Summary
Introduction
Elderly people are more likely to develop influenza-related complications. However, despite the recommendations, the optimal vaccination coverage is not reached. The use of deprivation indexes can help to identify subgroups with lower vaccination uptake. We analyzed vaccination coverage among elderly subjects living in the city of Rome on the basis of their socioeconomic characteristics by using a local deprivation index.
Methods
We focused on the population aged ≥ 65 years living in the city of Rome from 2009 to 2013. Information on vaccination coverage was collected from general practitioners. A combination of multivariate techniques, including multiple linear regression, factor and cluster analysis, was used to construct a composite area-based Index of Socio-Economic and Health Deprivation (SEHDI). The index was calculated for each census tract on the basis of data from the 2001 Italian census.
Results
The majority of elderly subjects living in Rome belonged to the medium (40.4%) and medium-high (24%) deprivation groups; only 4.5% of the population was in the low-deprivation group. An inverse relationship was found between influenza vaccination coverage and the deprivation index: elderly subjects in the low-deprivation group displayed lower coverage (55.45%) than those in the high-deprivation group (57.59%). Specifically, vaccination coverage decreased with the increase of replacement index, employment rate and the percentage of: single and divorced individuals; university and high-school graduates; employees, entrepreneurs and freelancers, family assistants, students; foreigners and stateless persons residing in Italy; families consisting of one person.
Conclusions
Our results show an inverse relationship between deprivation and vaccination coverage and may help to identify subgroups that could benefit from targeted initiatives to increase vaccination coverage.
Key words: Influenza vaccination, Vaccine coverage, Deprivation, Elderly
Introduction
Influenza is a common infectious disease, affecting around 8% of the entire population during the winter season each year [1]. Incidence rates reach the lowest values among the elderly, with peaks ranging from a minimum of 1.78 per 1,000 to a maximum of 8.55 per 1,000 in the last nine seasons. In the last influenza season, the overall incidence of influenza among the elderly was 0.46 per 1,000 in Italy and 0.39 per 1,000 in the Lazio Region [2]. Although less frequently affected by the disease, elderly people are more likely than other age-groups to develop influenza-related complications, which may even be fatal. Indeed, 90% of deaths due to influenza occur among the elderly [1, 3].
Because of these clinical characteristics, elderly people are among the targets of influenza vaccination campaigns each year. The risk of all-cause and cause-specific mortality has been shown to be higher in the unvaccinated elderly subjects than in their vaccinated counterparts [4]. Indeed, vaccination has been strongly recommended for the elderly since the National Health Plan 1998-2000 was formulated, which set the minimum vaccination coverage goal at 75% [5]. Furthermore, the last two National Immunization Plans indicated 95% as the optimal goal of vaccination coverage [6, 7]. Nonetheless, neither goal has been achieved since the 1999/2000 season. A peak coverage of 68.3% among the elderly was observed in 2005/2006. Thereafter, a steady decrease ensued, until the lowest value of 48.6% was reached in 2014/2015; the last two seasons, however, have seen an increase to values around 52% [8].
The decline in vaccination coverage has led to a significant increase in cases of influenza-like illness [9]. Furthermore, since December 2016, an excess in all cause-mortality, primarily explained by influenza, has been observed throughout Europe, particularly among elderly people [10]. In Italy, analysis of seasonal mortality from 2012 to 2015 showed a 13% increase in mortality among the elderly in the 2015 winter season, which seemed to be due to the peak in influenza [11].
It has been demonstrated that socioeconomic conditions play quite an important role in determining adherence to immunization programs against influenza, particularly in the elderly population [12, 13]. Indeed, influenza vaccination coverage shows local variations [14, 15] and is considerably lower among individuals from socioeconomically deprived areas [14, 16]. Our recent systematic review also concluded that individuals from different groups at risk for influenza were less likely to be vaccinated if they lived in more deprived areas in comparison with those from affluent areas, regardless of the vaccine type (seasonal or pandemic) [17]. Deprivation indexes are measures of the level of deprivation in an area that take into consideration the multidimensional aspects of social stratification; their implementation at the population level could be a useful strategy for measuring health disparities and distinguishing non-vaccinating groups [18].
The aim of our study was to identify groups of subjects aged ≥ 65 years with lower vaccination coverage, living in the city of Rome, on the basis of their socioeconomic characteristics. To this end, we constructed and applied a local deprivation index.
Methods
STUDY POPULATION
The study focused on elderly subjects ≥ 65 years old living in the city of Rome from 2009 to 2013. Rome is located in the central part of Italy, in the Lazio region, has a population of about 2.5 million and a surface area of 1,290 km2. Elderly people constitute 21.5-22.4% of the entire population of the city, a percentage that is in line with the national figures [19].
To ascertain vaccination coverage, all general practitioners (GPs) working in the city of Rome were considered.
DATA SOURCES
Data on influenza vaccination coverage were provided by the Lazio Health and Social Policy Directorate, which collects and validates data from the GPs. The data covered the influenza seasons from 2009-10 to 2013-14 and included the street addresses of GPs’ offices. These latter were georeferenced in terms of census tract by the Statistics Office of the city of Rome.
Demographic and socioeconomic characteristics of the study population were collected from the National Institute for Statistics, whereas the number of observed deaths due to all causes and to specific causes were obtained from the Department of Epidemiology of the Regional Health Service of the Lazio region. The data obtained were stratified by gender and census tract, as per the 2001 national census. The ICD-10 codes were converted into ICD-9 codes for the query.
STATISTICAL ANALYSIS
A composite area-based Index of Socio-Economic and Health Deprivation (SEHDI) was constructed by using a combination of multivariate techniques, including multiple linear regression, factor and cluster analysis for the local population, as reported elsewhere [20]. In calculating the index, each census tract was used as the unit of observation. Standardized Mortality Ratios (SMRs) were calculated on the basis of expected deaths, computed at the regional level, in order to validate the index with respect to the relationship between deprivation and the causes of death, as reported in the literature [19], and to describe the health condition of the population considered. SMRs were computed as the ratio between observed and expected mortality. Expected cases were computed on the basis of expected regional mortality (overall and for each specific cause, by gender and age-group). SMR values higher than 1 indicated a risk of mortality higher than the regional one, while SMR values lower than 1 indicated a risk of mortality lower than the regional one.
The relationship between the SEHDI and vaccination coverage was analyzed by means of one-way analysis of variance (ANOVA) (statistical significance at p < 0.05) in order to evaluate the trend among the deprivation groups. A Pearson bivariate correlation, with statistical significance threshold at p < 0.05, was used to test the association between single specific socioeconomic and demographic census variables and the vaccination coverage in order to identify peculiar characteristics that could influence vaccination uptake.
The relationship between the SEHDI and mortality due to all causes and to specific causes was tested through ANOVA (statistical significance at p < 0.05) [19]. SMR and the results of ANOVA were reported for all-cause mortality and two causes of deaths, namely cardiovascular and respiratory diseases, as well as for influenza and pneumonia. These choices were supported by the fact that the calculation of influenza-associated deaths generally takes into consideration respiratory and circulatory diseases as underlying causes of death.
Results
During the study period, the population ranged from a minimum of 554,028 to a maximum of 590,603 elderly people, with men accounting for between 40.8% and 40.9% [21-23].
According to the factor analysis for the construction of the SEHDI, the contribution of the first factor to the explanation of the whole variance was 18.6%; this factor comprised the following variables: percentage of widows/widowers, percentage of males, old-age index, index of structural dependence, and average number of members of households. The contribution of the second factor was 13.8%; the third and fourth factors contributed 9.6% and 9.5%, respectively, while the last factor had a value of 7.7% (Tab. I).
Tab. I.
Factors used for constructing the deprivation index and their corresponding contribution values.
| Factor 1 = 18.6% | Factor 2 = 13.8% | Factor 3 = 9.6% | Factor 4 = 9.5% | Factor 5 = 7.7% |
|---|---|---|---|---|
| % widows / widowers | % primary school diploma | Replacement index | % divorced | % family helpers |
| Index of structural dependence | % employed in industry | % separated | % employed in agriculture | |
| Old-age index | % rented homes | % students | ||
| % men | ||||
| Average number of household components |
Total variance explained = 59.3%
According to results, the category of medium deprivation comprised the highest percentage (40.4%) of elderly people living in the city of Rome; 22.7% were classed as medium-low deprived while about 1/3 belonged to the categories medium-high (24%) or high (8.4%) deprivation. The low-deprivation group accounted for only 4.5%. Mapping was performed in order to show the spatial distribution of the various groups in the city; the distribution of census tracts, with their assigned index value, is shown in Fig. 1. The population of the historical center of Rome has a higher socioeconomic position than the rest of the city. A greater concentration of subjects belonging to high and medium-high deprivation groups can be seen in the peripheral quarters of the city, particularly in the eastern, north-western and southern areas (Fig. 1).
Fig. 1.
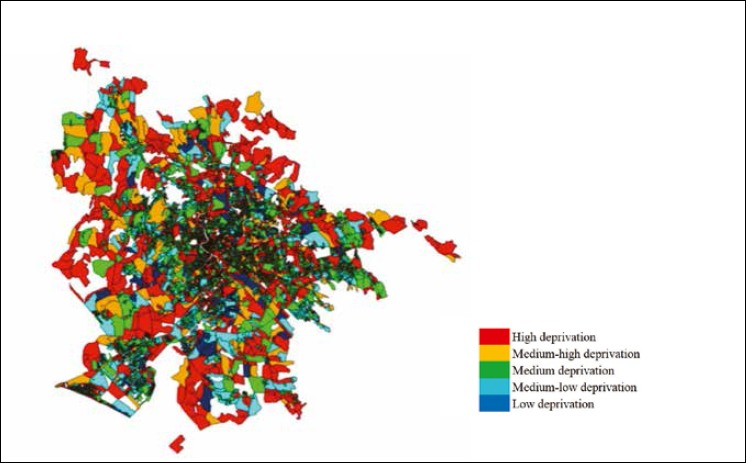
Map of Rome showing the spatial distribution of the deprivation index by census tract. Some census tracts (20.1%), comprising 1.3% of the entire population of Rome, were not analyzed owing to data incompleteness.
A significant linear trend was found in the correlation between vaccination coverage and the deprivation index, with coverage increasing slightly as deprivation increases: from 55.45% in the low-deprivation group to 57.59% in the high-deprivation group (Fig. 2). Specifically, vaccination coverage decreased as the following variables increased: replacement index, employment rate and the percentages of: singles, divorced; graduates and higher school graduates; employees, entrepreneurs and freelancers, family assistants, students; foreigners and stateless persons residing in Italy; one-person families.
Fig. 2.
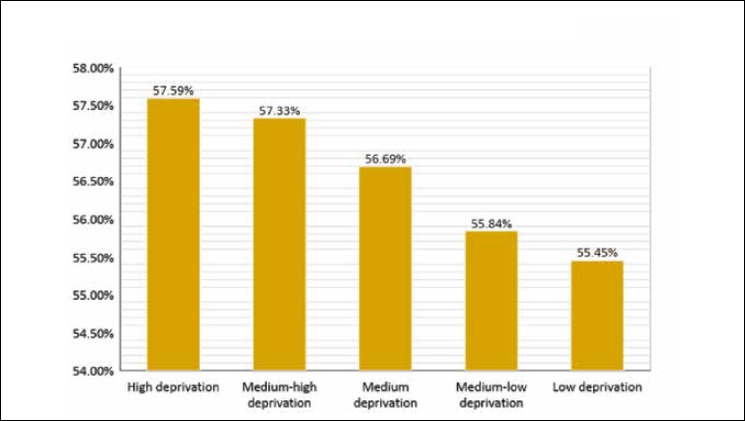
Vaccination coverage (%) among the elderly by deprivation group in the period 2009-2013.
We observed a nonlinear significant relationship between the deprivation index and mortality due to all causes and cardiovascular diseases, with high, medium-low and low deprivation groups showing the highest SMRs. Specifically, with regard to all-cause mortality, the highest SMRs were seen in the low deprivation group among men (SMR = 1.17, 95% CI: 1.11-1.24), women (SMR = 1.36, 95% CI: 1.29-1.43) and the total population (SMR = 1.26, 95% CI: 1.22-1.31). Analogously, the highest SMRs for cardiovascular diseases were observed in low deprivation groups (SMR = 1.17, 95% CI: 1.07-1.27 in men; SMR = 1.23, 95% CI: 1.14-1.33 in women; SMR = 1.20, 95% CI: 1.13-1.27 in the total population).
A significant linear trend was observed in males with respect to mortality due to respiratory diseases, with the highest SMRs being recorded in high deprivation groups (SMR = 1.14, 95% CI: 1.03-1.24) and the lowest in low deprivation groups (SMR = 0.86, 95% CI: 0.67-1.05). A significant nonlinear trend was observed in women and the total population, with the highest SMR in the high deprivation group (SMR = 1.27, 95% CI: 1.16-1.38 in women and SMR = 1.21, 95% CI: 1.13-1.28 in the total population).
The SMR due to influenza and pneumonia showed a linear inverse correlation in men (high deprivation group: SMR = 0.66, 95% CI: 0.48-0.85; low deprivation group: SMR = 1.41, 95% CI: 0.87-1.95) and in the total population (high deprivation group: SMR = 0.76, 95% CI: 0.63-0.89; low deprivation group: SMR = 1.08, 95% CI: 0.73-1.42), while the trend was non-linear in women (low deprivation group: SMR = 0.71, 95% CI: 0.31-1.12; medium-low deprivation group: SMR = 1.05, 95% CI: 0.88-1.23) (Tab. II).
Tab. II.
Standardized mortality due to all causes and to cardiovascular and respiratory diseases, pneumonia and influenza in the period 2009-2013.
| All causes 65+ M | All causes 65+ F | Total all causes 65+ | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Deprivation groups | Observed | SMR | 95% CI | Observed | SMR | 95% CI | Observed | SMR | 95% CI | |||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| High deprivation | 5912 | 1.13 | 1.10 | 1.16 | 7670 | 1.22 | 1.20 | 1.25 | 13582 | 1.18 | 1.16 | 1.20 |
| Medium-high deprivation | 13800 | 1.07 | 1.05 | 1.09 | 17469 | 1.16 | 1.14 | 1.18 | 31269 | 1.12 | 1.11 | 1.13 |
| Medium deprivation | 20156 | 1.06 | 1.05 | 1.07 | 24656 | 1.16 | 1.15 | 1.17 | 44812 | 1.11 | 1.10 | 1.12 |
| Medium-low deprivation | 9599 | 1.14 | 1.12 | 1.17 | 10552 | 1.24 | 1.21 | 1.26 | 20151 | 1.19 | 1.17 | 1.21 |
| Low deprivation | 1451 | 1.17 | 1.11 | 1.24 | 1515 | 1.36 | 1.29 | 1.43 | 2966 | 1.26 | 1.22 | 1.31 |
| Total | 50918 | 1.09 | 1.08 | 1.10 | 61862 | 1.18 | 1.18 | 1.19 | 112780 | 1.14 | 1.13 | 1.15 |
| Trend | p<0.05 n.l. | p<0.05 n.l. | p<0.05 n.l. | |||||||||
| Cardiovascular diseases 65+ M | Cardiovascular diseases 65+ F | Total Cardiovascular diseases 65+ | ||||||||||
| Deprivation groups | Observed | SMR | 95% CI | Observed | SMR | 95% CI | Observed | SMR | 95% CI | |||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| High deprivation | 2100 | 1.17 | 1.12 | 1.22 | 3288 | 1.15 | 1.11 | 1.19 | 5388 | 1.16 | 1.13 | 1.19 |
| Medium-high deprivation | 5072 | 1.15 | 1.12 | 1.18 | 7544 | 1.10 | 1.08 | 1.13 | 12616 | 1.12 | 1.10 | 1.14 |
| Medium deprivation | 7185 | 1.10 | 1.07 | 1.12 | 10796 | 1.12 | 1.10 | 1.14 | 17981 | 1.11 | 1.09 | 1.13 |
| Medium-low deprivation | 3318 | 1.15 | 1.11 | 1.19 | 4417 | 1.14 | 1.11 | 1.17 | 7735 | 1.14 | 1.12 | 1.17 |
| Low deprivation | 497 | 1.17 | 1.07 | 1.27 | 623 | 1.23 | 1.14 | 1.33 | 1120 | 1.20 | 1.13 | 1.27 |
| Total | 18172 | 1.13 | 1.11 | 1.15 | 26668 | 1.12 | 1.11 | 1.14 | 44840 | 1.13 | 1.12 | 1.14 |
| Trend | p<0.05 n.l. | p<0.05 n.l. | p<0.05 n.l. | |||||||||
| Respiratory diseases 65+ M | Respiratory diseases 65+ F | Total Respiratory diseases 65+ | ||||||||||
| Deprivation groups | Observed | SMR | 95% CI | Observed | SMR | 95% CI | Observed | SMR | 95% CI | |||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| High deprivation | 447 | 1.14 | 1.03 | 1.24 | 521 | 1.27 | 1.16 | 1.38 | 968 | 1.21 | 1.13 | 1.28 |
| Medium-high deprivation | 1004 | 1.04 | 0.97 | 1.10 | 1093 | 1.11 | 1.04 | 1.18 | 2097 | 1.07 | 1.03 | 1.12 |
| Medium deprivation | 1440 | 1.01 | 0.96 | 1.06 | 1611 | 1.16 | 1.10 | 1.22 | 3051 | 1.08 | 1.04 | 1.12 |
| Medium-low deprivation | 668 | 1.06 | 0.98 | 1.14 | 704 | 1.26 | 1.17 | 1.36 | 1372 | 1.15 | 1.09 | 1.22 |
| Low deprivation | 80 | 0.86 | 0.67 | 1.05 | 83 | 1.14 | 0.90 | 1.39 | 163 | 0.98 | 0.83 | 1.14 |
| Total | 3639 | 1.04 | 1.00 | 1.07 | 4012 | 1.17 | 1.14 | 1.21 | 7651 | 1.10 | 1.08 | 1.13 |
| Trend | p<0.05 l. | p<0.05 n.l. | p<0.05 n.l. | |||||||||
| Influenza and pneumonia 65+ M | Influenza and pneumonia 65+ F | Total Influenza and pneumonia 65+ | ||||||||||
| Deprivation groups | Observed | SMR | 95% CI | Observed | SMR | 95% CI | Observed | SMR | 95% CI | |||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| High deprivation | 52 | 0.66 | 0.48 | 0.85 | 80 | 0.84 | 0.66 | 1.03 | 132 | 0.76 | 0.63 | 0.89 |
| Medium-high deprivation | 135 | 0.70 | 0.58 | 0.82 | 202 | 0.89 | 0.76 | 1.01 | 337 | 0.80 | 0.72 | 0.89 |
| Medium deprivation | 217 | 0.76 | 0.66 | 0.87 | 272 | 0.85 | 0.75 | 0.95 | 489 | 0.81 | 0.74 | 0.88 |
| Medium-low deprivation | 94 | 0.75 | 0.60 | 0.90 | 136 | 1.05 | 0.88 | 1.23 | 230 | 0.90 | 0.79 | 1.02 |
| Low deprivation | 26 | 1.41 | 0.87 | 1.95 | 12 | 0.71 | 0.31 | 1.12 | 38 | 1.08 | 0.73 | 1.42 |
| Total | 524 | 0.75 | 0.69 | 0.81 | 702 | 0.89 | 0.82 | 0.95 | 1226 | 0.82 | 0.78 | 0.87 |
| Trend | p<0.05 l. | p<0.05 n.l. | p<0.05 l. | |||||||||
SMR: Standardized Mortality Ratio; M: male; F: female; l.: linear; n.l.: non-linear.
Discussion
Our study showed that more than half of the elderly population living in the city of Rome in the period 2009-2013 belonged to the medium, medium-high and high deprivation groups, and that there was an inverse relationship between influenza vaccination coverage and the SEHDI, with people in the low deprivation group showing the lowest coverage (more than two percentage points less than the high deprivation group). A linear relationship was observed between deprivation and mortality due to influenza and pneumonia in the total population and among men, with higher SMRs in low deprivation groups. By contrast, women in the low deprivation group showed the lowest SMR. The highest SMRs due to all-cause and cardiovascular disease mortality were also observed in low deprivation groups.
Socioeconomic position is a multidimensional concept and must be interpreted with caution, since different factors have been considered for its evaluation in the literature [24]. Nonetheless, our results are in concordance with those of published studies regarding the city of Rome. Indeed, the areas that displayed high deprivation in our analysis mostly correspond to those with low average income [25], low socioeconomic position [26] and a high index of social disadvantage [27].
In Rome, people belonging to medium/high social classes mainly reside in the prestigious central areas of the city, while those of lower social class tend to live in the peripheral areas. Using the socioeconomic position (SEP), Cesaroni et al. [26] found a similar distribution of socioeconomic inequalities in Rome and reported that the peripheral areas of the city (especially eastern and northern parts) had a low SEP, while the city center had a high SEP.
A recent report by the statistical office of the city of Rome concluded that the central area (municipalities I and II) and the northern part of the city had the highest economic welfare [25], while the municipalities located in the eastern part (municipality V and VI) had lower average incomes. The municipalities with the highest average income were those that displayed low or medium-low deprivation in our analysis (municipality I, II, XV) [25]. The same report also revealed that the percentage of elderly people living in conditions of economic difficulty (under € 11,000 gross a year) was higher in the eastern municipalities, particularly municipalities V and VI (32.5% and 37.5% of the total population aged ≥65 years, respectively) [25].
With regard to the association between vaccination coverage and deprivation, our findings are not in line with those of most studies. Indeed, most studies conducted in elderly populations across different seasons and countries have reported higher influenza vaccination uptake in low deprivation groups [14, 15, 28]. Only two studies, conducted in Colombia [29] and Germany [30], had findings similar to ours, and reported that elderly people from higher social classes had lower influenza vaccination coverage than those from lower and middle classes. We hypothesize that our findings might be the consequence of anti-vaccination campaigns [31], which have grown in Italy, and of the increased perception of the potential risks of vaccination [32], as people from higher socioeconomic classes may be more susceptible to both influences. Another possible explanation is that, in the high deprivation groups, people with chronic and/or co-morbid conditions are more likely to visit health-care facilities and have vaccination advised and given [29].
Our finding of an association between vaccination coverage and deprivation is to some extent corroborated by the relationship between deprivation and mortality. Indeed, in our study, both all-cause SMRs and SMRs for cardiovascular diseases and for influenza and pneumonia showed the highest values in low deprivation groups, although the SMRs for respiratory diseases displayed the opposite trend. Nevertheless, the evidence on the specific topic of influenza-associated mortality and socio-economic condition is still contrasting. A recent cross-sectional ecological study conducted in 15 European cities showed that SMRs for influenza and pneumonia in women were directly associated with socioeconomic deprivation in London, Rotterdam and Kosice and inversely associated in Madrid, while in men a direct association was found in all 15 cities [33].
Our study has some limitations. The main one is that it did not allow us to make inferences about causal association, as the observation unit was the census tract. Indeed, the ecological fallacy could not be ruled out. Another limit may be connected with the possible under-reporting of vaccination coverage by GPs and, therefore, the possible incompleteness of the data. On the other hand, one of the main strengths of the study lies in its use of validated administrative data, which makes the analysis transparent and repeatable.
Conclusions
In conclusion, our study allowed us to robustly depict the situation of deprivation of elderly people living in the city of Rome and to ascertain that people from low deprivation groups showed lower vaccination coverage. These results should be taken into account in the organization of vaccination campaigns and should prompt differential intervention according to the local area.
Acknowledgements
The project received financial support from the Ministry of Health - CCM, as in Article 4, paragraph 7 of the collaboration agreement.
We would like to thank: Enrico Volpe and Maurizio Faraone from the Regional Directorate for Health and Social Policy, Lazio Region, Rome, Italy for providing influenza vaccination coverage data; the Department of Epidemiology of Lazio Regional Health Service - ASL Roma 1 for providing the data of the Regional Register of Causes of Death (ReNCaM); Gino Casale and Francesca Di Stefano from the Statistics Office of the city of Rome for georeferencing data.
Footnotes
Conflict of interest statement
None declared.
Authors’ contributions
RL and CdW designed the study. FA and FC collected the data, RL performed the statistical analysis and CdW and VV contributed to data interpretation. VV and CdW drafted the manuscript and RL, FA and FC critically revised it. All authors have read and approved the final manuscript and agreed to be accountable for all aspects of the work.
References
- [1].Ministero della Salute. Prevenzione e controllo dell’influenza. Available at: www.salute.gov.it/portale/influenza/dettaglioContenutiInfluenza.jsp?lingua=italiano&id=685&area=influenza&menu=vuoto. [Accessed on 19/12/2018].
- [2].Rapporto epidemiologico InfluNet N. 26 del 7 maggio 2018. [Google Scholar]
- [3].Istituto Nazionale di statistica. Cause di morte, anno 2000. ISTAT; editor. Annuario 16, 2004. [Google Scholar]
- [4].Francia F, Pandolfi P, Odone A, Signorelli C. Excess mortality in Italy: Should we care about low influenza vaccine uptake? Scand J Public Health 2018;46:170-4. doi.org/10.1177/1403494817720102. [DOI] [PubMed] [Google Scholar]
- [5].Piano Sanitario Nazionale 1998-2000. Available at: www.salute.gov.it/imgs/C_17_pubblicazioni_947_allegato.pdf. [Accessed on 19/12/2018]. [PubMed]
- [6].Piano Nazionale Prevenzione Vaccinale 2012-2014. Available at: www.salute.gov.it/imgs/C_17_pubblicazioni_1721_allegato.pdf. [Accessed on 19/12/2018].
- [7].Piano Nazionale Prevenzione Vaccinale 2017-2019. Available at: www.salute.gov.it/imgs/C_17_pubblicazioni_2571_allegato.pdf. [Accessed on 19/12/2018].
- [8].Vaccinazione antinfluenzale in Italia: coperture vaccinali negli anziani (età ≥ 65 anni) (per 100 abitanti). Stagioni 1999-2000/2017-2018. Available at: www.salute.gov.it/imgs/C_17_tavole_19_allegati_iitemAllegati_0_fileAllegati_itemFile_3_file.pdf. [Accessed on 19/12/2018].
- [9].Manzoli L, Gabutti G, Siliquini R, Flacco ME, Villari P, Ricciardi W. Association between vaccination coverage decline and influenza incidence rise among Italian elderly. Eur J Public Health 2018;28:740-2. doi: 10.1093/eurpub/cky053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Vestergaard LS, Nielsen J, Krause TG, Espenhain L, Tersago K, Bustos Sierra N, Denissov G, Innos K, Virtanen MJ, Fouillet A, Lytras T, Paldy A, Bobvos J, Domegan L, O’Donnell J, Scortichini M, de Martino A, England K, Calleja N, van Asten L, Teirlinck AC, Tønnessen R, White RA, P Silva S, Rodrigues AP, Larrauri A, Leon I, Farah A, Junker C, Sinnathamby M, Pebody RG, Reynolds A, Bishop J, Gross D, Adlhoch C, Penttinen P, Mølbak K. Excess all-cause and influenza-attributable mortality in Europe, December 2016 to February 2017. Euro Surveill 2017;22:30506 doi: 10.2807/1560-7917.ES.2017.22.14.30506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Michelozzi P, De’Donato F, Scortichini M, De Sario M, Asta F, Agabiti N, Guerra R, de Martino A, Davoli M. On the increase in mortality in Italy in 2015: analysis of seasonal mortality in the 32 municipalities included in the Surveillance system of daily mortality. Epidemiol Prev 2016;40:22-8. doi: 10.19191/EP16.1.P022.010. [DOI] [PubMed] [Google Scholar]
- [12].Nagata JM, Hernández-Ramos I, Kurup AS, Albrecht D, Vivas-Torrealba C, Franco-Paredes C. Social determinants of health and seasonal influenza vaccination in adults ≥ 65 years: a systematic review of qualitative and quantitative data. BMC Public Health 2013;13:388 doi: 10.1186/1471-2458-13-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Topuzoglu A, Ozaydın GAN, Cali S, Cebeci D, Kalaca S, Harmanci H. Assessment of sociodemographic factors and socio-economic status affecting the coverage of compulsory and private immunization services in Istanbul, Turkey. Public Health 2005;119:862-9. doi: 10.1016/j.puhe.2005.01.015. [DOI] [PubMed] [Google Scholar]
- [14].Coupland C, Harcourt S, Vinogradova Y, Smith G, Joseph C, Pringle M, Hippisley-Cox J. Inequalities in uptake of influenza vaccine by deprivation and risk group: time trends analysis. Vaccine 2007;25:7363-71. doi: 10.1016/j.vaccine.2007.08.032. [DOI] [PubMed] [Google Scholar]
- [15].Norbury M, Fawkes N, Guthrie B. Impact of the GP contract on inequalities associated with influenza immunisation: a retrospective population-database analysis. Br J Gen Pract 2011;61:e379-85. doi: 10.3399/bjgp11X583146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Breeze E, Mangtani P, Fletcher AE, Price GM, Kovats SJR. Trends in influenza vaccination uptake among people aged over 74 years 1997-2000: survey of 73 general practices in Britain. BMC Fam Pract 2004;5:8 doi: 10.1186/1471-2296-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Vukovic V, Lillini R, Lupi S, Fortunato F, Cicconi M, Matteo G, Arata L, Amicizia D, Boccalini S, Bechini A, Prato R, Stefanati A, Panatto D, de Waure C. Identifying people at risk for influenza with low vaccine uptake based on deprivation status: a systematic review. Eur J Public Health 2018. doi: 10.1093/eurpub/cky264. [DOI] [PubMed] [Google Scholar]
- [18].Pasetto R, Caranci N, Pirastu R. Deprivation indices in small-area studies of environment and health in Italy. Epidemiol Prev 2011;35(Suppl. 4):1-204. [PubMed] [Google Scholar]
- [19].Health for all - Italia. Available at: www.istat.it/it/archivio/14562. [Accessed on 19/12/2018].
- [20].Lillini R, Quaglia A, Vercelli M; Registro mortalità Regione Liguria. Building of a local deprivation index to measure the health status in the Liguria Region. Epidemiol Prev 2012;36:180-7. [PubMed] [Google Scholar]
- [21].Geodemo. Available at: http://demo.istat.it/ricostruzione2013/index.php?lingua=ita. [Accessed on 19/12/2018].
- [22].Geodemo. Available at: http://demo.istat.it/pop2012/index.html. [Accessed on 19/12/2018].
- [23].Geodemo. Available at: http://demo.istat.it/pop2013/index.html. [Accessed on 19/12/2018].
- [24].Cesaroni G, Agabiti N, Rosati R, Forastiere F, Perucci CA. [An index of socioeconomic position based on 2001 Census, Rome].Epidemiol Prev 2006;30:352-7. [PubMed] [Google Scholar]
- [25].Rapporto Statistico sull’Area Metropolitana Romana - 2017. [Google Scholar]
- [26].Cesaroni G, Badaloni C, Romano V, Donato E, Perucci CA, Forastiere F. Socioeconomic position and health status of people who live near busy roads: the Rome Longitudinal Study (RoLS). Environ Health 2010;9:41 doi: 10.1186/1476-069X-9-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Ragioneria Generale. - I Direzione Sistemi informativi di pianificazione e controllo finanziario - U.O. Statistica. Indicatori di fabbisogno. Valutazione delle condizioni esterne nei municipi - 2016. [Google Scholar]
- [28].Mangtani P, Breeze E, Kovats S, Ng ESW, Roberts JA, Fletcher A. Inequalities in influenza vaccine uptake among people aged over 74 years in Britain. Prev Med (Baltim) 2005;41:545-53. doi: 10.1016/j.ypmed.2005.02.001. [DOI] [PubMed] [Google Scholar]
- [29].Cano Gutierrez C, Reyes-Ortiz C, Borda MG, Arciniegas A. Self-reported vaccination in the elderly: SABE Bogota study, Colombia. Colomb Medica (Cali) 2016;47:25-30. [PMC free article] [PubMed] [Google Scholar]
- [30].Böhmer MM, Walter D, Krause G, Müters S, Gösswald A, Wichmann O. Determinants of tetanus and seasonal influenza vaccine uptake in adults living in Germany. Hum Vaccin 2011;7:1317-25. doi: 10.4161/hv.7.12.18130. [DOI] [PubMed] [Google Scholar]
- [31].Signorelli C, Odone A, Conversano M, Bonanni P. Deaths after Fluad flu vaccine and the epidemic of panic in Italy. BMJ 2015;350:h116 doi: 10.1136/bmj.h116. [DOI] [PubMed] [Google Scholar]
- [32].Larson HJ, Cooper LZ, Eskola J, Katz SL, Ratzan S. Addressing the vaccine confidence gap. Lancet 2011;378:526-35. doi: 10.1016/S0140-6736(11)60678-8. [DOI] [PubMed] [Google Scholar]
- [33].Marí-Dell’Olmo M, Gotsens M, Palència L, Burström B, Corman D, Costa G, Deboosere P, Díez È, Domínguez-Berjón F, Dzúrová D, Gandarillas A, Hoffmann R, Kovács K, Martikainen P, Demaria M, Pikhart H, Rodríguez-Sanz M, Saez M, Santana P, Schwierz C, Tarkiainen L, Borrell C. Socioeconomic inequalities in cause-specific mortality in 15 European cities. J Epidemiol Community Health 2015;0:1-10. doi:10.1136/jech-2014-204312. [DOI] [PubMed] [Google Scholar]


