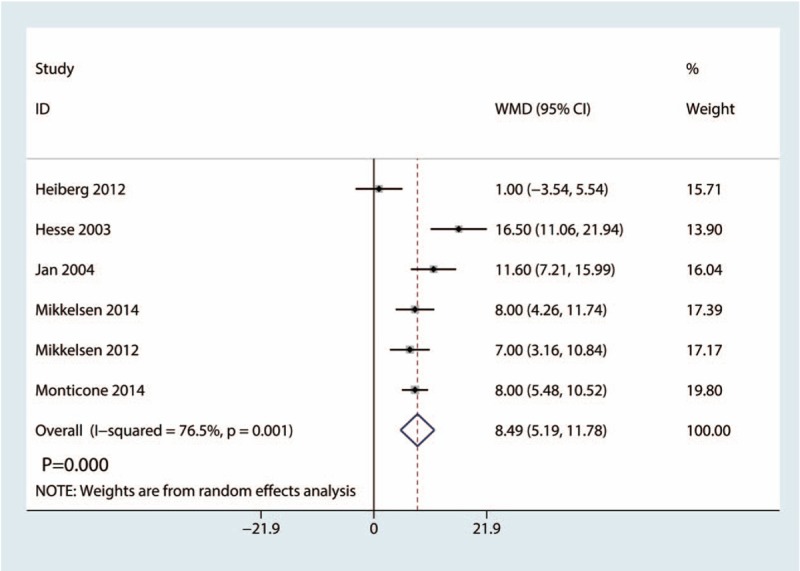
Forest plots of the included studies comparing the Harris hip score.
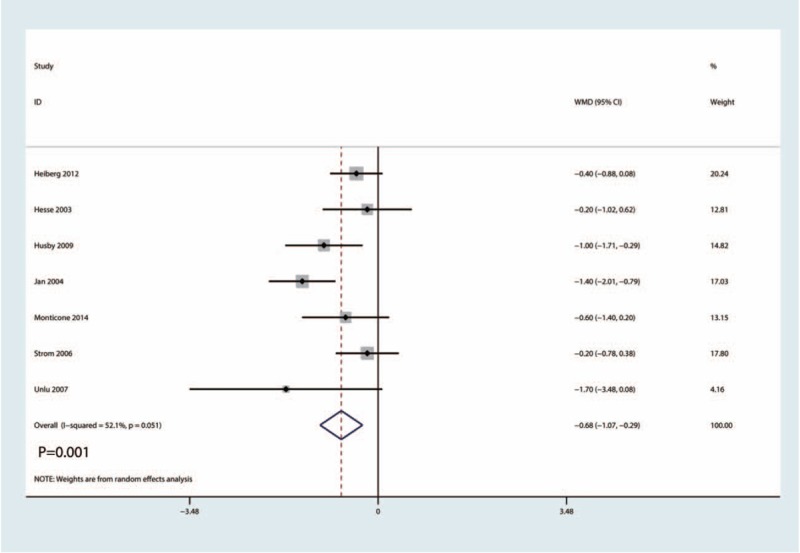
3.6. Pain scores
Pain scores were reported in 8 studies totaling 452 THAs. Compared with control group, exercise group was associated with a reduction of pain scores (WMD −1.32; 95% CI −2.07, −0.57; P = .001; Fig. 7).
Figure 7.
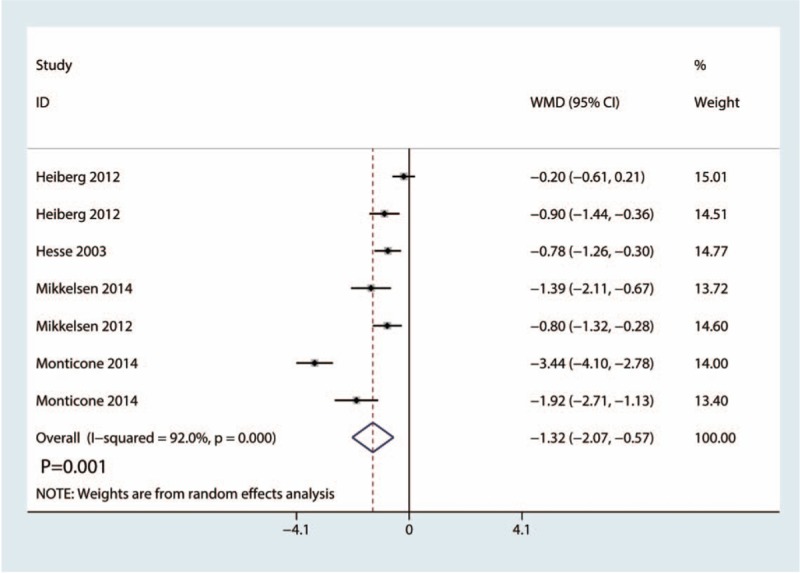
Forest plots of the included studies comparing the pain scores.
3.7. Abduction strength
Six studies totaling 293 patients gave available data for abduction strength of exercise group and control group. Result showed that, compared with the control group, exercise group was associated with an increase of the abduction strength (WMD 9.75; 95% CI 5.33, 14.17; P = .000; Fig. 8).
Figure 8.
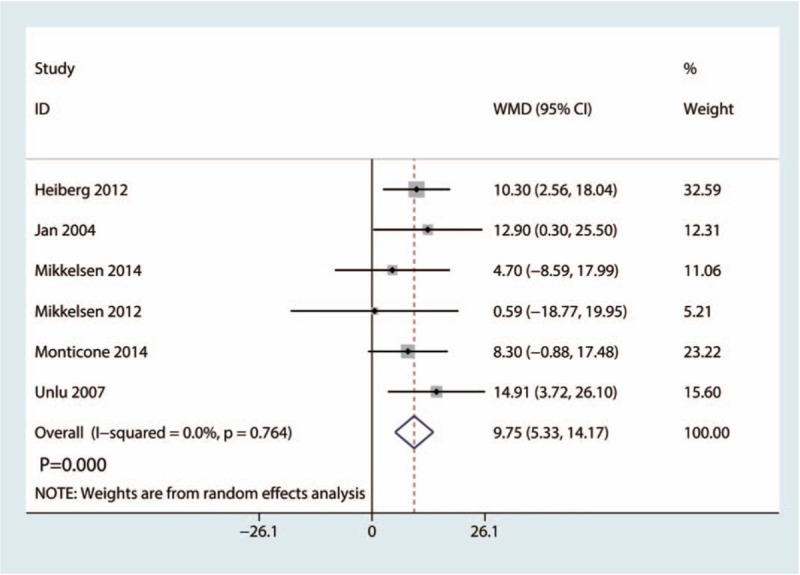
Forest plots of the included studies comparing the abduction strength.
3.8. Length of hospital stay
Seven studies totaling 396 patients provided data for the length of hospital stay of exercise group and control group. Result showed that, compared with control group, exercise group was associated with a decrease of length of hospital stay (WMD −0.68; 95% CI −1.07, −0.29; P = .001; Fig. 9).
Figure 9.
Forest plots of the included studies comparing the length of hospital stay.
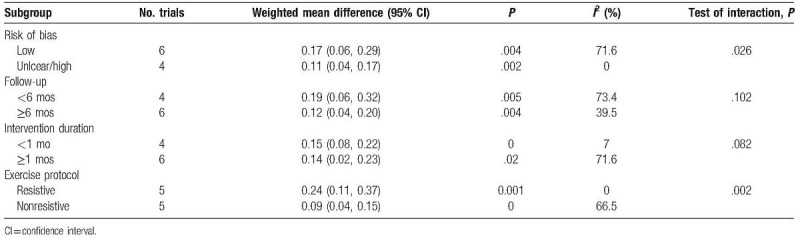
3.9. Subgroup analysis, sensitivity analysis, and publication bias
Table 2 presents the results of subgroup analyses. The findings of walking speed were consistent in all subgroup analyses except for the exercise protocol subgroups. Resistive exercise shows better walking speed than nonresistive exercise.
Table 2.
Subgroup analysis for the walking speed between exercise and control group.
Sensitivity analysis results showed that the results were relatively consistent (Fig. 10). And no obvious publication bias was detected, as based on Egger funnel plots (Fig. 11).
Figure 10.
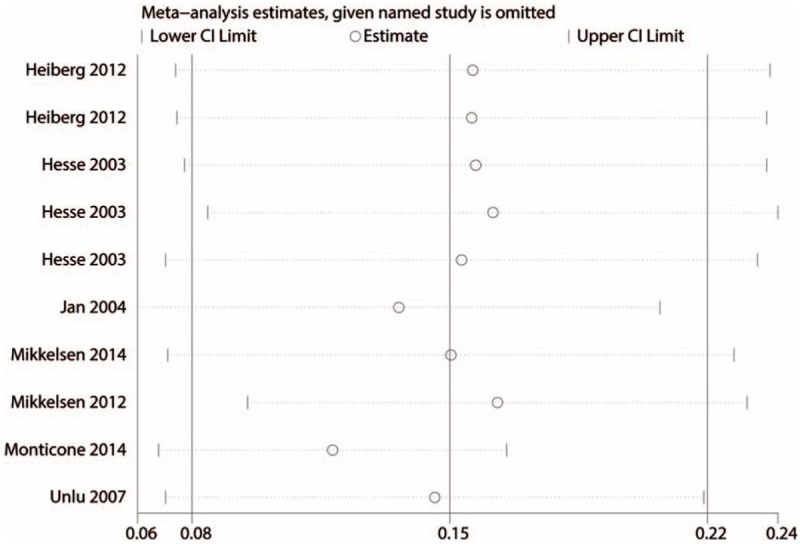
Sensitivity analysis of the walking speed.
Figure 11.
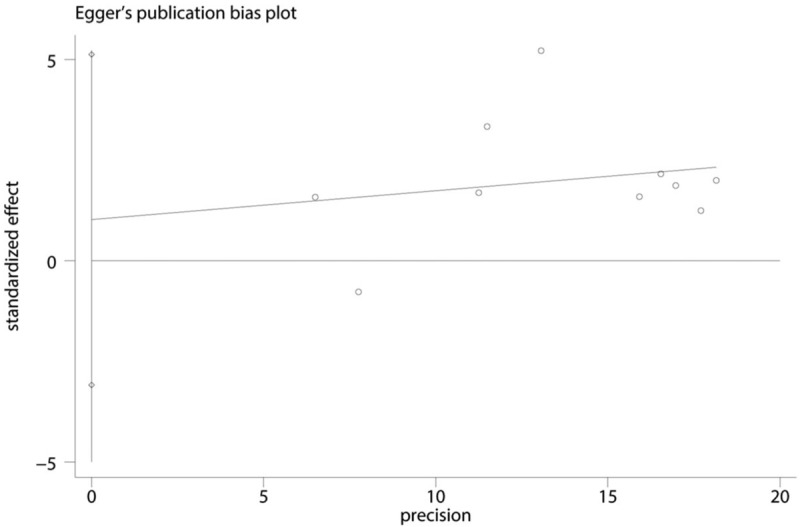
Begg test of the walking speed.
4. Discussion
As far as we know, this is the first meta-analysis investigating exercise efficacy for functional outcomes after THA. We finally included 10 clinical trials. We found that exercise has a beneficial role in improving hip muscle strength, decreasing postoperative pain, and improving hip function.
A major strength of our meta-analysis was that we systematically searched the relevant studies using key words and Mesh terms. Furthermore, we used random-effects model to analyze the final results. Next, we used the sensitivity analysis and subgroup analysis to further increase the robustness of the meta-analysis. An important finding was that resistive exercise was more preferable than nonresistive exercise in improving walking speed.
We identified walking speed as the primary outcome, and results indicated that exercise could increase the walking speed by 0.15 m/s. Subgroup analysis found that exercise has the effects both in short and long-term follow-up. Efficacy of postoperative exercise for hip function recovery was in debated. Kuijlaars et al[21] found that home-based exercise therapy has no effects on hip surgery recovery. Difference between THA and hip surgery should be noticed. Heiberg et al[9] investigate the efficacy of walking skill exercise for THA patients. Included patients were follow-up within 1 year. Results show that exercise was effective in improving walking, both immediate after intervention and 1 year after THA. Wijnen et al[22] found that physiotherapeutic exercise has a beneficial role in improving function after THA. We further analyzed different exercise protocols for walking speed and results show that resistive exercise was more preferable than nonresistive exercise. Moyer et al[23] found that exercise has a beneficial role in improving function, quadriceps strength, and length of stay for knee surgery patients.
Next, we measured the physical activity scale; results found that there was no significant difference in terms of the physical activity scale between the exercise group and control group. Suetta et al[12] compared resistance training with standard rehabilitation regime and results show that compared with standard rehabilitation regime, postoperative resistance training effectively increased maximal muscle strength, muscle mass, and muscle function. Though these results were in contradict with our results, difference between the interventions should be noticed. First, they compared resistance training with standard rehabilitation. Second, muscle strength methods were different. We also compared Harris hip score between exercise group and control group. Results show that exercise after THA could increase the Harris hip scores. Moyer et al[23] compared preoperative exercise training for total knee and hip arthroplasty patients. Results show that significant improvements were observed in function and quadriceps strength in exercise group. We only included postoperative exercise, and the purpose was to observe the efficacy of postoperative exercise for hip functional recovery.
There are some limitations in our meta-analysis, which are listed as follows:
-
1.
Only 10 RCTs enrolling 296 hips were included, and more RCTs were needed to enhance the statistical efficacy of our meta-analysis.
-
2.
Exercise protocol, time, and frequency were different in the included studies, and optimal exercise protocol was need to further study.
-
3.
The follow-up period in the included studies was different and relatively short. More studies with long follow-up periods are necessary.
-
4.
Potential heterogeneity was unavoidable because of the age difference, sex difference, racial difference, and comorbidity difference. But methods such as random-effects model and subgroup analysis were used to reduce the influence of it.
-
5.
Only English RCTs were included in our meta-analysis.
Several limitations exist in our meta-analysis, while we strictly screened available articles before inclusion; moreover, Cochrane Handbook and PRISMA guidelines were used to evaluate the quality of results contained in all included studies.
5. Conclusions
Compared with the control group in the management of THA, postoperative exercise has a better pain relief and clinical outcomes. Considering the beneficial effects of the postoperative exercise, we take a positive attitude toward use exercise for patients with THA.
Author contributions
JQW and LBM conceived the study design. JW performed the study, collected the data and contributed to the study design. LBM and JW prepared the manuscript. JW edited the manuscript.
All authors read and approved the final manuscript.
Project administration: Jia-qi Wu.
Software: Lin-bo Mao, Jian Wu.
Supervision: Lin-bo Mao, Jian Wu.
Visualization: Jian Wu.
Footnotes
Abbreviations: CI = confidence interval, OA = osteoarthritis, PRISMA = Preferred Reporting Items for Systematic reviews and Meta-Analyses, RCTs = randomized controlled trials, SD = standard deviation, THA = total hip arthroplasty, WMD = weighted mean difference.
The authors declare that they have no competing interests.
References
- [1].Li Y, Yin P, Lv H, et al. A meta-analysis and systematic review evaluating the use of erythropoietin in total hip and knee arthroplasty. Ther Clin Risk Manag 2018;14:1191–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Fillingham YA, Ramkumar DB, Jevsevar DS, et al. The efficacy of tranexamic acid in total hip arthroplasty: a network meta-analysis. J Arthroplasty 2018;33:3083–9. [DOI] [PubMed] [Google Scholar]
- [3].Li Q, Xu B. Oral risedronate increases Gruen zone bone mineral density after primary total hip arthroplasty: a meta-analysis. J Orthop Surg Res 2018;13:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Lowe CJ, Davies L, Sackley CM, et al. Effectiveness of land-based physiotherapy exercise following hospital discharge following hip arthroplasty for osteoarthritis: an updated systematic review. Physiotherapy 2015;101:252–65. [DOI] [PubMed] [Google Scholar]
- [5].Umpierres CS, Ribeiro TA, Marchisio AE, et al. Rehabilitation following total hip arthroplasty evaluation over short follow-up time: randomized clinical trial. J Rehabil Res Dev 2014;51:1567–78. [DOI] [PubMed] [Google Scholar]
- [6].Ikutomo H, Nagai K, Tagomori K, et al. Gait abnormality predicts falls in women after total hip arthroplasty. J Arthroplasty 2018;33:3215–9. [DOI] [PubMed] [Google Scholar]
- [7].Leijendekkers RA, Marra MA, Kolk S, et al. Gait symmetry and hip strength in women with developmental dysplasia following hip arthroplasty compared to healthy subjects: a cross-sectional study. PloS One 2018;13:e0193487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chan DC, Chang CB, Han DS, et al. Effects of exercise improves muscle strength and fat mass in patients with high fracture risk: A randomized control trial. J Formos Med Assoc 2018;117:572–82. [DOI] [PubMed] [Google Scholar]
- [9].Heiberg KE, Bruun-Olsen V, Ekeland A, et al. Effect of a walking skill training program in patients who have undergone total hip arthroplasty: Followup one year after surgery. Arthritis Care Res (Hoboken) 2012;64:415–23. [DOI] [PubMed] [Google Scholar]
- [10].Hesse S, Werner C, Seibel H, et al. Treadmill training with partial body-weight support after total hip arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil 2003;84:1767–73. [DOI] [PubMed] [Google Scholar]
- [11].Husby VS, Helgerud J, Bjorgen S, et al. Early maximal strength training is an efficient treatment for patients operated with total hip arthroplasty. Arch Phys Med Rehabil 2009;90:1658–67. [DOI] [PubMed] [Google Scholar]
- [12].Suetta C, Magnusson SP, Rosted A, et al. Resistance training in the early postoperative phase reduces hospitalization and leads to muscle hypertrophy in elderly hip surgery patients: a controlled, randomized study. J Am Geriatr Soc 2004;52:2016–22. [DOI] [PubMed] [Google Scholar]
- [13].GS HJ. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; 2011. Available at: http://handbook.cochrane.org/ Accessed 2011. [Google Scholar]
- [14].Jan MH, Hung JY, Lin JC, et al. Effects of a home program on strength, walking speed, and function after total hip replacement. Arch Phys Med Rehabil 2004;85:1943–51. [DOI] [PubMed] [Google Scholar]
- [15].Mikkelsen LR, Mechlenburg I, Soballe K, et al. Effect of early supervised progressive resistance training compared to unsupervised home-based exercise after fast-track total hip replacement applied to patients with preoperative functional limitations. A single-blinded randomised controlled trial. Osteoarthritis Cartilage 2014;22:2051–8. [DOI] [PubMed] [Google Scholar]
- [16].Mikkelsen LR, Mikkelsen SS, Christensen FB. Early, intensified home-based exercise after total hip replacement: a pilot study. Physiother Res Int 2012;17:214–26. [DOI] [PubMed] [Google Scholar]
- [17].Monticone M, Ambrosini E, Rocca B, et al. Task-oriented exercises and early full weight-bearing contribute to improving disability after total hip replacement: a randomized controlled trial. Clin Rehabil 2014;28:658–68. [DOI] [PubMed] [Google Scholar]
- [18].Strom H, Huss K, Larsson S. Unrestricted weight bearing and intensive physiotherapy after uncemented total hip arthroplasty. Scand J Surg 2006;95:55–60. [DOI] [PubMed] [Google Scholar]
- [19].Unlu E, Eksioglu E, Aydog E, et al. The effect of exercise on hip muscle strength, gait speed and cadence in patients with total hip arthroplasty: a randomized controlled study. Clin Rehabil 2007;21:706–11. [DOI] [PubMed] [Google Scholar]
- [20].Patterson AJ, Murphy NM, Nugent AM, et al. The effect of minimal exercise on fitness in elderly women after hip surgery. Ulster Med J 1995;64:118–25. [PMC free article] [PubMed] [Google Scholar]
- [21].Kuijlaars IAR, Sweerts L, Nijhuis-van der Sanden MWG, et al. Effectiveness of supervised home-based exercise therapy compared to a control intervention on functions, activities and participation in older patients after hip fracture: a systematic review and meta-analysis. Arch Phys Med Rehabil 2018;100:101–14. [DOI] [PubMed] [Google Scholar]
- [22].Wijnen A, Bouma S, Seeber G, et al. The therapeutic validity and effectiveness of physiotherapeutic exercise following total hip arthroplasty for osteoarthritis: a systematic review. PloS One 2018;13:e0194517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Moyer R, Ikert K, Long K, et al. The value of preoperative exercise and education for patients undergoing total hip and knee arthroplasty: a systematic review and meta-analysis. JBJS Rev 2017;5:e2. [DOI] [PubMed] [Google Scholar]


