Abstract
BACKGROUND:
Rib fractures (RFx) continue to be a source of morbidity and mortality. A RFx care pathway has been used based on forced vital capacity (FVC). The objective of this study was to test the hypothesis that deterioration of FVC to less than 1 after admission is a marker for high-risk patients and affects outcomes.
METHODS:
A retrospective study of patients enrolled in an RFx care pathway at a Level 1 trauma center from 2009 to 2014. All patients had an admission FVC greater than 1. 2 groups were analyzed: patients with a lowest inpatient FVC less than 1 (Group A) compared to patients with lowest inpatient FVC of 1 or greater (Group B). Complications [pneumonia, upgrade to the intensive care unit, readmission, and intubation] and demographics were examined. Patients without documented admission FVCs were excluded. p < 0.05 was considered significant.
RESULTS:
A total of 1,106 patients were analyzed (Group A, 187; Group B, 919). Patients whose FVC dropped less than 1 (Group A) had a higher complication rate [15% (Group A) vs 3.2% (Group B); p < 0.001]. Rates of pneumonia, readmission, unplanned upgrade, and intubation were all significantly higher in Group A [pneumonia: 9% (Group A) vs 1.4% (Group B), p < 0.001; readmission: 4% (Group A) vs 1.7% (Group B), p = 0.04; upgrade; 3.7% (Group A) vs 0.2% (Group B), p < 0.001; intubation: 1.6% (Group A) vs 0.1% (Group B), p = 0.02]. Hospital length of stay was longer in Group A [10 days (Group A) vs 4 days (Group B), p < 0.001].
CONCLUSIONS:
Forced vital capacity predicts complications in patients with RFx. Patients whose FVC falls less than 1 during admission are at high risk for pulmonary complications. Daily FVC testing for patients admitted with RFx can predict outcomes. Forced vital capacity less than 1 should be considered as a marker for complications. Once FVC drops less than 1, patients should be considered for increased interventions. Even if the patient has not yet clinically deteriorated, consideration for higher level of care is warranted.
Keywords: Rib fractures, FVC, ICU, complications
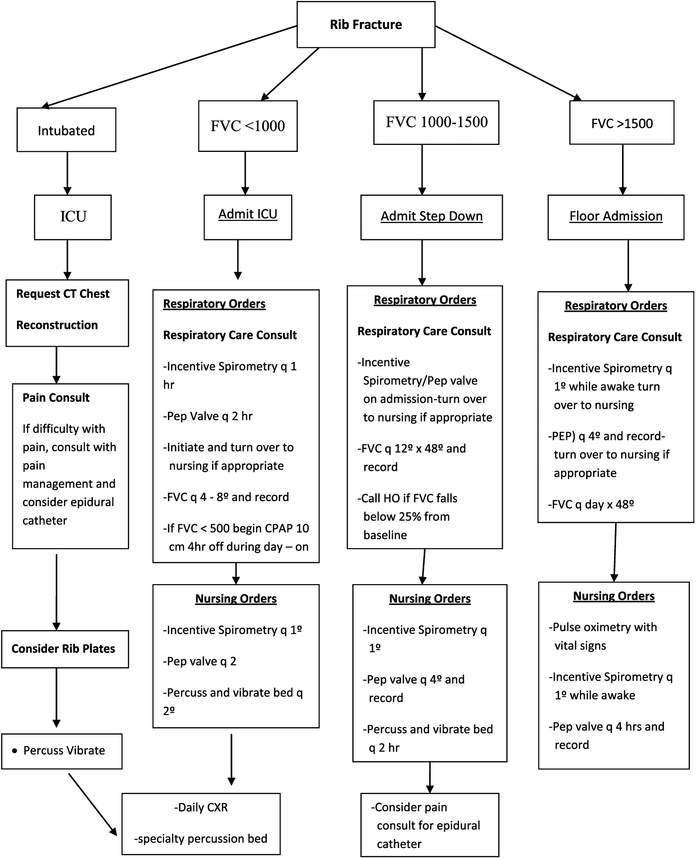
Rib fractures (RFx) account for approximately 10% of all traumatic injuries.1 They continue to be a significant source of morbidity and mortality among trauma patients and can result in severe respiratory complications. Predictive models have been used to identify those patients at high risk for complications and death secondary to traumatic rib fractures. These models have used variables such as number of rib fractures or age to identify a select group of patients who require a high level of care.2–5 Literature supports that patients with six or more RFx or those older than age 65 are at high risk and advocate those patients be admitted to the intensive care unit (ICU) for monitoring.2–5 However, there is not a consensus on the best method to identify patients who are high risk for complications after RFx. A simple reproducible method to identify high-risk patients so resources could be focused would be of benefit. At our institution, a rib fracture care pathway has been adopted and used. Our previous studies have validated the use of forced vital capacity (FVC), a measurement of the amount of air that can be forcibly exhaled from the lungs after taking the deepest breath possible, in triaging patients to admission level of care.6 More specifically, a RFx care pathway (Fig. 1) using admission FVC (aFVC) has been shown to predict patients at risk for complications and determine the need for ICU admission.6 This pathway indicates that patients with an aFVC of less than 1.0 L be admitted to the ICU secondary to high risk of complications and death. The objective of this study was to test the hypothesis that deterioration of FVC to less than 1 after admission is a marker for high-risk patients and affects outcomes.
Figure 1.
Rib fracture care pathway used in the study. PEP, positive expiratory pressure.
METHODS
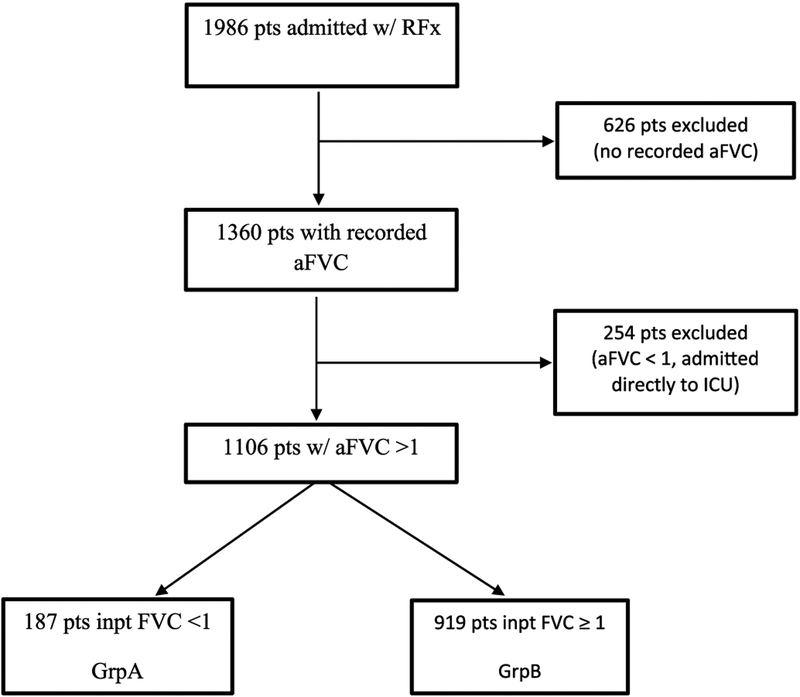
The West Virginia University Institutional Review Board approved this retrospective cohort study conducted at a university-based American College of Surgeons–verified Level 1 trauma center from 2009 to 2014. All patients 18 years or older with RFx admitted to the trauma service and enrolled in the RFx care pathway were evaluated. This pathway indicated patients to be triaged on admission to the ICU, step down unit (SDU), or floor based on admission FVC (<1, 1–1.5, >1.5). All patients included in the statistical analysis had an aFVC of 1.0 or greater and were initially admitted to the SDU or floor. Those with an aFVC less than 1.0 were excluded. Patients in whom an aFVC was not obtainable or those with missing FVC values were excluded from analysis; this includes those with altered mental status due to any cause or those who were intubated on arrival. Patients with concomitant injuries were not excluded from analysis. Inclusion criteria are shown in Figure 2. Admission FVC was tested in the emergency department by trained respiratory therapist. Testing was completed after patient evaluation, imaging, and stabilization. The average of three attempts was recorded and used for the protocol. After admission, all patients were managed by the trauma service in accordance with the Rib Fracture Care Protocol (Fig. 1). This guideline includes at least daily FVC measurements and specifies nursing and respiratory interventions based on the patients’ pulmonary function. Pain management guidelines were also included in the pathway. Each patient was given multimodal pain control on admission including nonsteroidal anti-inflammatory medications, topical analgesia, muscle relaxants, and narcotics. Those whose FVC was less than 1 are evaluated for epidural placement. The care pathway was not altered in any way during the study. Values for admission, highest, and lowest FVC were collected from the patients’ medical record.
Figure 2.
Inclusion criteria for statistical analysis. aFVC, admission FVC; pts, patients; inpt, inpatient.
The patients were divided into two groups for statistical analysis. Group A (GrpA) included those patients whose aFVC was 1 or greater and lowest inpatient FVC was less than 1.0. Group B (GrpB) included all patients with an aFVC of 1 or greater and lowest inpatient FVC was 1.0 or greater. Data including age, sex, chest Abbreviated Injury Scale score, and injury severity score were examined. Characteristics across the two groups were analyzed with the use of t-test and χ2 analysis (Table 1). Outcome measures included hospital length of stay (LOS) and Trauma Quality Improvement Program-defined complications: pneumonia, unplanned intubation, readmission, and unplanned upgrade to the ICU. Statistical analysis was completed by a biostatistician to compare the outcomes of the patients in GrpA to GrpB. The relationships between groups and rates of complications and mortality were determined by the Fisher exact test. The difference in hospital LOS was measured with a Kruskal-Wallis test.
TABLE 1.
Patients’ Characteristics
| Characteristics | GrpA Lowest FVC <1 | GrpB Lowest FVC >1 | p |
|---|---|---|---|
| n = 187 | n = 919 | ||
| Age | 58.0 (18–95) | 47.4 (18–93) | <0.001 |
| Sex, male | 115 (61%) | 731 (79%) | <0.001 |
| AIS chest | 2.9 (1–5) | 2.5 (1–5) | <0.001 |
| ISS | 17.2 (5–41) | 13.3 (1–38) | <0.001 |
| Chest tube present | 51 (27.3%) | 95 (10%) | <0.001 |
| COPD | 33 (17.6%) | 78 (8.4%) | <0.001 |
| Average admission FVC | 1.3 (1–3.7) | 1.9 (1–2.5) | <0.001 |
| Average highest FVC | 1.6 (1–3.7) | 2.3 (1–4.8) | <0.001 |
| Average lowest FVC | 0.7 (0.2–0.9) | 1.7 (1–2) | <0.001 |
Characteristics of patients in GrpA versus GrpB. Characteristics listed as average and range. p value calculated by t-test or χ2. FVC is in liters.
COPD, chronic obstructive pulmonary disease.
RESULTS
A total of 1,986 patients were admitted with RFx during the study period. One thousand one hundred six patients met inclusion criteria. These patients were divided into two groups: GrpA, those patients with the lowest inpatient FVC, less than 1 (187 patients), and GrpB patients with the lowest inpatient FVC, 1 or greater (919 patients). Individual characteristics of each group are shown in Table 1.
Patients whose FVC deteriorated to less than 1.0 at any point during admission (GrpA) had a higher rate of overall complications [15% (GrpA) vs 3.2% (GrpB); p < 0.001]. In addition, when complications are examined individually, rates of pneumonia, readmission, unplanned upgrade to the ICU and intubation (int) were all significantly more likely to occur in patients in GrpA when compared to those in GrpB [pneumonia: 9% (GrpA) vs 1.4% (GrpB), p < 0.001; readmission: 4% (GrpA) vs 1.7% (GrpB), p = 0.04; upgrade; 3.7% (GrpA) vs 0.2% (GrpB), p < 0.001; intubation: 1.6% (GrpA) vs 0.1% (GrpB), p = 0.02]. Complication rates are shown in Table 2 The single intubation in GrpB was attributed to altered mental status, while all the intubations in GrpA were related to respiratory failure. Group B also had two patients with unplanned upgrades to the ICU, both of which were for reasons unrelated to pulmonary complications; one patient was upgraded due to concern for stroke, while the second was upgraded postoperatively for blood loss after orthopedic procedure. Seven patients in GrpA had unplanned upgrades to the ICU, six of these were due to worsening respiratory status on the floor. There were 16 readmissions in GrpB; of these, only two were related to complications from rib fractures. The remainders included neurologic symptoms, wound infections, ileus, and delayed splenic rupture as reasons for readmission. Half of the patients who were readmitted from GrpA were due to pulmonary-related reasons such as chest pain and shortness of breath. Hospital LOS was longer in patients whose FVC declined to less than 1 (GrpA), with a mean of 10 days versus 4 days for those whose inpatient FVC remained 1 or greater (GrpB) (H = 13.37, p < 0.001). Lastly, patients whose inpatient FVC dropped below 1 (GrpA) during admission were at a higher risk of death when compared to those whose FVC remained greater than 1 (GrpB) during hospitalization [GrpA, 3.2%, vs GrpB, 0.2%; p < 0.001]. There were a total of two patients in GrpB who died during admission; both of these patients died due to sepsis from an abdominal source not related to rib fractures, while three of six deaths in GrpA were due to respiratory failure.
TABLE 2.
Complication Rates
| Complications | GrpA (Lowest FVC <1) |
GrpB (Lowest FVC ≥ 1) |
p |
|---|---|---|---|
| n = 187 | n = 919 | ||
| Pneumonia | 17 (9%) | 13 (1.4%) | <0.001 |
| Readmission | 8 (4.2%) | 16 (1.7%) | 0.04 |
| Intubation | 3 (1.6%) | 1 (0.1%) | 0.02 |
| Unplanned ICU | 7 (3.7%) | 2 (0.2%) | <0.001 |
| Any complication | 29 (15.5%) | 30 (3.2%) | <0.001 |
| Hospital LOS | 10 days | 4 days | <0.001 |
| Mortality | 6 (3.2%) | 2 (0.2%) | <0.001 |
Complication rates of patients with inpatient FVC < 1 (GrpA) versus those with inpatient FVC ≥ 1 (GrpB).
DISCUSSION
Rib fractures lead to pulmonary complications, pain control issues, prolonged hospital stays, and even death in the trauma patient. Many studies have attempted to identify the subset of patients who are at high risk for poor outcomes. Previous literature has used number of ribs fractured or age as a determinant for patients at risk for complication secondary to traumatic rib fractures.3–5,7 Mortality is greatly increased in patients with six or more ribs broken, and these patients require ICU admission.3,8 Three or more rib fractures has been shown to indicate the need for transfer of a patient to a higher level of care due to the increased risk of complications.4,8 In addition, it has been suggested that patients’ age 65 and older should be treated in the ICU setting due to a high risk of mortality after traumatic rib fractures.5,7 This study demonstrates that FVC, a dynamic physiologic parameter, can be used as a marker for patients who are at a higher risk for complications and identify patients who require transfer to a higher level of care.
Patients with admission FVC of 1 or greater, initially admitted to the SDU or floor, whose inpatient FVC deteriorated to less than 1 had significantly higher rates of complications compared to patients whose FVC remained at 1 or greater during his/her entire hospital stay. We suggest that following a patient’s FVC during admission can identify a decline in pulmonary reserve and impending respiratory complication. A deterioration of FVC may be the first sign of worsening clinical status. Often a patient’s FVC declines before obvious clinical changes. Identifying this decline early can allow increased intervention aimed at reducing or eliminating the patients’ risk for complication.
Carver et al.9 demonstrated that for each 10% decline in vital capacity patients were more likely to experience pulmonary complications. The results of this study are concurrent with those reported by Carver et al.,9 indicating that a decline in FVC during admission is a mark for high-risk patients. Implementation of pathways based on body weight or percentages is challenged in that calculations are required and the resultant numbers are variable making it more difficult to implement when educating large numbers of nurses, physicians, and respiratory therapists. Although this method may be more specific to an individual, it is harder to adopt across a hospital system. This care pathway uses a standard FVC value (1.0 L) as opposed to a percentage of estimated FVC, thus making it easier for the bedside physician to implement. Having three standard levels of care has been easier for education and broad application and adoption. Forced vital capacity is a low-cost and efficient test that can be done at the bedside by a respiratory therapist multiple times a day. It does not require the patient to be transported off the floor; it is done quickly and is minimal cost to the hospital system. The values are easy to interpret and can be used as a tool to monitor respiratory reserve in the setting of compromised chest wall function from rib fractures.
Unplanned upgrade to the ICU is associated with prolonged hospital LOS, mechanical ventilation, and increased mortality compared to planned upgrades to the ICU.10 Patients in whom FVC declines to less than 1 should be considered for planned upgrade to the ICU for pulmonary hygiene. These patients are at a higher risk for requiring unplanned upgrades to the ICU and respiratory complications. In nearly all the patients in our study with an unplanned upgrade to the ICU, the cause was respiratory distress or failure. We suggest that when daily FVC falls below 1, these patients should be preemptively transferred to a higher level of care. With early transfers and increased pulmonary intervention before clinical decline outcomes may be improved. In addition, these patients should also be considered for transfer to a tertiary facility if not already admitted to one. These patients are at higher risk for developing pneumonia, requiring intubation, and have a higher mortality compared to patients with FVC greater than 1 during the entire hospital stay.
The baseline characteristics and preexisting comorbidities of individuals in each group were also examined (Table 1). While all patients in both groups had an admission FVC of 1 or greater, the baseline characteristics of the two groups were significantly different. Patients whose FVC declined to less than 1 during admission (GrpA) had significantly higher rates of chronic obstructive pulmonary disease, chest tube placement, and age. In addition, the highest, lowest, and admission FVCs were lower in GrpA. These results indicate that these baseline characteristics may be indicators for patients who are more likely to have declining FVC while inpatient. Such characteristics need closer examination and should be looked at for additions to the current rib fracture care pathway.
There are several limitations to this study. This is a single-institution retrospective review with inherent limitations. Patients with injuries other than rib fractures were not excluded from analysis. Although some data may be confounded by concomitant injuries, many patients sustain rib fractures in addition to other injuries. We desired to develop a bedside tool that would be useful to providers in a variety of settings and not be limited to isolated injuries. Patients unable to perform FVC were automatically excluded, which would include those who were intubated or altered on arrival.
CONCLUSION
This study elucidates a predictive model for patients at high risk for pulmonary complications and death after traumatic rib fractures. Daily measurements of FVC for patients with rib fracture can predict outcomes. Patients with an FVC that drops to less than 1 during hospital admission are at a significantly higher risk for complications. Patients in whom FVC declines to less than 1 should be considered for increased interventions. Even if the patient has not yet clinically deteriorated, consideration for transfer to a higher level of care is warranted.
Footnotes
This paper was presented at the 31st Annual Meeting of the Eastern Association for the Surgery of Trauma Scientific Assembly, Raymond H. Alexander Paper Competition, January 9, 2017, in Orlando, FL.
DISCLOSURE
The authors declare no conflicts of interest.
REFERENCES
- 1.Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37(1):975–979. [DOI] [PubMed] [Google Scholar]
- 2.Battle CE, Hutchings H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury. 2012;43:8–17. [DOI] [PubMed] [Google Scholar]
- 3.Flagel BT, Luchette FA, Reed RL, Esposito TJ, Davis KA, Santaniello JM, Gamelli RL. Half-a-dozen ribs: the breakpoint for mortality. Surgery. 2005; 138(4):717–723. [DOI] [PubMed] [Google Scholar]
- 4.Lee RB, Bass SM, Morris JA Jr, Mackenzie EJ. Three or more rib fractures as an indicator for transfer to a Level I trauma center: a population-based study. J Trauma. 1990;30(6):689–694. [DOI] [PubMed] [Google Scholar]
- 5.Bergeron E, Lavoie A, Clas D, Moore L, Ratte S, Tetreault S, Lemaire J, Martin M. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54(3):478–485. [DOI] [PubMed] [Google Scholar]
- 6.Warner RW, Cornell N, Knollinger P, Hobbs G, Khan U, Grabo D, Wilson A. Is an FVC of 1.5 adequate to predict respiratory sufficiency in rib fractures? submitted for publication 2017. J Trauma Acute Care Surg. [Google Scholar]
- 7.Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma. 2000;48(6):1040–1046. [DOI] [PubMed] [Google Scholar]
- 8.Sirmali M, Türüt H, Topçu S, Gülhan E, Yazici U, Kaya S. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorac Surg. 2003;24:133–138. [DOI] [PubMed] [Google Scholar]
- 9.Carver TW, Milia DJ, Somberg C, Brasel K, Paul J. Vital capacity helps predict pulmonary complications after rib fractures. J Trauma Acute Care Surg. 2015;79(3):413–416. [DOI] [PubMed] [Google Scholar]
- 10.Rubano JA, Vosswinkel JA, McCormack JE, Huang EC, Shapiro MJ, Jawa RS. Unplanned intensive care unit admission following trauma. J Crit Care. 2016;33:174–179. [DOI] [PubMed] [Google Scholar]