ABSTRACT
Background: The variables that underlie comorbid chronic pain and posttraumatic stress symptoms (PTSS) are not yet clearly established.
Objective: The aim of the present study was to analyse the role of the behavioural inhibition system (BIS), behavioural approach system (BAS) and experiential avoidance (EA) in pain adjustment (i.e. pain intensity, daily functioning and pain-related impairment) in patients with chronic pain and PTSS.
Methods: A battery of instruments was administered to 388 chronic pain patients. The sample was divided into those with PTSS (n = 194) and those without PTSS (n =194).
Results: Significant differences were found between groups in the BIS, EA, impairment and daily functioning. No differences were found between groups in the BAS. Structural equation modelling showed that the BIS and EA were associated with worse adjustment in the 194 patients with both chronic pain and PTSS. The BAS was associated with a lower level of pain and greater daily functioning.
Conclusion: The findings provide evidence that BIS and BAS activation and EA play a role in adjustment to chronic pain in patients with concurrent PTSS. These results may help guide the development of psychological treatments for patients with both conditions.
KEYWORDS: Chronic pain, posttraumatic stress symptoms, behavioural inhibition system, behavioural approach system, experiential avoidance, pain adjustment
HIGHLIGHTS
• This is the first study to examine the role of the behavioural inhibition system, the behavioural activation system, experiential avoidance in comorbid chronic pain and posttraumatic stress symptoms. • Differences between patients with and without posttraumatic stress symptoms in behavioural inhibition system and experiential avoidance were found, thus providing a preliminary comprehensive framework for understanding the co-occurrence of both disorders. • The findings may help guide the development of psychological treatments for patients with both conditions.
Abstract
Antecedentes: las variables que subyacen al dolor crónico comórbido y síntomas de estrés postraumático aún no están claramente establecidas.
Objetivo: el propósito del presente estudio fue analizar el rol del Sistema de Inhibición del Comportamiento (BIS), el Sistema de activación del Comportamiento (BAS) y la Evitación Experiencial (EA) en la adaptación all dolor (es decir, intensidad del dolor, funcionamiento diario e incapacidad relacionada con dolor) en pacientes con dolor crónico y síntomas de estrés postraumático (PTSS).
Métodos: Se administró una batería de instrumentos a 388 pacientes con dolor crónico. La muestra se dividió en aquellos con PTSS (n = 194) y aquellos sin PTSS (n = 194).
Resultados: Se encontraron diferencias significativas entre grupos en el BIS, EA, incapacidad y funcionamiento diario. No se encontraron diferencias entre grupos en el BAS. El modelo de ecuaciones estructurales mostró que BIS y EA se asociaron con un peor ajuste en los 194 pacientes con dolor crónico y PTSS concomitante. El BAS se asoció con menor nivel de dolor y funcionamiento diario mayor.
Conclusión: los hallazgos proveen evidencia de que la activación de BIS y BAS y la EA desempeñan un rol en el ajuste al dolor crónico en pacientes con PTSS concurrente. Estos resultados podrían ayudar a guiar el desarrollo de tratamientos psicológicos para pacientes con ambas afecciones.
PALABRAS CLAVE: Dolor crónico, síntomas de estrés postraumático, sistema de inhibición del comportamiento, sistema de activación del comportamiento, evitación experiencial, adaptación al dolor
Abstract
背景:尚未明确慢性疼痛共病创伤后应激症状的影响变量。
目的:本研究的目的是分析慢性疼痛共病创伤后应激症状(PTSS)的病人中,行为抑制系统(BIS)、行为激活系统(BAS)和经验避免(EA)在疼痛适应(即疼痛强度,日常功能和疼痛相关的伤害)中的作用。
方法:对388名慢性疼痛患者使用一套测量工具,分成具有PTSS(n = 194)和没有PTSS(n = 194)的两组。
结果:在BIS、EA、损伤和日常功能方面,两组之间存在显著差异。各组之间未发现BAS差异。结构方程模型显示,在194例慢性疼痛+PTSS患者组中,BIS和EA与较差的疼痛适应相关。 BAS与较低水平的疼痛和较高的日常功能相关。
结论:该研究结果提供证据表明BIS、BAS激活和EA在并发PTSS的患者对慢性疼痛的适应中起作用。这些结果可能有助于指导患有这两种疾病的患者的心理治疗的发展。
关键词: 慢性疼痛,创伤后应激症状,行为抑制系统,行为方法系统,经验避免,疼痛调节
1. Introduction
A substantial body of evidence has demonstrated the co-occurrence of posttraumatic stress disorder (PTSD) and chronic pain syndromes (e.g. Siqveland, Hussain, Lindstrøm, Ruud, & Hauff, 2017). Their comorbidity ranges between 10 and 50% of patients; thus, the prevalence of PTSD in patients with chronic pain (CP) is 2–5 times higher than its average prevalence in the general population (Defrin, Schreiber, & Ginzburg, 2015). This result may be explained by the fact that both health problems seem to be central sensitization syndromes (e.g. Fleming & Volcheck, 2015), which are characterized by hyperexcitability of the central nervous system (Arendt-Nielsen et al., 2018).
Two neuropsychological systems could potentially underlie both disorders and contribute to explaining the aforementioned differences: the behavioural inhibition system (BIS) and the behavioural approach system (BAS). The original version of Gray’s Reinforcement Sensitivity Theory (Gray, 1987a, 1987b; Gray & McNaughton, 2000) describes the BIS and BAS as neuropsychological systems that are automatically activated by environmental or internal cues. The initial version of this broad framework of motivation, emotion and learning (Smillie, Pickering, & Jackson, 2006) outlined three major biobehavioural components that are automatically and relatively independently activated: the BIS, the BAS and the fight/flight system (FFS) (Gray, 1987a, 1987b). It was hypothesized that the BIS is automatically activated by aversive or new/intense stimuli, the BAS is activated by cues associated with the reinforcement or disappearance of expected punishment, and the FFS is activated by unconditioned aversive stimuli. Nevertheless, some of these initial postulates were revised (for a review, see Smillie et al., 2006). Thus, Gray and McNaughton (2000) proposed that the FFS is activated by unconditioned and conditioned aversive stimuli, and renamed as the fight/flight/freeze system (FFFS). The authors also suggested that the BIS mediates the resolution of goal conflicts between the BAS and FFS, and between the BAS-BAS and/or FSS-FSS. Subsequently, McNaughton and Corr (2008) noted that the BIS and FFFS were closely associated, because FFFS activation was thought to be preceded by BIS activation. Therefore, both systems could be combined into a single ‘punishment sensitivity’ factor, as named by Corr (2009). In fact, Corr (2002) had already formulated a ‘joint subsystems hypothesis’, which postulated that the BIS and BAS may work synergistically such that the impact of one function would be influenced by the relative activation of the other. As a result, dysfunction is higher in individuals with both high BIS activation and lower BAS activation and vice versa.
Jensen, Ehde, and Day (2016) recently formulated the BIS-BAS model of CP, which hypothesizes that experience of pain would result in (1) more behavioural inhibition and subsequent negative psychological function and (2) less behavioural activation and subsequent positive emotions. The model also hypothesizes that a BIS-BAS interaction is possible in some contexts, but is unlikely to emerge across all settings (Serrano-Ibáñez, López-Martínez, Ramírez-Maestrea, Esteve, & Jensen, 2019). Initial empirical evidence supports this model. Thus, it has been found that the BIS has a significant nonlinear association with pain intensity and that the BIS are associated with headache frequency in college students (Jensen, Tan, & Chua, 2015). Studies using clinical samples of patients with CP have shown that the BIS moderated the association between pain-related cognitions and psychological function (Jensen et al., 2017). Consistent with this result, Muris et al. (2007) showed that the BIS accounted for a proportion of the variance in pain catastrophizing.
In addition, Jensen et al. (2015) showed that BAS scores were not significantly associated with pain intensity or pain frequency, although having severe headaches was associated with lower BAS scale scores. Becerra-García and Robles Jurado (2014) found BAS hypoactivity in patients with fibromyalgia, who were less sensitive to reward signals than the control group. The authors suggested that this would lead to a decreased tendency to have positive affective states, which is a frequent emotional response in patients with CP. It is has also been demonstrated that reward responsiveness is reduced in CP patients. The study by Elvemo, Landrø, Borchgrevink, and Haberg (2015) demonstrated a reduced hedonic response to rewards in individuals with CP of heterogeneous etiology. It is of interest that a significant correlation was found between a reduction in reward responsiveness and a smaller nucleus accumbens, which plays a significant role in reward processing (Salamone & Correa, 2012) and is associated with the dopaminergic neurotransmitter system (Elvemo et al., 2015).
On the other hand, it has been suggested that PTSD is a disorder characterized by an altered balance between approach (the BAS) and avoidance (the BIS), in which an external trauma modulates this balance by up-regulating or down-regulating the sensitivity of neural substrates that process reward or fear (Stein & Paulus, 2009). In fact, several studies have demonstrated an association between both systems and PTSD. Thus, a positive association has been found between the BIS and increased PTSD severity (Contractor, Elhai, Ractliffe, & Forbes, 2013; Myers, VanMeenen, & Servatius, 2012). Longitudinal studies in young Latinos have shown that high baseline levels of BIS increased the risk of developing PTSD (Gudiño, 2013; Gudiño, Nadeem, Kataoka, & Lau, 2012). In addition, some results have suggested that the BAS is associated with PTSD, although the direction of this association has not been clearly established (Pickett, Bardeen, & Orcutt, 2011). However, recent research has supported the inclusion of PTSD within a reward deficiency spectrum characterized by the hypofunctionality of reward circuitry, manifesting as a decrease in the motivation and capacity to experience pleasure that is mediated by abnormalities in dopamine receptors (Elman et al., 2009).
It is worth noting that individual differences in the BIS and BAS may have implications for emotion regulation, as has been suggested by Tull, Gratz, Latzman, Kimbrel, and Lejuez (2010). A recent study by Serrano-Ibáñez et al. (2018) found a positive association between BIS activation and emotion regulation difficulties (i.e. increased use of expressive suppression and decreased use of cognitive reappraisal), whereas no association was found between the BAS and the regulatory strategies assessed. The authors concluded that individuals with CP with increased BIS activation would be expected to be less able to identify and manage their emotions. This response could lead to an increase in maladaptive emotional regulation patterns.
Empirical studies have demonstrated that the way in which patients regulate their emotions could be relevant to CP (Hamilton, Karoly, & Kitzman, 2004) and to PTSD (Shepherd & Wild, 2014). In this sense, EA could be of relevance as a form of emotional (dys)regulation strategy used to avoid negative experiences that reduces levels of distress in the short term but increases emotional dysregulation in the long term (Hayes, Luoma, Bond, Masuda, & Lillis, 2006). Experiential avoidance (EA) has been considered to be involved in the etiology and maintenance of PTSD (e.g. Marx & Sloan, 2005) and has also been shown to play a relevant role in adjustment to CP with PTSD symptoms (Ruiz-Párraga & López-Martínez, 2015) and CP without PTSD symptoms (Esteve, Ramírez-Maestre, & López-Martínez, 2012). In addition, significant differences in EA have been reported between patients with CP who experienced a traumatic experience and developed PTSD symptoms and similar patients who did not develop PTSD symptoms (Ruiz-Párraga & López-Martínez, 2014). Furthermore, some findings have also suggested that EA moderates the association between the BIS and PTSD (e.g. Maack, Tull, & Gratz, 2012). For example, Pickett et al. (2011) found significant differences in PTSD symptoms associated with BIS sensitivity in patients with higher levels of EA: higher scores on measures of the BIS were associated with higher scores on measures of PTSD symptoms. This result suggests that an unwillingness to experience unwanted private experiences in conjunction with increased BIS sensitivity contributes to the severity of PTSD symptoms (Pickett et al., 2011). Similarly, these authors found a significant positive association between the BAS and EA: higher levels of ‘fun seeking’ were associated with higher levels of EA. They suggested that seeking new rewards or approaching rewards impulsively could be associated with emotion regulation difficulties and could lead to maladaptive self-regulatory strategies.
In summary, and taking into account the foregoing considerations, we assumed that the BIS could play a more relevant role than the BAS in individuals with both CP and PTSD because they have a reduced responsiveness to rewards. We also assumed that individual differences in BIS and BAS activation could affect EA (as a form of emotion regulation approach). Given the demonstrated role of EA in the maintenance of PTSD and in the psychological and physical functioning of individuals with CP, we predicted that persons with comorbid CP and PTSD symptoms would have increased BIS activation, decreased BAS activation and higher EA.
Given these considerations, the aim of the study was to better understand the role of the BIS, BAS and EA in pain adjustment in patients with comorbid PTSD symptoms and CP. Specifically, we investigated differences in the BIS, BAS, EA and pain adjustment (i.e. pain intensity, daily functioning and impairment) in two groups of chronic musculoskeletal pain patients. The two groups comprised patients who had been exposed to traumatic events and developed PTSD symptoms [TE with PTSS group] before the onset of pain and similar patients who did not develop PTSD symptoms [TE group]. It was hypothesized that the TE with PTSS group would have significantly higher scores on measures of the BIS, EA, impairment and pain intensity, and lower scores on measures of the BAS and daily functioning. We also assessed the contribution of the BIS, BAS and EA to PTSD symptoms and pain adjustment in the TE with PTSS group. The following predictions were made: a significant positive association would be found between higher levels of the BIS and EA; a significant negative association would be found between higher levels of the BAS and EA; a significant positive association would be found between EA and PTSD symptoms; a positive direct association would be found between PTSD symptoms and pain intensity and impairment; and a negative association would be found between PTSD symptoms and daily functioning.
2. Method
2.1. Participants and procedures
The participants comprised patients with chronic musculoskeletal pain of benign origin. Several inclusion criteria were considered. Firstly, participants had to be between 18 and 65 years of age. Secondly, participants had to have (a) pain of benign origin for at least the last three months, (b) pain intensity equal to or greater than 3 on a 0 to 10 scale and (c) continuous or intermittent pain at least five or more days per week (Guerra de Hoyos et al., 2007). Finally, to ensure that the physical and psychological symptoms of the participants were not due to PTSD symptoms or to a CP diagnosis, exclusion criteria were (a) the absence of other chronic physical disease (e.g. neurological disease) or (b) the absence of psychiatric disease (e.g. bipolar disorder). Patients who fulfilled these criteria were informed by physicians from several hospital pain units in Málaga (Spain) of the study aim and their participation was requested. In addition, participants were recruited from several local associations of patients with pain and fibromyalgia. Participants who accepted were given an appointment.
A total of 516 participants were interviewed by two trained psychologists in a semi-structured interview. Signed informed consent was provided by all participants prior to data collection. The study procedures complied with the Declaration of Helsinki recommendations and the Hospital Institutional Review Board reviewed the protocols and approved the study.
Additional criteria were applied to divide the group into the TE group and the TE with PTSS group. Figure 1 shows the selection process. Firstly, patients were considered to be trauma-exposed if they answered Yes to one or more items on the Life Events Checklist (Gray, Litz, Hsu, & Lombardo, 2004). This process excluded 34 patients. Secondly, only participants who had been exposed to traumatic events before the onset of pain were selected. This second process excluded nine participants. Thirdly, patients living in a high-stress situation at the time of the evaluation were excluded. Thus, another three patients were excluded. Fourthly, patients who reported having experienced a traumatic situation completed the Spanish version of the Posttraumatic Stress Disorder Checklist-Civilian Version (PCL-C; Orlando & Marshall, 2002). Patients who had a score equal to or greater than 36 were considered to have PTSS. This score is considered to be the cutoff for PTSD in specialized medical clinics (Sherman, Carlson, Wilson, Okeson, & McCubbin, 2005).
Figure 1.

Selection process of the participants groups.
Of the remaining 469 participants, 57.05% (275 patients) did not have PTSS and 40.46% (194 patients) had PTSS. Participants in the TE group were randomly selected in order to adjust the size of the two groups. Thus, the final sample comprised 388 patients divided into the two subgroups: (a) 194 patients with chronic musculoskeletal pain who had experienced one or more traumatic events but did not have PTSS (TE group); and (b) 194 patients who had experienced one or more traumatic events and had PTSS (TE with PTSS).
2.2. Measures
2.2.1. Demographic and medical history
Participants provided information on demographic characteristics (sex, age, marital status, highest level of education completed and employment status) and their medical history (such as the time of onset of pain and pain duration).
2.2.2. BIS and BAS activity
BIS and BAS activity was assessed using the Sensitivity to Punishment and Sensitivity to Reward Questionnaire (SPSRQ-20; Aluja & Blanch, 2011), which is a 20-item measure with a dichotomous response (Yes or No). This instrument was developed to test the BIS (10 items) and BAS (10 items) constructs in Gray’s theory. The SPSRQ-20 has been shown to have a robust bivariate structure (BIS/BAS), demonstrated construct validity, and adequate levels of internal consistency (Aluja & Blanch, 2011). In the present study, Cronbach´s alphas were 0.90 and 0.81 for the BIS and BAS, respectively.
2.2.3. Experiential avoidance
EA was assessed using the Spanish version (Ruiz, Langer Herrera, Luciano, Cangas, & Beltrán, 2013) of the 7-item Acceptance and Action Questionnaire-II (AAQ-II). Items are measured on a 7-point Likert scale (ranging from 1 = never true to 7 = always true). The psychometric properties of the Spanish version of this questionnaire are similar to the original, with good reliability, internal consistency, test-retest reliability and concurrent validity (Ruiz et al., 2013). In this study, Cronbach’s alpha for the AAQ-II was 0.94.
2.2.4. Trauma exposure
Trauma exposure was assessed using the Life Events Checklist (LEC; Gray et al., 2004). This instrument assesses 13 specific DSM-IV PTSD Criterion-A events. An extra Yes/No question was included to determine whether each traumatic event was experienced before or after the onset of pain. The LEC has adequate temporal stability, good convergence with an established measure of trauma history and concurrent validity (Gray et al., 2004).
2.2.5. Posttraumatic stress symptoms
Posttraumatic stress symptoms (PTSS) were assessed using the Spanish version (Orlando & Marshall, 2002) of the Posttraumatic Stress Disorder Checklist-Civilian Version (PCL-C). This instrument comprises a 17-item checklist developed to assess the degree to which each particular posttraumatic stress symptom was experienced over the past month. Participants were asked to rate each item on a 5-point Likert-scale ranging from 1 (Not at all) to 5 (Extremely). This scale has good psychometric properties (internal consistency, test-retest reliability and convergent validity with other PTSD symptom scale) (Orlando & Marshall, 2002). In addition, it has been shown that the English and Spanish versions of the PCL-C are broadly equivalent (Miles, Marshall, & Schell, 2008). In this study, Cronbach´s alpha for the PCL-C was 0.94.
2.2.6. Perceived pain intensity
Participants were asked about their current, worst, least and average pain intensity during the previous two weeks (Jensen, Turner, Romano, & Fisher, 1999). Each of these was scored on an 11-point scale ranging from 0 (No pain) to 10 (Worst pain). The composite pain intensity score was calculated for each participant by averaging the mildest, average, worst and current pain scores. Composites of the 0–10 ratings have been demonstrated to be very reliable measures of pain intensity in CP patients (Jensen et al., 1999).
2.2.7. Functioning and impairment
Functioning and impairment were assessed using the 30-item Impairment and Functioning Inventory-Revised (IFI-R; Ramírez-Maestre & Esteve, 2015). The IFI was developed to assess specific activities associated with autonomous behaviour, household, social relationships and leisure in CP patients. Participants indicate how many times they performed each activity in the previous week on a scale ranging from 0 (Never) to 4 (10 or more times). In the event that they did not perform a specific activity, the participants indicate if they did not do so because of pain. ‘Functioning’ and ‘impairment’ were calculated by summing the frequencies of each activity and summing the number of activities that the participant did not perform because of pain, respectively. This instrument provides an index of functioning, an index of impairment, and scores for each of these areas, and offers advantages in assessing patients with a long history of pain where the degree of deterioration is at least as informative as the current level of functioning. The subscales and the global scales showed adequate reliability, convergent validity and criterion validity (Ramírez-Maestre & Esteve, 2015). In this study, Cronbach´s alphas were 0.87 for functioning and 0.84 for impairment.
2.3. Analytic strategy
We calculated means, standard deviations and Pearson’s correlations between variables, and tested the assumptions of normality, multicollinearity and homoscedasticity. Differences between the TE and TE with PTSS groups in demographic and clinical variables were calculated to analyse homogeneity. Specifically, chi-square Pearson tests were conducted for marital status, level of education and pain diagnosis. Student t-tests were conducted to analyse differences in age and pain duration. Several within-groups Student t-tests were conducted to analyse differences between men and women in each dependent variable.
Six univariate linear models were conducted to investigate differences between the TE and TE with PTSS groups in the BIS, BAS, EA, perceived pain, impairment and functioning. Pain diagnosis and the number of traumas were used as covariates in the analyses. Partial eta squared (η2p) was used to estimate effect size, with values of .06, .14 and > .14 considered to be small, moderate and large effects, respectively (Cohen, 1988).
Structural equation modelling (SEM) was conducted to test the hypothetical model (see Figure 2) in the TE with PTSS group. Maximum likelihood estimation was used because all the variables were normally distributed. The following goodness-of-fit indexes were applied: (a) The Satorra-Bentler chi-square divided by the degrees of freedom: values less than or equal to 3 indicate acceptable model fit (Kline, 2005); (b) the root mean square error approximation (RMSEA): values less than 0.06 indicate a good fit; (c) the adjusted goodness of fit index (AGFI): values equal to or greater than 0.90 indicate a good fit; and (d) the comparative fit index (CFI): values greater than 0.90 indicate a good fit. All these fit indices are based on the published guidelines (e.g. Bentler, 1990; Byrne, 2010). The final model was improved by applying modification indexes. Since the study sample was not large, the model could not be cross-validated.
Figure 2.

Graphic representation of the study hypotheses.
Nevertheless, following the recommendations of several authors (e.g. Byrne, 2010; Hoyle, 2012; Klein, 2013; for a review, see Whittaker, 2012), a sequential modification of the model was conducted based on: (a) the examination of modification index values greater than a χ2 critical value of 3.84 in order to decide whether it would be theoretically plausible to include them in the model and be freely estimated; (b) the expected parameter change in conjunction with the modification indices, which indicates the estimated value of a fixed parameter if it is added to a model and freely estimated; and (c) the repetition of the process until adding any fixed parameters would not significantly reduce the model’s χ2, or until it was no longer theoretically possible to include any of the statistically significant potential respecifications.
All statistical analyses were conducted using the SPSS and AMOS Graphics software packages (version 22.0, SPSS Inc. and Small Waters Corp., Chicago, IL).
3. Results
3.1. Sample characteristics
All study variables in the TE and TE with PTSS groups were normally distributed. In the TE group, the skewness and kurtosis values ranged from −.54 to 2.65 and from .32 to 2.75, respectively. In the TE with PTSS group, the skewness and kurtosis values ranged from −.39 to 2.18 and from .07 to 2.50, respectively. None of the variables had problems associated with homoscedasticity or multicollinearity.
The mean ages of the TE and TE with PTSS groups were 52.11 years (SD = 9.98) and 51.14 years (SD = 8.45), respectively. This difference was nonsignificant [t (384) = 1.04, p = .301]. Mean pain duration in the TE and TE with PTSS groups was 10.94 years (SD = 9.82) and 12.23 years (SD = 9.80), respectively. This difference was also nonsignificant [t (377) = −1.28, p = .377]. The average number of traumas in the TE and TE with PTSS groups was 3.85 (SD = 2.14) and 4.74 (SD = 2.06), respectively. This difference was statistically significant [t (385) = −4.37, p < .01]. The TE and TE with PTSS groups differed by pain diagnosis. The most common diagnoses in the TE and TE with PTSS group were generalized pain (63.4%) and spinal pain (44.33%), respectively. This difference reached statistical significance [x2 (3, n = 388) = 42.07, p < .01]. No significant differences were found between men and women in both groups in the BIS, BAS, EA, PTSS, perceived pain, functioning and impairment. Because there were significant differences between groups in the number of traumas and in pain diagnosis, both variables were considered as covariates in the analyses. Table 1 shows the demographic and clinical characteristics of the two groups of participants.
Table 1.
Demographic and clinical characteristics of the two groups of participants.
| TE |
TE with PTSS |
||||
|---|---|---|---|---|---|
| Variables | N | % | N | % | x2 |
| Marital status | 3.49 | ||||
| Single | 18 | 9.28 | 19 | 9.79 | |
| Married | 142 | 73.20 | 128 | 65.98 | |
| Divorced | 25 | 12.88 | 38 | 19.59 | |
| Widowed | 9 | 4.64 | 9 | 4.64 | |
| Highest level of education+ | 6.54 | ||||
| Without education | 30 | 15.46 | 33 | 17.01 | |
| Primary education | 66 | 34.02 | 86 | 44.33 | |
| Secondary education | 69 | 35.57 | 58 | 29.90 | |
| University education | 27 | 13.92 | 16 | 8.25 | |
| Pain diagnostic | 42.07* | ||||
| Generalized pain | 60 | 30.93 | 123 | 63.40 | |
| Spinal pain | 86 | 44.33 | 51 | 26.29 | |
| Limbs pain | 47 | 24.23 | 20 | 10.31 | |
| Others | 1 | 0.51 | 0 | 0 | |
| Trauma events | |||||
| Natural disasters | 31 | 15.98 | 34 | 17.52 | 0.15 |
| Accidents | 62 | 31.96 | 74 | 38.14 | 1.54 |
| Physical assault | 55 | 28.35 | 109 | 56.18 | 30.37* |
| Witnessed physical assault | 42 | 21.65 | 47 | 24.23 | 0.33 |
| Assault with weapon | 71 | 36.60 | 91 | 46.91 | 4.07** |
| Witnessed assault with weapon | 23 | 11.86 | 25 | 12.89 | 0.08 |
| Sexual assault | 18 | 9.28 | 32 | 16.49 | 4.42** |
| Witnessed sexual assault | 19 | 9.80 | 39 | 20.10 | 7.99** |
| Other uncomfortable sexual experienced | 32 | 16.49 | 52 | 26.80 | 5.95** |
| Combat/war/captivity | 13 | 6.70 | 11 | 5.67 | 0.19 |
| Life-threatening illness or injure | 66 | 34.02 | 82 | 42.27 | 2.66 |
| Life-threatening illness or injure of close person | 149 | 76.80 | 171 | 88.14 | 8.09** |
| Sudden violence/ accidental death | 163 | 84.02 | 162 | 83.50 | .07 |
Note: TE = trauma-exposed; TE with PTSS = trauma-exposed with posttraumatic stress symptoms.
+Missing values in highest level of education (n = 2 in TE, n = 1 in TE with PTSS).
*p < .01; ** = p < .05
3.2. Differences between TE and TE with PTSS groups
Table 2 shows the means and standard deviations of the variables for both groups. Significant differences were found between the TE and TE with PTSS groups in all dependent variables (see Table 3). The only exception was the BAS. The TE with PTSS group had higher mean scores in the BIS, EA and impairment, and lower mean scores in functioning, with large size effects. This group also had a higher mean in pain intensity, but with a small size effect.
Table 2.
Descriptive statistical for both groups of participants.
| TE |
TE with PTSS |
|||
|---|---|---|---|---|
| Variables (range) | Mean | SD | Mean | SD |
| BIS (10–20) | 11.84 | 2.40 | 14.74 | 3.07 |
| BAS (10–20) | 10.93 | 1.50 | 11.15 | 1.78 |
| EA (7–49) | 19.80 | 8.91 | 35.03 | 8.09 |
| Perceived pain (0–10) | 6.06 | 1.43 | 6.90 | 1.40 |
| Functioning (0–120) | 52.11 | 13.26 | 42.65 | 14.70 |
| Impairment (0–30) | 6.77 | 3.22 | 10.47 | 4.40 |
Note: TE = trauma-exposed; TE with PSS = trauma-exposed with posttraumatic stress symptoms; BIS = behavioural inhibition system; BAS = behavioural approach system; EA = experiential avoidance.
Table 3.
Differences between groups (TE and TE with PTSS) in dependent variables.
| Variable | F | df | p | Power | η2p |
|---|---|---|---|---|---|
| BIS | 95.36 | 1/388 | .000 | 1.00 | .20 |
| BAS | 2.15 | 1/388 | .140 | .31 | .01 |
| EA | 261.23 | 1/388 | .000 | 1.00 | .40 |
| Perceived pain | 17.02 | 1/388 | .000 | .99 | .04 |
| Functioning | 50.52 | 1/388 | .000 | 1.00 | .15 |
| Impairment | 76.63 | 1/388 | .000 | 1.00 | .17 |
Note: TE = trauma-exposed; TE with PSS = trauma-exposed with posttraumatic stress symptoms; BIS = behavioural inhibition system; BAS = behavioural approach system; EA = experiential avoidance.
3.3. Evaluation of the measurement and structural models
The initial empirical model (Figure 2) showed a poor fit [χ2 (df = 13, N = 194) = 49.88, p = .000]. We eliminated the nonsignificant paths between the BAS and PTSS (β = 0.05; p = .652), PTSS and perceived pain (β = 0.01; p = .159) and PTSS and functioning (β = −0.19; p = .072). Next, we incorporated the theoretically plausible modifications indexes. Thus, any changes suggested by the modification indices were made if the modification improved the model fit, had a sound theoretical basis and did not result in significant changes to the model’s parameters. Firstly, the paths between the BAS and perceived pain and the BAS and functioning were allowed [χ2 (df = 13, N = 194) = 35.01, p = .001]. Second, a path between EA and perceived pain was also added. We consider that the inclusion of these paths was theoretically justified, given the empirical literature on the relationships between the BAS and pain experience (e.g. Becerra-García & Robles Jurado, 2014; Jensen et al., 2015; Serrano-Ibáñez et al., 2018), and between EA and pain experience (e.g. Costa & Pinto-Gouveia, 2011; Esteve et al., 2012). After these changes, the final model showed a good fit [χ2 (df = 12, N = 194) = 18.88, p = .092; RMSEA = .05; AGFI = .99; CFI = .98] (see Figure 3).
Figure 3.
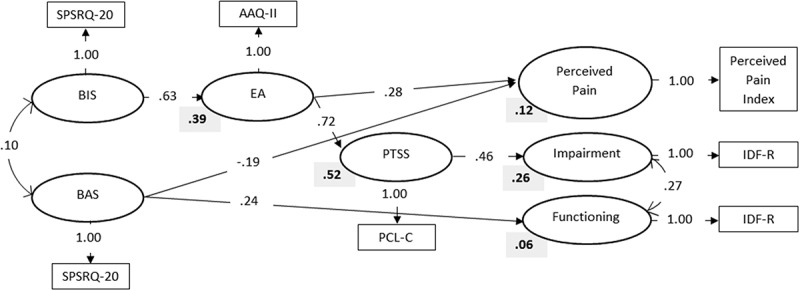
Structure standardized coefficients (in the arrows) and R2 values (bold) for the final model. Observed variables are represented by square and latent variables by circles. SPSRQ-20 = Sensitivity to Punishment and Sensitivity to Reward Questionnaire; AAQ-II = Acceptance and Action Questionnaire-II; PCL-C = Posttraumatic Stress Disorder Checklist-Civilian Version; IDF-R = Impairment and Functioning Inventory Revised.
The BIS had a direct positive path to EA, explaining 39% of the variance of this variable. EA had two statistically significant positive paths coefficients: one to PTSS (explaining 52% of its variance) and one to pain intensity. PTSS had a statistically significant association with impairment, explaining 26% of its variance. Finally, the BAS had a direct path to pain intensity and to functioning. Higher scores on the BAS were associated with lower scores in pain intensity and with higher scores in functioning. EA and the BAS together explained 12% of the variance of pain intensity. The BAS explained 6% of the variance of functioning.
4. Discussion
The aim of the present study was to better understand the role of the BIS, BAS and EA in pain adjustment in patients with comorbid CP and PTSS. These variables have been proposed as vulnerability factors for both disorders. Thus, we first analysed differences between patients with chronic musculoskeletal pain who had experienced a traumatic experience and developed PTSS before the onset of pain, and similar patients who did not develop PTSS. We also analysed differences between groups in their adjustment to CP.
The findings showed that the TE with PTSS group had worse pain adjustment than the TE group. The TE with PTSS group had significantly high levels of perceived pain, more impairment and less functioning. These results are in line with previously studies which found that patients with concurrent TE and PTSS have more pain intensity (Defrin et al., 2008) and lower levels of daily activity. This finding suggests that the development of PTSS would increase the effects of CP (Åkerblom, Perrin, Rivano Fischer, & McCracken, 2017). According to previous studies on EA (Ruiz-Párraga & López-Martínez, 2014, 2015), and as predicted, patients with PTSS had high scores on this variable. Therefore, these patients tend to show increased reluctance to remain in contact with private emotions, sensations, thoughts or memories, and instead direct their behaviour to alter the events that elicit them (Hayes et al., 2006). Furthermore, previous studies on CP patients with and without PTSS (e.g. Costa & Pinto-Gouveia, 2011; Esteve et al., 2012; Mehta et al., 2016; Ruiz-Párraga & López-Martínez, 2015) have found that EA is associated with higher levels of pain. This result supports the notion that avoiding private unpleasant events not only exacerbates trauma symptoms but also exacerbates the pain experience, thus leading to worse adjustment to pain.
SEM analysis found that EA mediated the association between the BIS and PTSS. This finding supports previous studies (Maack et al., 2012; Pickett et al., 2011) that found that after trauma exposure individuals with increased BIS sensitivity may evaluate stimuli associated with their traumatic event as threatening, thus motivating the avoidance of internal or external experiences associated with the traumatic event.
In contrast with the results of Ruiz-Párraga and López-Martínez (2014), PTSS was not associated with perceived pain or daily functioning in the final model. An explanation for this result could be that in their study perceived pain, impairment and functioning were considered as composite measures of a latent variable called pain adjustment, whereas in the present study these variables were analysed separately. This speculation merits future empirical research. However, as predicted, PTSS was associated with impairment, explaining 26% of this variable. A sizeable empirical literature has accumulated in support of this result (e.g. Asmundson, Gomez-Perez, & Fetzner, 2014).
As hypothesized, the results show that the TE with PTSS group had significantly higher BIS scores than the TE group, which result is in line with those of previous studies (Contractor et al., 2013; Myers et al., 2012). Furthermore, some longitudinal studies have demonstrated that baseline levels of the BIS increase the risk of PTSD development (Gudiño, 2013; Gudiño et al., 2012). Our findings support conceptual models that have attempted to explain comorbid PTSD and CP. Thus, according to the shared vulnerability model (Asmundson, Coons, Taylor, & Katz, 2002), certain individual characteristics that are partially genetically determined are common predisposing factors for both PTSD and pain disorders. In this respect, the BIS has been postulated as a neuropsychological system of defensive motivation that mediates a range of attentional and action reflexes, which presumably evolved from primitive withdrawal tendencies (Balconi, Brambilla, & Falbo, 2009). Given that the BIS is thought to regulate aversive motivation and that its activation is associated with negative valence (i.e. fear or anxiety), increased BIS has been associated with attentional bias for affective negative events that may be potentially threatening to individual safety (Everhart & Harrison, 2000). In addition, a significant positive association has been found between high BIS functioning and negative emotional experiences and negative affect (Carver & White, 1994).
BIS sensitivity has been conceptualized as a vulnerability factor for psychopathology. Thus, Maack et al. (2012) postulated that the relationship between the BIS and PTSD is likely not direct and that EA may mediate the association between the BIS and PTSD, given that the BIS is associated with withdrawal and avoidance behaviours. These suggestions are supported by the measurement model because higher scores on the BIS were associated with higher scores on EA, which were associated with increased levels of PTSS. Taking these results into account, as well as the differences between the TE and TE with PTSS groups, the findings of the present study provide partial and indirect support for the shared vulnerability model (Asmundson et al., 2002).
Regarding the BAS, no study could be found that investigated the BAS in patients with CP and PTSS. No significant differences were found between the TE and TE with PTSS groups in the BAS; thus, the results of the present study suggest that PTSS is not associated with this system in patients with CP. Previous research has suggested that the increased impulsive behaviour characteristic of PTSD can be explained by emotional dysregulation, which may lead to reward-approach behaviour (i.e. impulsive risk-seeking behaviour) as a strategy to alleviate or avoid negative emotions (Contractor et al., 2013; Pickett et al., 2011). However, the results of the present study do not support this hypothesis.
Against our predictions, the BAS was not associated with EA. Nevertheless, this result is consistent with those of Maack et al. (2012), who found no association between the BAS or its dimensions (i.e. responsiveness, fun-seeking and drive) and EA in a sample of undergraduates. Similarly, Pickett et al. (2011) did not find a significant positive association between EA and BAS-reward responsiveness in a sample of college students, although a significant positive association was found between EA and BAS-fun seeking. According to these authors, this result suggests that BAS-fun seeking could be associated with emotion regulation difficulties. It is noteworthy that both of these studies used the BIS/BAS Scales (Carver & White, 1994), whereas the present study used the short form of SPSRQ, which includes only two dimensions (sensitivity to punishment and sensitivity to reward functioning). In fact, it may be the case that the BAS is a multidimensional construct that cannot be adequately represented using a unidimensional scale such as sensitivity to reward (Contractor et al., 2013).
A positive association was found between the BAS and functioning and a negative association between the BAS and perceived pain. Sava and Sperneac (2006) suggested that the SPSRQ punishment and reward scales seem to be more closely associated with the concepts of impulsivity than the BIS/BAS Scales. Given that the BAS regulates appetitive motivation, it is associated with sensitivity to positive affect and approach behaviour, and thus when this system is activated it causes movement toward goals and increases motor activity (Maack et al., 2012). In fact, impulsivity has been associated with the BAS (e.g. Aluja & Blanch, 2011), which finding could provide a potential explanation of our results. The empirical model found a significant positive association between this system and daily functioning, thus supporting the postulates of Maack et al. (2012). In addition, previous research (e.g. Esteve et al., 2017) has found that patients with CP with high levels of task-contingent persistence and daily functioning reported the lowest levels of pain. Therefore, it is not surprising that the BAS involves increased activity and performance, which is associated with decreased pain perception. Nevertheless, more empirical attention is needed in this regard.
Our findings shed some light on the role of the BIS in particular and the BAS in relation to the variables that explain adjustment to CP in patients with comorbid CP and PTSS. In summary, the results suggest that after exposure to trauma, individuals with increased BIS sensitivity may evaluate the stimuli associated with their traumatic event as threatening, thus motivating the avoidance of internal (i.e. EA) and external experiences associated with trauma. This behaviour may then interfere with the processing of feared stimuli and emotions, ultimately increasing the risk of the development and maintenance of PTSD. This line of reasoning could be extrapolated to people with CP, as pain could also increase BIS activation in particularly sensitive individuals, who could have a greater disposition to develop PTSS. The appearance of these symptoms might lead to a worst pain adjustment (i.e. increased pain intensity, decreased daily functioning and higher pain-related impairment), as has been already shown (e.g. Ruiz-Párraga & López-Martínez, 2015).
If corroborated by future studies, these results could help inform the development of psychological treatments to reduce BIS activation, which could consequently decrease EA. This decrease would be expected to reduce PTSS and impairment. Although the role of the BAS remains uncertain, an increase its activity could be beneficial because it has been shown to be associated with decreased levels of self-reported pain and increased daily functioning. In this respect, Jensen et al. (2016) proposed that both Acceptance and Commitment Therapy (ACT) would be expected to influence BIS and BAS activity, while also contributing to reduce levels of EA. ACT would focus on psychological flexibility and on increasing valued activities associated with positive meaning and roles (Jensen et al., 2016). In addition, ACT has been considered as a behaviour therapy approach directed to weakening EA (Hayes et al., 2004). On the other hand, Cognitive Therapy would include components that would encourage patients to take a detached stance toward their thoughts. Jensen et al. (2016) also suggested that Cognitive Therapy could be viewed as a treatment that can decrease BIS activity or make it less likely that pain activates the BIS, given that this therapy is focused on reducing maladaptive cognitions. Likewise, some cognitive behavioural therapies for pain that target activity level (i.e. behavioural activation) may achieve their primary beneficial effects by increasing BAS activity.
We could locate no study that investigated all these variables simultaneously in patients with CP and PTSS. For this reason, the results of our study are limited in some ways that may provide directions for future research. Firstly, although the participants in the TE with PTSS group were selected according to the cutoff point established for pain patients by the authors of the PCL-C, the sample could not fulfil the DSM-5 criteria for PTSD (American Psychiatric Association, 2013). Secondly, the number of traumas experienced by the participants was the only covariate considered in the analyses. Although polytraumatization has been particularly associated with interpersonal traumas and has been claimed to be a relevant and specific factor in highly-traumatized individuals (Contractor, Caldas, Fletcher, Shea, & Armour, 2018), it would also have been of interest to have used the type of trauma experienced as a covariate. However, the study participants were not selected on the basis of the type of trauma experienced, and so they could have been exposed to several different types of traumatic events (i.e. interpersonal or noninterpersonal). Thirdly, this study did not include a group of participants with CP who had not experienced trauma. However, this group could differ from the study groups in terms of the BIS, BAS, EA and pain-related variables, and thus future research could include this subsample, thereby gaining a better understanding of the role of trauma in this field of study. Fourthly, self-report measures were used for data collection and the design was cross-sectional; thus, it was not possible to determine a cause-and-effect direction between the variables of interest. Fifthly, the BAS was measured using the only instrument with adequate psychometric properties for the Spanish population (SPSRQ-20); however, this instrument does not distinguish between dimensions of the BAS. Therefore, it was not possible to investigate differences between groups and associations between variables in relation to the dimensions of the BAS. Given that the present study represents a novel line of research, more studies are needed to be able to draw clear conclusions on this topic. Finally, the empirical model should be cross-validated to provide more support for its re-specified structure because we have applied several modifications to the hypothetical model.
Despite these limitations, the present study found differences between CP patients with and without PTSS in dispositional variables (the BIS and EA), thus providing a preliminary comprehensive framework for understanding the co-occurrence of both disorders. Although these findings represent new and relevant information, more research is needed given the incipient character of research in this field.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Åkerblom S., Perrin S., Rivano Fischer M., & McCracken L. M. (2017). The Impact of PTSD on Functioning in Patients Seeking Treatment for Chronic Pain and Validation of the Posttraumatic Diagnostic Scale. International Journal of Behavioral Medicine, 24(2), 249–13. doi: 10.1007/s12529-017-9641-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aluja A., & Blanch A. (2011). Neuropsychological behavioral inhibition system (BIS) and behavioral approach system (BAS) assessment: A shortened sensitivity to punishment and sensitivity to reward questionnaire version (SPSRQ-20). Journal of Personality Assessment, 93(6), 628–636. doi: 10.1080/00223891.2011.608760 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, DSM-5 Task Force (2013). Diagnostic and statistical manual of mental disorders: DSM-5™ (5th ed.). Arlington, VA: American Psychiatric Publishing, Inc. doi: 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Arendt-Nielsen L., Morlion B., Perrot S., Dahan A., Dickenson A., Kress H. G., … Mohr Drewes A. (2018). Assessment and manifestation of central sensitisation across different chronic pain conditions. European Journal of Pain (United Kingdom), 22(2), 216–241. doi: 10.1002/ejp.1140 [DOI] [PubMed] [Google Scholar]
- Asmundson G. J. G., Coons M. J., Taylor S., & Katz J. (2002). PTSD and the experience of pain: Research and clinical implications of shared vulnerability and mutual maintenance models. Canadian Journal of Psychiatry, 47(10), 930–937. doi: 10.1177/070674370204701004 [DOI] [PubMed] [Google Scholar]
- Asmundson G. J. G., Gomez-Perez L., & Fetzner M. (2014). Posttraumatic stress disorder and chronic pain In Feeny N. & Zoellner L. (Eds.), Facilitating resilience and recovery following traumatic events (pp. 265–290). New York: Guilford. [Google Scholar]
- Balconi M., Brambilla E., & Falbo L. (2009). BIS/BAS, cortical oscillations and coherence in response to emotional cues. Brain Research Bulletin, 80(3), 151–157. doi: 10.1016/j.brainresbull.2009.07.001 [DOI] [PubMed] [Google Scholar]
- Becerra-García J. A., & Robles Jurado M. J. (2014). Behavioral approach system activity and self-reported somatic symptoms in fibromyalgia: An exploratory study. International Journal of Rheumatic Diseases, 17(1), 89–92. doi: 10.1111/1756-185X.12034 [DOI] [PubMed] [Google Scholar]
- Bentler P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. doi: 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Byrne B. (2010). Structural equation modelling with AMOS. Londres: L.E.A. [Google Scholar]
- Carver C. S., & White T. L. (1994). Behavioral Inhibition, Behavioral Activation, and Affective Responses to Impending Reward and Punishment: The BIS/BAS Scales. Journal of Personality and Social Psychology, 67(2), 319–333. doi: 10.1037/0022-3514.67.2.319 [DOI] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Earlbaum Associates. [Google Scholar]
- Contractor A. A., Caldas S., Fletcher S., Shea M. T., & Armour C. (2018). Empirically derived lifespan polytraumatization typologies: A systematic review. Journal of Clinical Psychology, 74(7), 1137–1159. doi: 10.1002/jclp.22586 [DOI] [PubMed] [Google Scholar]
- Contractor A. A., Elhai J. D., Ractliffe K. C., & Forbes D. (2013). PTSD’s underlying symptom dimensions and relations with behavioral inhibition and activation. Journal of Anxiety Disorders, 27(7), 645–651. doi: 10.1016/j.janxdis.2013.07.007 [DOI] [PubMed] [Google Scholar]
- Corr P. J. (2009). The reinforcement sensitivity theory of personality In P. J. Corr & G. Matthews (Eds.), The Cambridge handbook of personality psychology (pp. 347–376). Cambridge: Cambridge University Press. [Google Scholar]
- Corr P.J. (2002). J.A. Gray’s reinforcement sensitivity theory: tests of the joint subsystems hypothesis of anxiety and impulsivity. Personality and Individual Differences, 33, 511-532. doi: 10.1016/S0191-8869(01)00170-2 [DOI] [Google Scholar]
- Costa J., & Pinto-Gouveia J. (2011). The mediation effect of experiential avoidance between coping and psychopathology in chronic pain. Clinical Psychology and Psychotherapy, 18(1), 34–47. doi: 10.1002/cpp.699 [DOI] [PubMed] [Google Scholar]
- Defrin R., Ginzburg K., Solomon Z., Polad E., Bloch M., Govezensky M., & Schreiber S. (2008). Quantitative testing of pain perception in subjects with PTSD - Implications for the mechanism of the coexistence between PTSD and chronic pain. Pain, 138(2), 450–459. doi: 10.1016/j.pain.2008.05.006 [DOI] [PubMed] [Google Scholar]
- Defrin R., Schreiber S., & Ginzburg K. (2015). Paradoxical Pain Perception in Posttraumatic Stress Disorder: The Unique Role of Anxiety and Dissociation. Journal of Pain, 16(10), 961–970. doi: 10.1016/j.jpain.2015.06.010 [DOI] [PubMed] [Google Scholar]
- Elman I., Lowen S., Frederick B. B., Chi W., Becerra L., & Pitman R. K. (2009). Functional Neuroimaging of Reward Circuitry Responsivity to Monetary Gains and Losses in Posttraumatic Stress Disorder. Biological Psychiatry, 66(12), 1083–1090. doi: 10.1016/j.biopsych.2009.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elvemo N., Landrø N. I., Borchgrevink P. C., & Haberg A. K. (2015). Reward responsiveness in patients with chronic pain. European Journal of Pain, 19(10), 1537–1543. doi: 10.1002/ejp.687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esteve R., López-Martínez A. E., Peters M. L., Serrano-Ibáñez E. R., Ruíz-Párraga G. T., González-Gómez H., & Ramírez-Maestre C. (2017). Activity Pattern Profiles: Relationship With Affect, Daily Functioning, Impairment, and Variables Related to Life Goals. Journal of Pain, 18(5), 546–555. doi: 10.1016/j.jpain.2016.12.013 [DOI] [PubMed] [Google Scholar]
- Esteve R., Ramírez-Maestre C., & López-Martínez A. E. (2012). Experiential avoidance and anxiety sensitivity as dispositional variables and their relationship to the adjustment to chronic pain. European Journal of Pain, 16(5), 718–726. doi: 10.1002/j.1532-2149.2011.00035.x [DOI] [PubMed] [Google Scholar]
- Everhart D. E., & Harrison D. W. (2000). Facial affect perception in anxious and nonanxious men without depression. Psychobiology, 28(1), 90–98. [Google Scholar]
- Fleming K. C., & Volcheck M. M. (2015). Central Sensitization Syndrome and the Initial Evaluation of a Patient with Fibromyalgia: A Review. Rambam Maimonides Medical Journal, 6(2), e0020. doi: 10.5041/RMMJ.10204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray J. A. (1987a). The psychology of fear and stress. Londres: Cambridge University Press. [Google Scholar]
- Gray J. A. (1987b). The neuropsychology of emotion and personality In Stahl S. M., Iversen S. D., & Goodman E. C. (Eds.), Cognitive Neurochemistry (pp. 171–190). Oxford: Oxford University Press. [Google Scholar]
- Gray J. A., & McNaughton N. (2000). The neuropsychology of anxiety: an enquiry into the functions of the septo-hippocampal system. Oxford: Oxford University Press. [Google Scholar]
- Gray M. J., Litz B. T., Hsu J. L., & Lombardo T. W. (2004). Psychometric properties of the life events checklist. Assessment, 11(4), 330–341. doi: 10.1177/1073191104269954 [DOI] [PubMed] [Google Scholar]
- Gudiño O. G. (2013). Behavioral inhibition and risk for posttraumatic stress symptoms in Latino children exposed to violence. Journal of Abnormal Child Psychology, 41(6), 983–992. doi: 10.1007/s10802-013-9731-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudiño O. G., Nadeem E., Kataoka S. H., & Lau A. S. (2012). Reinforcement sensitivity and risk for psychopathology following exposure to violence: A vulnerability-specificity model in latino youth. Child Psychiatry and Human Development, 43(2), 306–321. doi: 10.1007/s10578-011-0266-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra de Hoyos J. A., Cabeza R., Cáliz R. A., Domínguez J. C., García I., Lubian M., & Sanz R. (2007). Proceso Asistencial Integrado del dolor crónico no oncológico. Sevilla: Junta de Andalucía: Consejería de Igualdad Salud y Políticas Sociales. [Google Scholar]
- Hamilton N. A., Karoly P., & Kitzman H. (2004). Self-Regulation and Chronic Pain: The Role of Emotion. Cognitive Therapy & Research, 28(5), 559–576. [Google Scholar]
- Hayes S. C., Luoma J. B., Bond F. W., Masuda A., & Lillis J. (2006). Acceptance and Commitment Therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. doi: 10.1016/j.brat.2005.06.006 [DOI] [PubMed] [Google Scholar]
- Hayes S. C., Strosahl K. D., Wilson K. G., Bissett R. T., Pistorello J., Toarmino D., … Mccurry S. M. (2004). Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record, 54, 553–578. [Google Scholar]
- Hoyle R. H. (2012). Handbook of structural equation modeling. New York: Guildford Press. [Google Scholar]
- Jensen M. P., Ehde D. M., & Day M. A. (2016). The Behavioral Activation and Inhibition Systems: Implications for Understanding and Treating Chronic Pain. Journal of Pain, 17(5), 529.e1-529.e18. doi: 10.1016/j.jpain.2016.02.001 [DOI] [PubMed] [Google Scholar]
- Jensen M. P., Solé E., Castarlenas E., Racine M., Roy R., Miró J., & Cane D. (2017). Behavioral inhibition, maladaptive pain cognitions, and function in patients with chronic pain. Scandinavian Journal of Pain, 17, 41–48. doi: 10.1016/j.sjpain.2017.07.002 [DOI] [PubMed] [Google Scholar]
- Jensen M. P., Tan G., & Chua S. M. (2015). Pain intensity, headache frequency, and the behavioral activation and inhibition systems. Clinical Journal of Pain, 31(12), 1068–1074. doi: 10.1097/AJP.0000000000000215 [DOI] [PubMed] [Google Scholar]
- Jensen M. P., Turner J. A., Romano J. M., & Fisher L. D. (1999). Comparative Reliability and Valididty of Chronic Pain Intensity measures. Pain, 83, 157–162. [DOI] [PubMed] [Google Scholar]
- Klein R. B. (2013). Principles and practice of structural equation modeling (3rd ed.). New York: Guildford Press. [Google Scholar]
- Kline R. B. (2005). Principles and practice of structural equation modelling. New York: Guilford Press. [Google Scholar]
- Maack D. J., Tull M. T., & Gratz K. L. (2012). Experiential avoidance mediates the association between behavioral inhibition and posttraumatic stress disorder. Cognitive Therapy and Research, 36(4), 407–416. doi: 10.1007/s10608-011-9362-2 [DOI] [Google Scholar]
- Marx B. P., & Sloan D. M. (2005). Peritraumatic dissociation and experiential avoidance as predictors of posttraumatic stress symptomatology. Behaviour Research and Therapy, 43(5), 569–583. doi: 10.1016/j.brat.2004.04.004 [DOI] [PubMed] [Google Scholar]
- McNaughton N., & Corr P. J. (2008). The neuropsychology of fear and anxiety: A foundation for Reinforcement Sensitivity Theory In Corr P. J. (Ed.), The reinforcement sensitivity theory of personality (pp. 44–94). New York, NY: Cambridge University Press. doi: 10.1017/CBO9780511819384.003 [DOI] [Google Scholar]
- Mehta S., Rice D., Janzen S., Serrato J., Getty H., Shapiro A. P., … Teasell R. W. (2016). The long term role of Anxiety sensitivity and experiential avoidance on pain intensity, mood, and disability among Individuals in a specialist pain clinic. Pain Research and Management, 2016. doi: 10.1155/2016/6954896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles J. N. V., Marshall G. N., & Schell T. L. (2008). Spanish and English versions of the PTSD Checklist–Civilian version (PCL-C): Testing for differential item functioning. Journal of Traumatic Stress, 21, 369–376. doi: 10.1002/jts.20349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P., Meesters C., Van den Hout A., Wessels S., Franken I., & Rassin E (2007). Personality and temperament correlates of pain catastrophizing in young adolescents. Child Psychiatry & Human Development, 38, 171–181. doi: 10.1007/s10578-007-0054-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers C. E., VanMeenen K. M., & Servatius R. J. (2012). Behavioral inhibition and PTSD symptoms in veterans. Psychiatry Research, 196(2–3), 271–276. doi: 10.1016/j.psychres.2011.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlando M., & Marshall G. N. (2002). Differential item functioning in a Spanish translation of the PTSD checklist: detection and evaluation of impact. Psychological Assessment, 14(1), 50–59. doi: 10.1037//1040-3590.14.1.50 [DOI] [PubMed] [Google Scholar]
- Pickett S. M., Bardeen J. R., & Orcutt H. K. (2011). Experiential avoidance as a moderator of the relationship between behavioral inhibition system sensitivity and posttraumatic stress symptoms. Journal of Anxiety Disorders, 25(8), 1038–1045. doi: 10.1016/j.janxdis.2011.06.013 [DOI] [PubMed] [Google Scholar]
- Ramírez-Maestre C., & Esteve R. (2015). A New Version of the Impairment and Functioning Inventory for Patients With Chronic Pain (IFI-R). PM and R, 7(5), 455–465. doi: 10.1016/j.pmrj.2014.11.013 [DOI] [PubMed] [Google Scholar]
- Ruiz F. J., Langer Herrera A. I., Luciano C., Cangas A. J., & Beltrán I. (2013). Midiendo la evitación experiencial y la inflexibilidad psicológica: Versión española del cuestionario de aceptación y acción - II. Psicothema, 25(1), 123–129. doi: 10.7334/psicothema2011.239 [DOI] [PubMed] [Google Scholar]
- Ruiz-Párraga G. T., & López-Martínez A. E. (2014). The contribution of posttraumatic stress symptoms to chronic pain adjustment. Health Psychology, 33(9), 958–967. doi: 10.1037/hea0000040 [DOI] [PubMed] [Google Scholar]
- Ruiz-Párraga G. T., & López-Martínez A. E. (2015). The Role of Experiential Avoidance, Resilience and Pain Acceptance in the Adjustment of Chronic Back Pain Patients Who Have Experienced a Traumatic Event: A Path Analysis. Annals of Behavioral Medicine, 49(2), 247–257. doi: 10.1007/s12160-014-9654-3 [DOI] [PubMed] [Google Scholar]
- Salamone J. D., & Correa M. (2012). The mysterious motivational functions of mesolimbic dopamine. Neuron, 76(3), 470–485. doi: 10.1016/j.neuron.2012.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sava F. A., & Sperneac A. M. (2006). Sensitivity to reward and sensitivity to punishment rating scales: A validation study on the Romanian population. Personality and Individual Differences, 41(8), 1445–1456. doi: 10.1016/j.paid.2006.04.024 [DOI] [Google Scholar]
- Serrano-Ibáñez E. R., López-Martínez A. E., Ramírez-Maestrea C., Esteve R., & Jensen M. P. (2019). The behavioral inhibition and activation systems and function in patients with chronic pain. Personality and Individual Differences, 138, 56–62. doi: 10.1016/j.paid.2018.09.021 [DOI] [Google Scholar]
- Serrano-Ibáñez E. R., Ramírez-Maestre C., López-Martínez A. E., Esteve R., Ruiz-Párraga G. T., & Jensen M. P (2018). Behavioral inhibition and activation systems, and emotional regulation in individuals with chronic musculoskeletal pain. Frontiers in Psychiatry, 9, 1–10. doi: 10.3389/fpsyt.2018.00394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serrano-Ibáñez E. R., Ramírez-Maestre C., López-Martínez A. E., Esteve R., Ruiz-Párraga G. T., & Jensen M. P. (2018). Behavioral Inhibition and Activation Systems, and Emotional Regulation in Individuals with Chronic Musculoskeletal Pain. Frontiers in Psychiatry, 9, 1–10. doi: 10.3389/fpsyt.2018.00394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepherd L., & Wild J. (2014). Emotion regulation, physiological arousal and PTSD symptoms in trauma-exposed individuals. Journal of Behavior Therapy and Experimental Psychiatry, 45(3), 360–367. doi: 10.1016/j.jbtep.2014.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman J. J., Carlson C., Wilson J. F., Okeson J., & McCubbin J. A. (2005). Posttraumatic stress disorder among patients with orofacial pain. Journal of Orofacial Pain, 19(4), 309–317. doi: 10.1016/j.prosdent.2006.05.019 [DOI] [PubMed] [Google Scholar]
- Siqveland J., Hussain A., Lindstrøm J. C., Ruud T., & Hauff E. (2017). Prevalence of posttraumatic stress disorder in persons with chronic pain: A meta-analysis. Frontiers in Psychiatry, 8. doi: 10.3389/fpsyt.2017.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smillie L. D., Pickering A. D., & Jackson C. J. (2006). The new Reinforcement Sensitivity Theory: implications for psychometric measurement. Personality and Social Psychology Review, 10(4), 320–335. doi: 10.1207/s15327957pspr1004 [DOI] [PubMed] [Google Scholar]
- Stein M. B., & Paulus M. P. (2009). Imbalance of Approach and Avoidance: The Yin and Yang of Anxiety Disorders. Biological Psychiatry, 66(12), 1072–1074. doi: 10.1016/j.biopsych.2009.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull M. T., Gratz K. L., Latzman R. D., Kimbrel N. A., & Lejuez C. W. (2010). Reinforcement Sensitivity Theory and emotion regulation difficulties: A multimodal investigation. Personality and Individual Differences, 49(8), 989–994. doi: 10.1016/j.paid.2010.08.010 [DOI] [Google Scholar]
- Whittaker T. A. (2012). Using the modification index and standardized expected parameter change for model modification. The Journal of Experimental Education, 80, 26–44. doi: 10.1080/00220973.2010.531299 [DOI] [Google Scholar]


