Abstract
The association between adiposity parameters and cognition is complex. The purpose of this study was to assess the relationship between adiposity parameters and cognition in middle-aged and elderly people in China.
Data were obtained from a cross-sectional study. Cognitive function was evaluated in 5 domains, and adiposity parameters were measured. The association between adiposity parameters and cognition was analyzed using multiple linear and binary logistic regression analyses.
After controlling for confounders, men with overweight and obesity had better scores in TICS-10 ([1] total, overweight vs normal: P = .006, β = 0.04; obesity vs normal: P = .005, β = 0.04. [2] stratification by age, with age ≥ 59 years, overweight vs normal: P = .006, β = 0.05; obesity vs normal: P = .014, β = 0.05. [3] stratification by educational levels, with less than elementary education, overweight vs normal: P = .011, β = 0.05; obesity vs normal: P = .005, β = 0.05), immediate word recall ([1] total, overweight vs normal: P = .015, β = 0.04. [2] stratification by age, with age 45–58 years, overweight vs normal: P = .036, β = 0.05. [3] stratification by educational levels, with less than elementary education, overweight vs normal: P = .044, β = 0.04; above high school, overweight vs normal: P = .041, β = 0.09), self-rated memory ([1] stratification by age, with age ≥ 59 years, overweight vs normal: P = .022, β = 0.05. [2] stratification by educational levels, with less than elementary education, overweight vs normal: P = .023, β = 0.04), and drawing a picture ([1] total, overweight vs normal: OR = 1.269, 95% CI = 1.05–1.53. [2] stratification by educational levels, with less than elementary education, overweight vs normal: OR = 1.312, 95% CI = 1.06–1.63); obesity vs normal: OR = 1.601, 95% CI = 1.11–2.31 than the normal weight; women with overweight and obesity had better measure scores in the TICS-10 ([1] total, overweight vs normal: P < .0001, β = 0.06; obesity vs normal: P < .0001, β = 0.05. [2] stratification by age, with age 45–58 years, obesity vs normal: P = .007, β = 0.05; with age ≥ 59 years: overweight vs normal: P < .0001, β = 0.07, obesity vs normal: P = .002, β = 0.06. [3] stratification by educational levels, with illiterate, overweight vs normal: P = .001, β = 0.08; obesity vs normal: P = .004, β = 0.06; with less than elementary education, overweight vs normal: P < .0001, β = 0.07; obesity vs normal: P = .010, β = 0.05), immediate word recall ([1] total, overweight vs normal: P = .011, β = 0.04; obesity vs normal: P = .002, β = 0.04. [2] stratification by age, with age 45–58 years, obesity vs normal: P = .021, β = 0.05; with age ≥ 59 years: overweight vs normal: P = .003, β = 0.06. [3] stratification by educational levels, with illiterate, obesity vs normal: P = .028, β = 0.05; with less than elementary education, obesity vs normal: P = .016, β = 0.05), delay word recall ([1] total, overweight vs normal: P = .015, β = 0.03; obesity vs normal: P = .031, β = 0.03. [2] stratification by age, with age ≥ 59 years: overweight vs normal: P = .004, β = 0.06. [3] stratification by educational levels, with less than elementary education, obesity vs normal: P = .043, β = 0.04), self-rated memory ([1] total, obesity vs normal: P = .026, β = 0.03. [2] stratification by age, with age ≥ 59 years, overweight vs normal: P = .044, β = 0.04; obesity vs normal: P = .018, β = 0.05), and drawing a picture ([1] total, overweight vs normal: OR = 1.226, 95% CI = 1.06–1.42. [2] stratification by age, with age 45–58 years: overweight vs normal: OR = 1.246, 95% CI = 1.02–1.53) than the normal weight. Regarding the association between WC and cognitive function, the obesity demonstrated better mental capacity ([1] total, men: P < .0001, β = 0.06; women: P < .0001, β = 0.05. [2] stratification by age, men with age 45–58 years: P < .0001, β = 0.08; men with ≥ 59 years: P = .006, β = 0.05. women with age 45–58 years: P = .001, β = 0.06; women with ≥ 59 years: P = .012, β = 0.04. [3] stratification by educational levels, men with illiterate: P = .045, β = 0.09; men with less than elementary education: P < .0001, β = 0.08; women with illiterate: P < .0001, β = 0.09), ability to recall immediately ([1] total, men: P = .030, β = 0.03; women: P = .001, β = 0.05. [2] stratification by age, women with age 45–58 years: P = .028, β = 0.04; women with ≥ 59 years: P = .007, β = 0.05. [3] stratification by educational levels, men with less than elementary education: P = .007, β = 0.05; women with illiterate: P = .027, β = 0.05; women with less than elementary education: P = .002, β = 0.06), delay word recall ([1] total, women: P = .044, β = 0.03. [2] stratification by educational levels, men with less than elementary education: P = .023, β = 0.04), self-rated memory (stratification by educational levels, women with less than elementary education: P = .030, β = 0.04), and draw a picture ([1] total, men: OR = 1.399, 95% CI = 1.17–1.67; women: OR = 1.273, 95% CI = 1.12–1.45. [2] stratification by age, men with age 45–58 years: OR = 1.527, 95% CI = 1.15–2.03; men with age ≥ 59 years: OR = 1.284, 95% CI = 1.02–1.61; women with age 45–58 years: OR = 1.320, 95% CI = 1.10–1.58; women with age ≥ 59 years: OR = 1.223, 95% CI = 1.01–1.49. [3] stratification by educational levels, men with less than elementary education: OR = 1.528, 95% CI = 1.25–1.87; women with illiterate: OR = 1.404, 95% CI = 1.14–1.73) than the participants with normal weight after the multivariate adjustment.
Our study demonstrated a significant relationship between adiposity parameters and cognition that supports the “jolly fat” hypothesis.
Keywords: adiposity, body mass index, cognition, jolly fat, waist circumference
1. Introduction
It is well known that the prevalence of overweight and obesity has increased in adults. Specifically, the prevalence is 21.8% in China,[1] compared with >50% in the United States.[2] The highest prevalence was observed among adults aged ≥45 years.[3] Overweight and obesity are associated with many adverse conditions such as heart disease,[4] hypertension, cognitive dysfunction,[5] and diabetes mellitus.[6] Dementia, a cognitive dysfunction, is the most challenging disease associated with overweight and obesity, because patients with dementia require more complex care and experience economic, psychosocial, and physical difficulties. Recently, both adiposity and cognitive dysfunction have become important public problems in many countries.
The relationship between adiposity parameters and cognition has recently attracted the interest of researchers. A review[7] was conducted on studies that reported an association between obesity and cognition across the lifespan, including children and adolescents (aged 4–18 years), adults (aged 19–65 years), and elderly persons (aged 66–95 years). A relatively consistent finding was that obesity is associated with cognitive dysfunction, especially in the aspects of memory and executive function, across the lifespan (i.e., in children, adolescents, and adults). Overweight and obesity have been associated with self-reported functional decline[8] and performance-based measurement decline[9] in the elderly population; however, the relationship between adiposity parameters and cognition remains controversial. In humans, previous studies have suggested that individuals with obesity were likely to have a higher cognitive function (i.e., the “jolly fat” hypothesis),[10,11] and several studies have reported outcomes consistent with this hypothesis. However, most studies[12–14] found that obesity was associated with an increased risk for cognitive dysfunction. Further, other studies[15,16] have demonstrated that in some individuals weight loss or being underweight was associated with cognitive decline. Animal studies[17] have shown that rats with obesity had worse learning and memory task performances than normal-weight rats.
To date, the relationship between adiposity and cognitive function, especially the effect of obesity on cognitive function in middle-aged and elderly individuals, remains uncertain. Thus, our study aimed to investigate the relationship between adiposity parameters and cognitive function in middle-aged and elderly Chinese people, and to apply the “jolly fat” hypothesis to cognition.
2. Methods
2.1. Study sample
The data for this cross-sectional study were taken from the China Health and Retirement Longitudinal Study (CHARLS), a biennial and nationally representative longitudinal survey conducted by the China Centre for Economic Research at Peking University.[18] The baseline survey had a 4-stage, stratified, cluster probability sampling design. All participants enrolled for the study signed the consent, and the institutional review board of the Peking University approved the study protocol. The cross-section and observational design follow the STROBE guidelines.[19] The data is publicly available (http://charls. pku.edu.cn/zh-CN), and our study have no direct contact with the individual participants.
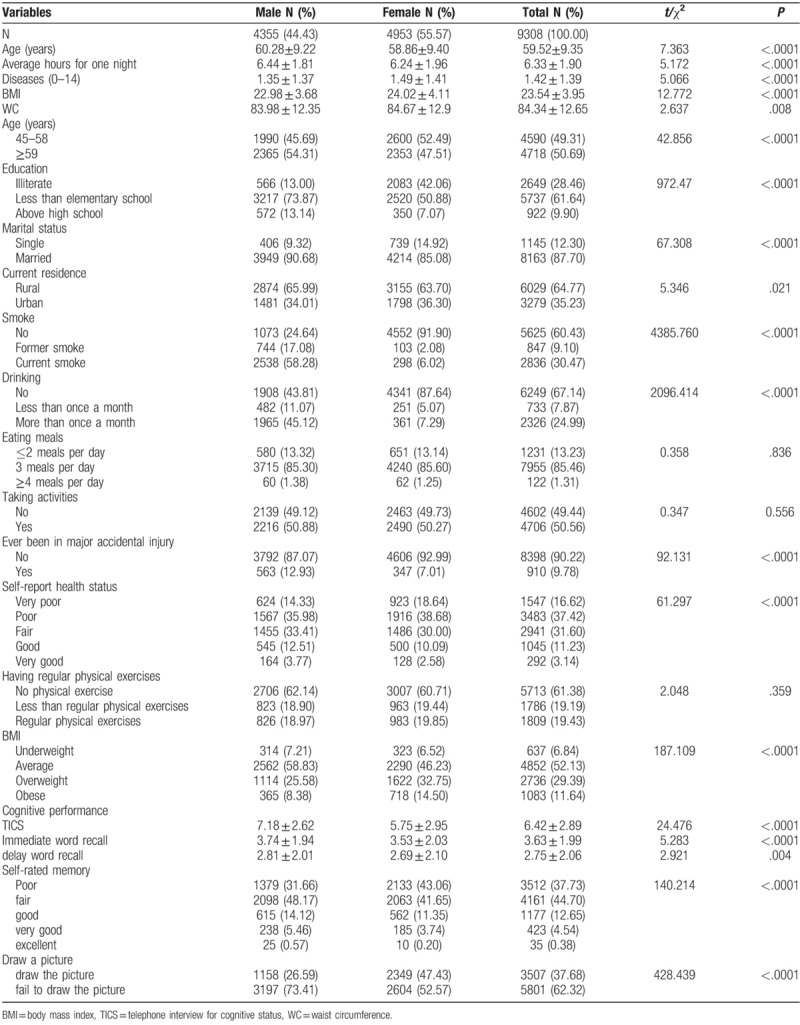
In the first stage, all counties in China were stratified by region, rural/urban status, and gross domestic product per capita. A random sample of 150 counties was selected to represent the socioeconomic and geographic pattern of all counties. In the second stage, 3 primary sampling units (PSUs) were selected in each county, with the probability of inclusion of each county in the sample being proportional to its population size. In the third stage, all households in each selected PSU were mapped and a random sample of 24 households was selected among all households, with residents aged ≥45 years within each PSU. Finally, for each selected household, 1 resident aged ≥45 years was randomly selected as a survey participant. The 2011 CHARLS Wave1 sample (N = 9308) consisted of 44.43% men (age: mean [M], 60.28 years; standard deviation [SD], 9.22; range, 45–93 years) and 55.57% women (M, 58.86 years; SD, 9.40; range, 45–96 years). Of the respondents, 6.68% and 3.22% had completed high school and had more than vocational school education, respectively. By contrast, 28.46% of the respondents were illiterate and 61.64% had less than elementary school education. Moreover, 64.77% live in rural areas and 35.23% live in urban areas. Table 1 presents the baseline characteristics of the sample for all studied variables, most of which were based on our previous study.[3,20,21]
Table 1.
Baseline characteristics with full samples (N = 9308).
2.2. Demographic characteristics and self-reported risk factors
Data, including age, education, marital status, current residence, smoking status, alcohol consumption, eating habits, activity performance, accidental injury, physical exercise, self-reported health status, sleeping hours, and diseases, were obtained using a self-reported questionnaire.
-
1.
The median age was 59 years, and age was classified into < 59 years and ≥59 years.
-
2.
Educational level was classified into illiterate, less than elementary school, and above high school.
-
3.
Marital status was classified into married and single.
-
4.
Current residence was classified into rural and urban.
-
5.
Smoking status was classified into never smoking, ex-smoking, and current smoking.
-
6.
Alcohol consumption was classified into none, less than once a month, and once a month.
-
7.
Eating habits were categorized into 2 meals per day or fewer, 3 meals per day, and 4 meals per day or more.
-
8.
Activity performance was dichotomized into at least once a month and never.
-
9.
Major accidental injury information was obtained by asking the participant whether he or she has experienced any type of major accidental injury and received medical treatment, with the answer being “yes” or “no.”
-
10.
Regular physical exercise was defined as exercising at least 3 days/week and >30 min/day, including moderate to vigorous physical activity and walking.
-
11.
Self-reported health status was categorized into poor, fair, good, very good, and excellent.
-
12.
The number of sleeping hours was defined as the average hours of sleep per night during the past month.
-
13.
Following Chang,[22] a continuous variable that reflects the presence of chronic health conditions was used, by assessing 14 common chronic symptoms among the middle aged and elderly, including hypertension; dyslipidemia; diabetes or high blood sugar; cancer or malignant tumor; chronic lung diseases; liver disease; heart problems; stroke; kidney disease; digestive disease; emotional, nervous, or psychiatric problems; memory-related disease; arthritis or rheumatism; and asthma. The presence of each symptom was scored 1, and the sum of scores for all symptoms, which ranged from 0 to 14, was used as an indicator of disease.
-
14.
menopause information was obtained by asking the participant whether she has started menopause, with the answer being “yes” or “no.”
2.3. Cognition assessment
Cognitive function was evaluated in 5 domains: Telephone Interview for Cognitive Status (TICS-10), immediate word recall, delayed word recall, self-rated memory, and drawing a picture.
TICS-10 was used to measure mental capacity.[23] It includes 10 questions about awareness of the date (year, month, day, week, and season) and consecutive 5 times 100 minus 7. The total TICS-10 score was based on correct answers, ranging from 0 to 10.
Self-rated memory was evaluated using the following questions: “How would you rate your memory at the present time? Would you say it is excellent, very good, good, fair, or poor?” The answer was defined using 5 possible ordinal categories, including poor (1), fair (2), good (3), very good (4), and excellent (5).[24]
Immediate word recall and delayed word recall were used to assess the respondents’ memory.[24] Of 4 lists that each contain 10 nouns (list A: rice, river, doctor, clothes, egg, cat, bowl, child, hand, and book; list B: stool, foot, sky, money, pillow, dog, house, wood, school, and tea; list C: mountain, stone, blood, mother, shoes, eye, girl, house, road, and sun; and list D: water, hospital, tree, father, fire, tooth, moon, village, boy, and table), 1 list was randomly selected and read slowly with an interval of approximately 2 s between each word. Immediately after reading, the respondents were given approximately 2 minutes to recall as many of those words as they possibly could. Thereafter, the respondents were again asked to repeat the words they could remember. On the basis of the correctly recalled words, we obtained 2 scores for immediate recall and delayed word recall memory, which ranged from 0 to 10.
Drawing a picture was also used in the survey,[23] in which a picture was shown and the respondents were asked to draw the image as similarly as possible. If the respondents successfully finished or failed to finish the task, the score assigned was 1 or 0, respectively.
2.4. Adiposity parameter measurement
Weight was measured using a weighing instrument. Height was measured with a height gauge, with the participant standing in an upright position on stocking feet or barefoot on the floor, with the back resting on the vertical back of the meter, the upper limbs drooping naturally, the heels close together, the toes separated by 60°, and the head straight forward The waist circumference (WC) was measured using a tapeline, which was placed at the navel level to measure the waist perimeter at the end of exhalation.
The body mass index (BMI) was calculated using the weight and height measurements, and the participants were classified into 4 categories according to BMI: underweight (BMI <18.5 kg/m2), normal weight (18.5–24 kg/m2), overweight (24–28 kg/m2), and obese (×28 kg/m2).[25]
The WC was measured over the umbilicus between the lower border of the ribs and the iliac crest in a horizontal plane, with a cloth measuring tape. According to the standard Chinese definition,[26] central obesity was defined as a WC of ≥90 cm for men and ≥85 cm for women.
2.5. Statistical analysis
Data are presented as means ± SDs (continuous data) and as numbers and percentages (categorical data). Differences between men and women and between normal-weight and underweight participants or those with adiposity were evaluated using the t-test or chi-square test, followed by Bonferroni adjustment. The associations of adiposity with cognitive function were first assessed using binary logistic (drawing a picture) or linear (TICS, immediate word recall, delayed word recall, self-rated memory) regression models, as appropriate. Thereafter, multiple linear regression models or binary logistic regression models adjusting for potential confounders (i.e., age, education level, marital status, residence, cigarette smoking, alcohol drinking, eating habits, activity performance, history of a major accidental injury, self-reported health, physical exercises, sleeping hours, and diseases) were used to examine the odds ratios (ORs) or β values for cognition across a range of adiposity. All data were analyzed using SPSS version 17.0 (SPSS Inc., Chicago, IL).
3. Results
Table 1 shows the baseline characteristics of the participants. The sample (N = 9308) consists of 44.43% men and 55.57% women. Among the female participants 74.90% had started menopause, the mean age was 47.80 (SD = 5.04) years. Among the male participants, 13.14% had above high school education. By contrast, 13.00% of the male participants were illiterate and 73.87% had less than elementary school education. Among the women, only 7.07% had above high school education, 42.06% were illiterate, and 50.88% had less than elementary school education. Of the men, 65.99% live in rural areas and 34.01% in urban areas. Of the women, 63.70% live in rural areas and 36.30% in urban areas. Among all participants, the mean scores in TICS-10, immediate word recall, and delayed word recall were 6.42, 3.36, and 2.75, respectively. Further, 37.68% of the participants drew the picture successfully, whereas 62.32% failed. Among the total participants, 37.73% showed poor self-rated memory; 44.70%, fair; 12.65%, good; 4.54%, very good; and 0.38%, excellent. Specifically, 31.66% of the men showed poor self-rated memory; 48.17%, fair; 14.12%, good; 5.46%, very good; and 0.57%, excellent. Conversely, 43.06% of the women showed poor self-rated memory; 41.65%, fair; 11.35%, good; 3.74%, very good; and 0.20%, excellent. Among the men, the mean WC was 83.98 cm and the mean BMI was 22.98 kg/m2. Among the women, the mean WC was 84.67 cm and the mean BMI was 24.02 kg/m2. According to the modified Chinese criteria for BMI,[25] 25.58% of the men were overweight and 8.38% were obese, whereas 32.75% of the women were overweight and 14.50% were obese. According to the modified Chinese criteria for WC,[26] 29.80% of the men and 52.29% of the women were obese.
Table 2 shows the relationship between BMI and baseline characteristics in both men and women. History of a major accidental injury and performance of exercise had no significant difference between the BMI groups in men. Only history of a major accidental injury had no significant difference between the BMI groups in women. The differences in the other variables were insignificant.
Table 2.
Relationship of various characteristics and BMI in study population (N = 9308).
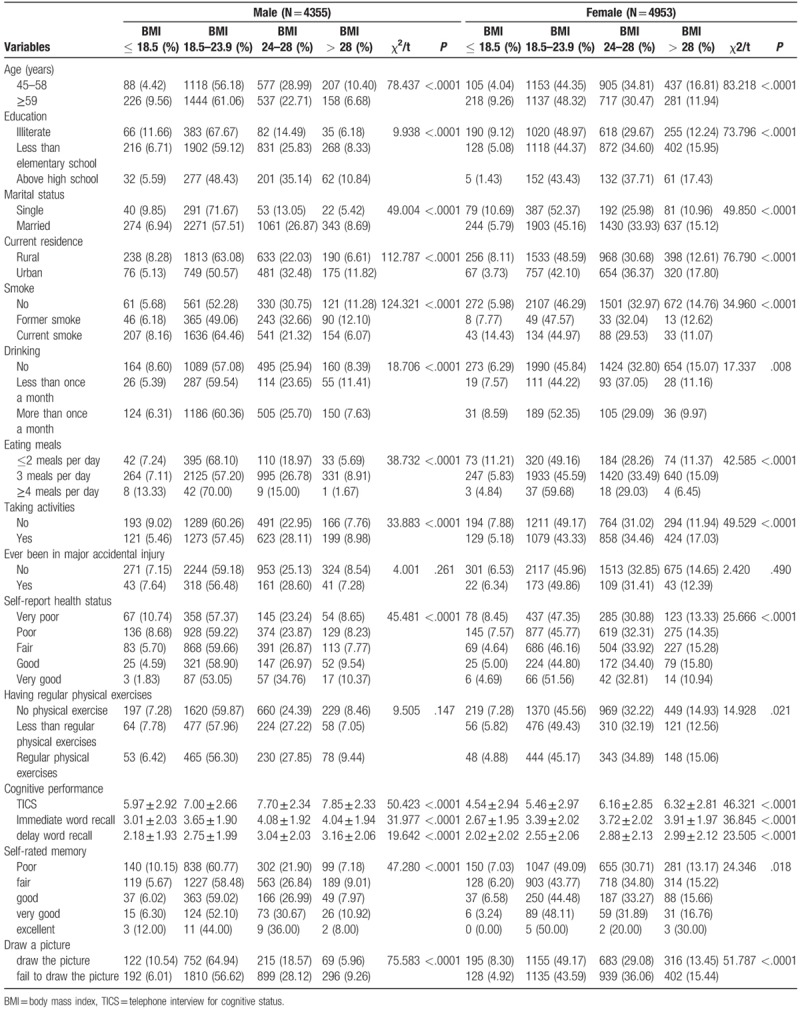
Table 3 shows the relationship between WC and baseline characteristics in both men and women. Alcohol drinking, history of a major accidental injury, and performance of exercise had no significant difference between the WC groups in men. Marital status, cigarette smoking, history of a major accidental injury, self-reported health, physical exercises, and self-rated memory had no significant difference between the WC groups in women. The differences in the other variables were insignificant.
Table 3.
Relationship of various characteristics and BMI in study population (N = 9308).
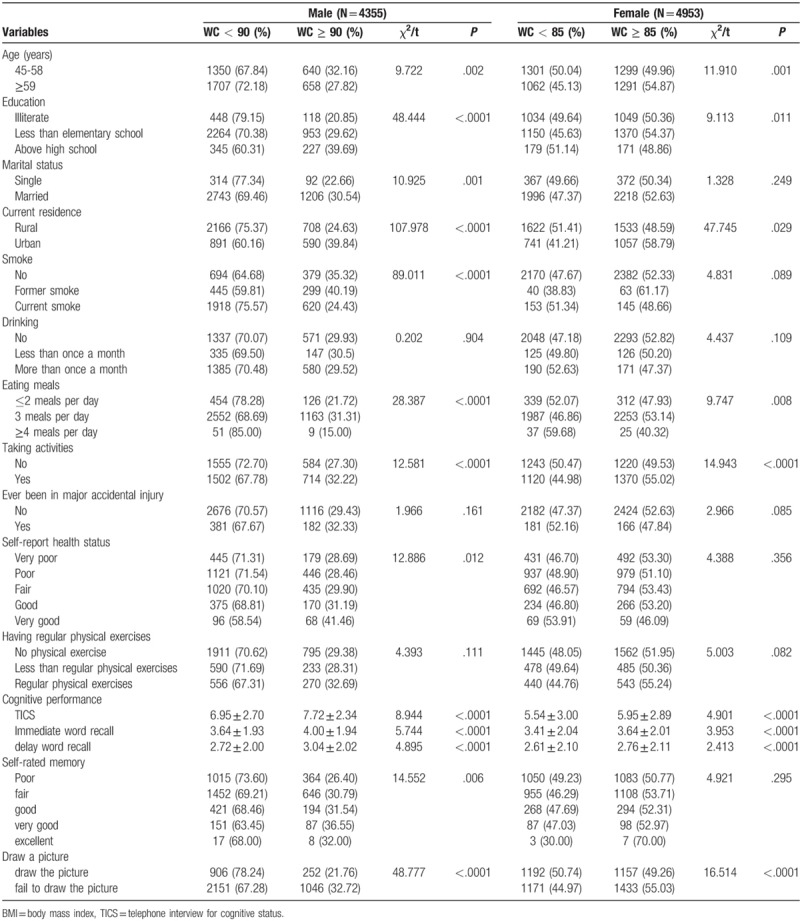
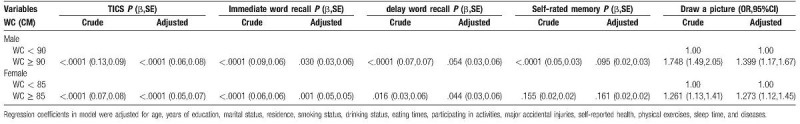
The regression analysis indicated that BMI and WC were linearly and positively associated with the domains of cognitive function (Table 4). After adjusting for age, education level, marital status, residence, cigarette smoking, alcohol drinking, eating habits, activity performance, history of a major accidental injury, self-reported health, physical exercises, sleeping hours, and diseases, we determined the outcomes of interest in the relationship between BMI and cognition (Table 4). First, compared with normal weight, overweight (men: P = .006, β = 0.04, standard error [SE] = 0.09; women: P < .0001, β = 0.06, SE = 0.08) and obesity (men: P = .005, β = 0.04, SE = 0.14; women: P < .0001, β = 0.05, SE = 0.11) had a significant positive association with mental capacity. Conversely, underweight in men (P < .0001, β = -0.07, SE = 0.14) had a significant negative association with mental capacity. Second, compared with normal weight, overweight (men: P = .015, β = 0.04, SE = 0.07; women: P = .011, β = 0.04, SE = 0.06) had a significant positive association with immediate recall; women with obesity (P = .002, β = 0.04, SE = 0.08) showed a similar ability to perform the task as in their ability of immediate recall. Underweight (men: P = .006, β = −0.04, SE = 0.11; women: P = .041, β = −0.03, SE = 0.11) had a significant negative association with the ability of immediate recall. Third, in women, overweight (P = .015, β = 0.03, SE = 0.06) and obesity (P = .031, β = 0.03, SE = 0.08) had a significant positive association with the ability of delayed recall. Lastly, middle-aged participants who were overweight (men: OR = 1.269, 95% confidence interval [CI] = 1.05–1.53; women: OR = 1.226, 95% CI = 1.06–1.42) tended to draw a more correct picture than middle-aged and elderly participants with normal weight.
Table 4.
Estimated crude and adjusting ORs for BMI and cognitive performance in population (N = 9308).
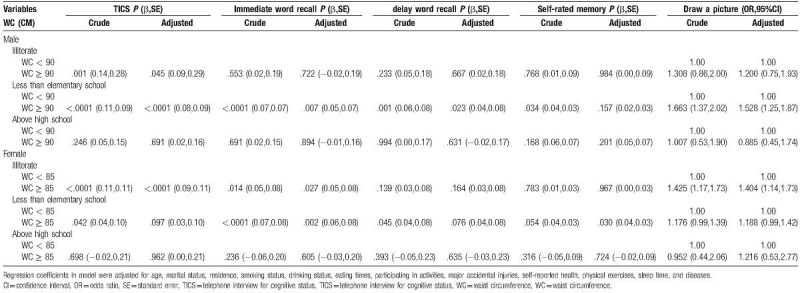
With respect to the association between WC and cognitive function (Table 5), participants with obesity demonstrated better mental capacity (men: P < .0001, β = 0.06, SE = 0.08; women: P < .0001, β = 0.05, SE = 0.07), ability to recall immediately (men: P = .030, β = 0.03, SE = 0.06; women: P = .001, β = 0.05, SE = 0.05), and ability to draw a picture (men: OR = 1.399, 95% CI = 1.17–1.67; women: OR = 1.273, 95% CI = 1.12–1.45) than those with normal weight after multivariate adjustment. Women with obesity (P = .044, β = 0.03, SE = 0.06) showed a better ability of delayed recall than participants with normal weight.
Table 5.
Estimated crude and adjusting ORs for WC and cognitive performance in population (N = 9308).
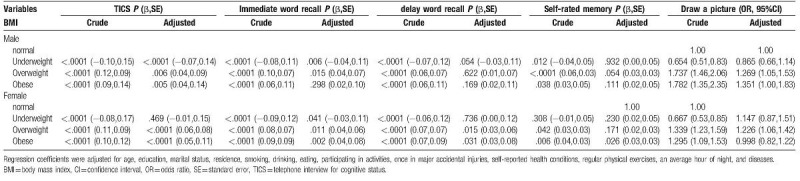
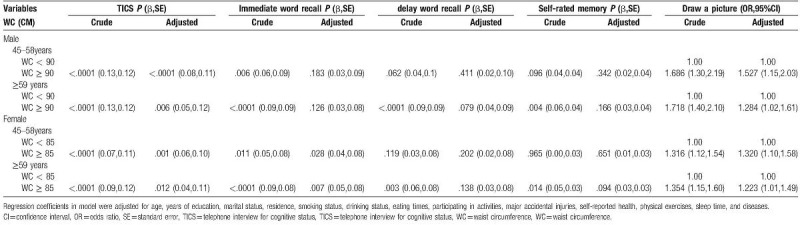
Tables 6 and 7 show relationships between BMI or WC and cognitive categorized by age in men and women. After adjusting for age, level of education, marital status, residence, cigarette smoking, alcohol drinking, eating habits, activity performance, history of a major accidental injury, self-reported health, physical exercises, sleeping hours, and diseases, we determined the outcomes of interest in the relationship between BMI and cognition (Table 6). First, compared with the participants with normal weight, the participants who were overweight (men with age of ≥ 59 years: P = .006, β = 0.05, SE = 0.13; women with age of ≥ 59 years: P < .0001, β = 0.07, SE = 0.12) and obese (men with age of ≥ 59 years: P = .014, β = 0.05, SE = 0.21; women with age of 45–58 years: P = .007, β=0.05, SE = 0.11; women with age of ≥59 years: P = .002, β = 0.06, SE = 0.17) had a significant positive association with mental capacity; Conversely, the participants who were underweight (men with age of 45–58 years: P = .002, β=-0.07, SE = 0.25; men with age of ≥59 years: P = .002, β = −0.06, SE = 0.18; women with age of 45–58 years: P = .023, β = −0.04, SE = 0.04) had a significant negative association with mental capacity. Second, compared with the participants with normal weight, the participants who were overweight (men with age of 45–58 years: P = .036, β = 0.05, SE = 0.10; women with age of ≥59 years: P = .003, β = 0.06, SE = 0.09) had a significant positive association with immediate recall; The women with age of 45–58 years who were obese (P = .021, β = 0.05, SE = 0.11) showed a similar ability to perform the task as in their ability of immediate recall. The men with age of ≥59 years who were underweight (P = .003, β = −0.06, SE = 0.13) had a significant negative association with the ability of immediate recall. Third, the women with age of ≥59 years who were overweight (P = .004, β=0.06, SE = 0.09) had a significant positive association with the ability of delay recall. Fourth, compared with the participants with normal weight, the participants who were overweight (men with age of ≥59 years: P = .022, β = 0.05, SE = 0.04; women with age of ≥59 years: P = .044, β = 0.04, SE = 0.04) and obese (women with age of ≥59 years: P = .018, β = 0.05, SE = 0.05) had a significant positive association with self-rated memory; Conversely, the men with age of 45–58 years (P < .0001, β = −0.12, SE = 0.02) had a significant negative association with self-rated memory. Lastly, the women with age 45–58 years (OR = 1.246, 95% CI = 1.02–1.53) were likely to draw a more correct picture than the middle-aged and elderly individuals with normal weight. Regarding the association between WC and cognitive function (Table 7), the subjects with obesity demonstrated better mental capacity (age of 45–58 years, men: P < .0001, β = 0.08, SE = 0.11; women: P = .001, β = 0.06, SE = 0.10. age of ≥59 years of age, men: P = .006, β = 0.05, SE = 0.12; women: P = .012, β = 0.04, SE = 0.11), ability to recall immediately (age of 45–58 years, women: P = .028, β = 0.04, SE = 0.08; age of ≥59 years, women: P = .007, β = 0.05, SE = 0.08), and ability to draw a picture (age of 45–58 years, men: OR = 1.527, 95% CI = 1.15–2.03; women: OR = 1.320, 95% CI = 1.10–1.58. age of ≥59 years, men: OR = 1.284, 95% CI = 1.02–1.61; women: OR = 1.223, 95% CI = 1.01–1.49) than those with normal weight after the multivariate adjustment.
Table 6.
Estimated crude and adjusting ORs for BMI and cognitive performance categorized by age in population (N = 9308).
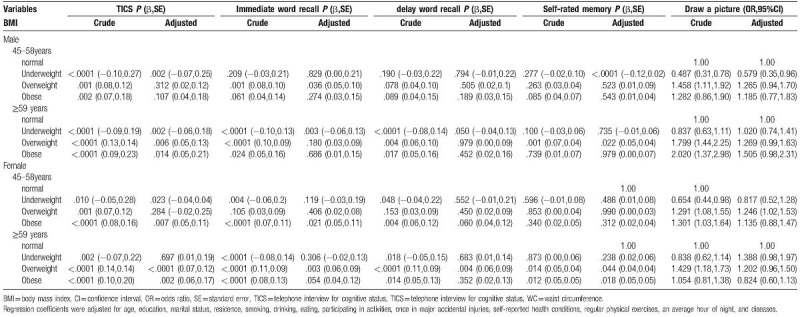
Table 7.
Estimated crude and adjusting ORs for WC and cognitive performance categorized by age in population (N = 9308).
Tables 8 and 9 show relationships between BMI or WC and cognitive categorized by educational levels in men and women. After adjusting for the related confounders, we determined the outcomes of interest in the relationship between BMI and cognition (Table 8). First, compared with the participants with normal weight, the participants who were overweight (men with less than elementary school education: P = .011, β = 0.05, SE = 0.10; women with illiterate: P = .001, β = 0.08, SE = 0.13) and obese (men with less than elementary school education: P = .005, β = 0.05, SE = 0.16; women with illiterate: P = .004, β = 0.06, SE = 0.18; women with less than elementary school education: P = 0.010, β = 0.05, SE = 0.15) had a significant positive association with mental capacity; conversely, the participants who were underweight (men with less than elementary school education: P < .0001, β = −0.07, SE = 0.17; men with above high school education: P = .014, β = −0.11, SE = 0.34) had a significant negative association with mental capacity. Second, compared with the participants with normal weight, the participants who were overweight (men with less than elementary school education: P = .044, β = 0.04, SE = 0.08; men with above high school education: P = .041, β = 0.09, SE = 0.17) had a significant positive association with immediate recall; The participants who were obese (women with illiterate: P = .028, β = 0.05, SE = 0.13; men with less than elementary school education: P = .016, β = 0.05, SE = 0.11) showed a similar ability to perform the task as in their ability of immediate recall. The men with illiterate who were underweight (P = .003, β = −0.12, SE = 0.24) had a significant negative association with the ability of immediate recall. Third, the women with less than elementary school education who were obesity (P = .043, β = 0.04, SE = 0.12) had a significant positive association with the ability of delay recall. Fourth, compared with the participants with normal weight, the men with less than elementary school education who were overweight (P = .023, β = 0.04, SE = 0.03) had a significant positive association with self-rated memory. Lastly, the men with less than elementary school education who were overweight (OR = 1.312, 95% CI = 1.06–1.63) and obesity (OR = 1.601, 95% CI = 1.11–2.31) were likely to draw a more correct picture than the middle-aged and elderly individuals with normal weight. Regarding the association between WC and cognitive function (Table 9), the subjects with obesity demonstrated better mental capacity (with illiterate, men: P = .045, β = 0.09, SE = 0.29; women: P < .0001, β = 0.09, SE = 0.11. with less than elementary school education, men: P < .0001, β = 0.08, SE = 0.09), ability to recall immediately (with illiterate, women: P = .027, β = 0.05, SE = 0.08. with less than elementary school education, men: P = .007, β = 0.05, SE = 0.07; women: P = .002, β = 0.06, SE = 0.08), ability to recall delay (men with less than elementary school education: P = .023, β = 0.04, SE = 0.08), self-rated memory(women with less than elementary school education: P = .030, β = 0.04, SE = 0.03), and ability to draw a picture (men with less than elementary school education: OR = 1.528, 95% CI = 1.25–1.87; women with illiterate: OR = 1.404, 95% CI = 1.14–1.73).
Table 8.
Estimated crude and adjusting ORs for BMI and cognitive performance categorized by education in population (N = 9308).
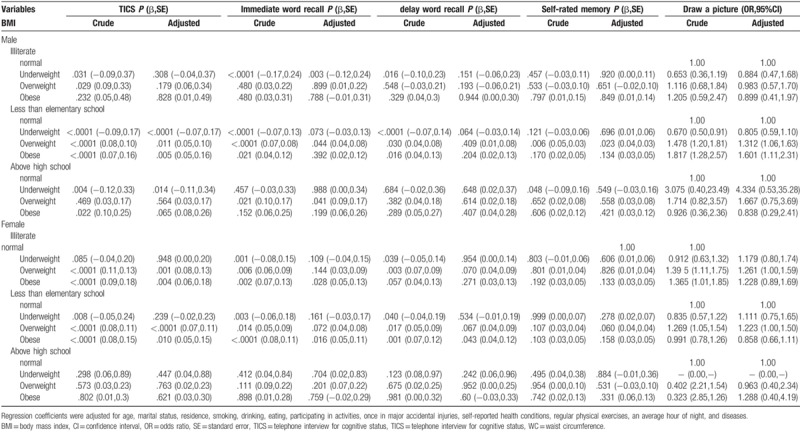
Table 9.
Estimated crude and adjusting ORs for WC and cognitive performance categorized by education in population (N = 9308).
4. Discussion
The association between adiposity parameters and cognition is complex in middle-aged and elderly individuals. Several studies have investigated the relationship between underweight or weight loss and dementia.[27,28] Kivipelto[29] and Johnson[30] reported that obesity at midlife was related to the risk of dementia, after adjusting for confounders of socio-demographic variables. Gorospe[31] suggested that the relationship between adiposity and cognition in late life remains controversial. However, Stewart[32] reported that no association or that being underweight is associated with dementia. Han[10] concluded that the relationship between obesity and cognitive defect differs between the sexes in the elderly. In men, the prevalence of obesity is increased over time when obesity in the baseline assessment has a positive effect on cognitive function. However, in women, the prevalence of obesity is decreased over time when obesity in the baseline assessment is associated with cognitive decline. Conversely, the prevalence is increased when normal weight is associated with cognitive decline.
In our study, we removed the possible confounders and discussed the relationship between 2 adiposity parameters and 5 domains of cognitive function. In this large cohort of middle-aged and older adults, we found a positive relationship between adiposity parameters and cognition in all variables after adjusting for age, education level, marital status, residence, cigarette smoking, alcohol drinking, eating habits, activity performance, history of a major accidental injury, self-reported health, physical exercise, sleeping hours, and diseases. Interestingly, we also found that there was a positive relationship between adiposity parameters and cognition in some domains. We also performed a stratified analysis according to age and education and found differences in the relationships between BMI or WC and cognitive function according to these variables. Specifically, participants with above high school education experienced no significant effect of BMI or WC on cognition. We carefully applied the “jolly fat” hypothesis,[33] which presumes that a relationship exists between adiposity and depression. It is well known that both adiposity and depression are associated with cognition;[3] thus, we examined whether the hypothesis could also be applied to the relationship between adiposity and cognition. Moreover, different relationships between adiposity parameters and cognition according to sex were observed in our study. Overweight and obese men had better cognitive performance in terms of mental capacity, immediate word recall, and ability to draw a picture, whereas overweight and obese women had better cognitive performance in terms of mental capacity, immediate and delayed word recall, and ability to draw a picture.
Our study found that a positive relationship between adiposity parameters and cognition exists in some domains in both sexes; however, the mechanisms were unclear. Considering the findings of our previous study,[34] this may be attributable to the fewer participants with depression in this study. Individuals who are less depressed tend to have the knowledge and attitude needed to cope with cognitive defects. Thus, these individuals tend to seek cognitive rehabilitation, which may contribute to the improved cognition found in middle-aged and elderly adults.
Pathophysiologic factors may play an important role in this sex difference. There are several possible explanations for the result. First, female sex is a well-known risk factor for dementia; the factors may have a greater effect on women than on men. Second, body fat, sex steroids, and their interaction in middle-aged and elderly participants may also contribute to the sex difference. As an important sex hormone, estrogen may have a key role in preventing cognitive defects. Middle-aged and elderly women with higher levels of adiposity have higher concentrations of estrogen, which may result in a strong protective effect against cognitive decline.
On the basis of the above-mentioned factors, our study demonstrated a significant relationship between adiposity parameters and cognition in both men and women, which supports the application of the “jolly fat” hypothesis.
This study has several limitations. First, the relationship between adiposity parameters and cognition in the elderly is complex. We considered as many confounders as possible; however, there are some unknown factors. Second, the relationship between adiposity parameters and cognition should be studied prospectively. We investigated cognition in middle-aged and elderly participants in a cross-sectional study. The follow-up duration was relatively short to observe changes comprehensively. Lastly, more studies are needed to confirm our results. Nevertheless, our study also has several strengths. First, this study was based on a nationwide survey. Second, we conducted the analyses according to sex. Third, we used 5 domains to measure the cognitive function and 2 parameters to classify the adiposity of the participants.
5. Conclusions
Our study demonstrated a significant relationship between adiposity parameters and cognition in both men and women, which supports the application of the “jolly fat” hypothesis.
Acknowledgments
We are grateful to the participants and members of the CHARLS. CHARLS was supported by the NIA.
Author contributions
LZ conceived and drafted the manuscript. J-lL, L-lZ, L-LG, HL, W-ZY and DL helped revise the manuscript.
Conceptualization: lin zhang, wenzhu yan.
Formal analysis: Lin Zhang.
Writing – original draft: Lin Zhang.
Writing – review and editing: Jin-long Li, Li-li Zhang, Lei-lei Guo, Hong Li, Dan Li.
Footnotes
Abbreviations: BMI = body mass index, CHARLS = China Health and Retirement Longitudinal Study, CI = confidence interval, NIA = national intelligence agency, OR = odds ratio, SE = Standard error, TICS = telephone interview for cognitive status, WC = waist circumference.
LZ and JlL contributed equally to this work.
The authors report no conflicts of interest.
References
- [1].Wang Y, Mi J, Shan XY, et al. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes (Lond) 2007;31:177–88. [DOI] [PubMed] [Google Scholar]
- [2].Zhao G, Ford ES, Li C, et al. Waist circumference, abdominal obesity, and depression among overweight and obese U.S. adults: National Health and Nutrition Examination Survey 2005–2006. BMC Psychiatry 2011;11:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Zhang L, Liu K, Li H, et al. Relationship between body mass index and depressive symptoms: the “fat and jolly” hypothesis for the middle-aged and elderly in China. BMC Publ Health 2016;16:1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Flint AJ, Rexrode KM, Hu FB, et al. Body mass index, waist circumference, and risk of coronary heart disease: a prospective study among men and women. Obes Res Clin Pract 2010;4:e171–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Regal P, Heatherington E. Body mass index and cognition. J Am Geriatr Soc 2012;60:1386–7. [DOI] [PubMed] [Google Scholar]
- [6].Su Y, Ma Y, Rao W, et al. Association between body mass index and diabetes in Northeastern China: based on dose-response analyses using restricted cubic spline functions. Asia Pac J Public Health 2016;28:486–97. [DOI] [PubMed] [Google Scholar]
- [7].Smith E, Hay P, Campbell L, et al. A review of the association between obesity and cognitive function across the lifespan: implications for novel approaches to prevention and treatment. Obes Rev 2011;12:740–55. [DOI] [PubMed] [Google Scholar]
- [8].Jensen GL, Friedmann JM. Obesity is associated with functional decline in community-dwelling rural older persons. J Am Geriatr Soc 2002;50:918–23. [DOI] [PubMed] [Google Scholar]
- [9].Davis JW, Ross PD, Preston SD, et al. Strength, physical activity, and body mass index: relationship to performance-based measures and activities of daily living among older Japanese women in Hawaii. J Am Geriatr Soc 1998;46:274–9. [DOI] [PubMed] [Google Scholar]
- [10].Han C, Jo SA, Seo JA, et al. Adiposity parameters and cognitive function in the elderly: application of “Jolly Fat” hypothesis to cognition. Arch Gerontol Geriatr 2009;49:e133–8. [DOI] [PubMed] [Google Scholar]
- [11].Kuo HK, Jones RN, Milberg WP, et al. Cognitive function in normal-weight, overweight, and obese older adults: an analysis of the advanced cognitive training for independent and Vital Elderly cohort. J Am Geriatr Soc 2006;54:97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Cournot M, Marquie JC, Ansiau D, et al. Relation between body mass index and cognitive function in healthy middle-aged men and women. Neurology 2006;67:1208–14. [DOI] [PubMed] [Google Scholar]
- [13].Sellbom KS, Gunstad J. Cognitive function and decline in obesity. J Alzheim Dis: JAD 2012;30Suppl 2:S89–95. [DOI] [PubMed] [Google Scholar]
- [14].Gunstad J, Lhotsky A, Wendell CR, et al. Longitudinal examination of obesity and cognitive function: results from the Baltimore longitudinal study of aging. Neuroepidemiology 2010;34:222–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ogunniyi A, Gao S, Unverzagt FW, et al. Weight loss and incident dementia in elderly Yoruba Nigerians: a 10-year follow-up study. Int Psychogeriatr 2011;23:387–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Barrett-Connor E, Edelstein S, Corey-Bloom J, et al. Weight loss precedes dementia in community-dwelling older adults. J Nutr Health Aging 1998;2:113–4. [PubMed] [Google Scholar]
- [17].Winocur G, Greenwood CE, Piroli GG, et al. Memory impairment in obese Zucker rats: an investigation of cognitive function in an animal model of insulin resistance and obesity. Behav Neurosci 2005;119:1389–95. [DOI] [PubMed] [Google Scholar]
- [18].Li C, Liu T, Sun W, et al. Prevalence and risk factors of arthritis in a middle-aged and older Chinese population: the China health and retirement longitudinal study. Rheumatology 2015;54:697–706. [DOI] [PubMed] [Google Scholar]
- [19].Chen CH, Liu LK, Chen MJ, et al. Associations between vitamin D deficiency, musculoskeletal health, and cardiometabolic risk among community-living people in Taiwan: age and sex-specific relationship. Medicine 2018;97:e13886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Zhang L, Li JL, Zhang LL, et al. No association between C-reactive protein and depressive symptoms among the middle-aged and elderly in China: Evidence from the China Health and Retirement Longitudinal Study. Medicine 2018;97:e12352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zhang L, Li JL, Zhang LL, et al. Association and interaction analysis of body mass index and triglycerides level with blood pressure in elderly individuals in China. BioMed Res Int 2018;2018:8934534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Chang HH, Yen ST. Association between obesity and depression: Evidence from a longitudinal sample of the elderly in Taiwan. Aging Ment Health 2012;16:173–80. [DOI] [PubMed] [Google Scholar]
- [23].Huang W, Zhou Y. Effects of education on cognition at older ages: evidence from China's Great Famine. Soc Sci Med 2013;98:54–62. [DOI] [PubMed] [Google Scholar]
- [24].Huang Z, Maurer J. Validity of self-rated memory among middle-aged and older chinese adults: results from the China health and retirement longitudinal study (CHARLS). Assessment 2017;1073191117741188. [DOI] [PubMed] [Google Scholar]
- [25].Zhou BF. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases–report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ Sci: BES 2002;15:245–52. [PubMed] [Google Scholar]
- [26].Zhou HC, Lai YX, Shan ZY, et al. Effectiveness of different waist circumference cut-off values in predicting metabolic syndrome prevalence and risk factors in adults in China. Biomed Environ Sci: BES 2014;27:325–34. [DOI] [PubMed] [Google Scholar]
- [27].Hansen ML, Waldorff FB, Waldemar G. Prognostic factors for weight loss over 1-year period in patients recently diagnosed with mild Alzheimer Disease. Alzh Dis Assoc Disord 2011;25:269–75. [DOI] [PubMed] [Google Scholar]
- [28].Sturman MT, de Leon CF, Bienias JL, et al. Body mass index and cognitive decline in a biracial community population. Neurology 2008;70:360–7. [DOI] [PubMed] [Google Scholar]
- [29].Kivipelto M, Ngandu T, Fratiglioni L, et al. Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch Neurol 2005;62:1556–60. [DOI] [PubMed] [Google Scholar]
- [30].Johnson DK, Wilkins CH, Morris JC. Accelerated weight loss may precede diagnosis in Alzheimer disease. Arch Neurol 2006;63:1312–7. [DOI] [PubMed] [Google Scholar]
- [31].Gorospe EC, Dave JK. The risk of dementia with increased body mass index. Age Ageing 2007;36:23–9. [DOI] [PubMed] [Google Scholar]
- [32].Stewart R, Masaki K, Xue QL, et al. A 32-year prospective study of change in body weight and incident dementia: the Honolulu-Asia Aging Study. Arch Neurol 2005;62:55–60. [DOI] [PubMed] [Google Scholar]
- [33].Crisp AH, Queenan M, Sittampaln Y, et al. ‘Jolly fat’ revisited. J Psychos Res 1980;24:233–41. [DOI] [PubMed] [Google Scholar]
- [34].Crisp AH, McGuiness B. Jolly fat: relation between obesity and psychoneurosis in general population. Br Med J 1976;1:7–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


