Abstract
This study compared post-operative complications and survival in horses with right dorsal displacement of the large colon (RDD) and horses with other non-strangulating large colon (NSLC) lesions. Data were obtained from medical records of horses undergoing exploratory laparotomy from 2000 to 2016 and from owner questionnaire. Of 137 horses that fitted the inclusion criteria, 67 (49%) had RDD and 70 (51%) had NSLC lesions. Twenty-eight horses with RDD (42%) and 27 horses with NSLC (39%) experienced ≥ 1 complication after surgery. The RDD group showed more severe complications than the NSLC group (P = 0.0145). Horses with RDD were more likely to develop colic in the short term (P = 0.0111), but not in the long-term (P = 0.453), and were more likely to have a 2nd laparotomy (P = 0.0003). There was no significant difference in short- or long-term survival between groups. Major post-operative complications in the RDD group did not influence short- or long-term survival.
Résumé
Complications et survie des chevaux atteints d’un déplacement dorsal droit du gros côlon confirmé par chirurgie. Cette étude a comparé les complications et la survie postopératoires chez les chevaux atteints d’un déplacement dorsal droit du gros côlon (DDD) et les chevaux atteints d’autres lésions non étranglantes du gros côlon (LNEGC). Des données ont été obtenues dans les dossiers médicaux de chevaux qui avaient subi une laparatomie exploratoire entre 2000 et 2016 et dans un questionnaire auprès des propriétaires. Parmi les 137 chevaux qui satisfaisaient aux critères d’inclusion, 67 (49 %) avaient eu un DDD et 70 (51 %) avaient eu des lésions LNEGC. Vingt-huit chevaux atteints d’un DDD (42 %) et 27 chevaux qui avaient une LNEGC (39 %) ont éprouvé ≥ 1 complication après la chirurgie. Le groupe DDD a manifesté des complications plus graves que le groupe LNEGC (P = 0,0145). Il était plus probable que les chevaux atteints de DDD développent des coliques à court terme (P = 0,0111), mais pas à long terme (P = 0,453) et il était plus probable qu’ils aient à subir une deuxième laparotomie (P = 0,0003). Il n’y avait aucune différence significative au niveau de la survie à court ou à long terme entre les groupes. Les complications postopératoires majeures du groupe DDD n’ont pas influencé la survie à court ou à long terme.
(Traduit par Isabelle Vallières)
Introduction
The large colon is a highly mobile part of the equine gastrointestinal tract and due to its limited attachments to the body wall, it can become abnormally positioned in various orientations (1–3). Four main types of non-strangulating displacements of the large colon are described: left dorsal displacement (nephrosplenic or renosplenic entrapment), right dorsal displacement, retroflexion of the pelvic flexure, and non-strangulating volvulus of the large colon (1–3). A displacement is non-strangulating if the bowel has moved sufficiently out of its normal orientation that functional obstruction (either complete or partial) of the lumen exists, without compromising vascular integrity (2). Strangulating obstruction of the large colon is colon rotation > 270° (1,4). The large colon may adopt a location intermediate to these 4 most commonly described orientations, and the displacement can sometimes be difficult to describe (3).
Right dorsal displacement of the large colon (RDD) was first defined by Huskamp and Kopf (5) as a non-strangulating torsion of the large colon (5,6). Right dorsal displacement is thought to be initiated by retropulsive movement of the pelvic flexure with subsequent migration of the left colon cranially and progressing towards the right abdominal side until the right ventral and dorsal colon are between the cecum and right body wall (3). The pathogenesis of large colon displacement is thought to involve alteration of gastrointestinal motility, which is initiated at the pelvic flexure pacemaker cells such that longitudinal shortening of the left large colon and movement of the pelvic flexure towards the diaphragm occur (3). Other possible causes include excess ingestion of soluble carbohydrates that lead to excessive fermentation, gas distension and large colon migration (3,7), and/or changes in fecal microbiota, which can alter colonic motility (8). It is possible that several of these theories are correct. As is the case for most horses presenting with colic, the cause of large colon displacement is often unknown.
A previous study reported that a population of horses in the UK with RDD had an increased risk of colic after surgery (2). Anectodally, a similar observation has been noted in the population of horses surgically diagnosed with RDD in our hospital. The aims of this study were to document short- and long-term survival rates and post-operative complications in horses with surgically confirmed RDD and compare the results to those for horses with other non-strangulating large colon lesions (NSLC). We hypothesized that horses with RDD would have a good prognosis for short- and long-term survival and that post-operative complications in those cases would be different compared with horses with other NSLC lesions.
Materials and methods
Study design and data collection
Medical records of all horses undergoing exploratory laparotomy at the University of Wisconsin-Madison, Veterinary Medical Teaching Hospital from 2000 to 2016 were reviewed. Horses with a surgical diagnosis of right dorsal displacement of the large colon were compared with horses that had other surgically diagnosed non-strangulating lesions of the large colon. All surgery reports were reviewed and only cases which declared the bowel free from significant vascular compromise were included in this study. Vascular compromise was based upon edema of the colon wall, serosal color, mucosal color, and active bleeding at the enterotomy site. Information obtained from patients’ records included: patient signalment, surgical diagnosis, major or minor post-operative complications, and hospitalization time (short-term survival). Complications were evaluated within the post-operative period, which was defined as the time from recovery from general anesthesia to discharge from hospital. A major complication was defined as an adverse problem that required surgical revision, major alteration of the colic after-care treatment plan, or resulted in a poor outcome such as death. Major complications included peritonitis, laminitis, post-operative reflux, or relaparotomy. Minor complications included diarrhea, surgical site infection, thrombophlebitis, or medical colic. Gastrointestinal specific complications were also evaluated and compared between the 2 groups.
Follow-up information was obtained by telephone conversation with the owner. Questions included the current status of the patient (dead, alive, or lost to follow-up), whether or not the horse returned to original function, post-operative complications experienced at home such as colic, and whether or not they had a relaparotomy following hospital discharge. When available, diagnosis at the second laparotomy was recorded. Five attempts were made to complete the standardized questionnaire by telephone. After this time, if the client was unable to be contacted, an e-mail, and/or written letter explaining the study was forwarded to the owner with the attached questionnaire for completion. If correspondence was then not received after 2 mo, the case was considered lost to follow-up.
Statistical analysis
Descriptive statistics were used to describe the population. A Chi-squared or Fisher’s Exact test was used as appropriate depending on the sample size to perform association analysis using commercial software (Prism version 7; GraphPad, La Jolla, California, USA). Kaplan-Meier survival analysis was used to determine the long-term survival rates for the RDD and the NSLC groups. Significance was set at P < 0.05.
Results
Animals
Of 402 horses treated surgically for colic between January 2000 and December 2016, 137 (34%) were diagnosed with a non-strangulating large colon lesion. Of these 137 horses, 67 (49%) had a primary diagnosis of right dorsal displacement of the large colon (RDD) and 70 (51%) had other non-strangulating large colon lesions (NSLC). Of the horses with RDD, 37 (55%) were female and 30 (45%) were male. In the NSLC group 47 (67%) and 23 (33%) were female and male, respectively. The mean ages of horses in the RDD and NSLC groups were 9.7 y and 9.8 y (range: 1 to 28 y and 8 mo to 30 y, respectively). Differences in gender and age between both groups were not significant.
The predominant breed in both populations was the Quarter Horse, which is consistent with the hospital’s general population. In the RDD group there were 24 Quarter Horses (36%), 8 draft breeds (12%), 9 Paints (13%), 6 Morgans (9%), 4 Warmbloods (6%), 7 Arabians (10), 5 Thoroughbreds (7%), 2 Standardbreds (3%), and 2 Pony breeds (3%). In the NSLC group there were 22 Quarter Horses (31%), 10 Thoroughbreds (14%), 6 Paints (9%), 7 pony breeds (10%), 5 Warmbloods (7%), 6 draft breeds (9%), 4 Arabians (6%), 3 Tennessee walkers (4%), and 7 other breeds (10%).
Surgical diagnosis
During surgery, 67 horses were diagnosed with RDD as a surgical finding. Of the horses with confirmed RDD, 3 were euthanized during surgery due to significant vascular compromise of the large colon. When considering all RDD surgical cases, 64 (96%) survived surgery. Of the 70 horses in the NSLC group, 16 had large colon impaction, 12 had retroflexed pelvic flexure, 11 had left dorsal displacement, and 31 had non-strangulating large colon volvulus. Of the horses with NSLC surgical lesions, 3 horses did not survive surgery and recovery from anesthesia: 1 had gastric rupture during surgery, 1 had severe ataxia and other neurologic signs during recovery, and 1 had complete rupture of a collateral ligament of the stifle during recovery. Only cases with non-strangulating lesions were considered for post-operative analysis. Horses that did not survive anesthesia in both RDD and NSLC groups were not included in any post-surgical statistical analyses of survival and complications.
Post-operative complications
Of the 64 RDD horses that survived surgery, 28 (44%) experienced ≥ 1 complication during the post-operative period. Of these 28 horses, 13 (46%) experienced minor complications and 15 (54%) experienced major complications. Eleven of the cases with major complication had concurrent minor complications. In 27 (96%) horses the complications were related to the gastrointestinal tract. The most common gastrointestinal tract complication was recurrent colic in 25 (39%) horses. Twenty-seven of the horses had a history of colic of ≥ 48 h duration and 16 (59%) of them encountered some type of complication after surgery. Five horses with RDD (8%) underwent a second exploratory laparotomy before discharge from hospital. Findings during the second laparotomy were ileus in 2 horses, RDD in 2 horses, and enterolith in small colon in 1 horse.
Twenty-seven of the 67 (40%) NSLC surgery survivors experienced ≥ 1 complication during the post-operative period. Of those 27 horses, 22 (81%) had minor complications and 5 (19%) experienced a major complication. Four of the horses with major complication also experienced minor complications. In 22 (81%) horses the complications were related to the gastrointestinal tract. The most common gastrointestinal tract complications were diarrhea (19%) and recurrent colic (18%). In 31 horses the colic signs were of ≥ 48 h duration and 11 (35%) of them had complications after surgery. None of the NSLC horses underwent a second exploratory laparotomy before discharge from hospital.
The complication rates for the RDD (44%) and NSLC (40%) groups were similar. The horses in the RDD group were more likely to experience major complications (P = 0.0145) and the horses in the NSLC group experienced more minor complications, but the difference was not significant (P = 0.118). The horses with RDD showed more recurrent colic episodes before hospital discharge (P = 0.0111). In addition, 5 horses with RDD had another surgical exploratory procedure before discharge, which was significantly different from the NSLC group (P = 0.0256).
Fifty-eight (87%) of the 67 RDD surgical cases and 65 (93%) of the 70 NSLC surgical cases survived to hospital discharge. Death after surgery was increased in the proportion of horses with major complications. Four out of 6 horses in the RDD group and 2 out of 2 horses in the NSLC group died due to major complications and did not survive to hospital discharge. Although the proportion of survival to hospital discharge was greater in the NSLC group, compared with the RDD group, the difference was not significant (P = 0.267).
Follow-up results
Long-term follow-up was available for 34 (59%) of the horses with RDD and 30 (46%) of the horses with NSLC that were discharged from hospital. At the time of follow-up, 26 horses (76%) from the RDD group were alive and 8 (24%) were dead, whereas 18 horses (60%) from the NSLC survivors were alive, and 12 (40%) were dead. Nineteen of the 34 (56%) RDD horses showed colic signs after discharge and 8 (24%) of the 34 horses required a second exploratory laparotomy. Diagnoses at surgery included: non-specified colon displacement (n = 1), non-strangulating large colon volvulus (n = 2), small intestinal adhesions with venous outflow impairment at the root of the mesentery (n = 1), 360° strangulating large colon volvulus (1 case), left dorsal large colon displacement (n = 1), and unknown (n = 2). Of the discharged NSLC horses available for follow up, 13 (43%) showed colic signs after hospital discharge and only 1 horse underwent a second exploratory laparotomy (3%). The diagnosis at the second surgery was gas distended small intestine and large colon. Although the proportion of horses with RDD (56%) showed more colic signs after discharge than the NSLC group of horses (43%), this difference was not significant (P = 0.453). The horses with RDD, however, were more likely to have a second laparotomy after hospital discharge (P = 0.0294) as well as in general after their first abdominal exploratory surgery overall compared to the horses with NSLC (P = 0.0003).
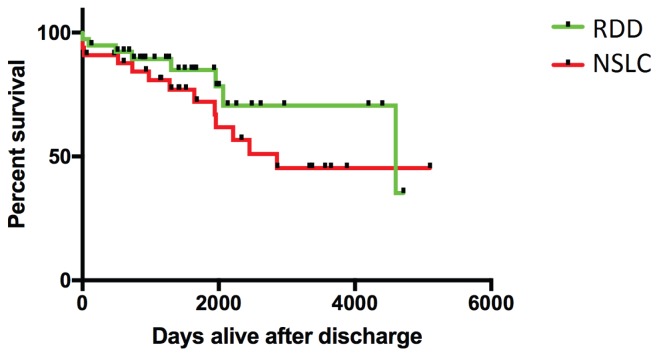
Twenty-five of the RDD cases (74%) and 23 of the NSLC cases (77%) available for follow-up had returned to their original function. Overall, owners of both groups were satisfied with the outcome (85% for the RDD group and 87% for the NSLC group). Although median long-term survival time was greater for RDD cases than NSLC cases (4599 and 2855 days, respectively), this difference was not significant (P = 0.237) (Figure 1).
Figure 1.
Kaplan-Meier survival curve for RDD and NSLC groups of horses that survived hospital discharge. RDD — right dorsal displacment of large colon; NSLC — non-strangulating large colon lesion.
Discussion
Although Smith and Mair (2) reported an increased incidence of colic after surgery in horses with RDD, no previous studies have specifically investigated complications experienced by horses with RDD for short- and long-term survival. The current study confirms that the incidence of post-operative colic between RDD and other non-strangulating conditions of the large colon in this US population of horses is similar to that in the Smith and Mair study (2). In addition, our study showed that the RDD group was more likely to experience severe complications. The RDD group also showed more gastrointestinal tract complications, which could potentially be associated with the increased incidence of recurrent colic episodes.
The types of post-operative complications identified here are similar to those in previous studies examining complications in colic patients (9–12). In previous reports, jugular thrombosis, ileus, wound suppuration/hernia, relaparotomy, and postoperative colic were often noted in the immediate post-operative period. These types of complications were also noted in our study; however, comparison between our study and other studies is difficult because of the difference in horse populations. In previous studies, horses with both small and large intestinal involvement were included and it was found that horses with small intestinal obstructions experienced more complications than horses with large intestinal obstructions (9,11–13). To our knowledge, only 2 studies have assessed complications after large intestinal surgery (2,4). These authors reported an increased risk of post-operative colic in RDD cases (2), as well as associations for post-operative survival in cases undergoing large intestinal surgery with heart rate and PCV on admission, age of the horse, and whether it underwent resection or relaparotomy (4).
Complications in the RDD group were more severe than in the NSLC group in this study. It was also noted that more horses in the RDD group had additional minor complications, and thus experienced a combination of major and minor complications more frequently than did the NSLC group. It is impossible to identify exactly why this was the case; however, it may be related to horses with RDD having a history of mild obstruction of longer duration than other large colon lesions such as large colon volvulus (14). This low-grade prolonged colic, plus delayed referral and decision to perform surgery affects complications and outcome, which could explain the difference in severity of complications (11,12,15). In this study, however, both groups had a similar number of horses with a history of ≥ 48 h of colic. In both right and left displacement of the large colon, the colon can rotate on its long axis causing various degrees of venous congestion (3,16,17). The additional component of gastric outflow obstruction may also be contributing to the severity of complications after surgery (16). If these factors as well as the duration of colic signs are taken into account, this could potentially provide an explanation for the increase in severity of complications in our RDD group. In the RDD group 59% of horses with these factors developed post-operative complications compared with 35% in the NSLC group.
Recurrent colic is one of the reported complications seen in large intestinal surgery, especially in right dorsal displacements of the large colon (2). Smith and Mair (2) found that horses with right dorsal displacement of the large colon had a 36% chance of recurrent colic compared with 1% to 9% in other non-strangulating large colon displacements. In this previous study no distinction was made between colic episodes that occurred immediately after surgery and those that were long-term recurrent. In comparison, episodes of recurrent colic were identified both before and after hospital discharge herein. We found that before hospital discharge, 39% of RDD cases showed signs of recurrent colic, which is a rate similar to the findings by Smith and Mair (2). Long-term recurrent colic signs were also more frequent in the RDD group than in the NSLC group, 56% compared to 43%, respectively. This recurrence rate is higher than previously reported; however, the number of follow-up cases in this population could have impacted this number. Overall, we concur that horses undergoing an exploratory laparotomy for right dorsal displacement of the large colon are predisposed to post-operative colic in the short- and long-term compared to horses with other forms of large colon displacement.
The more frequent recurrent colic episodes seen in RDD cases are hard to explain. Many of these horses have concurrent findings during exploratory laparotomy, such as impactions, colonic congestion, and edema (3,16,18). Other concurrent pathologies may contribute to systemic inflammation and development of motility disturbances that increase the risk of large colon displacement or other lesions leading to colic signs. Chronic hypoxia and inflammation are thought to contribute to risk of gastrointestinal tract displacement by influencing large colon motility (19). It has been documented that ≥18 h of inflammation are required to cause disruption of gastrointestinal pacemaker cells (interstitial cells of Cajal, ICC) (20). Previous studies have demonstrated reduced ICC density and decreased neuronal activity at the pelvic flexure in horses diagnosed with ascending colonic lesions (19,21). Such a scenario could explain the clinical presentation of many horses with RDD that experience prolonged low grade colic for more than 1 day before exploratory celiotomy. Further research to determine the degree of inflammation and impact on motility cells in the equine colon, could be beneficial in both guiding management practices in RDD cases and potentially identifying specific prevention measures.
The horses in the RDD group were more likely to have a second laparotomy immediately after surgery as well as in the long-term after hospital discharge. Of the horses that underwent a second exploratory laparotomy, the main surgical findings were motility problems such as ileus or a recurrence of some type of displacement of the large colon. Recurrence of RDD was the most common finding in previous work (2,3). However, RDD was not the most common finding in the horses of this report, although most surgical findings did involve the large colon. The number of horses that underwent a second surgery before hospital discharge was comparable to previous reports, 8% compared to 10%, respectively (2,22). However, the percentage of horses undergoing a second surgery long-term was higher (24%) than reported in the literature (2,22). Increased episodes of recurent colic long-term are reported indications of relaparotomy (13,22). The number of follow-up horses could also have impacted the incidence of relaparotomy long-term. If a larger number of horses were available for follow-up, the relaparotomy incidence could be comparable to previously reported numbers.
Limitations of this study include its retrospective nature and the relatively small number of horses in each group studied at a single institution. Although our data are considered an acceptable loss to follow-up for data missing at random in a cohort study (< 60%) (23), a greater response rate would have increased statistical power. Unfortunately there was a relatively large number of NSLC cases lost to follow-up, which may have impacted the analysis of long-term survival. Furthermore, post-operative treatment was dependent on individual surgeon’s clinical experience and training and this could have impacted development of complications after surgery. Studies show that surgeons can affect outcome, while other studies show no effect (11,24–26).
In conclusion, the increased incidence of major post-operative complications in horses with RDD in the present study does not seem to influence short- or long-term survival. Right dorsal displacement cases showed more recurrent colic after surgery than did NSLC cases, which is shown in our study as well as in the population reported by Smith and Mair (2). It is possible that the occurence of more severe complications identified in our study could potentially influence these recurrent colic episodes. Severe complications also increase the need for relaparotomy, which further increases the risk of recurrent colic. This knowledge may influence practitioners when attempting medical management, making decisions for referral, and advising horse owners. Prospective studies are warranted to further investigate the increased risk of post-operative colic in horses with RDD.
Acknowledgments
The authors thank Meaghan Threadgill for her assistance with data collection and Colin Longhurst, from the department of Biostatistics and Medical Informatics for his assistance with statistics. Preliminary results were presented as an Abstract at the 2016 ACVS Surgery Summit and the 2017 International Equine Colic Research Symposium. CVJ
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Hackett RP. Displacement of the large colon. In: Mair TS, Divers TJ, Ducharme NG, editors. Manual of Equine Gastroenterology. 1st ed. St. Louis, Missouri: WB Saunders; 2002. pp. 284–288. [Google Scholar]
- 2.Smith LJ, Mair TS. Are horses that undergo an exploratory laparotomy for correction of a right dorsal displacement of the large colon predisposed to post operative colic, compared to other forms of large colon displacement? Equine Vet J. 2010;42:44–46. doi: 10.2746/042516409X464122. [DOI] [PubMed] [Google Scholar]
- 3.Rakestraw PC, Hardy J. Large intestine. In: Auer JA, Stick JA, editors. Equine Surgery. 4th ed. St. Louis, Missouri: Elsevier; 2012. pp. 463–476. [Google Scholar]
- 4.Proudman CJ, Edwards GB, Barnes J, French NP. Modelling long-term survival of horses following surgery for large intestinal disease. Equine Vet J. 2005;37:366–370. doi: 10.2746/0425164054529328. [DOI] [PubMed] [Google Scholar]
- 5.Huskamp B, Kopf N. Right dorsal displacement of the large colon in the horse. Equine Pract. 1983;5:20–28. [Google Scholar]
- 6.Foerner JJ. Diseases of the large intestine: Differential diagnosis and surgical management. Vet Clin North Am Equine Pract. 1982;4:129–146. doi: 10.1016/s0196-9846(17)30122-2. [DOI] [PubMed] [Google Scholar]
- 7.Sellers AF, Lowe JE. Review of large intestinal motility and mechanisms of impaction in the horse. Equine Vet J. 1986;18:261–263. doi: 10.1111/j.2042-3306.1986.tb03621.x. [DOI] [PubMed] [Google Scholar]
- 8.Weese JS, Holcombe SJ, Embertson RM, et al. Changes in the faecal microbiota of mares precede the development of post partum colic. Equine Vet J. 2015;47:641–649. doi: 10.1111/evj.12361. [DOI] [PubMed] [Google Scholar]
- 9.French NP, Smith J, Edwards GB, Proudman CJ. Equine risk factors for postoperative complications. Equine Vet J. 2002;34:444–449. doi: 10.2746/042516402776117791. [DOI] [PubMed] [Google Scholar]
- 10.Proudman CJ, Smith JE, Edwards GB, French NP. Long-term survival of equine surgical colic cases. Part 1: Patterns of mortality and morbidity. Equine Vet J. 2002;34:432–437. doi: 10.2746/042516402776117845. [DOI] [PubMed] [Google Scholar]
- 11.Mair TS, Smith LJ. Survival and complication rates in 300 horses undergoing surgical treatment of colic. Part 1: Short-term survival following a single laparotomy. Equine Vet J. 2005;37:296–302. doi: 10.2746/0425164054529409. [DOI] [PubMed] [Google Scholar]
- 12.Mair TS, Smith LJ. Survival and complication rates in 300 horses undergoing surgical treatment of colic. Part 2: Short-term complications. Equine Vet J. 2005;37:303–309. doi: 10.2746/0425164054529364. [DOI] [PubMed] [Google Scholar]
- 13.Mair TS, Smith LJ. Survival and complication rates in 300 horses undergoing surgical treatment of colic. Part 3: Long-term complications and survival. Equine Vet J. 2005;37:310–314. doi: 10.2746/0425164054529445. [DOI] [PubMed] [Google Scholar]
- 14.Southwood LL, Bergsline K, Jacob A, et al. Large colon displacement and volvulus in horses: 495 cases 1987–1999. Proc 7th International Equine Colic Research Symposium; Manchester, UK. July 14–16, 2002; pp. 32–33. [Google Scholar]
- 15.Van der Linden MA, Laffont CM, Sloet van Oldruitenborgh-Oosterbaan MM. Prognosis in equine medical and surgical colic. J Vet Intern Med. 2003;17:343–348. doi: 10.1111/j.1939-1676.2003.tb02459.x. [DOI] [PubMed] [Google Scholar]
- 16.McGovern KF, Suthers JM, James FM, et al. Gastric impaction associated with displacement and volvulus of the large colon in seven mature horses. Equine Vet Educ. 2015;27:453–459. [Google Scholar]
- 17.Mc Govern KF, Bladon BM, Fraser BSL, Boston RC. Attempted medical management of suspected ascending colon displacement in horses. Vet Surg. 2011;41:399–403. doi: 10.1111/j.1532-950X.2011.00915.x. [DOI] [PubMed] [Google Scholar]
- 18.Blikslager AT. Gastric impaction and large colon volvulus: Can one lead to the other? Equine Vet Educ. 2015;27:460–461. [Google Scholar]
- 19.Pavone S, Gialletti R, Pepe M, Onofri A, Mandara MT. Histological and immunohistochemical studies of changes in myenteric plexuses and in interstitial cells of Cajal associated with equine colic. Res Vet Sci. 2012;93:350–359. doi: 10.1016/j.rvsc.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 20.Der T, Bercik P, Donnelly G, et al. Interstitial cells of Cajal and inflammation-induced motor dysfunction in the mouse small intestine. Gastroenterology. 2000;119:1590–1599. doi: 10.1053/gast.2000.20221. [DOI] [PubMed] [Google Scholar]
- 21.Fintl C, Hudson NP, Mayhew IG, Edwards GB, Proudman CJ, Pearson GT. Interstitial cells of Cajal (ICC) in equine colic: An immunohistochemical study of horses with obstructive disorders of the small and large intestines. Equine Vet J. 2004;36:474–479. doi: 10.2746/0425164044877314. [DOI] [PubMed] [Google Scholar]
- 22.Mair TS, Smith LJ. Survival and complication rates in 300 horses undergoing surgical treatment of colic. Part 4: Early (acute) relaparotomy. Equine Vet J. 2005;37:315–318. doi: 10.2746/0425164054529454. [DOI] [PubMed] [Google Scholar]
- 23.Kristman V, Manno M, Côté P. Loss to follow-up in cohort studies: How much is too much? Eur J Epidemiol. 2004;19:751–760. doi: 10.1023/b:ejep.0000036568.02655.f8. [DOI] [PubMed] [Google Scholar]
- 24.Shires GM, Kaneps AJ, Wagner PC, Schmotzer WB. A retrospective review of 219 cases of equine colic. Proc 2nd Equine Colic Research Symposium; Athens, Georgia. 1986; pp. 239–241. [Google Scholar]
- 25.Freeman DE, Hammock P, Baker GJ, et al. Short- and long-term survival and prevalence of postoperative ileus after small intestinal surgery in the horse. Equine Vet J. 2000;32:42–51. doi: 10.1111/j.2042-3306.2000.tb05333.x. [DOI] [PubMed] [Google Scholar]
- 26.Proudman CJ, Smith JE, Edwards GB, French NP. Long-term survival of equine surgical colic cases. Part 2: Modelling postoperative survival. Equine Vet J. 2002b;34:438–443. doi: 10.2746/042516402776117881. [DOI] [PubMed] [Google Scholar]