Abstract
Rationale:
Primary malignant melanoma of the esophagus (PMME) is a rare malignancy that only accounts for <2% of all primary esophageal tumors. Here, we report the even rarer occurrence of PMME in combination with poorly differentiated mucinous adenocarcinoma of the stomach.
Patient concerns:
A 64-year-old man was presented to the hospital with >1 month of eating dysphagia. Enhanced computed tomography (CT) scan only found a space-occupying lesion in the lower esophagus with moderate enhancement. However, gastroscope showed not only esophageal masses, but also gastric mucosa changes.
Diagnoses:
Poorly differentiated mucinous adenocarcinoma and PMME were diagnosed based on pathological biopsy and immunohistochemical methods.
Interventions:
The patient underwent laparoscopic gastric cancer radical surgery, esophageal resection, and colonic replacement of the esophagus.
Outcomes:
Abdominal CT and esophagography performed 1 week after surgery showed that it was consistent with postoperative changes without other abnormalities. However, the patient died 3 months after discharge without receiving any other treatment.
Lessons:
This case suggests more attention should be drawn to the diagnosis of multiple primary malignant neoplasms in elder patients, and also highlights the need to fulfill comprehensive examinations before surgery in case of misdiagnosis. Besides, it is challenging to finding a reasonable treatment for such rare condition.
Keywords: gastric mucinous adenocarcinoma, multiple primary malignant neoplasms, primary malignant melanoma of the esophagus
1. Introduction
Malignant melanoma occurs mostly in the skin and primary malignant melanoma of the esophagus (PMME) is very rare, accounting for approximately 0.1% to 0.2% of all esophageal tumors and 0.5% of all noncutaneous melanomas.[1,2] The average age of the patients with PMME is 60.5 years and the ratio of men to women is 2:1.[3] Along with the high aggressiveness of the disease, the median survival time of PMME is 13.4 months and 5-year overall survival rate is around 4%,[4,5] the rate may be improved to 37.5% after surgical resection according to a recent study.[6]
As the fourth most common malignancy and the second leading cause of cancer-related death worldwide,[7] gastric cancer is a serious problem to human health. Although both of the malignancies occur in digestive system, simultaneous occurrence of PMME and gastric adenocarcinoma has not been reported in China or elsewhere. Here, we report a case of PMME combined with poorly differentiated gastric mucinous adenocarcinoma and a review of the relevant literature. Our case suggests that comprehensive examinations before surgery are of vital importance to diagnosis and double primary malignancies indicate poor prognosis.
2. Case presentation
The patient was a nonsmoking 64-year-old man who had been admitted to a primary care unit because of >1 month of eating dysphagia. Gastroscopy showed a black protuberant lesion and chronic erosive gastritis. The patient then went to our hospital for further diagnosis and treatment. Pulmonary contrast-enhanced computed tomography (CT) showed a space-occupying lesion in the lower esophagus with moderate enhancement (Fig. 1). No other tumor or lymph node involvement was seen based on total body CT scan. Gastroscopy showed 2 black masses in the esophagus located at 22 to 24 cm and 30 to 35 cm, respectively, from the incisors that led to esophageal narrowing (Fig. 2A). Moreover, a 2.0 cm ulcer was observed in the posterior wall of the lower part of the stomach, and the surrounding mucosa showed nodular changes (Fig. 2B). Endoscopic ultrasonography detected abundant blood flow signals at the lesions of esophagus (Fig. 2C). Endoscopic biopsy was not performed in case of bleeding. The pathological findings for the gastric body revealed poorly differentiated mucinous adenocarcinoma. The clinical diagnosis was firstly made as poorly differentiated stomach adenocarcinoma and esophageal tumor. After discussion by a multidisciplinary treatment group including departments of thoracic and gastrointestinal surgery, the patient underwent laparoscopic gastric cancer radical surgery, esophageal resection, and colonic replacement of the esophagus under general anesthesia.
Figure 1.
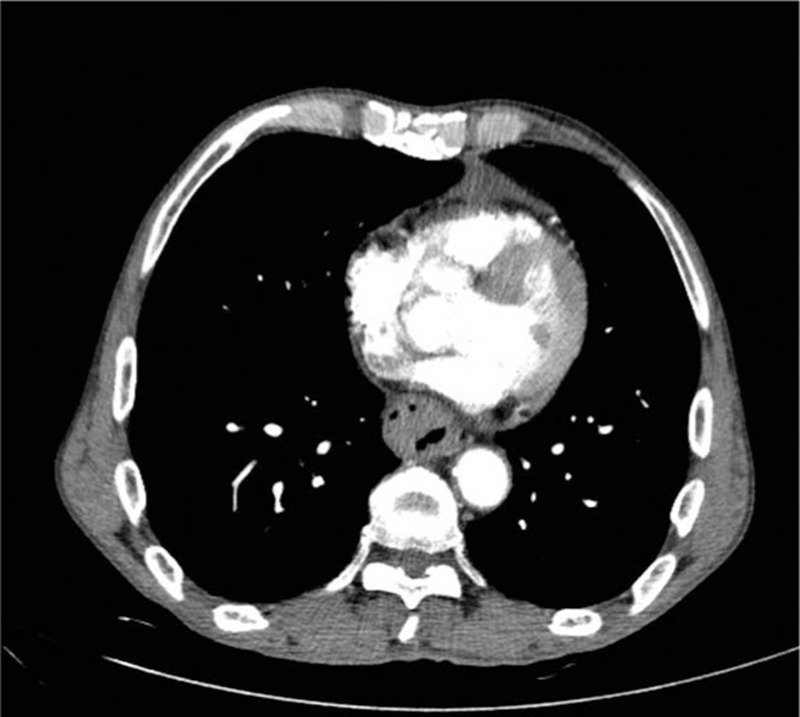
Enhanced CT showed a lesion of 8.7 cm long in the lower esophagus with moderate enhancement. CT = computed tomography.
Figure 2.

Gastroscopy and ultrasonography of esophagus and stomach. (A) Gastroscopy showed a black tumor that led to esophageal narrowing. It was located within the esophagus, 22 cm from the incisors. (B) Gastroscopy showed a 2.0 cm ulcer observed in the posterior wall of the lower part of the stomach, and the surrounding mucosa with nodular changes. (C) Endoscopic ultrasonography detected abundant blood flow signals at the lesion. Adjacent to the lesions, similar black satellite lesions could be seen.
Macroscopically, the esophageal tumors were scattered distributed, the biggest tumor was 7.5 × 3.0 × 0.8 cm in dimension. The cut surface was reddish brown, solid, and tough. Scattered black nodules (the diameter was around 0.2–1.0 cm; Fig. 3A) were observed in the surface of the esophageal mucosa. The gastric body near the lesser curvature showed a 2.0 × 1.5 × 0.4 cm anabrosis, and the cut surface was light brown, solid, and tough (Fig. 3B). Microscopic examination of the gastric body showed poorly differentiated mucinous adenocarcinoma; signet ring cells could also be seen. Superficial muscularis propria was invaded, but metastasis of lymph node was not observed (Fig. 4A). Malignant melanoma infiltration was seen in the esophagus and submucosa was invaded with no lymph node involved (Fig. 4B). Both were primary malignant tumors. Immunohistochemistry staining of the stomach showed CK-pan (+), Ki-67 (+50%), P53 (+<5%), and Her-2 (+) (Fig. 5A), as well as S-100 (±) for the lymph nodes. Immunohistochemistry staining of the esophagus demonstrated Ki-67 (+40%), Melan-A (+) (Fig. 5B), HMB45 (+) (Fig. 5C), CD117 (+), S-100 (+) (Fig. 5D), CK-pan (-), CK5/6 (−), P63 (−), Vimentin (−), and Dog-1 (−). The patient was diagnosed with esophageal malignant melanoma and poorly differentiated gastric mucinous adenocarcinoma. The stage of gastric adenocarcinoma was classified as IB (pT2N0M0), according to the American Joint Commission on Cancer (AJCC) Cancer Staging Manual (8th Edition). The stage of PMME is uncertain because there is no standard staging for PMME as far as we know, and using TNM stage of esophageal cancer or cutaneous melanoma is not accurate in such case. One week after surgery, results of abdominal CT and esophagography were consistent with postoperative changes without any other abnormalities. Two weeks after surgery, chest drainage, mediastinal drainage, and gastric tube were removed, and the patient could start to eat a small amount of liquid food. The patient was discharged with good condition 3 weeks after surgery. Neither radiotherapy nor chemotherapy was performed after surgery, and the patient died after 3 months of follow-up. The patient and his family provided informed consent for this case report. On the contrary, our case does not need ethical approval from ethics committee or institutional review board.
Figure 3.
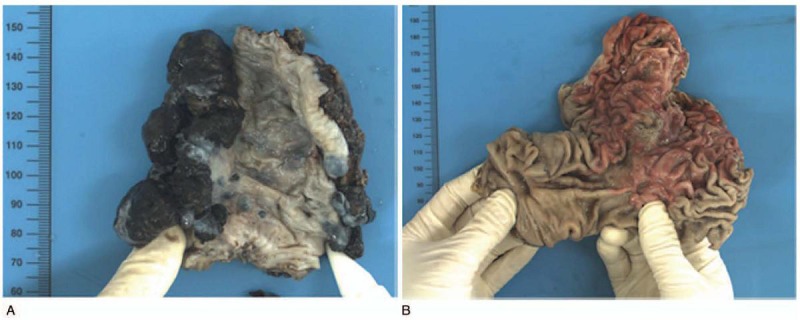
A macroscopic view of the cut-end surfaces of the resected specimens. (A) The surgical specimen showed a cauliflower-like bulge (7.5 × 3.0 × 0.8 cm in dimension) on the surface of esophagus, which was reddish brown, solid, and tough. In the mucosa of the esophageal, we observed scattered black brown nodules. (B) The gastric body near the lesser curvature showed an anabrosis (2.0 × 1.5 × 0.4 cm in dimension), and the section was light brown, solid, and tough.
Figure 4.
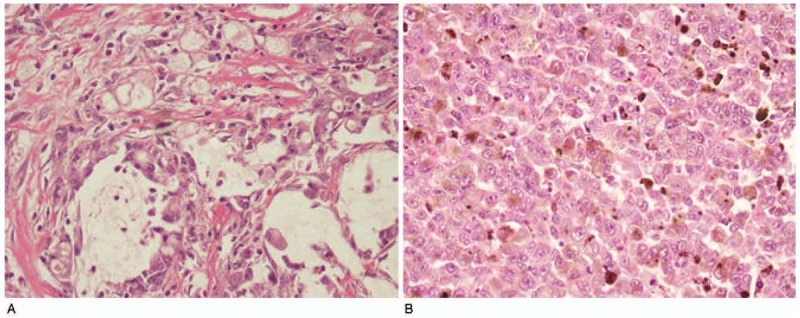
HE of GC and PMME. (A) The pathology results of the gastric body showed poorly differentiated adenocarcinoma, parts of mucinous adenocarcinoma, and signet ring cells. (B) The esophageal tissues were inflitrated by malignant melanoma (magnification: 200×). HE = hematoxylin–eosin, GC = gastric cancer, PMME = malignant melanoma of the esophagus. PMME = primary malignant melanoma of the esophagus.
Figure 5.
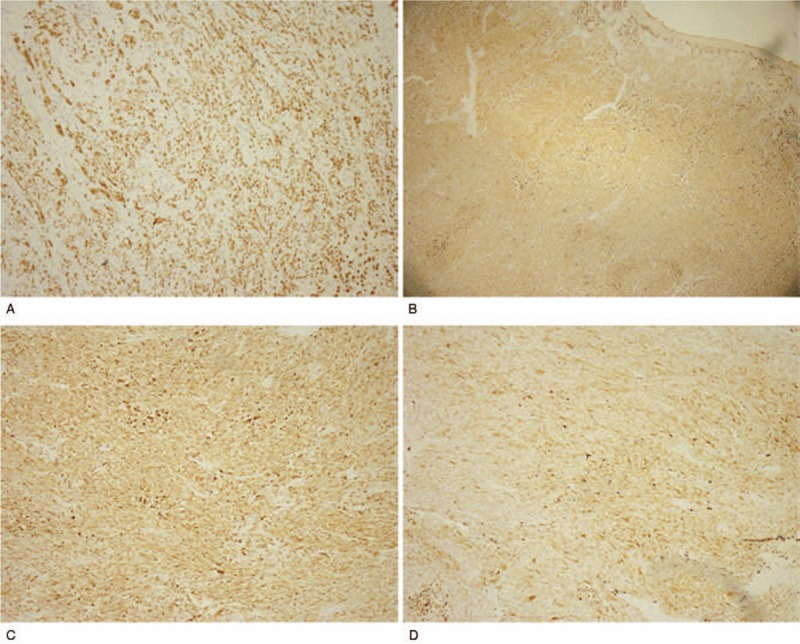
IHC staining of GC and PMME. (A) Positive staining of Her-2 in GC (magnification: 100×). (B) Positive staining of Melan-A (+) (magnification: 40×), (C) HMB-45 (magnification: 100×), and (D) S-100 (+) (magnification: 100×) in PMME. IHC = immunohistochemistry, GC = gastric cancer, PMME = malignant melanoma of the esophagus. PMME = primary malignant melanoma of the esophagus.
3. Discussion
Melanoma is a highly aggressive malignancy that mainly occurs at skin. As a noncutaneous melanoma, PMME has been occasionally reported since 1906.[2] To date, about 337 cases of esophageal melanoma have been published,[4,8] whereas copresentation with gastric cancer has not been reported.
Little has been discussed about the etiology of PMME. Over 80% of the PMME located in the lower and middle thirds of the esophagus because a large number of melanocytes gathered in the location,[2] which was consistent with our observation in this case. It has been indicated that the esophageal melanocytosis is a precancerous lesion of PMME,[9,10] and esophageal melanocytic dysplasia will eventually develop into PMME.[8,11]
The diagnosis of esophageal melanoma is often difficult because it mainly depends on clinical manifestations, endoscopy, and pathology. The clinical manifestations of PMME are not significantly different from other tumors of the esophagus. The most common symptoms is progressive dysphagia[5] as well as, in our case, other symptoms include antiacid, heartburn, retrosternal pain, hematemesis, black stool, and weight loss, whereas a few patients are asymptomatic at diagnosis.[3,12–14] The shape of the tumor can be polypoid, nodular, beaded, or cauliflower-like. In 85% of cases, the lesions had pale, brown, blue, black, or dark-brown pigmentation.[15] Gastroscopy always showed that the lesions were accompanied by ulceration or satellite nodules, which were fragile and easily bled. These were all in consistency with our findings. Although the accuracy rate of diagnosis by biopsy is approximately 80%,[16] we did not perform biopsy in our case because endoscopic ultrasonography showed abundant blood flow signals and biopsy might lead to bleeding. Besides, sometimes the tumors are amelanotic with no melanin granules, concentrated in foci or covered by normal squamous epithelium, which might influence the accuracy of endoscopic biopsy and lead to misdiagnosis.[2,5,17] If histological diagnosis is uncertain, immune-related markers such as S-100 protein, HMB-45, and Melan-A should be performed to improve the accuracy of the diagnosis[3,18] owing to the high sensitivity of S-100 and high specificity of HMB-45 and Melan-A in melanomas.[4] The pathological results in our case confirmed our diagnosis.
There is no standard strategy for the treatment of PMME. The studies on the effects of radiotherapy, chemotherapy, and immunotherapy were inconsistent; some cases reported survival benefits[19–23]; and others did not reach the same conclusion.[2,5,24] Currently, the main treatment for PMME is surgical excision.[3] Radical resection is also the main treatment for early poorly differentiated stomach adenocarcinoma. Although 2 malignant tumors were treated by surgical resection in our case, the patient died 3 months after surgery. The most important prognostic factor noted in the literature is lymph node metastasis,[25] which correlates with worse prognosis.[26] However, based on our experience with this case, lymph node metastasis is not a decisive factor in prognosis, the double malignancy may have significantly reduced the survival time.
In conclusion, the cooccurrence of poorly differentiated gastric adenocarcinoma greatly worsens the prognosis and reduces survival time. Comprehensive examinations should be performed to make the accurate diagnosis. Endoscopic ultrasonography might be useful to diagnose PMME and avoid unnecessary bleeding. The clinical features, endoscopic examinations, and pathological diagnosis of this case may provide important clinical guidance for clinicians developing individualized treatment plans for specific patients.
Acknowledgments
We thank Editage (www.editage.cn) for English language editing.
Author contributions
XWM and XS designed the study; JL was the major contributor in writing the manuscript; XS performed the histological examination and immunohistochemistry; BW and YL collected the patient data. All authors read and approved the final manuscript.
Methodology: Bin Wang, Xun Sun.
Resources: Yan Liu.
Writing – original draft: Ji Li.
Writing – review & editing: Xun Sun, Xiangwei Meng.
Footnotes
Abbreviations: CT = computed tomography, GC = gastric cancer, HE = hematoxylin–eosin, IHC = immunohistochemistry, PMME = primary malignant melanoma of the esophagus.
XM and XS equally contributed to this work.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Volpin E, Sauvanet A, Couvelard A, et al. Primary malignant melanoma of the esophagus: a case report and review of the literature. Dis Esophagu 2002;15:244–9. [DOI] [PubMed] [Google Scholar]
- [2].Sun H, Gong L, Zhao G, et al. Clinicopathological characteristics, staging classification, and survival outcomes of primary malignant melanoma of the esophagus. J Surg Oncol 2018;117:588–96. [DOI] [PubMed] [Google Scholar]
- [3].Liu H, Yan Y, Jiang CM. Primary malignant melanoma of the esophagus with unusual endoscopic findings: a case report and literature review. Medicine (Baltimore) 2016;95:e3479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bisceglia M, Perri F, Tucci A, et al. Primary malignant melanoma of the esophagus: a clinicopathologic study of a case with comprehensive literature review. Adv Anat Pathol 2011;18:235–52. [DOI] [PubMed] [Google Scholar]
- [5].Sabanathan S, Eng J, Pradhan GN. Primary malignant melanoma of the esophagus. Am J Gastroenterol 1989;84:1475–81. [PubMed] [Google Scholar]
- [6].Yu H, Huang XY, Li Y, et al. Primary malignant melanoma of the esophagus: a study of clinical features, pathology, management and prognosis. Dis Esophagus 2011;24:109–13. [DOI] [PubMed] [Google Scholar]
- [7].Van Cutsem E, Sagaert X, Topal B, et al. Gastric cancer. Lancet 2016;388:2654–64. [DOI] [PubMed] [Google Scholar]
- [8].Pun AH, Devitt PG. Primary malignant melanoma of the oesophagus: two case reports. J Surg Case Rep 2014;2014:rju005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].DiCostanzo DP, Urmacher C. Primary malignant melanoma of the esophagus. Am J Surg Pathol 1987;11:46–52. [DOI] [PubMed] [Google Scholar]
- [10].Morita FH, Ribeiro U, Jr, Sallum RA, et al. Primary malignant melanoma of the esophagus: a rare and aggressive disease. World J Surg Oncol 2013;11:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sanchez AA, Wu T, Prieto VG, et al. Comparison of primary and metastatic malignant melanoma of the esophagus: clinicopathologic review of 10 cases. Arch Pathol Lab Med 2008;132:1623–9. [DOI] [PubMed] [Google Scholar]
- [12].Izumi D, Ishimoto T, Yoshida N, et al. A clinicopathological analysis of primary mucosal malignant melanoma. Surg Today 2015;45:886–91. [DOI] [PubMed] [Google Scholar]
- [13].Imamura K, Adachi K, Enatsu K. Primary gastrointestinal malignant melanoma. Clin Gastroenterol Hepatol 2016;14:e5–6. [DOI] [PubMed] [Google Scholar]
- [14].Kobayashi J, Fujimoto D, Murakami M, et al. A report of amelanotic malignant melanoma of the esophagus diagnosed appropriately with novel markers: a case report. Oncol Lett 2018;15:9087–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Rawandale NA, Suryawanshi KH. Primary spindle cell malignant melanoma of esophagus: an unusual finding. J Clin Diagn Res 2016;10:OD03–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Kuwabara S, Ebihara Y, Nakanishi Y, et al. Primary malignant melanoma of the esophagus treated with subtotal esophagectomy: a case report. BMC Surg 2017;17:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Imai S, Suzuki A, Yamamoto Y, et al. Primary malignant melanoma of esophagus following chemoradiotherapy for esophageal squamous cell carcinoma: report of a case. Clin J Gastroenterol 2017;10:336–41. [DOI] [PubMed] [Google Scholar]
- [18].Gao S, Li J, Feng X, et al. Characteristics and surgical outcomes for primary malignant melanoma of the esophagus. Sci Rep 2016;6:23804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Asakage M, Kitayama J, Tsuno NH, et al. Primary malignant melanoma of the esophagus treated by esophagectomy and adjuvant dendritic-cell therapy. J Gastroenterol 2005;40:545–6. [DOI] [PubMed] [Google Scholar]
- [20].Ueda Y, Shimizu K, Itoh T, et al. Induction of peptide-specific immune response in patients with primary malignant melanoma of the esophagus after immunotherapy using dendritic cells pulsed with MAGE peptides. Jpn J Clin Oncol 2007;37:140–5. [DOI] [PubMed] [Google Scholar]
- [21].Naomoto Y, Perdomo JA, Kamikawa Y, et al. Primary malignant melanoma of the esophagus: report of a case successfully treated with pre- and post-operative adjuvant hormone-chemotherapy. Jpn J Clin Oncol 1998;28:758–61. [DOI] [PubMed] [Google Scholar]
- [22].Uetsuka H, Naomoto Y, Fujiwara T, et al. Primary malignant melanoma of the esophagus: long-term survival following pre- and postoperative adjuvant hormone/chemotherapy. Dig Dis Sci 2004;49:1646–51. [DOI] [PubMed] [Google Scholar]
- [23].Sasaki K, Uchikado Y, Omoto I, et al. Multidisciplinary therapy for metastatic primary malignant melanoma of the esophagus: a case report. Mol Clin Oncol 2018;8:533–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Rochefort P, Roussel J, de la Fouchardière A, et al. Primary malignant melanoma of the esophagus, treated with immunotherapy: a case report. Immunotherapy 2018;10:831–5. [DOI] [PubMed] [Google Scholar]
- [25].Wang S, Tachimori Y, Hokamura N, et al. Diagnosis and surgical outcomes for primary malignant melanoma of the esophagus: a single-center experience. Ann Thorac Surg 2013;96:1002–6. [DOI] [PubMed] [Google Scholar]
- [26].Harada K, Mine S, Yamada K, et al. Long-term outcome of esophagectomy for primary malignant melanoma of the esophagus: a single-institute retrospective analysis. Dis Esophagus 2016;29:314–9. [DOI] [PubMed] [Google Scholar]


