Abstract
The health effects of short-term exposure to air pollutants on respiratory deaths and its modifiers such as meteorological indexes have been widely investigated. However, most of the previous studies are limited to single pollutants or total respiratory deaths, and their findings are inconsistent.
To comprehensively examine the short-term effects of air pollutants on daily respiratory mortality.
Our analysis included 16,931 nonaccidental respiratory deaths (except lung cancer and tuberculosis) among older adults (>65 years) from 2011 to 2017 in Jinan, China. We used a generalized additive Poisson models adjusted for meteorology and population dynamics to examine the associations between air pollutants (particulate matter with an aerodynamic diameter of b2.5μm [PM2.5], particulate matter with an aerodynamic diameter of b10μm [PM10], SO2, NO2, O3) and daily mortality for the total patients, males, females, chronic airway diseases, pneumonia patients, and rest patients in Jinan.
Outdoor air pollution was significantly related to mortality from all respiratory diseases especially from chronic airway disease in Jinan, China. The effects of air pollutants had lag effects and harvesting effects, and the effects estimates usually reached a peak at lag 1 or 2 day. An increase of 10 μg/m3 or 10 ppb of PM2.5, PM10, SO2, NO2, and O3 corresponds to increments in mortality caused by chronic airway disease of 0.243% (95% confidence interval [CI]: −0.172–0.659) at lag 1 day, 0.127% (95% CI: −0.161–0.415) at lag 1 day, 0.603% (95% CI: 0.069–1.139) at lag 3 day, 0.649% (95% CI: −0.808–2.128) at lag 0 day and 0.944% (95% CI: 0.156–0.1598) at lag 1 day, respectively. The effects of air pollutants were usually greater in females and varied by respiratory subgroups. Spearman correlation analysis suggested that there was a significant association between meteorological indexes and air pollutants.
Sex, age, temperature, humidity, pressure, and wind speed may modify the short-term effects of outdoor air pollution on mortality in Jinan. Compared with the other pollutants, O3 had a stronger effect on respiratory deaths among the elderly. Moreover, chronic airway diseases were more susceptible to air pollution. Our findings provided new evidence for new local environmental and health policies making.
Keywords: air pollution, daily deaths, meteorological index, relative risk, respiratory disease
1. Introduction
It is known to all that air pollutants have obvious adverse effects on human health, especially on the respiratory system, and they are mainly composed of solid particles and gaseous pollutants such as SO2, NO, O3.[1] Over recent decades, China has become one of the most polluted countries around the world because of rapid economic development, accelerated urbanization, and industrialization.[2] So far, most of the previous studies were focused on the short-term or long-term relationship between air pollution and increased total respiratory or cardiovascular disease mortality, as well as increased rates of hospital admissions and emergency department visits.[3–6] For instance, a nationwide time-series analysis in 272 major Chinese cities from 2013 to 2015 found that a 10 μg/m3 increase in SO2 at lag 01 was associated with increments of 0.59%, 0.70%, and 0.55% in mortality from total non-accidental diseases, cardiovascular diseases, total respiratory diseases, respectively.[3] While the pollutants involved in each research were usually no more than 2. In studies by Wang,[3] Dominici,[4] and Chen[7] et al, health impacts of air pollutants on daily cause-specific mortality were limited to 1 pollutant such as SO2, fine particulate, and NO2, respectively. Moreover, the disease mortality was roughly divided into respiratory or cardiovascular disease mortality, and no further classification was made. So we conducted relatively comprehensive research on the association of the 5 main air pollutants and specific respiratory diseases mortality (J00-J99) in Jinan, Shandong province, Eastern China, modified by various meteorological indexes.[7,8] Jinan is one of the most polluted cities in China due to its heavy industry-led economic model and coal burning in winter.[9] To a certain extent, the conclusions of our study may have a reference value for other heavily polluted cities in China. We found that about 89.33% of deaths caused by respiratory diseases were observed among older adults (>65 years), suggesting that the elderly exposed to air pollutants were at higher risk of death than the young, consistently to other documented evidence.[3,7–9] Therefore it is urgently for us to explore the exact effects of air pollution on mortality especially among older adults with the aim of promoting public health policy-making. The objective of our study is to explore the lag impact and the cumulative impact of air pollutants on various respiratory diseases daily mortality in eastern China. We also examined the modifying effects of gender, age, and meteorological indexes.
2. Materials and methods
2.1. Ethics
Ethics approval was obtained from the Ethics Committee of Shandong Provincial Hospital, Affiliated to Shandong University, Jinan, Shandong, China. Patient records were anonymized and deidentified before our analysis.
2.2. Data
Causes of death were classified according to the International Classification of Diseases, Tenth Revision (ICD-10; WHO 1993). We examined total daily mortality caused by respiratory disease (J00–J99) and cause-specific daily mortality attributed to chronic airway diseases (J40–47, including chronic obstructive pulmonary diseases [COPD], asthma, chronic respiratory failure, bronchiectasis), pneumonia (J12–J18), the rest (J30–39, J60–J99). To gain a more accurate result, this research has ruled out acute respiratory infections (J00–J11, J20–J22) due to its negligible mortality, tuberculosis and lung cancer were excluded as well. Daily non-accidental mortality data from 2011 to 2017 were obtained from Jinan Municipal Center for Disease Control and Prevention. The data of daily air pollutants concentration during the same period, including particulate matter with an aerodynamic diameter of b2.5μm (PM2.5), particulate matter with an aerodynamic diameter of b10μm (PM10), SO2, NO2, and O3, were collected from the Environmental Monitoring Center of Jinan. The pollutant monitoring network was composed of 12 urban monitoring stations and 2 suburban monitoring stations. We abstracted the daily 24-hours average concentrations of air pollutants (PM2.5, PM10, SO2, and NO2) collected from these 14 monitoring stations as well as maximal 8-hours mean concentrations for O3. Meteorological data of Jinan from 2011 to 2017 were collected from the National Meteorological Information Center in China (http://www.nmic.gov.cn/web/channel-46 4.htm) to explore their impacts to the association of air pollution and daily mortality. Meteorological indexes were daily mean temperature, air pressure, humidity, and wind speed, respectively.
2.3. Method of analysis
We applied generalized additive Poisson models to examine the associations between air pollution (PM2.5, PM10, SO2, NO2, and O3) and day-to-day variations in the respiratory mortality for the total patients, males, females, chronic airway diseases, pneumonia patients, and rest patients in Jinan. The Quasi-Poisson distribution was adopted if there was an overdispersion in mortality data. Generalized additive models allow for highly flexible fitting as the outcome is assumed to be dependent on a sum of the smoothed and linear functions of the predictor variables. A smoothed function captures the nonlinear relationship between daily deaths and the time-varying covariates such as the temperature and the calendar time. The nonlinear term in generalized additive models can be estimated by using smoothing splines, which transform a possible nonlinear relationship into a linear form by separating the data into subintervals based on the basis functions. Degrees of freedom (df) of smoothed functions were determined by the Akaike information criterion (Akaike, 1987). The daily ambient air pollutant (PM10, PM2.5, SO2, and NO2) concentrations for the 0 to 6 day lags were analyzed separately in association with daily deaths. Then the cumulative effects of air pollution on daily mortality were conducted by using a moving average. We also applied 2-pollutant and all pollutant models, by including pollutants at the same lag. Briefly, we fitted the data into the following model:
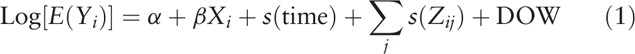 |
where E(Yi) is the expected number of daily COPD deaths at day i, α is the intercept term, β is the regression coefficient, and Xi is the pollutant measurements on day i s(time) denotes the smoothing splines of calendar time and s(Zij) denotes the smoothing splines of the meteorological variables Zj such as the temperature, relative humidity, pressure, and wind speed, respectively. The dummy variable DOW is the indicator for the day of the week. All statistical analyses were performed with R V.3.4.3 (URL http://www.R-project.org) using the package mgcv (V.1.8–17). Then all results were presented as the percentage change in the relative risk (RR) of mortality and its 95% confidence interval (CI) in association with a 10 μg/m3 or a 10 ppb increase in daily air pollutants.[10]
3. Results
3.1. Mortality and air pollution data
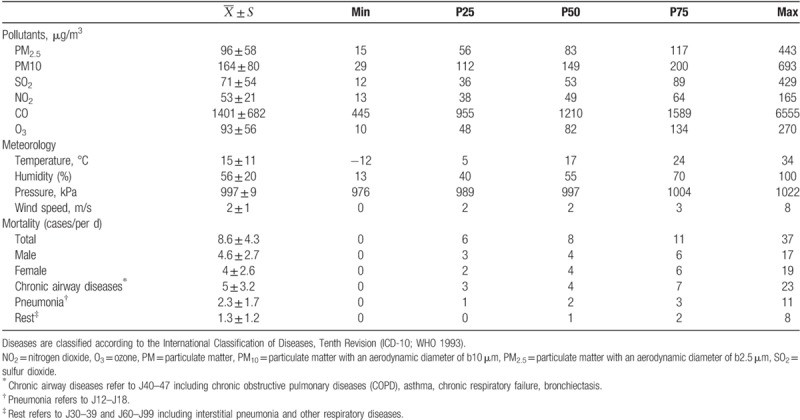
There were 18,952 deaths due to respiratory disease including chronic airway diseases (10,983), pneumonia (4942), acute respiratory infections (228), and others (2799) in Jinan, China from 2011 to 2017, of which 10,090 males, 8862 females, and 16,931 patients over 65 years old, 2020 records for those under 65. Table 1 provides data on daily mortality, air pollutants, temperature (°C), humidity (%), pressure (kPa), wind speed (m/s). The mean concentration of PM2.5, PM10, SO2, NO2, CO, O3 were 96 μg/m3, 164 μg/m3, 71 μg/m3, 53 μg/m3, 1401 μg/m3, respectively. Annual average value of temperature (°C), humidity (%), pressure (kPa), wind speed (m/s) were 15 (°C), 96 (%), 997 (kPa), 2 (m/s), respectively. Total daily death counts caused by respiratory disease (except lung cancer and lung tuberculosis) were 8.6, of which the males and the females are 4.6 cases and 4 cases, respectively. When the causes of death were further classified by disease entities, we found that daily death counts caused by chronic respiratory disease, pneumonia and the rest were 5 cases, 2.3 cases, 1.3 cases, respectively.
Table 1.
Descriptive statistics of air pollutants, daily mortality and weather condition in Jinan, China from 2011 to 2017.
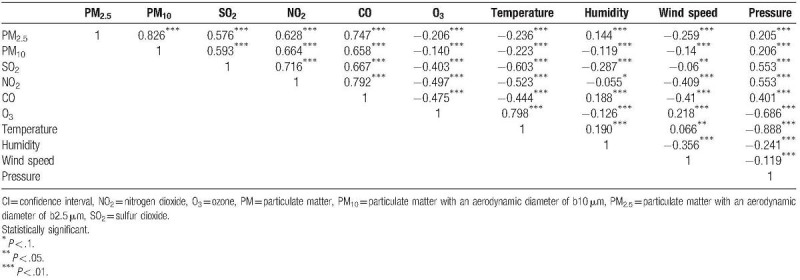
3.2. Spearman correlation analysis
Table 2 illustrates spearman correlation between air pollutants and weather conditions in Jinan, China from 2011 to 2017. At the mean level, there were positive and moderate-to-strong correlations among PM2.5, PM10, SO2, NO2, CO other than inverse and weak correlations for O3. The correlation coefficient of PM2.5 with PM10 and CO with NO2 was 0.862 (P < .01) and 0.797 (P < .01), respectively. Air pollutants (except for O3) had an inverse and weak-to-moderate correlation with temperature and wind. The correlation coefficient of temperature and O3 was as high as 0.798 (P < .01). In addition, as shown in Table 2, there was an inverse and weak correlation between humidity and air pollutants (except for CO and PM2.5). Pressure was weak-to-moderate correlated with air pollutants (except for O3), but negative with other weather conditions. The correlation coefficients of pressure with O3 and pressure with temperature were −0.686 (P < .01) and −0.888 (P < .01), respectively. The correlation coefficients were negative between weather conditions except for temperature with humidity and wind. It suggests that the research about estimates of air pollutants on daily specific-caused deaths should control the effects of other pollutants and meteorological factors.
Table 2.
Spearman correlation between air pollutants and weather conditions in Jinan, China, 2011–2017.
3.3. Single pollutant models
It is shown in Table 3 and Figure 1 that the association of air pollutants with respiratory diseases caused mortality varied by gender and respiratory disease categories in single-pollutant models. What's more, Table 3 also illustrated the single-day effects and the cumulative effects of a 10 μg/m3 or a 10 ppb increase in pollutants to the RR of mortality from respiratory diseases. However, all presented a trend of earlier increase and later decrease from lag 0 to 6 day. PM2.5 (lag 1), SO2 (lag 1),O3 (lag 3), PM10 (lag 1), NO2 (lag 0) had a highest positive association with the RR of mortality caused by total daily respiratory diseases, and the RR estimates of daily cause-specific mortality was associated with a 10 μg/m3 increase in pollutants is 0.383% (95% CI: 0.068, 0.699), 0.514% (95% CI: 0.095, 0.936), 0.975% (95% CI: 0.463, 1.489), 0.194% (95% CI: −0.023, 0.412), 0.822% (95% CI: −0.284, 1.941), respectively, of which the former 3 is statistically significant (P < .05). While considering a modifier of death estimates such as gender, we found that nothing but the increased RR of death estimates associated with a 10 μg/m3 increase in O3 (lag 1–3) was statistically significant (P < .05) among males and they were 1.139% (95% CI: 0.347, 1.937), 0.737% (95% CI: 0.028, 1.451), 1.034% (95% CI: 0.336, 1.738) in turn. In females, increments in SO2 exposure at lag 0 to 1 day and O3 exposure at lag 0, 3, 6 day had a statistically significant association with increases in RR of respiratory diseases caused deaths (P < .05), with an odds ratio of 0.841% (95% CI: 0.222, 1.463), 0.653% (95% CI: 0.059, 1.251), −1.180% (95% CI: −2.164, −0.187), 0.902% (95% CI: 0.161, 1.649), −0.623% (95% CI: −1.128, −0.115), respectively. However, when the causes of death were further divided into chronic airway diseases (including COPD, asthma, chronic respiratory failure, bronchiectasis), various pneumonia and the rest (including interstitial pneumonia and the rest respiratory diseases), the degree of correlation between exposure concentrations of pollutants and death and the optimal lag day were also changed. At the same time, the lag days corresponding to the maximum effect also varied. As shown in Table 3, for death counts attributed to chronic airway diseases, a 10 μg/m3 increase in 6, 7 day mean PM10, 3 day mean lag SO2, and 2, 4, 7 day mean O3 concentrations had a statistically significant association with a −0.285% (95% CI: −0.556, −0.013), −0.295% (95% CI: −0.565, −0.024), 0.603% (95% CI: 0.069, 1.139), 0.944% (95% CI: 0.156, 1.739), 0.897% (95% CI:0.200, 1.598), −0.772% (95% CI: −1.459, −0.081) increased OR of death, respectively. In addition, various pneumonia (except Interstitial pneumonia) mortality were associated with PM2.5 (lag 1) and O3 (lag 3) with 0.672% (95% CI: 0.049, 1.298) and 1.114% (95% CI: 0.159, 2.078) for an increase of 10 μg/m3 (P < .05). Moreover, a 10 μg/m3 increase in same day PM2.5 concentration contributed to an increased RR estimates of deaths caused by the rest respiratory diseases of 1.032% (95% CI: 0.110, 1.962) (P < .05). As for cumulative effects, we found that its RR estimates of different groups were usually larger than that of single-day effects, but the trends were consistent when the lag days were going on.
Table 3.
Percent increases in relative risk (RR) of daily non-accidental and cause-specific mortality associated with a 10 μg/m3 increase in air pollutants using single pollutant models at lag 0 to 7 day and lag 01 to 06 day in Jinan, China from 2011 to 2017. Results were controlled for seasonality, day of the week, temperature, relative humidity, air pressure, and wind speed.
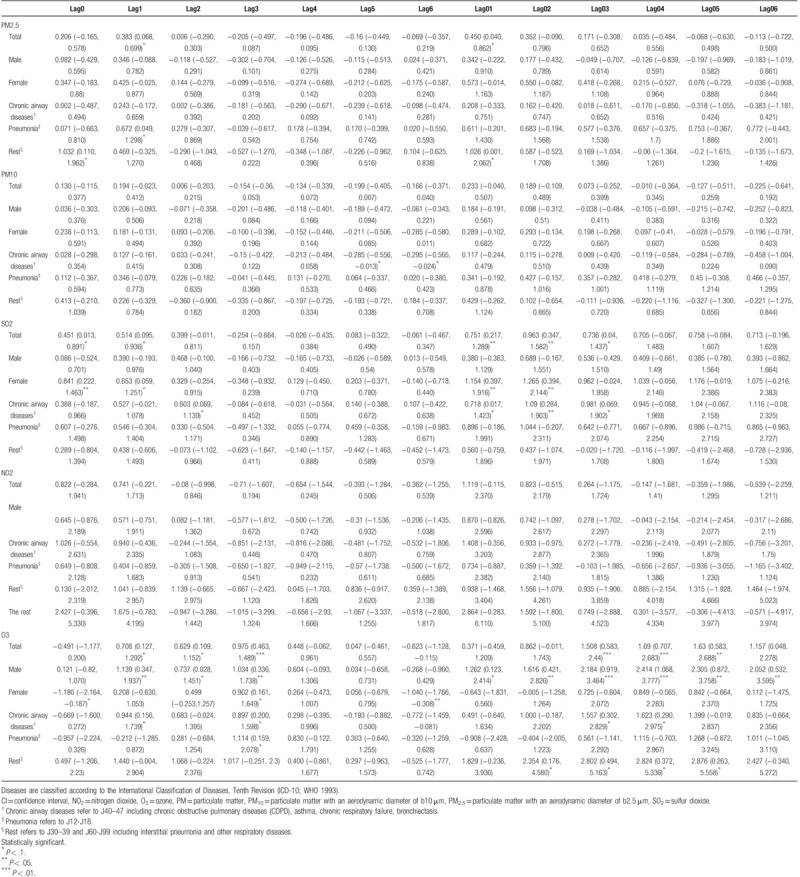
Figure 1.
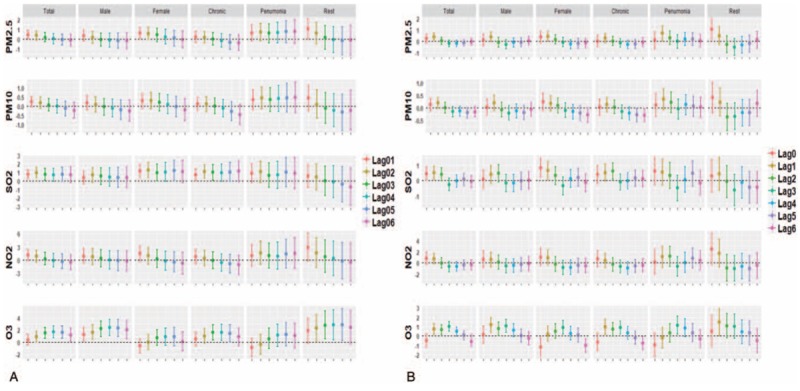
The excess risk and 95% CI per 10 μg/m3 increase of air pollutants on cause-specific daily deaths using single pollutant models at lag 0 to 7 day and lag 01 to 06 day in Jinan, China from 2011 to 2017. Results were controlled for seasonality, day of the week, temperature, relative humidity, air pressure, and wind speed. A. lag effects; B. cumulative effects. Chronic refers to chronic airway diseases (J40–47) including COPD, asthma, chronic respiratory failure, bronchiectasis. Pneumonia refers to J12–J18. Rest refers to J30–39 and J60–J99 including interstitial pneumonia and other respiratory diseases. Diseases are classified according to the International Classification of Diseases, Tenth Revision (ICD-10; WHO 1993). Statistically significant (∗P < .1, ∗∗P < .05, ∗∗∗P < .01). CI = confidence interval, COPD = chronic obstructive pulmonary diseases, NO2 = nitrogen dioxide, O3 = ozone, PM = particulate matter, PM10 = particulate matter with an aerodynamic diameter of b10 μm, PM2.5 = particulate matter with an aerodynamic diameter of b2.5 μm, SO2 = sulfur dioxide.
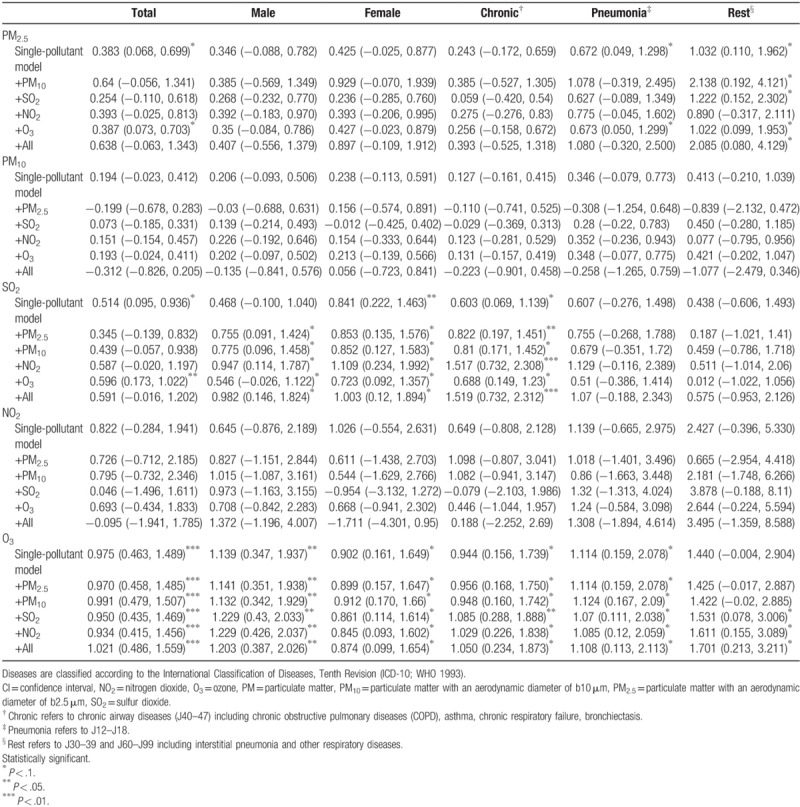
3.4. Copollutant models
Table 4 summarizes the relationship between PM2.5, PM10, SO2, NO2, O3 at lag 0 to 1 with excess daily total, gender-stratified and respiratory disease-stratified mortality count (%) of Jinan, China from 2011 to 2017 in single and copollutant models. In the single-pollutant models for PM2.5 and SO2, an increase of 10 μg/m3 were statistically related to the increased daily respiratory mortality of 0.383% (95% CI: 0.068, 0.699) and 0.514% (95% CI: 0.095, 0.936), respectively. We found that the excess mortality estimates increased to 0.387% (95% CI: 0.073, 0.703), 0.596 (95% CI: 0.173, 1.022), respectively when PM10 and SO2 were separately adjusted by O3. As shown in Table 4, the mortality estimates varied by gender and disease subgroups, which was higher in females than males, as well as among deaths caused by pneumonia than deaths caused by chronic airway disease. We also found that when O3 was adjusted by PM2.5, PM10, SO2, or NO2 in copollutant models, the mortality estimates still remained to be statistically significant.
Table 4.
Percent changes (95% posterior intervals) in the relative risk (RR) of daily total respiratory mortality, male/female respiratory mortality, chronic airway diseases/pneumonia /the rest mortality per 10 ug/m3 or per 10 ppb increase in 2-day moving average (lag 01) concentrations of PM2.5, PM10, SO2, NO2, O3 in Jinan, China from 2011–2017, with adjustment of copollutants.
4. Discussion
This time-series analysis of all deaths caused by respiratory diseases from 2011 to 2017 in Eastern China, Jinan found that 10 μg/m3 daily increments of PM2.5, SO2, and 10 ppb daily increments of O3 were statistically associated with percent changes on the RR of cause-specific daily mortality. In addition, We found that short-term exposure to PM10 had limited impacts on daily mortality, similar to the results of a study involved 0.235 million people in 2015.[11,12] However, some previous studies conducted in China showed an opposite conclusion that PM10 was significantly associated with respiratory disease,[13,14] especially among population suffered from chronic diseases rather than health groups.[15] Therefore, whether PM10 has an influence on respiratory mortality remains to be explored. Consistent with previous researches,[11,16,17] our study suggested that the estimates of health effects had a lag effect and harvesting effect, besides which they also differed between single pollutant models and multiple pollutants model as well as females and males. Previous studies have shown that exposure to air pollution has an impact on additional deaths and hospitalization rates among the public, especially among older adults and people who are sick. A decrease in mortality during the subsequent weeks has been observed because those whose health is already so compromised would be more likely to have died in the short term during early stages of ecological studies, and this would result in an overestimation of health effects attributed to air pollution in the early stages but an underestimation in the later stages. Therefore harvesting effect also refers to mortality displacement, which denotes a temporary increase in the mortality rate in a given population during the early period of ecological researches, indicating the important role of harvesting effect on ecological researches.[18,19] As the data shown in all Figure 1, single day effects of PM2.5, PM10, SO2, NO2, O3 on mortality risk of total respiratory disease usually reached a peak at lag 1 or lag 2 (Fig. 1B), consistently with which the moving average over the same day and the previous day (lag 01) of PM2.5, PM10, NO2 had a maximal effects, and the cumulative effects of SO2 and O3 reached a peak at lag 02 and lag 04, respectively (Fig. 1A). In single pollutant models, we observed a increased RR in mortality of 0.383% (95% CI: 0.068, 0.699), 0.194% (95% CI: −0.023, 0.412), 0.514% (95% CI: −0.095, 0.936), 0.822% (95% CI: −0.284, 1.941), 0.975% (95% CI: −0.463, 1.489) per 10 μg/m3 daily increments of PM2.5, PM10, SO2, NO2, and per 10 ppb daily increments of O3, respectively. As the results shown, gaseous pollutants, especially O3, had a greater impact on daily respiratory deaths than fine particulate matter, and the effects of ozone on mortality from chronic lower respiratory diseases observed in our research was identical with the results from a study of 265,223 deaths (aged ≥45 years) in the contiguous United States during 2007 to 2008.[20] A potential explanation was that O3 could induce or accelerate excess pulmonary inflammation through some pathophysiological pathways, resulting in damage on the airway epithelium cells which could make people especially COPD patients become more susceptible to environmental aggressions, meanwhile contributed to a reduced lung function.[20–22] We observed that there was a greater impact on total respiratory mortality among females than males. The opinions of previous studies on the gender-specific effects of air pollutants on mortality were inconsistent, a majority of studies[11,23,24] hold the opinion that females were more susceptible than males due to the narrower respiratory tract and slightly greater airway reactivity.[23,25] Another possible explanation was the different socioeconomic status and stress experiences between females and males, females were more likely to be unemployed thus spend more time outdoors.[26–28] In contrast, some studies supported that males were more sensitive because a larger proportion of women preferred to use a mask when outdoors.[11,29,30] Thus, further studies that assess the gender-stratified pattern of pollutant-health relationship are necessary. A number of previous studies[17,31–33] had revealed that the estimated effects of multiple pollutants models on total mortality were smaller than that of single pollutant models because of the colinearity among air pollutants as well as photochemical interactions and commonality of sources, which was also found in our study except for O3. We found a novel phenomenon that air pollutants especially SO2 exhibited greater health effects on chronic airway diseases (including COPD, asthma, chronic respiratory failure, and bronchiectasis) than pneumonia and the rest respiratory diseases. Actually, few previous studies had applied respiratory diseases subgroups-stratified pattern on the analysis of the association between air pollution and daily mortality. Our findings to some extent are consistent with earlier observation results that exposure to air pollution has been significantly related to non-infectious respiratory diseases, but few evidence has suggested the association of air pollutants with infectious respiratory diseases.[34–36]
This study has several strengths. First, unlike previous air pollution studies, most of which only analyzed the impact of 1 or 2 pollutants on daily mortality, 2 particulate matter (PM2.5, PM10) and 3 gas pollutants (SO2, NO2, O3) were considered in this study to make a comprehensive analysis. Second, the health effects of these 5 pollutants were estimated both in single-pollutant models and multiple pollutants models considering the highly colinear components of ambient air pollutants. Third, our study was distinguished from the former ecologic analysis in that we divided respiratory disease into 3 subgroups including chronic airway diseases, various pneumonia, and the rest, resulted in a novel finding that the estimates effects also varied by respiratory disease subgroups. Fourth, our study was conducted in a classical metropolitan area of heavy industries which was one of the most heavily polluted cities in China,[9] and the time span of this study was up to 7 years, which was contributed to make a more accurate estimation of air pollution effects.
There are also some limitations. The primary limitation of this research was that we used average ambient pollutant concentration as a surrogate of individual level rather than exact exposure, so it was inevitable to some unknown measurement errors. As a result, it may lead to a bias of pollution effects. However, this problem also exists in other investigations. Second, this study was limited to be performed in only 1 city, thus the generalizability of our finding is constrained. Moreover, personal behaviors such as smoking, time spent outdoors, and other factors such as occupational exposures also have an influence on the relationship of daily mortality and air pollution. For instance, the elderly were more likely to stay at home, so there may be an underestimation of the health effects on the elderly. However, relevant data is difficult to assess and obtain.
5. Conclusion
This study highlights the significant association of PM2.5, PM10, SO2, NO2, O3 with daily respiratory deaths in a heavily polluted city in Eastern China, and the association between daily respiratory deaths and air pollutants varied by disease subgroups. O3 had a stronger effect on respiratory deaths among the elderly than other pollutants. We found that the impacts of SO2 on chronic airway diseases among the elderly were greater than other respiratory diseases. Moreover, air pollution had a greater impact on total respiratory mortality among females than males. Our findings could make a contribution to develop public policy for individualized protection and protect human health. Our results suggested that in order to intensively explore the individual mechanism of pollutants on specific disease, the future study on the association of air pollution exposure and daily mortality may be conducted among cause-specific deaths, for instance, deaths caused by COPD, pneumonia, tuberculosis, lung cancer, asthma, and so on. There are still some limitations of mortality risk as an indicator to evaluate the health effects of air pollution, so new complementary indicators remains to be found such as years of life lost. Furthermore, it remains a great problem on how to control and evaluate individual risk factors during such ecological studies.
Acknowledgments
We thank China Weather Data Sharing System and the national Air Reporting System for providing weather data and air pollution data.
Author contributions
Conceptualization: Liu-Xin Wang, Huai-Chen Li.
Data curation: Huai-Chen Li.
Formal analysis: Wan-Mei Song, Yi Liu, Jin-Yue Liu, Yi-Fan Li, Yao Liu, Liu-Xin Wang, Huai-Chen Li.
Funding acquisition: Huai-Chen Li.
Investigation: Wan-Mei Song, Ning-Ning Tao, Yi Liu, Yi-Fan Li.
Methodology: Ning-Ning Tao, Yi Liu, Huai-Chen Li.
Project administration: Huai-Chen Li.
Resources: Huai-Chen Li.
Software: Yi Liu.
Validation: Huai-Chen Li.
Writing – original draft: Wan-Mei Song.
Writing – review and editing: Wan-Mei Song, Huai-Chen Li, Yi Liu.
Footnotes
Abbreviations: CI = confidence interval, NO2 = nitrogen dioxide, O3 = ozone, PM = particulate matter, PM10 = particulate matter with an aerodynamic diameter of b10μm, PM2.5 = particulate matter with an aerodynamic diameter of b2.5μm, RR = relative risk, SO2 = sulfur dioxide.
W-MS and YL contributed equally to this work.
This work was supported by Department of Health of Shandong Province (No. 2009GG10002054); Department of Science & Technology of Shandong Province (CN) (No. 2007GG30002033); (No. 2017GSF218052) and Jinan Science and Technology Bureau (CN) (No.201704100).
The authors have no conflicts of interest to disclose.
References
- [1].Organization W H. ES FS313 Ambient (outdoor) air quality and health[J] Centro De Prensa, 2014. [Google Scholar]
- [2].Bai R, Lam JCK, Li VOK. A review on health cost accounting of air pollution in China. Environ Int 2018;120:279–94. [DOI] [PubMed] [Google Scholar]
- [3].Wang L, Liu C, Meng X, et al. Associations between short-term exposure to ambient sulfur dioxide and increased cause-specific mortality in 272 Chinese cities. Environ Int 2018;117:33–9. [DOI] [PubMed] [Google Scholar]
- [4].Dominici F, Peng RD, Bell ML, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 2006;295:1127–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Pope CA, 3rd, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc 2006;56:709–42. [DOI] [PubMed] [Google Scholar]
- [6].Samoli E, Peng R, Ramsay T, et al. Acute effects of ambient particulate matter on mortality in Europe and North America: results from the APHENA study. Environ Health Perspect 2008;116:1480–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chen R, Yin P, Meng X, et al. Associations between ambient nitrogen dioxide and daily cause-specific mortality: evidence from 272 Chinese cities. Epidemiology 2018;29:482–9. [DOI] [PubMed] [Google Scholar]
- [8].Wu R, Zhong L, Huang X, et al. Temporal variations in ambient particulate matter reduction associated short-term mortality risks in Guangzhou, China: a time-series analysis (2006–2016). Sci Total Environ 2018;645:491–8. [DOI] [PubMed] [Google Scholar]
- [9].Zhang J, Liu Y, Cui L, et al. Ambient air pollution, smog episodes and mortality in Jinan, China. Sci Rep 2017;7:11209–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lin H, Liu T, Xiao J, et al. Mortality burden of ambient fine particulate air pollution in six Chinese cities: results from the Pearl River Delta study. Environ Int 2016;96:91–7. [DOI] [PubMed] [Google Scholar]
- [11].Xue X, Chen J, Sun B, et al. Temporal trends in respiratory mortality and short-term effects of air pollutants in Shenyang, China. Environ Sci Pollut Res Int 2018;25:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Carugno M, Randi G, Campagnolo D, et al. Mortality and morbidity health impact assessment of expected exposure to PM10 due to the major construction site for a large international exhibition. Occup Environ Med 2014;0257:A33–4. [Google Scholar]
- [13].Chen R, Pan G, Kan H, et al. Ambient air pollution and daily mortality in Anshan, China: a time-stratified case-crossover analysis. Sci Total Environ 2010;408:6086–91. [DOI] [PubMed] [Google Scholar]
- [14].Shang Y, Sun Z, Cao J, et al. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ Int 2013;54:100–11. [DOI] [PubMed] [Google Scholar]
- [15].Alessandrini ER, Stafoggia M, Faustini A, et al. Association between short-term exposure to PM2.5 and PM10 and mortality in susceptible subgroups: a multisite case-crossover analysis of individual effect modifiers. Am J Epidemiol 2016;184:744–54. [DOI] [PubMed] [Google Scholar]
- [16].Zhu J, Zhang X, Zhang X, et al. The burden of ambient air pollution on years of life lost in Wuxi, China, 2012-2015: A time-series study using a distributed lag non-linear model. Environ Pollut 2017;224:689–97. [DOI] [PubMed] [Google Scholar]
- [17].Guo Y, Li S, Tian Z, et al. The burden of air pollution on years of life lost in Beijing, China, 2004-08: retrospective regression analysis of daily deaths. BMJ 2014;347:f7139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Schwartz J. Harvesting and long term exposure effects in the relation between air pollution and mortality. Am J Epidemiol 2000;151:440–8. [DOI] [PubMed] [Google Scholar]
- [19].Qiao Z, Guo Y, Yu W, et al. Assessment of short-and long-term mortality displacement in heat-related deaths in Brisbane, Australia, 1996–2004. Environ Health Perspect 2015;123:766–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hao Y, Balluz L, Strosnider H, et al. Ozone, fine particulate matter, and chronic lower respiratory disease mortality in the United States. Am J Respir Crit Care Med 2015;192:337–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kinney PL, Nilsen DM, Lippmann M, et al. Biomarkers of lung inflammation in recreational joggers exposed to ozone. Am J Respir Crit Care Med 1996;154:1430–5. [DOI] [PubMed] [Google Scholar]
- [22].Mudway IS, Kelly FJ. An investigation of inhaled ozone dose and the magnitude of airway inflammation in healthy adults. Am J Respir Crit Care Med 2004;169:1089–95. [DOI] [PubMed] [Google Scholar]
- [23].Li G, Xue M, Zeng Q, et al. Association between fine ambient particulate matter and daily total mortality: an analysis from 160 communities of China. Sci Total Environ 2017;108:599–600. [DOI] [PubMed] [Google Scholar]
- [24].Renjie Chen, Haidong Kan, Bingheng Chen, et al. Association of particulate air pollution with daily mortality: the China Air Pollution and Health Effects Study. Am J Epidemiol 2012;175:1173–81. [DOI] [PubMed] [Google Scholar]
- [25].Yunginger JW, Reed CE, O’Connell EJ, et al. A community based study of the epidemiology of asthma. Incidence rates, 1964–1983. Am Rev Respir Dis 1992;146:888–94. [DOI] [PubMed] [Google Scholar]
- [26].Davis MC, Matthews KA, Twamley EW. Is life more difficult on Mars or Venus. A meta-analytic review of sex differences in major and minor life events. Ann Behav Med 1999;21:83–97. [DOI] [PubMed] [Google Scholar]
- [27].Seeman TE, Singer BH, Ryff CD, et al. Social relationships, gender, and allostatic load across two age cohorts. Psychosom Med 2002;64:395–406. [DOI] [PubMed] [Google Scholar]
- [28].Wen M, Kandula NR, Lauderdale DS. Walking for transportation or leisure: what difference does the neighborhood make. J Gen Intern Med 2007;22:1674–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Xu Q, Li X, Wang S, et al. Fine particulate air pollution and hospital emergency room visits for respiratory disease in urban areas in Beijing, China, in 2013. PLoS One 2016;11:e0153099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Qorbani M, Yunesian M, Fotouhi A, et al. Effect of air pollution on onset of acute coronary syndrome in susceptible subgroups. East Mediterr Health J 2012;18:550–5. [DOI] [PubMed] [Google Scholar]
- [31].Chen R, Huang W, Wong CM, et al. Short-term exposure to sulfur dioxide and daily mortality in 17 Chinese cities: the China air pollution and health effects study (CAPES). Environ Res 2012;118:101–6. [DOI] [PubMed] [Google Scholar]
- [32].Lu X, Lin C, Li W, et al. Analysis of the adverse health effects of PM2. 5 from 2001 to 2017 in China and the role of urbanization in aggravating the health burden. Sci Total Environ 2019;652:683–95. [DOI] [PubMed] [Google Scholar]
- [33].Guo Y, Jia Y, Pan X, et al. The association between fine particulate air pollution and hospital emergency room visits for cardiovascular diseases in Beijing, China. Sci Total Environ 2009;407:4826–30. [DOI] [PubMed] [Google Scholar]
- [34].Thurston GD, Kipen H, Annesi-Maesano I, et al. A joint ERS/ATS policy statement: what constitutes an adverse health effect of air pollution? An analytical framework. Eur Respir J 2017;49:1600419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Sun S, Tian L, Cao W, et al. Urban climate modified short-term association of air pollution with pneumonia mortality in Hong Kong. Sci Total Environ 2019;646:618–24. [DOI] [PubMed] [Google Scholar]
- [36].Dherani M, Pope D, Mascarenhas M, et al. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull World Health Organ 2008;86:390–8C. [DOI] [PMC free article] [PubMed] [Google Scholar]


