Abstract
The skin is the largest organ of the body, which meets the environment most directly. Thus, the skin is vulnerable to various damages, particularly burn injury. Skin wound healing is a serious interaction between cell types, cytokines, mediators, the neurovascular system, and matrix remodeling. Tissue regeneration technology remarkably enhances skin repair via re-epidermalization, epidermal-stromal cell interactions, angiogenesis, and inhabitation of hypertrophic scars and keloids. The success rates of skin healing for burn injuries have significantly increased with the use of various skin substitutes. In this review, we discuss skin replacement with cells, growth factors, scaffolds, or cell-seeded scaffolds for skin tissue reconstruction and also compare the high efficacy and cost-effectiveness of each therapy. We describe the essentials, achievements, and challenges of cell-based therapy in reducing scar formation and improving burn injury treatment.
Keywords: Burns, Skin regeneration, Cell-based therapy, Stem cells, Skin substitutes
Introduction
Burns remain as one of the most common injuries worldwide, with more than one million patients annually in the USA alone [1]. A burn ensues after the skin is damaged by heat, radiation, electricity, or chemicals. Serious complications of deep or widespread burns can happen, e.g., sepsis due to bacterial infection, shock caused by hypovolemia, or scaring tissue contraction after improper wound healing. The skin damage causes the death of skin cells, leading to an enormous loss of body fluids that is followed by dehydration, electrolyte imbalance, and renal and circulatory failure. Another serious threat to lives of burn patients is an infection. The burned skin is extremely susceptible to bacteria and other pathogens, due to the loss of protection by intact layers of the skin. Each of these complications can be fatal or make a patient suffer. Therefore, it is critical to promptly cover a burn injury using an appropriate approach to prevent them and save patients’ lives, besides providing intravenously fluids and nutrients to offset dehydration and replace lost proteins.
The survival rates of patients with burns have significantly improved due to the application of various skin grafts over the last decades. Despite wide use, autologous skin grafts are deficient in the treatment of severe burns for patients with limited donor site area [2, 3]. Skin substitutes, especially cell-based ones, play critical role in overcoming this scarcity. The cumulative effect of cell-sheets, scaffolds, cell-scaffolds, and hydrogels with healing promoting factors triggers, accelerates, and enhances wound healing and re-epithelialization that leads to a reduction in scar formation and prevention of burn injury complication. Skin substitutes have shown high efficacy and cost-effectiveness compared to autologous skin replacement [12, 13]. In this study, we focus on discussing the essentials, achievements, and challenges of cell-based therapy for skin tissue regeneration in the treatment of burn injury.
The skin plays an important role which cannot be overestimated; its functioning ensures homeostasis and protects us from aggressive and causative agents in the environment. It is constantly involved in numerous processes: water balance and temperature regulation, signal perception, hormone, neuropeptide and cytokine production and activation, etc. [4]. The skin is formed by three main layers (the epidermis, the dermis, and the hypodermis) with its appendages (hair, sweat and sebaceous glands, sensory neurons, blood and lymph vessels, etc.) [5]. The entire skin tissue contains various cells (epidermal, stromal, endothelial, and neuronal cells) and the extracellular matrix (ECM). Cells, growth factors, and matrix are the basic elements for use in the skin regeneration and replacement after an injury.
Skin anatomy
The skin is a complex tissue, and its structure is presented by the epidermis, the dermis, the hypodermis, and skin appendages [5].
The external first layer—the epidermis—is the main barrier between the environment and internal organs and tissues. It is structured in layers (strata): horny layer (stratum corneum), clear layer (stratum lucidum), granular layer (stratum granulosum), spinous layer (stratum spinosum), and basal layer (stratum basale) [6, 7]. The epidermis is thin and stratified and consists of cell populations such as keratinocytes, Merkel cells, melanocytes, and Langerhans cells [8]. Keratinocytes are the major cell component of the epidermis and responsible for its stratified structure; they form numerous and tight intercellular junctions. Melanocytes, which synthesize melanin (pigment absorbing UV radiation and protecting from its negative effects), are located in the basal layer (stratum basale) and form dendrites that can reach the spinous layer (stratum spinosum) [7]. Merkel cells, which are responsible for the mechanic perception, are also found in the stratum basale (above the basement membrane). Langerhans cells are distributed in the stratum spinosum and involved in immune protection: they act as an antigen-presenting cell and engulf pathogens or other foreign matter [5].
Being the main cell component in all epidermal layers, keratinocytes ensure keratinization due to their differentiation starting in the basal layer [9]. While differentiating and migrating towards a skin surface, keratinocytes become anucleated and have clustered keratin in the stratum granulosum. Then they flatten and die in the stratum corneum. Corneocytes (differentiated keratinocytes) have tight intercellular junctions that prevent water evaporation and skin dehydration, but they are expulsed because of the desmosome loss [10]. This process is involved in desquamation (i.e., skin peeling). However, the epidermis has no direct blood supply, and delivery of nutrients and elimination of residuals occur due to the diffusion from the underlying dermis through the epidermal basement membrane [8, 11]. The basement membrane is a semipermeable layer which is formed by ECM components such as collagen type IV, nidogen, laminin, and perlecan [12, 13].
Beneath the epidermis, there is the dermis which forms a thick layer mainly consisting of the connective tissue and ECM [7, 8]. It is more heterogeneous than the epidermis, and different structures like blood and lymph vessels, sweat and sebaceous glands, and hair follicles are located there. It can be divided into two layers: papillary and reticular. The first one is thin and superficial and presented by the flowing connective tissue, which includes reticular, elastic, and non-organized collagen (mostly type III) fibers and capillaries. The latter one is thick and deep and presented by the compact connective tissue, which has crosslinked elastic and well-organized collagen (type I and III) fibers and large blood vessels [7]. The connective tissue mainly consists of collagen, which enables the skin’s strength, but there are also elastin (elasticity and flexibility) and proteoglycans (hydration and viscosity) [12]. It is constantly remodeled because of the action of proteolytic enzymes (matrix metalloproteinases) synthesized by fibroblasts, neutrophils, keratinocytes, etc., and involved in numerous processes in the skin [14, 15]. The main cell type of the dermis is fibroblasts, which produce components of the ECM (collagen, elastin, and proteoglycans) and secrete various growth factors (TGF-β), cytokines (TNF-α), and matrix metalloproteinases. This “cocktail” ensures the formation of the ECM and keratinocyte proliferation and differentiation [16]. Therefore, fibroblasts are essential for the skin remodeling and wound healing [17]. Moreover, various immune cells (e.g., dendritic cells, leukocytes) are found and can migrate through the dermis [4].
Between the dermis and muscles, the hypodermis (subcutaneous tissue) is located [7]. It protects the internal tissues and organs from cold and trauma, provides energy, and participates in the hormone synthesis (e.g., estrone, leptin) [4]. The hypodermis is formed by adipocytes structured in lobules. These lobules are separated with the septa from the connective tissue and contain nerves and lymphatic and microvascular network, which ensures nutrient and oxygen delivery [7].
Moreover, the skin structure also includes the skin appendages [6, 18], e.g., nails, hair follicles, sweat glands, and sebaceous glands. Hair follicles, which are distributed all around the body (except palms and soles), are formed by basal cells in the basement membrane and responsible for the body temperature control and mechanic perception [6]. Keratinized and dead cells compose nails [7]. At the base of the hair follicles, there are sebaceous glands which produce sebum (oily substance), which ensures the skin and hair lubrication and waterproofness [19]. Sweat glands secrete sweat onto a skin surface [20], and ceruminous and mammary glands are the changed sweat glands that are responsible for the cerumen and milk (respectively) production [7, 21].
The recent findings have shown that the skin has its own stem cells which are rather heterogeneous and can be divided into various subtypes: epidermal, follicular, hematopoietic, melanocyte and sebaceous gland stem, mesenchymal stem-like, and neuronal progenitor cells [6, 22].
Skin tissue regeneration processes
Skin would healing is a systematic process, traditionally including four overlapping classic phases [23, 24]: hemostasis (coagulation), inflammation (mononuclear cell infiltration), proliferation (epithelialization, fibroplasia, angiogenesis, and formation of granulation tissue), and maturation (collagen deposit or scaring tissue formation). Several factors influence skin healing after burn injuries, e.g., the causes, the degree and size of burn, and the patient’s general condition and types of the graft or materials for covering burn wounds.
Depending on burn severity, the healing process may result in different consequences. Superficial burns recover within two weeks and cause minimal scarring. The re-epithelization of partial thickness burns is ensured by keratinocyte migration from skin dermal appendages within a few hours of the injury. In deeper burns, the healing starts around the edges, but not at the center because of the necessity of rapid wound closure [25–27]. The acceleration of early cell proliferation ensuring the rapid burn healing occurs due to dendritic cells releasing various factors. So, agents enhancing dendritic cells are considered as therapeutics improving burn wound care [28]. Angiogenesis during burn healing is induced by hypoxia-inducible factor 1 [29] and angiogenic cytokines such as VEGF and CXCL12 [30] and ensured by the increase in endothelial progenitor cell blood level correlating with the skin area burnt [30, 31]. The increased contraction is ensured by the activation of the TGF-β pathway that causes remodeling and scar formation [26].
Compared to other wound types, burns may have systemic effects [32, 33], influencing almost all body systems and causing changes in lung, kidney, heart, liver, gastrointestinal tract, bone marrow, and lymphoid organ functioning and multiple organ dysfunction syndrome [32]. At the burn site, inflammatory mediators such as tumor necrosis factor alpha (TNF-α) and interleukins 6, 8, and 1-beta, responsible for systemic effects, are released. Their concentration in serum correlates with the burn surface area. The rise in their concentrations is considered to increase risk of infections, multiple organ dysfunction syndrome, and death [34–36].
Moreover, burn healing is followed by significant immune imbalance [32]. At an early stage, the suppression of bone marrow leads to lymphoid and myeloid immune cell dysfunction, which makes infections resistant to common therapy, and may even cause sepsis. These infectious complications result in wound healing delay [1, 37]. Neutrophils are shown to overexpress heat shock proteins, leading to an increase in oxidative activity and a decrease in apoptosis. Thus, the inflammation phase is prolonged, and the wound site overexposed with growth factors and inflammatory mediators [37–39].
Cell types used in skin regeneration
Cells are the main component of the tissue-engineered skin used for burn therapies (Table 1). They include both stem and somatic cells and can be divided into three main groups: autologous, allogeneic, and xenogeneic. One of the main trends in choosing a cell type for patient treatment is the use of autologous cells as they do not cause immune rejection and their tumorigenicity is low due to the absence of epigenetic manipulations. Nowadays, animal cells are not widely used for skin tissue regeneration, only ECM or its components that they synthesize. Plant stem cells, which are commonly applied in cosmetics, can be interesting as they have no use limitations when compared to animal and human cells. Of course, they cannot be used in skin substitute development as a cell component; but they can provide bioactive substances, which can improve the wound healing process [40].
Table 1.
Somatic and stem cells used in skin tissue regeneration
| Cell types (Refs.) | Origin | Source | CT | Examples of commercial products and their indications |
|---|---|---|---|---|
| Fibroblasts [49–57] | Allogeneic | Skin | Yes | Apligraft - Venous leg ulcers - Diabetic foot ulcers OrCel - Partial-thickness burns |
| Neonatal foreskin | Yes | TransCyte - Full-thickness and deep partial-thickness burns - Partial-thickness burns Dermagraft - Full-thickness diabetic foot ulcers |
||
| Fetus | Yes | ND | ||
| Autologous | Skin | Yes | TissueTech Autograft System - -Diabetic foot ulcers Hyalograft 3D - Diabetic ulcer - Cartilage engineering |
|
| Keratinocytes [55, 56, 58–64] | Allogeneic | Skin | Yes | Apligraft - Venous leg ulcers - Diabetic foot ulcers OrCel - Partial-thickness burns |
| Neonatal foreskin | Yes | Lyphoderm - Chronic venous ulcer - Partial-thickness burns |
||
| Fetus | Yes | ND | ||
| Autologous | Skin | Yes | Epicel - Deep dermal or full thickness burns TissueTech Autograft System - Diabetic foot ulcers Bioseed-S - Chronic venous leg ulcers CellSpray - Partial and deep partial-thickness burns Karocells - Partial and deep partial-thickness burns |
|
| Outer root sheath of scalp hair follicles | Yes | EpiDex - Recalcitrant vascular leg ulcers - Partial-thickness burns |
||
| ESC [65] | Autologous | Epidermis (basal layer) | Yes | ND |
| MMSC [66–71] | Allogeneic | Adipose tissue | Yes | ND |
| Umbilical cord | Yes | ND | ||
| Bone marrow | Yes | ND | ||
| Autologous | Bone marrow | Yes | ND | |
| Adipose tissue | Yes | ND | ||
| Stromal vascular fraction [72] | Autologous | Adipose tissue | Yes | ND |
| BMSC [73–75] | Autologous | Bone marrow | Yes | ND |
| USC [76] and secretome[77] | Autologous or Allogeneic | Urine (kidney) | Yes | ND |
| iPSC [78] | Autologous | Skin | No | ND |
| Vascular progenitor cells [79] | Allogeneic | Vessels | Yes | ND |
| EPC [79, 80] | Allogeneic | Vessels | Yes | ND |
| Mononuclear cells [81] | Autologous | Bone marrow | Yes | ND |
CT cells approved or involved in clinical trials, ND no data available, ESC epidermal stem cells, MMSC multipotent mesenchymal stromal cells, BMSC bone marrow stem cells, USC urine derived stem cells, iPSC induced pluripotent stem cells, EPS endothelial progenitor cells
Fibroblasts and keratinocytes are common cells used in products for wound and burn healing [41]. Keratinocytes are the major cell component of the epidermis and responsible for its stratified structure and form numerous tight intercellular junctions. Fibroblasts are the main cell type of the dermis and produce ECM components and secrete various growth factors (TGF-β), cytokines (TNF-α), and matrix metalloproteinases, which ensure the ECM formation and keratinocyte proliferation and differentiation [16]. Commercial products such as Epicel, Cryoskin, and BioSeed-S contain keratinocytes; Dermagraft, TransCyte and Hyalograft 3D—fibroblasts; and Apligraf, Theraskin, and OrCell—a combination. The use of these cells enables the large-scale production of standardized product batches. However, these materials are mostly non-permanent bioactive dressings, which provide cytokines, ECM, and growth factors for the successful skin reparation [41–43]. Immune rejection is commonly reported with allogeneic fibroblasts and keratinocytes, [44] but this is mostly shown for allogeneic keratinocytes that can be explained by the difference in HLA expression and cytokine production [45]. Fetal fibroblasts are of particular interest because they can significantly improve skin repair due to the high expansion ability, low immunogenicity, and intense secretion of bioactive substances such as basic fibroblast growth factor, vascular endothelial growth factor, and keratinocyte growth factor. However, ethical issues limit their application [46–49].
Epidermal stem cells (ESC) are of particular interest for skin tissue regeneration as they have favorable features such as high proliferation rate and easy access and keep their potency and differentiation potential for long periods [65, 82]. They are one of the skin stem cell types, either heterogeneous or autogenous origins (Table 2). ESC are mostly connected to the process of skin regeneration [17]. They are rare, infrequently divide and generate short-lived and rapidly dividing cells, which are involved in the regeneration process [65]. Their main population, responsible for skin repair, is located in the basal layer of the epidermis; however, they can also be revealed in the base of sebaceous glands and the bulge region of hair follicles [6, 65, 82]. However, while working with ESC culture, we may face progressive aneuploidy or polyploidy and mutation accumulation after several passages. Moreover, as they can be easily derived from the patient’s skin and transplanted to the same patient, ESC are not restricted by ethical issues. Grafts containing autologous holoclones ESC have proven to be effective in treating vast skin defects: epidermolysis, skin and ocular burns, etc. [83, 84].
Table 2.
Subtypes of skin stem cells
| Cell type (Refs) | Localization | Specific markers |
|---|---|---|
| Epidermal stem cells [63, 64, 85, 86] | Basal layer of the epidermis | b1high/melanoma chondroitin sulfate proteoglycan positive, α6high/CD71dim, p63 |
| Melanocyte stem cells [87–89] | Follicle bulge region and hair germ | Dct, Pax3, Sox |
| Follicular stem cells [90–93] | Follicle bulge region | CD34, CD200, K15, K19, Lgr5, Lhx2, NFATC1, NFIB, PHLDA1, Sox9 |
| Hematopoietic stem cells [94] | Follicle dermal papillae | CD34 for lymphoid and hematopoietic progenitor cells |
| Sebaceous gland stem cells [95] | Sebaceous glands and infundibulum | Blimp1 |
| Mesenchymal stem-like cells[96] | Dermis | CD70+, CD90+, CD105+, CD34- |
| Neural progenitor cells [97] | Follicle dermal papillae | S100 for schwannomas, peripheral neural tissue astrocytes; HMB45, a neuraminidase-sensitive oligosaccharide side chain of a glycoconjugate |
Refs references
Mesenchymal stromal cells (MSC) have similar (not identical) features as ESC and can be derived from various tissues, even the skin as mentioned previously [98]. They have a high differentiation potential and a certain degree of plasticity and may generate cells of mesodermal, ectodermal, and endodermal lineages [99]. Moreover, paracrine, trophic, and immunomodulatory MSC properties enable their clinical use [100, 101]. MSC can migrate to the injured tissues, differentiate, and regulate the tissue regeneration by the production of growth factors, cytokines, and chemokines [102]. Their immunomodulatory activity is based on the release of anti-inflammatory cytokines and the inhibition of proliferation of CD4+ and CD8+ natural killer cells, T cells, and B cells. MSC are considered to be hypoimmunogenic because they do not express class I and II molecules of the major histocompatibility complex (MHC) and co-stimulatory proteins (e.g., CD40, CD80, CD86). Therefore, the transplantation of allogenic MSC has a low risk of the immune rejection [103–105]. In burn therapy, adipose-derived stromal cells refined from the stromal vascular fraction are widely applied because of their easy access and isolation procedure and inspiring improvement of the healing processes [106–108]. They are showed to preserve their therapeutic effects after freezing that ensures their multiple use [109]. It is worth mentioning that even the freshly isolated stromal vascular fraction is showed to be effective in burn therapy [110], but compared to adipose-derived stromal cells, it can release high concentrations of inflammatory mediators [111]. However, the number of randomized controlled preclinical and clinical trials remains insufficient [106].
Among the MSC derived from other tissues (adipose tissue, umbilical cord, etc.) the MSC derived from bone marrow (BMSC) requires special attention. They also possess plasticity and can differentiate into tissues of mesodermal, ectodermal, and endodermal origin [112, 113]. BMSC are considered to participate in the skin development. It has been reported that bone marrow can generate not only hematopoietic and mesenchymal cells but also fibroblast-like cells that are located in the dermis and actively proliferate in the skin during the regeneration processes [69, 114, 115]. The possible disadvantages of BMSC are that the tumor microenvironment may induce changes in the angiogenesis ability and anti-tumor response. Moreover, they may generate tumor-associated fibroblasts and shift a normal immune cell phenotype to an immunosuppressive and tumor promoting one [116].
However, nowadays, the greatest interest in tissue regeneration belongs to induced pluripotent stem cells (iPSC); using somatic cell reprogramming like a magic wand, we can develop patient-specific cells with a tailored phenotype and apply them in clinics [117]. The most commonly used cells for cell reprogramming are dermal fibroblasts, melanocytes, and keratinocytes since they can be easily accessed and isolated from punch biopsies [118]. Research has shown that both murine and human iPSC can be differentiated into dermal fibroblasts [119], keratinocytes [120], and melanocytes [121], opening a door for iPSC technology into dermatology applications. The interesting fact is that fibroblasts achieved via this technique may show increased properties compared to those of the parental fibroblasts, e.g., the exceeded ECM production [122]. This might be related to the changed epigenetic signature that occurs during iPSC differentiation and is critical for their use in skin tissue regeneration. However, when cells are reprogrammed with tumorigenic c-Myc and this transgene remains in iPSC, the risk of tumor formation increases, because c-Myc might be reactivated [123]. Since modern methods for cell purification cannot ensure the full separation of differentiated cells from iPSC, undifferentiated and partly differentiated cells may be implanted into a patient and increase the possibility of tumor formation [124].
Growth factor therapy
Growth factor therapy is to administrate pro-epidermal growth factors to promote wound healing. These growth factors are bioactive molecules secreted by the body whose function is to stimulate the growth and propagation of cells involved in skin wound healing and inflammation. The use of extra-growth factor increases the number of wound-healing cells, causing faster wound healing. Despite their variety, there are five types commonly used as invigorating molecules in wound healing and regaining via benign tissue repair processes (Table 3). They include compounds influencing epidermal tissue regrowth (epidermal growth factor (EGF); hepatocyte growth factor (HGF)), anti-scarring (transforming growth factor (TGF-ß3)), pro-angiogenesis (vascular endothelial growth factor (VEFG); platelet-derived growth factor (PDGF)), and stromal cell growth (fibroblast growth factor (FGF)). A combination of multiple growth factors may efficiently improve cellular functions: proliferation, migration, differentiation, collagen remodeling, inhibition of fibroblast overgrowth, ECM deposition, etc. Therefore, strategies to control growth factors release may prompt skin tissue regeneration. To optimize substance delivery and loading, bioactivity, therapeutic functionality, dosage form stability, etc., it is vital to develop platforms such as hydrogels, microbeads, or tissue-engineered constructs.
Table 3.
Growth factor therapy for skin tissue repair
| GFs (Refs) | Delivery approach | Dose | In vivo experiment | Outcomes |
|---|---|---|---|---|
| EGF [125, 126] | Topically HA-EGF conjugate immobilized within HA films |
1 μg per patch once | SD rat (full-thickness dorsal skin excision) | - Being secreted by the platelets and macrophages; - Stimulating proliferation of fibroblasts, the cells that produce collagen; - Reducing the healing time of wounds when applied topically |
| Topically rhEGF-loaded lipid nanoparticles |
20 μg per scar tissue twice a week | White pig (full-thickness dorsal skin excision) | ||
| KGF [127] | Topically KGF covalently attached to a fluorescent matrix-binding peptide encapsulated within fibrin |
500 ng/ml | Athymic mouse (full-thickness dorsal skin excision) | - Promotes keratinocytes growth |
| TGF-β1 [128] | Topically Incorporated into polyoxamer gel |
1 μg per wound | SD rat (full-thickness skin excision) | - Stimulating growth and migration of keratinocytes and fibroblasts to the affected area - Promoting the growth of new blood vessels (angiogenesis), ensuring adequate blood supply to the healing wound |
| TGF-β2 [129] | Subcutaneous implantation Gelatin microspheres |
0.5 μg per implant | Athymic rat (subcutaneous implantation) | |
| HGF [130] | Subcutaneous injection | 2 mg per scar tissue once | Rabbit (full-thickness skin excision) | - Reducing scarring |
| VEGF [131] | Implantation VEGF-loaded alginate microspheres |
2 and 4 μg | Wistar rat (small incision in the groin) | - Enabling the most extensive blood vessel formation with microspheres containing 4 μg of VEGF |
| PDGF Regranex® [132] |
Topically Carboxymethyl-cellulose hydrogel |
100 μg/g | Patients with type 1 or type 2 diabetes suffering from chronic ulcers | - Being secreted by the platelets, - Attracting fibroblasts and macrophages to the area of injured tissue |
| TGF-β3 [133] | Topically BMSC overexpressing TGF-β3 |
0.5 ml (1.3 × 105 cells/ml) | Rabbit (full-thickness skin excision) | - Reducing scar depth and density |
| bFGF [134] | Topically Poly(ethylene glycol)-poly(dl-lactide) microfibrous mats containing bFGF | ND | Diabetic SD rat (full-thickness dorsal skin excision) | - Enabling higher complete wound closure rate - Stimulating collagen deposition and ECM remodeling bFGF-loaded mats |
| HGF+bFGF [135] | Topically Collagen/gelatin sponge |
10 μg/cm2 + 7 μg/cm2 | C57BL/6JJcl mouse (full-thickness dorsal skin excision) | - Dual release of HGFC and bFGF ensured re-epithelization and angiogenesis. |
| Platelet-rich fibrin extract [136] | Topically Gelatin gel |
3.3 ml of blood per defect | Wistar rat (full-thickness dorsal skin excision) | - Promoting neovascularization and formation of granulation tissue. - Epidermalization started in 1 week |
| VEGF+PDGF+ bFGF+EGF [137] |
Topically Collagen-HA membrane |
0.1 μg/mg (each) | Diabetic SD rat (full-thickness dorsal skin excision) | - Increasing wound healing rate - Enhancing the collagen deposition and maturation of vessels. |
GFs growth factors, EGF epidermal growth factor, KGF keratynocyte growth factor, HGF hepatocyte growth factor, VEGF vascular endothelial growth factor, PDGF platelet-derived growth factor, TGF transforming growth factor, FGF fibroblast growth factor, bFGF basic FGF, HA hyaluronic acid, ND no data available, Refs references, wk week
To improve re-epithelialization after a burn injury, growth factors such as EGF and HGF are applied. EGF and HGF are shown to enhance epithelial cell proliferation, growth, and migration. Their potential in skin tissue regeneration is intensively studied, and various approaches to deliver them are under investigation (Table 3). For example, Lee at al. [138] achieved the improved wound healing of laser-induced burn after treatment with recombinant EGF conjugated with low molecular weight protamine. Regarding HGF, there are few in vivo studies [130, 139, 140]. The EGF efficacy was proven in clinical trials [141, 142].
Angiogenesis in a defect site can be promoted by PDGF and VEGF. PDGF-BB is approved by FDA for diabetic ulcer treatment [143], but it has low success in clinics probably due to its damage by proteolytic enzymes or low expression of PDGF-receptors. VEGF showed high efficacy in experiments in vivo (e.g., [144]) and passed a phase I trial proving its safety and efficacy in treatment of chronic wounds [145]. To promote vessel formation, both PDGF and VEGF require constant application during a treatment period that has induced research to develop delivery systems with sustained release. For instance, Tan et al. [146] revealed VEGF-loaded collagen scaffolds significantly improved the wound healing processes in diabetic rats followed by the increase in VEGF level in tissue and induced angiogenesis. Moreover, Gorkun et al. [147] showed that VEGF-induced spheroids from adipose-derived stromal cells encapsulated within modified fibrin gel can form tubule-like network that might be interesting as a new approach to enhance angiogenesis in a wound and improve skin tissue regeneration.
The increased stromal cell growth can be achieved by the application of FGF. FGF-2 (bFGF) was shown to control ECM formation, and its use enabled the decreased scar formation and inhibition of TGF-β1/SMAD-dependent pathway [148]. Treating deep partial-thickness burns in humans, Ma et al. revealed that recombinant aFGF accelerated the healing rate and the healing process required less time.
The main anti-scarring agent is TGF-ß3. In TGF family, TGF-β1 and TGF-β2 stimulate fibroblast differentiation, contraction, ECM synthesis and deposition, and scarring and TGF-β3 enables the reduction in scar formation. The concentration of TGF-β isoforms varies in the fetal and adult wound healing process; in the first, the TGF- β 3 concentration is high, but TGF-β1 and TGF-β2 isoforms are absent or in a small amount, while in the second, the situation is opposite and the high TGF-β1 and TGF-β2 concentrations are caused by the platelet degranulation and synthesis in monocytes during inflammation. When TGF-β1 and TGF-β2 isoforms were blocked and TGF-β3 isoform was externally added, the wound healing occurred with the less remarkable scar formation than that in control. However, blocking all three isoforms did not ensure the scarring decrease that the complexity of molecular pathways shows [149–151]. Clinical trials showed that avotermin (TGF-β3) ensured scar reduction and was well tolerated [152–154].
Growth factors for skin wounds are often applied locally (topically). One advantage of growth factor therapy is that it uses the body’s own cells to promote healing. Its use may also speed up the time it takes for wounds to heal, resulting in a greater reduction of disability or discomfort for the patient. Various delivery systems are offered to ensure growth factor stability and controlled release in wounds: particulate systems, scaffolds, hydrogels, and their combinations (described in [155]). Moreover, devices such as microneedles [156] and jet injectors [157] are of potential interest although to date no studies where they have been applied to treat burns were found.
Since it is often applied topically, the incidence of systemic side effects is minimal. However, for example, high VEGF serum level causes anasacra, edema, and edema-associated burn complications although, in general, VEGF is considered to promote burn healing [158]. EGF and PDGF can lead to the hypertrophic scarring [159]. Also, theoretically, growth factor therapy of wounds may induce oncogenesis (for instance, TGF-β can be both a pro-oncogenic and tumor suppressing factor [160], and VEGF is involved in tumor formation [161]), but in pre-clinical and clinical trials, tumor development was not revealed [162, 163]. Further long-term trials are required to confirm and strengthen growth factors safety.
In some cases, the use of a single growth factor may be insufficient because of the complexity of molecular pathways and wound chronicity that reveals a need to develop multiple growth factor systems with sustained release. For example, Lai et al. [137] designed a collagen-HA membrane with immobilized VEGF, PDGF, bFGF, and EGF and showed that it efficiently induced the increase in wound healing rate by enhancing collagen deposition and neovasculogenesis compared to the control group.
Scaffold for skin wound healing
Biomaterials are a crucial part of the different dressings and tissue-engineered constructs (Table 4) used in burn therapy. The main idea in using them is to imitate the skin ECM formed by collagen, elastin, proteoglycans, nidogen, laminin, and perlecan [20, 21] and its properties: the skin’s strength is enabled by collagen, elastin ensures its elasticity and flexibility, and proteoglycans provide hydration and viscosity [20]. In skin grafts and substitutes, biomaterials of various origins (natural, synthetic, or semi-synthetic) are used and their choice in the scaffold fabrication is essential because this can influence the in situ regeneration, with their features regulating cell behavior and enabling new tissue formation. The main requirements are biodegradability, temporary mechanical support, and permeability. Depending on the approach, scaffolds may be with or without cells, and the latter can be divided into dermal, epidermal, and epidermal-dermal composites [41].
Table 4.
Scaffolds applied in the skin tissue regeneration and wound healing
| Scaffolds (Refs) | Origin | BD | Cell component | CA | Example of commercial products |
|---|---|---|---|---|---|
| Decellularized material-based | |||||
| Small intestine, acellular lyophilized [164] | Porcine | Yes | Not included | Yes | OASIS Wound Matrix |
| Dermis, acellular lyophilized [165, 166] | Allogeneic | Yes | Not included | Yes | AlloDerm, Karoderm, SureDerm |
| Dermis, acellular pre-meshed [167] | Allogeneic | Yes | Not included | Yes | GraftJacket |
| Dermis, acellular lyophilized, coated with elastin hydrolysate [166] | Bovine | Yes | Not included | Yes | Matriderm |
| Dermis, acellular diisocyanate cross-linked [168, 169] | Porcine | Yes | Not included | Yes | Permacol Surgical Implant |
| Collagen-based scaffolds | |||||
| Collagen [50, 58, 60] | Bovine | Yes | Allogeneic keratinocytes and fibroblasts | Yes | Apligraft |
| Autologous keratinocytes and fibroblasts | Yes | PermaDerm | |||
| Collagen, aldehyde cross-linked reconstituted [170] | Porcine | Yes | Not included | Yes | EZ Derm |
| Collagen, sponge [52] | Bovine | Yes | Allogeneic keratinocytes and fibroblasts | Yes | OrCel |
| Collagen, cross-linked Glycosaminoglycan Polysiloxane [171] |
Bovine/synthetic | Yes/no | Not included | Yes | Integra Dermal Regeneration |
| Collagen, cross-linked Glycosaminoglycan Polysiloxane [70] |
Bovine/synthetic | Yes/no | Autologous adipose-derived regenerative cells | No | ND |
| Collagen, lyophilized cross-linked sponge, heat-denatured Silicone [172, 173] |
Bovine/synthetic | Yes/no | Not included | Yes | Terudermis |
| Atelocollagen Silicone/silicone fortified with silicone gaze TREX [172, 174] |
Porcine/synthetic | Yes/no | Not included | Yes | Pelnac Standard/Pelnac Fortified |
| Collagen Silicone, film Nylon, mesh [53, 175] |
Porcine/synthetic | Yes/no | Allogeneic fibroblasts | Yes | Biobrane/Biobrane-L, TransCyte |
| Hyaluronic acid-based | |||||
| Hyaluronic acid membrane (microperforated) [56, 57, 176] | Recombinant | Yes | Autologous keratinocytes and fibroblasts | Yes | TissueTech Autograft System, LaserSkin (Vivoderm) |
| Allogeneic | Yes | Autologous fibroblasts | Yes | Hyalograft 3D | |
| HYAFF, derivative of hyaluronan Silicone, membrane [177] |
Allogeneic/synthetic | Yes/no | Not included | Yes | Hyalomatrix PA |
| Other biopolymer-based | |||||
| Silk fibroin/alginate, sponge [178] | Xenogeneic/synthetic | Yes/no | Not included | No | ND |
| Cellulose, nanofibrils [179, 180] | Recombinant | No | Not included | No | ND |
| Synthetic material-based | |||||
| Polyethylene oxide terephthalate/Polybutylene terephthalate [55] | Synthetic | No | Autologous keratinocytes and fibroblasts | Yes | PolyActive |
| Polyglycolic acid/polylactic acid Extracellular matrix, derived from fibroblasts [54, 181] |
Synthetic | Yes | Allogeneic fibroblasts | Yes | Dermagraft |
BD biodegradability, CA commercial availability, ND no data available
To date, most products available on the world market contain collagen or decellularized tissues (Table 4). This is not surprising because one of the main skin component is collagen types I and III, and therefore, the product design will be more similar to the native tissue than others [139]. However, collagen possesses poor mechanical properties, and most scientists and manufacturers try to improve them via cross-linking or reinforcing with synthetic materials such as polylactide, polycaprolactone, and their copolymers [182, 183]. For instance, in TranCyte, the collagen gel is fortified with nylon mesh and covered with a silicone film; the latter enables the maintenance of moist environment. The products based on decellularized materials have more clinical limitations than collagen-based scaffolds mainly because they require specific raw materials (especially, allogeneic) and can evoke the strong immune response and calcification (especially, xenogeneic). What is remarkable is that the first FDA-approved skin substitute, Apligraf, contains bovine collagen [87].
It is worth mentioning that hydrogel has proven to provide the most favorable conditions for the burn healing process and is widely applied in tissue engineering [184]. The abovementioned collagen is also a gel, and apart from collagen, gels such as fibrin, hyaluronic acid, chitosan, and alginate are used in the skin substitute and bio-ink production (Table 5). The structure and properties of hydrogels (3D network, hydrophilicity, etc.) can be easily modified and are similar to those of the native ECM, enabling not only cell proliferation and differentiation but also in situ cell recruitment. Gels provide adequate moist environment that is favorable for the burn healing process [185]. Moreover, they can deposit and deliver bioactive compounds, which then enhance the healing process [186–190].
Table 5.
Hydrogels for cell and growth factor delivery in the skin tissue regeneration
| Polymer type | Hydrogels (Refs) | Origin | BD | CA | FDA approved | Commercial product |
|---|---|---|---|---|---|---|
| Protein | Collagen [58] | Xenogeneic | Yes | Yes | Yes | Apligraf |
| Gelatin [191, 192] | Xenogeneic | Yes | Yes | No | ND | |
| Fibrin [193] | Allogeneic | Yes | Yes | No | AcuDress | |
| Polysaccharide | Chitosan [194] | Xenogeneic | No | Yes | No | ND |
| Hyaluronic acid [176] | Recombinant, allogeneic | Yes | Yes | Yes | LaserSkin | |
| Dextran [195, 196] | Xenogeneic (microbial) | Yes | Yes | No | ND | |
| Alginate [197] | Xenogeneic | No | Yes | Yes | Kaltostat | |
| Glycosaminoglycan [198] | Xenogeneic, allogeneic | Yes | Yes | No | ND | |
| Polyether | Polyethylene glycol diacrylate [199, 200] | Synthetic | No | Yes | No | ND |
BD biodegradability, CA commercial availability, ND no data available, FDA Food and Drug Administration
Delivery approaches
Currently, dressings are the most common form of cell-based products used in burn therapy [41]. Their shape, however, does not provide a possibility to treat large and complex wounds with a heterogeneous surface profile. Therefore, such technologies as cell spraying and three-dimensional (3D) bioprinting were developed for these applications.
3D bioprinting is a multitasking platform that enables in situ cell deposition according to the wound pattern. In 3D bioprinting, cells are distributed within gels, and these mixtures are used as bio-inks. Commonly, the procedure involves printing hydrogel layers, which are further cross-linked via UV, enzymes, ions, etc., to give better support for cells [201–203].
In situ 3D bioprinting was first proposed by Campbell and Weiss [204] for an inkjet bioprinter and is particularly interesting as a delivery approach since it can ensure the full-thickness tissue restoration followed by vasculogenesis due to progenitor cell migration and angiogenesis. Nevertheless, despite promising results, the number of studies, where this technology is used, is limited [205]. This may be caused by the complexity of the equipment and commercial non-availability. For skin tissue applications, there are only two studies performed with human fibroblasts and keratinocytes [205] and amniotic fluid-derived stem cells [206] encapsulated within fibrin-collagen hydrogel and transplanted into a full-thickness wound in nude mice. Thus, after solving technical issues the idea of in situ skin bioprinting could be considered attractive for clinical translation.
Another promising delivery technology is cell spraying that allows clinicians to treat large deep burns [61, 207, 208]. In most studies, scientists used autologous epidermis-derived cells. Cells are not cultured but suspended in saline. The required amount can be derived only from a small donor site [61, 109]. A cell suspension is sprayed homogenously onto a wound so that cells proliferate and improve re-epithelialization [109]. Cell spraying cannot replace common autografting but can be applied easily and early to deep partial thickness burns [208]. Many complications (poor esthetic outcome, hypertrophic scarring, contracture, etc.) may be avoided or decreased due to the early re-epithelialization after a cell spray. Nevertheless, this technology is expensive and needs special equipment, aseptic rooms, and highly qualified personnel as 3D bioprinting.
Challenges and future directions
To date, despite imperfections, the existing dressings and tissue-engineered skin substitutes have significantly improved clinical insight into burn treatment, allowing clinicians to treat severe cases that increase patients’ survival rates and quality of life [42, 43, 209, 210]. Most of them only aim to temporarily protect the denuded tissue from the aggressive environment and provide cytokines and growth factors to enhance the wound healing process [43]. There is no doubt that commercial products based on autologous cells (fibroblasts and keratinocytes) are close to the native skin and enable the successful skin repair but they cannot fully replace the injured tissue [211].
Many issues limit the introduction and rapid expansion of new products for cell-based therapies. First of all, their production is time- and labor-consuming and requires complex and specific equipment. To cover the extensive burn areas, a huge number of cells is needed, and if they are not autologous or hypoimmunogenic, a substitute can be rejected. These products should be transported and stored under certain conditions, which are hard to maintain, and their shelf-life is short. When autologous cells are applied, the work of cell culture facilities and surgeons should be well coordinated [212]. Moreover, the cost of treatment with skin substitutes is high but the only one function, protective, can be replaced with them [209]: all these tissue-engineered constructs cannot restore thermoregulation, sensation, UV-protection, excretion, perspiration, etc.
Nowadays, in the design of skin substitute, there are three main approaches: cell-based, biomaterial-based, and delivery-based. In the first, scientists try to fabricate skin equivalents using not only fibroblasts and keratinocytes, but also melanocytes and endothelial cells in order to imitate native tissue morphology [213–215]. In many studies, stem cells derived from various sources are used for their properties such as hypo-immunogenicity and high differentiation potential. The use of autologous and allogeneic cells still remains questionable. Although there are studies showing that only autologous cells can promote rapid wound healing [107, 216], a bank of allogeneic cells can provide a possibility to treat quickly patients suffering extensive and deep second-degree burns, and in this case, the most preferable cells are stem cells (e.g., adipose-derived or bone-marrow derived stem cells) possessing hypo-immunogenicity. Moreover, attempts to reproduce skin appendages (for instance, hair follicles and sebaceous glands) in vitro and integrated into skin substitutes [217–219] are made. The second approach tries to functionalize scaffolds with different methods. For example, the immobilization of signaling molecules on their surface can promote the cell proliferation and differentiation and control cell-matrix adhesion [220–223]. According to the third approach, researchers try to develop a new delivery system or to improve the existing ones. To ensure burn healing, cells can be injected intravenously [108], or, more often, they are immobilized on various materials and applied topically as dressings. For sure, dressings are the most common system, but they cannot be precisely adjusted to the wound surface profile. Therefore, technologies such as cell spray and bio-printing are of particular interest and are able to solve this issue [205–208].
Moreover, the stem cells described above can enable true skin regeneration and decrease scar formation and have the clear manipulation step procedure for autologous use (Fig. 1). Preclinical and clinical studies have shown that bone marrow, urine, adipose-derived, and other stem cells can significantly improve the wound healing process in chronic wounds [51, 76, 187, 224, 225]. However, despite these successful results, still FDA has not approved any stem cell-based skin substitute for wound treatment, and for them to make the approval, certain points such as optimal cell type and population and time and way of administration should be clarified. There is an essential need to find out the mechanisms of cell action, survival, and incorporation after transplantation and their stability and differentiation features in the wound microenvironment. Moreover, the delayed postoperative outcomes should be studied in large-scale clinical trials to prove the safety of stem cell-based products. Thus, stem cells are a promising tool for skin substitute design and fabrication for advanced burn therapies.
Fig. 1.
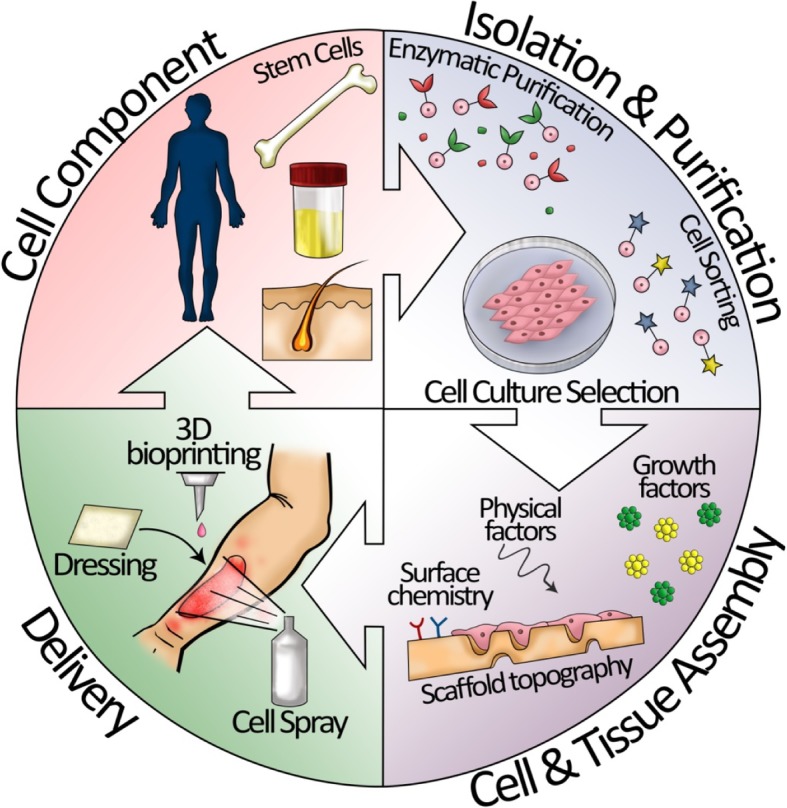
Procedure of autologous stem cell-based therapy on burn injury
As the number of findings proving its safety and efficacy is growing, cell-based therapy is becoming a great alternative in burn care. However, some essential points required to standardize all related procedures and prepare guidelines for clinicians are still unclear. In most studies, cells and cell-based products are applied once topically, but these measures can be insufficient in case of extensive burns causing systemic inflammation and hypohydration and only intravenous injections of cells can improve the patient’s condition. Autologous cells are considered to be preferable although their use is impossible in large burns because of the lack of donor sites and time. Moreover, especially in case of acute burns, the successful outcomes of cell-based therapy depend on intervention timing defined by coordination between clinicians and cell facilities staff. Thus, despite outstanding results of cell applications in burn care, the mentioned above issues should be solved to exploit the whole potential of cell-based therapy.
Acknowledgements
The authors would like to thank Anna Shpichka for drawing Fig. 1.
Funding
This work was supported by the Russian Science Foundation 18-15-00401 (description of cell-based products) and Russian academic excellence project 5-100 (discussion of challenges and future prospects).
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- 3D
Three-dimensional
- BD
Biodegradability
- bFGF
Basic fibroblast growth factor
- BMSC
Bone marrow stem cells
- CA
Commercial availability
- CT
Clinical trials
- ECM
Extracellular matrix
- EGF
Epidermal growth factor
- EPS
Endothelial progenitor cells
- ESC
Epidermal stem cells
- FDA
Food and Drug Administration
- FGF
Fibroblast growth factor
- GFs
Growth factors
- HA
Hyaluronic acid
- HGF
Hepatocyte growth factor
- HLA
Human leukocyte antigen
- iPSC
Induced pluripotent stem cells
- KGF
Keratinocyte growth factor
- MHC
Major histocompatibility complex
- MMSC
Multipotent mesenchymal stromal cells
- MSC
Mesenchymal stromal cells
- ND
No data available
- PDGF
Platelet-derived growth factor
- Refs
References
- TGF
Transforming growth factor
- TNF-α
Tumor necrosis factor alpha
- USC
Urine-derived stem cells
- VEGF
Vascular endothelial growth factor
Authors’ contributions
AS, YZ, and PT outlined the review. AS wrote the sections “Cell types used in skin regeneration” and “Scaffold for skin wound healing”; DB, the sections “Introduction” and “Skin tissue regeneration processes”; AA, the section “Delivery approaches”; YZ, the section “Growth factor therapy challenges”; and PT, the section “Challenges and future directions”. EB prepared Tables 1 and 4; RS, Tables 2 and 3; and VB, Table 5. AS, VB, YZ, and PT designed Fig. 1. AS drafted the manuscript with primary editing and revision support from AA, YZ, VB, and PT. PT and YZ coordinated the manuscript preparation. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Anastasia Shpichka, Email: ana-shpichka@yandex.ru.
Denis Butnaru, Email: butnaru_dv@mail.ru.
Evgeny A. Bezrukov, Email: eabezrukov@rambler.ru
Roman B. Sukhanov, Email: rb_suhanov@mail.ru
Anthony Atala, Email: aatala@wakehealth.edu.
Vitaliy Burdukovskii, Email: burdvit@mail.ru.
Yuanyuan Zhang, Email: fyyzhang2016@gmail.com.
Peter Timashev, Email: timashev.peter@gmail.com.
References
- 1.Church D, Elsayed S, Reid O, Winston B, Lindsay R. Burn wound infections 2006;19:403–434. [DOI] [PMC free article] [PubMed]
- 2.Atiyeh BS, Costagliola M. Cultured epithelial autograft (CEA) in burn treatment: three decades later. Burns. 2007;33:405–413. doi: 10.1016/j.burns.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Wood FM, Kolybaba ML, Allen P. The use of cultured epithelial autograft in the treatment of major burn injuries: a critical review of the literature. Burns. 2006;32:395–401. doi: 10.1016/j.burns.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Nejati R, Kovacic D, Slominski A. Neuro-immune-endocrine functions of the skin: An overview. Expert Rev Dermatol. 2013;8:581–583. doi: 10.1586/17469872.2013.856690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mathes SH, Ruffner H, Graf-Hausner U. The use of skin models in drug development. Adv Drug Deliv Rev. 2014;69–70:81–102. doi: 10.1016/j.addr.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Fuchs E. Skin stem cells: rising to the surface. J Cell Biol. 2008;180:273–284. doi: 10.1083/jcb.200708185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arda O, Göksügür N, Tüzün Y. Basic histological structure and functions of facial skin. Clin Dermatol. 2014;32:3–13. doi: 10.1016/j.clindermatol.2013.05.021. [DOI] [PubMed] [Google Scholar]
- 8.Strong AL, Neumeister MW, Levi B. Stem cells and tissue engineering: regeneration of the skin and its contents. Clin Plast Surg. 2017;44:635–650. doi: 10.1016/j.cps.2017.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rousselle P, Braye F, Dayan G. Re-epithelialization of adult skin wounds: cellular mechanisms and therapeutic strategies. Adv Drug Deliv Rev. 2018. 10.1016/j.addr.2018.06.019. [DOI] [PubMed]
- 10.Ishida-Yamamoto A, Igawa S, Kishibe M. Molecular basis of the skin barrier structures revealed by electron microscopy. Exp Dermatol. 2018:0–2. 10.1111/exd.13674. [DOI] [PubMed]
- 11.Han X, Bibb R, Harris R. Design of bifurcation junctions in artificial vascular vessels additively manufactured for skin tissue engineering. J Vis Lang Comput. 2015;28:238–249. doi: 10.1016/j.jvlc.2014.12.005. [DOI] [Google Scholar]
- 12.Pozzi A, Yurchenco PD, Iozzo RV. The nature and biology of basement membranes. Matrix Biol. 2017;57–58:1–11. doi: 10.1016/j.matbio.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kruegel J, Miosge N. Basement membrane components are key players in specialized extracellular matrices. Cell Mol Life Sci. 2010;67:2879–2895. doi: 10.1007/s00018-010-0367-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caley MP, Martins VLC, O’Toole EA. Metalloproteinases and wound healing. Adv Wound Care. 2015;4:225–234. doi: 10.1089/wound.2014.0581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vu TH, Werb Z. Matrix metalloproteinases: effectors of development and normal physiology. Genes Dev. 2000;14:2123–2133. doi: 10.1101/gad.815400. [DOI] [PubMed] [Google Scholar]
- 16.Wang JHC, Thampatty BP, Lin JS, Im HJ. Mechanoregulation of gene expression in fibroblasts. Gene. 2007;391:1–15. doi: 10.1016/j.gene.2007.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cerqueira MT, Pirraco RP, Marques AP. Stem cells in skin wound healing: are we there yet? Adv Wound Care. 2016;5:164–175. doi: 10.1089/wound.2014.0607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vary JC. Selected disorders of skin appendages-acne, alopecia, hyperhidrosis. Med Clin North Am. 2015;99:1195–1211. doi: 10.1016/j.mcna.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 19.Niemann C, Horsley V. Development and homeostasis of the sebaceous gland. Semin Cell Dev Biol. 2012;23:928–936. doi: 10.1016/j.semcdb.2012.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu C, Fuchs E. Sweat gland progenitors in development, homeostasis, and wound repair. Cold Spring Harb Perspect Med. 2014;4(2):a015222. [DOI] [PMC free article] [PubMed]
- 21.Mikkola ML, Millar SE. The mammary bud as a skin appendage: unique and shared aspects of development. J Mammary Gland Biol Neoplasia. 2006;11:187–203. doi: 10.1007/s10911-006-9029-x. [DOI] [PubMed] [Google Scholar]
- 22.Chu GY, Chen YF, Chen HY, Chan MH, Gau CS, Weng SM. Stem cell therapy on skin: mechanisms, recent advances and drug reviewing issues. J Food Drug Anal. 2017:1–7. 10.1016/j.jfda.2017.10.004. [DOI] [PMC free article] [PubMed]
- 23.Hermans MHE. A general overview of burn care. 2005. p. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lorenti A. Wound healing: from epidermis culture to tissue engineering 2012;2012:17–29.
- 25.Wolfram D, Tzankov A, Pulzi P, Piza-Katzer H. Hypertrophic scars and keloids—a review of their pathophysiology, risk factors, and therapeutic management. Dermatol Surg. 2009;35:171–181. doi: 10.1111/j.1524-4725.2008.34406.x. [DOI] [PubMed] [Google Scholar]
- 26.Sakallioglu EA, Basaran O, Ozdemir BH, Arat Z, Yucel M, Haberal M. Local and systemic interactions related to serum transforming growth factor- b levels in burn wounds of various depths. Burns. 2006;32:980–985. doi: 10.1016/j.burns.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 27.Wilgus TA, Ferreira AM, Oberyszyn TM, Bergdall VK, Dipietro LA. Regulation of scar formation by vascular endothelial growth factor. Lab Investig. 2008;88:579–590. doi: 10.1038/labinvest.2008.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vinish M, Cui W, Stafford E, Bae L, Hawkins H, Cox R, et al. Dendritic cells modulate burn wound healing by enhancing early proliferation. Wound Repair Regen. 2016;24:6–13. doi: 10.1111/wrr.12388. [DOI] [PubMed] [Google Scholar]
- 29.Zhang X, Liu L, Wei X, Tan YS, Tong L, Chang R. Impaired angiogenesis and mobilization of circulating angiogenic cells in HIF-1α heterozygous-null mice after burn wounding. Wound Repair Regen. 2014;18:193–201. doi: 10.1111/j.1524-475X.2010.00570.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fox A, Smythe J, Fisher N, Tyler MPH, Mcgrouther DA, Watt SM, et al. Mobilization of endothelial progenitor cells into the circulation in burned patients. Br J Surg. 2008;95:244–251. doi: 10.1002/bjs.5913. [DOI] [PubMed] [Google Scholar]
- 31.Foresta C, Schipilliti M, De Toni L, Magagna S, Lancerotto L, Azzena B, et al. Blood levels, apoptosis, and homing of the endothelial progenitor cells after skin burns and escharectomy. J TRAUMA Inj Infect Crit Care. 2011;70:459–465. doi: 10.1097/TA.0b013e3181fcf83c. [DOI] [PubMed] [Google Scholar]
- 32.Sarrazy V, Billet F, Micallef L, Coulomb B, Desmoulie A. Mechanisms of pathological scarring: role of myofibroblasts and current developments. Wound Repair Regen. 2011;19:10–15. doi: 10.1111/j.1524-475X.2011.00708.x. [DOI] [PubMed] [Google Scholar]
- 33.Atiyeh BS, Hayek SN, Gunn SW. New technologies for burn wound closure and healing - review of the literature. Burns. 2005;31:944–956. doi: 10.1016/j.burns.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 34.Van De Water L, Varney S. Mechanoregulation of the myofibroblast in wound contraction, scarring, and fibrosis : opportunities for new therapeutic intervention. Adv Wound Care. 2013;2:122–141. doi: 10.1089/wound.2012.0393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ghieh F, Jurjus R, Ibrahim A, Geagea AG, Daouk H, El BB, et al. The use of stem cells in burn wound healing: a review. Biomed Mater. 2015;2015:684084. doi: 10.1155/2015/684084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rowan MP, Cancio LC, Elster EA, Burmeister DM, Rose LF, Natesan S, et al. Burn wound healing and treatment: review and advancements. Crit Care. 2015:1–12. 10.1186/s13054-015-0961-2. [DOI] [PMC free article] [PubMed]
- 37.Hampson P, Dinsdale ÃRJ, Wearn ÃCM, Bamford AL, Bishop ÃJRB, Hazeldine J, et al. Neutrophil dysfunction, immature granulocytes, and cell-free: a prospective observational cohort study. 2016;XX X. [DOI] [PubMed]
- 38.Dunn JLM, Hunter RA, Cairns BA, Kartchner LB, Thurlow L, Maile R, et al. Mammalian target of rapamycin regulates a hyperresponsive state in pulmonary neutrophils late after burn injury. J Leukoc Biol. 2016;2018:1–10. doi: 10.1002/JLB.3AB0616-251RRR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaufman T, Magosevich D, Moreno MC, Guzman MA, Atri LPD, Carestia A, et al. Nucleosomes and neutrophil extracellular traps in septic and burn patients. Clin Immunol. 2017;183:254–262. doi: 10.1016/j.clim.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 40.Trehan S. Plant stem cells in cosmetics : current trends and future directions. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shevchenko RV, James SL, James SE. A review of tissue-engineered skin bioconstructs available for skin reconstruction. J R Soc Interface. 2010;7:229–258. doi: 10.1098/rsif.2009.0403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boateng JS, Matthews KH, Stevens HNE, Eccleston GM. Wound healing dressings and drug delivery systems: A review. J Pharm Sci. 2008;97:2892–2923. doi: 10.1002/jps.21210. [DOI] [PubMed] [Google Scholar]
- 43.Boateng J, Catanzano O. Advanced therapeutic dressings for effective wound healing - a review. J Pharm Sci. 2015;104:3653–3680. doi: 10.1002/jps.24610. [DOI] [PubMed] [Google Scholar]
- 44.Clark RAF, Ghosh K, Tonnesen MG. Tissue engineering for cutaneous wounds. J Invest Dermatol. 2007;127:1018–1029. doi: 10.1038/sj.jid.5700715. [DOI] [PubMed] [Google Scholar]
- 45.Ohyama H, Nishimura F, Meguro M, Takashiba S, Murayama Y, Matsushita S. Counter-antigen presentation: fibroblasts produce cytokines by signalling through HLA class II molecules without inducing T-cell proliferation. Cytokine. 2002;17:175–181. doi: 10.1006/cyto.2001.0976. [DOI] [PubMed] [Google Scholar]
- 46.Lim R. Fetal membranes in regenerative medicine : new tricks from an old dog ? Stem Cells Transl Med. 2017;6(9):1767–76. [DOI] [PMC free article] [PubMed]
- 47.Li M, Zhao Y, Hao H, Han W, Fu X. Theoretical and practical aspects of using fetal fibroblasts for skin regeneration. Ageing Res Rev. 2017;36:32–41. doi: 10.1016/j.arr.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 48.Parekh A, Hebda PA. The contractile phenotype of dermal fetal fibroblasts in scarless wound healing. Curr Pathobiol Rep. 2017. 10.1007/s40139-017-0149-3. [DOI] [PMC free article] [PubMed]
- 49.Taghiabadi E, Beiki B, Aghdami N, Bajouri A. Amniotic membrane seeded fetal fibroblasts as skin substitute for wound regeneration. Methods Mol Biol. 2018;8:1–9. [DOI] [PubMed]
- 50.Karr JC. Retrospective comparison of diabetic foot ulcer and venous stasis ulcer healing outcome between a dermal repair scaffold (PriMatrix) and a bilayered living cell therapy (Apligraf) Adv Skin Wound Care. 2011;24:119–125. doi: 10.1097/01.ASW.0000395038.28398.88. [DOI] [PubMed] [Google Scholar]
- 51.Jadlowiec C, Brenes RA, Li X, Lv W, Protack CD, Collins MJ, et al. Stem cell therapy for critical limb ischemia: What can we learn from cell therapy for chronic wounds? Vascular. 2012;20:284–289. doi: 10.1258/vasc.2011.201206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Still J, Glat P, Silverstein P, Griswold J, Mozingo D. The use of a collagen sponge/living cell composite material to treat donor sites in burn patients. Burns. 2003;29:837–841. doi: 10.1016/s0305-4179(03)00164-5. [DOI] [PubMed] [Google Scholar]
- 53.Noordenbos J, Doré C, Hansbrough JF. Safety and efficacy of TransCyte for the treatment of partial-thickness burns. J Burn Care Rehabil. 1999;20:275–281. doi: 10.1097/00004630-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 54.Purdue GF, Hunt JL, Still JMJ, Law EJ, Herndon DN, Goldfarb W, et al. A multicenter clinical trial of a biosynthetic skin replacement, dermagraft-TC, compared with cryopreserved human cadaver skin for temporary coverage of excised burn wounds. J Burn Care Rehabil. 1997;18:52–57. doi: 10.1097/00004630-199701000-00009. [DOI] [PubMed] [Google Scholar]
- 55.Beumer GJ, van Blitterswijk CA, Bakker D, Ponec M. A new biodegradable matrix as part of a cell seeded skin substitute for the treatment of deep skin defects: a physico-chemical characterisation. Clin Mater. 1993;14:21–27. doi: 10.1016/0267-6605(93)90043-7. [DOI] [PubMed] [Google Scholar]
- 56.Uccioli L. A clinical investigation on the characteristics and outcomes of treating chronic lower extremity wounds using the TissueTech Autograft System. Int J Low Extrem Wounds. 2003;2:140–151. doi: 10.1177/1534734603258480. [DOI] [PubMed] [Google Scholar]
- 57.Caravadggi C, De Giglio R, Pritelli C, Sommaria M, Dalla Noce S, Faglia E, et al. HYAFF 11 – based autologous dermal and epidermal grafts in the treatment of noninfected diabetic plantar and dorsal. Diabetes Care. 2003;26:2853–2859. doi: 10.2337/diacare.26.10.2853. [DOI] [PubMed] [Google Scholar]
- 58.Steinberg JS, Edmonds M, Hurley DP, King WN. Confirmatory data from EU study supports Apligraf for the treatment of neuropathic diabetic foot ulcers. J Am Podiatr Med Assoc. 2010;100:73–77. doi: 10.7547/1000073. [DOI] [PubMed] [Google Scholar]
- 59.Harding KG, Krieg T, Eming SA, Flour MLF, Jawien A, Cencora A, et al. Efficacy and safety of the freeze-dried cultured human keratinocyte lysate, LyphoDermTM 0.9%, in the treatment of hard-to-heal venous leg ulcers. Wound Repair Regen. 2005;13:138–147. doi: 10.1111/j.1067-1927.2005.130204.x. [DOI] [PubMed] [Google Scholar]
- 60.Dieckmann C, Renner R, Milkova L, Simon JC. Regenerative medicine in dermatology: biomaterials, tissue engineering, stem cells, gene transfer and beyond. Exp Dermatol. 2010;19:697–706. doi: 10.1111/j.1600-0625.2010.01087.x. [DOI] [PubMed] [Google Scholar]
- 61.Esteban-Vives R, Choi MS, Young MT, Over P, Ziembicki J, Corcos A, et al. Second-degree burns with six etiologies treated with autologous noncultured cell-spray grafting. Burns. 2016;42:e99–106. doi: 10.1016/j.burns.2016.02.020. [DOI] [PubMed] [Google Scholar]
- 62.Moustafa M, Bullock AJ, Creagh FM, Heller S, Jeffcoate W, Game F, et al. Randomized, controlled, single-blind study on use of autologous keratinocytes on a transfer dressing to treat nonhealing diabetic ulcers. Regen Med. 2007;2:887–902. doi: 10.2217/17460751.2.6.887. [DOI] [PubMed] [Google Scholar]
- 63.Johnsen S, Ermuth T, Tanczos E, Bannasch H, Horch RE, Zschocke I, et al. Treatment of therapy-refractive ulcera cruris of various origins with autologous keratinocytes in fibrin sealant. Vasa - J Vasc Dis. 2005;34:25–29. doi: 10.1024/0301-1526.34.1.25. [DOI] [PubMed] [Google Scholar]
- 64.Tausche AK, Skaria M, Böhlen L, Liebold K, Hafner J, Friedlein H, et al. An autologous epidermal equivalent tissue-engineered from follicular outer root sheath keratinocytes is as effective as split-thickness skin autograft in recalcitrant vascular leg ulcers. Wound Repair Regen. 2003;11:248–252. doi: 10.1046/j.1524-475x.2003.11403.x. [DOI] [PubMed] [Google Scholar]
- 65.Li Y, Zhang J, Yue J, Gou X, Wu X. Epidermal stem cells in skin wound healing. Adv Wound Care. 2017;6:297–307. doi: 10.1089/wound.2017.0728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lataillade JJ, Doucet C, Bey E, Carsin H, Huet C, Clairand I, et al. New approach to radiation burn treatment by dosimetry-guided surgery combined with autologous mesenchymal stem cell therapy. Regen Med. 2007;2:785–794. doi: 10.2217/17460751.2.5.785. [DOI] [PubMed] [Google Scholar]
- 67.Kim K, Blasco-Morente G, Cuende N, Arias-Santiago S. Mesenchymal stromal cells: properties and role in management of cutaneous diseases. J Eur Acad Dermatology Venereol. 2017;31:414–423. doi: 10.1111/jdv.13934. [DOI] [PubMed] [Google Scholar]
- 68.Maranda EL, Badiavas LR-M and , Badiavas EV Role of mesenchymal stem cells in dermal repair in burns and diabetic wounds. Curr Stem Cell Res Ther. 2017;12:61–70. 10.2174/1574888X11666160714115926. http://www.eurekaselect.com/143959/article. [DOI] [PubMed]
- 69.Fathke C, Wilson L, Hutter J, Kapoor V, Smith A, Hocking A, et al. Contribution of bone marrow–derived cells to skin: collagen deposition and wound repair Carrie. Stem Cells 2004;22:812–822. [DOI] [PMC free article] [PubMed]
- 70.Foubert P, Barillas S, Gonzalez AD. Uncultured adipose-derived regenerative cells ( ADRCs ) seeded in collagen scaffold improves dermal regeneration , enhancing early vascularization and structural organization followin ... ScienceDirect Uncultured adipose-derived regenerative cells ( ADRCs. Burns. 2015;41 1504–16. [DOI] [PubMed]
- 71.Kølle ST, Fischer-nielsen A, Mathiasen AB, Elberg JJ, Oliveri RS, Glovinski PV, et al. Enrichment of autologous fat grafts with ex-vivo expanded adipose tissue-derived stem cells for graft survival : a randomised placebo-controlled trial. Lancet. 2013;382:1113–1120. doi: 10.1016/S0140-6736(13)61410-5. [DOI] [PubMed] [Google Scholar]
- 72.Gentile P, De Angelis B, Pasin M, Cervelli ÞG, Curcio CB, Floris M, et al. Adipose-derived stromal vascular fraction cells and platelet-rich plasma: basic and clinical evaluation for cell-based therapies in patients with scars on the face. J Craniofac Surg. 2014;25:267–272. doi: 10.1097/01.scs.0000436746.21031.ba. [DOI] [PubMed] [Google Scholar]
- 73.Abbas OL, Özatik O, Gönen ZB, Öğüt S, Özatik FY, Salkın H, et al. Comparative analysis of mesenchymal stem cells from bone marrow, adipose tissue, and dental pulp as sources of cell therapy for zone of stasis burns. J Investig Surg. 1939;2018:1–14. doi: 10.1080/08941939.2018.1433254. [DOI] [PubMed] [Google Scholar]
- 74.Abo-Elkheir W, Hamza F, Elmofty AM, Emam A, Abdl-Moktader M, Elsherefy S, et al. Role of cord blood and bone marrow mesenchymal stem cells in recent deep burn: a case-control prospective study. Am J Stem Cells. 2017;6:23–35 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5675835/. [PMC free article] [PubMed]
- 75.Rasulov MF, Vasilchenkov AV, Onishchenko NA, Krasheninnikov ME, Kravchenko VI, Gorshenin TL, et al. First experience of the use bone marrow mesenchymal stem cells for the treatment of a patient with deep skin burns. Bull Exp Biol Med. 2005;139:141–144. doi: 10.1007/s10517-005-0232-3. [DOI] [PubMed] [Google Scholar]
- 76.Zhang Y, Niu X, Dong X, Wang Y, Li H. Bioglass enhanced wound healing ability of urine-derived stem cells through promoting paracrine effects between stem cells and recipient cells. J Tissue Eng Regen Med. 2018;12:e1609–e1622. doi: 10.1002/term.2587. [DOI] [PubMed] [Google Scholar]
- 77.Chen CY, Rao SS, Ren L, Hu XK, Tan YJ, Hu Y, et al. Exosomal DMBT1 from human urine-derived stem cells facilitates diabetic wound repair by promoting angiogenesis. Theranostics. 2018;8:1607–1623. doi: 10.7150/thno.22958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Itoh M, Umegaki-Arao N, Guo Z, Liu L, Higgins CA, Christiano AM. Generation of 3D skin equivalents fully reconstituted from human induced pluripotent stem cells (iPSCs) PLoS One. 2013;8:1–9. doi: 10.1371/journal.pone.0077673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.King A, Balaji S, Keswani SG, Crombleholme TM. The role of stem cells in wound angiogenesis. Adv Wound Care. 2014;3:614–625. doi: 10.1089/wound.2013.0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Das SK, Yuan YF, Li MQ. An overview on current issues and challenges of endothelial progenitor cell-based neovascularization in patients with diabetic foot ulcer. Cell Reprogram. 2017;19:75–87. doi: 10.1089/cell.2016.0050. [DOI] [PubMed] [Google Scholar]
- 81.Dubsky M, Jirkovska A, Bem R, Fejfarova V, Pagacova L, Sixta B, et al. Both autologous bone marrow mononuclear cell and peripheral blood progenitor cell therapies similarly improve ischaemia in patients with diabetic foot in comparison with control treatment. Diabetes Metab Res Rev. 2013;29:369–376. doi: 10.1002/dmrr.2399. [DOI] [PubMed] [Google Scholar]
- 82.Balañá ME. Epidermal stem cells and skin tissue engineering in hair follicle regeneration. World J Stem Cells. 2015;7:711. doi: 10.4252/wjsc.v7.i4.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mavilio F, Pellegrini G, Ferrari S, Di Nunzio F, Di Iorio E, Recchia A, et al. Correction of junctional epidermolysis bullosa by transplantation of genetically modified epidermal stem cells. Nat Med. 2006;12:1397–1402. doi: 10.1038/nm1504. [DOI] [PubMed] [Google Scholar]
- 84.De Luca M, Pellegrini G, Green H. Regeneration of squamous epithelia from stem cells of cultured grafts. Regen Med. 2006;1:45–57. doi: 10.2217/17460751.1.1.45. [DOI] [PubMed] [Google Scholar]
- 85.Suzuki D, Senoo M. Increased p63 phosphorylation marks early transition of epidermal stem cells to progenitors. J Invest Dermatol. 2012;132:2461–2464. doi: 10.1038/jid.2012.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pellegrini G, Dellambra E, Golisano O, Martinelli E, Fantozzi I, Bondanza S, et al. P63 identifies keratinocyte stem cells. Proc Natl Acad Sci. 2001;98:3156–3161. doi: 10.1073/pnas.061032098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Harris ML, Buac K, Shakhova O, Hakami RM, Wegner M, Sommer L, et al. A dual role for SOX10 in the maintenance of the postnatal melanocyte lineage and the differentiation of melanocyte stem cell progenitors. PLoS Genet. 2013;9:e1003644. doi: 10.1371/journal.pgen.1003644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lang D, Lu MM, Huang L, Engleka KA, Zhang M, Chu EY, et al. Pax3 functions at a nodal point in melanocyte stem cell differentiation. Nature. 2005;433:884–887. doi: 10.1038/nature03292. [DOI] [PubMed] [Google Scholar]
- 89.Osawa M. Molecular characterization of melanocyte stem cells in their niche. Development. 2005;132:5589–5599. doi: 10.1242/dev.02161. [DOI] [PubMed] [Google Scholar]
- 90.Liu Y, Lyle S, Yang Z, Cotsarelis G. Keratin 15 promoter targets putative epithelial stem cells in the hair follicle bulge. J Invest Dermatol. 2003;121:963–968. doi: 10.1046/j.1523-1747.2003.12600.x. [DOI] [PubMed] [Google Scholar]
- 91.Jaks V, Barker N, Kasper M, Van Es JH, Snippert HJ, Clevers H, et al. Lgr5 marks cycling, yet long-lived, hair follicle stem cells. Nat Genet. 2008;40:1291–1299. doi: 10.1038/ng.239. [DOI] [PubMed] [Google Scholar]
- 92.Nowak JA, Polak L, Pasolli HA, Fuchs E. Hair follicle stem cells are specified and function in early skin morphogenesis. Cell Stem Cell. 2008;3:33–43. doi: 10.1016/j.stem.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sellheyer K, Krahl D. PHLDA1 (TDAG51) is a follicular stem cell marker and differentiates between morphoeic basal cell carcinoma and desmoplastic trichoepithelioma. Br J Dermatol. 2011;164:141–147. doi: 10.1111/j.1365-2133.2010.10045.x. [DOI] [PubMed] [Google Scholar]
- 94.Shi C, Mai Y, Cheng T. Identification of hematopoietic cell populations from the dermal papillae of human hair follicles. Transplant Proc. 2004;36:3208–3211. doi: 10.1016/j.transproceed.2004.11.104. [DOI] [PubMed] [Google Scholar]
- 95.Horsley V, O’Carroll D, Tooze R, Ohinata Y, Saitou M, Obukhanych T, et al. Blimp1 defines a progenitor population that governs cellular input to the sebaceous gland. Cell. 2006;126:597–609. doi: 10.1016/j.cell.2006.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Garzón I, Miyake J, González-Andrades M, Carmona R, Carda C, Sánchez-Quevedo Mdel C, et al. Wharton’s jelly stem cells: a novel cell source for oral mucosa and skin epithelia regeneration. Stem Cells Transl Med. 2013;2:625–632. doi: 10.5966/sctm.2012-0157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Driskell RR, Giangreco A, Jensen KB, Mulder KW, Watt FM. Sox2-positive dermal papilla cells specify hair follicle type in mammalian epidermis. Development. 2009;136:2815–2823. doi: 10.1242/dev.038620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ichiro MS, Ishikawa O. Mesenchymal stem cells: the roles and functions in cutaneous wound healing and tumor growth. J Dermatol Sci. 2017;86:83–89. doi: 10.1016/j.jdermsci.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 99.Marfia G, Navone SE, Di Vito C, Ughi N, Tabano S, Miozzo M, et al. Mesenchymal stem cells: potential for therapy and treatment of chronic non-healing skin wounds. Organogenesis. 2015;11:183–206. doi: 10.1080/15476278.2015.1126018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Malgieri A, Kantzari E, Patrizi MP, Gambardella S. Bone marrow and umbilical cord blood human mesenchymal stem cells: state of the art. Int J Clin Exp Med. 2010;3:248–269. [PMC free article] [PubMed] [Google Scholar]
- 101.Oswald J, Boxberger S, Jørgensen B, Feldmann S, Ehninger G, Bornhäuser M, et al. mesenchymal stem cells can be differentiated into endothelial cells in vitro. Stem Cells. 2004;22:377–384. doi: 10.1634/stemcells.22-3-377. [DOI] [PubMed] [Google Scholar]
- 102.Burdon TJ, Paul A, Noiseux N, Prakash S, Shum-Tim D. bone marrow stem cell derived paracrine factors for regenerative medicine: current perspectives and therapeutic potential. Bone Marrow Res. 2011;2011:1–14. doi: 10.1155/2011/207326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ma S, Xie N, Li W, Yuan B, Shi Y, Wang Y. Immunobiology of mesenchymal stem cells. Cell Death Differ. 2014;21:216–225. doi: 10.1038/cdd.2013.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Castro-Manrreza ME, Montesinos JJ. Immunoregulation by mesenchymal stem cells: biological aspects and clinical applications. J Immunol Res. 2015;2015:394917. doi: 10.1155/2015/394917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ma OK-F, Chan KH. Immunomodulation by mesenchymal stem cells: interplay between mesenchymal stem cells and regulatory lymphocytes. World J Stem Cells. 2016;8:268. doi: 10.4252/wjsc.v8.i9.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Condé-Green A, Marano A, Lee E, Reisler T, Price L, Milner S, et al. Fat grafting and adipose-derived regenerative cells in burn wound healing and scarring: a systematic review of the literature. Plast Reconstr Surg. 2016;137:302–312. doi: 10.1097/PRS.0000000000001918. [DOI] [PubMed] [Google Scholar]
- 107.Chang Y, Wu Y, Huang S, Wang HD. Autologous and not allogeneic adipose- derived stem cells improve acute burn wound healing. PLoS One. 2018;13(5):1–16. [DOI] [PMC free article] [PubMed]
- 108.Foubert P, Liu M, Anderson S, Rajoria R, Gutierrez D, Zafra D, et al. Preclinical assessment of safety and efficacy of intravenous delivery of autologous adipose-derived regenerative cells ( ADRCs ) in the treatment of severe thermal burns using a porcine model. Burns. 2018:2–13. 10.1016/j.burns.2018.05.006. [DOI] [PubMed]
- 109.Foubert P, Gonzalez AD, Teodosescu S, Berard F, Doyle-Eisele M, Yekkala K, et al. Adipose-derived regenerative cell therapy for burn wound healing: a comparison of two delivery methods. Adv Wound Care. 2016;5:288–298. doi: 10.1089/wound.2015.0672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Atalay S, Coruh A, Deniz K. Stromal vascular fraction improves deep partial thickness burn wound healing. Burns. 2014:1–9. 10.1016/j.burns.2014.01.023. [DOI] [PubMed]
- 111.Prasai A, El Ayadi A, Mifflin RC, Wetzel MD, Andersen CR, Redl H, et al. Characterization of adipose-derived stem cells following burn injury. Stem Cell Rev Rep. 2017;13:781–792. doi: 10.1007/s12015-017-9721-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Grove JE, Bruscia E, Krause DS. Plasticity of bone marrow-derived stem cells. Stem Cells. 2004;22:487–500. doi: 10.1634/stemcells.22-4-487. [DOI] [PubMed] [Google Scholar]
- 113.Petrof G, Abdul-Wahab A, McGrath JA. Cell therapy in dermatology. Cold Spring Harb Perspect Med. 2014;4(6):a015156. doi: 10.1101/cshperspect.a015156. [DOI] [PMC free article] [PubMed]
- 114.Chino T, Tamai K, Yamazaki T, Otsuru S, Kikuchi Y, Nimura K, et al. Bone marrow cell transfer into fetal circulation can ameliorate genetic skin diseases by providing fibroblasts to the skin and inducing immune tolerance. Am J Pathol. 2008;173:803–814. doi: 10.2353/ajpath.2008.070977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sasaki M, Abe R, Fujita Y, Ando S, Inokuma D, Shimizu H. Mesenchymal stem cells are recruited into wounded skin and contribute to wound repair by transdifferentiation into multiple skin cell type. J Immunol. 2008;180:2581–2587. doi: 10.4049/jimmunol.180.4.2581. [DOI] [PubMed] [Google Scholar]
- 116.Hu X, Zhou Y, Dong K, Sun Z, Zhao D, Wang W, et al. Programming of the development of tumor-promoting neutrophils by mesenchymal stromal cells. Cell Physiol Biochem. 2014;33:1802–1814. doi: 10.1159/000362959. [DOI] [PubMed] [Google Scholar]
- 117.Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 118.Vangipuram M, Ting D, Kim S, Diaz R, Schüle B. Skin punch biopsy explant culture for derivation of primary human fibroblasts. J Vis Exp. 2013:9–11. 10.3791/3779. [DOI] [PMC free article] [PubMed]
- 119.Hewitt KJ, Shamis Y, Hayman RB, Margvelashvili M, Dong S, Carlson MW, et al. Epigenetic and phenotypic profile of fibroblasts derived from induced pluripotent stem cells. PLoS One. 2011;6(2):e17128. doi: 10.1371/journal.pone.0017128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Bilousova G, Chen J, Roop DR. Differentiation of mouse induced pluripotent stem cells into a multipotent keratinocyte lineage. J Invest Dermatol. 2011;131:857–864. doi: 10.1038/jid.2010.364. [DOI] [PubMed] [Google Scholar]
- 121.Ohta S, Imaizumi Y, Okada Y, Akamatsu W, Kuwahara R, Ohyama M, et al. Generation of human melanocytes from induced pluripotent stem cells. PLoS One. 2011;6:1–10. doi: 10.1371/journal.pone.0016182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hewitt KJ, Shamis Y, Knight E, Smith A, Maione A, Alt-Holland A, et al. PDGFR expression and function in fibroblasts derived from pluripotent cells is linked to DNA demethylation. J Cell Sci. 2012;125:2276–2287. doi: 10.1242/jcs.099192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chen S, Takahara M, Kido M, Takeuchi S, Uchi H, Tu Y, et al. Increased expression of an epidermal stem cell marker, cytokeratin 19, in cutaneous squamous cell carcinoma. Br J Dermatol. 2008;159:952–955. doi: 10.1111/j.1365-2133.2008.08731.x. [DOI] [PubMed] [Google Scholar]
- 124.Miura K, Okada Y, Aoi T, Okada A, Takahashi K, Okita K, et al. Variation in the safety of induced pluripotent stem cell lines. Nat Biotechnol. 2009;27:743–745. doi: 10.1038/nbt.1554. [DOI] [PubMed] [Google Scholar]
- 125.Kim H, Kong WH, Seong KY, Sung DK, Jeong H, Kim JK, et al. Hyaluronate - epidermal growth factor conjugate for skin wound healing and regeneration. Biomacromolecules. 2016;17:3694–3705. doi: 10.1021/acs.biomac.6b01216. [DOI] [PubMed] [Google Scholar]
- 126.Gainza G, Bonafonte DC, Moreno B, Aguirre JJ, Gutierrez FB, Villullas S, et al. The topical administration of rhEGF-loaded nanostructured lipid carriers (rhEGF-NLC) improves healing in a porcine full-thickness excisional wound model. J Control Release. 2015;197:41–47. doi: 10.1016/j.jconrel.2014.10.033. [DOI] [PubMed] [Google Scholar]
- 127.Geer DJ, Swartz DD, Andreadis ST. Biomimetic delivery of keratinocyte growth factor upon cellular demand for accelerated wound healing in vitro and in vivo. Am J Pathol. 2005;167:1575–1586. doi: 10.1016/S0002-9440(10)61242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Puolakkainen P, Twardzik D, Ranchalis J, Pankey S, Reed M, Gombotz W. The enhancement in wound healing by transforming growth factor-β1 (TGF-β1) depends on the topical delivery system. J Surg Res. 1995;58:321–329. doi: 10.1006/jsre.1995.1050. [DOI] [PubMed] [Google Scholar]
- 129.Kojima K, Ignotz RA, Kushibiki T, Tinsley KW, Tabata Y, Vacanti CA. Tissue-engineered trachea from sheep marrow stromal cells with transforming growth factor β2 released from biodegradable microspheres in a nude rat recipient. J Thorac Cardiovasc Surg. 2004;128:147–153. doi: 10.1016/j.jtcvs.2004.02.038. [DOI] [PubMed] [Google Scholar]
- 130.Xiao Z, Xi C. Hepatocyte growth factor reduces hypertrophy of skin scar: in vivo study. Adv Ski Wound Care. 2013;26:266–270. doi: 10.1097/01.ASW.0000429705.02588.f5. [DOI] [PubMed] [Google Scholar]
- 131.Elcin YM, Dixit V, Gitnick G. Extensive in vivo angiogenesis following controlled release of human vascular endothelial cell growth factor : implications for tissue engineering and wound healing. Artif Organs. 2001;25:558–565. doi: 10.1046/j.1525-1594.2001.025007558.x. [DOI] [PubMed] [Google Scholar]
- 132.Wieman TJ, Smiell JM, Su Y. Efficacy and safely of a topical gel (becaplermin) in patients with chronic platelet-derived growth factor-BB formulation of recombinant human neuropathic diabetic ulcers. Diabetes Care. 1998;21:822–827. doi: 10.2337/diacare.21.5.822. [DOI] [PubMed] [Google Scholar]
- 133.Li M, Qiu L, Hu W, Deng X, Xu H, Cao Y, et al. Genetically-modified bone mesenchymal stem cells with TGF-β3improve wound healing and reduce scar tissue formation in a rabbit model. Exp Cell Res. 2018;367:24–29. doi: 10.1016/j.yexcr.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 134.Yang Y, Xia T, Zhi W, Wei L, Weng J, Zhang C, et al. Promotion of skin regeneration in diabetic rats by electrospun core-sheath fibers loaded with basic fibroblast growth factor. Biomaterials. 2011;32:4243–4254. doi: 10.1016/j.biomaterials.2011.02.042. [DOI] [PubMed] [Google Scholar]
- 135.Ogino S, Morimoto N, Sakamoto M, Jinno C, Sakamoto Y, Taira T, et al. Efficacy of the dual controlled release of HGF and bFGF impregnated with a collagen/gelatin scaffold. J Surg Res. 2018;221:173–182. doi: 10.1016/j.jss.2017.08.051. [DOI] [PubMed] [Google Scholar]
- 136.Suzuki S, Morimoto N, Ikada Y. Gelatin gel as a carrier of platelet-derived growth factors. J Biomater Appl. 2013;28:595–606. doi: 10.1177/0885328212468183. [DOI] [PubMed] [Google Scholar]
- 137.Lai HJ, Kuan CH, Wu HC, Tsai JC, Chen TM, Hsieh DJ, et al. Tailored design of electrospun composite nanofibers with staged release of multiple angiogenic growth factors for chronic wound healing. Acta Biomater. 2014;10:4156–4166. doi: 10.1016/j.actbio.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 138.Lee JH, Bae IH, Choi JK, Park JW. Evaluation of a highly skin permeable low-molecular-weight protamine conjugated epidermal growth factor for novel burn wound healing therapy. J Pharm Sci. 2013;102:4109–4120. doi: 10.1002/jps.23725. [DOI] [PubMed] [Google Scholar]
- 139.Li JF, Duan HF, Wu CT, Zhang DJ, Deng Y, Yin HL, et al. HGF accelerates wound healing by promoting the dedifferentiation of epidermal cells through β 1 -Integrin/ILK pathway. Biomed Res Int. 2013;2013:470418. doi: 10.1155/2013/470418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yoshida S, Yamaguchi Y, Itami S, Yoshikawa K, Tabata Y, Matsumoto K, et al. Neutralization of hepatocyte growth factor leads to retarded cutaneous wound healing associated with decreased neovascularization and granulation tissue formation. J Invest Dermatol. 2003;120:335–343. doi: 10.1046/j.1523-1747.2003.12039.x. [DOI] [PubMed] [Google Scholar]
- 141.Shin JU, Kang SW, Jeong JJ, Nam KH, Chung WY, Lee JH. Effect of recombinant human epidermal growth factor on cutaneous scar quality in thyroidectomy patients. J Dermatolog Treat. 2015;26:159–164. doi: 10.3109/09546634.2014.906034. [DOI] [PubMed] [Google Scholar]
- 142.Yang S, Geng Z, Ma K, Sun X, Fu X. Efficacy of topical recombinant human epidermal growth factor for treatment of diabetic foot ulcer: a systematic review and meta-analysis. Int J Low Extrem Wounds. 2016;15:120–125. doi: 10.1177/1534734616645444. [DOI] [PubMed] [Google Scholar]
- 143.Dermidova Rice TN, IM HMRH. Acute and impaired wound healing: pathophysiology and current methods for drug delivery, part 2: role of growth factors in normal and pathological wound healing: therapeutic potential and methods of delivery. Adv Ski Wound Care. 2012;25:349–370. doi: 10.1097/01.ASW.0000418541.31366.a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Galiano RD, Tepper OM, Pelo CR, Bhatt KA, Callaghan M, Bastidas N, et al. Topical vascular endothelial growth factor accelerates diabetic wound healing through increased angiogenesis and by mobilizing and recruiting bone marrow-derived cells. Am J Pathol. 2004;164:1935–1947. doi: 10.1016/S0002-9440(10)63754-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Hanft JR, Pollak RA, Barbul A, van Gils C, Kwon PS, Gray SM, et al. Phase I trial on the safety of topical rhVEGF on chronic neuropathic diabetic foot ulcers. J Wound Care. 2008;17:30–37. doi: 10.12968/jowc.2008.17.1.27917. [DOI] [PubMed] [Google Scholar]
- 146.Tan Q, Chen B, Yan X, Lin Y, Xiao Z, Hou X, et al. Promotion of diabetic wound healing by collagen scaffold with collagen-binding vascular endothelial growth factor in a diabetic rat model. J Tissue Eng Regen Med. 2014;8:195–201. doi: 10.1002/term.1513. [DOI] [PubMed] [Google Scholar]
- 147.Gorkun AA, Shpichka AI, Zurina IM, Koroleva AV, Kosheleva NV, Nikishin DA, et al. Angiogenic potential of spheroids from umbilical cord and adipose-derived multipotent mesenchymal stromal cells within fibrin gel. Biomed Mater. 2018;13(4):044108. doi: 10.1088/1748-605X/aac22d. [DOI] [PubMed] [Google Scholar]
- 148.Borena BM, Martens A, Broeckx SY, Meyer E, Chiers K, Duchateau L, et al. Regenerative skin wound healing in mammals: state-of-the-art on growth factor and stem cell based treatments. Cell Physiol Biochem. 2015;36:1–23. doi: 10.1159/000374049. [DOI] [PubMed] [Google Scholar]
- 149.Ferguson MWJ, O’Kane S. Scar-free healing: From embryonic mechanism to adult therapeutic intervention. Philos Trans R Soc B Biol Sci. 2004;359:839–850. doi: 10.1098/rstb.2004.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Walraven M, Akershoek JJ, Beelen RHJ, Ulrich MMW. In vitro cultured fetal fibroblasts have myofibroblast-associated characteristics and produce a fibrotic-like environment upon stimulation with TGF-β1: is there a thin line between fetal scarless healing and fibrosis? Arch Dermatol Res. 2017;309:111–121. doi: 10.1007/s00403-016-1710-3. [DOI] [PubMed] [Google Scholar]
- 151.Walraven M, Gouverneur M, Middelkoop E, Beelen RHJ, Ulrich MMW. Altered TGF-β signaling in fetal fibroblasts: what is known about the underlying mechanisms? Wound Repair Regen. 2014;22:3–13. doi: 10.1111/wrr.12098. [DOI] [PubMed] [Google Scholar]
- 152.So K, McGrouther DA, Bush JA, Durani P, Taylor L, Skotny G, et al. Avotermin for scar improvement following scar revision surgery: a randomized, double-blind, within-patient, placebo-controlled, phase II clinical trial. Plast Reconstr Surg. 2011;128:163–172. doi: 10.1097/PRS.0b013e318217429b. [DOI] [PubMed] [Google Scholar]
- 153.McCollum PT, Bush JA, James G, Mason T, O’Kane S, McCollum C, et al. Randomized phase II clinical trial of avotermin versus placebo for scar improvement. Br J Surg. 2011;98:925–934. doi: 10.1002/bjs.7438. [DOI] [PubMed] [Google Scholar]
- 154.Occleston NL, O’Kane S, Laverty HG, Cooper M, Fairlamb D, Mason T, et al. Discovery and development of avotermin (recombinant human transforming growth factor beta 3): a new class of prophylactic therapeutic for the improvement of scarring. Wound Repair Regen. 2011;19(SUPPL. 1):s38–s48. doi: 10.1111/j.1524-475X.2011.00711.x. [DOI] [PubMed] [Google Scholar]
- 155.Park J, Hwang S, Yoon I. Advanced growth factor delivery systems in wound management and skin regeneration. Molecules. 2017;22:1–20. doi: 10.3390/molecules22081259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Mccrudden TC, Mcalister E, Courtenay AJ, Gonz P, Singh R, Donnelly RF. Microneedle applications in improving skin appearance. Exp Dermatol. 2015;24:561–566. doi: 10.1111/exd.12723. [DOI] [PubMed] [Google Scholar]
- 157.Hogan NC, Taberner AJ, Jones LA, Ian W, Hogan NC, Taberner AJ, et al. Delivery needle-free delivery of macromolecules through the skin using controllable jet injectors. Expert Opin Drug Deliv. 2015;5247:1637–1648. doi: 10.1517/17425247.2015.1049531. [DOI] [PubMed] [Google Scholar]
- 158.Infanger M, Schmidt O, Kossmehl P, Grad S, Ertel W, Grimm D. Vascular endothelial growth factor serum level is strongly enhanced after burn injury and correlated with local and general tissue edema. Burns. 2004;30:305–311. doi: 10.1016/j.burns.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 159.Lian N, Li T. Growth factor pathways in hypertrophic scars : Molecular pathogenesis and therapeutic implications. Biomed Pharmacother. 2016;84:42–50. doi: 10.1016/j.biopha.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 160.Jakowlew SB. Transforming growth factor- β in cancer and metastasis. Cancer Metastasis Rev. 2006;25(3):435–57. [DOI] [PubMed]
- 161.Lal Goel H. Mercurio AM. VEGF targets the tumour cell. 2014;13:871–882. doi: 10.1038/nrc3627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Berlanga-acosta J, Gavilondo-cowley J, Pedro L, Castro-santana MD, Ernesto L, Herrera-martinez L. Epidermal growth factor in clinical practice – a review of its biological actions , clinical indications and safety implications. Int Wound J. 2009;6:331–346. doi: 10.1111/j.1742-481X.2009.00622.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zhang Y, Wang T, He J, Dong J. Growth factor therapy in patients with partial-thickness burns : a systematic review and meta-analysis. Int Wound J. 2014;13(3):1–13. [DOI] [PMC free article] [PubMed]
- 164.Mostow EN, Haraway GD, Dalsing M, Hodde JP, King D. Effectiveness of an extracellular matrix graft (OASIS Wound Matrix) in the treatment of chronic leg ulcers: a randomized clinical trial. J Vasc Surg. 2005;41:837–843. doi: 10.1016/j.jvs.2005.01.042. [DOI] [PubMed] [Google Scholar]
- 165.Wainwright DJ. Use of an acellular allograft dermal matrix (AlloDerm) in the management of full-thickness burns. Burns. 1995;21:243–248. doi: 10.1016/0305-4179(95)93866-i. [DOI] [PubMed] [Google Scholar]
- 166.Juhasz I, Kiss B, Lukacs L, Erdei I, Peter Z, Remenyik E. Long-term followup of dermal substitution with acellular dermal implant in burns and postburn scar corrections. Dermatol Res Pract. 2010;2010:210150. doi: 10.1155/2010/210150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Landsman AS, Cook J, Cook E, Landsman AR, Garett P, Yoon J, et al. A retrospective clinical study to examine the effectiveness of 188 consecutive patients allograft (TheraSkin) on the cryopreserved human skin of a biologically active treatment of diabetic foot ulcers and venous leg ulcers. Foot Ankle Spec. 2011;4:29–41. doi: 10.1177/1938640010387417. [DOI] [PubMed] [Google Scholar]
- 168.MacLeod TM, Cambrey A, Williams G, Sanders R, Green CJ. Evaluation of PermacolTM as a cultured skin equivalent. Burns. 2008;34:1169–1175. doi: 10.1016/j.burns.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 169.Papadogeorgakis N, Petsinis V, Christopoulos P, Mavrovouniotis N, Alexandridis C. Use of a porcine dermal collagen graft (Permacol) in parotid surgery. Br J Oral Maxillofac Surg. 2009;47:378–381. doi: 10.1016/j.bjoms.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 170.Troy J, Karlnoski R, Downes K, Brown KS, Cruse CW, Smith DJ, et al. The use of EZ Derm® in partial-thickness burns: an institutional review of 157 patients. Eplasty. 2013;13:e14. [PMC free article] [PubMed] [Google Scholar]
- 171.Heimbach DM, Warden GD, Luterman A, Jordan MH, Ozobia N, Ryan CM, et al. Multicenter postapproval clinical trial of Integra® Dermal Regeneration Template for burn treatment. J Burn Care Rehabil. 2003;24:42–48. doi: 10.1097/00004630-200301000-00009. [DOI] [PubMed] [Google Scholar]
- 172.Eo S, Kim Y, Cho S. Vacuum-assisted closure improves the incorporation of artificial dermis in soft tissue defects: Terudermis®and Pelnac®. Int Wound J. 2011;8:261–267. doi: 10.1111/j.1742-481X.2011.00780.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Soejima K, Shimoda K, Kashimura T, Yamaki T, Kono T, Sakurai H, et al. One-step grafting procedure using artificial dermis and split-thickness skin in burn patients. Eur J Plast Surg. 2013;36:585–590. [Google Scholar]
- 174.Widjaja W, Maitz P. The use of dermal regeneration template (Pelnac®) in acute full-thickness wound closure: a case series. Eur J Plast Surg. 2016;39:125–132. [Google Scholar]
- 175.Lesher A, Curry R, Evans J, Smith V, FItzgerald M, Cina R, et al. Effectiveness of Biobrane for treatment of partial-thickness burns in children. J Pediatr Surg. 2011;46:1759–1763. doi: 10.1016/j.jpedsurg.2011.03.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lam PK, Chan ESY, To EWH, Lau CH, Yen SC, King WWK. Development and evaluation of a new composite Laserskin graft. J Trauma Acute Care Surg. 1999;47 https://insights.ovid.com/pubmed?pmid=10568722. Accessed 11 Mar 2019. [DOI] [PubMed]
- 177.Gravante G, Delogu D, Giordan N, Morano G, Montone A, Esposito G. The use of hyalomatrix PA in the treatment of deep partial-thickness burns. J Burn Care Res. 2007;28:269–274. doi: 10.1097/BCR.0B013E318031A236. [DOI] [PubMed] [Google Scholar]
- 178.Roh DH, Kang SY, Kim JY, Kwon YB, Hae YK, Lee KG, et al. Wound healing effect of silk fibroin/alginate-blended sponge in full thickness skin defect of rat. J Mater Sci Mater Med. 2006;17:547–552. doi: 10.1007/s10856-006-8938-y. [DOI] [PubMed] [Google Scholar]
- 179.Helenius G, Bäckdahl H, Bodin A, Nannmark U, Gatenholm P, Risberg B. In vivo biocompatibility of bacterial cellulose. J Biomed Mater Res - Part A. 2006;76:431–438. doi: 10.1002/jbm.a.30570. [DOI] [PubMed] [Google Scholar]
- 180.Fu L, Zhang J, Yang G. Present status and applications of bacterial cellulose-based materials for skin tissue repair. Carbohydr Polym. 2013;92:1432–1442. doi: 10.1016/j.carbpol.2012.10.071. [DOI] [PubMed] [Google Scholar]
- 181.Harding K, Sumner M, Cardinal M. A prospective, multicentre, randomised controlled study of human fibroblast-derived dermal substitute (Dermagraft) in patients with venous leg ulcers. Int Wound J. 2013;10:132–137. doi: 10.1111/iwj.12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Gundy S, Manning G, O’Connell E, Ellä V, Harwoko MS, Rochev Y, et al. Human coronary artery smooth muscle cell response to a novel PLA textile/fibrin gel composite scaffold. Acta Biomater. 2008;4:1734–1744. doi: 10.1016/j.actbio.2008.05.025. [DOI] [PubMed] [Google Scholar]
- 183.Zurina I, Shpichka A, Saburina I, Kosheleva N, Gorkun A, Grebenik E, et al. 2D/3D buccal epithelial cell self-assembling as a tool for cell phenotype maintenance and fabrication of multilayered epithelial linings in vitro. Biomed Mater. 2018;13:054104. doi: 10.1088/1748-605X/aace1c. [DOI] [PubMed] [Google Scholar]
- 184.Sun G, Shen YI, Harmon JW. Engineering pro-regenerative hydrogels for scarless wound healing. Adv Healthc Mater. 2018;1800016:1–12. doi: 10.1002/adhm.201800016. [DOI] [PubMed] [Google Scholar]
- 185.Rippon MG, Ousey K, Cutting KF. Wound healing and hyper-hydration: a counterintuitive model. J Wound Care. 2016;25:68–75. doi: 10.12968/jowc.2016.25.2.68. [DOI] [PubMed] [Google Scholar]
- 186.Murphy KC, Whitehead J, Zhou D, Ho SS, Leach JK. Engineering fibrin hydrogels to promote the wound healing potential of mesenchymal stem cell spheroids. Acta Biomater. 2017;64:176–186. doi: 10.1016/j.actbio.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Chen S, Shi J, Zhang M, Chen Y, Wang X, Zhang L, et al. Mesenchymal stem cell-laden anti-inflammatory hydrogel enhances diabetic wound healing. Sci Rep. 2015;5:1–12. doi: 10.1038/srep18104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Lei Z, Singh G, Min Z, Shixuan C, Xu K, Pengcheng X, et al. Bone marrow-derived mesenchymal stem cells laden novel thermo-sensitive hydrogel for the management of severe skin wound healing. Mater Sci Eng C. 2018;90:159–167. doi: 10.1016/j.msec.2018.04.045. [DOI] [PubMed] [Google Scholar]
- 189.Zhou Y, Gao L, Peng J, Xing M, Han Y, Wang X, et al. Bioglass activated albumin hydrogels for wound healing. Adv Healthc Mater. 2018;1800144:1–13. doi: 10.1002/adhm.201800144. [DOI] [PubMed] [Google Scholar]
- 190.Greiser U, Dong Y, Wang F, Tai H, Liu W. A hybrid injectable hydrogel from hyperbranched PEG macromer as a stem cell delivery and retention platform for diabetic wound healing. Acta Biomater. 2018. 10.1016/j.actbio.2018.05.039. [DOI] [PubMed]
- 191.Powell HM, Boyce ST. Fiber density of electrospun gelatin scaffolds regulates morphogenesis of dermal – epidermal skin substitutes. J Biomed Mater Res Part A. 2007;84(4):1078–86 [DOI] [PubMed]
- 192.Huang S, Zhang Y, Tang L, Deng Z, Lu W, Feng F, et al. Functional bilayered skin substitute constructed and microsphere-incorporated gelatin hydrogel. TISSUE Eng Part A. 2009;15:2617–2624. doi: 10.1089/ten.TEA.2008.0505. [DOI] [PubMed] [Google Scholar]
- 193.Krasna M, Planinsek F, Knezevic M, Arnez ZM, Jeras M. Evaluation of a fibrin-based skin substitute prepared in a defined keratinocyte medium. Int J Pharm. 2005;291:31–37. doi: 10.1016/j.ijpharm.2004.07.040. [DOI] [PubMed] [Google Scholar]
- 194.Mohd Hilmi AB, Halim AS, Jaafar H, Asiah AB, Hassan A. Chitosan dermal substitute and Chitosan skin substitute contribute to accelerated full-thickness wound healing in irradiated rats. Biomed Res Int. 2013;2013:795458. doi: 10.1155/2013/795458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Zhang Y, Zhang X, Xu L, Wei S, Zhai M. Radiation cross-linked collagen/dextran dermal scaffolds: effects of dextran on cross-linking and degradation. J Biomater Sci Polym Ed. 2015;26:162–180. doi: 10.1080/09205063.2014.985023. [DOI] [PubMed] [Google Scholar]
- 196.Sun G, Shen YI, Ho CC, Kusuma S, Gerecht S. Functional groups affect physical and biological properties of dextran-based hydrogels. J Biomed Mater Res - Part A. 2010;93:1080–1090. doi: 10.1002/jbm.a.32604. [DOI] [PubMed] [Google Scholar]
- 197.Vanstraelen P. Comparison of calcium sodium alginate (KALTOSTAT) and porcine xenograft (E-Z DERM) in the healing of split-thickness skin graft donor sites. Burns. 1992;18:145–148. doi: 10.1016/0305-4179(92)90014-l. [DOI] [PubMed] [Google Scholar]
- 198.Salbach J, Rachner TD, Franz S, Simon J, Hofbauer LC. Regenerative potential of glycosaminoglycans for skin and bone. J Mol Med. 2012;90:625–635. doi: 10.1007/s00109-011-0843-2. [DOI] [PubMed] [Google Scholar]
- 199.Cecelia C, Whaley D, Babu R, Zhang J. The effect of multifunctional polymer-based gels on wound healing in full thickness bacteria-contaminated mouse models. Biomaterials. 2008;28:3977–3986. doi: 10.1016/j.biomaterials.2007.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Casper C, Yamaguchi N, Kiick K, Rabolt J. Functionalizing electrospun fibers with biologically relevant macromolecules. Biomacromolecules. 2005;6:1998–2007. doi: 10.1021/bm050007e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Cubo N, Garcia M, Del Cañizo JF, Velasco D, Jorcano JL. 3D bioprinting of functional human skin: production and in vivo analysis. Biofabrication. 2016;9:015006. 10.1088/1758-5090/9/1/015006. [DOI] [PubMed]
- 202.Michael S, Sorg H, Peck CT, Koch L, Deiwick A, Chichkov B, et al. Tissue engineered skin substitutes created by laser-assisted bioprinting form skin-like structures in the dorsal skin fold chamber in mice. PLoS One. 2013;8(3):e57741. doi: 10.1371/journal.pone.0057741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Lee V, Singh G, Trasatti JP, Bjornsson C, Xu X, Tran TN, et al. Design and fabrication of human skin by three-dimensional bioprinting. Tissue Eng Part C Methods. 2014;20:473–484. doi: 10.1089/ten.tec.2013.0335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Campbell PG, Weiss LE. Tissue engineering with the aid of inkjet printers. 2007. pp. 1123–1128. [DOI] [PubMed] [Google Scholar]
- 205.Binder KW, Zhao W, Aboushwareb T, Dice D, Atala A, Yoo JJ. In situ bioprinting of the skin for burns. J Am Coll Surg. 2010;211:S76. doi: 10.1016/j.jamcollsurg.2010.06.198. [DOI] [Google Scholar]
- 206.Skardal A, Mack D, Kapetanovic E, Atala A, Jackson JD, Yoo J, et al. Bioprinted amniotic fluid-derived stem cells accelerate healing of large skin wounds. Stem Cells Transl Med. 2012;1:792–802. doi: 10.5966/sctm.2012-0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Allouni A, Papini R, Lewis D. Spray-on-skin cells in burns: a common practice with no agreed protocol. Burns. 2013;39:1391–1394. doi: 10.1016/j.burns.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 208.Esteban-Vives R, Corcos A, Choi MS, Young MT, Over P, Ziembicki J, et al. Cell-spray auto-grafting technology for deep partial-thickness burns: Problems and solutions during clinical implementation. Burns. 2018;44:549–559. doi: 10.1016/j.burns.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 209.Nicholas MN, Yeung J. Current status and future of skin substitutes for chronic wound healing. J Cutan Med Surg. 2017;21:23–30. doi: 10.1177/1203475416664037. [DOI] [PubMed] [Google Scholar]
- 210.Oryan A, E. Alemzadeh AM. Burn wound healing: present concepts, treatment strategies and future directions. Wound Care. 2017;26:5–19. doi: 10.12968/jowc.2017.26.1.5. [DOI] [PubMed] [Google Scholar]
- 211.Metcalfe AD, Ferguson MWJ. Bioengineering skin using mechanisms of regeneration and repair. Biomaterials. 2007;28:5100–5113. doi: 10.1016/j.biomaterials.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 212.El-Serafi AT, El-Serafi IT, Elmasry M, Steinvall I, Sjöberg F. Skin regeneration in three dimensions, current status, challenges and opportunities. Differentiation. 2017;96:26–29. doi: 10.1016/j.diff.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 213.Tonello C, Vindigni V, Zavan B, Abatangelo S, Abatangelo G, Brun P, et al. In vitro reconstruction of an endothelialized skin substitute provided with a microcapillary network using biopolymer scaffolds. FASEB J. 2005;19:1546–1548. doi: 10.1096/fj.05-3804fje. [DOI] [PubMed] [Google Scholar]
- 214.Biedermann T, Klar AS, Böttcher-Haberzeth S, Michalczyk T, Schiestl C, Reichmann E, et al. Long-term expression pattern of melanocyte markers in light- and dark-pigmented dermo-epidermal cultured human skin substitutes. Pediatr Surg Int. 2015;31:69–76. doi: 10.1007/s00383-014-3622-7. [DOI] [PubMed] [Google Scholar]
- 215.Chen L, Xing Q, Zhai Q, Tahtinen M, Zhou F, Chen L, et al. Pre-vascularization enhances therapeutic effects of human mesenchymal stem cell sheets in full thickness skin wound repair. Theranostics. 2017;7:117–131. doi: 10.7150/thno.17031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Morimoto N, Saso Y, Tomihata K, Taira T, Takahashi Y, Ohta M, et al. Viability and function of autologous and allogeneic fibroblasts seeded in dermal substitutes after implantation. J Surg Res. 2005;125:56–67. doi: 10.1016/j.jss.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 217.Roccia M, França K, Castillo D, Tchernev G, Wollina U, Tirant M, et al. Artificial Hair : By the Dawn to Automatic Biofibre ® Hair Implant. 2018;6:156–62. [DOI] [PMC free article] [PubMed]
- 218.Sriwiriyanont P, Lynch KA, McFarland KL, Supp DM, Boyce ST. Characterization of hair follicle development in engineered skin substitutes. PLoS One. 2013;8(6):e65664. doi: 10.1371/journal.pone.0065664. [DOI] [PMC free article] [PubMed]
- 219.Hou L, Hagen J, Wang X, Papautsky I, Naik R, Kelley-Loughnane N, et al. Artificial microfluidic skin for in vitro perspiration simulation and testing. Lab Chip. 2013;13:1868–1875. doi: 10.1039/c3lc41231h. [DOI] [PubMed] [Google Scholar]
- 220.Ma PX. Biomimetic materials for tissue engineering. Adv Drug Deliv Rev. 2008;60:184–198. doi: 10.1016/j.addr.2007.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Wilcke I, Lohmeyer JA, Liu S, Condurache A, Krüger S, Mailänder P, et al. VEGF165and bFGF protein-based therapy in a slow release system to improve angiogenesis in a bioartificial dermal substitute in vitro and in vivo. Langenbeck’s Arch Surg. 2007;392:305–314. doi: 10.1007/s00423-007-0194-1. [DOI] [PubMed] [Google Scholar]
- 222.Chouhan D, Thatikonda N, Nilebäck L, Widhe M, Hedhammar M, Mandal BB. Recombinant spider silk functionalized silkworm silk matrices as potential bioactive wound dressings and skin grafts. ACS Appl Mater Interfaces. 2018;0(28):23560–23572. doi: 10.1021/acsami.8b05853. [DOI] [PubMed] [Google Scholar]
- 223.Niu Y, Li Q, Ding Y, Dong L, Wang C. Engineered delivery strategies for enhanced control of growth factor activities in wound healing. Adv Drug Deliv Rev. 2018. 10.1016/j.addr.2018.06.002. [DOI] [PubMed]
- 224.Ojeh N, Pastar I, Tomic-Canic M, Stojadinovic O. Stem cells in skin regeneration, wound healing, and their clinical applications. Int J Mol Sci. 2015;16:25476–25501. doi: 10.3390/ijms161025476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Shu X, Shu S, Tang S, Yang L, Liu D, Li K, et al. Efficiency of stem cell based therapy in the treatment of diabetic foot ulcer: a meta-analysis. Endocr J. 2018;65:403–413. doi: 10.1507/endocrj.EJ17-0424. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.


