Abstract
Background:
Unplanned dialysis initiation is common in patients with chronic kidney disease (CKD).
Objective:
To determine common definitions and patient risk factors for unplanned dialysis.
Design:
Systematic review.
Setting:
MEDLINE, EMBASE, and the Cochrane Library were searched from inception to February 2018.
Patients:
Studies that included incident chronic dialysis patients or patients with CKD that cited a definition or examined risk factors for unplanned dialysis were included.
Measurements:
Definitions and criteria for unplanned dialysis reported across studies. Patient characteristics associated with unplanned dialysis.
Methods:
Two reviewers independently extracted data using a standardized data abstraction form and assessed study quality using a modified New Castle Ottawa Scale.
Results:
From 2797 citations, 48 met eligibility criteria. Reported definitions for unplanned dialysis were variable. Most publications cited dialysis initiation under emergency conditions and/or with a central venous catheter. The association of patient characteristics with unplanned dialysis was reported in 26 studies, 18 were retrospective and 21 included incident dialysis patients. The most common risk factors in univariate analyses were (number of studies) increased age (n = 7), cause of kidney disease (n = 6), presence of cardiovascular disease (n = 7), lower serum hemoglobin (n = 9), lower serum albumin (n = 10), higher serum phosphate (n = 6), higher serum creatinine or lower estimated glomerular filtration rate (eGFR) at dialysis initiation (n = 7), late referral (n = 5), lack of dialysis education (n = 6), and lack of follow-up in a predialysis clinic prior to dialysis initiation (n = 5). A minority of studies performed multivariable analyses (n = 10); the most common risk factors were increased age (n = 4), increased comorbidity score (n = 3), late referral (n = 5), and lower eGFR at dialysis initiation (n = 3).
Limitations:
Comparison of results across studies was limited by inconsistent definitions for unplanned dialysis. High-quality data on patient risk factors for unplanned dialysis are lacking.
Conclusions:
Well-designed prospective studies to determine modifiable risk factors are needed. The lack of a consensus definition for unplanned dialysis makes research and quality improvement initiatives in this area more challenging.
Keywords: systematic review, dialysis, risk, predialysis, CKD
Abrégé
Contexte:
L’initiation non planifiée d’un traitement de dialyse est fréquente chez les patients atteints d’insuffisance rénale chronique (IRC).
Objectifs:
L’étude visait à définir la dialyse non planifiée et à définir ses facteurs de risques chez les patients.
Type d’étude:
Une revue systématique.
Sources:
Les bases de données MEDLINE et EMBASE, de même que la bibliothèque Cochrane ont été consultées, de leur création à février 2018.
Sujets:
Les études traitant de patients atteints d’IRC ou dialysés de façon chronique, et qui citaient une définition ou examinaient les facteurs de risques associés à une dialyse non planifiée.
Mesures:
On a colligé les différentes définitions d’une dialyse non planifiée rapportées dans l’ensemble des études, ainsi que les critères la définissant et les caractéristiques des patients qui y étaient associées.
Méthodologie:
À l’aide d’un formulaire normalisé d’extraction des données, deux examinateurs ont compilé les données de façon indépendante. La qualité des études a été évaluée avec une échelle de Newcastle-Ottawa modifiée.
Résultats:
Des 2 797 études répertoriées, 48 satisfaisaient les critères d’admissibilité. Les définitions d’une dialyse non planifiée variaient d’une étude à l’autre. La plupart des publications mentionnaient une dialyse débutée en situation d’urgence et/ou avec un cathéter veineux central. L’association des caractéristiques des patients à une dialyse non planifiée a été signalée dans 26 études, desquelles 18 constituaient des études rétrospectives et 21 incluaient des patients dialysés incidents. Les facteurs de risque les plus souvent cités dans les analyses univariées étaient (en nombre d’études) : l’âge avancé du patient (n=7), la cause de la néphropathie (n=6), la présence d’une cardiopathie (n=7), de faibles taux d’hémoglobine (n=9) et d’albumine (n=10), un taux élevé de phosphate sérique (n=6), un taux élevé de créatinine sérique ou un faible DFGe à l’amorce de la dialyse (n=7), un aiguillage tardif (n=5), le manque d’information sur la dialyse (n=6), et l’absence de suivi dans une clinique de prédialyse avant l’initiation du traitement (n=5). Seules quelques études avaient procédé à des analyses multivariées (n=10). Dans ces dernières, les facteurs de risques les plus fréquemment cités étaient : l’âge avancé du patient (n=4), un score de comorbidité élevé (n=3), un aiguillage tardif (n=5), et un faible DFGe au moment de l’initiation de la dialyse (n=3).
Limites:
La comparaison des résultats d’une étude à l’autre était difficile en raison d’un manque d’uniformité dans les définitions d’une dialyse non planifiée. On manque de données robustes sur les facteurs de risque menant à une dialyse non planifiée chez les patients.
Conclusion:
On constate un besoin pour des études prospectives bien conçues examinant les facteurs de risque modifiables. L’absence d’une définition consensuelle pour la dialyse non planifiée rend plus difficiles les initiatives de recherche et d’amélioration de la qualité dans ce domaine.
What was known before
Unplanned dialysis initiation is common in patients with chronic kidney disease. Determining patient risk factors for this important outcome may help reduce the incidence.
What this adds
High-quality data on patient risk factors for unplanned dialysis are lacking. Well-designed prospective studies to determine modifiable risk factors are needed.
Introduction
Many patients with chronic kidney disease (CKD) start dialysis in an unplanned fashion and/or under urgent circumstances despite regular follow-up by a nephrologist. Most studies report a prevalence of unplanned dialysis between 40% and 60%.1-7 However, the prevalence varies, likely in large part due to inconsistent definitions across studies. An unplanned dialysis start is defined by varying criteria that may include dialysis initiation with a central venous catheter (CVC) as opposed to a permanent access (arteriovenous fistula, arteriovenous graft, or peritoneal dialysis catheter), and/or dialysis initiation during an acute hospitalization, and/or dialysis initiation under emergent circumstances.7 Unfortunately, there is no established consensus definition.
Unplanned dialysis is of concern because, theoretically, patients forego the opportunity to make an informed, shared decision with respect to timing and modality of renal replacement therapy (RRT). Instead, most centers in North America only offer one option for RRT under urgent conditions: hemodialysis with a CVC. In addition, unplanned dialysis is associated with increased patient morbidity and mortality and added health care costs.4,6-9 Given the high prevalence of unplanned dialysis and association with poor patient outcomes, we conducted a systematic review to determine patient risk factors for this outcome. As a secondary objective, we determined the most common criteria and terminology used to define the outcome. The results of this systematic review should help to inform future studies aimed at reducing the burden of unplanned dialysis starts.
Materials and Methods
Search Strategy
We performed a comprehensive, systematic search of articles published in peer-reviewed journals using MEDLINE, EMBASE, and the Cochrane Library (from inception to February 28, 2018). The search was carried out with the assistance of a librarian experienced in systematic reviews. We used a structured search strategy (outlined in Supplementary Appendix A), based on controlled vocabulary and relevant key terms that were broad to prioritize sensitivity. The references of included articles and existing reviews were scanned for additional studies. There were no restrictions based on study design or language in the search.
Study Selection
There were 2 independent investigators (A.O.M. and A.A.) who screened identified titles and abstracts. Those deemed to be clearly irrelevant were removed on the initial screen. If no abstract was available, the full text was obtained unless the article could be confidently excluded by title alone. Full-text versions of potentially eligible studies were obtained and independently screened by 2 reviewers (A.O.M. and R.H. or A.A.) to determine their eligibility based on the selection criteria. Any disagreements during the screening process were resolved through discussion among the authors in accordance with the selection criteria.
We included retrospective and prospective studies that reported criteria to define unplanned dialysis or characteristics of patients who had an unplanned versus planned dialysis start. We excluded non-English articles, studies published only in abstract form, case reports, narrative reviews, editorials, letters, practice guidelines, and pediatric studies. We excluded studies that focused primarily on late referral to nephrology.
Data Extraction and Synthesis
Two independent investigators (A.O.M. and R.H.) abstracted data using a standardized data abstraction form (see Supplementary Appendix B). The following data were abstracted: study methods, patient characteristics, criteria and terminology used to define unplanned dialysis, and patient characteristics by unplanned versus planned dialysis status. Patient characteristics significantly associated with unplanned dialysis were summarized, along with covariates included in multivariable models to identify independent associations. Statistical significance within studies was defined by individual study methods. Two investigators (A.O.M. and R.H.) independently performed a quality assessment for studies that reported patient characteristics associated with unplanned dialysis. A modified Newcastle-Ottawa Scale (NOS) was used to assess the quality of applicable observational studies.10 A score was given for the NOS domains of cohort selection and comparability (maximum scores of 4 and 2, respectively). The outcome domain was removed from the NOS, as we did not examine outcomes associated with unplanned dialysis. The reporting of this systematic review is in accordance with PRISMA guidelines (refer to Supplementary Appendix C for details).11 The methods were all prespecified, and the review protocol was registered with the international prospective register of systematic reviews (http://www.crd.york.ac.uk/PROSPERO; registration no. CRD42016032916).12
Results
Eligible Studies
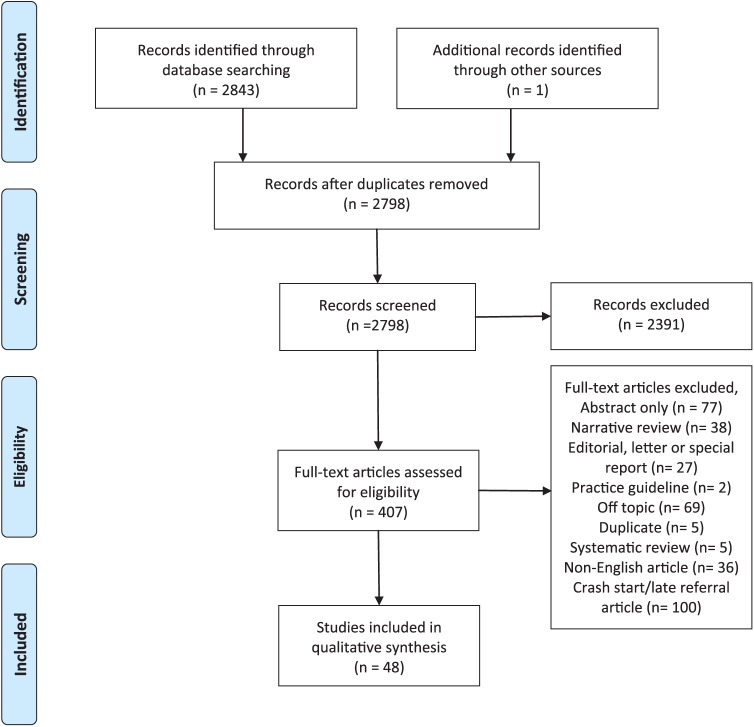
Study selection is outlined in Figure 1. The electronic database search identified 2843 records and one further record was identified from other sources. There were 2798 nonduplicate citations. After independently reviewing the title and abstract of all potentially relevant records, 407 articles were retrieved and reviewed in full text. Of these articles, 48 studies were found to meet inclusion criteria.
Figure 1.
Study selection.
Patient and Study Characteristics
The characteristics of the 48 eligible studies are outlined in Table 1. Eligible studies included incident chronic dialysis patients (n = 42)2-4,6,8,9,13-48 and patients with CKD known to nephrology (n = 6).5,49-53 Study designs included retrospective cohort studies (n = 27),2,3,5,6,14-16,19-24,26,28,31-36,38,47-50,53 cross-sectional studies (n = 2),9,52 prospective cohort studies (n = 17),4,8,17,18,25,27,29,30,37,39-45,51 retrospective before/after studies (n = 1),46 and unclear design (n = 1).13 No randomized control trials were found in the search. The majority of studies were conducted in Europe (n = 26; 22 unique cohorts)2,8,9,15-19,22-25,29,30,33,36,40-43,45-48,50,51; 11 studies were conducted in North America3-6,14,21,26,28,31,52,53 (Canada, n = 9; 8 unique cohorts). Study cohort sizes ranged from 43 to 45 785 persons.
Table 1.
Study Characteristics.
| Study | Study design | Participants/number of centers/country | Exclusion criteria | Number of participants with an unplanned dialysis start, n (%) | Mean (SD) age of participants | Definition of unplanned dialysis/terminology used | Patient characteristics reported by unplanned versus planned dialysis (y/n) | Adjusted analysis of characteristics associated with unplanned dialysis (y/n) |
|---|---|---|---|---|---|---|---|---|
| Holland and Lam5 | RCS | 201 patients age > 16 years with progressive CKD followed in a predialysis clinic who began dialysis during the study period/1/Canada | None specified | 91 (45) | 62 | Dialysis initiation during a hospitalization/suboptimal dialysis start | Yes | Yes |
| Metcalfe et al25 | PCS | 532 incident chronic dialysis patients/11/United Kingdom | Preemptive kidney transplant | 129 (24) | 65 (16-91)a | Followed by nephrology for ≥1 month, steady progression to ESRD and no permanent access at dialysis initiation/unplanned dialysis start | Yes | No |
| Abderrahim et al13 | Unclear | 299 patients with diabetes initiating chronic dialysis/1/Tunisia | Reversible AKI, nondiabetic nephropathy | 104 (35) | 58 (9)b
35 (7)c |
Dialysis started in emergency conditions (unspecified)/urgent or emergency onset of RRT | No | No |
| Caskey et al8 | PCS | 196 incident chronic dialysis patients known to nephrology for at least 1 month before starting RRT/9/7 European countries | None specified | 70 (36) | 62 (46-71)d | No previous creatinine >300 µmol/L or first dialysis not arranged in advance and performed urgently for life-threatening renal insufficiency/unplanned dialysis | Yes | No |
| Joly et al50 | RCS | 144 incident octogenarians with CKD and calculated CrCl < 10 mL/min referred to a renal unit/1/France | Death prior to therapeutic decision | 35 (24) | 83 (3) | Emergency dialysis (no further details)/unplanned dialysis | No | No |
| Loos et al9 | Cross-sectional | 169 hospitalized incident chronic dialysis patients ≥70 years with a predialysis CrCl <15 mL/min or creatinine >600 μmol/L/13/France | None specified | 78 (66) | 76 (5) | No specific criteria provided/unplanned dialysis | Yes | No |
| Ravani et al29,30 | PCS | 229 incident chronic dialysis patients/2/Italy | None specified | 103 (45) | 64 (15) | Development of uremic complications that required an emergency dialysis start/unplanned dialysis | No | No |
| Frimat et al18 | PCS | 148 incident chronic dialysis patients with diabetes/13/France | Acute, reversible renal failure, kidney graft failure | 87 (59) | 79 (44-89)e | Dialysis not initiated with an arteriovenous fistula/graft or a Tenckhoff catheter/unplanned dialysis | No | No |
| Marron et al23 | RCS | 621 incident chronic dialysis patients/24/Spain | None specified | 304 (49) | 62 (15) | Uremia requiring emergency initiation of dialysis/nonplanned dialysis start | Yes | No |
| Castellano et al15 | RCS | 117 incident chronic dialysis patients/1/Spain | None specified | 52 (44) | 64 (15) | Dialysis started for an emergency condition or it was not appropriate to delay starting dialysis for >24 hr/nonprogrammed dialysis | Yes | No |
| Marron et al24 | RCS | 1504 incident chronic dialysis patients/35/Spain | None specified | 695 (46) | 61 (16) | Dialysis start unscheduled, even if a permanent access was in place/nonplanned dialysis start | Yes | No |
| Buck et al2 | RCS | 109 patients initiating RRT known to renal services for at least 4 months/1 tertiary center and 4 satellite dialysis units/United Kingdom | No consent for data collection | 49 (45) | 63 | Dialysis started using a catheter or during an emergent hospitalization/known acute dialysis | Yes | Yes |
| Couchoud et al16 | RCS | 3512 incident chronic dialysis patients ≥75 years/multiple centers/France | AKI | 1134 (32) | 80 (75-100)a | First HD started under emergency conditions (dialysis required within 24 hr)/unplanned HD | No | No |
| Thilly et al33 | RCS | 1315 incident chronic dialysis patients/13/France | AKI | 559 (43) | 67 (15) | HD with a temporary catheter/unplanned dialysis | No | No |
| Wu et al34 | RCS | 486 incident chronic HD patients surviving >90 days following dialysis initiation/2/Taiwan | None specified | 368 (76) | Not available | Vascular access creation after HD initiation/urgent dialysis | Yes | No |
| Yoon et al35 | RCS | 503 incident HD patients/8/South Korea | None specified | 412 (82) | 59 (16-93)e | Initiation of HD without prior placement of a permanent access/unplanned dialysis | No | No |
| Crews et al4 | PCS | 652 incident chronic dialysis patients able to speak English or Spanish/71/USA | Incomplete data on location of dialysis | 410 (63) | 59 (14)f
60 (15)g |
HD initiation during a hospitalization/inpatient HD start | Yes | Yes (1 characteristic) |
| Teo et al32 | RCS | 168 incident chronic dialysis patients surviving more than 90 days on dialysis/1/Singapore | None specified | 109 (65) | 59 (14) | Immediate HD using a catheter/urgent dialysis | No | No |
| Gomis Couto et al19 | RCS | 43 incident HD patients/1/Spain | PD, kidney graft failure | 20 (47) | 61 (32-85)e | Dialysis initiated with a temporary venous catheter/unscheduled dialysis | Yes | No |
| Descamps et al17 | PCS | 495 incident chronic dialysis patients/1/France | AKI | 167 (34) | 62 (16) | Unplanned first dialysis session/emergency dialysis | No | No |
| Mendelssohn et al6 | RCS | 339 incident chronic dialysis patients or preemptive kidney transplants/10/Canada | Temporary RRT due to drug or environmental intoxication, AKI treated in the ICU, RRT initiation due to kidney transplant rejection | 205 (61) | 63 (16) | Dialysis started with a CVC or during a hospitalization/suboptimal dialysis start | Yes | No |
| Piwko28 (subcohort of Mendelssohn et al6) | RCS | 323 incident chronic dialysis patients/10/Canada | Temporary RRT due to drug or environmental intoxication, AKI treated in the ICU, RRT initiation due to kidney transplant rejection | 200 (62) | 64 (15) | Dialysis started with a CVC or during a hospitalization/suboptimal dialysis start | Yes (1 characteristic) | No |
| Chiu et al3 | RCS | 377 incident chronic dialysis patients/2/Canada | Requiring RRT for <3 months | 221 (59) | 66 (19-100)a | Dialysis started during a hospitalization or with a CVC following at least 1 outpatient consult with a nephrologist/suboptimal dialysis start | Yes | Yes |
| Cho et al49 | RCS | 298 adults with an eGFR <40 followed for at least 3 months in the nephrology clinic/1/South Korea | Graft failure, AKI, prior RRT, recently diagnosed cancer | 49 (16) | 58 (14) | Unplanned initiation of dialysis due to uremia at the emergency room/urgent dialysis | No | Yes (1 characteristic) |
| Hdez Ordonez et al20 | RCS | 51 incident PD patients with an unplanned initiation requiring hospitalization/1/Mexico | Prior HD treatment | 51 (100) | 49 (19) | No peritoneal dialysis-related clinic visits in the 3 months prior to dialysis initiation/unplanned dialysis | No | No |
| Hughes et al21 | RCS | 436 incident chronic dialysis patients 3/Canada | Missing data | 304 (70) | 67 (16) | Dialysis initiation during a hospitalization or with a CVC/suboptimal dialysis start | Yes | No |
| Lobbedez et al22 | RCS | 8499 incident PD patients/144/France | Primary PD failure, previously treated with PD, treated with HD for >30 days prior to PD, stopped PD because of renal recovery | 568 (7) | 71 (56-80)d,f
69 (50-79)d,g |
On HD for <30 days before peritoneal dialysis initiation (surrogate)/suboptimal dialysis start | Yes | No |
| Nadeau-Fredette et al26 | RCS | 95 patients with CKD who transitioned directly to home HD or were within 30 days of HD initiation/1/Canada | None specified | 51 (54) | 48 (14)f
44 (14)g |
Initiation of dialysis with a CVC or during a hospitalization/suboptimal dialysis start | Yes | Yes |
| Singhal et al31 | RCS | 12 143 incident chronic dialysis patients/multicenter/Canada | No outpatient nephrology visit prior to RRT, recovered renal function, residing in a long-term care facility | 5464 (45) | 65 (52-74)d | Inpatient dialysis initiation | No | Yes |
| Al-Jaishi et al14 | RCS | 17 183 adults initiating chronic HD/97/Canada | Missing data | 7655 (45) | 66 (15) | Dialysis as an inpatient within 2 weeks of starting RRT/acute dialysis | No | No |
| Arora et al52 | Cross-sectional | 249 patients with documented CKD (eGFR <60 on 2 occasions) who saw a nephrologist and started dialysis during the study period/multi-center/USA | Missing data | 129 (52) | 72a | At least 2 predialysis eGFR values <60 mL/min/1.73 m2, dialysis dependence after 90 days and initiated dialysis during a hospitalization/renal “crash” patient | Yes (1 characteristic) | No |
| Brown et al53 | RCS | 184 adults initiating chronic dialysis followed in a multidisciplinary CKD clinic prior to dialysis initiation/1/Canada | None specified | 76 (41) | 61 (16)f
65 (16)g |
Dialysis initiation in hospital/unplanned dialysis | Yes | Yes |
| Park et al27 | PCS | 643 incident chronic dialysis patients ≥20 years/31/Korea | Missing data | 295 (46) | 55 (14) | Dialysis initiated with a CVC or without education about dialysis/unplanned dialysis | Yes | No |
| Prieto-Velasco et al51 | PCS | 1044 patients followed in CKD clinics/26/Spain | None specified | 476 (46) | 67 (56-77)d | Previously unknown by the nephrology unit and/or started dialysis in an urgent situation and/or without permanent access and/or without having gone through a dialysis educational program/unplanned dialysis | Yes (1 characteristic) | No |
| Jin et al37 | PCS | 178 patients with ESRD who required urgent initiation of dialysis without preestablished functional vascular access or a PD catheter/1/China | Unable to tolerate PD catheter insertion or wait time to undergo PD catheter insertion | 178 (100) | 53 (19) | Refer to inclusion criteria/urgent start dialysis | No | No |
| Marron et al48 | RCS | 547 patients starting maintenance dialysis for CKD stage 5/25/Poland, Hungary, Romania | Preemptive kidney transplant | 316 (58) | 64 (42-81)d | Functional permanent access lacking or urgent start dialysis even if a permanent dialysis access was in place/nonplanned dialysis | Yes | Yes |
| Panocchia et al45 | PCS | 316 patients with CKD who were hospitalized, diagnosed with ESRD and started unplanned, urgent HD/1/Italy | AKI, prior history of RRT, multiple organ failure, coma, and dementia | 316 (100) | 67 (12) | Criteria not specified/unplanned, urgent HD | No | No |
| Kanno et al38 | RCS | 122 patients ≥85 years initiating HD/1/Japan | Recovery of renal function, received HD once then withdrew | 69 (57) | 87 (3) | HD initiation in an unplanned setting with a temporary noncuffed and nontunneled CVC, without preparation or use of a permanent access/suboptimal dialysis | Yes | No |
| Li et al39 | PCS | 507 incident ESRD patients /3/Taiwan | None specified | 348 (69) | 62 (16) | Acute dialysis for uremic emergency via a temporary CVC/emergent start | Yes | Yes |
| Machowska et al (4 studies, all the same patient population)40-43 | PCS | 270 patients with CKD stage 5, aged between 18 and 90 years starting dialysis in an unplanned way/26/Austria, Germany, Denmark, France, United Kingdom, Sweden | AKI, conservative kidney care, acute conditions precluding participation, life expectancy <6 months | 270 (100) | 69 (40-83)d | Presented to nephrology within 1 month of needing dialysis and/or being followed by a nephrologist but requiring urgent dialysis by CVC or acutely placed PD catheter/unplanned dialysis | No | No |
| Magalhaes et al44 | PCS | 424 patients admitted to the emergency room with uremia and immediate need for dialysis (within 24 hr of presentation)/1/Brazil | Kidney transplant, taking vitamin D, prior RRT, recovered renal function | 424 (100) | 50 (18) | Refer to inclusion criteria/urgent start dialysis | No | No |
| Schanz et al46 | Retrospective before/after study | 336 adults initiating dialysis during the study time frame and with availability of data and knowledge of implemented dialysis modality/3/Germany | None specified | 106 (70) preintervention and 113 (61) postintervention | 69 (67-71)h preintervention 68 (66-70)h postintervention |
Admitted to hospital with an acute deterioration of renal function reaching ESRD or with generally accepted acute indications for dialysis without a known prior history of ESRD/unplanned dialysis | No | No |
| Vigneau et al47 | RCS | 45 785 patients with ESRD undergoing dialysis/multicenter/France | AKI | 13 736 (30) | 71a | Any first treatment occurring under life-threatening circumstances that requires dialysis initiation within 24 hr/emergency dialysis | No | No |
| Bechade et al36 | RCS | 74 adult patients with incident cancer who initiated dialysis following their cancer diagnosis/multi-center/France | Prior history of cancer, AKI, dialysis prior to cancer diagnosis, history of kidney transplant | 34 (47) | 68 (11) | Dialysis initiation using a temporary nontunneled CVC/unplanned dialysis | No | No |
Note. RCS = retrospective cohort study; CKD = chronic kidney disease; PCS = prospective cohort study; ESRD = end-stage renal disease; AKI = acute kidney injury; RRT = renal replacement therapy; CrCl = creatinine clearance; HD = hemodialysis; ICU = intensive care unit; CVC = central venous catheter; eGFR = estimated glomerular filtration rate; PD = peritoneal dialysis.
Median age (range).
Patients with type 2 diabetes.
Patients with type 1 diabetes.
Median age (interquartile range).
Mean age (range).
Planned dialysis initiation.
Unplanned dialysis initiation.
Mean age (95% confidence interval).
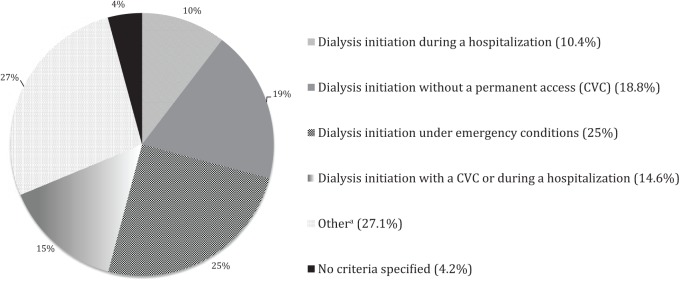
Terms and Definitions for Unplanned Dialysis
The terminology used to describe an unplanned dialysis start was variable across studies (Table 1). Examples of terminology included unplanned dialysis, urgent dialysis, unscheduled dialysis, and suboptimal dialysis start. Varying criteria were used to define unplanned dialysis; however, all definitions included some consideration of the conditions under which dialysis was started (ie, during a hospitalization or emergently) and/or the access that was used at dialysis initiation (ie, a CVC) (Table 1, Figure 2). The proportion of patients with an unplanned dialysis start differed across studies, ranging from 7% to 100%, but most studies reported a proportion between 40% and 60% (n = 21).2,3,5,6,14,15,19,23,24,26-31,36,38,48,51-53
Figure 2.
Definitions for unplanned dialysis among included studies (N = 48).
Note. CVC = central venous catheter; eGFR = estimated glomerular filtration rate.
aMost of the criteria in the “other” category include criteria composed of a combination of all other categories ± preexisting eGFR criteria or referral to nephrology within a specified time period prior to dialysis initiation.
Patient Risk Factors for Unplanned Dialysis
There were 26 studies (25 unique cohorts) that reported the association of patient characteristics with unplanned dialysis, 21 of which included incident chronic dialysis patients (retrospective cohort study, n = 15; cross-sectional study, n = 1; prospective cohort study, n = 5),2-4,6,8,9,15,19,21-28,31,34,38,39,48 and 5 of which included patients with CKD known to nephrology (retrospective cohort study, n = 3; cross-sectional study, n = 1; prospective cohort study, n = 1)5,49,51-53 (Table 1). Determining patient risk factors for unplanned dialysis was listed as an objective in 12 studies; all of these studies were retrospective or included incident dialysis patients.2-5,19,21,23,24,26,39,48,53
There were 24 studies that reported patient characteristics by unplanned versus planned dialysis status using descriptive, univariate analysis.2-6,8,9,15,19,21-28,34,38,39,48,51-53 Supplementary Table 1 summarizes the characteristics reported across studies and whether the characteristic significantly differed, based on a P value <.05, between patients with an unplanned versus planned dialysis start. All characteristics significantly associated with unplanned dialysis (P < .05) in univariate analysis are summarized in Table 2. The most common risk factors in univariate analysis were (number of studies) increased age (n = 7),3,5,6,24,25,28,38 cause of kidney disease (n = 6),3,5,23,24,48,53 congestive heart failure (n = 5),3,5,9,39,53 cardiovascular disease (n = 7),3-6,9,28,53 lower serum hemoglobin (n = 9),2,3,6,9,15,23,24,27,39 lower serum albumin (n = 10),2,3,6,15,23-25,39,48,53 lower serum calcium (n = 5),6,15,23,24,48 higher serum phosphate (n = 6),2,6,15,24,39,48 higher serum creatinine or lower eGFR/creatinine clearance at dialysis initiation (n = 7),2,6,15,23-25,48 late referral to a nephrologist (n = 6),3-5,27,28,52 lack of dialysis education (n = 6),2,23,24,39,48,53 and not followed in a dedicated predialysis clinic prior to dialysis initiation (n = 5).2,15,24,26,38 There was one study that reported a higher eGFR and lower serum creatinine in patients with an unplanned dialysis start.53 For cause of kidney disease, polycystic kidney disease, all genetic kidney disease, and glomerulonephritis were less common in patients with an unplanned start.3,15,24,53 Nephrosclerosis, renal artery stenosis, and diabetic nephropathy were more common in patients with an unplanned start.3,5,53
Table 2.
Characteristics Significantly Associated With Unplanned Dialysis in Univariate Analysis.
| Demographics |
Comorbidities |
Biochemistry |
Nephrology Care |
Medications | |||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Increased age | Race | Single | Social supports | Rural residence | Charlson comorbidity Index | Other comorbidity score | Congestive heart failure | Cause of kidney disease | BMI/Weight | Diabetes | Cardiovascular disease | Peripheral vascular disease | COPD | Smoking | Polycystic kidney disease | Higher systolic blood pressure | Cancer | Bed bound | Lower serum albumin | Lower serum hemoglobin | eGFR or CrCl at dialysis initiation | Creatinine at dialysis initiation | Lower serum calcium | Phosphate | Parathyroid hormone | eGFR variability | eGFR at first visit | Creatinine at first visit | Sodium | Urea | Ferritin | Late referral | Predialysis clinic | Dialysis education | Kidney Transplant clinic follow-up | Time known to nephrology | Medical visits in the prior year | Time from RRT discussion and start | Time from access referral to RRT | Number of nephrology visits | Phosphate Binders | Erythropoietin use | Intravenous iron use | Renin Angiotensin Inhibitors | Calcium channel blockers | |
| Patients with CKD known to nephrology | |||||||||||||||||||||||||||||||||||||||||||||||
| Holland and Lam5 | • | • | • | • | • | • | |||||||||||||||||||||||||||||||||||||||||
| Arora et al52 | • | ||||||||||||||||||||||||||||||||||||||||||||||
| Brown et al53 | • | • | • | • | • | • | • | • | • | • | • | • | • | ||||||||||||||||||||||||||||||||||
| Prieto-Velasco et al51 | • | ||||||||||||||||||||||||||||||||||||||||||||||
| Incident dialysis patients | |||||||||||||||||||||||||||||||||||||||||||||||
| Metcalfe et al25 | • | • | • | • | • | ||||||||||||||||||||||||||||||||||||||||||
| Loos et al9a | • | • | • | • | |||||||||||||||||||||||||||||||||||||||||||
| Marron et al23 | • | • | • | • | • | • | • | • | • | ||||||||||||||||||||||||||||||||||||||
| Castellano et al15 | • | • | • | • | • | • | • | • | • | • | • | ||||||||||||||||||||||||||||||||||||
| Marron et al24 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | ||||||||||||||||||||||||||||||||
| Buck et al2 | • | • | • | • | • | • | • | • | • | • | • | ||||||||||||||||||||||||||||||||||||
| Wu et al34 | • | ||||||||||||||||||||||||||||||||||||||||||||||
| Crews et al4 | • | • | • | • | • | • | • | • | |||||||||||||||||||||||||||||||||||||||
| Mendelssohn et al6 | • | • | • | • | • | • | • | • | • | ||||||||||||||||||||||||||||||||||||||
| Piwko28 | • | • | • | ||||||||||||||||||||||||||||||||||||||||||||
| Chiu et al3 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | |||||||||||||||||||||||||||||||||
| Nadeau-Fredette et al26b | • | • | • | ||||||||||||||||||||||||||||||||||||||||||||
| Park et al27 | • | • | • | • | |||||||||||||||||||||||||||||||||||||||||||
| Marron et al48 | • | • | • | • | • | • | • | • | |||||||||||||||||||||||||||||||||||||||
| Kanno et al38c | • | • | • | • | • | • | |||||||||||||||||||||||||||||||||||||||||
| Li et al39 | • | • | • | • | • | • | • | ||||||||||||||||||||||||||||||||||||||||
Note. BMI = body mass index; COPD = chronic obstructive pulmonary disease; CrCl = creatinine clearance; eGFR = estimated glomerular filtration rate; RRT = renal replacement therapy.
Markers indicate statistically significant associations with unplanned dialysis (P < .05).
Study included hospitalized incident chronic dialysis patients ≥70 years with a predialysis CrCl <15 mL/min or creatinine >600 μmol.
Study included patients on home hemodialysis.
Study included patients ≥85 years initiating hemodialysis.
There were 10 studies that used multivariable analysis or propensity matching to examine the association of patient characteristics with unplanned dialysis.2-5,26,31,39,48,49,53 All patient characteristics significantly associated with unplanned dialysis in multivariable or matched analyses (P < .05) are summarized in Table 3. The most commonly reported risk factors were increased age (n = 4),2,3,5,31 increased comorbidity score (n = 3),3,26,31 late referral to nephrology (n = 5),3-5,31,48 and lower eGFR at dialysis initiation (n = 3).2,39,48 Less cumulative nephrology care and less care during the period shortly prior to dialysis initiation (critical period) were significant in adjusted analyses (n = 1), as were other potential markers of quality of care (care in a predialysis clinic [n = 1] and dialysis education [n = 1]).2,31,49
Table 3.
Characteristics Associated With Unplanned Dialysis in Multivariable Analysis.
| Demographics |
Comorbidities |
Biochemistry |
Nephrology care |
Meds | |||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Younger age | Increased age | Race | Single | Low socioeconomic status | Social supports | Rural residence | Charlson comorbidity index | Other comorbidity score | Congestive heart failure | Cause of kidney disease | BMI/weight | Diabetes | Cardiovascular disease | Peripheral vascular disease | COPD | Smoking | Polycystic kidney disease | Higher systolic blood pressure | Valvular heart disease | Lower serum albumin | Lower serum hemoglobin | eGFR or CrCl at dialysis initiation | Creatinine at dialysis initiation | eGFR at first visit | Phosphate | Parathyroid hormone | Urea | Cumulative care | Late referral | Consistent critical care period care | Predialysis clinic | Dialysis education | Kidney Transplant clinic follow-up | Center | Time known to nephrology | Year of RRT start | Time from RRT discussion and start | Time from access referral to RRT | Number of nephrology visits | Phosphate binders | Erythropoietin use | |
| Patients with CKD known to nephrology | |||||||||||||||||||||||||||||||||||||||||||
| Holland and Lam5 | • | • | • | ||||||||||||||||||||||||||||||||||||||||
| Cho et al49a | • | ||||||||||||||||||||||||||||||||||||||||||
| Brown et al53 | • | • | • | ||||||||||||||||||||||||||||||||||||||||
| Incident dialysis patients | |||||||||||||||||||||||||||||||||||||||||||
| Buck et al2 | ▯ | • | ▯ | ▯ | ▯ | ▯ | • | ▯ | • | ▯ | • | ▯ | ▯ | ▯ | ▯ | ||||||||||||||||||||||||||||
| Crews et al4b | • | ||||||||||||||||||||||||||||||||||||||||||
| Chiu et al3 | • | • | ▯ | ▯ | ▯ | ▯ | ▯ | ▯ | ▯ | ▯ | • | ||||||||||||||||||||||||||||||||
| Nadeau-Fredette et al26c | ▯ | • | ▯ | • | • | ||||||||||||||||||||||||||||||||||||||
| Singhal et al31 | •^ | • | • | • | • | • | • | ||||||||||||||||||||||||||||||||||||
| Marron et al48 | • | • | • | • | |||||||||||||||||||||||||||||||||||||||
| Li et al39 | • | • | • | • | • | ||||||||||||||||||||||||||||||||||||||
Note. BMI = body mass index; COPD = chronic obstructive pulmonary disease; CrCl = creatinine clearance; eGFR = estimated glomerular filtration rate; RRT = renal replacement therapy.
Shaded boxes indicate variables included in multivariable model.
indicates variables that were removed from the multivariable model in stepwise regression.
Markers indicate statistically significant associations with unplanned dialysis (P < .05).
Female sex.
Propensity score matching.
Unclear if other variables were significant in multivariable analysis. Results only reported for late referral.
Study included patients on home hemodialysis.
Hughes et al21 examined potential underlying causes for unplanned dialysis in patients referred to a nephrologist >12 months prior to dialysis initiation and found the following causes of unplanned dialysis: patient-related delays (31%), acute on chronic kidney injury (31%), surgical delays (16%), late decision-making by the nephrologist (8.6%), and other (12.5%). Marron et al48 also examined reasons for unplanned dialysis and found a similar result, despite being conducted in another country: patient-related delays (36%), acute on chronic kidney injury or more rapid decline in eGFR than anticipated (28%), health care bureaucracy issues (11%).
Assessment of Study Quality
Study quality was assessed for the 26 studies that reported patient characteristics and their association with unplanned dialysis.2-6,8,9,15,19,21-28,31,34,38,39,48,49,51-53 One of the 26 studies was a secondary analysis of the Mendelssohn et al study.28 Study quality reported using a modified NOS is summarized in Supplementary Table 2. Only one study was awarded all 4 possible points for cohort selection. Unfortunately, this study was not primarily designed to examine risk factors for unplanned dialysis.51 Most studies lost a point for cohort selection because they were retrospective or included incident dialysis patients. The studies by Nadeau-Fredette et al,26 Kanno et al,38 and Loos et al9 lost 2 points for cohort selection because they only included home hemodialysis and very elderly patients, which are both a select group of patients. There were 16 studies that received 0 points for comparability because the study design or analysis did not address potential confounding, meaning that no form of statistical adjustment or matching was performed.6,8,9,15,19,21-25,27,28,34,38,51,52
Discussion
This systematic review of literature published until February 2018 includes 48 studies that outlined criteria for unplanned dialysis, of which 26 studies reported patient characteristics associated with unplanned dialysis, and 10 studies adjusted for covariates in multivariable models to identify independent associations. Increased age, increased comorbidity burden, late referral to nephrology, and lower eGFR at dialysis initiation were the most common independent risk factors for unplanned dialysis. The published literature is limited by the retrospective, cross-sectional, and often unadjusted, confounded nature of the data, along with varying terminology and criteria used to define unplanned dialysis across studies.
In univariate, unadjusted analyses, a lower hemoglobin, lower serum albumin, higher serum phosphate, lower serum calcium, and lower eGFR at dialysis initiation were often more common in patients with unplanned dialysis starts. However, these characteristics were often not examined in adjusted analyses or did not always persist as risk factors in multivariable analysis.2,3,6,15,23,24 The independent association of factors such as lower hemoglobin, calcium, or higher phosphate with unplanned dialysis is questionable, given that these characteristics may be surrogate markers for poor predialysis care or patient nonadherence, and were only measured once at dialysis initiation. Lower eGFR at dialysis initiation could be due to late referral, a higher rate of eGFR decline, or patient, physician, or system-related delays with respect to RRT preparation. The retrospective nature of the data makes it difficult to comment on the underlying reasons for observed associations.
Increased age was an independent risk factor in 4 studies following adjustment for comorbidity burden and late referral.2,3,5,31 This could be due to physician-related factors; nephrologists may delay discussions about dialysis with elderly patients due to the uncertainty of meaningful survival and quality of life benefits and the high competing risk of death.54-60 As well, the benefits of arteriovenous fistulas in elderly patients are uncertain; therefore, nephrologists may decide that initiation of hemodialysis with a CVC, if needed, is entirely appropriate.61-63 For these reasons, labeling all dialysis starts with a CVC as unplanned is contentious. Increased age may be associated with unplanned dialysis primarily due to increased “planned” CVC use, but studies that included access criteria in the definition for unplanned dialysis did not differentiate between CVC insertions under planned, stable conditions in the outpatient setting versus urgent conditions during a hospitalization.2,3 Differentiating between planned, elective and urgent, unplanned CVC insertions could help to better delineate the association between age and unplanned dialysis. Another potential contributor to the association between increased age and unplanned dialysis could be that elderly patients are at increased risk for acute illnesses and acute kidney injury.64
The study by Nadeau-Fredette et al26 included only home hemodialysis patients and was the only study that reported younger age as an independent risk factor for unplanned dialysis. This discrepant result is likely due to the fact that home hemodialysis patients are not representative of the general dialysis population. The study by Nadeau-Fredette et al26 also reported that patients with a failed transplant were more likely to have an unplanned dialysis start. This was not examined in other studies but is an interesting finding that suggests an important care gap in preparing patients with a failing transplant for dialysis. Increased comorbidity burden and congestive heart failure were reported as independent risk factors in three3,26,31 and two5,53 studies, respectively. This suggests that patients with multiple medical issues, poor cardiac function, and issues with volume overload may require RRT planning at higher levels of kidney function and closer follow-up. Late referral to nephrology was an independent risk factor in 5 studies.3-5,31,48 The definition of late referral varied in these studies from less than 3 months48 to less than 12 months.3 This finding supports the complexity of optimal RRT preparation, which may be underappreciated by both patients and physicians. Several studies found that follow-up in a dedicated predialysis clinic and the receipt of dialysis education were less common in patients with an unplanned dialysis start.2,15,23,24,26,38,39,48,49,53 These findings were mostly reported in univariate analysis, but suggest that specialized care and education can facilitate the difficult transition onto dialysis. The finding of diabetic nephropathy and nephrosclerosis being more common than genetic kidney disease or glomerulonephritis in patients with unplanned dialysis starts was mostly reported in univariate analyses and may be explained by the fact that patients with diabetic nephropathy and nephrosclerosis tend to be older and have more comorbidities.
A prior systematic review examined outcomes and costs associated with unplanned dialysis and included literature up to 2008. This previously published review by Mendelssohn et al7 included 8 European studies and found that unplanned dialysis was associated with increased morbidity and mortality, along with significant health care costs. Our review includes the 8 studies from the Mendelssohn et al review, along with 40 further studies, and is the first systematic review to summarize the published evidence on risk factors for unplanned dialysis.
Our review benefits from a comprehensive, broad search strategy with all methods clearly defined and prespecified. However, the conclusions of our review are limited for several reasons. Only 12 studies actually specified the determination of risk factors for unplanned dialysis as a study objective and none of these studies had prospective follow-up of patients with CKD.2-5,19,21,23,24,26,39,48,53 Due to the retrospective or cross-sectional nature of the published data, results are largely limited to one-time data collection at dialysis initiation and data collected as part of routine clinical care. As well, many studies did not perform adjusted or matched analyses. The variable terminology and criteria used to define unplanned dialysis makes comparisons across studies difficult. Some studies focused solely on dialysis initiations during a hospitalization or under acute circumstances while other studies also included dialysis initiations with a CVC in their definition of unplanned dialysis. As well, not all studies that included incident dialysis patients specified the exclusion of patients with AKI (without prior CKD) requiring dialysis (Table 1). Such patients would obviously require inpatient/urgent dialysis with a CVC but are not of interest when considering the issue of risk factors for planned versus unplanned dialysis. Finally, some studies were conducted more than 10 years ago, and practice patterns with respect to predialysis care and dialysis initiation have changed. In particular, national guidelines have adopted a delayed approach to dialysis initiation, largely based on the results of the Initiating Dialysis Early and Late (IDEAL) Trial.65-67 There may also be regional or country-specific practice patterns and patient population differences that are not fully captured by the published data, ie, there are very little data from the United States published on this topic.4
Conclusions
High-quality data on patient risk factors for unplanned dialysis are lacking. As a first step toward reducing the incidence of unplanned dialysis starts, well-designed studies to determine modifiable risk factors are needed. Potential modifiable factors could include the timing of RRT education and factors that impact patient adherence and decision-making. The lack of a consensus definition for unplanned dialysis makes research and quality improvement initiatives in this area more challenging.
Supplemental Material
Supplemental material, Supplementary_Tables_and_appendix_A,_B,_C_final_CJKHD for Risk Factors for Unplanned Dialysis Initiation: A Systematic Review of the Literature by Rana Hassan, Ayub Akbari, Pierre A. Brown, Swapnil Hiremath, K. Scott Brimble and Amber O. Molnar in Canadian Journal of Kidney Health and Disease
Footnotes
Author Contributions: A.O.M., S.H., and A.A. contributed to conception and design of the study; A.O.M., S.H., A.A., K.S.B., and P.A.B. provided intellectual content of critical importance to the work described; A.O.M. and R.H. interpreted the data; R.H. and A.O.M. drafted the first version of the article and revisions; all authors read and approved the final version of the article.
Availability of Data and Materials: This study is a systematic review of previously published data and materials.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: K.S.B. reports the receipt of personal fees from the Ontario Renal Network unrelated to this work.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Amber O. Molnar receives salary support from the KRESCENT Foundation and the McMaster Department of Medicine. The funders had no role in the study or in the writing of this report.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD: Swapnil Hiremath  https://orcid.org/0000-0003-0010-3416
https://orcid.org/0000-0003-0010-3416
References
- 1. Combes C, Sein K, Allen K. How does pre-dialysis education need to change? Findings form a qualitative study with staff and patients. BMC Nephrology. 2017;18:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Buck J, Baker R, Cannaby A-M, Nicholson S, Peters J, Warwick G. Why do patients known to renal services still undergo urgent dialysis initiation? A cross-sectional survey. Nephrol Dial Transplant. 2007;22:3240-3245. [DOI] [PubMed] [Google Scholar]
- 3. Chiu K, Alam A, Iqbal S. Predictors of suboptimal and crash initiation of dialysis at two tertiary care centers. Hemodial Int. 2012;16(suppl 1):S39-S46. [DOI] [PubMed] [Google Scholar]
- 4. Crews DC, Jaar BG, Plantinga LC, Kassem HS, Fink NE, Powe NR. Inpatient hemodialysis initiation: reasons, risk factors and outcomes. Nephron Clin Pract. 2010;114:c19-c28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Holland DC, Lam M. Suboptimal dialysis initiation in a retrospective cohort of predialysis patients—predictors of in-hospital dialysis initiation, catheter insertion and one-year mortality. Scand J Urol Nephrol. 2000;34:341-347. [DOI] [PubMed] [Google Scholar]
- 6. Mendelssohn DC, Curtis B, Yeates K, et al. Suboptimal initiation of dialysis with and without early referral to a nephrologist. Nephrol Dial Transplant. 2011;26:2959-2965. [DOI] [PubMed] [Google Scholar]
- 7. Mendelssohn DC, Malmberg C, Hamandi B. An integrated review of “unplanned” dialysis initiation: reframing the terminology to “suboptimal” initiation. BMC Nephrol. 2009;10:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Caskey FJ, Wordsworth S, Ben T, et al. Early referral and planned initiation of dialysis: what impact on quality of life? Nephrol Dial Transplant. 2003;18:1330-1338. [DOI] [PubMed] [Google Scholar]
- 9. Loos C, Briancon S, Frimat L, Hanesse B, Kessler M. Effect of end-stage renal disease on the quality of life of older patients. J Am Geriatr Soc. 2003;51:229-233. [DOI] [PubMed] [Google Scholar]
- 10. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 11. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-e34. [DOI] [PubMed] [Google Scholar]
- 12. Molnar AO, Hiremath S, Brown PA, Akbari A. Risk factors for unplanned and crash dialysis starts: a protocol for a systematic review and meta-analysis. Syst Rev. 2016;5:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Abderrahim E, Zouaghi K, Hedri H, et al. Renal replacement therapy for diabetic end-stage renal disease. Experience of a Tunisian hospital centre. Diabetes Metab. 2001;27:584-590. [PubMed] [Google Scholar]
- 14. Al-Jaishi AA, Lok CE, Garg AX, Zhang JC, Moist LM. Vascular access creation before hemodialysis initiation and use: a population-based cohort study. Clin J Am Soc Nephrol. 2015;10:418-427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Castellano I, Gallego S, Labrador PJ, Gomez-Martino JR, Covarsi A. [The start of renal replacement therapy in a Spanish department]. Nefrologia. 2006;26:445-451. [PubMed] [Google Scholar]
- 16. Couchoud C, Moranne O, Frimat L, Labeeuw M, Allot V, Stengel B. Associations between comorbidities, treatment choice and outcome in the elderly with end-stage renal disease. Nephrol Dial Transplant. 2007;22:3246-3254. [DOI] [PubMed] [Google Scholar]
- 17. Descamps C, Labeeuw M, Trolliet P, et al. Confounding factors for early death in incident end-stage renal disease patients: role of emergency dialysis start. Hemodial Int. 2011;15:23-29. [DOI] [PubMed] [Google Scholar]
- 18. Frimat L, Loos-Ayav C, Panescu V, Cordebar N, Briancon S, Kessler M. Early referral to a nephrologist is associated with better outcomes in type 2 diabetes patients with end-stage renal disease. Diabetes Metab. 2004;30:67-74. [DOI] [PubMed] [Google Scholar]
- 19. Gomis Couto A, Teruel Briones JL, Fernandez Lucas M, et al. Causes of unplanned hemodialysis initiation. Nefrologia. 2011;31:733-737. [DOI] [PubMed] [Google Scholar]
- 20. Hdez Ordonez SO, Walton SM, Ramos A, Valle L, Rivera AS, Liu FX. Economic burden of incident unplanned starts on peritoneal dialysis in a high specialty health care facility in Mexico City. Value Health Reg Issues. 2012;1:184-189. [DOI] [PubMed] [Google Scholar]
- 21. Hughes SA, Mendelssohn JG, Tobe SW, McFarlane PA, Mendelssohn DC. Factors associated with suboptimal initiation of dialysis despite early nephrologist referral. Nephrol Dial Transplant. 2013;28:392-397. [DOI] [PubMed] [Google Scholar]
- 22. Lobbedez T, Verger C, Ryckelynck J-P, Fabre E, Evans D. Outcome of the sub-optimal dialysis starter on peritoneal dialysis. Nephrol Dial Transplant. 2013;28:1276-1283. [DOI] [PubMed] [Google Scholar]
- 23. Marron B, Martinez Ocana JC, Salgueira M, et al. Analysis of patient flow into dialysis: role of education in choice of dialysis modality. Perit Dial Int. 2005;25(suppl 3):S56-S59. [PubMed] [Google Scholar]
- 24. Marron B, Ortiz A, de Sequera P, et al. Impact of end-stage renal disease care in planned dialysis start and type of renal replacement therapy—a Spanish multicentre experience. Nephrol Dial Transplant. 2006;21(suppl 2):ii51-ii55. [DOI] [PubMed] [Google Scholar]
- 25. Metcalfe W, Khan IH, Prescott GJ, Simpson K, MacLeod AM. Can we improve early mortality in patients receiving renal replacement therapy? Kidney Int. 2000;57:2539-2545. [DOI] [PubMed] [Google Scholar]
- 26. Nadeau-Fredette A-C, Tennankore KK, Kim SJ, Chan CT. Suboptimal initiation of home hemodialysis: determinants and clinical outcomes. Nephron Clin Pract. 2013;124:132-140. [DOI] [PubMed] [Google Scholar]
- 27. Park JI, Kim M, Kim H, et al. Not early referral but planned dialysis improves quality of life and depression in newly diagnosed end stage renal disease patients: a prospective cohort study in Korea. PLoS ONE. 2015;10:e0117582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Piwko C, Vicente C, Marra L, et al. The STARRT trial: a cost comparison of optimal vs sub-optimal initiation of dialysis in Canada. J Med Econ. 2012;15:96-104. [DOI] [PubMed] [Google Scholar]
- 29. Ravani P, Marinangeli G, Stacchiotti L, Malberti F. Structured pre-dialysis programs: more than just timely referral? J Nephrol. 2003;16:862-869. [PubMed] [Google Scholar]
- 30. Ravani P, Marinangeli G, Tancredi M, Malberti F. Multidisciplinary chronic kidney disease management improves survival on dialysis. J Nephrol. 2003;16:870-877. [PubMed] [Google Scholar]
- 31. Singhal R, Hux JE, Alibhai SMH, Oliver MJ. Inadequate predialysis care and mortality after initiation of renal replacement therapy. Kidney Int. 2014;86:399-406. [DOI] [PubMed] [Google Scholar]
- 32. Teo BW, Ma V, Xu H, Li J, Lee EJ, Nephrology Clinical Research Group. Profile of hospitalisation and death in the first year after diagnosis of end-stage renal disease in a multi-ethnic Asian population. Ann Acad Med Singapore. 2010;39:79-87. [PubMed] [Google Scholar]
- 33. Thilly N, Boini S, Loos-Ayav C, Kessler M, Briancon S, Frimat L. Factors associated with anemia among incident pre-dialysis patients managed within a French care network. Clin Nephrol. 2007;67:81-88. [DOI] [PubMed] [Google Scholar]
- 34. Wu L-C, Lin M-Y, Hsieh C-C, et al. Planned creation of vascular access saves medical expenses for incident dialysis patients. Kaohsiung J Med Sci. 2009;25:521-529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yoon HE, Chung S, Chung HW, et al. Status of initiating pattern of hemodialysis: a multi-center study. J Korean Med Sci. 2009;24(suppl 1):S102-S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bechade C, Dejardin O, Bara S, et al. Incidence and characteristics of chronic renal replacement therapy in patients with cancer: data from kidney and cancer registries in Basse-Normandie. J Nephrol. 2018;31:111-118. [DOI] [PubMed] [Google Scholar]
- 37. Jin H, Fang W, Zhu M, et al. Urgent-start peritoneal dialysis and hemodialysis in ESRD patients: complications and outcomes. PLoS ONE. 2016;11:e0166181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kanno A, Nakayama M, Sanada S, Sato M, Sato T, Taguma Y. Suboptimal initiation predicts short-term prognosis and vulnerability among very elderly patients who start haemodialysis. Nephrology (Carlton). 2019;24:94-101. [DOI] [PubMed] [Google Scholar]
- 39. Li W-Y, Wang Y-C, Hwang S-J, Lin S-H, Wu K-D, Chen Y-M. Comparison of outcomes between emergent-start and planned-start peritoneal dialysis in incident ESRD patients: a prospective observational study. BMC Nephrol. 2017;18:359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Machowska A, Alscher MD, Reddy Vanga S, et al. Factors influencing access to education, decision making, and receipt of preferred dialysis modality in unplanned dialysis start patients. Patient Prefer Adherence. 2016;10:2229-2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Machowska A, Alscher MD, Vanga SR, et al. Offering Patients Therapy Options in Unplanned Start (OPTiONS): implementation of an educational program is feasible and effective. BMC Nephrol. 2017;18:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Machowska A, Alscher MD, Vanga SR, et al. Dialysis access, infections, and hospitalisations in unplanned dialysis start patients: results from the OPTiONS study. Int J Artif Organs. 2017;40:48-59. [DOI] [PubMed] [Google Scholar]
- 43. Machowska A, Alscher MD, Vanga SR, Koch M, Aarup M, Rutherford P. Offering patients therapy options in unplanned start: development and implementation of an education program for unplanned-start patients. Adv Perit Dial. 2015;31:69-73. [PubMed] [Google Scholar]
- 44. Magalhaes LP, Dos Reis LM, Graciolli FG, et al. Predictive factors of one-year mortality in a cohort of patients undergoing urgent-start hemodialysis. PLoS ONE. 2017;12:e0167895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Panocchia N, Tazza L, Di Stasio E, et al. Mortality in hospitalized chronic kidney disease patients starting unplanned urgent haemodialysis. Nephrology (Carlton). 2016;21:62-67. [DOI] [PubMed] [Google Scholar]
- 46. Schanz M, Ketteler M, Heck M, Dippon J, Alscher MD, Kimmel M. Impact of an in-hospital patient education program on choice of renal replacement modality in unplanned dialysis initiation. Kidney Blood Press Res. 2017;42:865-876. [DOI] [PubMed] [Google Scholar]
- 47. Vigneau C, Kolko A, Stengel B, et al. Ten-years trends in renal replacement therapy for end-stage renal disease in mainland France: lessons from the French Renal Epidemiology and Information Network (REIN) registry. Nephrol Ther. 2017;13:228-235. [DOI] [PubMed] [Google Scholar]
- 48. Marron B, Ostrowski J, Torok M, et al. Type of referral, dialysis start and choice of renal replacement therapy modality in an international integrated care setting. PLoS ONE. 2016;11:e0155987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Cho EJ, Park HC, Yoon HB, et al. Effect of multidisciplinary pre-dialysis education in advanced chronic kidney disease: propensity score matched cohort analysis. Nephrology (Carlton). 2012;17:472-479. [DOI] [PubMed] [Google Scholar]
- 50. Joly D, Anglicheau D, Alberti C, et al. Octogenarians reaching end-stage renal disease: cohort study of decision-making and clinical outcomes. J Am Soc Nephrol. 2003;14:1012-1021. [DOI] [PubMed] [Google Scholar]
- 51. Prieto-Velasco M, Quiros P, Remon C, Spanish Group for the Implementation of a Shared Decision Making Process for RRT Choice with Patient Decision Aid Tools. The concordance between patients’ renal replacement therapy choice and definitive modality: is it a Utopia? PLoS ONE. 2015;10:e0138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Arora P, Elkin PL, Eberle J, et al. An observational study of the quality of care for chronic kidney disease: a Buffalo and Albany, New York metropolitan area study. BMC Nephrol. 2015;16:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Brown PA, Akbari A, Molnar AO, et al. Factors associated with unplanned dialysis starts in patients followed by nephrologists: a retrospective cohort study. PLoS ONE. 2015;10:e0130080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Brown MA, Collett GK, Josland EA, Foote C, Li Q, Brennan FP. CKD in elderly patients managed without dialysis: survival, symptoms, and quality of life. Clin J Am Soc Nephrol. 2015;10:260-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Carson RC, Juszczak M, Davenport A, Burns A. Is maximum conservative management an equivalent treatment option to dialysis for elderly patients with significant comorbid disease? Clin J Am Soc Nephrol. 2009;4:1611-1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Chandna SM, Da Silva-Gane M, Marshall C, Warwicker P, Greenwood RN, Farrington K. Survival of elderly patients with stage 5 CKD: comparison of conservative management and renal replacement therapy. Nephrol Dial Transplant. 2011;26:1608-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Murtagh FE, Marsh JE, Donohoe P, Ekbal NJ, Sheerin NS, Harris FE. Dialysis or not? A comparative survival study of patients over 75 years with chronic kidney disease stage 5. Nephrol Dial Transplant. 2007;22:1955-1962. [DOI] [PubMed] [Google Scholar]
- 58. O’Connor NR, Kumar P. Conservative management of end-stage renal disease without dialysis: a systematic review. J Palliat Med. 2012;15:228-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Verberne WR, Geers AB, Jellema WT, Vincent HH, van Delden JJ, Bos WJ. Comparative survival among older adults with advanced kidney disease managed conservatively versus with dialysis. Clin J Am Soc Nephrol. 2016;11:633-640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med. 2009;361:1539-1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Moist LM, Lok CE, Vachharajani TJ, et al. Optimal hemodialysis vascular access in the elderly patient. Semin Dial. 2012;25:640-648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Quinn R, Ravani P. ACCESS HD pilot: a randomised feasibility trial comparing catheters with fistulas in elderly patients starting haemodialysis. BMJ Open. 2016;6:e013081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Vachharajani TJ, Moist LM, Glickman MH, et al. Elderly patients with CKD—dilemmas in dialysis therapy and vascular access. Nat Rev Nephrol. 2014;10:116-122. [DOI] [PubMed] [Google Scholar]
- 64. Anderson S, Eldadah B, Halter JB, et al. Acute kidney injury in older adults. J Am Soc Nephrol. 2011;22:28-38. [DOI] [PubMed] [Google Scholar]
- 65. Cooper BA, Branley P, Bulfone L, et al. A randomized, controlled trial of early versus late initiation of dialysis. N Engl J Med. 2010;363:609-619. [DOI] [PubMed] [Google Scholar]
- 66. Tattersall J, Dekker F, Heimburger O, et al. When to start dialysis: updated guidance following publication of the Initiating Dialysis Early and Late (IDEAL) study. Nephrol Dial Transplant. 2011;26:2082-2086. [DOI] [PubMed] [Google Scholar]
- 67. Nesrallah GE, Mustafa RA, Clark WF, et al. Canadian Society of Nephrology 2014 clinical practice guideline for timing the initiation of chronic dialysis. CMAJ. 2014;186:112-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_Tables_and_appendix_A,_B,_C_final_CJKHD for Risk Factors for Unplanned Dialysis Initiation: A Systematic Review of the Literature by Rana Hassan, Ayub Akbari, Pierre A. Brown, Swapnil Hiremath, K. Scott Brimble and Amber O. Molnar in Canadian Journal of Kidney Health and Disease