Abstract
Background:
Previous meta-analyses have been conducted to compare outcomes of various treatment injections for lateral epicondylitis (LE), including corticosteroid injection (CSI) and autologous blood products such as autologous blood (AB) and platelet-rich plasma (PRP).
Purpose:
To conduct a systematic review of overlapping meta-analyses comparing different injection treatments (CSI, AB, PRP) for LE to determine which meta-analyses provide the best available evidence.
Study Design:
Systematic review; Level of evidence, 2.
Methods:
A systematic review was performed by searching PubMed, Embase, and the Cochrane Library to locate meta-analyses that compared clinical outcomes of CSI, AB, and PRP for the treatment of LE. Search terms included “injection,” “corticosteroid,” “platelet-rich plasma,” “autologous blood,” “tennis elbow,” “lateral epicondylitis,” and “meta-analysis.” Results were reviewed to determine study eligibility. Patient outcomes were extracted from these meta-analyses. Meta-analysis quality was assessed with the Oxman-Guyatt and Quality of Reporting of Meta-analyses (QUOROM) systems. The Jadad decision algorithm was then used to determine which meta-analyses provided the best level of evidence.
Results:
Nine meta-analyses (two level 1 studies, seven level 2 studies) containing 8656 patients met the eligibility criteria. Seven meta-analyses found that autologous blood products such as AB and PRP significantly improved pain and elbow function in the intermediate term (12-26 weeks), while 4 studies found that CSI effectively relieved pain and improved elbow function in the short term (<12 weeks). The study by Arirachakaran et al in 2016 received the highest QUOROM and Oxman-Guyatt scores; therefore, this meta-analysis appears to have the highest level of evidence. In addition, this study was rated the highest-quality study in this systematic review according to the Jadad decision algorithm. Lower-quality meta-analyses indicated that dosage, number of injections, and differences in therapeutic duration between CSI and autologous blood products may be essential factors in determining the appropriate treatment injection protocol for LE.
Conclusion:
The current best available evidence suggests that CSI improves functional outcomes and pain relief in the short term, while AB and PRP are the most effective treatments in the intermediate term.
Keywords: injection, corticosteroid, platelet-rich plasma, autologous blood, tennis elbow
Lateral epicondylitis (LE), more commonly known as tennis elbow, is frequently diagnosed among individuals aged 35 to 50 years and affects approximately 1% to 3% of the general population.1,23,29 The dominant elbow is more commonly affected owing to repetitive/forceful occupational or athletic activities involving wrist extension and supination.29,30,33 Symptoms that are usually associated with LE include lateral elbow pain, pain with wrist extension, and weakened grip strength.30,33 With or without treatment, LE is frequently considered a self-limiting condition resolving in approximately 8 to 12 months; however, some patients experience symptoms for years.4,6,12 Treatment of LE includes rest, nonsteroidal anti-inflammatory drugs, splinting, physical therapy, shock wave therapy, injection therapies, and surgery, although none of these are universally effective.1,3,6,16,18,25,28,31,34
The most commonly used injection therapy is corticosteroid injection (CSI), which is extensively used in the treatment of tendinopathy because of the low cost and easy application; however, the effects are short term at reducing pain and improving function.6,25,31 More recently, biological solution injections are being used as an alternate option.1,3,18 Biological therapeutics—termed autologous blood products (ABPs)—such as autologous blood (AB) and platelet-rich plasma (PRP), have been used for the management of orthopaedic diagnoses such as osteoarthritis, bone healing, muscle strain, tendinopathy, ligament, cartilage, and other soft tissue injuries.14,25,35 PRP is prepared from AB and contains an increased concentration of autologous platelets; however, PRP and AB both contain growth factors that might be beneficial for the healing of soft tissue injuries.7,18,22,25,35,36 Multiple studies1,5,6,15,25 have concluded that CSIs are advantageous in the short term, while ABPs may be a more effective treatment modality for pain reduction in the long term.
The purpose of this study was to conduct a systematic review of overlapping meta-analyses comparing different injection treatments (CSI, AB, and PRP) for LE to determine which meta-analyses provide the best available evidence.
Methods
The methods of this study are similar to previous systematic reviews of overlapping meta-analyses.10,17 Two independent reviewers (D.A.H., L.B.T.) searched the PubMed, Embase, and Cochrane Library databases up to June 8, 2017. The following search terms were used: “injection,” “corticosteroid,” “platelet-rich plasma,” “autologous blood,” “tennis elbow,” “lateral epicondylitis,” and “meta-analysis.” Inclusion criteria consisted of meta-analyses that compared at least 2 of the 3 injection therapies for LE (AB, PRP, and CSI). Exclusion criteria consisted of (1) systematic reviews that did not pool data or perform a meta-analysis and (2) meta-analyses without at least 2 of the 3 injection therapies for LE. The full articles of all studies that met the inclusion and exclusion criteria were obtained by 2 reviewers (D.A.H., L.B.T.). The authors then thoroughly reviewed the articles to confirm that all pertinent studies were included in this systematic review.
From the studies that met inclusion and exclusion criteria, the following data were collected: primary author, year of publication, levels of evidence included, number and publication dates of primary studies included, inclusion and exclusion criteria, performance of heterogeneity analytics, patient demographics, follow-up period, duration of disease, patient-reported outcomes, and objective outcomes. The following outcome scores were collected: adverse events, escape treatments/nonresponses, upper extremity function,24 grip strength, Patient-Rated Tennis Elbow Evaluation,27 visual analog scale (VAS) for pain,9 DASH (Disabilities of the Arm, Shoulder and Hand) score,11 Likert global assessment scale,2 pressure pain threshold,32 EQ-5D (EuroQoL score),8 Roles and Maudsley score,26 and Nirschl score.20
The number of “possible” previous meta-analyses cited relative to the number “actually” cited was recorded, as was the database used in the literature search. Additionally, the primary studies and their type (eg, randomized controlled trial and prospective comparative studies) were recorded. We also recorded which studies included the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. We scored the meta-analyses using the Oxman-Guyatt quality appraisal tool.21 The methodological quality of these meta-analyses was scored with the Quality of Reporting of Meta-analyses (QUOROM) system.19 This scoring system assesses meta-analyses based on the quality of their methodology and reporting in 18 categories. Of the meta-analyses that met criteria, each category was awarded a point, with a total of 18 possible points. Any known biases were recorded within the reviewed literature.
We used the Jadad decision algorithm to guide interpretation of discordant meta-analyses. Jadad et al13 described 6 discordant sources among meta-analyses: clinical question, study selection and inclusion, data extraction, assessment of study quality, assessment of the ability to combine studies, and statistical methods for data synthesis. Two authors (D.A.H., L.B.T.) independently applied the Jadad decision algorithm and compared results to determine which of the included meta-analyses proposed the best treatment option for tennis elbow through the current best evidence. When discrepancies were present, the 2 reviewers discussed the results and came to agreement.
Results
The initial search revealed 36 total articles. Of these, 9 studies1,3,6,15,18,25,28,31,34 met the inclusion and exclusion criteria and are included in this systematic review. These studies were published between 2012 and 2017, with all 9 studies performing a meta-analysis. The number of primary studies included in these meta-analyses ranged from 4 studies31 to 26 studies.6 The number of patients analyzed ranged from 307 patients34 to 2280 patients,28 with a mean of 962 per study. All of the studies described patients receiving CSIs, with a mean of 283 patients being treated. Eight1,3,6,15,25,28,31,34 studies described sample sizes of patients receiving AB injections, with a mean of 126 patients being treated, while 7 studies1,3,6,15,18,25,28 described sample sizes of patients receiving PRP injections, with a mean of 118 patients receiving treatment. The follow-up period ranged from 6 to 52 weeks. The mean age ranged from 43 years18 to 47 years,15,28 and the disease duration ranged from 1 month18 to 18 months.1
Assessment of Previous Meta-analysis Literature
The authors of these studies generally cited most of the previously published meta-analyses, with only 1 study34 not citing any of them (Table 1). For 1 study, there were no previous meta-analyses to cite,15 whereas 4 studies1,3,6,28 cited all available meta-analyses, 1 study25 cited 1 of 2 available meta-analyses, and 1 study18 cited only 2 of the 7 available meta-analyses. These 7 studies,1,3,6,18,25,28,31 which used previously published meta-analyses, most likely were repeated because of limitations of previous meta-analyses, which did not provide strong evidence, owing to methodologically different studies.
TABLE 1.
Systematic Reviews or Meta-analyses Actually Cited Versus Maximum Number That Could Have Been Cited
| Date | Systematic Reviews or Meta-analyses, n | |||
|---|---|---|---|---|
| First Author | Online Publication | Last Literature Search | Possible to Cite | Cited |
| Krogh15 | Sep 2012 | Jun 2011 | 0 | 0 |
| Sayegh28 | Oct 2014 | Jan 2014 | 1 | 1 |
| Chou3 | Jun 2015 | Jun 2014 | 1 | 1 |
| Arirachakaran1 | Sep 2015 | Jan 2015 | 1 | 1 |
| Dong6 | Sep 2015 | Aug 2014 | 1 | 1 |
| Tsikopoulos34 | Feb 2016 | May 2015 | 2 | 0 |
| Qian25 | Mar 2016 | May 2015 | 2 | 1 |
| Sirico31 | Sep 2016 | Apr 2015 | 2 | 1 |
| Mi18 | Mar 2017 | Sep 2016 | 7 | 2 |
Outcome Measures
There was a wide range of clinical outcomes assessed in these meta-analyses (Table 2). The most commonly analyzed outcome, reported by all 9 studies, was VAS for pain, followed by 7 studies1,3,15,18,25,28,34 reporting Patient-Rated Tennis Elbow Evaluation.
TABLE 2.
Outcomes Reported by Each Included Studya
| Krogh15 | Sayegh28 | Chou3 | Arirachakaran1 | Dong6 | Tsikopoulos34 | Qian25 | Sirico31 | Mi18 | |
|---|---|---|---|---|---|---|---|---|---|
| Objective outcomes | |||||||||
| Adverse events | + | − | + | + | − | + | − | − | − |
| Escape treatments/nonresponse | + | + | − | + | − | − | − | − | − |
| Upper extremity function | − | + | + | − | − | + | + | + | − |
| Grip strength | + | + | + | − | − | + | + | − | − |
| Patient-reported outcomes | |||||||||
| PRTEE | + | + | + | + | − | + | + | − | + |
| DASH | − | + | + | + | + | + | + | − | + |
| Pain intensity | + | + | − | − | + | + | + | − | + |
| VAS for pain | + | + | + | + | + | + | + | + | + |
| Roles and Maudsley | + | + | − | − | − | + | − | − | − |
| Nirschl stage | + | − | + | − | − | + | + | − | − |
| Likert scale | − | + | − | − | + | − | − | − | − |
| EQ-5D | − | + | − | − | − | − | − | − | − |
| PPT | − | + | + | + | − | + | − | − | − |
aA plus (+) or minus (–) indicates that an outcome measure was or was not reported, respectively. DASH, Disabilities of the Arm, Shoulder and Hand; EQ-5D, EuroQoL score; PPT, pressure pain threshold; PRTEE, Patient-Rated Tennis Elbow Evaluation; VAS, visual analog scale.
Search Methodology
Every study searched PubMed/Medline as part of the literature search, while 8 of the 9 studies searched the Cochrane Library.3,6,15,18,25,28,31,34 There was variability in the use of other databases, including Embase, Scopus, the Cumulative Index to Nursing and Allied Health Literature, Web of Science, and SpringerLink (Table 3).
TABLE 3.
Search Methodology Used by Each Included Studya
| Databaseb | Primary Studies | Score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First Author | PubMed / Medline |
EMBASE | Cochrane Library | CINAHL | Scopus | Web of Science | SpringerLink | n | Only RCTsc | PRISMAd | Oxman- Guyatt | QUOROM |
| Krogh15 | + | + | + | + | − | + | − | 17 | + | + | 7 | 16 |
| Sayegh28 | + | − | + | − | − | − | − | 22 | + | + | 5 | 18 |
| Chou3 | + | − | + | + | + | − | − | 9 | + | − | 7 | 16 |
| Arirachakaran1 | + | − | − | − | + | − | − | 10 | + | − | 7 | 18 |
| Dong6 | + | + | + | − | − | − | − | 27 | + | + | 5 | 17 |
| Tsikopoulos34 | + | − | + | − | + | + | − | 9 | + | + | 5 | 18 |
| Qian25 | + | + | + | − | − | + | − | 10 | + | + | 5 | 18 |
| Sirico31 | + | + | + | + | + | + | − | 4 | + | + | 7 | 17 |
| Mi18 | + | + | + | − | − | − | + | 8 | + | + | 7 | 17 |
aCINAHL, Cumulative Index to Nursing and Allied Health Literature; EMBASE, Excerpta Medica Database; Medline, Medical Literature Analysis and Retrieval System Online; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; RCT, randomized controlled trial; QUOROM, Quality of Reporting of Meta-analyses.
bA plus (+) or minus (–) indicates that a database was or was not used in the search strategy, respectively.
cA plus (+) indicates that the primary studies included only RCTs.
dA plus (+) or minus (–) indicates that the PRISMA guidelines were or were not used in the search strategy, respectively.
Study Quality and Validity
QUOROM scores were assessed for each study and ranged from 163,15 to 18,1,25,28,34 with 18 being the maximum possible score. The mean and median were each 17. Oxman-Guyatt scores ranged from 56,25,28,34 to 7.1,3,15,18,31 The mean score was 6, with a median of 7 (Table 3).
A total of 54 prospective comparative studies were included among meta-analyses. Appendix Table A1 shows the primary studies in each meta-analysis. Of the 54 prospective studies, 24 were assessed by only 1 meta-analysis, 17 by 2 meta-analyses, 5 by 3 meta-analyses, 2 by 4 meta-analyses, 4 by 5 meta-analyses, 1 by 6 meta-analyses, and 1 by 7 meta-analyses (Table A1).
Study Results
A heterogeneity analysis was performed in all 9 studies.1,3,6,15,18,25,28,31,34 Heterogeneity was assessed with I 2 statistics. Krogh et al15 found no differences between CSI and placebo in terms of pain reduction beyond 8 weeks. The investigators also found that AB and PRP showed a significantly greater improvement as compared with placebo between 8 and 52 weeks.15 Sayegh et al28 compared any form of nonsurgical treatment injection (CSI, PRP, AB, sodium hyaluronate, or glycosaminoglycan polysulfate) or other nonsurgical treatment (physical therapy, shock wave therapy, laser, ultrasound, corticosteroid iontophoresis, topical glyceryl trinitrate, or oral naproxen) with observation only or placebo (saline injection), with a follow-up of at least 6 months. The authors found an overall lack of intermediate- to long-term clinical benefits after any nonsurgical treatment of LE as compared with observation only or placebo.28 However, the aggregation of multiple nonsurgical treatments in the same analysis may counterbalance more effective treatments with less effective treatments.
Chou et al3 compared the clinical outcomes of AB injections with CSIs or PRP injections in treating LE. This study demonstrated that AB was significantly more effective than CSI, but no significant differences were found between AB and PRP. The results reported by Chou et al3 were comparable with those of Krogh et al,15 reporting analogous efficacies of AB and PRP injection in decreasing pain for LE. Arirachakaran et al1 performed a network meta-analysis comparing clinical outcomes among the use of CSI, PRP, and AB injections. The researchers found that PRP can improve pain and lower the risk of complications, but AB has a higher risk of adverse effects despite the ability to improve pain, disability scores, and pressure pain threshold. Dong et al6 conducted a network meta-analysis that evaluated different treatment injections for LE at the intermediate term (6 months) and concluded that PRP and AB injections represent an effective treatment option for LE, while CSI is not recommended. Tsikopoulous et al34 concluded that AB injections provided significantly greater clinical relief as compared with CSI among patients with LE at both intermediate- and medium-term follow-up (8-26 weeks).
Qian et al25 compared ABPs with CSI, grouping AB and PRP into the ABP category, which could have influenced the results, as the 2 have different mechanisms of action. Specifically, the stimulus for repair mechanisms needed for tenocyte proliferation and tendon healing may vary when growth factors are released by the platelets with (AB) or without (PRP) other cytokines or cellular and humoral mediators. Their results were comparable with previous studies supporting the use of CSI for pain relief in the short term, with ABPs being more effective in the intermediate term (6-24 weeks). Sirico et al31 conducted a meta-analysis comparing CSI and AB and found that CSI led to nonsignificantly lower VAS pain scores in the short term, with no differences in the medium term (4-12 weeks) and longer term compared with AB. Additionally, these authors concluded that there is no evidence to support AB injections for longer-term pain management. Finally, Mi et al18 found that CSI could relieve pain and significantly improve function of the elbow in the short term (2-8 weeks), while PRP was the most effective treatment option in terms of pain relief and functional improvement in the intermediate (12 weeks) and longer term (6-12 months).
Heterogeneity Assessment
All 9 studies included in this systematic review performed a heterogeneity analysis. All meta-analyses performed a subgroup or sensitivity analysis to compare study designs, interventions, and outcomes (Table 4). Additional parameters, such as age, sex, dominant elbow, and follow-up interval, were analyzed.
TABLE 4.
Heterogeneity or Subgroup Analyses of Primary Studiesa
| Krogh15 | Sayegh28 | Chou3 | Arirachakaran1 | Dong6 | Tsikopoulos34 | Qian25 | Sirico31 | Mi18 | |
|---|---|---|---|---|---|---|---|---|---|
| Statistical heterogeneity analysis | + | + | + | + | + | + | + | + | + |
| Subgroup or sensitivity analysis | |||||||||
| Primary study quality | + | + | + | + | + | + | + | + | + |
| Age | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Sex | 0 | 0 | − | 0 | 0 | 0 | 0 | 0 | 0 |
| Dominant elbow | − | 0 | 0 | 0 | − | 0 | − | − | − |
| Number of injections | 0 | − | 0 | − | − | + | − | − | − |
| Dosage | 0 | − | 0 | − | 0 | + | 0 | 0 | 0 |
| Follow-up interval | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | − |
| Trial duration | + | 0 | 0 | 0 | 0 | + | + | − | 0 |
| Postintervention protocols | − | − | − | − | − | + | − | − | 0 |
| Pain score | + | 0 | + | + | + | + | + | + | + |
| VAS pain | 0 | 0 | 0 | + | 0 | 0 | 0 | + | 0 |
| PPT | − | 0 | 0 | + | − | 0 | − | − | − |
| Adverse effects / nonresponse rates | 0 | − | 0 | + | − | 0 | 0 | 0 | 0 |
| Overall function | 0 | + | 0 | − | − | + | + | − | + |
| Nirschl score | 0 | − | 0 | − | − | 0 | + | − | − |
| Overall improvement | 0 | + | 0 | − | − | − | − | − | − |
| Treatment failure | − | + | 0 | − | − | − | − | − | − |
| Escape treatment | 0 | + | − | − | − | − | − | − | − |
| Analgesics/NSAIDs | 0 | + | − | − | − | − | − | − | − |
| Outside consultation | 0 | + | − | − | − | − | − | − | − |
| Surgery | 0 | + | − | − | − | − | − | − | − |
| PRTEE | 0 | + | 0 | + | − | 0 | 0 | − | 0 |
| DASH | − | + | 0 | + | 0 | 0 | 0 | − | 0 |
| Pain-free functional index | − | + | − | − | − | − | − | − | − |
| EQ-5D | − | + | − | − | − | − | − | − | − |
| Maximum grip strength | 0 | + | 0 | − | − | 0 | + | − | − |
| Pain-free grip strength | 0 | + | 0 | − | − | 0 | 0 | − | − |
aA plus sign (+) or minus sign (–) indicates that formal sensitivity or subgroup analysis was or was not performed, respectively; 0 indicates that descriptive data were performed or discussed but no analysis was performed. DASH, Disabilities of the Arm, Shoulder and Hand; EQ-5D, EuroQoL score; NSAIDs, nonsteroidal anti-inflammatory drugs; PPT, pressure pain threshold; PRTEE, Patient-Rated Tennis Elbow Evaluation; VAS, visual analog scale.
Results of Jadad Decision Algorithm
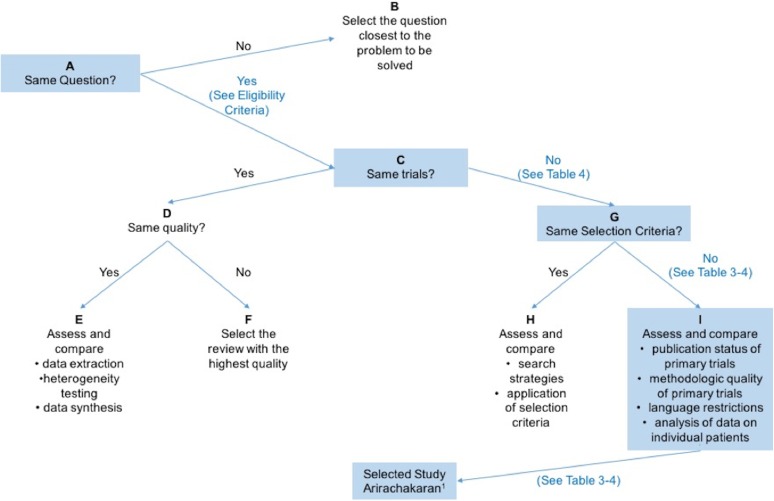
The Jadad decision algorithm was applied to determine which of the 9 included studies provided the best available evidence.13 All outcomes of the included meta-analyses are shown in Figure 1. The selection criteria were not accordant among the included meta-analyses; therefore, the Jadad algorithm suggests that the highest-quality review be selected according to the publication characteristics of primary trials, the methods of primary trials, the language restrictions, and whether analysis of data on individual patients was included in the study. Arirachakaran et al1 was selected as the study with the best methodological quality of primary trials.
Figure 1.
Flow diagram of Jadad decision algorithm.13
Discussion
The purpose of this study was to conduct a systematic review of overlapping meta-analyses comparing different injection treatments for the treatment of LE and to determine which meta-analyses provide the best available evidence. Most studies found that ABPs (ie, AB and PRP) were the most effective treatment options for LE in terms of pain relief and elbow function in the intermediate term (12-26 weeks).1,3,6,15,18,25,34 In addition, CSI was an effective treatment for pain relief and elbow function in the short term (<12 weeks).18,25,31,34 Many studies found that although CSIs exhibit positive short-term outcomes regarding pain relief and functional improvement, the recurrence rate of tennis elbow with CSI should be taken into consideration.3,18,25,31,34 Qian et al25 reported recurrence rates after CSI of 37% at 6 months and 72% at 6 weeks. Additionally, the lack of a significant short-term effect with injection of ABPs could represent the period needed for proper tendon tissue regeneration.18,25,31,34
The pathogenesis of LE is predominantly related to degeneration, while inflammation minimally affects LE.3,18 The high rate of recurrence with CSI could be explained by the effectiveness of steroids in decreasing pain intensity with the inhibition of neuropeptides and cytokines. However, tendon healing may be disrupted with the use of steroids by inhibiting the migration and proliferation of the cell and by inducing the differentiation of the nontenocyte.3,18,25 Additionally, overuse of the elbow attributed to short-term pain relief following treatment with CSI could be a reason for the high rate of recurrence.25 Furthermore, ABPs contain growth factors, which may be beneficial for tendon healing, although this may take >3 months.16 This extended period for healing may be the reason why ABPs were shown to be more effective in the intermediate term.1,3,6,15,18,25,34
Of the 9 studies we evaluated, 1 study had an Oxman-Guyatt score of 7 with a QUOROM score of 18,1 and 2 studies had an Oxman-Guyatt score of 7 with a QUOROM score of 17.18,31 These were the highest scores achieved in this review; therefore, these meta-analyses appear to have the highest level of evidence. The first of these was a level 1 meta-analysis by Arirachakaran et al.1 This meta-analysis found that PRP and AB are both superior to CSI within and after 2 months. The investigators found that AB was advantageous in improving pain, disability scores, and pressure pain threshold and that PRP can improve pain as compared with CSI. The investigators found an increased risk of adverse effects in AB as compared with PRP.1 The second of these studies was a level 2 meta-analysis by Sirico et al.31 This meta-analysis found that CSI nonsignificantly lowered the VAS pain score more so than AB in the short term but did not find any differences in the medium and long term. Sirico et al31 proposed a multiple-treatment injection protocol using CSI for short-term pain relief combined with ABPs for long-term functional improvement. The third of these studies was a level 2 meta-analysis by Mi et al.18 This study supported our hypothesis that CSI could relieve pain and significantly improve function in the short term, while PRP was the most effective treatment option for the intermediate to long term. However, the dosage and various dose options of PRP and CSI made it difficult to compare main outcomes, and this study lacked high-quality randomized controlled trials to verify the results.
Only 1 of the meta-analyses included in this review found no clinical benefits after nonsurgical injections (CSI, PRP, AB, sodium hyaluronate, or glycosaminoglycan polysulfate) and other nonsurgical treatments (physical therapy, shock wave therapy, laser, ultrasound, corticosteroid iontophoresis, topical glyceryl trinitrate, or oral naproxen) as compared with observation only or placebo (saline injection) at intermediate to long term.28 However, the aggregation of multiple nonsurgical treatments in the same analysis may have allowed the effectiveness of each treatment to counterbalance the other treatment.
Rather than conducting further reviews or meta-analyses, further research efforts should be aimed toward creating a single, large level 1 clinical trial to determine the most effective treatment option for LE given the lack of a confident conclusion in these meta-analyses. Since ABPs are not currently covered under the majority of insurance plans, a cost-effectiveness analysis is needed to compare PRP and AB when combined with physical therapy to examine functional outcomes, pain thresholds, disability scores, and adverse events.1 The effectiveness of ABP must be obvious to justify out-of-pocket cost to the patient. Therefore, it is clear that ABPs for the treatment of LE need to be further examined clinically to determine the intermediate- to long-term benefits when utilized alone or in combination with CSI for short-term pain relief.
One of the strengths of this review is the use of multiple validated quality assessment tools by 2 independent reviewers.19,21 The limitations of this study should also be noted. These include differences in pain scoring systems, treatment schedules and dosages, and follow-up period. Moreover, improvements in treatment groups versus nontreatment groups may be partially attributed to a placebo effect, activity modification, additional physical therapy, commercial bias, and outside treatments, in addition to the natural history of the condition.28 This study examined the more invasive treatments for LE, and conservative treatment measures, such as wrist bracing, nonsteroidal anti-inflammatory drug use, and rest, were not considered in the majority of the included studies. Furthermore, some nonoperative treatment options for LE, including hyaluronic acid, glycosaminoglycan polysulfate, prolotherapy, and botulinum toxin, were not included in this review. In addition, the lack of uniformity among the trials related to the preparation of PRP and the concentration of platelets (leukocyte rich vs poor) was not able to be assessed in any of the included meta-analyses. Finally, the small number of studies evaluating outcomes of particular pairs of treatments and the high risk of bias in the ABP treatment injections, owing to a lack of blinding, may have had a significant effect on our findings. Further research in which a blood sample is obtained from the control groups is necessary to associate the dosage, number of injections, and ideal combination and sequence of various treatment injections for LE.
Conclusion
The results of this systematic review of overlapping meta-analyses suggest that CSI improves functional outcomes and pain relief for LE in the short term, while AB and PRP are the most effective treatment options in the intermediate term. Despite lacking significant support, the results of this review indicate that dosage, number of injections, and combination of various treatment injections may be critical factors and dependent variables in determining the success of CSI, AB, and PRP, which necessitates a more detailed evaluation and longer follow-up to determine the appropriate injection protocol for the treatment of LE.
APPENDIX
TABLE A1.
Primary Studies Included in Meta-analysesa
| Prospective Comparative Study | Krogh15 | Sayegh28 | Chou3 | Arirachakaran1 | Dong6 | Tsikopoulos34 | Qian25 | Sirico31 | Mi18 | Meta- analyses, nb |
|---|---|---|---|---|---|---|---|---|---|---|
| Akermark (1995) | + | + | − | − | + | − | − | − | − | 3 |
| Creaney (2011) | + | − | + | + | − | − | − | − | − | 3 |
| Dogramaci (2009) | + | − | − | − | + | − | − | − | − | 2 |
| Espandar (2010) | + | − | − | − | + | − | − | − | − | 2 |
| Kazemi (2010) | + | − | + | + | + | + | + | + | − | 7 |
| Lin (2010) | + | − | − | − | + | − | − | − | − | 2 |
| Lindenhovius (2008) | + | − | − | − | + | − | − | − | − | 2 |
| Newcomer (2001) | + | − | − | − | + | − | − | − | − | 2 |
| Ozturan (2010) | + | − | + | − | + | + | + | − | − | 5 |
| Peerbooms (2010) | + | − | − | + | + | − | + | − | + | 5 |
| Petrella (2010) | + | + | − | − | + | − | − | − | − | 3 |
| Placzek (2007) | + | − | − | − | + | − | − | − | − | 2 |
| Price (1991; study 1) | + | − | − | − | + | − | − | − | − | 2 |
| Price (1991; study 2) | + | − | − | − | + | − | − | − | − | 2 |
| Scarpone (2008) | + | − | − | − | + | − | − | − | − | 2 |
| Wong (2005) | + | − | − | − | + | − | − | − | − | 2 |
| Zeisig (2008) | + | − | − | − | − | − | − | − | − | 1 |
| Chesterton (2013) | − | + | − | − | − | − | − | − | − | 1 |
| Krogh (2013) | − | + | − | + | + | − | + | − | + | 5 |
| Coombes (2013) | − | + | − | − | + | − | − | − | − | 2 |
| McCallum (2011) | − | + | − | − | − | − | − | − | − | 1 |
| Wolf (2011) | − | + | + | − | + | + | + | + | − | 6 |
| Staples (2008) | − | + | − | − | − | − | − | − | − | 1 |
| Bisset (2006) | − | + | − | − | + | − | − | − | − | 2 |
| Spacca (2005) | − | + | − | − | − | − | − | − | − | 1 |
| Pettrone (2005) | − | + | − | − | − | − | − | − | − | 1 |
| Rompe (2004) | − | + | − | − | − | − | − | − | − | 1 |
| Mehra (2003) | − | + | − | − | − | − | − | − | − | 1 |
| Melikyan (2003) | − | + | − | − | − | − | − | − | − | 1 |
| Haake (2002) | − | + | − | − | − | − | − | − | − | 1 |
| Runeson (2002) | − | + | − | − | − | − | − | − | − | 1 |
| Smidt (2002) | − | + | − | − | + | − | − | − | − | 2 |
| Hay (1999) | − | + | − | − | + | − | − | − | − | 2 |
| Haker (1990) | − | + | − | − | − | − | − | − | − | 1 |
| Haker (1991; Pain) | − | + | − | − | − | − | − | − | − | 1 |
| Haker (1991; J Pain Symptom Manage) | − | + | − | − | − | − | − | − | − | 1 |
| Haker (1991; Scand J Rehabil Med) | − | + | − | − | − | − | − | − | − | 1 |
| Dojode (2012) | − | − | + | + | − | + | + | − | − | 4 |
| Jindal (2013) | − | − | + | − | + | + | + | + | − | 5 |
| Raeissadat (2014; study 1) | − | − | + | + | − | − | − | − | − | 2 |
| Raeissadat (2014; study 2) | − | − | − | + | − | − | − | − | − | 1 |
| Singh (2013) | − | − | + | + | − | − | − | − | − | 2 |
| Thanasas (2011) | − | − | + | + | + | − | − | − | − | 3 |
| Omar (2012) | − | − | − | + | + | − | + | − | + | 4 |
| Tonks (2007) | − | − | − | − | + | − | − | − | − | 1 |
| Mardani-Kivi (2013) | − | − | − | − | + | − | − | − | − | 1 |
| Rabago (2013) | − | − | − | − | + | − | − | − | − | 1 |
| Stenhouse (2013) | − | − | − | − | + | − | − | − | − | 1 |
| Arik (2014) | − | − | − | − | − | + | + | + | − | 3 |
| Gautam (2015) | − | − | − | − | − | − | + | − | + | 2 |
| Khaliq (2015) | − | − | − | − | − | − | − | − | + | 1 |
| Lebiedzinkski (2015) | − | − | − | − | − | − | − | − | + | 1 |
| Palacio (2016) | − | − | − | − | − | − | − | − | + | 1 |
| Yadav (2015) | − | − | − | − | − | − | − | − | + | 1 |
aA plus (+) or minus (–) indicates that a primary study was or was not used in the designated meta-analysis, respectively.
bRepresents how many meta-analyses assessed each primary study.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: E.C.M. has received research support from Mitek, Smith & Nephew, Stryker, and Zimmer Biomet; is a paid consultant for DePuy and Zimmer Biomet; and receives royalties from Elsevier and Zimmer Biomet. J.T.B. has received research support from Stryker; is a paid consultant for DJ Orthopaedics, Encore Medical, Smith & Nephew, and Stryker; has received educational fellowship funding from Mitek; and receives royalties from Shukla Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Arirachakaran A, Sukthuayat A, Sisayanarane T, Laoratanavoraphong S, Kanchanatawan W, Kongtharvonskul J. Platelet-rich plasma versus autologous blood versus steroid injection in lateral epicondylitis: systematic review and network meta-analysis. J Orthop Traumatol. 2016;17(2):101–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. BMJ. 2006;333(7575):939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chou LC, Liou TH, Kuan YC, Huang YH, Chen HC. Autologous blood injection for treatment of lateral epicondylosis: a meta-analysis of randomized controlled trials. Phys Ther Sport. 2016;18:68–73. [DOI] [PubMed] [Google Scholar]
- 4. Cook JL, Purdam CR. The challenge of managing tendinopathy in competing athletes. Br J Sports Med. 2014;48(7):506–509. [DOI] [PubMed] [Google Scholar]
- 5. Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010;376(9754):1751–1767. [DOI] [PubMed] [Google Scholar]
- 6. Dong W, Goost H, Lin XB, et al. Injection therapies for lateral epicondylalgia: a systematic review and Bayesian network meta-analysis. Br J Sports Med. 2016;50(15):900–908. [DOI] [PubMed] [Google Scholar]
- 7. Dragoo JL, Wasterlain AS, Braun HJ, Nead KT. Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial. Am J Sports Med. 2014;42(3):610–618. [DOI] [PubMed] [Google Scholar]
- 8. EuroQol G. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. [DOI] [PubMed] [Google Scholar]
- 9. Hoher J, Munster A, Klein J, Eypasch E, Tiling T. Validation and application of a subjective knee questionnaire. Knee Surg Sports Traumatol Arthrosc. 1995;3(1):26–33. [DOI] [PubMed] [Google Scholar]
- 10. Houck DA, Kraeutler MJ, Schuette HB, McCarty EC, Bravman JT. Early versus delayed motion after rotator cuff repair: a systematic review of overlapping meta-analyses. Am J Sports Med. 2017;45(12):2911–2915. [DOI] [PubMed] [Google Scholar]
- 11. Hudak PL, Amadio PC, Bombardier C; Upper Extremity Collaborative Group. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand) [corrected]. Am J Ind Med. 1996;29(6):602–608. [DOI] [PubMed] [Google Scholar]
- 12. Hudak PL, Cole DC, Haines AT. Understanding prognosis to improve rehabilitation: the example of lateral elbow pain. Arch Phys Med Rehabil. 1996;77(6):586–593. [DOI] [PubMed] [Google Scholar]
- 13. Jadad AR, Cook DJ, Browman GP. A guide to interpreting discordant systematic reviews. CMAJ. 1997;156(10):1411–1416. [PMC free article] [PubMed] [Google Scholar]
- 14. Kraeutler MJ, Garabekyan T, Mei-Dan O. The use of platelet-rich plasma to augment conservative and surgical treatment of hip and pelvic disorders. Muscles Ligaments Tendons J. 2016;6(3):410–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Krogh TP, Bartels EM, Ellingsen T, et al. Comparative effectiveness of injection therapies in lateral epicondylitis: a systematic review and network meta-analysis of randomized controlled trials. Am J Sports Med. 2013;41(6):1435–1446. [DOI] [PubMed] [Google Scholar]
- 16. Krogh TP, Fredberg U, Stengaard-Pedersen K, Christensen R, Jensen P, Ellingsen T. Treatment of lateral epicondylitis with platelet-rich plasma, glucocorticoid, or saline: a randomized, double-blind, placebo-controlled trial. Am J Sports Med. 2013;41(3):625–635. [DOI] [PubMed] [Google Scholar]
- 17. Mascarenhas R, Erickson BJ, Sayegh ET, et al. Is there a higher failure rate of allografts compared with autografts in anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Arthroscopy. 2015;31(2):364–372. [DOI] [PubMed] [Google Scholar]
- 18. Mi B, Liu G, Zhou W, et al. Platelet rich plasma versus steroid on lateral epicondylitis: meta-analysis of randomized clinical trials. Phys Sportsmed. 2017;45(2):97–104. [DOI] [PubMed] [Google Scholar]
- 19. Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354(9193):1896–1900. [DOI] [PubMed] [Google Scholar]
- 20. Nirschl RP. Tennis elbow. Orthop Clin North Am. 1973;4(3):787–800. [PubMed] [Google Scholar]
- 21. Oxman AD, Guyatt GH. Validation of an index of the quality of review articles. J Clin Epidemiol. 1991;44(11):1271–1278. [DOI] [PubMed] [Google Scholar]
- 22. Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013;41(2):356–364. [DOI] [PubMed] [Google Scholar]
- 23. Peerbooms JC, Sluimer J, Bruijn DJ, Gosens T. Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double-blind randomized controlled trial: platelet-rich plasma versus corticosteroid injection with a 1-year follow-up. Am J Sports Med. 2010;38(2):255–262. [DOI] [PubMed] [Google Scholar]
- 24. Pransky G, Feuerstein M, Himmelstein J, Katz JN, Vickers-Lahti M. Measuring functional outcomes in work-related upper extremity disorders: development and validation of the Upper Extremity Function Scale. J Occup Environ Med. 1997;39(12):1195–1202. [DOI] [PubMed] [Google Scholar]
- 25. Qian X, Lin Q, Wei K, Hu B, Jing P, Wang J. Efficacy and safety of autologous blood products compared with corticosteroid injections in the treatment of lateral epicondylitis: a meta-analysis of randomized controlled trials. PM R. 2016;8(8):780–791. [DOI] [PubMed] [Google Scholar]
- 26. Roles NC, Maudsley RH. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg Br. 1972;54(3):499–508. [PubMed] [Google Scholar]
- 27. Rompe JD, Overend TJ, MacDermid JC. Validation of the Patient-Rated Tennis Elbow Evaluation Questionnaire. J Hand Ther. 2007;20(1):3–10. [DOI] [PubMed] [Google Scholar]
- 28. Sayegh ET, Strauch RJ. Does nonsurgical treatment improve longitudinal outcomes of lateral epicondylitis over no treatment? A meta-analysis. Clin Orthop Relat Res. 2015;473(3):1093–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shiri R, Viikari-Juntura E, Varonen H, Heliovaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol. 2006;164(11):1065–1074. [DOI] [PubMed] [Google Scholar]
- 30. Sims SE, Miller K, Elfar JC, Hammert WC. Non-surgical treatment of lateral epicondylitis: a systematic review of randomized controlled trials. Hand (N Y). 2014;9(4):419–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sirico F, Ricca F, di Meglio F, et al. Local corticosteroid versus autologous blood injections in lateral epicondylitis: meta-analysis of randomized controlled trials. Eur J Phys Rehabil Med. 2017;53(3):483–491. [DOI] [PubMed] [Google Scholar]
- 32. Smidt N, van der Windt DA, Assendelft WJ, et al. Interobserver reproducibility of the assessment of severity of complaints, grip strength, and pressure pain threshold in patients with lateral epicondylitis. Arch Phys Med Rehabil. 2002;83(8):1145–1150. [DOI] [PubMed] [Google Scholar]
- 33. Tosti R, Jennings J, Sewards JM. Lateral epicondylitis of the elbow. Am J Med. 2013;126(4):357. [DOI] [PubMed] [Google Scholar]
- 34. Tsikopoulos K, Tsikopoulos A, Natsis K. Autologous whole blood or corticosteroid injections for the treatment of epicondylopathy and plantar fasciopathy? A systematic review and meta-analysis of randomized controlled trials. Phys Ther Sport. 2016;22:114–122. [DOI] [PubMed] [Google Scholar]
- 35. Wang-Saegusa A, Cugat R, Ares O, Seijas R, Cusco X, Garcia-Balletbo M. Infiltration of plasma rich in growth factors for osteoarthritis of the knee short-term effects on function and quality of life. Arch Orthop Trauma Surg. 2011;131(3):311–317. [DOI] [PubMed] [Google Scholar]
- 36. Wei LC, Lei GH, Sheng PY, et al. Efficacy of platelet-rich plasma combined with allograft bone in the management of displaced intra-articular calcaneal fractures: a prospective cohort study. J Orthop Res. 2012;30(10):1570–1576. [DOI] [PubMed] [Google Scholar]