Abstract
Background:
Previous studies have reported that acupuncture combined Bobath approach (BA) can be used to treat limbs paralysis (LP) after hypertensive intracerebral hemorrhage (HICH) effectively. However, no systematic review has explored its effectiveness and safety for LP following HICH. In this systematic review, we aim to assess the effectiveness and safety of acupuncture plus BA for the treatment of LP following HICH.
Methods:
The following 7 databases will be searched from their inception to the February 1, 2019: Cochrane Central Register of Controlled Trials, EMBASE, PUBMED, the Cumulative Index to Nursing and Allied Health Literature, the Allied and Complementary Medicine Database, Chinese Biomedical Literature Database, and China National Knowledge Infrastructure without any language restrictions. The randomized controlled trials (RCTs) of acupuncture plus BA that evaluate the effectiveness and safety for LP after HICH will be included. The methodological quality of all included studies will be assessed by using Cochrane risk of bias tool. Two authors will independently perform study selection, data extraction, and methodological quality evaluation. Any disagreements occurred between 2 authors will be resolved by a third author involved through discussion. Data will be pooled and analyzed by using RevMan 5.3 Software.
Results:
This review will evaluate the effectiveness and safety of acupuncture combined BA for LP following HICH. The primary outcome is limbs function. The secondary outcomes are muscle strength, muscle tone, and quality of life, as well as the adverse events.
Conclusion:
The results of this study will summarize the latest evidence of acupuncture combined BA for LP following HICH.
Keywords: acupuncture, Bobath approach, effectiveness, hypertension, intracerebral hemorrhage, limbs paralysis, safety, systematic review
1. Introduction
Hypertensive intracerebral hemorrhage (HICH) is a devastating and costly disorder, which often accompanies high mortality and morbidity.[1–4] Many factors are reported to account for this condition, such as hypertension, current smoking, excessive alcohol consumption, hypocholesterolemia, and any other factors, especially for the hypertension.[5–8] It has been reported that HICH account for 10% to 20% of all strokes.[9,10] Moreover, its incidence still increases with advanced age.[11] Patients experience such disorder often manifest with headache, nausea, and vomiting initially, then followed by the limbs paralysis (LP), decreased consciousness, difficulty speaking, or sensitivity deficits and so on.[12,13] Of these, LP is one of the trickiest conditions, and greatly affects the quality of life in patients with such disorder.[14–16]
Acupuncture and Bobath approach (BA) are both reported to widely treat LP after HICH, and also have achieved very satisfied outcome results.[17–23] However, no systematic review has evaluated its effectiveness and safety with higher level evidence. Thus, it is very necessary to conduct a systematic review and meta-analysis to assess the effectiveness and safety of acupuncture combined with BA for the treatment of LP following HICH.
2. Methods and analysis
2.1. Eligibility criteria
2.1.1. Participants/population
Patients with LP after HICH, regarding sex, age, and race will be considered for inclusion. However, if LP is diagnosed before the HICH, or caused by other disorders will not be included.
2.1.2. Interventions/exposure
Any types of acupuncture combined with BA alone will be utilized to treat LP in the experimental group. The treatments in the control group can be any kinds of interventions, except the acupuncture, BA or combination of both.
2.1.3. Study types
We will include randomized controlled trials (RCTs) of acupuncture combined with BA for the treatment of HICH without any restrictions. Studies will be excluded if they are nonclinical trials, case studies, crossover studies, non-RCTs, and quasi-RCTs.
2.1.4. Outcome measurements
The primary outcome includes limbs function, as measured by the Fugl-Meyer Assessment scale, or other associated scales. The secondary outcomes include muscle strength, as assessed by the motricity index or other related scored tools; muscle tone, as evaluated by modified Ashworth scale, or other relevant scales; and quality of life, as examined by activities of daily living scale or any other specific scales. In addition, adverse events are also assessed.
2.2. Literature search
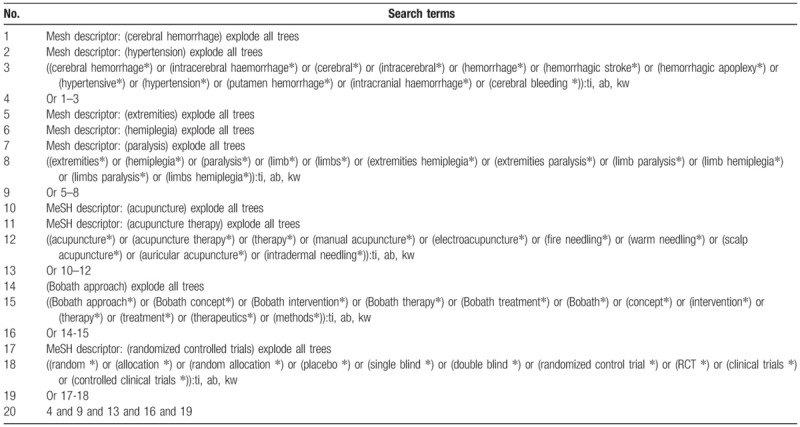
We will search the following 7 databases from their inception to the February 1, 2019: Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, PUBMED, the Cumulative Index to Nursing and Allied Health Literature, the Allied and Complementary Medicine Database, Chinese Biomedical Literature Database, and China National Knowledge Infrastructure without any language restrictions. The studies of RCTs regarding the effectiveness and safety of acupuncture plus BA for LP after HICH will be included. The detailed strategy of CENTRAL is presented in Table 1. The equivalent search strategies will be applied to other databases.
Table 1.
Search strategy applied in CENTRAL database.
The secondary data sources include Google scholar, website of clinical registrations, reference lists of all relevant reviews and included studies, as wells as the conference proceedings.
2.3. Data selection
The NoteExpress 3.2.0 will be used for study selection. Two authors will independently scrutinize the titles or abstracts initially, and then full texts will be read for eligible trials based on the predefined eligibility criteria. All study selection procedures will present in flowchart and will follow the Preferred Reporting Items for Systematic review and Meta-Analysis Flow Chart. The flowchart will include exact reason of inclusion or exclusion for each study at each stage. Any disagreements about the study selection will be settled down through discussion with a third author.
2.4. Data extraction and management
Two authors will extract following information from each included study and will save all the data in a data extraction sheet: general information (first author, published year, region, age, sex, ethnicity, disease types); relevant study methods (sample size, randomization, allocation, and blinding); interventions methods (details of interventions, including dosage, frequency, treatment duration); and outcome measurements (primary and secondary outcomes, adverse events, and any others). Any divergences between 2 authors will be resolved by a consensus or arbitration with a third author.
2.5. Dealing with missing data
The primary authors will be contacted to acquiring the insufficient or missing data if any of them arise. If we are not able to obtain those data, we will just analyze the available data, and also will discuss its potential impact in the discussion section.
2.6. Risk of bias assessment
Two independent authors will assess the methodology quality for each included study by using Cochrane risk of bias tool. This tool comprises 7 domains, and each one will classify into 3 levels: low, unclear, and high risk of bias. A third author will be invited to tackle the oppositions between 2 authors.
2.7. Reporting bias
We will also plan to conduct funnel plot and Egg's regression to detect the reporting bias if >10 eligible studies are included.
2.8. Statistical analysis
The statistical analysis will be carried out by using RevMan 5.3 software. Continuous data will be synthesized and shown as mean difference or standardized mean difference with 95% confidence intervals (CIs), while the dichotomous data will be synthesized and presented as risk ratio with 95% CIs.
Heterogeneity among included studies will be identified by using I2 test. I2 ≤50% is regarded as having fair heterogeneity, and fixed-effect model will be used to pool the data. Otherwise, heterogeneity is considered as mild or significant and random-effect model will be applied to pool the data. Meanwhile, subgroup analysis is suggested to be performed according to the different types of treatments, control interventions, and outcome measurements. If the heterogeneity remains substantial after subgroup analysis, then data will not be pooled, and a narrative summary will be presented instead. Sensitivity analysis will be carried out to ensure the robustness of pooled results by removing low quality studies.
3. Discussion
This systematic review will be conducted to evaluate the effectiveness and safety of acupuncture combined with BA for the treatment of LP in patients with HICH. To our best knowledge, no previous systematic review has addressed this issue. Thus, this systematic review will first assess the effectiveness and safety of acupuncture plus BA for treating LP following HICH.
In this systematic review, we will search as comprehensive data sources as possible without any language restrictions. All potential studies regarding the acupuncture plus BA for the treatment of HICH will be fully considered. The results of this systematic review may provide an up-to-date summary of the current evidence on the effectiveness and safety of acupuncture plus BA for LP following HICH.
Author contributions
Conceptualization: Guang-fu Song, Yao Feng, Chang-hong Yu.
Data curation: Guang-fu Song, Xin Li, Xiao-yu Lian.
Formal analysis: Guang-fu Song, Xin Li, Yao Feng, Chang-hong Yu.
Funding acquisition: Guang-fu Song.
Investigation: Xiao-yu Lian.
Methodology: Guang-fu Song, Xin Li, Yao Feng, Chang-hong Yu.
Project administration: Xiao-yu Lian.
Resources: Guang-fu Song, Xin Li, Yao Feng, Chang-hong Yu, Xiao-yu Lian.
Software: Guang-fu Song, Xin Li, Yao Feng.
Supervision: Xiao-yu Lian.
Validation: Xin Li, Yao Feng, Chang-hong Yu, Xiao-yu Lian.
Visualization: Xin Li, Chang-hong Yu.
Writing – original draft: Guang-fu Song, Xin Li, Xiao-yu Lian.
Writing – review and editing: Guang-fu Song, Xin Li, Yao Feng, Chang-hong Yu, Xiao-yu Lian.
Footnotes
Abbreviations: BA = Bobath approach, CENTRAL = Cochrane Central Register of Controlled Trials, CIs = confidence intervals, HICH = hypertensive intracerebral hemorrhage, LP = limbs paralysis, RCTs = randomized controlled trials.
Dissemination and ethics: The findings of this systematic review will be published in peer-reviewed journals. This systematic review dose not needs ethic approval because it just analyzes the published data without individual information involvement.
Systematic review registration: PROSPERO CRD42019120838.
G-fS and XL equally contributed to this work.
This work has been supported by the Jiamusi University Foundation Research Project (No. JMSUJCMS2016-027). The financial supporter will not participate any parts of this study.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Weimar C, Kleine-Borgmann J. Epidemiology, prognosis and prevention of non-traumatic intracerebral hemorrhage. Curr Pharm Des 2017;23:2193–6. [DOI] [PubMed] [Google Scholar]
- [2].An SJ, Kim TJ, Yoon BW. Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update. J Stroke 2017;19:3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Alerhand S, Lay C. Spontaneous intracerebral hemorrhage. Emerg Med Clin North Am 2017;35:825–45. [DOI] [PubMed] [Google Scholar]
- [4].Lei C, Geng J, Chen C, et al. Accuracy of the blend sign on computed tomography as a predictor of hematoma growth after spontaneous intracerebral hemorrhage: a systematic review. J Stroke Cerebrovasc Dis 2018;27:1705–10. [DOI] [PubMed] [Google Scholar]
- [5].Wang HC, Lin WC, Yang TM, et al. Risk factors for acute symptomatic cerebral infarctions after spontaneous supratentorial intra-cerebral hemorrhage. J Neurol 2009;256:1281–7. [DOI] [PubMed] [Google Scholar]
- [6].Celikbilek A, Goksel BK, Zararsiz G, et al. Spontaneous intra-cerebral hemorrhage: a retrospective study of risk factors and outcome in a Turkish population. J Neurosci Rural Pract 2013;4:271–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chang L, Dong Y, Zhou P. Investigation on risk factors of ventilator-associated pneumonia in acute cerebral hemorrhage patients in intensive care unit. Can Respir J 2017;2017:7272080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zhou HX, Hao N, Xu XL. Related factors of early mortality in young adults with cerebral hemorrhage. Open Med (Wars) 2018;13:214–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Feigin VL, Lawes CM, Bennett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009;8:355–69. [DOI] [PubMed] [Google Scholar]
- [10].Sacco S, Marini C, Toni D, et al. Incidence and 10-year survival of intracerebral hemorrhage in a population-based registry. Stroke 2009;40:394–9. [DOI] [PubMed] [Google Scholar]
- [11].Broderick JP, Brott T, Tomsick T, et al. Intracerebral hemorrhage more than twice as common as subarachnoid hemorrhage. Neurosurg 1993;78:188–91. [DOI] [PubMed] [Google Scholar]
- [12].Zheng J, Yu Z, Ma L, et al. Association between blood glucose and functional outcome in intracerebral hemorrhage: a systematic review and meta-analysis. World Neurosurg 2018;114:e756–65. [DOI] [PubMed] [Google Scholar]
- [13].Burns JD, Fisher JL, Cervantes-Arslanian AM. Recent advances in the acute management of intracerebral hemorrhage. Neurosurg Clin N Am 2018;29:263–72. [DOI] [PubMed] [Google Scholar]
- [14].Jang SH, Yeo SS. Recovery of an injured corticoreticular pathway via transcallosal fibers in a patient with intracerebral hemorrhage. BMC Neurol 2014;14:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Yeo SS, Jang SH. Recovery of an injured corticospinal tract and an injured corticoreticular pathway in a patient with intracerebral hemorrhage. NeuroRehabilitation 2013;32:305–9. [DOI] [PubMed] [Google Scholar]
- [16].Cho SH, Kim SH, Choi BY, et al. Motor outcome according to diffusion tensor tractography findings in the early stage of intracerebral hemorrhage. Neurosci Lett 2007;421:142–6. [DOI] [PubMed] [Google Scholar]
- [17].Qi L, Han Z, Zhou Y, et al. Dynamic scalp acupuncture combined with PNF therapy for upper limb motor impairment in ischemic stroke spastic hemiplegia. Zhongguo Zhen Jiu 2018;38:234–8. [DOI] [PubMed] [Google Scholar]
- [18].Sun R, Tian L, Fang X, et al. Clinical study of post-stroke upper limb spasmodic hemiplegia treated with jingou diaoyu needling technique and Bobath therapy. Zhongguo Zhen Jiu 2017;37:372–6. [DOI] [PubMed] [Google Scholar]
- [19].Zhang Y, Ma TM, Bai ZH, et al. Meta-analysis on the therapeutic effect of acupuncture at meridian sinew for spastic paralysis after stroke. Zhen Ci Yan Jiu 2017;42:178–82. [PubMed] [Google Scholar]
- [20].Liu J, Chen L, Zhou J, et al. Efficacy on the range of motion of the lower limbs in patients of post-stroke spasmodic paralysis regulated with multi-directional stimulation technique. Zhongguo Zhen Jiu 2016;36:1013–7. [DOI] [PubMed] [Google Scholar]
- [21].Wang N, Li ZF, Wu HH. Clinical observation on therapeutic effect of red-hot needle therapy for spastic hemiplegia in stroke patients. Zhen Ci Yan Jiu 2015;40:304–8. [PubMed] [Google Scholar]
- [22].Shi G, Zheng X, Song N. Acupuncture at tendons node combined with movement for 30 cases of post-stroke spastic paralysis in lower limbs. Zhongguo Zhen Jiu 2015;35:212. [PubMed] [Google Scholar]
- [23].Zhang S, Wu B, Liu M, et al. all Investigators. Acupuncture efficacy on ischemic stroke recovery: multicenter randomized controlled trial in China. Stroke 2015;46:1301–6. [DOI] [PubMed] [Google Scholar]


