Abstract
BACKGROUND:
The association between migraine headache and cardiovascular events has been inconsistent. This study determines the long-term risk of cardiovascular events among women with and without a history of migraine headache who were under evaluation for suspected myocardial ischemia in the Women’s Ischemia Syndrome Evaluation (WISE).
METHODS:
The WISE is a National Heart, Lung and Blood Institute-sponsored prospective, multicenter study that aims to improve myocardial ischemia evaluation in women. A total of 936 women presenting with symptoms of myocardial ischemia underwent structured data collection and coronary angiography. Information pertaining to migraine headache was available in 917 women. All-cause mortality data were available on all women for a median of 9.5 years, and nonfatal cardiovascular event data were available on 888 women for a median of 6.5 years.
RESULTS:
A total of 224 (24.4%) women reported a history of migraine headache. Compared with women who did not report a history of migraine headache, women with a history of migraine headache had an increased adjusted risk of cardiovascular event (cardiovascular death, nonfatal myocardial infarction, heart failure, or stroke) (hazard ratio 1.83; 95% confidence interval, 1.22-2.75) at a median follow-up of 6.5 years. This result was driven mainly by a twofold increase in the risk of stroke (hazard ratio 2.33; 95% confidence interval, 1.16-4.68).
CONCLUSION:
Among women being evaluated for ischemic heart disease, those reporting a history of migraine headache had increased risk of future cardiovascular events on long-term follow-up. This risk was primarily driven by a more-than twofold increase in the risk of stroke.
Keywords: Cardiovascular disease, Migraine, Mortality, Stroke, Women
Migraine headache is a common disorder affecting 14.2% of the US population, with a higher prevalence among women.1 The prevalence is highest (23.5%) in women aged 18 to 44 years. In recent years, several studies have evaluated the association between migraine headache and cardiovascular outcomes, with inconsistent results.2-5 A recent report from the Nurses’ Health Study II participants showed an increased risk of major cardiovascular disease, myocardial infarction, stroke, and angina/coronary revascularization among women with a history of migraine headache at long-term follow-up of 20 years.5 In contrast, a meta-analysis of 10 cohort studies concluded that migraine headache is not associated with coronary heart disease, cardiovascular disease, or all-cause mortality.2 In the meta-analysis, studies with longer-term follow up (ie, 10, 15.7, and 25.9 years) did show an association with migraine headache and cardiovascular events, whereas studies with shorter-term follow-up (ie, 1.4 and 3 years) did not show an association between migraine headache and cardiovascular events. These inconsistencies could be explained by a time-dependent association between migraine headache and cardiovascular events.
In a prior analysis of the Women’s Ischemia Syndrome Evaluation (WISE) study, we demonstrated that in women presenting with signs and symptoms of myocardial ischemia and undergoing coronary angiography, a history of migraine headache was not associated with increased cardiovascular events at mid-term follow-up of 4.4 years.6 This current analysis was intended to further examine the relationship between migraine headache and longer-term cardiovascular outcomes among women enrolled in the National Heart, Lung, and Blood Institute-sponsored WISE study to further add to the literature of prospective long-term studies evaluating the association between migraine headache and cardiovascular events.
METHODS
The WISE study was a 4-center study that aimed to improve the diagnostic reliability of cardiovascular testing in the evaluation of ischemic heart disease in women. In brief, women with chest pain symptoms or suspected ischemia underwent an initial evaluation that included collection of demographic and symptom data, medical and psychosocial histories, blood sampling, and coronary angiography.7 A total of 936 women underwent a full medical history, physical examination, psychosocial evaluation, coronary artery disease risk-factor assessment, and detailed laboratory evaluation. Of the 936 women, 917 women completed baseline information pertaining to migraine headache, and 888 were prospectively followed for cardiovascular events for a median of 6.5 years.
Cardiac Risk Factors and Coronary Angiography
Cardiac risk assessment was done using a questionnaire administered by study nurses inquiring about history of diabetes, dyslipidemia, hypertension, and family history of coronary artery disease and other cardiac risk factors. The 10-year risk of myocardial infarction was assessed using the Adult Treatment Panel III guidelines.8,9 All coronary angiograms obtained at enrollment were quantitatively and qualitatively evaluated for the presence and extent of coronary artery disease by the WISE angiographic core laboratory as previously described.10 Severe coronary artery disease was defined as ≥50% stenosis in ≥1 epicardial coronary artery. The WISE coronary artery disease severity score was developed with points assigned according to the category of severity of the stenosis (0 to 19, 20 to 49, 50 to 69, 70 to 89, 90 to 98, and 99 to 100), adjusting for partial (any filling of the occluded vessel or its distal branches anterograde or retrograde via channels other than the original lumen) and complete (complete filling of the vessel distal to the occlusion) collaterals. Scores were then adjusted according to the lesion location, with more proximal lesions receiving a higher weighting factor.10
Migraine and Symptom Reporting
Women were asked about a history of migraine headache with possible responses of “yes,” “no,” or “unknown.” Chest pain symptoms were assessed using questions about pain or discomfort above the waist in the last 12 months. The quality of chest pain was further characterized as typical angina, atypical angina, or nonanginal chest pain. Chest pain symptoms were present in 94% of all women. Women were also asked about vasomotor symptoms related to perimenopause and menopause to assess overall symptom-reporting behavior.
Cardiovascular Outcomes
Follow-up was conducted by telephone interview at 6 weeks and annually thereafter. Follow-up consisted of a scripted interview by an experienced nurse or physician. The primary outcome of cardiovascular event was the composite of cardiovascular death, fatal and nonfatal myocardial infarction, congestive heart failure, or stroke. Each patient was asked about occurrence of a cardiovascular event, angina hospitalizations, repeat angiograms, revascularization procedures, or change in symptoms. In addition, we performed secondary analyses of individual endpoints, including angina hospitalization, myocardial infarction, and death. In the event of a death, a death certificate was obtained to ascertain cause of death. In a subset of patients at the University of Florida, patient-reported nonfatal events were confirmed by review of hospital and clinic records and the morbidity data as reported by the women were found to be accurate.
Statistical Analysis
Data are presented as means ± standard deviation for continuous variables and percentages for categorical variables. Differences in continuous baseline characteristics by history of migraine headache were assessed by t tests or Wilcoxon rank-sum tests where appropriate. The chi-squared statistic was computed for categorical comparisons of baseline characteristics by the presence or absence of migraine headache; Fisher’s exact tests were utilized when expected cell counts were <5. Stepwise Cox proportional hazards regression was used to model cardiovascular outcomes as a function of migraine headache and other significant cardiac risk factors including age, race, hypertension, body mass index, history of diabetes, dyslipidemia, tobacco use, family history of coronary artery disease, (log) WISE coronary artery disease severity score, and aspirin use. P values <.05 were considered statistically significant. All analyses were performed using SAS 9.3 software (SAS Institute Inc, Cary, NC).
RESULTS
Among the 917 women who completed the question on migraine headache, 224 reported a history of migraine headache (24.4%). Follow-up data on mortality were available on all women for a median of 9.5 years, and follow-up data on nonfatal events were available on 888 women for a median of 6.5 years.
The mean age of women in the study was 58 years. Compared with women with no migraine headache history, women with migraine headache were younger, were less likely to be postmenopausal, and had lower incomes. They were more likely to have a history of depression and hysterectomy than women without migraine headache. Overall cardiac risk profile differed in the 2 groups; women with migraine headache had lower Adult Treatment Panel III risk scores in comparison with women without migraine headache. Women reporting migraine headache were less likely to be on lipid-lowering medications, aspirin, beta-blockers, and angiotensin-converting enzyme inhibitors, and were more likely to be on antidepressant medications (Table 1).
Table 1.
Baseline Characteristics Among Patients with and Without a History of Migraine Headaches
| Characteristic | History of Migraines n = 224 |
No History of Migraines n = 693 |
Age-Adjusted P-Value |
|---|---|---|---|
| Demographic characteristics | |||
| Age | 54 ± 11 | 59 ± 12 | <.001 |
| Postmenopausal (%) | 68 | 79 | <.001 |
| History of hysterectomy (%) | 63 | 50 | <.001 |
| History of depression (%) | 37 | 20 | <.001 |
| Income >35K (%) | 33 | 41 | .008 |
| Education ≥HS (%) | 77 | 82 | .011 |
| Non-White race (%) | 21 | 18 | .42 |
| CV risk factors | |||
| Diabetes (%) | 19 | 26 | .07 |
| Metabolic syndrome (%) | 38 | 47 | .09 |
| Family history of CAD (%) | 71 | 65 | .17 |
| Dyslipidemia (%) | 49 | 57 | .38 |
| Obese (BMI >30) (%) | 41 | 41 | .71 |
| Current smoker (%) | 24 | 19 | .79 |
| Hypertension (%) | 57 | 59 | .88 |
| Current medication use | |||
| Lipid-lowering meds (%) | 17 | 33 | <.001 |
| ATP III cardiac risk score (median, IQR) | 2.0 (1, 5) | 4.0 (1, 8) | <.001 |
| Antidepressant or other psychotropic meds (%) | 38 | 28 | .016 |
| Beta-blockers (%) | 34 | 41 | .12 |
| Aspirin (%) | 53 | 62 | .21 |
| ACE inhibitors (%) | 24 | 26 | .89 |
ACE = angiotensin-converting enzyme; ATP = adult treatment panel; BMI = body mass index; CAD = coronary artery disease; CV = cardiovascular; HS = high school; IQR = interquartile range.
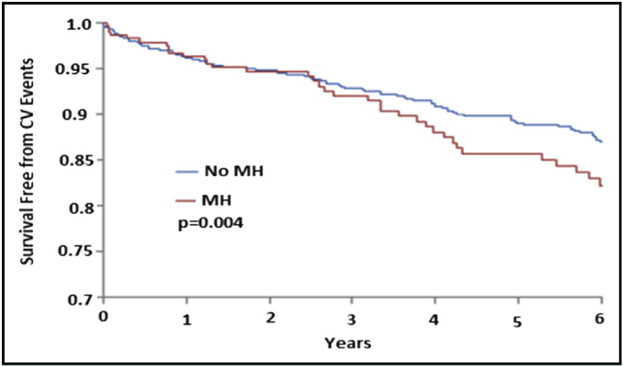
At a median of 9.5 years there were 142 (20.5%) deaths in women with no history of migraine headache and 32 (14.3%) deaths in women with a history of migraine headache. Compared with women with no history of migraine headache, women who reported a history of migraine headache had an increased adjusted hazard ratio (HR) for cardiovascular event (cardiovascular death, nonfatal myocardial infarction, heart failure, or stroke) (HR 1.83; 95% confidence interval [CI], 1.22-2.75) (Table 2). The adjusted HR for individual endpoints of death from all causes, cardiovascular death, nonfatal myocardial infarction, and heart failure did not differ significantly between the 2 groups; however, there was a more-than twofold increase in the incidence of stroke in women with a history of migraine headache (HR 2.33; 95% CI, 1.16-4.68). Cumulative event rates for cardiovascular events over the follow-up period among patients with and without migraine headache are shown in the Figure.
Table 2.
Multivariate Adjusted Hazard Ratios for Vascular Events and All-Cause Death Among Women with Migraine Headache Compared with Those Without Migraine Headache
| Event | Raw Number of Events |
Adjusted* HR (95% CI) |
|
|---|---|---|---|
| No MH (n = 693) |
MH (n = 224) |
n = 917 | |
| CV event | 120 | 41 | 1.83 (1.22-2.75) |
| CV death or MI | 52 | 16 | 1.64 (0.91-2.95) |
| All-cause death or MI | 131 | 30 | 1.25 (0.74-2.11) |
| CV death | 89 | 21 | 1.23 (0.71-2.13) |
| All-cause death | 142 | 32 | 1.11 (0.72-1.71) |
| n = 888 | |||
| Stroke | 28 | 14 | 2.33 (1.16-4.68) |
| HF | 47 | 14 | 1.30 (0.64-2.63) |
| Angina hospitalization | 178 | 68 | 1.21 (0.89-1.64) |
| MI | 23 | 7 | 1.10 (0.40-3.02) |
CI = confidence interval; CV event = CV death, MI, CHF, or stroke; HF = heart failure; HR = hazard ratio; MH = migraine headache; MI = myocardial infarction.
Full model includes: age, race, BMI, history of diabetes, hypertension, dyslipidemia, smoking, family history of coronary artery disease (CAD), (log) WISE CAD severity score and aspirin use.
Figure.
Survival from cardiovascular events (CV) modeled against time in women with and without a history of migraine headache (MH).
DISCUSSION
Our data support the presence of an association between a history of migraine headache and cardiovascular events in a cohort of women with suspected myocardial ischemia at a median follow-up of 6.5 years. This effect was predominately driven by a twofold-increased risk of stroke among women with migraine headache. The risk of all-cause mortality was similar in both groups at a median of 9.5 years of follow-up.
In a previous study, we showed that on mid-term follow-up (4.4 years), there was no notable association between migraine headache and angiographic coronary artery disease or any cardiovascular events.6 Since the publication of the previous study, several studies have evaluated the long-term association between migraine headache and cardiovascular events. Data from 115,541 young women enrolled in the Nurses’ Health Study II study were published recently and showed an increased risk of cardiovascular events in women with a history of migraine headache on 20-year follow-up.5 In this study, 20.7% of the women were diagnosed with migraine headache. Women with migraine headache had a 1.5-fold higher risk of cardiovascular event, including higher risk of myocardial infarction, stroke, angina, or need for revascularization. Furthermore, migraine headache was associated with a higher risk of cardiovascular-related death. Similarly, in another study with extended follow-up of 26 years in an Icelandic population, migraine headache was associated with higher rates of mortality.3 In this study, 15% of the 9681 women were classified as having migraine headache. Women with a history of migraine headache had a 16% increased risk of both all-cause mortality and mortality from cardiovascular disease, and a 14% increased risk of mortality from noncardiovascular disease. These associations were more profound in women who reported a history of migraine headache with aura.
Our current findings add to the growing body of evidence that show an association between migraine headache and long-term cardiovascular events. Our results highlight, in particular, an association between migraine headache and stroke. A history of migraine headache has been more consistently linked with the outcome of ischemic stroke.11-13 Over the past 4 decades, several studies12,14 and 3 meta-analyses2,13,15 have all shown that a history of migraine headache roughly doubles the risk of ischemic stroke. Among prospective studies, the association is strongest among patients with migraine with aura. This risk is amplified in direct proportion to the frequency of migraine attack.16,17 Our findings further strengthen this association in a higher risk cohort of women presenting with signs and symptoms of myocardial ischemia.
Although not statistically significant, it is worth noting that there is an increased risk of all-cause death or myocardial infarction, and cardiovascular death in women with migraine headache on long-term follow-up when compared with our previous study of short-term follow-up. The absence of a statistically significant association with cardiovascular outcomes such as myocardial infarction, heart failure, angina, or death may be due, in part, to inclusion of a broader population of migraine headache patients in our study who were not further characterized to be with or without aura. Migraine headache without aura has not shown as robust an association as the presence of auras for cardiovascular events, even on longer-term follow-up studies.3,4 In addition, the high prevalence of risk factors for ischemia among study participants could, in part, explain the lack of association of migraine headache with other cardiovascular outcomes. Perhaps a more extended follow-up of our cohort would be necessary to see statistically significant associations with other cardiovascular events.
Despite the increasing literature pointing toward an association between migraine headache and cardiovascular events on long-term follow-up, the mechanism of this association remains incompletely understood. Vascular endothelial dysfunction is one proposed mechanism. This has been demonstrated in another analysis of WISE to have an adverse impact on morbidity and mortality in women with chest pain in the setting of nonobstructive coronary artery disease.11 Other proposed mechanisms include the stimulation of inflammatory responses by increased release of prothrombotic and vasoactive factors, patent foramen ovale, and shared genetic markers leading to elevated risks for vascular events seen previously in women with a history of migraine headache.5
Future research should examine the long-term association between migraine headache and cardiovascular events among men who are undergoing evaluation for suspected myocardial ischemia. In addition, in a previous psychosocial study of WISE examining the effects of depression and anxiety symptoms as predictors of cardiovascular disease in 489 women, it was concluded that the value of depression (measured using the Beck Depression Inventory) in predicting cardiovascular disease varied by severity of comorbid anxiety (measured using State-Trait Anxiety Inventory).18 An interesting extension of our research could report on the history of migraine headache among WISE women with comorbid depression and anxiety symptoms and their long-term cardiovascular outcomes. Future research should also focus on further elucidating the mechanism of association between migraine headache and long-term cardiovascular events in women.
Limitations
Our analysis relies on a self-reported history of migraine headache; thus, recall bias could not be excluded. Second, data about the presence or absence of aura are lacking, precluding further stratification based on the presence of aura. Third, although we have performed an adjusted multivariate analysis, other unmeasured confounders could not be entirely excluded. Fourth, data on the duration or severity of migraine headache were not captured. Fifth, data on the type of stroke experienced by the study population were not available. Finally, WISE enrolled women presenting with signs and symptoms of myocardial ischemia who are at higher cardiovascular risk. Our results may not be generalizable to a lower-risk general population.
CONCLUSIONS
Among women presenting with signs and symptoms of ischemia, those reporting a history of migraine headache are at increased risk of cardiovascular events at long-term follow-up. This is mainly driven by a twofold higher risk of stroke among those with migraine. These results suggest that particular attention should be placed on higher-risk women reporting a history of migraine headache for optimization of future cardiovascular risk by intensive secondary prevention.
CLINICAL SIGNIFICANCE.
Women with migraine headache have an 83% increased risk of cardiovascular events on long-term follow-up.
Women with migraine headache have a more-than twofold increase in the risk of stroke when compared with women without a history of migraine headache.
Although not statistically significant, when compared with short-term follow-up, women with migraine headache have an increased risk of myocardial infarction, heart failure hospitalization, and cardiovascular death.
Acknowledgments
Funding: This work was supported by contracts from the National Heart, Lung and Blood Institutes nos. N01-HV-68161, N01-HV-68162, N01-HV-68163, N01-HV-68164, grants U0164829, U01 HL649141, U01 HL649241, K23HL105787, T32HL69751, R01 HL090957, 1R03AG032631 from the National Institute on Aging, GCRC grant MO1-RR00425 from the National Center for Research Resources, the National Center for Advancing Translational Sciences Grant UL1TR000124, and grants from the Gustavus and Louis Pfeiffer Research Foundation, Danville, NJ, The Women’s Guild of Cedars-Sinai Medical Center, Los Angeles, CA, The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, PA, QMED, Inc, Laurence Harbor, NJ, the Edythe L. Broad and the Constance Austin Women’s Heart Research Fellowships, Cedars-Sinai Medical Center, Los Angeles, California, the Barbra Streisand Women’s Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles, The Society for Women’s Health Research (SWHR), Washington, DC, The Linda Joy Pollin Women’s Heart Health Program, and the Erika Glazer Women’s Heart Health Project, and the Adelson Family Foundation, Cedars-Sinai Medical Center, Los Angeles, Calif.
Footnotes
Conflict of Interest: The following authors report that they have no conflicts of interest related to the content of this manuscript: CAR, IYE, BDJ, SER, DVT, BLS, GS, BA. VB reports that she serves on the steering committees for ODYSSEY (Sanofi/Regeneron) and PCSK9 inhibitor trial (Eli Lilly); is an investigator for Pharmacoepidemiology (Amgen); National Coordinator for DalGene (DalCor) and STREMGTH (Astra-Zeneca); site PI for ARTEMIS (Astra-Zeneca) and COMPASS (Bayer); and participates in TNT-related manuscripts (Pfizer), grant proposal review (PackHealth), and the CVD Question Writing Committee for ABIM. CNBM reports the following: Lectures, paid to Cedars Sinai Medical Center (CSMC); Beaumont 7th Annual Heart Disease; C3; European Horizon 2020; Florida Hospital; INOVA; Korean Cardiology Society; 5th Annual Flagstaff Cardiology Symposium; PCP Symposium — Santa Rosa; Practice Point Communication; Pri-Med; Valley Health Grand Rounds; VBWG; University of Colorado; University of Utah; Washington University Grand Rounds; WomenHeart. Consulting, paid to CSMC: Gilead and Medscape. Lectures, paid to CNBM; NIH-CASE grant review study section; Research Triangle Institute (RTI) International. Research funding: WISE HFpEF, RWISE, Microvascular, Normal Control (Cedars); FAMRI (Flight Attendant Medical Research Institute). CJP received funding from grants from the National Institutes of Health-National Heart, Lung, and Blood Institute during the conduct of the study (WISE); unrestricted educational grants to the University of Florida for the Vascular Biology Working Group — Significant: Amarin, AstraZeneca, Baxter, Boehringer Ingelheim, Caladasis, Daiichi Sankyo, Genentech, Sanofi/Aventis; Modest: Amgen, Cytori, Esperion, Gilead, ISIS Pharmaceuticals, Mesoblast, Neostem, Unified Therapeutics.
Authorship: All authors had access to the data and a role in writing the manuscript. This work is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or National Institutes of Health.
References
- 1.Burch RC, Loder S, Loder E. The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies. Headache. 2015;55(1):21–34. [DOI] [PubMed] [Google Scholar]
- 2.Schurks M, Rist PM, Shapiro RE, Kurth T. Migraine and mortality: a systematic review and meta-analysis. Cephalalgia. 2011;31(12):1301–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gudmundsson LS, Scher AI, Aspelund T, et al. Migraine with aura and risk of cardiovascular and all cause mortality in men and women: prospective cohort study. BMJ. 2010;341(10):c3966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurth T, Gaziano M, Cook NR, Logroscino G, Diener HC, Buring JE. Migraine and risk of cardiovascular disease in women. JAMA. 2006;296(3):283–291. [DOI] [PubMed] [Google Scholar]
- 5.Kurth T, Winter AC, Eliassen AH, et al. Migraine and risk of cardiovascular disease in women: prospective cohort study. BMJ. 2016;353:i2610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed B, Bairey Merz CN, McClure C, et al. ; WISE Study Group. Migraines, angiographic coronary artery disease and cardiovascular outcomes in women. Am J Med. 2006;119(8):670–675. [DOI] [PubMed] [Google Scholar]
- 7.Bairey Merz CN, Kelsey SF, Pepine CJ, et al. The Women’s Ischemia Syndrome Evaluation (WISE) study: protocol design, methodology and feasibility report. J Am Coll Cardiol. 1999;33(6):1453–1461. [DOI] [PubMed] [Google Scholar]
- 8.Chambless LE, Folsom AR, Richey Sharrett A, et al. Coronary heart disease risk prediction in the Atherosclerosis Risk in Communities (ARIC) study. J Clin Epidemiol. 2003;56(9):880–890. [DOI] [PubMed] [Google Scholar]
- 9.Folsom AR, Chambless LE, Duncan BB, Gilbert AC, Pankow JS; Atherosclerosis Risk in Communities Study Investigators. Prediction of coronary heart disease in middle-aged adults with diabetes. Diabetes Care. 2003;26(10):2777–2784. [DOI] [PubMed] [Google Scholar]
- 10.Sharaf BL, Pepine CJ, Kerensky RA, et al. Detailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation [WISE] Study Angiographic Core Laboratory). Am J Cardiol. 2001;87(8):937–941. [DOI] [PubMed] [Google Scholar]
- 11.Henrich JB, Horwitz RI. A controlled study of ischemic stroke risk in migraine patients. J Clin Epidemiol. 1989;42(8):773–780. [DOI] [PubMed] [Google Scholar]
- 12.Kurth T, Slomke MA, Kase CS, et al. Migraine, headache, and the risk of stroke in women: a prospective study. Neurology. 2005;64(6):1020–1026. [DOI] [PubMed] [Google Scholar]
- 13.Etminan M, Takkouche B, Isorna FC, Samii A. Risk of ischaemic stroke in people with migraine: systematic review and meta-analysis of observational studies. BMJ. 2005;330(63):7482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stang PE, Carson AP, Rose KM, et al. Headache, cerebrovascular symptoms, and stroke: the Atherosclerosis Risk in Communities Study. Neurology. 2005;64(9):1573–1577. [DOI] [PubMed] [Google Scholar]
- 15.Spector JT, Khan SR, Jones MR, Jayakumar M, Dalal D, Nazarian S. Migraine headache and ischemic stroke risk: an updated meta-analysis. Am J Med. 2010;123(7):612–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kurth T, Schurks M, Logroscino G, Buring JE. Migraine frequency and risk of cardiovascular disease in women. Neurology. 2009;73(8):581–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donaghy M, Chang C, Poulter N; European Collaborators of the World Health Organisation Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Duration, frequency, recency, and type of migraine and the risk of ischaemic stroke in women of childbearing age. J Neurol Neurosurg Psychiatry. 2002;73(6):747–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rutledge T, Linke SE, Krantz DS, et al. Comorbid depression and anxiety symptoms as predictors of cardiovascular events: Results from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study. Psychosom Med. 2009;71(9):958–964. [DOI] [PMC free article] [PubMed] [Google Scholar]