Abstract
Background:
Some trials have stated that there is no benefit to tamsulosin administration for clearing ureteral stones, which is contrary to previous studies. To confirm the efficacy of tamsulosin for treating symptomatic ureteral stones, we performed this review.
Methods:
We searched the PubMed, Embase, and Cochrane Library databases to identify all studied variables, including tamsulosin, urinary stones, expulsion, and side effects. In addition, for all patients and different stone sizes, the treatment efficacy, expulsion rate, and expulsion time were also recorded for this treatment.
Results:
Forty-nine studies involving 6436 patients met the inclusion criteria. The data synthesized from these studies indicated that tamsulosin improved the renal stone clearance rate (80.5% vs 70.5%; mean difference (MD), 1.16; 95% confidence interval (CI), 1.13–1.19; P <.00001) and reduced the expulsion time (MD, −3.61; 95% CI, −3.77 to −3.46; P ≤.00001). Regarding complications, no significant difference was found between the 2 groups in terms of the total side effects (MD, 1.15; 95% CI, 0.97–1.35; P = .10) or divided complications, including retrograde ejaculation (P = .01), hypotension (P = .52), dizziness (P = .07), diarrhea (P = .58), vomiting (P = .88), headache (P = .84), nausea (P = .91), and fatigue (P = .10).
Conclusions:
Tamsulosin should be strongly recommended for patients with ureteral stones to increase treatment efficacy. The side effects were not significantly different between the tamsulosin and control treatments.
Keywords: expulsive, side effects, tamsulosin, urinary stone
1. Introduction
The prevalence of urolithiasis, or urinary stone disease (USD), is increasing among adults and children worldwide. Because the most common symptoms of USD include severe flank and abdominal pain, nausea, vomiting and hematuria, patients often present to the emergency department for treatment.[1] Many clinical studies have been performed.[2–50] In general, trials have supported the use of tamsulosin to achieve higher stone expulsion rates and lower analgesic requirements. The presumed mechanism of action of α-blockers is inhibition of smooth muscle contraction in the ureter, facilitating passage of the stone into the bladder.[4] Nevertheless, these guidelines have been called into question by several recently published high-quality randomized controlled trials (RCTs), and the effectiveness of α-blockers has been questioned for the management of ureteral colic.[4,7–11] For instance, a phase III trial that included multiple centers reported no benefit of tamsulosin for patients with distal ureteral calculi in terms of spontaneous stone passage, time to stone expulsion, or analgesic requirements.[7] In addition, the results of a 28-day course of tamsulosin showed that this treatment did not increase the overall stone passage rate or improve a wide range of secondary outcomes in patients who presented to the emergency department with symptomatic ureteral stones less than 9 mm in diameter.[4] The contradictory results provided by several RCTs versus the findings of other studies encouraged us to conduct this meta-analysis to address this issue.
2. Methods
A comprehensive search strategy was used to investigate the efficacy of tamsulosin for the treatment of USD and included the PubMed (updated to current), the Embase (updated to current), the Cochrane Central Register of Controlled Trials, and the Cochrane Database of Systematic Reviews electronic databases. No ethical review was necessary to conduct this meta-analysis. The initial search process was designed to capture all relevant studies using the following search terms: tamsulosin, urinary colic, and expulsion. The reference lists from the retrieved documents were also searched. In addition, the included patients had to meet the following criteria: adults aged 18 to 60 years; emergency admission for renal colic; presence of a single ureteral stone confirmed by plain abdominal radiography (kidney–ureters–bladder), urinary ultrasonography, and/or non-contrast-enhanced computed tomography (CT). A distal ureteral stone location was defined as a stone located below the level of the sacroiliac joint on CT, stone size was defined by the largest diameter in 3 planes, and all stone were evaluated by the reporting radiologist on CT images. The exclusion criteria were fever; urinary tract infection; severe hydronephrosis; renal insufficiency, which was defined as an estimated glomerular filtration rate of <60 mL/min per 1.73 m2; abnormal anatomy, such as a solitary kidney, horseshoe kidney, or duplex urinary system; urethrostenosis; history of ureteral stricture; diabetes mellitus; current use of α-adrenoceptor antagonists or corticosteroids; and known or suspected allergy to the studies medications. The quality of the studies included was determined according to the Cochrane Collaboration Reviewer's Handbook and the Quality of Reporting of Meta-analysis guidelines.[50,51] The assessment tool contained 6 core items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. Each study classified as having a low, unclear, or high risk of bias was resolved by a third author. All of the included studies were also evaluated using the Jadad scale, and the trials were considered to be of high quality if the Jadad score was ≥3 and low quality if the score was ≤2.[52]
We divided patients into 2 groups according to the different treatment methods in this meta-analysis. Analysis 1 included patients who were treated with tamsulosin, and analysis 2 included patients who were treated with control treatments, including placebo and conservative treatments. The outcome measures were expulsion rate, expulsion time and side effects. Data were extracted independently by 2 authors using a predesigned data extraction form. Data extraction included the data source, eligibility, methods, participant characteristics, interventions, and results.
Data analysis for this meta-analysis was performed using RevMan 5.1.4. Continuous outcomes are presented as the weighted mean difference (MD) with the 95% confidence interval (CI). Dichotomous data are presented as the relative risk (RR) with the 95% CI. A fixed-effects or random-effects method was used to analyze the data. The fixed-effects method was used to combine the results when no significant heterogeneity was present. The random-effects method was applied when heterogeneity was present. Statistical heterogeneity among the trials was evaluated using the I2 test, with significance set at P <.05. Publication bias was evaluated using a funnel plot. In addition, a sensitivity analysis was performed if low-quality trials were included in the analysis.
3. Results
3.1. Description of the included studies
A total of 6436 reports were initially identified from the database and manual search. After removing redundant publications, reviews and meta-analyses, and after scanning titles and abstracts of unrelated records, 6238 reports were excluded from the study. After referring to the full texts, 21 articles with different baselines, 11 articles with different results criteria, and 27 articles with different group settings were excluded. Finally, 49 publications involving 8987 patients were included in this study. The conditions of these studies and the clinical details of the patients are presented in Table 1. The search flow diagram is presented in Figure 1. All of the included trials were assessed by Jadad score for quality: 45 (91.84%) trials were graded as high quality, and only 4 (8.16%) trials were graded as low quality.
Table 1.
Patient's characteristics at baseline.
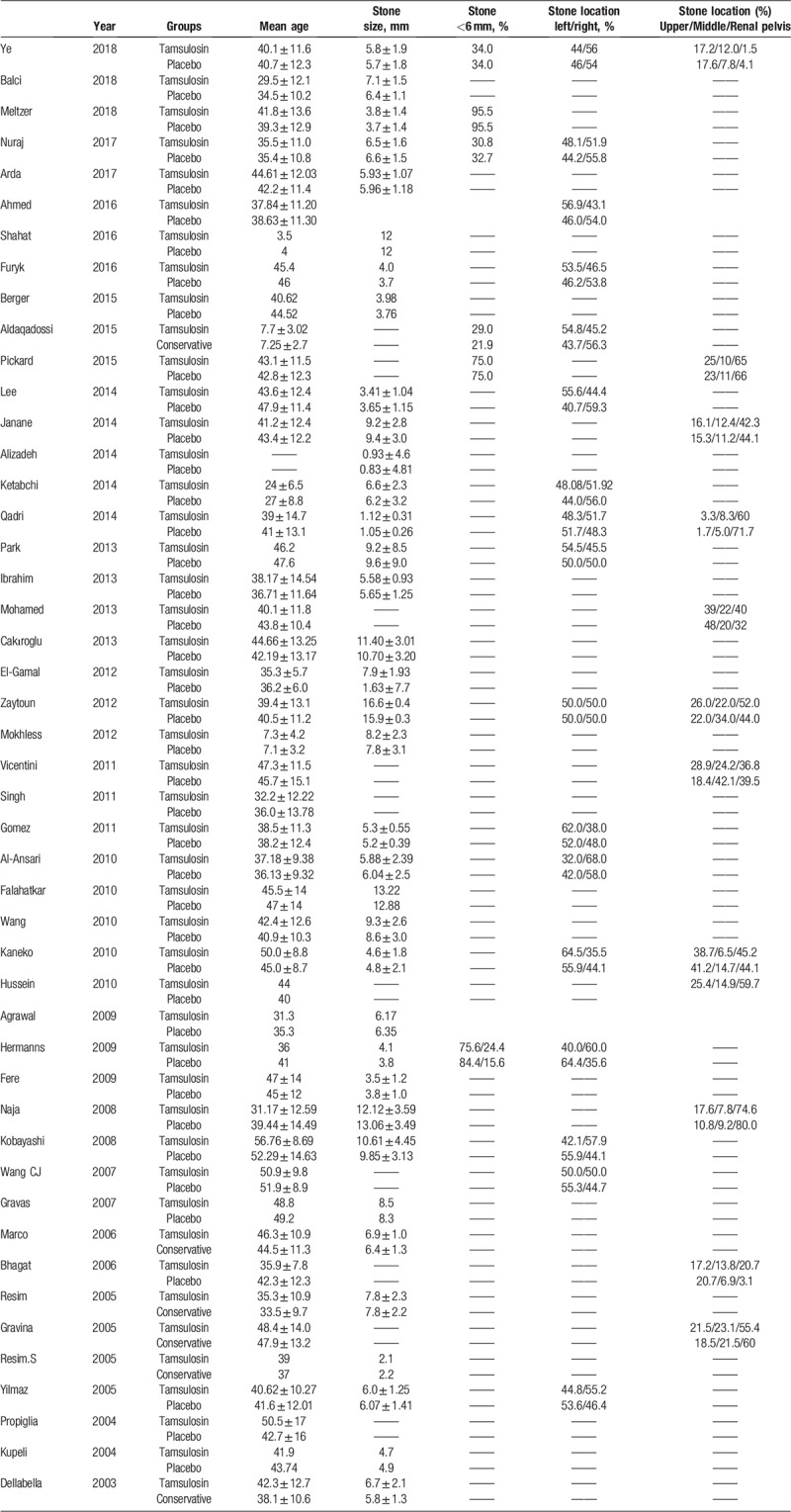
Figure 1.
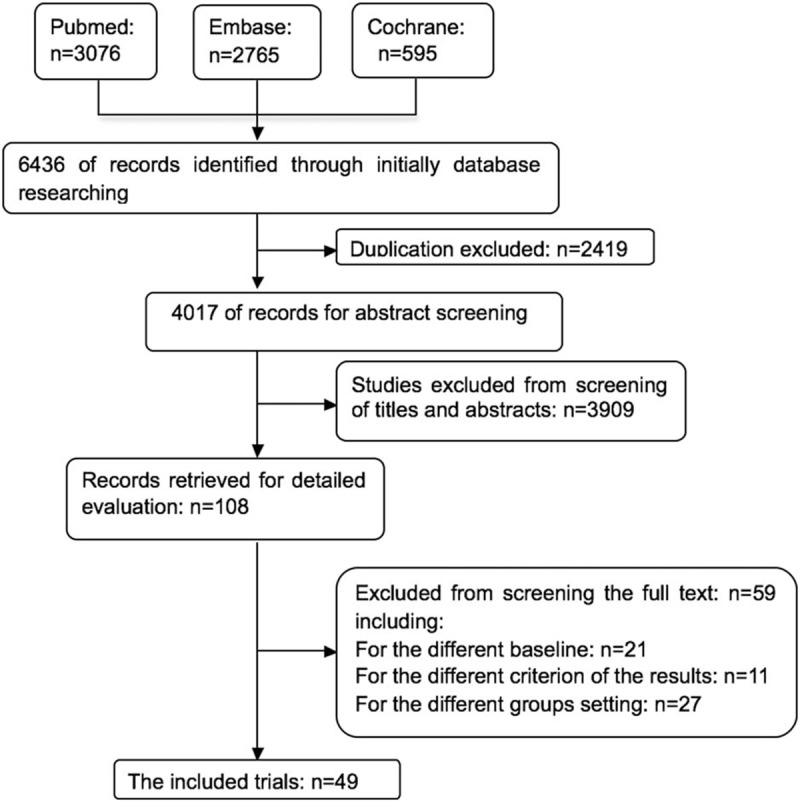
The search flow diagram.
3.2. Comparison of the expulsion rates
The results comparing the efficacy of tamsulosin and the control treatment are presented in Table 2. Forty-six studies compared the expulsion rate between tamsulosin and control treatment. Tamsulosin was better than the control treatment in terms of the expulsion rate (80.5% vs 70.5%; MD, 1.16; 95% CI, 1.13–1.19; P <.00001; Fig. 2a). Additionally, 3 studies compared the expulsion rate of stones less than 6 mm (32.9% vs 32.51; MD, 1.02; 95% CI, 0.93–1.12; P = .62; Fig. 2b) and more than 6 mm (51.8% vs 44.8%; MD, 1.16; 95% CI, 1.09–1.24; P <.00001; Fig. 2c). The expulsion rate of stones less than 6 mm seemed to be similar to the 2 different treatments, but the expulsion rate of stones greater than 6 mm was better with tamsulosin than with the control treatment. The overall expulsion rate was higher with tamsulosin treatment than with the control treatment.
Table 2.
Patient's outcomes by treatment group.
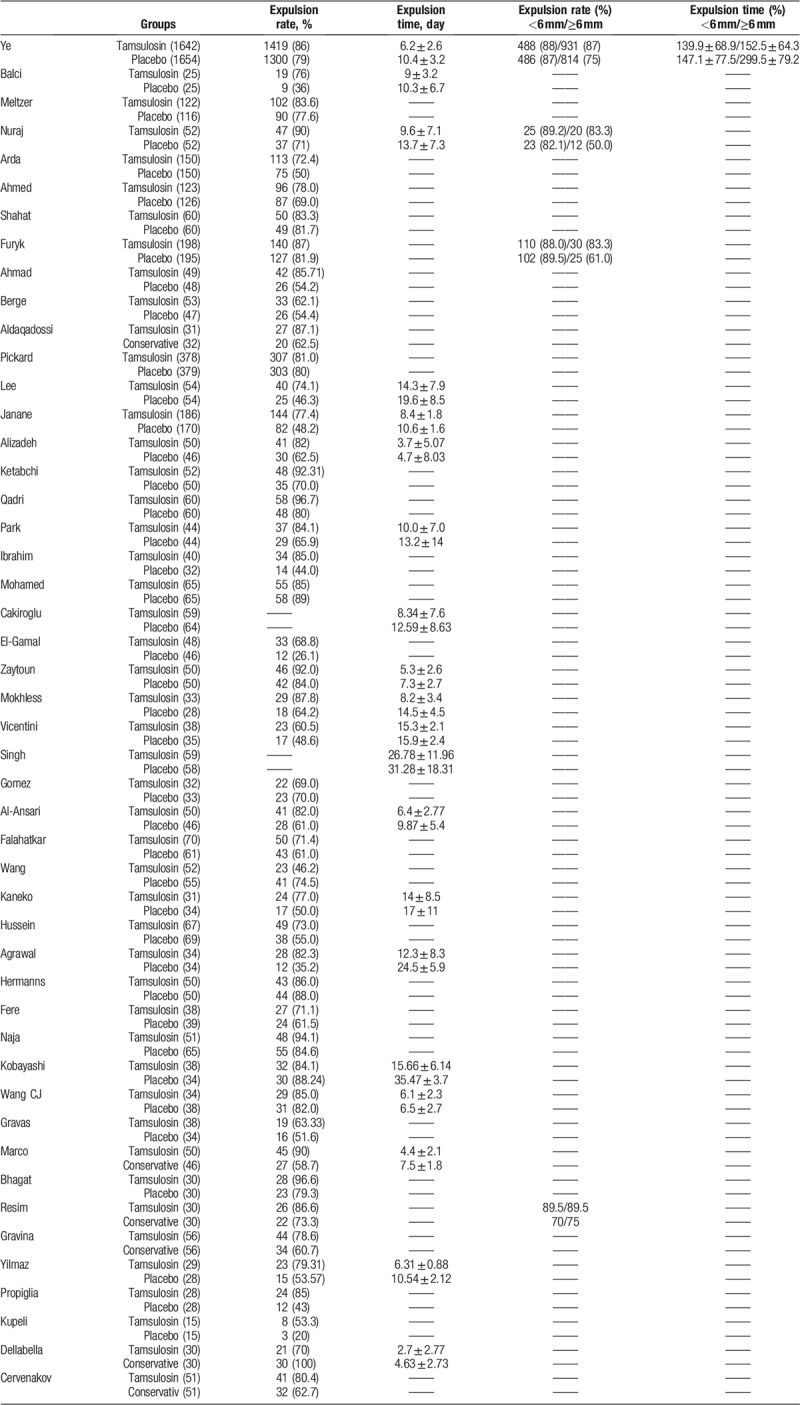
Figure 2.
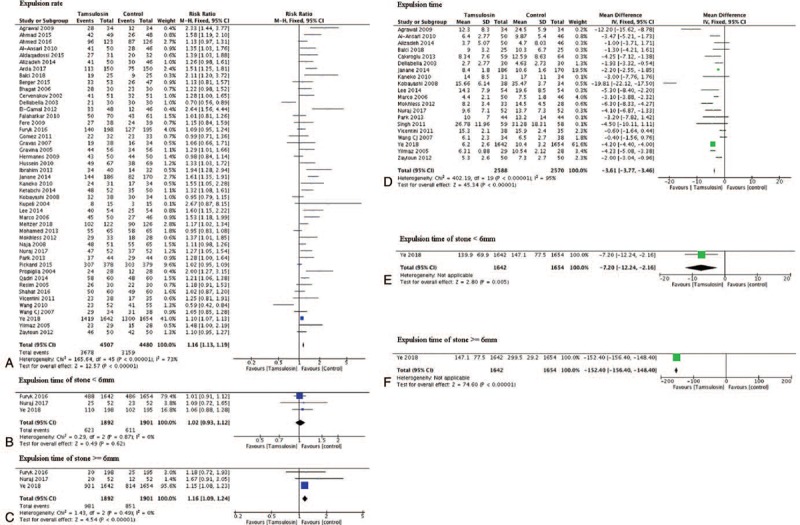
Compare the efficacy of stone expulsion between tamsulosin and the control treatment.
In addition, 20 studies compared the expulsion time between tamsulosin and the control treatment, and tamsulosin treatment had a shorter expulsion time than the control treatment (MD, −3.61; 95% CI, −3.77 to −3.46; P ≤.00001; Fig. 2d). Only 1 study explored the expulsion time between tamsulosin and the control treatment of stones less than 6 mm (MD, −7.20; 95% CI, −12.24 to −2.16; P = .005; Fig. 2e) and more than 6 mm (MD, -152.40; 95% CI, −156.40 to −148.80; P <.00001; Fig. 2f).
3.3. Comparison of side effects between the 2 treatments
The results comparing the side effects of tamsulosin and the control treatment are presented in Table 3. Nine studies showed that the incidence rate of retrograde ejaculation was higher in the tamsulosin group than in the control group (MD, 1.36; 95% CI, 1.07–1.73; P = .01; Fig. 3a). Eight studies showed that there was no difference in the occurrence of hypotension between the 2 treatments (MD, 1.26; 95% CI, 0.63–2.52; P = .52; Fig. 3b). Eleven studies compared the dizziness rate and found no difference between the 2 groups (MD, 1.25; 95% CI, 0.99–1.58; P = .07; Fig. 3c). Five studies compared the diarrhea rate and found no difference between the tamsulosin and control groups (MD, 1.13; 95% CI, 0.74–1.71; P = .58; Fig. 3d). Four reviews showed that the rate of vomiting was not different between the 2 treatments (MD, 1.02; 95% CI, 0.79–1.31; P = .88; Fig. 3e). Seven studies found that the occurrence of headache was no difference between the 2 groups (MD, 0.98; 95% CI, 0.81–1.19; P = .84; Fig. 3f). Only 2 studies included the rate of nausea and found no difference between the 2 groups (MD, 1.01; 95% CI, 0.79–1.31; P = .91; Fig. 3g), and only 3 studies evaluated the rate of fatigue (MD, 1.21; 95% CI, 0.89–1.64; P = .24; Fig. 3h). The total complication rate was also not significantly different between the 2 groups (MD, 1.15; 95% CI, 0.97–1.35; P = .10; Fig. 3i).
Table 3.
Patient's adverse events by treatment group (%).
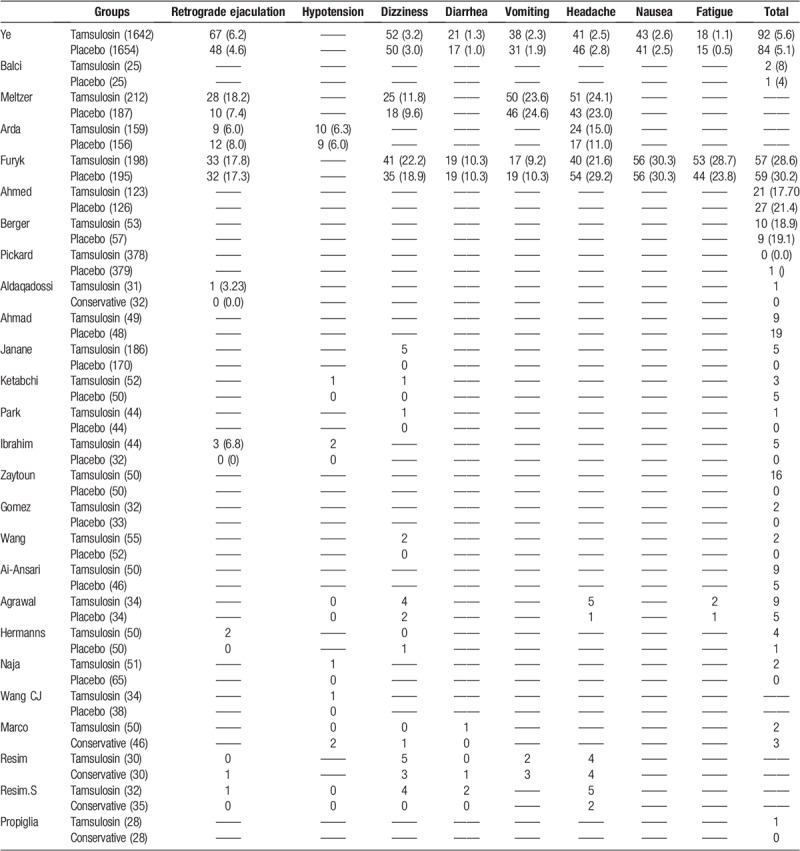
Figure 3.
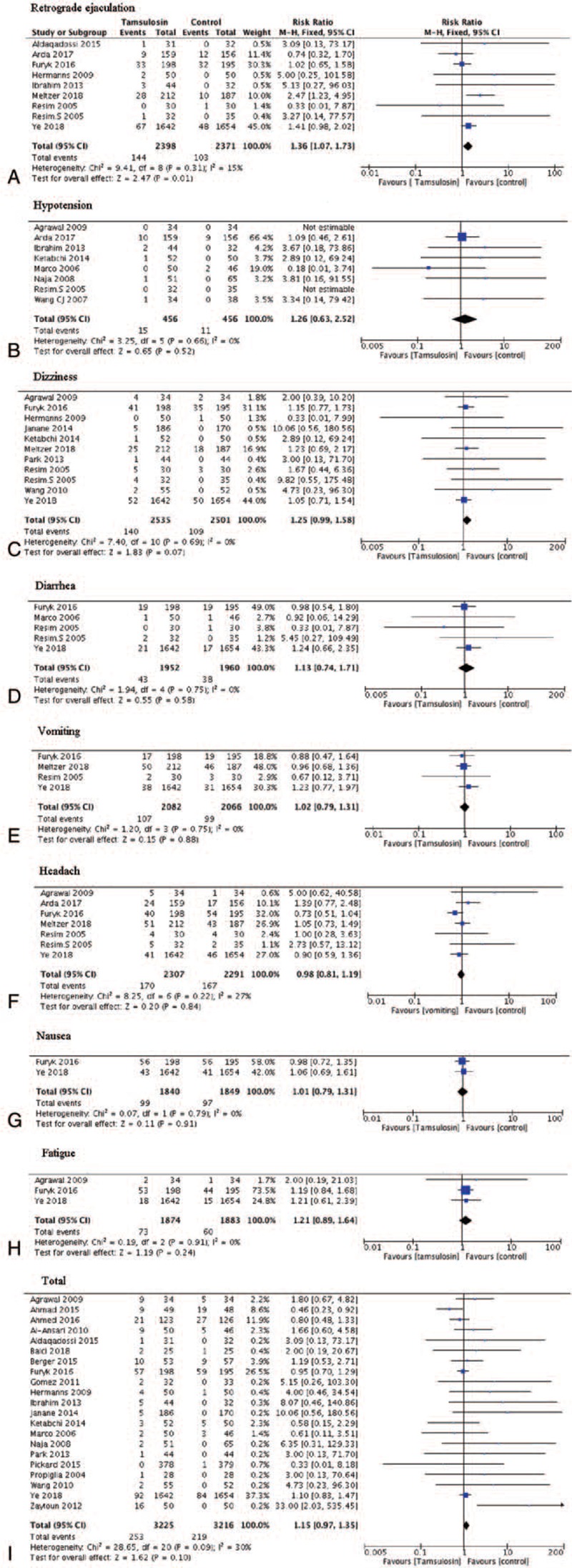
Compare the complications between tamsulosin and the control treatment.
3.4. Publication bias
The low risk of publication bias in the outcomes of expulsion rate and complications is shown by the shapes of the inverted funnel plots (Fig. 4).
Figure 4.
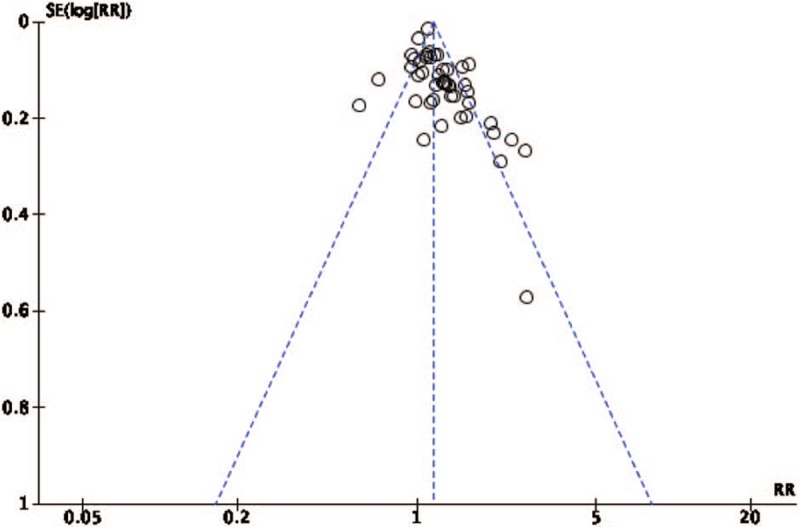
The risk of publication bias.
4. Discussion
The management of ureteral stones has largely evolved from open surgery to minimally invasive methods, such as extracorporeal shockwave lithotripsy (ESWL), ureterorenoscopic removal of stones, or watchful waiting, due to the many advances in endourological techniques and instrumentation. The management of ureteral stones with open surgery has evolved to the use of minimally invasive methods due to advances in endourological techniques and instrumentation. Currently, the most widely accepted therapies for ureteral colic are minimally invasive and are the gold standard treatments. However, these techniques are quite expensive, even though they are associated with decreased risk, and are not widely available in developing countries. A treatment that can aid in the passage of urinary stones without surgery could reduce both patient morbidity and healthcare costs associated with this condition.[5] Watchful waiting and medical expulsion therapy are the 2 most commonly used conservative methods that have been increasingly more frequently used in the treatment of distal ureteral stones to allow spontaneous stone passage, especially in patients who have less than grade 2 hydronephrosis.[53] Prior published meta-analyses, as well as the current American Urological Association Guidelines on the Surgical Management of Colic, provide a strong recommendation that tamsulosin be used in these patients.[4] In addition, other types of α-adrenoceptor antagonists, such as nifedipine, have also been suggested to have efficacy in some studies; at the time of the trial design, a trial by Pickard et al showed that the duration of use of agents including nifedipine could increase the rate of spontaneous stone passage and relieve pain.[11] However, tamsulosin remains the most commonly used pharmaceutical.
Some recently published studies have reported that treatment with tamsulosin does not seem to improve renal stone clearance. Alizadeh et al reported that tamsulosin did not increase the overall stone passage rate compared with placebo, even though this treatment can reduce the duration of expulsion, pain and the need for analgesics and has been found to be beneficial. A study by Ketabchi et al also demonstrated that the expulsion time was reduced by tamsulosin.[16] These studies call into question the therapeutic application of tamsulosin. On the other hand, several published meta-analyses regarding the therapeutic effectiveness of tamsulosin have demonstrated the clinical benefit of this treatment.[2] However, the evidence from these reviews is limited due to the number of included studies; however, in our review, which contained 49 studies, the level of evidence was stronger than in previous studies due to the large number of patients. In our study, we found that the use of tamsulosin was safe and clinically effective in patients with ureteral stones and was not associated an increase in side effects. When we performed the subgroup analysis, the results identified a specific clinical benefit of tamsulosin for stones measuring greater than 6 mm. Based on the evidence of many studies, we confirmed that treatment with tamsulosin is better than other conservative treatments, such as watchful waiting and massive intake of water. As a result, the dosages of pain relief medications were also reduced when tamsulosin was used.[2]
Above all, this review strengthens the evidence that tamsulosin is a useful and promising treatment method for large stones, and this finding is in accordance with the study by Ye et al.[2] Moreover, some studies have also shown that when α-1-adrenoceptors are applied to the smooth muscle of the ureters to blockade these receptors, they can significantly diminish the transmission of pain signals to the central nervous system.[2] Ureteral stones are a common, painful disease, and simple treatment may facilitate more efficient and rapid spontaneous stone passage, which is very important for patients. However, different trials have suggested opposing ideas, and a review including a sufficient number of studies for strong evidence is necessary for clinical application. This study provides strong evidence for the use of tamsulosin. However, there are some published reviews about this topic, such as the study performed by Wang et al, which only included 8 studies and the latest research included in this meta-analysis was published in 2015. We included 49 studies in our research, and the latest study was published in 2018.
There are some limitations in this study. First, the control methods used in the included studies were different; some used a placebo, some used watchful waiting, and some used massive intake of water; second, we did not compare tamsulosin with other α-blockers or medicines. Most of the studies focused on stone expulsion, and few explored pain relief, even though this symptom is the most important reason why patients present to emergency clinics. The exploration of pain relief requires further study.
5. Conclusion
Our results show that tamsulosin significantly facilitates the passage of distal ureteral stones. Subgroup analyses provided evidence of a superior expulsion rate for stones measuring greater than 6 mm. In addition, evaluation of complications also showed that this method did not increase the rate of side effects. In summary, tamsulosin is a safe and effective medical expulsion therapy for ureteral stones.
Author contributions
Data curation: Yi Sun, Qiang Wei, Xin Wei.
Formal analysis: Yi Sun, Guo-lin Lei, Qiang Wei.
Investigation: Guo-lin Lei.
Methodology: Guo-lin Lei.
Project administration: Guo-lin Lei, Lu Yang, Qiang Wei.
Resources: Lu Yang.
Supervision: Yi Sun, Qiang Wei.
Validation: Yi Sun, Xin Wei.
Visualization: Yi Sun.
Writing – original draft: Yi Sun, Xin Wei.
Writing – review & editing: Xin Wei.
Footnotes
Abbreviations: CI = confidence interval, CT = computed tomography, MD = mean difference, RCT = randomized controlled trial, RR = relative risk, USD = urinary stone disease.
YS, G-LL and XW contributed equally to this work and should share the co-first author.
This study was supported by the National Natural Science Foundation of China (Grant No. 81370855, 81300627, 81702536, 81770756 and 81200551), This study was supported by the National key research and development program of China (Grant No. SQ2017YFSF090096), the Prostate Cancer Foundation Young Investigator Award 2013, Foundation of Science &Technology Department of Sichuan Province (Grant No. 2015SZ0230, 2013SZ0006 and 2013SZ0093), Programs from Science and Technology Department of Sichuan Province (Grant No. 2018JY0089 and 2017HH0063), Young Investigator Award of Sichuan University 2017, and the Scientific Research Project of Health Department of Sichuan Province (No. 120203).
The authors have no conflicts of interest to disclose.
References
- [1].Burrows Pamela K, Hollander Judd E, Wolfson Allan B, et al. Design and challenges of a randomized clinical trial of medical expulsive therapy (tamsulosin) for urolithiasis in the emergency department. Contemp Clin Trials 2017;52:91–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ye Zhangqun, Zeng Guohua, Yang Huan, et al. Efficacy and safety of tamsulosin in medical expulsive therapy for distal ureteral colics with renal colic: a multicenter, randomized, double-blind, placebo-controlled trial. Eur Urol 2018;73:385–91. [DOI] [PubMed] [Google Scholar]
- [3].Balci M, Tuncel A, Aydin O, et al. Tamsulosin versus nifedipin in medical expulsive therapy for distal ureteral colics and the predictive value of Hounsfield unit in colic expulsion. Ren Fail 2014;36:1541–4. [DOI] [PubMed] [Google Scholar]
- [4].Meltzer Andrew C, Burrows Pamela K, Wolfson Allan B, et al. Effect of tamsulosin on passage of symptomatic ureteral colics. A randomized clinical trial. JAMA Internal Med 2018;178:1051–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Nuraj P, Hyseni N. The role of the tamsulosin in the medical expulsion therapy for distal. Ureteral Colics 2017;71:137–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Arda E, Cakiroglu B, Yuksel I, et al. Medical expulsive therapy for distal ureteral colics: tamsulosin versus silodosin in the Turkish population. Cureus 2017;9:e1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Furyk Jeremy S, Chu K, Banks C, et al. Distal ureteric colics and tamsulosin: a double-blind, placebo-controlled, randomized, multicenter trial. Ann Emerg Med 2016;67:86–95.e2. [DOI] [PubMed] [Google Scholar]
- [8].Shahat A, Elderwy A, Safwat AS, et al. Is tamsulosin effective after shock wave lithotripsy for pediatric renal colics? a randomized, controlled study. J Urol 2016;195:1284–8. [DOI] [PubMed] [Google Scholar]
- [9].Af A, Shalaby E, El-Feky M, et al. Role of tamsulosin therapy after extracorporeal shockwave lithotripsy for renal colics: randomized controlled trial. Urol Int 2016;97:266–72. [DOI] [PubMed] [Google Scholar]
- [10].Berger DA, Ross MA, Hollande JB, et al. Tamsulosin does not increase 1-week passage rate of ureteral colics in ED patients. Am J Emerg Med 2015;33:1721–4. [DOI] [PubMed] [Google Scholar]
- [11].Pickard R, Starr K, Maclennan G, et al. Use of drug therapy in the management of symptomatic ureteric colics in hospitalised adults: a multicentre, placebo-controlled, randomised controlled trial and cost-effectiveness analysis of a calcium channel blocker (nifedipine) and an alpha-blocker (tamsulosin) (the SUSPEND trial). Health Technol Assess 2015;386:341–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ha Aldaqadossi, Shaker H, Saifelnasr M, et al. Efficacy and safety of tamsulosin as a medical expulsive therapy for colics in children. Arab J Urol 2015;13:107–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ahmad H, Azim W, Akmal M, et al. Medical expulsive treatment of distal ureteral colic using tamsulosin. J Ayub Med Coll Abbottabad 2015;27:48–50. [PubMed] [Google Scholar]
- [14].Janane A, Hamdoun A, Hajji F, et al. Usefulness of adjunctive alpha1-adrenergic antagonists after single extracorporeal shock wave lithotripsy session in ureteral colic expulsion. Can Urol Assoc J 2014;8:E8–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Alizadeh M, Magsudi M. The effect of tamsulosin in the medical treatment of distal ureteral colics. Global J Health Sci 2014;6:44–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Aa K, Mehrabi S. The effect of tamsulosin, an alpha-1 receptor antagonist as a medical expelling agent in success rate of ureteroscopic lithotripsy. Nephrourol Mon 2013;6:e12836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ss Qadri, El Khalid S, Mahmud Sm. Effects and outcome of tamsulosin more thanjust colic clearance after extracorporeal shockwave lithotripsy for renal calculi. J Pak Med Assoc 2014;64:644–8. [PubMed] [Google Scholar]
- [18].Sw L, Sh W, Ds Y, et al. Effect of tamsulosin on colic expulsion in proximal ureteral calculi: an open-label randomizedcontrolled trial. Int J Clin Pract 2014;68:216–21. [DOI] [PubMed] [Google Scholar]
- [19].Yh P, He L, Jy P, et al. A prospective randomized controlled trial of the efficacy of tamsulosin after extracorporeal shock wave lithotripsy for a single proximal ureteral colic. Korean J Urol 2013;54:527–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ak I, Ih M, Ns. M. Efficacy and safety of tamsulosin vs. alfuzosin as medical expulsive therapy for ureteric colics. Arab J Urol 2013;11:142–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Hi Mohamed. The efficacy of tamsulosin therapy after extracorporeal shock-wave lithotripsy for ureteric calculi: a prospective randomised, controlled study. Arab J Urol 2013;11:398–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Cakiroglu B, Sinanoglu O, Mahmure Uraz. The effect of tamsulosin on pain and clearance according to ureteral colic location after shock wave lithotripsy. Curr Ther Res Clin Exp 2013;74:33–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Om Z, Yakoubi R, Ar Zahran, et al. Tamsulosin and doxazosin as adjunctive therapy following shock-wave lithotripsy of renal calculi: randomized controlled trial. Urol Res 2012;40:327–32. [DOI] [PubMed] [Google Scholar]
- [24].El-Gamal O, El-Bendary M, Ragab M. Role of combined use of potassium citrate and tamsulosin in the management of uric acid distal ureteral calculi. Urol Res 2012;40:219–24. [DOI] [PubMed] [Google Scholar]
- [25].Mokhless I, Ar Zahran, Youssif M, et al. Tamsulosin for the management of distal ureteral colics in childrena prospective randomizedstudy. J Pediatr Urol 2012;8:544–8. [DOI] [PubMed] [Google Scholar]
- [26].Fc Vicentini, Mazzucchi E, Ah Brito, et al. Adjuvant tamsulosin or nifedipine after extracorporeal shock wave lithotripsy for renal colics: a double blind, randomized, placebo-controlled trial. Urology 2011;78:1016–21. [DOI] [PubMed] [Google Scholar]
- [27].Sk Singh, Ds Pawar, Ms Griwan, et al. Role of tamsulosin in clearance of upper ureteral calculi after extracorporeal shock wave lithotripsy: a randomized controlled trial. Urol J 2011;8:14–20. [PubMed] [Google Scholar]
- [28].Mez RaúL, Ochoa-Gó Vez Emilio, Prieto-D Iaz-Cha, et al. In Trujillo-Herna and́Squez Clemente Va. Tamsulosin does not have greater efficacy than conventional treatment for distal ureteral colic expulsion in Mexican patients. Urol Res 2011;39:491–5. [DOI] [PubMed] [Google Scholar]
- [29].Wang H, Liu K, Ji Li. Effect of alpha1-adrenergic antagonists on lower ureteral colics with extracorporeal shock wave lithotripsy. Asian J Surg 2010;33:37–41. [DOI] [PubMed] [Google Scholar]
- [30].Al-Ansari, Al-Naimi, Alobaidy, et al. Efficacy of tamsulosin in the management of lower ureteral colics: a randomized double-blindplacebo-controlled study of 100 patients. Urology 2010;75:4–7. [DOI] [PubMed] [Google Scholar]
- [31].Kaneko T, Matsushima H, Morimoto H, et al. Efficacy of low dose tamsulosin in medical expulsive therapy for ureteral colics in Japanese male patients: a randomized controlled study. Int J Urol 2010;17:462–5. [DOI] [PubMed] [Google Scholar]
- [32].Hussein Mm. Does tamsulosin increase colic clearance after shockwave lithotripsy of renal colics? A prospective, randomized controlled study. Scand J Urol Nephrol 2010;44:27–31. [DOI] [PubMed] [Google Scholar]
- [33].Falahatkar S, Khosropanah I, Ad Vajary, et al. Is there a role for tamsulosin after shock wave lithotripsy in the treatment of renal and ureteralcalculi? J Endourol 2011;25:495–8. [DOI] [PubMed] [Google Scholar]
- [34].Hermanns T, Sauermann, Rufibach K. Is there a role for tamsulosin in the treatment of distal ureteral colics of 7 mm or less? results of a randomised, double-blind, placebo-controlled trial. Eur Urol 2009;56:407–12. [DOI] [PubMed] [Google Scholar]
- [35].Ferre Robinson M, Capt Usaf, Wasielewski Jessica N, et al. Tamsulosin for ureteral colics in the emergency department: a randomized, controlled trial. Ann Emerg Med 2009;54:432–9. [DOI] [PubMed] [Google Scholar]
- [36].Agrawal M, Gupta M, Gupta A, et al. Prospective randomized trial comparing efficacy of alfuzosin and tamsulosin in management of lower ureteral colics. Urology 2009;73:706–9. [DOI] [PubMed] [Google Scholar]
- [37].Naja V, Agarwal MM, Mandal AK, et al. Tamsulosin facilitates earlier clearance of colic fragments and reduces pain after shockwave lithotripsy for renal calculi: results from an open-label randomized study. Urology 2008;72:1007–11. [DOI] [PubMed] [Google Scholar]
- [38].Kobayashi M, Naya Y, Kino M, et al. Low dose tamsulosin for colic expulsion after extracorporeal shock wave lithotripsy: efficacy in Japanese male patients with ureteral colic. Int J Urol 2008;15:495–8. [DOI] [PubMed] [Google Scholar]
- [39].Wang CJ, Huang SW, Chang CH. Adjunctive medical therapy with an alpha-1 specific blocker after shock wave lithotripsy of lowerureteral colics. Urol Int 2009;82:166–9. [DOI] [PubMed] [Google Scholar]
- [40].Gravas S, Tzortzis V, Karatzas A, et al. The use of tamsulozin as adjunctive treatment after ESWL in patients with distal ureteral colic: do we really need it? Results from a randomised study. Urol Res 2007;35:231–5. [DOI] [PubMed] [Google Scholar]
- [41].De Sio M, Autorino R, Di Lorenzo G, et al. Medical expulsive treatment of distal-ureteral colics using tamsulosin: a single center experience. J Endourol 2006;20:12–6. [DOI] [PubMed] [Google Scholar]
- [42].Bhagat SK, Chacko NK, Kekre NS, et al. Is there a role for tamsulosin in shock wave lithotripsy for renal and ureteral calculi? J Urol 2007;177:2185–8. [DOI] [PubMed] [Google Scholar]
- [43].Resim S, Ekerbicer HC, Ciftci A. Role of tamsulosin in treatment of patients with steinstrasse developing after extracorporeal shock wave lithotripsy. Urology 2005;66:945–8. [DOI] [PubMed] [Google Scholar]
- [44].Giovanni LG, Alessia MC, Piero R, et al. Tamsulosin treatment increases clinical success rate of single extracorporeal shock wave lithotripsy of renal colics. Urology 2005;66:24–8. [DOI] [PubMed] [Google Scholar]
- [45].Yilmaz E, Batislam E, Basar MM, et al. The comparison and efficacy of 3 different alpha1-adrenergic blockers for distal ureteral colics. J Urol 2005; 2010-;173:2. [DOI] [PubMed] [Google Scholar]
- [46].Küpeli B, Irkilata L, Gürocak S, et al. Does tamsulosin enhance lower ureteral colic clearance with or without shock wave lithotripsy. Urology 2004;64:1111–5. [DOI] [PubMed] [Google Scholar]
- [47].Porpiglia F, Ghignone G, Fiori C, et al. Nifedipine versus tamsulosin for the management of lower ureteral colics. J Urol 2004;172:568–71. [DOI] [PubMed] [Google Scholar]
- [48].Dellabella M, Milanese G, Muzzonigro G. Randomized trial of the tamsulosin, nifedipine and phloroglucinol in medical expulsive therapy for distal ureteral calculi. J Urol 2005;174:167–72. [DOI] [PubMed] [Google Scholar]
- [49].Cervenàkov I, Fillo J, Mardiak J, et al. Speedy elimination of ureterolithiasis in lower part of ureters with the alpha 1-blocker—Tamsulosin. Int Urol Nephrol 2002;34:25–9. [DOI] [PubMed] [Google Scholar]
- [50].J Higgins and S Green. Cochrane handbook for systematic reviews of interventions version 5.1.4 (updated March 2011). The Cochrane collaboration. Available at: http://wwwcochrane-hand-/bookorg [Access date 27, 2012]. [Google Scholar]
- [51].Moher D, Liberati A, Tetzlaff J. Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Ll Kjaergard J, Villumsen C, Gluud Reported methodo logic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med 2001;135:982–9. [DOI] [PubMed] [Google Scholar]
- [53].Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of colics: what is the evidence? Eur Urol 2009;56:455–71. [DOI] [PubMed] [Google Scholar]


