Supplemental Digital Content is Available in the Text.
Key Words: PrEP, adherence, MSM, Black MSM, Hispanic, HIV prevention
Abstract
Background:
HPTN 067 assessed the feasibility of daily and non-daily dosing of open-label emtricitabine/tenofovir disoproxil fumarate (FTC/TDF)-based pre-exposure prophylaxis (PrEP).
Methods:
Factors associated with sex-related PrEP adherence were assessed among men who have sex with men (MSM) randomized to one of 3 PrEP dosing arms in HPTN 067 in New York City. Sex-related PrEP adherence was defined per protocol as at least 1 PrEP tablet taken within 4 days pre-sex and at least 1 additional PrEP tablet taken within 24 hours post-sex, assessed via electronic drug monitoring and weekly interviews. Demographic data and behavioral measures were evaluated for association with sex-related PrEP adherence. Logistic regression for clustered data was used to estimate the unadjusted and adjusted odds ratios.
Results:
Of 176 randomized MSM participants, 59% were Black, 10% White, 25% Hispanic, and 6% other; median age was 31 years. In the multivariable analyses, higher sex-related PrEP adherence was significantly associated with daily dosing arm, older age, employment, and higher PrEP adherence behavioral skills. Lower sex-related PrEP adherence was significantly associated with identifying as Black or Hispanic (compared with White), opiate use, and reporting “I forgot” as an adherence barrier.
Conclusions:
This analysis identified populations of MSM who might benefit from additional support to optimize PrEP adherence, including those who are younger, unemployed, or opiate users. MSM with lower PrEP behavioral skills may benefit from targeted interventions. Further study is needed to assess racial and ethnic disparities in PrEP adherence, which may reflect broader social and economic inequalities not captured in this study.
INTRODUCTION
Men who have sex with men (MSM) account for most of the new HIV infections in the United States, with Black MSM, in particular, being disproportionately affected.1,2 Emtricitabine/tenofovir disoproxil fumarate (FTC/TDF)-based pre-exposure prophylaxis (PrEP) is an effective HIV prevention tool with great potential for reducing new infections among MSM.3–8 Whereas PrEP awareness has been increasing in the United States since its initial approval in 2012 and the release of national guidelines in 2014,9 the estimates of its use among populations at risk remain low.10–14
Among those who initiate PrEP, the suboptimal adherence has been shown to limit its effectiveness.5 Factors associated with adherence to PrEP are not well understood and may vary in different populations. Some factors that have been identified as potential contributors to suboptimal PrEP adherence include younger age,15 lower education levels,15 unstable housing,8 side effects,16 and stigma.16–18 Additional reasons for missing doses reported by PrEP users have included being away from home or busy.16 Barriers to long-term PrEP use have included concern over long-term toxicity, the cost of PrEP medication and medical visits, and simply forgetting to take daily pills.18,19 Some studies have noted racial disparities with lower drug concentrations in US Black participants,8,16 which remains poorly understood. It is critically important to understand barriers to PrEP adherence for key populations most affected by HIV in the United States, particularly Black MSM. Understanding the factors associated with PrEP adherence among US MSM can inform future prevention support interventions to maximize the benefit of PrEP.
This current study uses data from US MSM participants enrolled in the New York City (NYC) site of HPTN 067, the ADAPT study, a feasibility study comparing daily to intermittent dosing regimens of FTC/TDF PrEP for individuals at risk for HIV acquisition. The ADAPT study was also conducted at 2 other sites (Bangkok and Cape Town); each site was powered to be analyzed independently. The New York and Bangkok sites enrolled at-risk MSM and transgender women (TGW), whereas Cape Town enrolled at-risk heterosexual women. Participants at each site were randomized 1:1:1 to one of 3 open-label PrEP dosing strategies: daily, time driven (twice weekly with an additional dose post-sex events), and event driven (pre- and post-sex events). Among MSM and TGW participants in HPTN 067, participants at the US site in Harlem, NYC, had lower adherence in general, and also specifically before and after sex events (termed PrEP “coverage” of sex events, or sex-related PrEP adherence), when compared with the other HPTN 067 MSM and TGW cohort in Bangkok, Thailand.20 As reported previously, NYC participants assigned to daily PrEP dosing were able to adhere to pre- and post-sex dosing for 66% of sex events over the 24-week study period compared with 47% for those in the time-driven arm and 52% for those in the event-driven arm. By contrast, Thai participants adhered to pre- and post-sex PrEP dosing for 85% of sex events in the daily arm, 84% in the time-driven arm, and 74% in the event-driven arm (P < 0.0001 for NYC vs. Bangkok results). In the placebo-controlled IPERGAY trial for comparison, the self-reported adherence to pre- and post-sex dosing of on-demand PrEP, which would be similar to the event-driven arm in this trial, was 43%.3
The current analysis of HPTN 067 data from the New York site was conducted to gain additional insight about factors that may have contributed to low PrEP adherence surrounding sexual events among US MSM. Because the 3 study sites enrolled such different populations, only the NYC participants were included in the current analysis to focus on the issues relevant to US MSM.
METHODS
The HPTN 067/ADAPT study procedures have been previously described in detail.20,21 Briefly, the study participants were randomized 1:1:1 to 24 weeks of one of 3 self-administered FTC/TDF PrEP dosing strategies, designed based on the available animal and human data at the time of study initiation,5,22–24 including (1) daily arm—1 TDF/FTC pill daily; (2) time-driven arm—1 TDF/FTC pill taken twice a week, plus 1 FTC/TDF pill within 2 hours post-sex; or (3) event-driven arm—1 TDF/FTC pill 24–48 hours pre-sex and 1 additional FTC/TDF pill within 2 hours post-sex. Participant study visits occurred every 4 weeks while receiving self-administered PrEP. The trial was conducted in 3 sites: Cape Town, South Africa; Bangkok, Thailand; and New York, NY, USA. Cape Town enrolled heterosexual young women, whereas the Bangkok and New York sites enrolled MSM and TGW. Each site was powered independently for separate analyses. The trial was performed with informed consent and followed all guidelines for experimental investigation with human subjects required by the institutions with which the authors are affiliated. Study procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. The protocol was registered at ClinicalTrials.gov (NCT01327651; https://www.hptn.org/research/studies/82).
For the 2 sites (NYC and Bangkok) that enrolled MSM and TGW, HIV-uninfected men and TGW aged 18 years or above with normal renal function and no acute or chronic hepatitis B were eligible for the study if they reported anal and/or receptive neovaginal intercourse with a man or TGW in the past 6 months and reported at least one additional risk factor in the past 6 months: (1) sexual intercourse with more than 1 man or TGW, (2) a history of an acute sexually transmitted infection, (3) sex in exchange for money, goods, or favors, and/or (4) condomless intercourse (oral, anal, vaginal, or neovaginal) with a partner known to be HIV infected or of unknown HIV infection status.20
US participants were recruited from the Harlem Prevention Center Clinical Research Site located in central Harlem in NYC, an area with one of the highest rates of HIV diagnoses and HIV prevalence (2.8%) in NYC.25
Data Collection
Demographic data were collected from participants by site research staff.20,21 Other baseline data were collected from participants via computer-assisted self-interview (CASI), including depressive symptoms via Center for Epidemiologic Studies Depression Scale (CES‐D) (score of ≥16 suggestive of symptomatic depression),26 alcohol use via AUDIT alcohol use scale (score of ≥8 considered hazardous and harmful drinking),27 and other substance use including stimulants and opiates.
Information, Motivation, and Behavioral (IMB) Skills28 measures were adapted to PrEP use and were included in the CASI. The items were structured around the LifeWindows Information Motivation Behavioral Skills Adherence Assessment Questionnaire to reflect the IMB model of health behavior applied specifically to PrEP use.29–31 For example, participants were asked to rate on a 5-point Likert scale their agreement or disagreement with several statements related to PrEP information (total information score range: 0–6), including “I know how study pills are supposed to be taken.” Similarly, several CASI items assessed the level of PrEP motivation (score range: 0–32), including “I do not like taking the study pills,” and PrEP behavioral skills (score range: 0–32), including answering “How difficult or easy is it to make the study pills part of my routine” (see Appendix for further details, Supplemental Digital Content, http://links.lww.com/QAI/B278).
Follow-up CASI questionnaires included items assessing participant knowledge, attitudes, and behavior related to PrEP and their assigned dosing arm, stigma, PrEP adherence, and barriers and facilitators of PrEP adherence. Study-specific items assessing optimistic attitude toward PrEP and the extent to which participants perceived their assigned regimen fit their daily life were included in the CASI measure. Optimistic attitude toward PrEP was defined with a 5-point Likert response (strongly agree to strongly disagree) to a single item (“If I am taking the study pills I would worry less about HIV”). Participants were also asked about their regimen's fit to daily life (“How well does this recommended (prescribed) schedule fit your life?”) with a 5-point Likert scale (good fit, somewhat good fit, neither a good or bad fit, somewhat bad fit, bad fit).
During monthly follow-up study visits, participants were assessed by research staff for symptoms and medication side effects and had laboratory monitoring including HIV testing.
Study Outcome
The primary outcome in HPTN 067 and in the current analysis was adherence to FTC/TDF PrEP dosing before and after anal, vaginal, or neovaginal intercourse (sex) events, defined as the participant taking at least 1 PrEP dose (1 FTC/TDF tablet) within 96 hours (4 days) pre-sex and also taking another dose within 24 hours (1 day) post-sex. This definition was based on the available human and non-human primate data at the time of study design, which suggested that twice-weekly dosing was protective.32,33 All sex events with any penile intromission, regardless of condom use, were included. Oral sex events are not included in these analyses. Note that sex-related PrEP adherence was defined per the protocol before the release of evidence for the efficacy of another intermittent dosing regimen (“on-demand” PrEP) for FTC/TDF-based PrEP.3
Pill-taking data were collected through electronic drug monitoring (EDM) using a Wisepill device. Participants were interviewed weekly to verify or adjust information from the Wisepill device and to report details on sex events, including sex date and time, type, condom use, and partner’s HIV status.20
Statistical Analysis
To evaluate the association between sex-related PrEP adherence and covariates among MSM participants, logistic regression for clustered data (generalized estimating equations) with robust standard errors were used. Although the study aimed to enroll both MSM and TGW, only 3 of the 179 randomized participants (1.7%) at the NYC site were TGW, which limited the ability to identify the associations specific for that population. Given this limitation, this study included analyses restricted to the 176 NYC MSM participants. Variables considered in the univariate analysis included randomization arm, age, race, education, employment, alcohol use, depressive symptoms, drug use, perceived drug use as a problem, side effects, PrEP-related IMB scale scores, report of any condomless anal intercourse in the past 3 months, exchange sex, perceived vulnerability to HIV, unrealistic HIV optimism, PrEP optimism, PrEP regimen fit to daily life, not having study pills when away from home, confusion about medication instructions, inability to forecast sex, lack of privacy for taking study pill, concern others would think participant had HIV, perceived efficacy of PrEP, able to take study pills as directed when changes in routine, satisfaction with prescribed schedule, forgetfulness, and whether PrEP schedule was changed by the participant from what was prescribed. All scales were treated as continuous variables.
Variables significant at P value of <0.1 were considered in a multivariable analysis. Variables were kept in the final model if P value was <0.05. Individuals were censored after HIV seroconversion. All analyses were conducted in SAS software (version 9.4; SAS Institute Inc., Cary, NC).
To better understand the relationship between race/ethnicity and sex-related PrEP adherence, a post-hoc analysis was conducted, in which a group of CASI items was selected based on the adherence and racial disparity literature, including substance use, alcohol use, depression score, HIV risk behavior, study acceptability, perceived vulnerability to HIV, and PrEP barriers and facilitators. To assess the potential confounding effect from these CASI variables on the association between race/ethnicity and sex-related PrEP adherence, each variable was added into the final multivariable model respectively, and the odds ratio (OR) for race/ethnicity in the augmented model was compared with the OR for race/ethnicity in the multivariate model to determine whether a meaningful change occurred. ORs and adjusted odds ratios (aORs) are presented with 95% confidence intervals (95% CI).
RESULTS
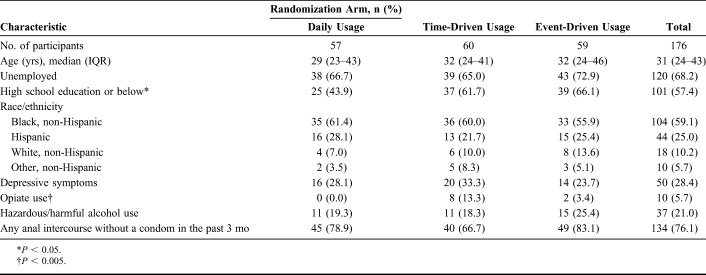
At the NYC site of the HPTN 067/ADAPT study, 176 MSM participants were randomized (from 2013 to 2014) 1:1:1 to one of the 3 PrEP dosing strategy arms: daily, time-driven, or event-driven dosing.20 Baseline characteristics of the 176 randomized MSM participants included 59% who self-identified as non-Hispanic Black, 25% Hispanic, and 10% White; median age was 31 years [interquartile range (IQR), 24–43]; 68% were unemployed (Table 1). About 6% of participants reported opiate use and 21% reported hazardous or harmful alcohol use. More than 1 in 4 reported depressive symptoms. Participant characteristics were similar across the 3 study arms, except for education and opiate use that were associated with arm assignment (P < 0.05 and P < 0.005, respectively).
TABLE 1.
Baseline Characteristics of New York HPTN 067 MSM Participants
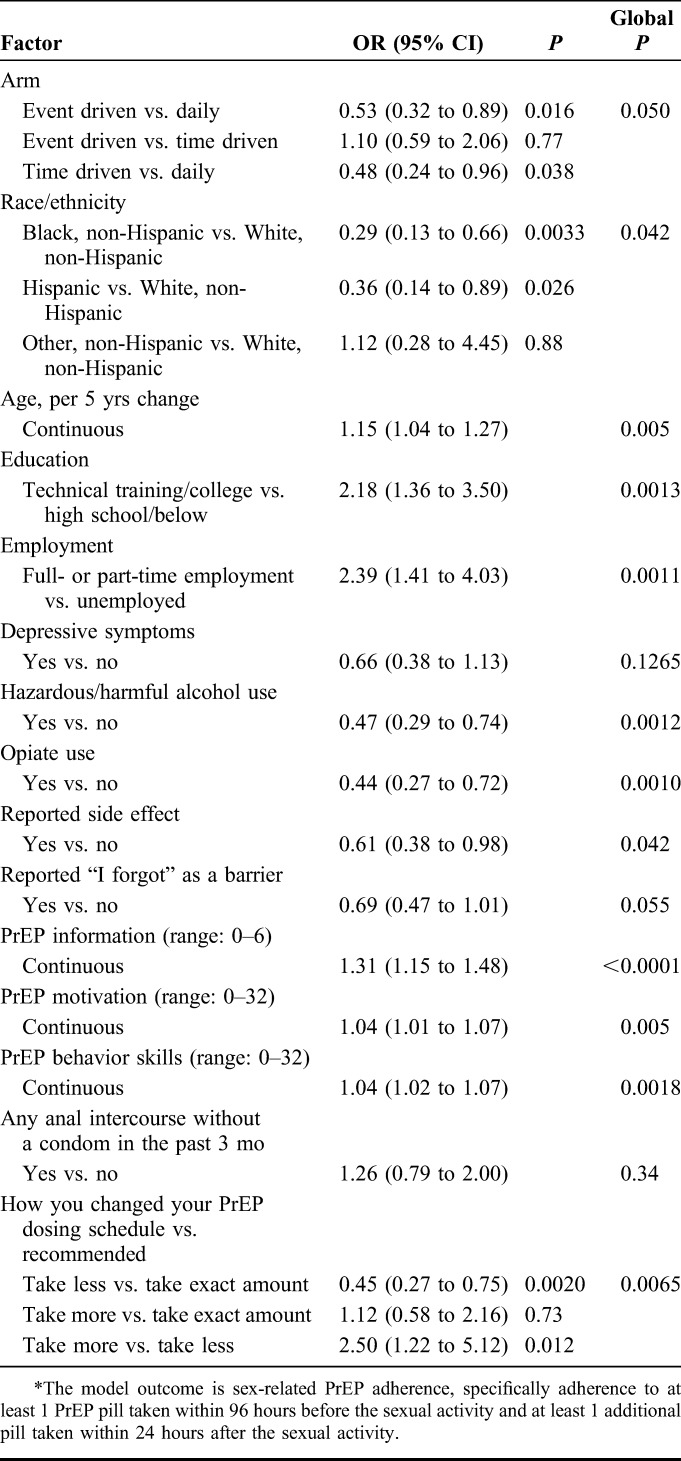
In the univariate analyses (Table 2), factors significantly associated with higher sex-related PrEP adherence included older age; higher education; employment; having higher scores in PrEP motivation, PrEP information, and PrEP behavioral skills; and self-report of intentionally changing one's assigned PrEP regimen schedule to take more than recommended (compared with those reporting taking less than recommended). Factors significantly associated with lower sex-related PrEP adherence included randomization to the non-daily arms (both event- and time-driven arms when compared with daily arm); identifying as Black, non-Hispanic (compared with White, non-Hispanic) or as Hispanic (vs. White, non-Hispanic); hazardous/harmful alcohol use; opiate use; reported side effect; and participant self-report of changing assigned PrEP schedule to take less than recommended (compared with those reporting taking exact amount as recommended). Reporting “I forgot” as a reason for missed doses was also included in the multivariate model (P < 0.1). The following additional factors were not included in the multivariable analysis because they were not associated with sex-related PrEP adherence in the univariate analyses (P ≥ 0.1): depressive symptoms, reports of any anal intercourse without a condom in the past 3 months, exchange sex, unrealistic HIV optimism, stimulant use, popper use, Methadone use, perceived drug use as a problem, neurologic side effects, gastrointestinal side effects, not having pill when away from home, confusion about medication instructions, inability to forecast sex, lack of privacy for taking pill, concern others would think participant had HIV, perceived vulnerability to HIV, perceived efficacy of PrEP, PrEP optimism, regimen fit to daily life, able to take pills as directed when changes in routine, and satisfaction with prescribed schedule.
TABLE 2.
Factors Associated With Sex-Related PrEP Adherence: Univariate Analysis*
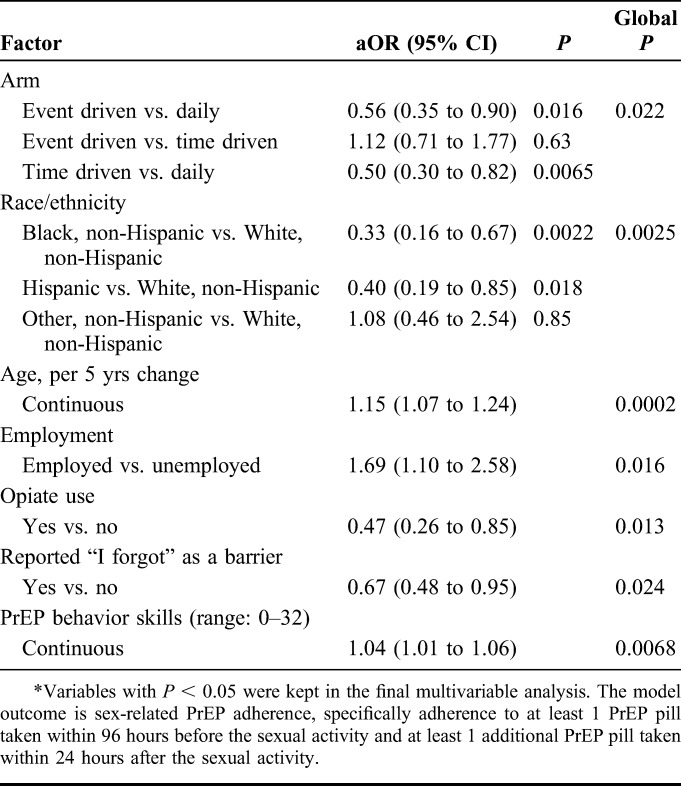
All factors associated with sex-related PrEP adherence in the univariate analysis at P value of < 0.1 as described previously were considered in the multivariable analysis. Both factors that differed by study arm (education and opiate use) were among the factors considered; opiate use remained significant (P < 0.05), whereas education did not. Forcing education into the model did not meaningfully change the results (data not shown). Several other factors remained significantly associated (P < 0.05) with sex-related PrEP adherence in the multivariable analysis, including assigned PrEP dosing arm, race/ethnicity, age, employment, reporting “I forgot” as a barrier to PrEP adherence, and PrEP behavioral skills (Table 3). Specifically, participants assigned to either the event- or time-driven intermittent dosing arms had lower sex-related PrEP adherence when compared with those assigned to the daily dosing arm (aOR 0.56, 95% CI: 0.35 to 0.90, and aOR 0.50, 95% CI: 0.30 to 0.82, respectively). Lower sex-related PrEP adherence was also significantly associated with opiate use (aOR 0.47, 95% CI: 0.26 to 0.85) and reporting “I forgot” as a barrier to PrEP adherence (aOR 0.67, 95% CI: 0.48 to 0.95). Sex-related PrEP adherence differed by race/ethnicity, with lower sex-related PrEP adherence occurring among both Black, non-Hispanic and Hispanic participants when compared with White, non-Hispanic participants (aOR 0.33, 95% CI: 0.16 to 0.67, and aOR 0.40, 95% CI: 0.19 to 0.85, respectively). The lower sex-related PrEP adherence seen among Black and Hispanic participants remained even after adjusting for age, employment, randomization arm, opiate use, and PrEP behavioral skills. Greater sex-related PrEP adherence was significantly associated with older age (aOR 1.15, 95% CI: 1.07 to 1.24), being employed (aOR 1.69, 95% CI: 1.10 to 2.58), and scoring higher in PrEP behavioral skills (aOR 1.04, 95% CI: 1.01 to 1.06).
TABLE 3.
Factors Associated With Sex-Related PrEP Adherence: Multivariable Analysis*
In the post-hoc analysis, the lower sex-related PrEP adherence among Black, non-Hispanic and Hispanic MSM when compared with White, non-Hispanic MSM remained significant after adjustment for any of the pre-selected CASI items (data not shown). Thus, the significant racial/ethnic differences in sex-related PrEP adherence were seen even after controlling for participants' age, employment, randomization arm, substance use, alcohol use, depressive symptoms, side effects, perceived vulnerability to HIV, reported barriers to PrEP use (including reporting being worried about others knowing about the use of PrEP), PrEP behavioral skills, and indicators of poverty (exchange sex, reporting best part of the study was financial incentives).
DISCUSSION
This analysis identified several factors that were associated with adherence to pre- and post-sex PrEP doses among MSM HPTN 067 study participants in NYC, USA. As reported previously for this cohort, daily dosing of PrEP was associated with the highest sex-related PrEP adherence, when compared with either of the non-daily PrEP dosing arms (time- and event-driven arms).20 In this analysis, higher sex-related PrEP adherence was also more likely among participants who were older and employed and who had better PrEP behavioral skills as scored by the study IMB questionnaire. Lower sex-related PrEP adherence of sex events was more likely among Black and Hispanic participants than among White participants, opiate users, MSM randomized to one of the non-daily dosing arms, and MSM reporting “I forgot” as a factor making it harder to adhere.
Many of the findings in this study are consistent with the growing literature on PrEP experiences in different populations. Younger age and lower education level have been associated with poorer adherence in previous PrEP studies.13,15 Other social determinants, including income and unstable housing, have also been previously shown to negatively affect PrEP adherence.8,19 Previous studies have had varied findings in terms of the association between substance use and PrEP use/adherence among US MSM, ranging from a positive association, no association, to an inverse relationship. For example, popper use has been associated with higher PrEP uptake in one study of young Black MSM.19 No association between substance use and PrEP adherence was noted in another study,34 whereas the number of substances used (polysubstance use) and the severity of substance use were both associated with lower PrEP adherence levels in a third study.35 Of note, the benefit of PrEP for reducing the risk of HIV infection among injection drug users was first published during the conduct of HPTN 067,36 though studies have shown that there is still limited knowledge of PrEP among people who inject drugs.37
Racial disparities in PrEP awareness, uptake, and adherence have been described previously among US Black MSM.8,11,13,15,19,38–40 Racial differences in PrEP adherence have also been previously noted in PrEP demonstration projects and in large cohorts of PrEP recipients in clinical practice.8,16,41,42 In addition to finding lower adherence to pre- and post-sex PrEP doses among Black MSM, our study also found lower sex-related PrEP adherence among Hispanic MSM participants. In our additional post-hoc analyses, the overall global adherence differences between racial/ethnic groups persisted after adjustment for the numerous variables assessed. Additionally, none of the variables eliminated the adherence difference between Black, non-Hispanic or Hispanic participants and White, non-Hispanic participants. Unfortunately, the study assessments did not specifically ask about perceived discrimination or racism which may have been the contributing factors.
In this clinical trial setting, lower PrEP adherence was not due to the cost of medication or access to care—issues identified as barriers in other studies,14,19,43,44 as the PrEP was provided by the study and participants were reimbursed for transportation costs. Other adherence barriers not directly measured in this study may have played a role, such as competing priorities, poverty, health literacy, perceived racism, and/or stigma. PrEP-related stigma has been described as an individual's being perceived (or fear of perception) as HIV infected or as promiscuous when taking PrEP.45 PrEP stigma has been reported to affect PrEP uptake and adherence and also to contribute to PrEP discontinuation.18,46 The research team for this study site was racially diverse and included community members with similar backgrounds to participants, which is recommended for eliminating racial and ethnic disparities in health outcomes.47 As with other examples of racial health disparities, the findings in this study may reflect the broader context of social and economic inequalities in the United States.
The finding of an association between behavioral skills and sex-related PrEP adherence is encouraging, as this is something that is measurable and can potentially be improved on with skills building interventions.48,49 Consistent with the IMB model,28 behavioral skills are thought to be the mediator for the influence of information and motivation on behavior—in this case, adherence to pre- and post-sex PrEP dosing. To assess behavioral skills specific to PrEP use, participants were asked about the ease or difficulty of PrEP pill-taking behavior (swallowing pills), planning and preparation behaviors (having medication on hand when needed), and dosing in specific situations (when drinking alcohol or using drugs, feeling side effects, or routine interruptions). IMB model–based interventions to support PrEP-related decision making, uptake, and optimal use may be helpful in promoting PrEP adherence, particularly if situated to also address affective and structural levels of influence.50
In this study, reporting “I forgot” was associated with lower sex-related PrEP adherence. Simply forgetting is one of the most commonly reported reasons for missed PrEP doses16 and also missed doses of other medication.51,52 In previous studies, however, forgetting was reported at similarly high frequencies for those with higher and lower adherence rates51 and was not correlated with outcomes such as lack of viral suppression in antiretroviral adherence in the treatment of HIV.53
Other participant characteristics (including harmful or hazardous alcohol use and less education) were associated with lower sex-related PrEP adherence in unadjusted analyses but did not remain significant as independent predictors in the adjusted analysis. One factor associated with uptake and adherence in previous PrEP trials8,13,15,19 but not seen in our study was sexual risk.
A strength of this study includes its focus on one of the populations most at risk for HIV in the United States: young Black and Hispanic MSM living in a high HIV prevalence area.54 This study was conducted in NYC, which remains an epicenter for HIV in the United States. In addition, much of the data were collected via CASI, meant to overcome social desirability.55,56 Another strength of the study was the detailed assessment of adherence. Sex-related PrEP adherence was ascertained using EDM data on pill box opening, which was adjusted by weekly participant interviews to obtain recall of sex events and verification if pill box openings represented ingested medication and/or whether any additional doses not documented by the EDM were taken (eg, whether doses were pocketed).20 Sex-related PrEP adherence measured using the Wisepill electronic monitoring device in HPTN 067 has been shown to be moderately to highly correlated with other objective measures, including plasma and hair FTC/TDF drug concentrations.57,58 However, Wisepill had its limitations, with 10%–12% of HPTN 067 participants reporting that the Wisepill device was the worst part of being in the study.59 In addition, Wisepill and interview data were more likely to be missing for NYC participants when compared with plasma for drug concentration. Reasons for missing Wisepill or interview data included loss or confiscation of the device, lack of signal or battery issues, lack of Wisepill use (concern about size, privacy, stigma), and lack of cell phone minutes.
Additional limitations that should be noted to contextualize our findings include our focus in this study on the MSM NYC HPTN 067 participants given the small number of TGW enrolled and randomized at the NYC site. The number of TGW enrolled was too small to draw any specific conclusions about the predictors of PrEP adherence in that population. In addition, HPTN 067 did not collect detailed information about perceived and experienced racism, discrimination, or stigma—factors that may have contributed to the racial and ethnic differences in adherence. Other unmeasured factors such as poverty and structural barriers likely also contributed to the racial and ethnic disparities. Also, although this study cohort represents one of the target populations for HIV prevention efforts in the United States, the findings may not be generalizable to all US MSM. In addition, sex-related PrEP adherence in this study may not necessarily be the same as effective PrEP adherence, based on the protocol-defined intermittent PrEP dosing regimens used in the HPTN 067 study.
CONCLUSIONS
Encouragingly, MSM in New York adhered to the open-label PrEP provided through this study. The results highlight specific populations of MSM in NYC who might benefit from interventions to optimize adherence to PrEP, particularly those who are younger, unemployed, Black, Hispanic, or opiate users. Further study is needed to better understand the causes of the racial and ethnic disparities in PrEP adherence seen in this study. To ensure that those most at risk for HIV can benefit fully from PrEP, supportive programs that offer theory-based education and skills building within the context of wrap-around services for a diversity of issues that disrupt daily living (racism, low/no income, low/no employment, unstable housing) may be needed.
Supplementary Material
ACKNOWLEDGMENTS
The authors are grateful to the HPTN 067/ADAPT study participants who shared their time so generously and the staff of the Harlem Prevention Center, New York, NY. The authors also acknowledge and appreciate the feedback from the HPTN 067/ADAPT study publications committee.
Footnotes
Supported by award numbers UM1 AI068619, UM1 AI068613, and RO1 AI118575 from the National Institutes of Health (NIH): NIAID, National Institute of Mental Health, and National Institute on Drug Abuse. Gilead Sciences donated study medication to the NIH to support this study.
Presented in part at the 8th IAS Conference on HIV Pathogenesis, Treatment, & Prevention (IAS 2015); July 19–22, 2015; Vancouver, Canada.
S.M. has been a site investigator for a clinical trial funded by Gilead Sciences to NYC Health + Hospitals (2016 till present). K.R.A. has received an unrestricted educational grant to the University of Michigan from Gilead Sciences (2015). R.M.G. has been a site investigator for clinical trials funded by ViiV/GSK and Gilead Sciences to the Gladstone Institutes and the San Francisco AIDS Foundation. The remaining authors have no funding or conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
REFERENCES
- 1.Centers for Disease Control and Prevention. Epidemiology of HIV Infection Through 2015; 2016. Available at: https://www.cdc.gov/hiv/pdf/library/slidesets/cdc-hiv-surveillance-genepi.pdf. Accessed May 28, 2017. [Google Scholar]
- 2.Maulsby C, Millett G, Lindsey K, et al. HIV among Black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2014;18:10–25. [DOI] [PubMed] [Google Scholar]
- 3.Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 Infection. N Engl J Med. 2015;373:2237–2246. [DOI] [PubMed] [Google Scholar]
- 4.McCormack S, Dunn DT, Desai M, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387:53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desai K, Sansom SL, Ackers ML, et al. Modeling the impact of HIV chemoprophylaxis strategies among men who have sex with men in the United States: HIV infections prevented and cost-effectiveness. AIDS. 2008;22:1829–1839. [DOI] [PubMed] [Google Scholar]
- 7.Juusola JL, Brandeau ML, Owens DK, et al. The cost-effectiveness of preexposure prophylaxis for HIV prevention in the United States in men who have sex with men. Ann Intern Med. 2012;156:541–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu AY, Cohen SE, Vittinghoff E, et al. Preexposure prophylaxis for HIV infection integrated with municipal- and community-based sexual health services. JAMA Intern Med. 2016;176:75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2014: a clinical practice guideline. Available at: http://www.cdc.gov/hiv/pdf/guidelines/PrEPguidelines2014.pdf. Accessed March 12, 2018.
- 10.Eaton LA, Driffin DD, Bauermeister J, et al. Minimal awareness and stalled uptake of pre-exposure prophylaxis (PrEP) among at risk, HIV-negative, Black men who have sex with men. AIDS Patient Care STDs. 2015;29:423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garnett M, Hirsch-Moverman Y, Franks J, et al. Limited awareness of pre-exposure prophylaxis among black men who have sex with men and transgender women in New York city. AIDS Care. 2018;30:9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khanna AS, Michaels S, Skaathun B, et al. Preexposure prophylaxis awareness and use in a population-based sample of young Black men who have sex with men. JAMA Intern Med. 2016;176:136–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mayer KH, Oldenburg CE, Novak DS, et al. Early adopters: correlates of HIV chemoprophylaxis use in recent online samples of US men who have sex with men. AIDS Behav. 2016;20:1489–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strauss BB, Greene GJ, Phillips G, II, et al. Exploring patterns of awareness and use of HIV pre-exposure prophylaxis among young men who have sex with men. AIDS Behav. 2017;21:1288–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grant RM, Anderson PL, McMahan V, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14:820–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hosek SG, Rudy B, Landovitz R, et al. An HIV preexposure prophylaxis demonstration project and safety study for young MSM. J Acquir Immune Defic Syndr. 2017;74:21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haire BG. Preexposure prophylaxis-related stigma: strategies to improve uptake and adherence—a narrative review. HIV AIDS (Auckl). 2015;7:241–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu A, Cohen S, Follansbee S, et al. Early experiences implementing pre-exposure prophylaxis (PrEP) for HIV prevention in San Francisco. PLoS Med. 2014;11:e1001613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holloway IW, Dougherty R, Gildner J, et al. Brief report: PrEP uptake, adherence, and discontinuation among California YMSM using geosocial networking applications. J Acquir Immune Defic Syndr. 2017;74:15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grant RM, Mannheimer S, Hughes JP, et al. Daily and nondaily oral preexposure prophylaxis in men and transgender women who have sex with men: the human immunodeficiency virus prevention trials network 067/ADAPT study. Clin Infect Dis. 2018;66:1712–1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bekker LG, Roux S, Sebastien E, et al. Daily and non-daily pre-exposure prophylaxis in African women (HPTN 067/ADAPT Cape Town Trial): a randomised, open-label, phase 2 trial. Lancet HIV. 2018;5:e68–e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367:399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367:423–434. [DOI] [PubMed] [Google Scholar]
- 24.Garcia-Lerma JG, Otten RA, Qari SH, et al. Prevention of rectal SHIV transmission in macaques by daily or intermittent prophylaxis with emtricitabine and tenofovir. PLoS Med. 2008;5:e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.New York City Department of Health and Mental Hygiene. New York City HIV/AIDS Annual Surveillance Statistics. New York, NY: Available at: http://www1.nyc.gov/site/doh/data/data-sets/hiv-aids-annual-surveillance-statistics.page. Accessed November 15, 2017. [Google Scholar]
- 26.Radloff L. The CES-D scale. A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 27.Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction. 1993;88:791–804. [DOI] [PubMed] [Google Scholar]
- 28.Fisher WA, Fisher JD, Harman J. The information–motivation– behavioral skills model: a general social psychological approach to understanding and promoting health behavior. In: Suls J, Wallston KA, eds. Social Psychological Foundations of Health and Illness . Hoboken, NJ: Wiley Blackwell; 2003. [Google Scholar]
- 29.Amico KR, Mansoor LE, Corneli A, et al. Adherence support approaches in biomedical HIV prevention trials: experiences, insights and future directions from four multisite prevention trials. AIDS Behav. 2013;17:2143–2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amico KR, McMahan V, Goicochea P, et al. Supporting study product use and accuracy in self-report in the iPrEx study: next step counseling and neutral assessment. AIDS Behav. 2012;16:1243–1259. [DOI] [PubMed] [Google Scholar]
- 31.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–474. [DOI] [PubMed] [Google Scholar]
- 32.Anderson PL, Glidden DV, Liu A, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4:151ra125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garcia-Lerma JG, Cong ME, Mitchell J, et al. Intermittent prophylaxis with oral truvada protects macaques from rectal SHIV infection. Sci Transl Med. 2010;2:14ra14. [DOI] [PubMed] [Google Scholar]
- 34.Hoenigl M, Jain S, Moore D, et al. Substance use and adherence to HIV preexposure prophylaxis for men who have sex with men. Emerg Infect Dis. 2018;24:2292–2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pasipanodya EC, Jain S, Sun X, et al. Trajectories and predictors of longitudinal preexposure prophylaxis adherence among men who have sex with men. J Infect Dis. 2018;218:1551–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381:2083–2090. [DOI] [PubMed] [Google Scholar]
- 37.Bazzi AR, Biancarelli DL, Childs E, et al. Limited knowledge and mixed interest in pre-exposure prophylaxis for HIV prevention among people who inject drugs. AIDS Patient Care STDs. 2018;32:529–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arnold T, Brinkley-Rubinstein L, Chan PA, et al. Social, structural, behavioral and clinical factors influencing retention in pre-exposure prophylaxis (PrEP) care in Mississippi. PLoS One. 2017;12:e0172354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuhns LM, Hotton AL, Schneider J, et al. Use of pre-exposure prophylaxis (PrEP) in young men who have dex with men is asssociated with race, sexual risk behavior and peer network size. AIDS Behav. 2017;21:1376–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marks SJ, Merchant RC, Clark MA, et al. Potential healthcare insurance and provider barriers to pre-exposure prophylaxis utilization among young men who have sex with men. AIDS Patient Care STDs. 2017;31:470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marcus JL, Hurley LB, Hare CB, et al. Preexposure prophylaxis for HIV prevention in a large integrated health care system: adherence, renal safety, and discontinuation. J Acquir Immune Defic Syndr. 2016;73:540–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van Epps P, Maier M, Lund B, et al. Medication adherence in a nationwide cohort of veterans initiating pre-exposure prophylaxis (PrEP) to prevent HIV infection. J Acquir Immune Defic Syndr. 2018;77:272–278. [DOI] [PubMed] [Google Scholar]
- 43.Bauermeister JA, Meanley S, Pingel E, et al. PrEP awareness and perceived barriers among single young men who have sex with men. Curr HIV Res. 2013;11:520–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.King HL, Keller SB, Giancola MA, et al. Pre-exposure prophylaxis accessibility research and evaluation (PrEPARE Study). AIDS Behav. 2014;18:1722–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Franks J, Hirsch-Moverman Y, Loquere AS, Jr, et al. Sex, PrEP, and Stigma: experiences with HIV pre-exposure prophylaxis among New York City MSM participating in the HPTN 067/ADAPT study. AIDS Behav. 2018;22:1139–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Golub SA. PrEP Stigma: implicit and explicit drivers of disparity. Curr HIV/AIDS Rep. 2018;15:190–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2003. Available at: 10.17226/10260. Accessed March 12, 2018. [DOI] [PubMed] [Google Scholar]
- 48.Mannheimer SB, Morse E, Matts JP, et al. Sustained benefit from a long-term antiretroviral adherence intervention. Results of a large randomized clinical trial. J Acquired Immune Defic Syndr. 2006;43(suppl 1):S41–S47. [DOI] [PubMed] [Google Scholar]
- 49.Shrestha R, Altice FL, Karki P, et al. Integrated bio-behavioral approach to improve adherence to pre-exposure prophylaxis and reduce HIV risk in people who use drugs: a pilot feasibility study. AIDS Behav. 2018;22:2640–2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Amico KR. A situated-information motivation behavioral skills model of care initiation and maintenance (sIMB-CIM): an IMB model based approach to understanding and intervening in engagement in care for chronic medical conditions. J Health Psychol. 2011;16:1071–1081. [DOI] [PubMed] [Google Scholar]
- 51.Barfod TS, Sorensen HT, Nielsen H, et al. Simply forgot' is the most frequently stated reason for missed doses of HAART irrespective of degree of adherence. HIV Med. 2006;7:285–290. [DOI] [PubMed] [Google Scholar]
- 52.Reynolds NR, Testa MA, Marc LG, et al. Factors influencing medication adherence beliefs and self-efficacy in persons naive to antiretroviral therapy: a multicenter, cross-sectional study. AIDS Behav. 2004;8:141–150. [DOI] [PubMed] [Google Scholar]
- 53.Saberi P, Neilands TB, Vittinghoff E, et al. Barriers to antiretroviral therapy adherence and plasma HIV RNA suppression among AIDS clinical trials group study participants. AIDS Patient Care STDs. 2015;29:111–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.National HIV AIDS strategy. 2015. Available at: https://files.hiv.gov/s3fs-public/nhas-update.pdf. Accessed March 12, 2018.
- 55.Catania JA, Gibson DR, Chitwood DD, et al. Methodological problems in AIDS behavioral-research—influences on measurement error and participation bias in studies of sexual-behavior. Psychol Bull. 1990;108:339–362. [DOI] [PubMed] [Google Scholar]
- 56.Langhaug LF, Sherr L, Cowan FM. How to improve the validity of sexual behaviour reporting: systematic review of questionnaire delivery modes in developing countries. Trop Med Int Health. 2010;15:362–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Velloza J, Gandhi M, Hendrix CW, et al. Pharmacologic measures of PrEP adherence among high-risk MSM in HPTN 067. Presented at: Conference on Retroviruses and Opportunistic Infections; March 4–7, 2018 (Poster #463), Boston, MA.
- 58.Dye BJ, Hughes JP, Li M, et al. Interviewer Adjustment of Smart Pillbox Monitoring Did Not Improve Accuracy in Measuring Oral PrEP Adherence in HPTN 067. Poster Presented at: HIV Research for Prevention (HIVR4P); October 21–25, 2018, Madrid, Spain.
- 59.Mannheimer S, Franks J, Loquere A, et al. Challenges to Collecting PrEP Adherence Data in the New York City (NYC) Site of the HPTN 067 Study. Poster presented at: HIV Research for Prevention (HIVR4P); October 21–25, 2018, Madrid, Spain.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.