ABSTRACT
Background
There is a discrepancy in the way dystonia is classified in the literature, as articles continue to reference the old criteria or fail to use the 2013 criteria correctly.
Methods
We performed a systematic review of the dystonia literature and distinguished between studies that use the new classification correctly, made errors in implementing the new classification, or continued to use the old classification methods.
Results
Of the 990 articles included in the study, 59.8% used the classification correctly, 31.3% used mixed terminology, and 8.9% continued to use the old classification. Articles relating to surgery were significantly less likely to use the new classification correctly. There is an upward trend in the annual rate of articles properly referencing the new classification.
Conclusions
The 2013 classification has been well received in scientific literature, and more studies are adapting to its use.
Keywords: Classification, Diagnosis, Dystonia
Introduction
The classification of dystonia has been revised multiple times.1, 2, 3, 4, 5 It was first categorized in 1976 by Fahn and Eldridge as primary (sporadic or hereditary), secondary (associated with hereditary, degenerative, or environmental causes), and psychological dystonia.1 In 1984, the advisory board of the Dystonia Medical Research Foundation distinguished idiopathic from symptomatic dystonia.2 However, following the discovery of the DYT1 locus,2 the term “primary” was retained instead of idiopathic, to indicate “syndromes in which dystonia is the sole phenotypic manifestation with the exception that tremor can be present as well.”5 This revised classification also introduced the concepts of dystonia‐plus and heredodegenerative dystonia.
These classifications were widely used, particularly by dystonia experts, but did not clearly distinguish phenomenology from etiology, which challenged their external value and their implementation in research contexts.6 To specifically address this concern, in 2013, an international panel of dystonia experts proposed a classification based on two axes.7 Axis I describes clinical features (age of onset, body distribution, temporal pattern, coexistence of neurological or systemic symptoms) and Axis II describes etiology (idiopathic, inherited, acquired, structural, and degenerative). By distinguishing symptomatology from etiology, the current classification attempts to provide a systematic approach to the clinical examination of dystonia and discarded several terms that were in common usages, such as “primary,” “heredodegenerative,” or “dystonia plus.” However, a formula for translating from old terminology to the new has been proposed only recently,2 and clinicians have gone five years without clear instructions on how to make the new terminology compatible with existing notes and data.
Therefore, some articles continue to reference the old criteria, or fail to use the new criteria properly. In this report, we critically review the dystonia literature to determine whether the studies published since the 2013 classification have adapted to the new terminology. We further determine the types of studies that reference the terminology incorrectly.
Methods
A search strategy was conducted using the PubMed database (www.ncbi.nlm.nih.gov/pubmed). The inclusion criteria consisted of all English language articles published after the 2013 classification, containing “dystonia” in the title, where the full text is accessible (Fig. 1A). This retrieved 1525 records. The exclusion criteria were studies that did not classify dystonia, were still in press, or were not written or translated to English. This identified 990 articles that fit the study criteria.
Figure 1.
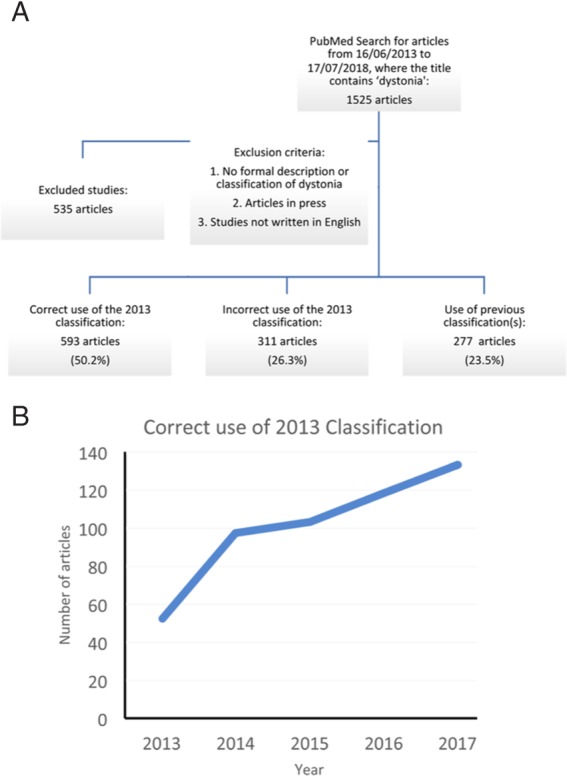
(A) Flowchart of the search strategy. (B) The number of studies with a correct usage of the 2013 classification increases annually.
The articles were read in their entirety to identify if they used the new terminology appropriately. They were separated into three groups, based on the type of errors made, including articles that referenced the new classification correctly (e.g., idiopathic generalized dystonia), incorrectly implemented the new classification (e.g., primary focal dystonia), or continued to use the old classification (e.g., primary dystonia). Articles that referenced dystonia syndromes (e.g., early‐onset dystonia‐parkinsonism, primary cervical dystonia, etc.) without further description were grouped under using the old classification.
We further divided the articles into broad subject categories, based on author interest and subspecialty, to assess if there were differences in the adaptation in the new criteria: “phenomenology,” “surgery,” (e.g., deep brain stimulation, focused ultrasound, etc.) “genetics,” “botulinum toxin,” treatment, and “other.” The latter group, “other,” included studies that did not fit into the previous categories, and instead related to physiology, biochemistry, imaging, non‐surgical therapies, rating scales or drug‐induced dystonia. To ensure reproducibility of analysis, we also grouped articles based on journal type to assess if this showed a similar trend.
Statistical Analysis
A Pearson chi‐squared test of independence was performed on the categorical data, with the significance threshold set to 0.05. The Bonferroni correction was applied to counteract the Type 1 error that arises during multiple comparisons.8 The data were analyzed using Microsoft Excel for Mac, version 15.33.
Results
Of the 990 articles included in the study, 592 (59.8%) used the classification correctly, 310 (31.3%) used mixed terminology, and 88 (8.9%) articles continued to use the old classification (Fig. 1A). Table 1 shows the distribution of articles by subject into each classification subtype. A chi‐square test revealed significant difference between these subgroups [χ2 (8, n = 15) = 33.46, P < 0.005] and post hoc z‐test on the adjusted residuals with Bonferroni correction revealed that articles relating to surgery were significantly less likely to use the new classification correctly (P < 0.003) while those in the “Other” category performed significantly better in using the new classification correctly (P < 0.003) and were less likely to the new terminology incorrectly (P < 0.003).
Table 1.
Usage of the dystonia classification by article subtype
| Phenomenology | Surgical | Genetic | Botulinum toxin | Other | |
|---|---|---|---|---|---|
| Correct use of new classification | 257 (56.6%) | 87 (48.3%)* | 117 (66.1%) | 36 (76.6%) | 95 (72%)† |
| Use of old classification | 40 (8.8%) | 25 (13.9%) | 9 (5.1%) | 2 (4.3%) | 12 (9.1%) |
| Incorrect use of new classification | 157 (34.6%) | 68 (37.8%) | 51 (28.8%) | 9 (19.1%) | 25 (18.9%)§ |
| Total | 454 | 180 | 177 | 47 | 132 |
Percentage indicates the number of articles within the same subject. Pearson chi‐square analysis shows significant difference between subgroups [χ2 (8, n = 15) = 33.46, P < 0.005]. Post hoc z‐test (with Bonferroni's correction) indicated that articles in surgery were less likely to use the new classification correctly (*P < 0.003), and articles classified under “Other” used the new classification correctly († P < 0.003) and were less likely to the new terminology incorrectly (§ P < 0.003).
When adjusted for proportion of publications, physical medicine and rehabilitation (PMR) journals most frequently used the new classification correctly (87.5%) while surgery journals (which included journals in neurosurgery, maxillofacial surgery, and otolaryngology) used it least frequently (42.5%). Of the two articles in epidemiology journals published after the 2013 criteria, both used the classification incorrectly. Surgery journals were the second most likely to do so at 45%. PMR journals were least likely to use the classification incorrectly (12.5%).
Neurology journals performed comparably in their reference to dystonia, regardless of whether it was a specialized movement disorders journal. The distribution of referencing among general neurology journals was: 61.3% correct use of classification, 32.3% incorrect use and 6.4% use of old classification. Among movement disorders journals, 62.1% used the classification correctly, 33.6% used it incorrectly, and 4.3% used the old classification.
A ratio of the number of articles that referenced the new classification correctly, divided by the total number of articles published each year, reveals an upward trend in the correct use of the 2013 classification (Figure 1B).
Discussion
Dystonia has been described more recently than other hyperkinetic disorders, and its classification has been subject to several revisions since the 1970s. The most recent update was in 2013, but the literature demonstrates considerable variety in the terminology used to describe dystonia.
We observed that a large proportion of studies (59.8%) use the 2013 classification correctly, and that there is an annual increase in the trend towards its implementation (Figure 1B).
Studies classified under “Other” were more likely to use the terminology frequently, and accurately. These included articles in physiology, biochemistry, imaging, rating scales and non‐surgical interventions of dystonia. This was comparable when the articles were divided according to journal type, with PMR journals most frequently referencing the classification correctly.
Surgical studies, by contrast, were significantly less likely to reference the 2013 classification. There are several reasons for this. Firstly, most large prospective DBS trials were initiated when the previous classification was still used.10 A diagnosis of “primary dystonia” was often the main inclusion criterion, without further differentiation of the genetic background, while patients categorized as “secondary dystonia” were excluded in several studies. The same considerations apply to reports of long‐term follow‐up data on motor outcome and quality of life in DBS patients operated on more than five years ago.11 Resistance to the new terminology may arise from difficulty in translating this classic terminology to the new. The recently published guideline for translating from old terminology may facilitate using the new classification for long‐term studies that were designed using the older definitions.2 There is a general belief that “primary” dystonia has a better post‐surgical outcome compared to “secondary” dystonia.2, 10, 11, 12 This would be translated to say that idiopathic isolated dystonia has a more favorable outcome than acquired dystonia. Using the new classification would allow to further detail such a general statement, because it is widely recognized that characterizing dystonia as thoroughly as possible is the first step in identifying predictors of surgical success (e.g., genetic etiology).12 Denominations such as “primary” served as a rather wide umbrella to rule out inherited dystonias with anatomical abnormalities visible at brain imaging.5 The group of inherited dystonias is broad, and subgrouping may be warranted, particularly when dealing with surgical registries in the pediatric population.13
The purpose of our study is to demonstrate the adaptation of the 2013 classification of dystonia. However, we recognize that its reproducibility is limited because of the categories we chose to classify publications (“phenomenology,” “surgery,” “genetics,” “botulinum toxin treatment,” and “other”). These were determined based on author interest, and served as a means of self‐reflection on the limitations to its adaptation amongst different subspecialties.
Nevertheless, it demonstrates that the 2013 update is not without its drawbacks. In an attempt to clarify the distinction between phenomenology and etiology of dystonia, the update introduces a more complex classification based on a dual axis. This carries the risk of classifying patients under multiple categories (for example, primary focal dystonia can refer to idiopathic or inherited etiologies under Axis II) and complicates the report of long‐term outcome in patients classified under the old criteria.
A similar dual‐axis paradigm has been recently implemented for tremor classification,14 suggesting a cultural shift in our field. This shift is confirmed by an improving trend of correct usage of the terminology, which is encouraging and likely reflects the successful educative efforts of the International Parkinson Disease and Movement Disorders Society. The criteria for translating from old terminology to the 2013 terminology has been published only this year,2 which can further help clarify the reasoning and implementation of the classification. So, we can be hopeful that highlighting this issue will lead to publications being more cognizant of their terminology, and ensure consistency in the dialogue about dystonia.
Author Roles
1) Research project: A. Conception, B. Organization, C. Execution; 2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; 3) Manuscript: A. Writing of the first draft, B. Review and Critique.
S.S.: 1C, 2A, 2B, 3A
A.A.: 1A, 2C, 3B
J.K.: 1A, 2C, 3B
A.F.: 1A, 1B, 2A, 2C, 3B
Disclosures
Ethical Compliance Statement: The authors confirm that the approval of an institutional review board was not required for this work. Informed consent was not required for this work. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Funding Sources and Conflict of Interest: The authors have no funding sources or conflicts of interest to report.
Financial Disclosures for previous 12 months: S.S. has no disclosures to report. A.A. receives a speaker's honoraria from Allergan, Ipsen, Merz, Medtronic, and Zambon. J.K. reports the following: consultancies with Medtronic and Boston Scientific; honoraria from Medtronic, St Jude/ Abbott, and Boston Scientific; and grants from DFG (German Research Council). A.F. reports the following: consultancies with Abbvie, Medtronic, Boston Scientific, Sunovion, Chiesi Farmaceutici, UCB, and Ipsen; advisory boards of Abbvie, Boston Scientific, and Ipsen; honoraria from Abbvie, Medtronic, Boston Scientific, Sunovion, Chiesi Farmaceutici, UCB, and Ipsen; and grants from University of Toronto, Weston Foundation, Abbvie, Medtronic, and Boston Scientific.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Fahn S, Eldridge R. Definition of dystonia and classification of the dystonic states. Adv Neurol 1976;14:1–5. [PubMed] [Google Scholar]
- 2. Albanese A, Di Giovanni M, Lalli S. Dystonia: diagnosis and management. Eur J Neurol 2019;26(1):5–17. [DOI] [PubMed] [Google Scholar]
- 3. Marsden CD. Dystonia: the spectrum of the disease. Res Publ Assoc Res Nerv Ment Dis 1976;55:351–367. [PubMed] [Google Scholar]
- 4. Fahn S, Marsden CD, Calne DB. Classification and investigation of dystonia In: Marsden CD, Fahn S, eds. Movement disorders 2 London: Butterworths; 1987:332–358. [Google Scholar]
- 5. Fahn S, Bressman SB, Marsden CD. Classification of dystonia. Adv Neurol 1998;78:1–10. [PubMed] [Google Scholar]
- 6. Balint B, Bhatia KP. Dystonia: an update on phenomenology, classification, pathogenesis and treatment. Curr Opin Neurol 2014;27(4):468–476. [DOI] [PubMed] [Google Scholar]
- 7. Albanese A, Bhatia K, Bressman SB, DeLong MR, Fahn S, Fung VS, Hallett M, Jankovic J, Jinnah HA, Klein C, Lang AE. Phenomenology and classification of dystonia: a consensus update. Mov Disord 2013;28:863–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ 1995;310(6973):170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marras C, Lang A, van de Warrenburg BP, et al. Nomenclature of genetic movement disorders: recommendations of the International Parkinson and Movement Disorder Society task force. Mov Disord 2017;32:724–725. [DOI] [PubMed] [Google Scholar]
- 10. Volkmann J, Mueller J, Deuschl G, et al. Pallidal neurostimulation in patients with medication‐refractory cervical dystonia: a randomised, sham‐controlled trial. Lancet Neurol 2014. Sep;13(9):875–884. [DOI] [PubMed] [Google Scholar]
- 11. Hogg E, During E, E Tan E, et al. Sustained quality‐of‐life improvements over 10 years after deep brain stimulation for dystonia. Mov Disord 2018. Jul;33(7):1160–1167. [DOI] [PubMed] [Google Scholar]
- 12. Beaulieu‐Boire I, Aquino CC, Fasano A, et al. Deep brain stimulation in rare inherited dystonias. Brain Stimul 2016;9(6):905–910. [DOI] [PubMed] [Google Scholar]
- 13. Koy A, Weinsheimer M, Pauls KAM, et al. German registry of paediatric deep brain stimulation in patients with childhood‐onset dystonia (GEPESTIM). Eur J Paediatr Neurol 2017;21(1):136–146. [DOI] [PubMed] [Google Scholar]
- 14. Bhatia KP, Bain P, Bajaj N, et al. Consensus statement on the classification of tremors. from the task force on tremor of the International Parkinson and Movement Disorder Society. Mov Disord. 2018;33(1):75–87. [DOI] [PMC free article] [PubMed] [Google Scholar]


