Abstract
Patient: Male, 55
Final Diagnosis: Auto-immune heparin thrombocytopenia -Treatment obstacles and challenging length of stay
Symptoms: Thrombocytopenia • thrombosis
Medication: —
Clinical Procedure: IVIG
Specialty: Hematology
Objective:
Unusual clinical course
Background:
Autoimmune heparin-induced thrombocytopenia (aHIT) refers to a condition, in which antiplatelet factor-4 (PF4) antibodies activate platelets even in the absence of heparin (heparin independent platelet activation). This is a severe hypercoagulable state triggering massive thrombin storm needing additional therapies and aggressive anticoagulation apart from stopping heparin. Thrombocytopenia in these cases seems to be very severe and prolonged compared to classic HIT and poses additional clinical challenges in terms of anticoagulation management. Recently, direct oral anticoagulants (DOACs) seem to be an attractive option in the management of HIT as an alternative to vitamin K antagonists (VKA).
Case Report:
We describe a case of a 55-year African American male who presented with pleuritic chest pain and was found to have worsening kidney disease. Clinical and electrocardiogram findings suggested uremic pericarditis, and dialysis was warranted. After 5 days of exposure to heparin flushes during dialysis, the patient developed thrombocytopenia, and subsequently HIT was diagnosed. Argatroban was started initially, however, his platelets count continued to drop, and he developed acute deep venous thrombosis of the right lower leg. IVIG (intravenous immunoglobulin) was started and his platelet count started to improve after several days. The patient was discharged on Eliquis and his platelet count returned to normal levels after 3 months.
Conclusions:
This case emphasizes the challenge managing HIT, a condition that has a high rate of complications. Several studies have reported platelet recovery with IV immunoglobulin when standard therapies fail. Recent evidence also supports the safety and efficacy of DOACs in offering a simplified way of managing these patients, especially in outpatient settings.
MeSH Keywords: Anticoagulants; Heparin; Immunoglobulins, Intravenous; Thrombocytopenia
Background
Heparin induced thrombocytopenia (HIT) is a prothrombotic condition caused by antibodies capable of recognizing cationic platelet factor 4 complexes bound to anionic heparin and forms PF4/heparin/IgG immune complexes on the platelet surfaces and cross-link with platelet FcgIIa receptors and activates platelets in a heparin-dependent fashion. Autoimmune HIT (aHIT) refers to certain variants of HIT that behave differently from the classic form. The antibodies in these patients activate platelets even in heparin absence. These patients also tend to present with severe thrombocytopenia (platelet count of <20×10 L−1) which may persist for weeks to months despite discontinuing heparin. Disseminated intravascular coagulation (DIC) and microvascular thrombosis may also be associated features of this variant. Baseline partial thromboplastin time (PTT) may be elevated when associated with DIC which may pose difficulty in using standard anticoagulation requiring PTT monitoring. Hence anticoagulants independent of activated PTT (aPTT) monitoring like fondaparinux, danaparoid and direct oral anticoagulants are used for long term management. Since aHIT is a severe hypercoagulable state, triggering massive thrombin generation, alternative therapy like intravenous immunoglobulin (IVIG) and aggressive anticoagulation remains the cornerstone of treatment and heparin cessation alone does not interrupt the pathogenesis. Thrombocytopenia may be severe and more prolonged when compared to classical HIT and hence should not preclude starting and continuing anticoagulation long-term as risk of thrombosis is high when compared to risk of bleeding.
Case Report
A 55-year-old African American male with a past medical history significant for alcohol abuse, cocaine abuse, and a 30-pack-year smoking history was admitted to the emergency department due to a 3-day history of dyspnea, hemoptysis, and left-sided pleuritic chest pain. In addition, his electrocardiogram was remarkable for ST elevations noted on anterior and inferior leads along with elevated blood urea nitrogen (BUN) of 104 mg/dL and creatinine of 10.70 mg/dL, that continued to rise during the hospital course. With suspicion of chronic kidney disease and uremic pericarditis, hemodialysis was newly initiated in the patient with exposure to unfractionated heparin intravascular flush. Heparin doses of 5000 U/mL were used during hemodialysis sessions over a period of 8 days. Five days after exposure to heparin, clotting of the venous line was noted 1.5 hours into the dialysis session and the patient’s platelet count showed a precipitous drop. Prior to hemodialysis with heparin flush, his platelet count was 253 000/μL, which steadily decreased to 169 000/μL and then to 50 000/μL by the tenth day.
Due to the high suspicion for HIT, heparin flushes were withheld from further dialysis sessions and peripheral smear, platelet factor-4 (PF-4) antibody, and serotonin release assay were evaluated. A peripheral smear was unremarkable for schistocytes or platelet clumps. However, PF-4 antibodies were reported to be strongly positive with a value of 2.493 OD. Serotonin release assay was also positive thereby confirming the diagnosis of HIT.
The patient was started on argatroban, initially at 0.5 mcg/kg/min when his platelet count was 16 000/μL which then was increased subsequently to 2.5 mcg/kg/min over time when no evidence of bleeding was observed. However, his platelet counts did not show any improvement and the patient developed an acute deep venous thrombosis in the right lower extremity despite 6 days of argatroban therapy. Suspicion of autoimmune-mediated HIT was high and intravenous immunoglobulin (IVIG) was administered to offset the decline. The patient’s platelet counts showed a very slow improvement after several days, but since the patient remained stable and PTT was in therapeutic range, he was discharged on apixaban for outpatient management. Finally, platelet counts returned to baseline after 3 months of starting IVIG (Figure 1).
Figure 1.
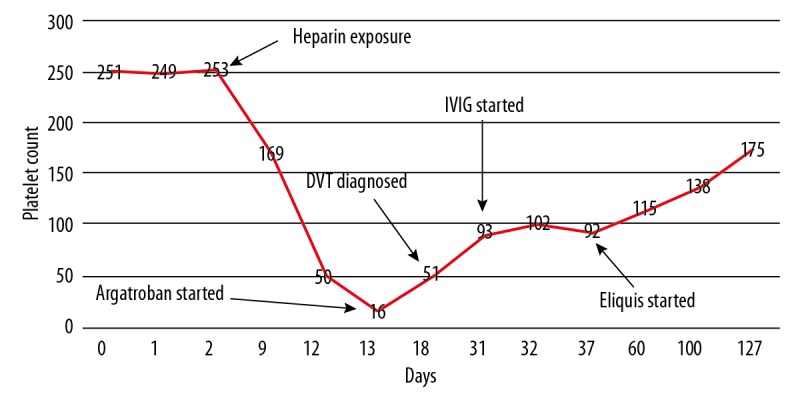
Trend in platelet counts depicted from the time of heparin exposure until platelet recovery.
Our case was unique in that it showed the failure of standard therapy and a response with IVIG. Our case is the first one to show a very slow response to IVIG, which has not been previously reported in literature studies. Our case also emphasizes the importance of starting anticoagulation therapy even in the setting of severe thrombocytopenia and this case is also the first of its kind where Eloquis was used for anticoagulation rather than warfarin.
Discussion
Autoimmune HIT (aHIT) refers to a range of syndromes that share a common feature; the presence of antiPF4 antibodies which causes platelet activation even in the absence of heparin (heparin-independent platelet activation). The syndromes which involve this phenomenon include spontaneous HIT, delayed onset HIT, persisting HIT, HIT induced by exposure to heparin “flushes”, fondaparinux-associated HIT, and HIT associated DIC [1,2]. Sometimes severe thrombocytopenia (platelet count of <20×109/L−) may be one of the presenting feature which may persists for weeks and is often accompanied by DIC and microvascular thrombosis [1,2]. Although heparin cessation is the cornerstone of management of HIT, in the case of aHIT, it does not interrupt the pathogenesis. Treatment options in acute HIT have always focused on either on-label therapies such as argatroban or danaparoid, or off-label use of fondaparinux or bivalirudin. When long-term anticoagulation is needed due to associated thrombosis, then transition to vitamin K antagonist (VKA) such as warfarin is made when platelet count recovers. Due to an increased risk of warfarin associated microthrombosis, earlier transition to VKA antagonist should be avoided. In recent times, there has been an increasing trend in the use of direct oral anticoagulants (DOACs) such as direct factor Xa inhibitors which includes apixaban, rivaroxaban, and edoxaban, or direct thrombin inhibitors such as dabigatran. A few attractive reasons to consider using these agents are the absence of any immunological interactions between them and HIT antibodies, the absence of reduction in protein C during acute phase of HIT thereby reducing the risk of microthrombosis, and lastly the quick transition from parenteral therapy to oral DOACs without waiting for platelet count recovery thereby reducing the longer hospitalization otherwise required when transitioning to VKA antagonists.
Patients with aHIT require full dose anticoagulation, and especially for a longer duration due to associated thrombosis. Severe thrombocytopenia usually associated with aHIT is not a contraindication for anticoagulation therapy and indeed patients require aggressive anticoagulation therapy to control the hypercoagulable state. An interesting finding in aHIT patients seems to be prolonged thrombocytopenia despite using alternative anticoagulation therapy. This represents the platelet activating effects of aHIT antibodies rather than ineffective anticoagulation. Hence measuring fibrinogen and D-dimers and sometimes measuring levels of anticoagulants, if possible, may be helpful in assessing the adequacy of anticoagulation. Dose increase is made based on the DIC parameters and the platelet counts.
Not much data is available on the use of DOACs in aHIT, although a few case reports show effectiveness of rivaroxaban in these cases. Poudel et al. reported a case wherein spontaneous HIT syndrome was observed after knee replacement surgery which showed failure of direct thrombin inhibitor (DTI) therapy [3], as was found in the case with our patient. Alternatively, some case reports have described the efficacy of rivaroxaban in controlling hypercoagulability in aHIT patients who previously failed argatroban or fondaparinux. One of the possible disadvantages may be the fluctuating levels of DOACs during the first 24 hours, which may be overcome by increasing the dose and frequency.
Warkentin et al. described the identification and classification of HIT patients treated with a DOAC [4]. The study involved 64 patients in total, of which 46 patients who had a probable HIT were treated with rivaroxaban [5–12]. Of these 46 patients, 25 patients were started on rivaroxaban as primary therapy and 21 patients as secondary therapy. In all, 2.2% of these patients had possible progression of thrombosis (central venous catheter-associated deep venous thrombosis resolved after catheter removal and during continued therapy with rivaroxaban). None of the 46 patients had any complications of major bleed whilst on rivaroxaban. Twenty-three patients were randomized to receive either apixaban (n=12) [7,13–15] or dabigatran (n=11) [8,16–20]. Possible thrombotic event was reported in 1 patient whilst on DOAC (multiple strokes, which might have been present before starting dabigatran).
The use of IVIG has been introduced for the management of aHIT, with the concept of interrupting the pathogenesis in aHIT. Tvito et al. reported abrupt platelet count recovery in 12 patients after administration of IVIG. One of these patients had a complication of recurrence of thrombocytopenia and was treated with a second dose of IVIG leading to complete recovery [21]. Plasma exchange theoretically would reduce aHIT antibodies thereby improving outcomes in aHIT; however, there is not enough evidence to support this technique. Our case was complex in that the platelet counts was very low when anticoagulation was initiated and there was also a delayed response to IVIG therapy for up to 3 months, which has not been reported so far.
Conclusions
In summary, aHIT is a devastating hypercoagulable state which continues to remain an important cause of mortality and morbidity in hospitalized patients. It needs special laboratory diagnostics and special treatment options. Differentiating HIT from aHIT is important when standard therapy fails, as immediate commencement of alternative therapy like IVIG is needed to reduce the mortality due to the high risk of complications associated with it when compared with classic HIT. Aggressive anticoagulation is often required to control the massive thrombin generation, and severe thrombocytopenia is not a contraindication for starting therapy. Adequate anticoagulation is achieved with non-PTT dependent rather than PTT dependent anticoagulants due to the associated DIC confounding the baseline PTT. DOAC offer a reasonable and practical option for these patients, although not much data is available to support their usage. Plasma exchange would theoretically reduce the burden of aHIT antibodies, but further studies are required to clarify its role.
References:
- 1.Greinacher A, Selleng K, Warkentin TE. Autoimmune heparin-induced thrombocytopenia. J Thromb Haemost. 2017;15:2099–114. doi: 10.1111/jth.13813. [DOI] [PubMed] [Google Scholar]
- 2.Warkentin TE, Pai M, Linkins LA. Direct oral anticoagulants for treatment of HIT: Update of Hamilton experience and literature review. Blood. 2017;130:1104–13. doi: 10.1182/blood-2017-04-778993. [DOI] [PubMed] [Google Scholar]
- 3.Poudel DR, Ghimire S, Dhital R, et al. Spontaneous HIT syndrome post-knee replacement surgery with delayed recovery of thrombocytopenia: A case report and literature review. Platelets. 2017;28:614–20. doi: 10.1080/09537104.2017.1366973. [DOI] [PubMed] [Google Scholar]
- 4.Kopolovic I, Warkentin TE. Progressive thrombocytopenia after cardiac surgery in a 67-year-old man. CMAJ. 2014;186:929–33. doi: 10.1503/cmaj.131449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kopolovic I, Warkentin TE. Progressive thrombocytopenia after cardiac surgery in a 67-year-old man. CMAJ. 2014;186(12):929–33. doi: 10.1503/cmaj.131449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ng HJ, Than H, Teo EC. First experiences with the use of rivaroxaban in the treatment of heparin-induced thrombocytopenia. Thromb Res. 2015;135(1):205–7. doi: 10.1016/j.thromres.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Sharifi M, Bay C, Vajo Z, et al. New oral anticoagulants in the treatment of heparin-induced thrombocytopenia. Thromb Res. 2015;135(4):607–9. doi: 10.1016/j.thromres.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 8.Hantson P, Lambert C, Hermans C. Rivaroxaban for arterial thrombosis related to heparin-induced thrombocytopenia. Blood Coagul Fibrinolysis. 2015;26(2):205–6. doi: 10.1097/MBC.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 9.Abouchakra L, Khabbaz Z, Abouassi S, Badaoui G. Rivaroxaban for treatment of heparin-induced thrombocytopenia after cardiac surgery: A case report. J Thorac Cardiovasc Surg. 2015;150(2):e19–20. doi: 10.1016/j.jtcvs.2015.04.054. [DOI] [PubMed] [Google Scholar]
- 10.Sartori M, Favaretto E, Cini M, et al. Rivaroxaban in the treatment of heparin induced thrombocytopenia. J Thromb Thrombolysis. 2015;40(3):392–94. doi: 10.1007/s11239-015-1208-4. [DOI] [PubMed] [Google Scholar]
- 11.Casan JM, Grigoriadis G, Chan N, Chunilal S. Rivaroxaban in treatment refractory heparin induced thrombocytopenia. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2016-216110. pii: bcr2016216110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samoš M, Bolek T, Ivanková J, et al. Heparin induced thrombocytopenia presenting with deep venous thrombosis and pulmonary embolism successfully treated with rivaroxaban: Clinical case report and review of current experiences. J Cardiovasc Pharmacol. 2016;68(5):391–94. doi: 10.1097/FJC.0000000000000421. [DOI] [PubMed] [Google Scholar]
- 13.Larsen PB, Jørgensen M, Friis-Hansen L, Ingeberg S. Apixaban used for the management of heparin-induced thrombocytopenia in a 72-year-old woman with lung cancer. Clin Case Rep. 2015;3(12):987–89. doi: 10.1002/ccr3.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delgado-García G, Monreal-Robles R, Gallegos-Arguijo D, Marfil-Rivera J. [Apixaban as therapeutic option in nephropathy patients with heparin-induced thrombocytopenia (HIT)] Gac Med Mex. 2015;151(6):798–801. [in Spanish] [PubMed] [Google Scholar]
- 15.Kunk PR, Brown J, McShane M, et al. Direct oral anticoagulants in hypercoagulable states. J Thromb Thrombolysis. 2017;43(1):79–85. doi: 10.1007/s11239-016-1420-x. [DOI] [PubMed] [Google Scholar]
- 16.Anniccherico FJ, Alonso JL. Dabigatran for heparin-induced thrombocytopenia. Mayo Clin Proc. 2013;88(9):1036. doi: 10.1016/j.mayocp.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 17.Mirdamadi A. Dabigatran, a direct thrombin inhibitor, can be a life-saving treatment in heparin induced thrombocytopenia. ARYA Atheroscler. 2013;9(1):112–14. [PMC free article] [PubMed] [Google Scholar]
- 18.Tardy-Poncet B, Piot M, Montmartin A, et al. Delayed-onset heparin induced thrombocytopenia without thrombosis in a patient receiving postoperative thromboprophylaxis with rivaroxaban. Thromb Haemost. 2015;114(3):652–54. doi: 10.1160/TH14-07-0593. [DOI] [PubMed] [Google Scholar]
- 19.Noel E, Abbas N, Skaradinskiy Y, Schreiber Z. Heparin-induced thrombocytopenia in a patient with essential thrombocythemia: A case-based update. Case Rep Hematol. 2015;2015:985253. doi: 10.1155/2015/985253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bircan HA, Alanoglu EG. Massive pulmonary embolism in a patient with heparin induced thrombocytopenia: successful treatment with dabigatran. Eurasian J Med. 2016;48(1):65–68. doi: 10.5152/eurasianjmed.2015.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tvito A, Bakchoul T, Rowe JM, et al. Severe and persistent heparin-induced thrombocytopenia despite fondaparinux treatment. Am J Hematol. 2015;90:675–78. doi: 10.1002/ajh.23971. [DOI] [PubMed] [Google Scholar]


