Abstract
Background
Patient reminders are recommended to increase vaccination rates. The objectives of this study were to estimate the percentage of children 6 months–17 years for whom a patient reminder for influenza vaccination was received by a child’s parent or guardian, estimate influenza vaccination coverage by receipt of a patient reminder, and identify factors associated with receipt of a patient reminder.
Methods
National Immunization Survey-Flu (NIS-Flu) data for the 2013–14 influenza season were analyzed. Tests of association between patient reminders and demographic characteristics were conducted using Wald chi-square tests and pairwise comparison t-tests. Multivariable logistic regression was used to determine variables independently associated with receiving a patient reminder.
Results
Approximately 22% of children had a parent or guardian report receiving a patient reminder for influenza vaccination for their child, ranging from 12.9% in Idaho to 41.2% in Mississippi. Children with a patient reminder were more likely to be vaccinated compared with children without a patient reminder (73.7% versus 55.5%). In the multivariable model, reminder receipt was higher for children 6–23 months compared with children 13–17 years, black children compared with white children, and children whose parent completed the survey in English compared with children whose parent completed the survey in a language other than English or Spanish.
Conclusions
Although patient reminders are associated with a higher likelihood of influenza vaccination, nationally, less than one-fourth of children had a parent report receiving one. Although based on parental report, with its limitations, this study suggests that increasing the number of parents who receive patient reminders for their children may improve vaccination coverage among children.
Keywords: Child, Immunization, Influenza, human, Surveys and questionnaires, Vaccination, Vaccination coverage
Introduction
Since 2008, the Advisory Committee on Immunization Practices (ACIP) has recommended annual influenza vaccination for all children 6 months through 18 years to reduce the substantial burden of influenza among children in the United States.[1–5] Influenza vaccination of children has been demonstrated to prevent influenza-related pediatric illnesses, outpatient visits, hospitalizations, and deaths in children, and even to reduce influenza illness in non-vaccinated persons where pediatric coverage rates are high.[1;3-7] However, influenza vaccination coverage levels for children have remained stagnant since the 2013–14 influenza season at approximately 59%.[8]
The U.S. Community Preventive Services Task Force recommends, based on strong evidence, the use of patient reminders to improve vaccination rates in children, adolescents, and adults.[9] Published studies have shown a positive association between patient reminders and influenza vaccination rates among children, but primarily focused on children of a particular age group or with high risk conditions, such as asthma.[10–17] To our knowledge, there are no published studies on the receipt of patient reminders for influenza vaccination among all children 6 months–17 years, regardless of health conditions, that provide national and state-level estimates.
The objectives of this study were to: 1) quantify the proportion of children 6 months–17 years for whom a patient reminder for influenza vaccination was received at the state and national level by sociodemographic characteristics, 2) identify factors associated with parental receipt of a patient reminder for their child’s influenza vaccination, 3) determine whether parental receipt of a patient reminder is independently associated with influenza vaccination status among children, and 4) describe the type and source of patient reminders received.
Methods
Data from the National Immunization Survey-Flu (NIS-Flu) from the 2013–14 influenza season were analyzed.[18;19] The NIS-Flu is an ongoing, national list-assisted random-digit-dialed dual frame land line and cellular telephone survey of households with children. It includes three components: the NIS-Child for children 19–35 months, the NIS-Teen for children 13–17 years, and the NIS Child Influenza Module for children 6–18 months and 3–12 years identified during the screening of households for the NIS-Child and NIS-Teen.[18–25] Data were collected by parental report from all 50 states and the District of Columbia. The Council of American Survey and Research Organizations (CASRO) response rate was 58.6% for landline and 32.1% for cellular telephones.[26;27]
The study sample (n=33,538) included children of respondents who provided information about patient reminders during interviews conducted in April, May, and June 2014 when questions about patient reminders were added to the NIS-Flu. Survey respondents were asked, “Since July 1st, did [sample child’s] doctor or other health professional remind you by mail, phone call, email, or text message that [sample child] should get a flu vaccination this season?”. Children were excluded if the respondent answered “Don’t Know” or refused to answer (4.5%). Respondents who answered “Yes” were then asked, “How did you get a reminder? Was it by mail, phone, email, or text message?” and “Who sent you this reminder: a doctor’s office, health clinic, insurance company, pharmacy, health department, or some other place?” and instructed to choose all that apply. All respondents were also asked if their child had received an influenza vaccination since July 1, 2013, and, if so, during which month and year. Information on child, maternal, and household sociodemographic characteristics were also collected during the interviews.
National and state level influenza vaccination coverage estimates and methods were published previously for children 6 months and older, and were calculated for this study using the same methodology for children who met the inclusion criteria described previously.[26] Tests of association between receipt of a patient reminder for influenza vaccination and demographic variables were conducted using Wald chi-square tests followed by pair-wise comparison t-tests. Multivariable logistic regression was used to determine 1) variables independently associated with receipt of a patient reminder, and 2) whether receipt of a patient reminder was independently associated with receipt of an influenza vaccination. Adjusted prevalence ratios (APR) and adjusted prevalences (AP) based on predicted marginals from the logistic regression models are reported. In addition, population attributable risk (PAR) was calculated using the prevalence of patient reminder receipt and the prevalence ratio of influenza vaccination by patient reminder receipt to assess the potential contribution of patient reminders to the observed influenza vaccination level. Finally, among children for whom a reminder was received, the type and source of the reminder was assessed.
A two-sided significance level of 0.05 was adopted for all statistical tests. Percentages and corresponding 95% confidence intervals (95% CI) were weighted, while sample sizes were unweighted. All analyses were weighted to population totals and to adjust for households having multiple telephone lines, unit non-response, and non-coverage of non-telephone households. Analyses were conducted using SAS (version 9.3) and SUDAAN (version 11.0.0) statistical software to account for the complex design. Institutional review board (IRB) approval for conducting the NIS was obtained through the National Center for Health Statistics Research Ethics Review Board and the IRB of NORC at the University of Chicago.
Results
Demographic and other characteristics of children in the study sample are presented in Table 1. National and state level estimates for parental receipt of a patient reminder for influenza vaccination among children are shown in Table 2 and Figure 1. In the United States, 22.0% of children had a parent report receiving a patient reminder for influenza vaccination of their child. Influenza vaccination coverage among children for whom a patient reminder was received was 73.7% compared with 55.5% among children without a patient reminder, resulting in a PAR estimate of 6.7%. At the state level, the proportion of children for whom a patient reminder was received ranged from 12.9% (Idaho) to 41.2% (Mississippi). For 29 states, vaccination coverage was higher for children who had a patient reminder compared with those who did not; the PAR ranged from 4.8% (New Hampshire) to 16.9% (Wisconsin).
Table 1.
Characteristics of children 6 months–17 years, United States, National Immunization Survey-Flu (NIS-Flu), April–June Interviews, 2013–14 influenza season
| Characteristics | Unweighted n |
Weighted % (± 95% CI*) |
|---|---|---|
| Total | 33,538 | 100.0 |
| Child’s age | ||
| 6–23 months | 3,785 | 8.6 (± 0.8) |
| 2–4 years | 4,826 | 14.5 (± 1.7) |
| 5–12 years | 16,920 | 46.2 (± 1.8) |
| 13–17 years | 8,007 | 30.7 (± 1.7) |
| Child’s sex | ||
| Male | 17,253 | 51.1 (± 1.9) |
| Female | 16,285 | 48.9 (± 1.9) |
| Child’s race/ethnicity† | ||
| White, non-Hispanic | 20,206 | 53.3 (± 2.0) |
| Black, non-Hispanic | 3,434 | 13.9 (± 1.3) |
| Hispanic | 6,104 | 23.6 (± 2.0) |
| Other, non-Hispanic | 3,794 | 9.2 (± 1.2) |
| Language survey completed | ||
| English | 30,859 | 88.5 (± 1.2) |
| Spanish | 2,241 | 10.0 (± 1.1) |
| Other language | 438 | 1.4 (± 0.3) |
| Mother’s education | ||
| < High school | 3,197 | 14.0 (± 1.5) |
| High school or equivalent | 5,736 | 18.9 (± 1.5) |
| Some college | 8,549 | 26.2 (± 1.6) |
| ≥ College degree | 14,683 | 41.0 (± 2.0) |
| Poverty/annual household income‡ | ||
| Above poverty (> $75,000) | 13,148 | 34.3 (± 1.9) |
| Above poverty (≤ $75,000) | 11,337 | 32.5 (± 1.8) |
| Below poverty | 5,461 | 22.5 (± 1.7) |
| Unknown | 3,592 | 10.7 (± 1.1) |
| Number of children in household | ||
| 1 | 10,646 | 24.8 (± 1.5) |
| 2–3 | 19,689 | 62.3 (± 1.8) |
| ≥ 4 | 3,134 | 12.9 (± 1.4) |
| Urban/rural residence§ | ||
| Urban (MSA, principle city) | 8,745 | 25.5 (± 1.6) |
| Suburban (MSA, not principle city) | 17,748 | 60.1 (± 1.8) |
| Rural (non-MSA) | 7,045 | 14.4 (± 1.1) |
| Region of residence | ||
| Northeast | 6,726 | 16.4 (± 1.2) |
| Midwest | 7,052 | 21.4 (± 1.3) |
| South | 12,299 | 37.9 (± 1.8) |
| West | 7,461 | 24.3 (± 1.9) |
| Influenza vaccination status | ||
| ≥ 1 dose | 20,617 | 59.6 (± 1.8) |
| Not vaccinated | 12,921 | 40.4 (± 1.8) |
| Patient reminder for influenza vaccination | ||
| Received | 7,553 | 22.0 (± 1.3) |
| Not received | 25,985 | 78.0 (± 1.3) |
| Provider recommendation for influenza vaccination | ||
| Received | 16,667 | 50.1 (± 2.0) |
| Not received | 7,023 | 22.5 (± 1.7) |
| No provider visit | 8,664 | 27.4 (± 1.5) |
| Provider recommendation/patient reminder | ||
| Recommendation/reminder received | 4,796 | 14.5 (± 1.1) |
| Recommendation/no reminder received | 11,871 | 35.6 (± 2.0) |
| No recommendation/reminder received | 674 | 1.8 (± 0.3) |
| No recommendation/no reminder received | 6,349 | 20.7 (± 1.7) |
| No provider visit/reminder received | 1,872 | 6.0 (± 0.7) |
| No provider visit/no reminder received | 6,792 | 21.3 (± 1.4) |
CI = confidence interval half-width.
Race/ethnicity is based on parental report. Children of Hispanic ethnicity may be of any race. Children categorized as white, black, or other were identified as non-Hispanic. The other race category included children reporting Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, other, or multiple (i.e. selected more than one race category) races.
Poverty level was defined based on the reported number of people living in the household and annual household income, according the U.S. Census poverty thresholds (https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html).
MSA = metropolitan statistical area. MSA was based on parent/guardian respondent-reported city, state, county, and zip code of residence using the (https://www.census.gov/programs-surveys/metro-micro.html ) MSA definitions file.
Table 2.
Weighted prevalence (%) of children 6 months–17 years whose parents received a patient reminder for influenza vaccination for their child, and children 6 months–17 years who received influenza vaccination stratified by parental receipt of a patient reminder, by state of residence, United States, National Immunization Survey-Influenza (NIS-Flu), April–June Interviews, 2013–14 influenza season
|
State of residence |
Parental receipt of a patient reminder |
Influenza vaccination coverage* by parental receipt of a patient reminder |
PAR† |
||
|---|---|---|---|---|---|
| Reminder received |
Reminder not received |
||||
|
n |
% (± 95% CI‡) |
% (± 95% CI) |
% (± 95% CI) |
% |
|
| United States | 33,538 | 22.0 (± 1.3) | 73.7 (±2.7) | 55.5 (±2.3)§ | 6.7 |
| Alabama | 545 | 21.2 (± 7.4) | 75.2 (±10.9)∥ | 54.0 (±15.4)§,∥ | 7.7 |
| Alaska | 608 | 15.6 (± 4.7) | 60.9 (±13.1)∥ | 41.2 (±10.2)§,∥ | 6.9 |
| Arizona | 537 | 23.2 (±10.7)∥ | 47.5 (±27.7)∥ | 43.7 (±8.9) | 2.0 |
| Arkansas | 586 | 20.4 (±11.7)∥ | 69.6 (±19.5)∥ | 47.7 (±29.5)¶ | 8.6 |
| California | 655 | 24.8 (± 6.1) | 77.7 (±8.3) | 61.4 (±10.1)§,∥ | 6.2 |
| Colorado | 771 | 19.0 (± 4.9) | 73.6 (±9.2) | 52.7 (±11.0)§,∥ | 7.0 |
| Connecticut | 598 | 24.6 (± 6.6) | 78.7 (±9.4) | 67.9 (±8.8) | 3.8 |
| Delaware | 672 | 25.2 (± 8.7) | 68.6 (±22.7)∥ | 61.2 (±14.1)∥ | 3.0 |
| District of Columbia | 488 | 25.5 (±11.4)∥ | 57.6 (±30.5)∥ | 66.5 (±10.6)∥ | −3.5 |
| Florida | 533 | 21.6 (± 6.5) | 78.5 (±13.0)∥ | 44.4 (±9.6)§ | 14.2 |
| Georgia | 525 | 21.6 (± 5.6) | 66.7 (±12.9)∥ | 56.5 (±9.6) | 3.8 |
| Hawaii | 418 | 35.5 (± 8.7) | 80.1 (±10.6)∥ | 59.6 (±12.7)§,∥ | 10.9 |
| Idaho | 439 | 12.9 (± 5.7) | 81.6 (±12.9)∥ | 41.0 (±10.0)§ | 11.3 |
| Illinois | 1,277 | 23.8 (± 7.4) | 60.6 (±18.5)∥ | 47.2 (±9.6) | 6.3 |
| Indiana | 711 | 18.8 (± 4.8) | 75.5 (±9.8) | 37.6 (±7.8)§ | 15.9 |
| Iowa | 550 | 20.4 (± 7.2) | 74.6 (±16.7)∥ | 42.2 (±9.5)§ | 13.5 |
| Kansas | 433 | 19.9 (± 7.2) | 73.9 (±13.1)∥ | 64.7 (±10.6)∥ | 2.8 |
| Kentucky | 490 | 17.4 (± 5.1) | 73.3 (±12.7)∥ | 43.8 (±9.6)§ | 10.5 |
| Louisiana | 675 | 22.2 (± 9.9) | 75.5 (±15.6)∥ | 51.9 (±9.5)§ | 9.2 |
| Maine | 552 | 24.1 (± 8.0) | 79.8 (±11.0)∥ | 55.2 (±13.5)§,∥ | 9.7 |
| Maryland | 594 | 28.9 (± 9.6) | 67.0 (±15.4)∥ | 65.1 (±10.6)∥ | 0.8 |
| Massachusetts | 625 | 36.2 (±10.4)∥ | 80.3 (±11.7)∥ | 62.9 (±12.6)§,∥ | 9.1 |
| Michigan | 524 | 22.7 (± 7.8) | 65.1 (±19.3)∥ | 48.6 (±9.4) | 7.2 |
| Minnesota | 474 | 19.2 (± 7.7) | 67.5 (±19.1)∥ | 50.6 (±18.1)∥ | 6.0 |
| Mississippi | 561 | 41.2 (±17.7)∥ | 64.6 (±39.1)¶ | 40.2 (±8.4) | 20.0 |
| Missouri | 546 | 18.3 (± 5.4) | 70.9 (±13.0)∥ | 48.5 (±9.4)§ | 7.8 |
| Montana | 516 | 16.8 (± 5.0) | 72.5 (±13.2)∥ | 46.4 (±8.5)§ | 8.6 |
| Nebraska | 479 | 16.5 (± 8.7) | 85.9 (±8.2) | 40.7 (±22.2)§,∥ | 15.5 |
| Nevada | 708 | 26.3 (± 9.8) | 74.6 (±15.8)∥ | 46.0 (±8.0)§ | 14.1 |
| New Hampshire | 632 | 23.1 (± 5.0) | 80.8 (±7.7) | 66.2 (±7.1)§ | 4.8 |
| New Jersey | 661 | 19.2 (± 5.8) | 85.4 (±8.3) | 62.8 (±8.1)§ | 6.5 |
| New Mexico | 737 | 22.9 (± 9.2) | 78.0 (±12.9)∥ | 67.7 (±14.4)∥ | 3.4 |
| New York | 1,080 | 22.7 (± 4.8) | 68.1 (±8.9) | 64.3 (±8.5) | 1.3 |
| North Carolina | 654 | 19.2 (± 7.0) | 83.3 (±9.3) | 63.2 (±11.0)§,∥ | 5.8 |
| North Dakota | 572 | 13.7 (± 4.4) | 82.6 (±11.8)∥ | 59.8 (±8.7)§ | 5.0 |
| Ohio | 574 | 16.5 (± 5.2) | 76.1 (±12.2)∥ | 47.1 (±12.4)§,∥ | 9.2 |
| Oklahoma | 572 | 25.7 (±11.3)∥ | 80.5 (±13.3)∥ | 54.3 (±9.6)§ | 11.0 |
| Oregon | 547 | 18.0 (± 5.2) | 68.9 (±13.7)∥ | 53.9 (±8.6) | 4.8 |
| Pennsylvania | 1,425 | 24.3 (± 6.6) | 83.6 (±6.9) | 60.7 (±10.6)§,∥ | 8.4 |
| Rhode Island | 571 | 31.2 (±10.1)∥ | 88.5 (±6.9) | 72.8 (±8.7)§ | 6.3 |
| South Carolina | 623 | 15.5 (± 4.3) | 84.5 (±7.3) | 56.8 (±9.6)§ | 7.0 |
| South Dakota | 448 | 25.5 (± 8.4) | 66.9 (±21.6)∥ | 65.8 (±8.8) | 0.4 |
| Tennessee | 521 | 19.2 (± 7.7) | 72.8 (±11.3)∥ | 73.2 (±12.5)∥ | −0.1 |
| Texas | 2,923 | 17.8 (± 4.0) | 82.1 (±7.3) | 59.3 (±7.7)§ | 6.4 |
| Utah | 453 | 17.3 (± 5.5) | 56.1 (±17.9)∥ | 51.0 (±8.4) | 1.7 |
| Vermont | 582 | 23.6 (± 8.0) | 60.8 (±21.6)∥ | 54.7 (±10.5)∥ | 2.6 |
| Virginia | 688 | 19.9 (± 7.0) | 55.7 (±18.8)∥ | 63.5 (±11.0)∥ | −2.5 |
| Washington | 511 | 24.8 (± 7.2) | 70.5 (±18.6)∥ | 56.4 (±8.8) | 5.8 |
| West Virginia | 649 | 22.3 (± 6.7) | 74.6 (±13.8)∥ | 47.2 (±9.4)§ | 11.5 |
| Wisconsin | 464 | 30.8 (± 6.8) | 77.6 (±10.6)∥ | 46.8 (±8.9)§ | 16.9 |
| Wyoming | 561 | 23.4 (±13.8)¶ | 35.9 (±25.3)¶ | 41.1 (±7.4) | −3.1 |
Influenza vaccination coverage calculated by the Kaplan Meier method.
PAR = population attributable risk. Population attributable risk is a measure to assess the potential contribution of patient reminder to the observed vaccination level and was calculated using the formula: P (PR-1) / [P (PR-1)+1], where P was the prevalence of receiving a patient reminder for influenza vaccination and PR was the prevalence ratio of vaccination by patient reminder.
CI = confidence interval half-width.
Vaccination coverage among children for whom a patient reminder for influenza vaccination was received was significantly different statistically from children without a patient reminder. These estimates are also in bold.
Estimates might not be reliable because confidence interval half-width is >10.
Estimates not reliable because relative standard error is >0.3.
Figure 1.
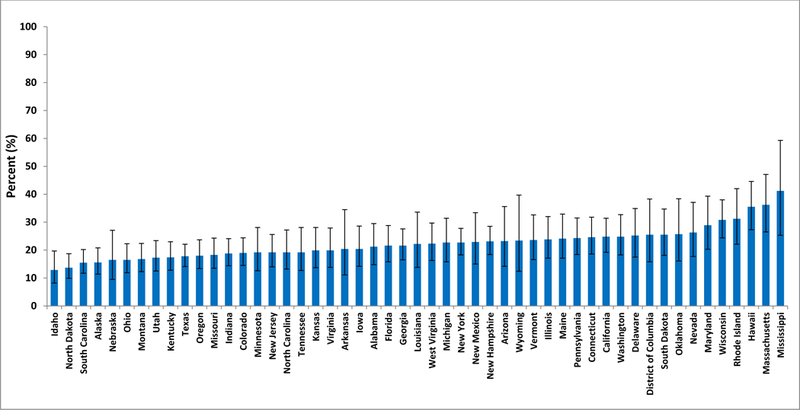
Parental receipt of a patient reminder for influenza vaccination for their child by state, United States, National Immunization Survey-Flu (NIS-Flu), April–June interviews, 2013–14 influenza season
In bivariate analysis, receipt of a provider recommendation for influenza vaccination, child’s age, child’s race/ethnicity, language of survey completion, and household income/poverty status were all found to be associated with parental receipt of a patient reminder for influenza vaccination for the child (Table 3). Children for whom a provider recommendation for influenza vaccination had been received were more likely to have a parent report receipt of a patient reminder (29.0%) than children without a provider recommendation (22.1%) and children who did not visit a provider (7.9%).
Table 3.
Weighted prevalence (%) of children 6 months–17 years whose parents received a patient reminder for influenza vaccination for their child, and children 6 months–17 years who received influenza vaccination stratified by parental receipt of a patient reminder, by selected demographic characteristics and receipt of a provider recommendation, United States, National Immunization Survey-Influenza (NIS-Flu), April–June Interviews, 2013–14 influenza season
|
Characteristics |
Parental receipt of a patient reminder |
Influenza vaccination coverage* by parental receipt of a patient reminder |
||
|---|---|---|---|---|
| Reminder received |
Reminder not received |
PAR† | ||
| % (± 95% CI‡) | % (± 95% CI) | % (± 95% CI) | % | |
| Overall | 22.0 | 73.7 (±2.7) | 55.5 (±2.3)§ | 6.7 |
| Provider recommendation | ||||
| a. Recommendation received | 29.0 (± 2.2)||,b,c | 78.1 (±3.5)b,c | 68.0 (±3.3)§,b,c | 4.1 |
| b. No recommendation | 7.9 (± 1.4)a,c | 59.8 (±7.7)a | 35.1 (±5.1)§,a,c | 5.3 |
| c. No provider visit | 22.1 (± 2.4)a,b | 67.9 (±5.3)a | 56.5 (±3.4)§,a,b | 4.3 |
| Child’s age | ||||
| a. 6–23 months | 28.2 (± 4.4)b,c,d | 81.6 (±6.5)c,d | 63.6 (±6.1)§,d | 7.4 |
| b. 2–4 years | 20.9 (± 3.4)a | 82.1 (±4.4)c,d | 67.4 (±5.8)§,c,d | 4.4 |
| c. 5–12 years | 22.5 (± 1.8)a | 72.0 (±3.9)a,b | 59.4 (±2.9)§,b,d | 4.6 |
| d. 13–17 years | 20.1 (± 2.4)a | 69.3 (±5.9)a,b | 42.4 (±3.8)§,a,b,c | 11.3 |
| Child’s sex | ||||
| a. Male | 22.3 (± 1.9) | 76.3 (±3.2) | 57.5 (±3.3)§ | 6.8 |
| b. Female | 21.7 (± 1.8) | 71.0 (±4.3) | 53.5 (±2.9)§ | 6.6 |
| Child’s race/ethnicity¶ | ||||
| a. White, non-Hispanic | 19.3 (± 1.6)b,c | 69.3 (±4.5)c,d | 51.8 (±2.5)§,c,d | 6.1 |
| b. Black, non-Hispanic | 25.2 (± 3.5)a | 76.3 (±5.5) | 52.0 (±6.2)§,c,d | 10.5 |
| c. Hispanic | 25.9 (± 3.5)a | 77.2 (±4.6)a | 63.4 (±5.6)§,a,b | 5.3 |
| d. Other, non-Hispanic | 23.5 (± 4.6) | 80.9 (±5.5)a | 64.3 (±7.3)§,a,b | 5.7 |
| Language survey completed | ||||
| a. English | 21.5 (± 1.4)b,c | 72.8 (±3.0)c | 53.9 (±2.4)§,b,c | 3.4 |
| b. Spanish | 27.7 (± 4.8)a,c | 79.4 (±7.2)c | 66.8 (±6.7)§,a,c | 11.2 |
| c. Other language | 15.6 (± 5.6)a,b | 90.1 (±7.8)a,b | 78.5 (±8.0)§,a,b | 5.8 |
| Mother’s education | ||||
| a. < High school | 24.6 (± 4.1) | 72.0 (±8.2) | 62.0 (±6.4)b,c | 6.8 |
| b. High school or equivalent | 24.1 (± 3.2) | 71.3 (±6.7) | 49.0 (±5.3)§,a,d | 7.8 |
| c. Some college | 20.7 (± 2.3) | 71.2 (±5.4) | 51.0 (±4.0)§,a,d | 3.8 |
| d. ≥ College degree | 21.1 (± 2.1) | 77.7 (±3.7) | 60.0 (±3.5)§,b,c | 3.0 |
| Poverty/annual household income** | ||||
| a. Above poverty (> $75,000) | 21.2 (± 2.3)c | 78.2 (±4.0)b | 60.3 (±3.7)§,b,d | 5.9 |
| b. Above poverty (≤ $75,000) | 21.4 (± 2.3)c | 67.2 (±5.7)a,d | 49.6 (±3.6)§,a,c | 7.1 |
| c. Below poverty | 25.4 (± 3.0)a,b,d | 74.3 (±5.3) | 58.4 (±5.2)§,b | 6.5 |
| d. Unknown | 19.6 (± 3.1)c | 78.0 (±5.4)b | 52.7 (±6.5)§,a | 8.6 |
| Number of children in household | ||||
| a. 1 | 20.9 (± 2.3) | 74.5 (±4.3) | 51.2 (±3.8)§,b | 8.7 |
| b. 2–3 | 21.5 (± 1.7) | 73.0 (±3.8) | 57.9 (±2.9)§,a | 5.3 |
| c. ≥ 4 | 26.8 (± 4.4) | 75.6 (±6.0) | 52.5 (±7.0)§ | 10.5 |
| Urban/rural residence†† | ||||
| a. Urban (MSA, principle city) | 24.7 (± 2.6) | 75.1 (±5.2) | 54.6 (±4.1)§ | 8.5 |
| b. Suburban (MSA, not principle city) | 21.0 (± 1.8) | 73.8 (±3.6) | 57.5 (±3.1)§,c | 5.6 |
| c. Rural (non-MSA) | 21.7 (± 3.0) | 70.8 (±7.0) | 49.0 (±4.5)§,b | 8.8 |
| Region of residence | ||||
| a. Northeast | 24.3 (± 2.9) | 77.6 (±4.3) | 63.2 (±4.4)§,b,c | 5.2 |
| b. Midwest | 21.0 (± 2.4) | 69.9 (±6.4) | 47.5 (±3.9)§,a,c,d | 9.0 |
| c. South | 20.9 (± 2.0) | 74.7 (±4.4) | 56.4 (±3.4)§,a,b | 6.4 |
| d. West | 23.3 (± 3.4) | 72.5 (±6.3) | 56.3 (±5.8)§,b | 6.3 |
Influenza vaccination coverage calculated by the Kaplan Meier method.
PAR = population attributable risk. Population attributable risk is a measure to assess the potential contribution of patient reminder to the observed vaccination level and was calculated using the formula: P (PR-1) / [P (PR-1)+1], where P was the prevalence of receiving a patient reminder for influenza vaccination and PR was the prevalence ratio of vaccination by patient reminder.
CI = confidence interval half-width.
Vaccination coverage among children for whom a patient reminder for influenza vaccination was received was statistically significantly different from children without a patient reminder.
The presence or absence of superscripted letters denotes whether that estimate was statistically significantly different at P < 0.05 from another row, and denotes which row it differed from (a, b, c, or d), based on pair-wise comparison t-test. For example, the percentage of children 2–4 years (b) who received a patient reminder (20.9%) was significantly different statistically from the percentage of children 6–23 months (a) who received a patient reminder (28.2%).
Race/ethnicity is based on parental report. Children of Hispanic ethnicity may be of any race. Children categorized as white, black, or other were identified as non-Hispanic. The other race category included children reporting Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, other, or multiple (i.e. selected more than one race category) races.
Poverty level was defined based on the reported number of people living in the household and annual household income, according the U.S. Census poverty thresholds (https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html).
MSA = metropolitan statistical area. MSA was based on parent/guardian respondent-reported city, state, county, and zip code of residence using the (https://www.census.gov/programs-surveys/metro-micro.html) MSA definitions file.
A higher percentage of children 6–23 months had a parent report receipt of a patient reminder than children 2–4 years, 5–12 years, and 13–17 years (Table 3). The proportion of children for whom a patient reminder was received was lower among non-Hispanic white children than non-Hispanic black and Hispanic children. Children of parents who completed the survey in Spanish were more likely to have a reminder than those of parents who completed the survey in English; children of parents who completed the survey in a language other than English or Spanish were the least likely to report receiving a patient reminder. More children living below poverty had a parent report receiving a patient reminder compared with those living above poverty. Estimates by sociodemographic characteristics and differences in estimates between groups are presented in Table 3.
Multivariable analysis to determine factors associated with parental receipt of a patient reminder for influenza vaccination for the child resulted in some findings that were consistent with the bivariate analysis (Table 4). Younger children 6–23 months (APR 1.33) and non-Hispanic black children (APR 1.29) were more likely to have a parent report receipt of a patient reminder than children 13–17 years and non-Hispanic white children, respectively. Children for whom the survey was completed in a language other than English or Spanish were less likely to have a patient reminder than those for whom the survey was completed in English (APR 0.63). In addition, children living in households with 4 or more children and children living in the Northeast were more likely to have a parent report receipt of a patient reminder compared with children living in households with only one child and children living in the South, respectively.
Table 4.
Association of parental receipt of a patient reminder for influenza vaccination with demographic characteristics among children 6 months–17 years, United States, National Immunization Survey-Influenza (NIS-Flu), April–June Interviews, 2013–14 influenza season
| Characteristics | APR* ± 95% CI† | AP‡ % |
|---|---|---|
| Child’s age | ||
| 6–23 months | 1.33 (1.09–1.63) | 27.6 |
| 2–4 years | 0.98 (0.80–1.21) | 20.4 |
| 5–12 years | 1.08 (0.93–1.24) | 22.4 |
| 13–17 years | Referent | 20.7 |
| Child’s sex | ||
| Male | 1.03 (0.92–1.16) | 22.4 |
| Female | Referent | 21.7 |
| Child’s race/ethnicity§ | ||
| White, non-Hispanic | Referent | 19.8 |
| Black, non-Hispanic | 1.29 (1.07–1.55) | 25.6 |
| Hispanic | 1.21 (0.97–1.50) | 24.0 |
| Other, non-Hispanic | 1.22 (0.97–1.53) | 24.1 |
| Language survey completed | ||
| English | Referent | 21.9 |
| Spanish | 1.11 (0.84–1.47) | 24.3 |
| Other language | 0.63 (0.42–0.94) | 13.7 |
| Mother’s education | ||
| < High school | Referent | 21.8 |
| High school or equivalent | 1.08 (0.85–1.37) | 23.5 |
| Some college | 0.97 (0.76–1.22) | 21.0 |
| ≥ College degree | 1.01 (0.80–1.28) | 22.1 |
| Poverty/annual household income∥ | ||
| Above poverty (> $75,000) | 0.98 (0.81–1.18) | 22.5 |
| Above poverty (≤ $75,000) | 0.95 (0.80–1.13) | 21.8 |
| Below poverty | Referent | 23.0 |
| Unknown | 0.80 (0.64–1.01) | 18.5 |
| Number of children in household | ||
| 1 | Referent | 21.1 |
| 2–3 | 1.02 (0.89–1.17) | 21.6 |
| ≥ 4 | 1.24 (1.01–1.52) | 26.1 |
| Urban/rural residence¶ | ||
| Urban (MSA, principle city) | 1.04 (0.86–1.25) | 23.5 |
| Suburban (MSA, not principle city) | 0.93 (0.79–1.10) | 21.2 |
| Rural (non-MSA) | Referent | 22.7 |
| Region of residence | ||
| Northeast | 1.20 (1.02–1.40) | 24.7 |
| Midwest | 1.07 (0.91–1.24) | 21.9 |
| South | Referent | 20.6 |
| West | 1.10 (0.92–1.31) | 22.6 |
APR = Adjusted Prevalence Ratio. Estimates in bold are statistically significantly different from the referent (P < 0.05). All variables listed in the table were included in the model.
CI = Confidence Interval.
AP = Adjusted Prevalence.
Race/ethnicity is based on parental report. Children of Hispanic ethnicity may be of any race. Children categorized as white, black, or other were identified as non-Hispanic. The other race category included children reporting Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, other, or multiple (i.e. selected more than one race category) races.
Poverty level was defined based on the reported number of people living in the household and annual household income, according the U.S. Census poverty thresholds (https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html).
MSA = metropolitan statistical area. MSA was based on parent/guardian respondent-reported city, state, county, and zip code of residence using the (https://www.census.gov/programs-surveys/metro-micro.html) MSA definitions file.
The results of the multivariable analysis to determine whether parental receipt of a patient reminder was independently associated with the child’s receipt of influenza vaccination showed that children whose parent reported receipt of a patient reminder were approximately 20% more likely to be vaccinated compared with children whose parent did not report receiving a patient reminder, even after controlling for demographic characteristics and receipt of a provider recommendation for influenza vaccination for the child (APR 1.19). We found through additional exploratory analyses that all types of patient reminders (i.e. phone, mail, and email/text) were associated with influenza vaccination.
Among respondents who received a patient reminder for their child, 66.3% reported receiving one from a doctor’s office, 14.5% reported receiving one from an insurance company, and 13.3% reported receiving one from a health clinic (Figure 2). Health departments and pharmacies were infrequently reported as a source of patient reminders. Nearly half of respondents who received a patient reminder reported they received one in the mail, nearly one-third received one by phone, and 16.7% by email. Only 3.3% of respondents who received a patient reminder reported receiving a text message.
Figure 2.
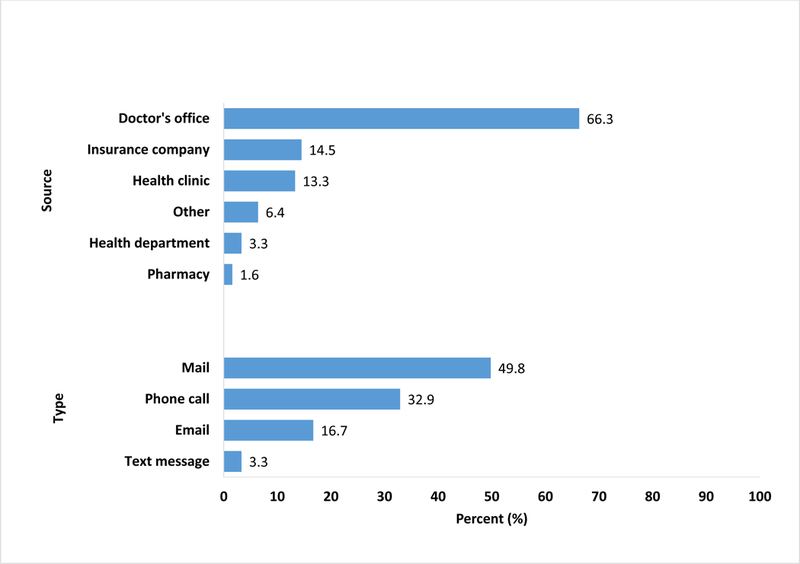
Source and type* of patient reminder for influenza vaccination received by the parent for their child, United States, National Immunization Survey-Flu (NIS-Flu), April–June interviews, 2013–14 influenza season (n=7,553) *Respondents could select more than one source and\or type of reminder.
Discussion
Our study is the first to assess parental receipt of patient reminders for influenza vaccination for their children at the national and state level and the contribution of patient reminders to the influenza vaccination status of children. Our study and others have demonstrated that provider reminders are associated with higher vaccination rates.[9;14] However, nearly 4 out of 5 parents did not receive a reminder about influenza vaccination for their child. Given the consistent association between patient reminders and vaccination, the limited use of this evidence-based strategy likely contributes to low influenza vaccination rates among children in the United States. Reports of patient reminder for influenza vaccination varied substantially by state (12.9%–41.5%) and suggest states where promotion of patient reminders may be improved to increase influenza vaccinations. A recent study also found variation by state, with 22% of primary care providers for children reporting that they use of patient reminders for influenza vaccination in Colorado and 33% in New York during the 2015–16 season.[28] Our estimate of 22% of parents having received a patient reminder during the 2013–14 influenza season is somewhat lower than two earlier national studies on patient reminders from 2010 and the 2010–11 season. In the 2010 study, based on a nationally representative Internet panel survey, 31% of parents of children 0–17 years had ever received a reminder for childhood vaccinations.[29] In the 2010–11 study, only 25% of interviewed U.S.-based primary care physicians reported that they issued influenza vaccination reminders during the 2010–11 season, the first year of universal vaccination recommendations.[30]
Influenza vaccination coverage during the 2013–14 season was significantly higher among children for whom a patient reminder was received (73.7%) than among children for whom a patient reminder was not received (55.5%). In addition, we estimated that, nationally, during the 2013–14 season, approximately 7% of vaccination coverage among children could be attributed to parental receipt of a patient reminder. Several clinical trials have also documented a positive association between patient reminders and influenza vaccination status among children. A study on young children with high risk conditions at a pediatric practice in Denver, Colorado during the 2002–03 season found that influenza vaccination coverage was higher in the intervention group who received a reminder for influenza vaccination by mail compared with children in the control group who did not receive a reminder (42% versus 25%).[10] Similar findings were reported for young children with high risk conditions who resided in three Michigan counties during the 2008–09 season (30.8% versus 24.3% were vaccinated).[11] Two studies on children with asthma found that coverage during the early 1990s was higher in intervention groups who received influenza vaccination reminder letters compared with control groups at pediatric clinics in Rochester, NY (30% versus 7%) and Seattle, Washington (47% versus 21%), respectively.[15;17] Another study reported a small but significant difference in influenza vaccination coverage during the 2010–11 season among children at four pediatric clinics in New York City who received text message reminders compared with children who received the usual care which included an automated phone call reminder (43.6% versus 39.9%).[16] In addition, a significant increase in influenza vaccination coverage during the 1997–98 season was noted among children with asthma at a pediatric clinic in Temple, TX after the implementation of an intervention that included both a reminder letter and an automated phone call.[13]
Younger children (6–23months) were found to be more likely than older children (13–17 years) to have a parent report receiving a patient reminder. It is possible that providers are more likely to target younger children with reminders, especially those younger than 2 years, because they are at higher risk of serious adverse complications compared with older children.[31–34] Children younger than 2 years have also been recommended to receive an annual influenza vaccination by the ACIP for the longest amount of time (since 2004) in comparison with other child age groups, so providers may be most familiar with the need to vaccinate these younger children.[2;35-37] However, the ACIP recommends annual influenza vaccination for all persons 6 months and older, so it is important for pediatric providers to consider the implementation of a patient reminder system that includes all patients.[37]
We found that non-Hispanic black and Hispanic children were more likely than non-Hispanic white children to have a parent report receipt of a patient reminder for influenza vaccination for their child. Receipt of a patient reminder was associated with influenza vaccination among children regardless of race/ethnicity. Providers may improve vaccination coverage among children of all races/ethnicities by expanding the use of patient reminders, and also employing other strategies including ensuring they make a strong recommendation for vaccination.[9]
It is also notable that children of parents who completed the NIS-Flu survey in a language other than English or Spanish were less likely to report receiving a patient reminder for influenza vaccination for their child than children of parents who completed the survey in English. Language barriers could prevent the understanding or recognition of a patient reminder for influenza vaccination. It is critical that patient communications be delivered in the preferred language in order to be effective.
In the 2013–14 season, children who had a parent report receipt of a patient reminder for influenza vaccination for their child were approximately 20% more likely to be vaccinated than children without a patient reminder, even when controlling for demographic characteristics and receipt of a provider recommendation. This demonstrates the importance of patient reminders for influenza vaccination among children, regardless of characteristics such as age, race/ethnicity, and poverty status, and even whether a provider recommendation was received, which has been shown to be strongly associated with vaccination status.[38–40]
As seen in other studies, the majority of parents who received a patient reminder for influenza vaccination for their child reported receiving a reminder from a doctor’s office.[8;26;41;42] Health departments and pharmacies were infrequently reported as a source of patient reminders. Despite the low percentage of children receiving their influenza vaccination at a health department, a study conducted in Colorado found that the majority of parents of children 19–35 months strongly supported the health department sending reminders for children who need shots.[43] Pharmacies that provide immunizations can expand access to influenza vaccinations for children. A study of parents in Wisconsin found them to be supportive of pharmacists as an immunization resource.[44] It is important to note, however, that states have different laws regarding the minimum patient age that pharmacists are allowed to provide influenza vaccination (e.g. >6 years to >19 years), with some states allowing pharmacists to vaccinate persons of any age.[45]
In our study, mail was the most common type of patient reminder received, followed by phone, email, and text message. These findings are in-line with parent preferences identified by another study where 57.7%, 17%, 12.7%, and 10.7% of parents preferred mail, telephone, e-mail, and text message reminders, respectively.[43] Although not preferred, 60.1% reported it would be acceptable to receive reminders by e-mail and 46.2% by text message.[43] We found that only 3.3% of children whose parent reported receipt of a patient reminder had received a text message. In a study of parents and providers of children 6–59 months in New York City, 84% of parents reported never receiving health-related text messages, but 88% were comfortable receiving them, and nearly all were interested in receiving reminder text messages, many endorsing them over phone calls and/or letters. In addition, most providers were supportive of using text messaging to remind parents to schedule a vaccine appointment (88%).[46] These reports indicate there is parental and provider support of patient reminders for childhood vaccination, including approaches such as text messages and e-mail which appear to be under-utilized, although our study is from the 2013–14 season and the use of text messaging and email have likely increased.
The findings of this study are subject to several limitations. First, receipt of a patient reminder for influenza vaccination for the child and influenza vaccination status of the child were based on parental report and were not validated with medical records. If the child was vaccinated, the parent might be more likely to remember receiving a patient reminder, so the study findings may overstate the association between patient reminders and vaccination rates. Furthermore, the questions about patient reminders were only asked during April–June, potentially several months after a patient reminder or vaccination might have been received. Therefore, the results are subject to respondent recall bias. In addition, the NIS-Flu is a telephone survey that excludes households with no telephone service which may lead to selection bias. The CASRO response rate was low, especially for the cellular telephone sample, which is another limitation. Non-response bias can result if respondents and non-respondents differed in receipt of reminders or vaccination. Non-coverage and non-response bias may remain even after weighting adjustments. It is also important to note that providers who are sending patient reminders may also be more likely to be implementing other strategies known to increase vaccination rates, and it was not possible to control for this in our model. Finally, the study data are from 4 years ago which could affect the prevalence of patient reminders, although still provide important evidence.
Conclusions
This study highlights the positive relationship between patient reminders and influenza vaccination among children and the under-utilization of this intervention. While improvement is needed for all children across the United States, targeted efforts may be most beneficial in states with the lowest rates of vaccination of children and use of reminders. Use of reminders should include parents of children >2 years and accommodate preferred languages other than English. Policy makers, healthcare providers, and healthcare systems should consider potential access barriers and mitigation strategies to improve the proportion of children whose parents receive an influenza vaccination reminder from their child’s provider.
Acknowledgments
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Abbreviations:
- ACIP
Advisory Committee on Immunization Practices
- NIS-Flu
National Immunization Survey-Flu
- NIS-Child
National Immunization Survey-Child
- NIS-Teen
National Immunization Survey-Teen
- CASRO
Council of American Survey and Research Organizations
- APR
Adjusted Prevalence Ratio
- AP
Adjusted Prevalence
- PAR
Population Attributable Risk
- CI
Confidence Interval
- MSA
Metropolitan Statistical Area
Footnotes
Disclosure
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Declarations of interest: none
References
- [1].Buchan SA, Chung H, Campitelli MA, et al. Vaccine effectiveness against laboratory-confirmed influenza hospitalizations among young children during the 2010–11 to 2013–14 influenza seasons in Ontario, Canada. PLOS ONE 2017;12(11):e0187834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].CDC. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2008. MMWR 2008;57(RR07):1–60. [PubMed] [Google Scholar]
- [3].Flannery B, Reynolds SB, Blanton L, et al. Influenza vaccine effectiveness against pediatric deaths: 2010–2014. Pediatrics 2017;139(5):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Jain VK, Rivera L, Zaman K, et al. Vaccine for prevention of mild and moderate-to-severe influenza in children. N Engl J Med 2013;369:2481–91. [DOI] [PubMed] [Google Scholar]
- [5].Neuzil KM, Dupont WD, Wright PF, Edwards KM. Efficacy of inactivated and cold-adapted vaccines against influenza A infection, 1985 to 1990: The pediatric experience. Pediatr Infect Dis J 2001;20(8):733–40. [DOI] [PubMed] [Google Scholar]
- [6].Grohskopf LA, Sokolow LZ, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices - United States, 2017–18 influenza season. MMWR 2017;66(2):1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Loeb M, Russell ML, Moss L, et al. Effect of influenza vaccination of children on infection rates in Hutterite communities: A randomized trial. JAMA 2010;303(10):943–50. [DOI] [PubMed] [Google Scholar]
- [8].CDC. Flu vaccination coverage, United States, 2016–17 influenza season. FluVaxView 2017. Available at: https://www.cdc.gov/flu/fluvaxview/coverage-1617estimates.htm [accessed Oct 30, 2017] [Google Scholar]
- [9].Guide to community preventive services. Vaccination programs: Client reminder and recall systems. 2017. Available at: https://www.thecommunityguide.org/findings/vaccination-programs-client-reminder-and-recall-systems [accessed May 10, 2018]
- [10].Daley MF, Barrow J, Pearson K, et al. Identification and recall of children with chronic medical conditions for influenza vaccination. Pediatrics 2004;113(1):e26–e33. [DOI] [PubMed] [Google Scholar]
- [11].Dombkowski KJ, Harrington LB, Dong S, Clark SJ. Seasonal influenza vaccination reminders for children with high-risk conditions, a registry-based randomized trial. Am J Prev Med 2012;42(1):71–5. [DOI] [PubMed] [Google Scholar]
- [12].Dombkowski KJ, Cowan AE, Reeves SL, Foley MR, Dempsey AF. The impacts of email reminder/recall on adolescent influenza vaccination. Vaccine 2017;35(23):3089–95. [DOI] [PubMed] [Google Scholar]
- [13.Gaglani M, Riggs M, Kamenicky C, Glezen WP. A computerized reminder strategy is effective for annual influenza immunization of children with asthma or reactive airway disease. Pediatr Infect Dis J 2001;2001(20):1155–60. [DOI] [PubMed] [Google Scholar]
- [14].Jacobson Vann JC, Jacobson RM, Coyne-Beasley T, Asafu-Adjei JK, Szilagyi PG. Patient reminder and recall interventions to improve immunization rates. Cochrane Database Syst Rev 2018;2018(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kemper K, Goldberg H. Computer-generated reminder letters improve the rate of influenza immunization in an urban pediatric clinic? Am J Dis Child 1993;147(7):717–8. [DOI] [PubMed] [Google Scholar]
- [16].Stockwell MS, Kharbanda EO, Martinez RA, Vargas CY, Yawdrey DK, Camargo S. Effect of a text messaging intervention on influenza vaccination in an urban, low income pediatric and adolescent population, a randomized controlled trial. JAMA 2012;307(16):1702–8. [DOI] [PubMed] [Google Scholar]
- [17].Szilagyi P, Rodewald L, Savageau J, Yoos L, Doane C. Improving influenza vaccination rates in children with asthma: A test of a computerized reminder system and an analysis of factors predicting vaccination compliance. Pediatrics 1992;90(6):871–5. [PubMed] [Google Scholar]
- [18].CDC. Surveillance of influenza vaccination coverage - United States, 2007–08 through 2011–12 influenza seasons. MMWR 2013;62(SS04):1–29. [PubMed] [Google Scholar]
- [19].CDC. About the National Immunization Surveys. 2017. Available at: https://www.cdc.gov/vaccines/imz-managers/nis/about.html [accessed Sep 8, 2017]
- [20].Hill HA, Elam-Evans LD, Yankey D, Singleton JA, Kang Y. Vaccination coverage among children aged 19–35 months - United States, 2016. MMWR 2017;66(43):1171–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Jain N, Singleton JA, Montgomery M, Skallard B. Determining accurate vaccination coverage rates for adolescents: The National Immunization Survey-Teen 2006. Public Health Rep 2009;124(5):642–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Smith PJ, Battaglia MP, Huggins VJ, et al. Overview of the sampling design and statistical methods used in the National Immunization Survey. Am J Prev Med 2001;20(4 Suppl):17–24. [DOI] [PubMed] [Google Scholar]
- [23].Smith PJ, Hoaglin DC, Battaglia MP, Khare M, Barker LE. Statistical methodology of the National Immunization Survey, 1994–2002. National Center for Health Statistics; 2005. Report No.: 138. [PubMed] [Google Scholar]
- [24].Walker TY, Elam-Evans LD, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years - United States, 2016. MMWR 2017;66(33):874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Wolter KM, Smith PJ, Khare M, et al. Statistical methodology of the National Immunization Survey, 2005–2014. National Center for Health Statistics. Vital and Health Statistics 1(61). 2017. Available at: https://www.cdc.gov/nchs/data/series/sr_01/sr01_061.pdf [accessed Mar 21, 2018] [PubMed] [Google Scholar]
- [26].CDC. Flu vaccination coverage, United States, 2013–14 influenza season. FluVaxView 2014. Available at: https://www.cdc.gov/flu/fluvaxview/coverage-1314estimates.htm [accessed Dec 28, 2016] [Google Scholar]
- [27].Frankel L The report of the CASRO task force on response rates In: Wiseman F, editor. Improving Data Quality in Sample Surveys.Cambridge, MA, Marketing Science Institute, 1983. [Google Scholar]
- [28].Saville A, Szilagyi P, Helmkamp L, et al. Potential strategies to achieve universal influenza vaccination for children: provider attitudes in two states. Acad Pediatr 2018;(in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Clark SJ, Butchart A, Kennedy A, Dombkowski KJ. Parents’ experiences with and preferences for immunization reminder/recall technologies. Pediatrics 2011;128(5):e1100–e1105. [DOI] [PubMed] [Google Scholar]
- [30].Maurer J, Harris KM. Issuance of patient reminders for influenza vaccination by US-based primary care physicians during the first year of universal influenza vaccination recommendations. Am J Public Health 2014;104(6):e60–e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Bourgeois FT, Valim C, Wei JC, McAdam AJ, Mandl KD. Influenza and other respiratory virus-related emergency department visits among young children. Pediatrics 2016;118(1). [DOI] [PubMed] [Google Scholar]
- [32].CDC. Children, the flu, and the flu vaccine. 2017. Available at: https://www.cdc.gov/flu/protect/children.htm [accessed Oct 27, 2017]
- [33].Poehling KA, Edwards KM, Weinberg GA, et al. The underrecognized burden of influenza in young children. N Engl J Med 2006;355:31–40. [DOI] [PubMed] [Google Scholar]
- [34].Rolfes MA, Foppa IM, Garg S, et al. Estimated influenza illnesses, medical visits, hospitalizations, and deaths averted by vaccination in the United States. CDC; 2017. Available at: https://www.cdc.gov/flu/about/disease/2015-16.htm [accessed Dec 12, 2017] [Google Scholar]
- [35].CDC. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2004;53(RR06):1–40. [PubMed] [Google Scholar]
- [36].CDC. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2006;55(RR-10):1–42. [PubMed] [Google Scholar]
- [37].CDC. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR 2010;59(RR08):1–62. [PubMed] [Google Scholar]
- [38].Gnanasekaran SK, Finkelstein JA, Hohman K, O’Brien M, Kruskal B, Lieu TA. Parental perspectives on influenza vaccination among children with asthma. Public Health Rep 2006;121(2):181–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Kahn KE, Santibanez TA, Zhai Y, Bridges CB. The association between provider recommendation and influenza vaccination status among children 6 months–17 years, United States, 2013–14 through 2015–16 influenza seasons. Presented at the 48th National Immunization Conference Atlanta, GA May 17; 2018. [Google Scholar]
- [40].Nowalk MP, Zimmerman RK, Lin CJ, et al. Parental perspectives on influenza immunization of children aged 6 to 23 months. Am J Prev Med 2005;29(3):210–4. [DOI] [PubMed] [Google Scholar]
- [41].CDC. Flu vaccination coverage, United States, 2014–15 influenza season. FluVaxView 2015. Available at: https://www.cdc.gov/flu/fluvaxview/coverage-1415estimates.htm [accessed Dec 13, 2017] [Google Scholar]
- [42].CDC. Flu vaccination coverage, United States, 2015–16 influenza season. FluVaxView 2016. Available at: https://www.cdc.gov/flu/fluvaxview/coverage-1516estimates.htm [accessed Dec 13, 2017] [Google Scholar]
- [43].Saville AW, Beaty B, Dickinson LM, Lockhart S, Kempe A. Novel immunization reminder/recall approaches: Rural and urban differences in parent perceptions. Acad Pediatr 2014;14(3):249–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Deshpande M, Schauer J, Mott DA, Young HN, Cory P. Parents’ perceptions of pharmacists as providers of influenza vaccine to children. J Am Pharm Assoc 2013;53(5):488–95. [DOI] [PubMed] [Google Scholar]
- [45].American Pharmacists Association. Pharmacist administered vaccines. 2014. Available at: http://www.pharmacist.com/sites/default/files/files/Pharmacist_IZ_Authority_01_17_14.pdf [accessed Dec 13, 2017]
- [46].Hofstetter AN, Vargas CY, Kennedy A, Kitayama K, Stockwell MS. Parental and provider preferences and concerns regarding text message reminder/recall for early childhood vaccinations. Prev Med 2013;57(2):75–80. [DOI] [PubMed] [Google Scholar]


