Abstract
Background:
Tubularized incised plate (TIP) urethroplasty is the most common technique noted to correct hypospadias. However, urethrocutaneous fistula (UCF) is still one of the most common complications of this technique. Several techniques of providing vascularized flaps to the neourethra have been recommended to decrease this complication rate. The aim of the study was to assess the outcome of primary repair of hypospadias using tunica vaginalis (TV) flap with those using preputial dartos (PD) fascia.
Patients and Methods:
Children diagnosed with hypospadias between the age group of 9 months to 18 years, who fulfilled the criteria were randomly divided into two groups by computerized randomization technique. Initially, TIP urethroplasty was done. Children with PD vascular cover were included in Group A and those with TV vascular cover were included in Group B. All the patients were followed up for a minimum of 6 months after surgery.
Results:
Two (10%) patients in Group A developed UCF and one (5%) patient developed stricture urethra in the follow-up period. None of the patients developed UCF in the Group B. One (5%) patient had stricture urethra in Group B. Two (10%) patient developed meatal stenosis in Group A. Two (10%) patient in Group B developed meatal stenosis.
Conclusions:
TV flap could be an alternative to PD flap as a vascular cover of neourethra in patients undergoing primary hypospadias repair by TIP urethroplasty.
Keywords: Hypospadias, preputial dartos, tubularized incised plate urethroplasty, tunica vaginalis, urethrocutaneous fistula
INTRODUCTION
Hypospadias surgery is one of the challenging areas in pediatric urology and has undergone continuous evolution even in the well-described surgeries. Tubularized incised plate (TIP) urethroplasty, described by Dr. Warren Snodgrass in 1994,[1] has become the choice of repair in most cases with suitable features. However, urethrocutaneous fistula (UCF) is still a bothersome complication following this technique with the conventional use of preputial dartos (PD) as a vascular cover. The use of tunica vaginalis (TV) flap in primary repair of hypospadias has been sparse according to studies, whereas we have many studies showing its extensive use in secondary repairs after failed hypospadias surgeries.[2,3,4,5,6,7,8] Hence, the need of the study with an aim to compare the outcome of primary hypospadias repair with TIP urethroplasty using TV as a vascular cover with those using PD flap. The objective of the study was to assess the results and complication rate in each group.
PATIENTS AND METHODS
Ethics
This study was in accordance with the ethical standards of the institutional ethical committee and was approved by the institutional ethical and research committee before the commencement of the study. The parents or guardians of children fulfilling the selection criteria were informed in detail about the nature of the study and written informed consent was obtained.
Study design
The study was a randomized controlled trial. The sample size of 40 was appropriate for the study (20 in each group). All children with diagnosis of hypospadias amenable for TIP repair who were admitted for surgery from January 1, 2016 to December 31, 2016 were eligible for the study. Children with hypospadias who were in the age group of 9 months to 18 years were included in the study. Children with failed hypospadias repair, previous inguinoscrotal surgery, that is, hernia or hydrocele repair or orchidopexy, associated undescended testis, patients who have undergone circumcision surgery, glandular hypospadias, severe chordee, no or poor urethral plate, and disorders of sexual development were excluded from the study.
The children who had fulfilled the criteria were randomly divided into 2 groups by computerized randomization technique. Children undergoing TIP urethroplasty with PD vascular cover were included in Group A and those with TV vascular cover were included in Group B. Demographic data such as age and history were obtained through an interview. Further, these children were subjected to clinical examination and findings such as meatal position, characteristics of meatus, shape of glans, adequacy of preputial fold, chordee, and corporal bodies were noted on a predesigned and pretested pro forma. Complete blood counts were done in all the children before surgery.
Operative procedure
In both the groups, the initial urethroplasty technique was the same, and was initial steps of Snodgrass urethroplasty. It was done using 2.5 magnification loupes and by a single surgeon. The patient was catheterized with 6–10 F number feeding tube approximately according to age and size of the urethra. A Firlit's collar incision was made around the corona of glans and 2 mm proximal to the hypospadiac meatus, and the penis was then degloved to the penoscrotal junction. An artificial erection test was done if chordee was still persistent after degloving and corrected accordingly. If the skin overlying the distal urethra was thin, the incision was extended proximally and the urethra was opened to this normal urethra before tubularization. Parallel longitudinal incisions approximately of 8 mm apart were taken to define the urethral plate, the glandular wings were raised laterally to facilitate subsequent glans closure. The edges of the urethral plate were gently elevated and retracted laterally with fine forceps. The plate is then incised in the midline from few mm within the meatus to the tip of the glans. This incision is carried deeply, dividing all transverse webs and exposing the underlying corporeal bodies. The epithelial strips created by longitudinal incision of the plate were confirmed to be separately mobile. Subsequently, the urethral plate was tubularized in single layer extra epithelially. Continous 6–0 polydioxanone suture with taper cut needle was used to close the plate over a 6–10 F infant feeding tube catheter, which provides urinary drainage for 10 days. Neourethra was then covered with PD flap [Figures 1 and 2] or TV flap [Figures 3 and 4] depending on which group the child belonged to and accordingly preuptial skin was dealt with. TV was dissected from the right testis and blanket cover was given over TIP repair in Group B. Glansplasty was done and the skin closure was achieved finally. The aseptic dressing was done and was removed on the postoperative day 10. All the children were followed up for a minimum period of 6 months [Figures 5-8]. None of the children were lost to follow-up.
Figure 1.
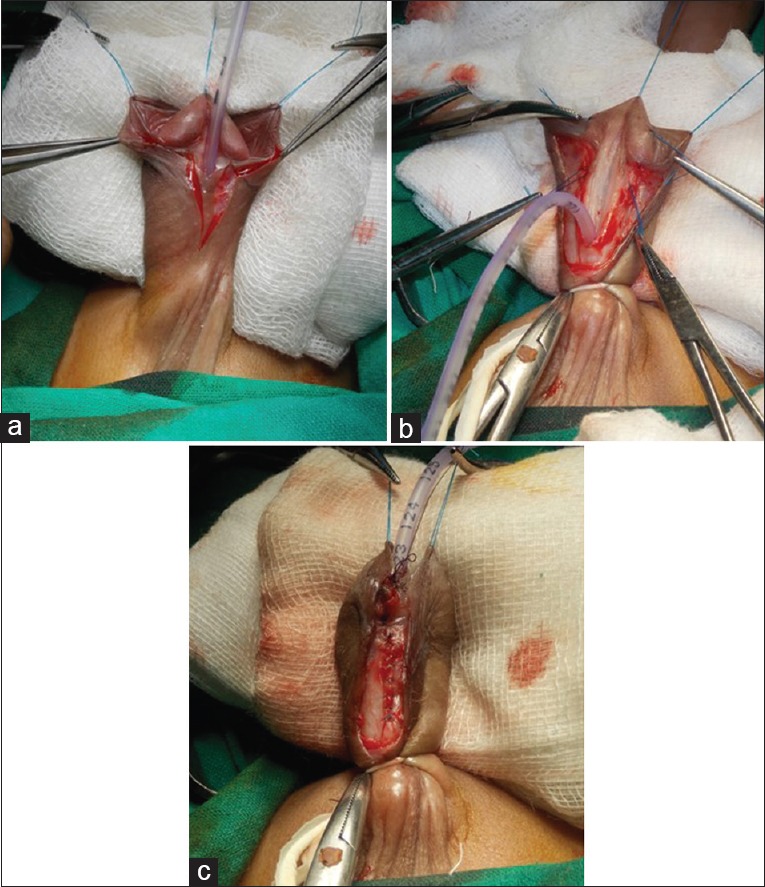
Intraoperative photographs of tubularized incised plate urethroplasty with preputial dartos vascular cover. (a) Skin incision for dissecting the skin flaps. (b) Incised urethral plate. (c) Neourethra covered with preputial dartos vascular cover
Figure 2.
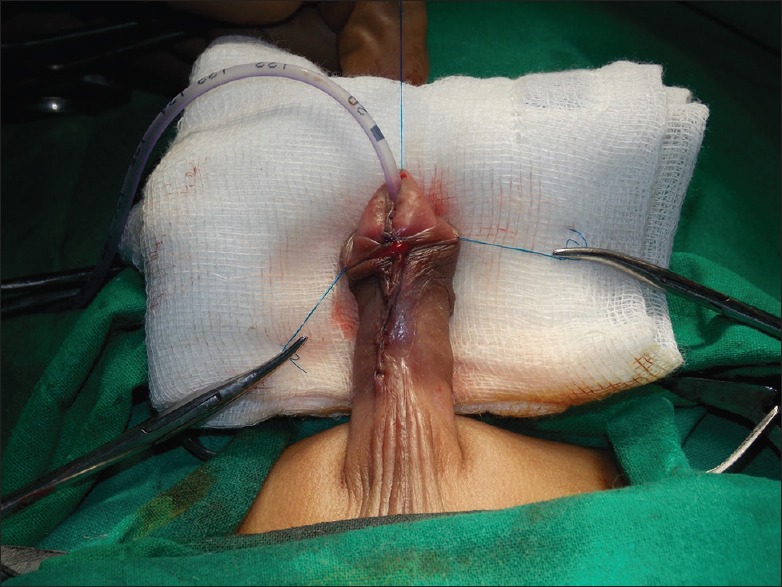
Immediate postoperative photograph of tubularized incised plate urethroplasty with preputial dartos vascular cover showing completed repair
Figure 3.
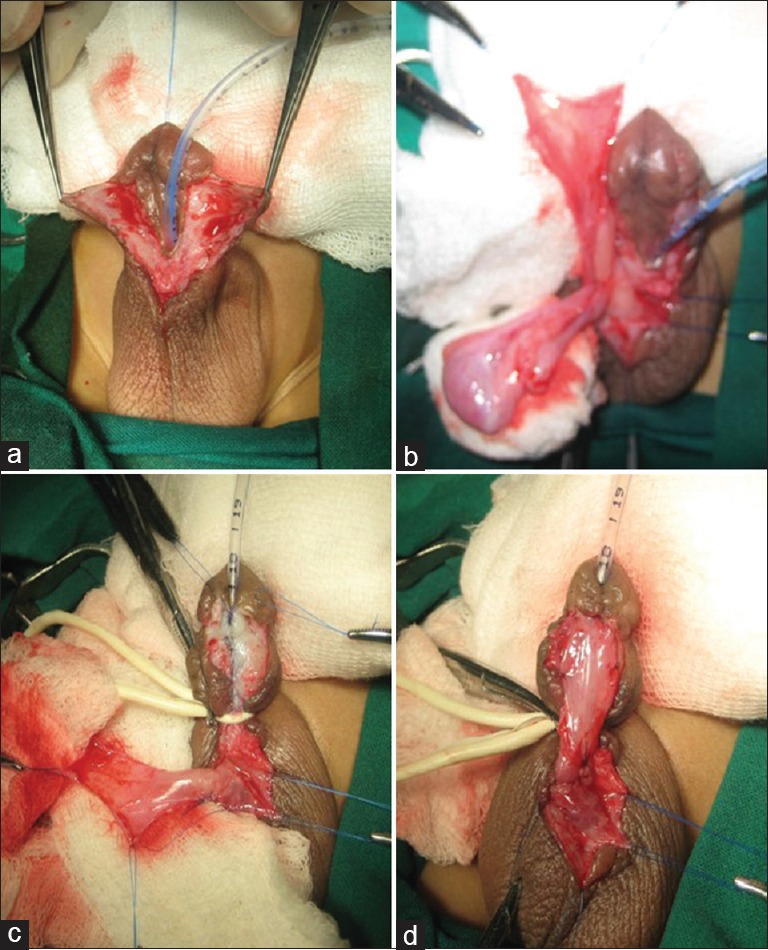
Intraoperative photographs of tubularized incised plate urethroplasty with tunica vaginalis vascular cover. (a) Dissected skin flaps. (b) Testis being delivered into operative field for harvesting tunica vaginalis flap. (c) Harvested tunica vaginalis flap. (d) Tunica vaginalis flap covering neourethra
Figure 4.

Immediate postoperative photograph of tubularized incised plate urethroplasty with tunica vaginalis flap showing completed repair
Figure 5.

Clinical photograph of a follow-up patient of preputial dartos flap repair showing well-healed scar
Figure 8.

Clinical photograph of a follow-up patient who underwent tubularized incised plate urethroplasty with tunica vaginalis vascular cover showing good caliber single urinary stream
Figure 6.

Clinical photograph of follow-up patient of tunica vaginalis flap repair showing well-healed scar
Figure 7.

Clinical photograph of a follow-up patient who underwent tubularized incised plate urethroplasty with preputial dartos vascular cover showing good caliber single urinary stream
Statistical analysis
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean and standard deviation. Quantitative variables were compared using unpaired t-test between two groups. Qualitative variables were compared using Chi-square test and Fisher's exact test as appropriate. P < 0.05 was considered statistically significant. The data were entered into MS Excel spreadsheet and analysis was done using Statistical Package for the Social Sciences version 21.0 (IBM Corp., IBM SPSS Statistics for Windows, Armonk, NY).
RESULTS
The data obtained were entered into Microsoft Excel Spreadsheet. The data were analyzed and the observations were tabulated.
The mean age of the children is shown in Tables 1 and 2. The detailed distribution of each clinical finding is summarized in Table 3. After the intraoperative correction of chordee, there were 20 cases of distal hypospadias, 8 cases of middle hypospadias, and 12 cases of proximal hypospadias [Table 4].
Table 1.
Mean age of the children considered in the study
| n | Minimum | Maximum | Mean | |
|---|---|---|---|---|
| Age (years) | 40 | 1.0 | 16.0 | 4.850 |
Table 2.
Mean age of the children in each group
| Vascular cover | Mean age (years) | SD |
|---|---|---|
| Preputial dartos | 4.17 | 3.112 |
| Tunica vaginalis | 5.25 | 4.97 |
SD: Standard deviation
Table 3.
Detailed distribution of clinical findings between two groups
| Vascular cover |
P | ||
|---|---|---|---|
| Group A (n=20) | Group B (n=20) | ||
| Meatal position | |||
| Distal | 13 | 9 | 0.164 |
| Mid-penile | 2 | 7 | |
| Proximal | 5 | 4 | |
| Characteristics of meatus | |||
| Normal | 16 | 16 | 1.00 |
| Stenotic | 4 | 4 | |
| Shape of glans | |||
| Conical | 18 | 19 | 0.548 |
| Flat | 2 | 1 | |
| Chordee | |||
| Absent | 14 | 13 | 0.270 |
| Present <30° | 1 | 4 | |
| Present >30° | 5 | 3 | |
| Corporal bodies | |||
| Good | 19 | 19 | 1.00 |
| Poor | 1 | 1 | |
Table 4.
Frequency of intraoperative diagnosis
| Diagnosis (intraoperative – after correction of chordee) | Frequency, n (%) |
|---|---|
| Distal hypospadias | 20 (50.0) |
| Mid-penile hypospadias | 8 (20.0) |
| Proximal hypospadias | 12 (30.0) |
| Total | 40 (100.0) |
In 34 patients, hypospadias repair was done under caudal anesthesia with IV sedation, and in the remaining patients, it was done under general anesthesia. Of the 34 children, 8 children required general anesthesia intraoperatively. Excessive blood loss was noted in 7 children, but none of the children required postoperative blood transfusion.
In our study, all the patients were followed up for a minimum of 6 months. Two (10%) patient developed meatal stenosis and one (5%) patient developed mild torsion of the testis in A group. Two (10%) patient in B group developed meatal stenosis. In the present study, two (10%) patients in A group developed UCF [Figure 9] and one (5%) patient developed stricture urethra in the follow-up period. None of the patients developed UCF in the B group. One (5%) patient had stricture urethra in B group. However, no significant difference was noted between the two groups for major complications (P = 0.442).
Figure 9.
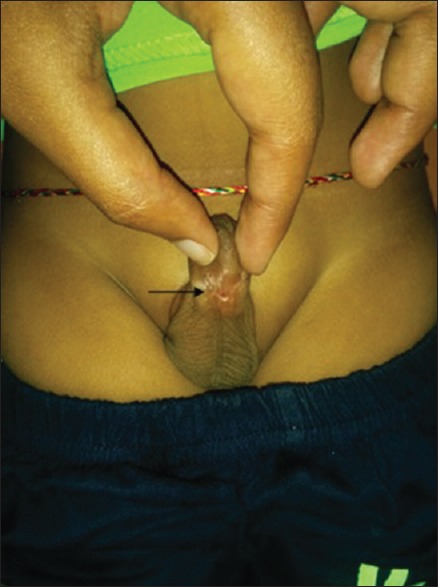
Clinical photograph of a follow-up patient of preputial dartos repair showing urethrocutaneous fistula (arrow), 3 months after surgery
DISCUSSION
Several techniques have been described for hypospadias repair, but no single surgery is considered ideal because of the unacceptable complication rates. Introduction of TIP urethroplasty by Snodgrass has revolutionized the outcome of hypospadias surgery, especially with reference to UCF. One of the major principles of TIP urethroplasty repair was to provide additional coverage to the neourethra to decrease the incidence of fistula formation. Various modifications have been tried to provide protective intermediate vascular cover to the neourethra, for example, Smith's flap,[9] Buck's fascial flap,[10] buccal mucosa,[11] dorsal dartos flap from the prepuce, dartos flap from the scrotum,[12] and TV.[13]
Snodgrass described the use of vascularized dartos tissue, dissected from dorsal preputial and shaft skin, for providing additional coverage to the neourethra.[14] Dartos based flaps require skillful dissection, and there are high chances that the vascularity of the overlying skin may get compromised leading to dermal necrosis. The advantage of dartos-based flaps is that they are locally available, are conventional and is universally practiced method.
Snow first described the use of TV as interposition graft and reported a fistula rate of 9%.[13] Since then many authors have used TV as interposition graft and have reported similar results.[2,15] TV vascular cover has several advantages. TV is thin, elastic in nature, expandable, easy to harvest, and close to the penile shaft. It has an independent blood supply from the cremasteric vessels, and its pedicle length can safely be increased even up to the external inguinal ring.[2]
In our study, total 40 children were considered in the study with a mean age of 5 years. Children requiring any kind of augmentation with either local application of testosterone cream or intramuscular testosterone injection were not included in the study. Chordee was present in 6 patients in A group and in 7 patients in B group. The correlation of age, position of the meatus, presence or absence of chordee, and preputial skin with the occurrence of complications as independent factors did not have any statistical significance. Excessive blood loss was present in 7 children, but none of the children required blood transfusion.
All the children were followed up for a minimum period of 6 months after surgery. Children were assessed for major complications, which included UCF, stricture urethra, complete wound dehiscence, and glans breakdown; and minor complications such as skin necrosis, local infection, and meatal stenosis.
In A group, 2 (10%) patients developed UCF. There was no fistula reported in B group. Similar results were reported by other authors as well. Snodgrass reported zero fistula rate in 14 patients with proximal hypospadias who were treated with double-layered urethroplasty and TV vascular cover.[14] Fistula formation and other complications were found to be low with the use of TV vascular cover as demonstrated by Guralnick et al.[16] and Landau et al.[6] Routh et al. reported fistula rate of 0% when TV flap was used along with operative microscope.[8] Chatterjee et al.[17] reported fistula rate of 0% and 15%–20% for cases with TV flap and dartos flap, respectively. Dhua et al.[10] in their study found a fistula rate of 12% with dartos flap and 0% with TV flap. Hamid et al.[7] reported fistula rate of 2.85% with TV flap cover. The fistula rate reported by our study was found to be similar to other reported series. Decreased fistula rate in our study might be due to shorter duration of follow up. Both the patients with UCF required redo surgery. Redo surgery was done with TV flap cover, and the follow-up period was uneventful without any complications.
Meatal stenosis occurred in four (10%) patients, two in each group and required surgical management with ventral meatoplasty. Meatal stenosis was reported in one patient (2.85%) in study conducted by Hamid et al.[7] where TV flap was used. Babu et al.[18] encountered 4 (6.4%) and 1 (4.77%) cases of meatal stenosis in dartos flap and TV group, respectively. Chatterjee et al.[17] did not report any cases of meatal stenosis in their study.
Stricture urethra occurred in two patients, one in each group, and was adequately managed with urethral dilatation/calibration. However, there was no statistical significance noted between the two groups with respect to major (P = 0.442) complications.
Use of dartos flap is associated with higher morbidity. Complications such as dermal necrosis and complete breakdown of repair are known. This is because of the compromise in the blood supply to the dorsal skin while dissection of dartos fascia. In cases of distal hypospadias, the ventral skin cover is adequate. However, in midshaft and proximal hypospadias, there is insufficient skin and ventral cover is provided by rotating the dorsal outer foreskin. If the blood supply to this gets compromised while dissecting dartos flap, it can result in ventral skin necrosis and UCF.[18] Total breakdown of repair is also known in repair with dartos flap. However, TV flap is easier to dissect and has an independent blood supply. Since the outcome of hypospadias surgery depends on the vascularity of the flap used to cover neourethra, TV flap is a good alternative to dartos flap. This supports the available evidence that use of TV flap is associated with decreased complications, especially the rate of UCF. Hence, decreasing the exposure of pediatric group to multiple surgeries and repeated anesthesia. TV flap can be used as waterproofing layer in previously circumscribed patients as well.[10]
The limitation of our study was small sample size and shorter duration of follow-up. There are no guidelines specifying the duration of follow-up following hypospadias repair. A study was conducted by Snodgrass et al., to determine the timing of development of urethroplasty complications in patients undergoing primary and reoperative TIP repair to determine the duration of follow-up. They concluded that majority of urethroplasty complications are diagnosed at the first postoperative visit or within the first year following TIP hypospadias repair.[19]
The strength of the study is that it is a randomized controlled trial, procedures were performed by a single surgeon and most variables were matched including similar population.
CONCLUSIONS
In the study, repair with TV flap was associated with lesser complications; however, it was statistically not significant, as compared to that of PD repair. Use of TV flap has been extended for use in primary repair apart from its regular use with redo hypospadias repair. In difficult cases where PD is unavailable, or where it is difficult to give vascular cover, TV may be used with ease, is also efficacious and even safe. The time and skill required to create a PD flap is more, compared to TV flap, which was found in this study. The complications specifically arising due to dissection of the flap are rare with TV and are treatable. Hence, it is advisable to judiciously choose one of the vascular cover either TV or PD cover.
TV flap could be an alternative to PD flap for covering the neourethra with a vascularized flap, resulting in fewer complications and acceptable results. However, long-term studies are required to conclude the same.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Snodgrass W. Tubularized, incised plate urethroplasty for distal hypospadias. J Urol. 1994;151:464–5. doi: 10.1016/s0022-5347(17)34991-1. [DOI] [PubMed] [Google Scholar]
- 2.Handoo YR. Role of tunica vaginalis interposition layer in hypospasdias surgery. Indian J Plast Surg. 2006;39:152–6. [Google Scholar]
- 3.Kadian YS, Rattan KN, Singh J, Singh M, Kajal P, Parihar D, et al. Tunica vaginalis: An aid in hypospadias fistula repair: Our experience of 14 cases. Afr J Paediatr Surg. 2011;8:164–7. doi: 10.4103/0189-6725.86054. [DOI] [PubMed] [Google Scholar]
- 4.Sharma N, Bajpai M, Panda SS, Singh A. Tunica vaginalis flap cover in repair of recurrent proximal urethrocutaneous fistula: A final solution. Afr J Paediatr Surg. 2013;10:311–4. doi: 10.4103/0189-6725.125421. [DOI] [PubMed] [Google Scholar]
- 5.Muruganandham K, Ansari MS, Dubey D, Mandhani A, Srivastava A, Kapoor R, et al. Urethrocutaneous fistula after hypospadias repair: Outcome of three types of closure techniques. Pediatr Surg Int. 2010;26:305–8. doi: 10.1007/s00383-009-2490-z. [DOI] [PubMed] [Google Scholar]
- 6.Landau EH, Gofrit ON, Meretyk S, Katz G, Golijanin D, Shenfeld OZ, et al. Outcome analysis of tunica vaginalis flap for the correction of recurrent urethrocutaneous fistula in children. J Urol. 2003;170:1596–9. doi: 10.1097/01.ju.0000084661.05347.58. [DOI] [PubMed] [Google Scholar]
- 7.Hamid R, Baba AA, Shera A, Ahmad S. Tunica vaginalis flap following 'Tubularised Incised Plate' urethroplasty to prevent urethrocutaneous fistulaa. Indian J Plast Surg. 2015;48:187–91. doi: 10.4103/0970-0358.163059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Routh JC, Wolpert JJ, Reinberg Y. Tunneled tunica vaginalis flap is an effective technique for recurrent urethrocutaneous fistulas following tubularized incised plate urethroplasty. J Urol. 2006;176:1578–80. doi: 10.1016/j.juro.2006.06.032. [DOI] [PubMed] [Google Scholar]
- 9.Smith D. A de-epithelialised overlap flap technique in the repair of hypospadias. Br J Plast Surg. 1973;26:106–14. doi: 10.1016/s0007-1226(73)80003-7. [DOI] [PubMed] [Google Scholar]
- 10.Dhua AK, Aggarwal SK, Sinha S, Ratan SK. Soft tissue covers in hypospadias surgery: Is tunica vaginalis better than dartos flap? J Indian Assoc Pediatr Surg. 2012;17:16–9. doi: 10.4103/0971-9261.91080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmed S, Gough DC. Buccal mucosal graft for secondary hypospadias repair and urethral replacement. Br J Urol. 1997;80:328–30. doi: 10.1046/j.1464-410x.1997.00134.x. [DOI] [PubMed] [Google Scholar]
- 12.Motiwala HG. Dartos flap: An aid to urethral reconstruction. Br J Urol. 1993;72:260–1. doi: 10.1111/j.1464-410x.1993.tb00710.x. [DOI] [PubMed] [Google Scholar]
- 13.Snow BW. Use of tunica vaginalis to prevent fistulas in hypospadias surgery. J Urol. 1986;136:861–3. doi: 10.1016/s0022-5347(17)45106-8. [DOI] [PubMed] [Google Scholar]
- 14.Snodgrass WT. Editorial comment. J Urol. 2007;178:1456. doi: 10.1016/j.juro.2008.03.077. [DOI] [PubMed] [Google Scholar]
- 15.Shankar KR, Losty PD, Hopper M, Wong L, Rickwood AM. Outcome of hypospadias fistula repair. BJU Int. 2002;89:103–5. [PubMed] [Google Scholar]
- 16.Guralnick ML, al-Shammari A, Williot PE, Leonard MP. Outcome of hypospadias repair using the tubularized, incised plate urethroplasty. Can J Urol. 2000;7:986–91. [PubMed] [Google Scholar]
- 17.Chatterjee US, Mandal MK, Basu S, Das R, Majhi T. Comparative study of dartos fascia and tunica vaginalis pedicle wrap for the tubularized incised plate in primary hypospadias repair. BJU Int. 2004;94:1102–4. doi: 10.1111/j.1464-410X.2004.05111.x. [DOI] [PubMed] [Google Scholar]
- 18.Babu R, Hariharasudhan S. Tunica vaginalis flap is superior to inner preputial dartos flap as a waterproofing layer for primary TIP repair in midshaft hypospadias. J Pediatr Urol. 2013;9:804–7. doi: 10.1016/j.jpurol.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 19.Snodgrass W, Villanueva C, Bush NC. Duration of follow-up to diagnose hypospadias urethroplasty complications. J Pediatr Urol. 2014;10:208–11. doi: 10.1016/j.jpurol.2013.11.011. [DOI] [PubMed] [Google Scholar]


