Abstract
Executive control is a set of cognitive abilities that may impact a variety of adolescent health behaviors and outcomes; however, research on executive control as a contributor to the physical health of youth is relatively limited. Therefore, the current article explores the possible role of executive control in adolescent health by reviewing relevant literature and proposing a conceptual framework to guide future research in this area. The development of executive control from preschool through adolescence is described, with particular attention to executive control in the unique health context of adolescence. A new conceptual model is proposed, focusing on how executive control may play a critical role in supporting health in adolescence and beyond through the mechanisms of attentional, behavioral, and emotional control. Literature exploring associations between youth executive control and key health behaviors (including diet, physical activity, sleep and substance use) is reviewed. Researchers and clinicians are encouraged to consider executive control as an important cross-cutting contributor to health during adolescence and beyond and to incorporate this construct into longitudinal studies of health.
Keywords: executive control, health, health behaviors, child, adolescent
Introduction
Identifying modifiable factors that affect adolescent health is a critical focus for research and informs interventions to promote health across the lifespan. In recent years, executive control has been proposed as one such factor that may have an important impact on child and adolescent health. Executive control (also known as “executive function”) is a set of higher-order cognitive processes that are essential for directing attention and behavior (Diamond, 2013). Executive control is typically conceptualized as comprised of three related abilities: working memory (the ability to hold information in mind and work with it); inhibitory control (the ability to inhibit prepotent responses); and flexible shifting (the ability to shift between changing task demands) (Espy, 2016). Deficits in these abilities have long been recognized as contributors to poor academic achievement (Blair & Razza 2007) and disruptive behavior problems (Espy, Sheffield, Wiebe, Clark, & Moehr, 2011), but the potential relevance of poor executive control to child and adolescent health has only recently emerged as a topic for systematic investigation.
To support the integration of executive control into adolescent health research and practice, the current article provides a theoretical framework for conceptualizing the role of executive control in adolescent health. The article is organized around five main goals. First, some unique developmental issues in adolescent health are discussed to provide a context for exploring executive control and health during this period. Second, a brief introduction to executive control is provided, with a focus on its development, neurological underpinnings, and measurement. Third, a conceptual model for the role of executive control in adolescent health is proposed, exploring mechanisms by which early executive control may impact health (and vice versa) during adolescence and across the lifespan. Fourth, the extant literature regarding associations between executive control and selected key child and adolescent health behaviors is briefly surveyed. Fifth, future directions for research on executive control and adolescent health, including recommendations for addressing limitations in previous executive control-health research, are discussed.
Developmental Issues in Adolescent Health
Although executive control is likely important for health across development, the current article gives special consideration to adolescence, when the influence of executive control abilities may be particularly salient for health. Adolescence is a unique developmental period, distinct from childhood and adulthood, and presents a unique health context (Jaworska & MacQueen, 2015). In addition to the numerous biological changes that occur during adolescence, most adolescents also experience significant changes in social, cognitive and affective context, which shape the health challenges of this period and the need for strong executive control to promote health. Cognitively, adolescence is a time of growing abilities (Luna, Garver, Urban, Lazar, & Sweeny, 2004) but also substantial reorganization in the brain (Blakemore & Choudhury, 2006). Importantly, executive control abilities continue to develop across adolescence and into young adulthood (Luna, Marek, Larsen, Tervo-Clemmens, & Chahal, 2015). The result of this protracted cognitive development is that, although adolescents generally have more developed executive control abilities than children, these abilities are still relatively immature compared to adults (Best & Miller, 2011). This relative immaturity and ongoing development can confer substantial health risk when combined with social and affective changes that increasingly demand strong self-regulation.
Adolescence is typically characterized by increasing autonomy from parents (McElhaney, Allen, & Stephenson, 2009) and a rise in peer influence (Prinstein & Dodge, 2008). In the health realm, adolescents have increased independence in their health behaviors, making more of their own decisions about diet, sleep, physical activity, and substance use (Bassett, Chapman, & Beagan, 2008). Greater mobility that comes with driving also gives many adolescents increased autonomy away from the immediate supervision of their parents (Allen & Brown, 2008), providing them with increased freedom to select their environments and make important health choices independently. The result of increased health behavior autonomy is that adolescents increasingly face “adult” decisions with potentially serious health implications, but they do so while the neural mechanisms that support optimal decision-making and regulation of behavior are still developing, creating a potential mismatch between abilities and environmental demands. Adolescents with strong executive control may be able to navigate this challenging time, but those with executive control deficits may be especially ill-equipped to successfully meet the increasing demands of adolescence. Further, adolescence can be a time of increased affective reactivity, as evidenced by increases in amygdala activity (Hare, Tottenham, Galvan, Voss, Glover, & Casey, 2008) and increased risk for depression and anxiety symptoms (Merikangas et al., 2010). Greater negative affect can further complicate the demands on adolescents in directing their attention and behavior toward health goals: Adolescents must navigate their affective experiences and social context to choose and enact healthy behaviors, all with regulatory abilities that are not yet mature. The result is a developmental period with unique health risks (Sawyer et al., 2012), particularly for those with poor executive control, and health behavior patterns emerging during adolescence may become the foundation of lifelong health behavior (Lake, Adamson, Craigie, Rugg-Gunn, & Mathers, 2009).
The Nature of Executive Control
Neurological bases of executive control.
Executive control relies upon neural activation localized to the prefrontal cortex, yet interconnected to developing, specialized neural pathways that traverse multiple executive control-related functional regions of the brain. These executive control regions include the prefrontal, basal ganglia, anterior cingulate, and parietal regions. Connectivity between the prefrontal cortex and subcortical and posterior regions of the brain relate to enhanced executive control, as this connectivity allows for communication between regions monitoring sensory input and regions dedicated to higher cognitive functioning (see Espy, 2016 for detailed review of neural bases of child executive control). Neural activation related to executive control task performance is gradually localized to the prefrontal cortex after birth, so that this region is predominantly activated in children as young as three years of age completing executive control tasks (Moriguchi & Hiraki, 2009). This activation increases through childhood and adolescence as interconnectivity is established between the prefrontal region and other executive control functional regions (Fair et al., 2007). The neural bases of executive control, therefore, progress from generalized neural activation, to localized prefrontal activation, and finally to specialized network(s) activation.
The shift from generalized to more specialized executive control-related neural activation unfolds over the course of development; however, adolescence in particular is a critical period of change for the neural processes that mediate executive control (Best & Miller, 2010). For example, although excess neurons and synaptic connections are routinely eliminated during infancy and childhood, this process of synaptic pruning accelerates during adolescence, especially within the prefrontal cortex. Synaptic pruning enhances the efficiency of neural processing, which in turn supports more complex patterns of integration between the prefrontal region and other networks needed to support executive control (Selemon, 2013). Increases in the volume of white matter also promote greater interconnectivity during adolescence. White matter contains myelin, a substance that accumulates around axons in order to accelerate synaptic connections. Increased myelination during this period improves the integrity of white matter pathways and increases rates of neuronal transmissions (Luna et al., 2015). Together, greater synaptic pruning and increases in white matter volume and subsequent myelination gradually enable adolescents’ brains to function more like adults’. However, as these changes are still in progress, excess synapses and relatively slower neural activation may still impede adolescents’ optimal engagement of the neural mechanisms underlying executive control (Luna et al., 2015).
Developmental trajectory of executive control.
Long-term longitudinal studies of executive control are generally lacking; however, cross-sectional and short-term longitudinal investigations can inform our understanding of executive control development across childhood and adolescence. A substantial body of literature has documented that preschool is a critical period in the development of executive control and that important individual differences emerge during this time (see Espy, 2016). Across the preschool years, executive control abilities increase markedly, although the rate of growth differs between individuals (Clark et al., 2013). Measurement studies have repeatedly demonstrated the unitary nature of executive control in preschool, with executive control most parsimoniously represented as a single latent construct comprised of working memory, inhibitory control, and flexible shifting tasks all loading on a general executive control factor (e.g., Wiebe et al., 2011). Further, some research suggests that executive control begins to differentiate from other foundational cognitive abilities (e.g., vocabulary, visual-spatial perception) during preschool. Specifically, Espy (2016) found that at age 3, the contribution of executive control to performance on executive tasks was indistinguishable from that of foundational cognitive abilities, but by age 4.5 years, executive control and foundational cognitive abilities were best represented as distinct but overlapping constructs that each contributed to task performance.
Executive control abilities continue to develop in elementary school, although relatively little is known about the structure of the construct and normative patterns of development during this time. More research has examined executive control in adolescence, which is considered another important period for executive control maturation. Substantial brain reorganization during adolescence contributes to increasing executive control abilities during this time, as well as increasing differentiation of the different components of executive control (Lee, Bull, & Ho, 2013). Although exactly when this differentiation typically occurs is not yet clearly established, studies have found that the early unitary structure of executive control differentiates into two components (i.e., working memory and flexible shifting/inhibition) as early as kindergarten (van de Ven, Kroesbergen, Boom, & Lesemen, 2013) or elementary school (Brydges, Fox, Reid, & Anderson, 2014), and that executive control abilities can be separated into three distinct, yet interrelated, components (working memory, inhibitory control, flexible shifting) by late childhood (Rose, Feldman, & Jankowski, 2011) or early adolescence (Lee et al., 2013). Consistent with evidence that prefrontal cortex maturation and integration continues throughout adolescence and even into young adulthood, individuals continue to show improvements on certain executive control tasks into early adulthood (see Luna, Padmanabhan, & O’Hearn, 2010 for review).
The protracted developmental course of executive control from early childhood to young adulthood creates vulnerabilities while executive control is immature, and factors that compromise early executive control development can have major long-term implications by changing developmental trajectories. On the other hand, the protracted nature of executive control maturation may create opportunities for intervention at critical periods when neural plasticity may enable remediation of emerging deficits (Diamond, 2011). The potential health benefits of executive control promotion during critical developmental periods are not well-understood at this time, and developmentally-informed intervention studies are needed.
Contributors to executive control development.
Consistent with biopsychosocial models of health, research has identified a variety of biological, environmental, and behavioral factors that contribute to executive control abilities across development. Genetic influences are the dominant contributor, with twin studies suggesting that genetic factors account for up to 90% of executive control trait variance, making it one of the most heritable of all cognitive phenotypic traits (see Morton, 2010 for review). Further, a twin study by Lenroot et al. (2009) found that genetic factors accounted for more than half of the variance in cortical thickness in the dorsolateral and medial areas of the prefrontal cortex, and these genetic effects increased between childhood and early adolescence. Several neurotransmitters, including dopamine, serotonin, and norepinephrine, are involved in executive control, and certain polymorphisms in genes that are associated with these neurotransmitters have in turn been linked with phenotypic differences in executive control in children (e.g., Althaus et al., 2009). Beyond genetic factors, early environmental considerations also affect executive control. For example, the association between childhood poverty and poorer executive control is well documented (e.g., Hackman, Gallup, Evans, & Farah, 2015; see Clark, James, & Espy, 2016 for consideration of associations between poverty, executive control and foundational cognitive abilities), and factors such as family structure (Sarsour et al., 2011), parenting practices (Bernier, Carlson, & Whipple, 2010), and the availability of home enrichment materials (Nelson et al., 2015) have all been linked to early executive control development. Finally, executive control can be affected by specific behaviors that may undermine executive abilities through their negative effects on brain development (e.g., substance use, major dietary deficiencies, chronic sleep deprivation; Spear & Silveri, 2016).
Measurement of executive control in children and adolescents.
Investigation of child and adolescent executive control for both research and clinical purposes requires reliable and valid measurement of these abilities. The field has made great progress in developing and refining performance-based measures of youth executive control, often drawing from neuropsychological tasks originally designed for adults and then adapted for children and adolescents. Here, the need for tasks that are developmentally-appropriate and sufficiently sensitive to developmental gains should be apparent. Recognizing that preschool children, for example, cannot be given the same tasks as adolescents or adults, researchers have developed and validated individual tasks and multi-task batteries specifically for this critical developmental period (e.g., Beck, Schaefer, Pang, & Carlson, 2011). Common tasks appearing in the literature include developmentally-appropriate modifications of the go-no-go, Stroop test, Flanker task, list recall, sorting tasks, and other tasks believed to capture children’s executive control abilities (see Diamond, 2013 for review of executive control measurement). Although many studies rely on a single executive control task or only a couple of tasks, more extensive batteries have been developed in recent years to more comprehensively assess different aspects of developing executive control at different ages, including preschool (e.g., Espy, 2016) and adolescence (e.g., Lee et al., 2013). Expanded batteries have important advantages including a broader coverage of the executive control construct (as opposed to single-task measures, which usually assess only inhibitory control) and the ability to address the challenge of task impurity. Because performance on any individual executive control task necessarily draws on more than just the targeted ability–including abilities subordinate to executive control (Espy, 2016) – batteries including several tasks create the opportunity to distinguish what is shared across diverse tasks (and believed to reflect underlying executive control abilities) from task-specific and other non-executive control variance. Latent modeling approaches have become a popular method for statistically isolating executive control abilities drawn from children’s (Espy, 2016) and adolescents’ (e.g., Lee et al., 2013) performance on multi-task batteries, creating more “pure” representations of executive control.
In addition to performance-based tasks to measure youth executive control, norm-referenced questionnaires are available to assess problems with executive function across the developmental spectrum. For example, the Behavioral Rating Inventory of Executive Function – Second Edition (Gioia, Isquith, Guy, & Kenworthy, 2015) is a widely-used standardized rating system for assessing behavioral manifestations of executive dysfunction in children and adolescents (e.g., impulsive behaviors, problems completing tasks) on a day to day basis. Parents and teachers can report on symptoms for children as young as two years old, and a self-report version is available for older children and adolescents. As with any rating scale, caution is needed in interpreting subjective reports (from parent, teacher or child/adolescent), but norm-referenced measures can complement performance-based tasks as a part of multimethod assessment.
A Conceptual Model for the Impact of Executive Control on Adolescent Health
The role of executive control in health has been proposed in adults, with useful conceptual frameworks discussing possible mechanisms (see Hall & Marteau, 2014), but parallel developmentally-informed models for youth are currently lacking. Therefore, such a framework is proposed here, with an emphasis on pathways through which early executive control impairment may threaten health outcomes during adolescence and beyond (see Figure 1). The model is intentionally general, cutting across a range of physical and mental health problems, because executive control may impact key health behaviors and emotion regulation processes that affect risk for a variety conditions. It is proposed that poor executive control from early in development may compromise health through several mechanisms, including impairment in attentional, behavioral, and emotional control, as well as indirectly through academic difficulties.
Figure 1.
Conceptual Model for Youth Executive Control (EC) and Health.
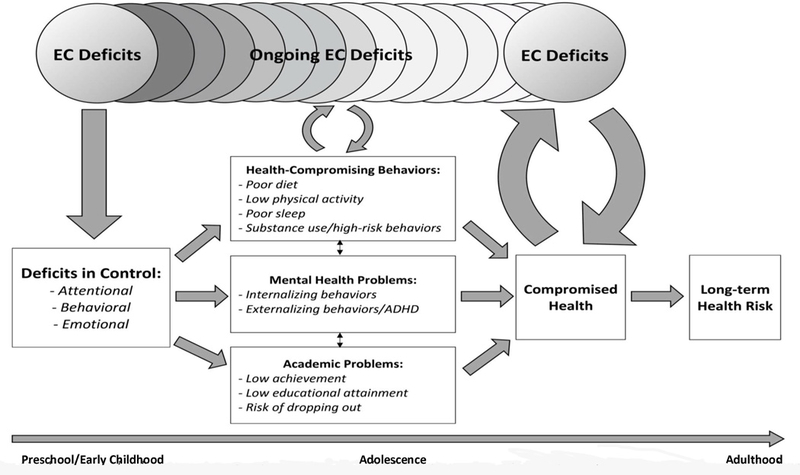
Note: Overlapping circles depict ongoing executive control (EC) development over time. EC is depicted as a single construct across development for the sake of simplicity in the figure; however, EC is known to progress from a single unitary construct in preschool to a differentiated set of related components (inhibitory control, working memory, flexible shifting) by adolescence
Attentional Control
The first potential mechanism by which executive control may affect adolescent health is through attentional control. Deficits in executive control may undermine the youth’s ability to control and direct attention in ways that support health. Consistent with the “impairment disengagement hypothesis,” individuals with poor executive control may find it particularly difficult to interrupt negative thought patterns and redirect their attention to more positive stimuli (Koster, De Lissnyder, Derakshan, & De Raedt, 2011). Therefore, executive control deficits contribute to perseverative and repetitive thoughts because the individual cannot effectively disengage from these thoughts and focus attention elsewhere. The impaired disengagement mechanism has been proposed primarily to explain how poor executive control can contribute to internalizing problems such as depression or anxiety (Koster et al., 2011), but it may also apply to problems with key child and adolescent health behaviors. For example, children and adolescents with poor executive control may have difficulty directing their attention away from tempting environmental or internal stimuli suggesting they engage in unhealthy food consumption, especially as parental supervision typically decreases during adolescence. Youth are frequently bombarded with advertisements for fast food, energy-dense snacks and sugary beverages, and those with deficits in executive control may be especially vulnerable to over-attending to these cues for unhealthy consumption because they cannot direct their attention elsewhere. These adolescents may also be at risk for excessive rumination about desired (but unhealthy) foods because they struggle to disengage from repetitive thoughts about consumption. Similarly, internal stimuli such as cravings may be especially powerful for youth with poor executive control because they may lack the cognitive control to shift attention away from thoughts that are likely to ultimately lead to unhealthy behavior. The inability to disengage from negative or unhealthy thoughts may also interfere with key health behaviors such as sleep because rumination on negative thoughts can interfere with sleep onset. In contrast, strong executive control allows for better attentional control, including disengaging from unhealthy thoughts and environmental triggers to allow for redirection of attention to more health-promoting stimuli. Better attentional control in turn supports healthier behavior and, ultimately, better health outcomes.
Behavioral Control
Another mechanism that could link executive control and youth health outcomes is behavioral control. In addition to underlying direction of attention, executive control is critical in supporting the intentional direction of behavior toward goals (Diamond, 2013). Deficits in any of the major components of executive control, therefore, could result in problems with behavioral control. Perhaps most obviously, poor inhibitory control could undermine efforts to resist engaging in an immediately gratifying, but potentially unhealthy, behavior. For example, energy-dense and high-sugar snacks are usually considered quite palatable and therefore are immediately rewarding to consume in the moment, even though the long-term effects of this consumption are well-known to be detrimental. Refraining from such consumption – either by abstaining entirely or limiting portion size – requires inhibition of the prepotent behavioral response, an ability that is compromised in adolescents with poor executive control. Further, strong inhibitory control also allows for more than merely resisting an unhealthy behavior, but also makes it possible to direct behavior toward a different (and perhaps more healthful) activity. This kind of intentional behavioral direction toward healthy goals may be a challenge for many children and adolescents, but it would seem virtually impossible for those with deficits in inhibitory control.
Although inhibitory control is well-recognized as critical to healthy behavior, the other aspects of executive control – working memory and flexible shifting – may also play a key, yet under-appreciated, role in behavioral control. Working memory supports remembering and updating personal health behavior goals and strategies in the moment, especially when distracted by tempting environmental stimuli. For example, working memory is needed to recall individual dietary plans when making food choices in the moment, and individuals with poor working memory may frequently forget the goals they set until after they have made food choices inconsistent with those goals. Finally, flexible shifting is needed to flexibly pursue health goals in the face of environmental obstacles. For example, making healthy food decisions while eating away from home or engaging in physical activity amid competing scheduling demands requires considerable cognitive flexibility and problem-solving to plan – and ultimately enact – health behaviors. For adolescents with deficits in flexible shifting, problem-solving and planning may be compromised, resulting in a disconnect between behavioral intentions and actual behavior, contributing to behavior patterns that compromise long-term health.
Emotional Control
A third mechanism by which executive control may impact health trajectories is through emotional control. Executive control plays an important role in the “top-down” control of emotions, and executive control is critical in developing emotion regulation abilities (Carlson & Wang, 2007). Connections between the prefrontal cortex and emotion centers in the brain allow for executive oversight to provide a “check” on negative emotions like fear, anxiety, and anger. Poor executive control, however, undermines this top-down regulatory process and may allow for chronically “unchecked” negative emotions that can threaten health over time. Chronic depression, anxiety, and anger have all been linked to long-term risk for physical health conditions and associated impairment (see Gallo & Matthews, 2003). The risk for “unchecked” negative emotions may be particularly apparent in adolescence, when amygdala hyperactivity has been observed (Guyer et al., 2008), necessitating regulation from the still-immature prefrontal cortex. Effective top-down regulation is a challenge for many adolescents due to the developmental mismatch between active emotion centers and still-developing prefrontal cortex (as evidenced by increases in depression symptoms in adolescence; Merikangas et al., 2010), but executive control deficits can further widen this gap, thus contributing to risk for significant emotional difficulties (Nelson et al., 2018) and associated physical health risks.
Executive control deficits may also disrupt the healthy development of physiological and psychological responses to stress. Poor executive control is associated with negative emotions such as depression and anxiety (Kertz et al., 2016), and research shows that clinical depression can have deleterious effects on physiological stress response systems (Burke et al., 2005), which develop throughout childhood and adolescence. This can lead to patterns of dysfunctional stress reactivity, which in turn can increase risk for a variety of chronic health conditions (Chida & Steptoe, 2010). Detrimental effects on how the body responds to stress may be particularly problematic in adolescence, when social stressors are common, and in high-risk environments, in which stressful experiences often cluster. Executive control may also be important for psychological responses to stress like active coping. Specifically, executive control may support intentional efforts to regulate emotions by engaging in coping behaviors such as stress-reducing activities and actively seeking appropriate social support during difficult times. On the other hand, children and adolescents with poor executive control may struggle to direct their thoughts and behavior in a way that supports effective emotion regulation, resulting in increased risk for long-term stress-related health problems.
Academic Failure
In addition to the mechanisms discussed above, executive control deficits may also compromise health through more indirect pathways, including the academic consequences of poor early executive control. Notably, executive control deficits have been consistently associated with poor academic outcomes (Bull, Espy, Wiebe, Sheffield, & Nelson, 2011), and a large body of research has linked lower educational attainment to long term risk for chronic disease (Smith, Anderson, Salinas, Horvatek, & Backer, 2015). Given these associations, it is possible that poor executive control early in life is a risk factor for long term health problems through its negative effects on academic performance.
Summary of Conceptual Model
Taken together, the attentional, behavioral, emotional, and indirect mechanisms proposed above could work in concert to undermine health for children and adolescents with poor executive control (see Figure 1). Specifically, deficits in executive control abilities emerging early in life may set the stage for long-term negative impacts on health. Early deficits that are not remediated may persist throughout childhood and adolescence when key health behavior patterns are forming and health behavior independence creates a demand for strong executive control to direct behavior toward health. Engaging in unhealthy behaviors during childhood and adolescence could result in both short-term adverse health effects (e.g., risk for obesity and related conditions) and more long-term risk (e.g., type II diabetes, emerging cardiovascular disease risk). While some studies have shown links between poor early executive control and emerging health concerns in childhood (Nelson et al., 2017) and early adolescence (Anzman et al., 2009), long-term studies are needed to document the full impact of EC deficits for chronic disease into adolescence and beyond. Understanding the lifelong implications of poor executive control could inform powerful prevention and early intervention strategies with potential long-term impact.
Although the current conceptual framework focuses primarily on how executive control may affect youth health trajectories, it is important to note that associations between executive control and health are likely bidirectional. In fact, substantial research has documented the negative effect of certain chronic health conditions – both physical and mental – on executive control abilities. For example, studies have shown the negative effects of conditions such as obesity (Smith, Hay, Campbell, & Trollor, 2011) and depression (Snyder, 2013) on individual executive control. Similarly, substance abuse can compromise executive control during vulnerable developmental periods (Nixon, 2013). Therefore, it is likely that executive control deficits and health problems interact in a cyclical way over time (as depicted by bidirectional arrows in Figure 1), with poor early executive control leading to compromised health, which in turn further compromises executive control, and so on.
Youth Executive Control and Key Health Behaviors: A Survey of the Literature
Consistent with the conceptual framework presented, the effects of executive control on health are likely at least partially mediated through key health behaviors that develop and solidify in childhood and adolescence. Therefore, provided here is a brief discussion of how executive control might influence some of the most important youth health behaviors – diet, physical activity, sleep, and substance use – as well as a brief summary of the extant literature on associations between executive control and these behaviors in pediatric samples. These reviews are not meant to be exhaustive but rather illustrative of some of the emerging evidence for links between youth executive control and critical health behaviors.
Executive Control and Diet
One key health behavior that has received considerable theoretical and empirical attention in the child and adolescent executive control literature is diet. As discussed in the conceptual model, healthy dietary behavior requires repeated direction of attention and behavior toward foods goals (e.g., consumption of healthy foods, limited intake of unhealthy food, portion size control), which requires an individual to draw on executive control, particularly in the face of ubiquitous environmental cues for unhealthy consumption (Martin & Davidson, 2014). Along these lines, studies have found associations between poor executive control abilities and greater intake of high-calorie snacks (Riggs, Chou, Spruijt-Metz, & Pentz, 2010), lower consumption of fruits and vegetables (Riggs et al., 2010), and more eating in the absence of hunger (Pieper & Laugero, 2013). Research with pediatric samples has also linked inhibitory control, specifically, with greater energy intake (Tan & Holub, 2010) and overeating (van den Berg et al., 2011). Relatedly, an emerging body of literature has documented longitudinal associations between child EC abilities and greater subsequent BMI accumulation (Anzman et al., 2009) and risk for clinical weight problems (Nelson et al., 2017).
Executive Control and Physical Activity
Executive control may also be important in supporting regular physical activity for children and adolescents. Youth must refrain from engaging in other immediately gratifying sedentary activities (e.g., watching television, playing video games) and instead direct attention and behavior toward being active. Consistent physical activity may also require cognitive flexibility to find opportunities for activity in the face of time limitations or built environments that do not provide easy exercise opportunities. Research to date on youth executive control as a predictor of physical activity is relatively limited (although a more robust literature demonstrates effects in the opposite direction with physical activity improving executive control; e.g., Hillman et al., 2014). Concurrent associations have been found between poor executive control and low physical activity (see Hall & Marteau, 2014 for review), but more research is needed to explicate longitudinal relations.
Executive Control and Sleep
Executive control abilities could play a key role in developing healthy sleep habits in childhood and adolescence. Establishing and maintaining a regular sleep schedule requires setting clear sleep goals and then directing behavior toward meeting those goals consistently. In adolescence, academic and social demands often extend into the evening hours, so adolescents must draw heavily on executive control abilities to manage their time and get to bed at the target bedtime each night. Further, children and adolescents must control their attention and behavior in preparation for sleep by “down-regulating” from the activity of the day and transitioning into sleep at night. Individuals with poor executive control may find it especially difficult to “wind down” at bedtime and “turn off” sleep-interfering cognitive processes (e.g., rumination), resulting in difficulty falling asleep and insufficient sleep duration. Research on youth executive control affecting sleep is quite limited. (Again, more research has focused on the reverse association, with poor sleep leading to compromised executive control.) In a rare longitudinal study, Nelson and colleagues (2016) found that poorer early executive control (in preschool) predicted later sleep/wake problems and daytime sleepiness in early adolescence.
Executive Control and Substance Use
It is also plausible that executive control abilities protect against substance involvement (Pentz & Riggs, 2013), a health risk behavior which typically emerges in adolescence (Miech et al., 2018). For example, working memory may be critical in retaining and acting on information related to substance use norms and rules that support substance non-use. Inhibitory control may be essential in refraining from immediately gratifying, but unhealthy, substance intake in favor of delayed onset, as well as in redirecting attention away from substance-related cues in the environment. Flexible shifting may be important for breaking unhealthy habits and problem-solving ways to avoid substance involvement (e.g., in the face of a substance offer). Executive control in late childhood and adolescence has been shown to be associated with substance use initiation and frequency of use, both cross-sectionally (Giancola & Mezzich, 2003) and longitudinally (Peeters et al., 2015). For example, Pentz and Riggs (2013) found that a composite measure of executive cognitive function, measured via self-report in a sample of fourth-graders, was associated negatively with lifetime alcohol and tobacco use six months later. More commonly, investigators have examined only certain aspects of executive control, usually response inhibition, in relation to substance use, with findings generally showing that inhibition in school-aged children and adolescents is a significant correlate and predictor of substance use (e.g., delayed alcohol onset; Nigg et al., 2006). Other aspects of childhood and adolescent executive control, such as working memory, have received less attention, but also have been shown to be negatively related to substance use (e.g., Khurana et al., 2013). However, additional studies have reported non-significant associations of executive control abilities with substance use (e.g., Wilens et al., 2011), particularly in clinical samples of youth (e.g., those with attention-deficit/hyperactivity disorder).
Executive Control and Psychopathology
Although not a health behavior, per se, executive control may affect physical health partially through its effects on youth psychopathology. A thorough review of the extensive literature linking poor executive control with psychopathology is beyond the scope of this article, but it is worth noting some consistent findings. Executive control deficits have long been theorized to contribute to disruptive behavior problems such as attention-deficit/hyperactivity disorder and conduct problems (Barkley, 1997), and empirical research has generally supported these theories (Willcutt, Doyle, Nigg, Faraone, & Pennington, 2005). A smaller literature has examined youth executive control as a predictor of internalizing problems, with longitudinal studies finding that poor executive control in preschool, as measured by both performance-based tasks (Nelson et al., 2018) and caregiver ratings (Kertz et al., 2016) is a precursor to depression and/or anxiety. Given the physical health implications of chronic psychopathology (Gallo & Matthews, 2003), it is possible that early executive control deficits contribute to the development of psychopathology, which in turn undermine long-term physical health trajectories, although longitudinal studies examining such pathways are needed.
Executive Control and Health Disparities
As suggested in Figure 1, poor executive control can undermine youth health through its effects on key health behaviors and mental health functioning, with individual differences in early executive control affecting individual health trajectories throughout childhood, adolescence, and beyond. However, it is worth noting that early executive control is associated with socioeconomic status, raising the possibility that executive control deficits are a mechanism by which early socioeconomic disadvantage is translated into long-term health risk. Studies have found that youth from lower socioeconomic status families have, on average, poorer executive control abilities (Hackman et al., 2015), perhaps due to growing up in less cognitively enriching early environments to support brain development (Sarsour et al., 2011). Poor early executive control development, in turn, can compromise health trajectories through the attentional, behavioral, and emotional pathways discussed in this article. Essentially, socioeconomic disadvantage early in life may critically undermine the healthy brain development needed to make and enact healthy choices across the lifespan. Research testing this socioeconomic status-executive control-health process contributing to health disparities is needed.
Implications for Intervention
Given the potential importance of executive control for child and adolescent health, we propose that health professionals consider incorporating executive control into their assessments, case conceptualizations, and interventions. Although formal executive control assessment is already common in some specific circumstances (e.g., assessing cognitive changes following certain cancer treatments), targeted executive control assessment could be utilized in a broader range of cases in which health-compromising behaviors are present (e.g., pediatric obesity, adolescent substance use, non-adherence to medical regimens). Relatedly, child and adolescent health psychologists should incorporate consideration of executive control deficits into their case conceptualizations, especially when youth appear to have difficulty directing their attention and behavior toward health goals. Finally, executive control should be considered as a potential target for prevention and intervention efforts to promote child and adolescent health. A significant body of research indicates that executive control is modifiable, with accumulating evidence suggesting the effectiveness of cognitive training (Diamond, 2013), physical exercise (Hillman et al., 2014), and other interventions in improving youth executive control (Diamond & Lee, 2011). Although outcomes vary, some studies have documented clinically significant improvements in executive control (Tamm, Nakoneznv, & Hughes, 2014), including normalization and sustained effects (Holmes et al., 2009). Further, it has been suggested that executive control interventions may have the greatest effect for youth with significant executive control deficits, and the critical periods of preschool and adolescence may be times of particular malleability for executive control (Zelazo & Carlson, 2012). The modifiability of executive control makes it a potentially ideal target for early intervention, but executive control enrichment remains a largely untapped area for child and adolescent health promotion.
Limitations of Existing Research and Future Directions
Although some literature has found associations between executive control and various youth health behaviors, this literature has important limitations. First, previous research in this area has suffered from an overly narrow conceptualization of executive control as synonymous with inhibitory control. While inhibitory control is certainly a critical component of executive control – and one that may be especially important for certain health behaviors – this almost exclusive focus on a single aspect of executive control has resulted in insufficient attention to other key components of the construct (i.e., working memory and flexible shifting). Therefore, it is recommended that future youth executive control-health research take a broader perspective on executive control abilities to reflect the rich conceptualizations of this construct that dominate the developmental executive control literature (e.g., Espy, 2016). Second, and relatedly, much of the executive control-health literature has been plagued by measurement issues. In addition to insufficient coverage of executive control components other than inhibitory control, there has also been an overreliance on subjective report measures instead of objective performance-based executive control tasks. While parent-, teacher- and youth-report questionnaires of executive impairments can provide valuable insights into child and adolescent functioning, the executive control -health literature would be strengthened by greater use of a multi-method measurement approach, including neuropsychological task batteries that more comprehensively and objectively assess youth abilities. Further, it is critical that these executive control tasks be developmentally appropriate for the age range being studied; tasks developed for adults may require substantial modification to ensure that they can be completed by children or adolescents and are sensitive enough to detect subtle but potentially important individual differences. Fortunately, recent years have seen increased attention to executive control testing in children (e.g., Espy, 2016) and adolescents (e.g., Lee et al., 2013), so well-conceptualized and validated batteries for different developmental periods are currently available. Of particular note is the National Institutes of Health Toolbox Cognition Battery, which includes tests of executive control and related abilities and provides extensive normative comparison data for children and adolescents (Zelazo & Bauer, 2013).
Third, much of the existing executive control-health literature has lacked attention to critical developmental considerations regarding the timing of typical executive control development. Although theory and empirical research identifies preschool and adolescence as critical periods in the development of executive control, studies assessing executive control across these developmental periods and linking developing abilities to key health constructs are limited. Fourth, longitudinal research examining early executive control as a precursor to subsequent health behaviors during adolescence – when key health behavior patterns often solidify – and clinical health outcomes remains rare. Longitudinal studies that assess executive control during critical periods and examine associations over time with developing key health behaviors and risk for chronic illness are needed to inform the timing of targeted intervention to bolster executive control and, consequently, promote long-term health. Further, studies with repeated measurements of both executive control and health constructs across development will be critical in determining causal directions and possible cyclical effects between poor executive control and compromised health. Finally, because youth executive control development is a promising potential target for health promotion intervention, it will be important to study the short- and long-term effects of executive control enhancement efforts on youth health behaviors and outcomes. Emerging evidence suggests that executive control can be improved with a variety of interventions, but the potential health benefits of stronger executive control are yet to be systematically examined.
Conclusions
Adolescence is a time of changing health behaviors and unique influences on health. Because health behavior patterns developed in adolescence can have both short- and long-term effects on an individual’s health, it is important to understand factors that contribute to health behaviors during this critical period. The current article argued that executive control is a cross-cutting factor affecting health trajectories across development and particularly in adolescence. Core deficits in executive control could have effects across many areas of health behaviors, leading to long-term risk for a range of health problems that may emerge in adolescence or beyond. Early deficits could alter developmental trajectories and create sequential cascades, with poor early executive control leading to compromised health behaviors, which in turn further compromise executive control, leading to a vicious cycle threatening physical and cognitive well-being over time. Fortunately, the protracted developmental trajectory of executive control across childhood and adolescence creates potential opportunities for intervention to remediate emerging deficits and positively impact health trajectories over time. The preceding literature review demonstrates emerging evidence for associations between executive control and health in youth. However, longitudinal studies with careful conceptualization and measurement of executive control and health constructs at critical periods are needed to better explicate the ways in which child and adolescent executive control affects health (and vice versa), and to inform the development and testing of novel intervention strategies to support youth health through executive control promotion. The conceptual model presented here provides a framework for guiding such research.
Acknowledgements
Funding
Preparation of this publication was supported by the National Institute On Drug Abuse of the National Institutes of Health under Award Number R01DA041738 and by the National Institute of Diabetes And Digestive and Kidney Diseases of the National Institutes of Health under Award Number R01DK116693. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest
The authors report no conflicts of interest.
References
- Allen JP, & Brown B (2008). Adolescents, peers, and motor vehicles: The perfect storm? Adolescent Development, 35(3), S289–S293. doi: 10.1016/j.amepre.2008.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Althaus M, Groen Y, Wijers AA, Mulder LM, Minderaa RB, Kema IP, &… Hoekstra PJ (2009). Differential effects of 5-HTTLPR and DRD2/ANKK1 polymorphisms on electrocortical measures of error and feedback processing in children. Clinical Neurophysiology, 120(1), 93–107. doi: 10.1016/j.clinph.2008.10.012 [DOI] [PubMed] [Google Scholar]
- Anzman SL, & Birch LL (2009). Low inhibitory control and restrictive feeding practices predict weight outcomes. The Journal of Pediatrics, 155(5), 651–656. doi: 10.1016/j.jpeds.2009.04.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA (1997). Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin, 121(1), 65–94. doi: 10.1037/0033-2909.121.1.65 [DOI] [PubMed] [Google Scholar]
- Bassett R, Chapman GE, & Beagan BL (2008). Autonomy and control: The co-construction of adolescent food choice. Appetite, 50(2–3), 325–332. doi: 10.1016/j.appet.2007.08.009. [DOI] [PubMed] [Google Scholar]
- Beck DM, Schaefer C, Pang K, & Carlson SM (2011). Executive function in preschool children: Test–retest reliability. Journal of Cognition and Development, 12(2), 169–193. doi: 10.1080/15248372.2011.563485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernier A, Carlson SM, & Whipple N (2010). From external regulation to self-regulation: Early parenting precursors of young children’s executive functioning. Child Development, 81(1), 326–339. doi: 10.1111/j.1467-8624.2009.01397.x [DOI] [PubMed] [Google Scholar]
- Best JR, & Miller PH (2010). A developmental perspective on executive function. Child Development, 81(6), 1641–1660. doi: 10.1111/j.1467-8624.2010.01499.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakemore S, & Choudhury S (2006). Development of the adolescent brain: Implications for executive function and social cognition. Journal of Child Psychology and Psychiatry, 47(3/4), 296–312. doi: 10.1111/j.1469-7610.2006.01611.x [DOI] [PubMed] [Google Scholar]
- Blair C, & Razza RP (2007). Relating effortful control, executive function, and false belief understanding to emerging math and literacy ability in kindergarten. Child Development, 78(2), 647–663. doi: 10.1111/j.1467-8624.2007.01019.x [DOI] [PubMed] [Google Scholar]
- Brydges CR, Fox AM, Reid CL, & Anderson M (2014). The differentiation of executive functions in middle and late childhood: A longitudinal latent-variable analysis. Intelligence, 47, 34–43. doi: 10.1016/j.intell.2014.08.010 [DOI] [Google Scholar]
- Bull R, Espy KA, Wiebe SA, Sheffield TD, & Nelson JM (2011). Using confirmatory factor analysis to understand executive control in preschool children: Sources of variation in emergent mathematic achievement. Developmental Science, 14(4), 679–692. doi: 10.1111/j.1467-7687.2010.01012.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke HM, Davis MC, Otte C, & Mohr DC (2005). Depression and cortisol responses to psychological stress: A meta-analysis. Psychoneuroendocrinology, 30(9), 846–856. doi: 10.1016/j.psyneuen.2005.02.010 [DOI] [PubMed] [Google Scholar]
- Carlson SM, & Wang TS (2007). Inhibitory control and emotion regulation in preschool children. Cognitive Development, 22(4), 489–510. doi: 10.1016/j.cogdev.2007.08.002 [DOI] [Google Scholar]
- Chida Y, & Steptoe A (2010). Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: A meta-analysis of prospective evidence. Hypertension, 55(4), 1026–1032. doi: 10.1161/hypertensionaha.109.146621 [DOI] [PubMed] [Google Scholar]
- Clark CAC, James TD, & Espy KA (2016). A new look at the implications of the socio-familial context for young children’s executive control: Clarifying the mechanisms of individual differences. Monographs of the Society for Research in Child Development, 81(4), 69–95. doi: 10.1111/mono.v81.4/issuetoc [DOI] [PubMed] [Google Scholar]
- Clark CAC, Sheffield TD, Chevalier N, Nelson JM, Wiebe SA, & Espy KA (2013). Charting early trajectories of executive control with the Shape School. Developmental Psychology, 49(8), 1481–1493. doi: 10.1037/a0030578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond A (2013). Executive functions. Annual Review of Psychology, 64, 135–168. doi: 10.1146/annurev-psych-113011-143750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond A, & Lee K (2011). Interventions shown to aid executive function development in children 4–12 years old. Science, 333(6045), 959–964. doi: 10.1126/science.1204529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espy KA (2016). The changing nature of executive control in preschool. Monographs of the Society for Research in Child Development, 81(4), 1–179. [DOI] [PubMed] [Google Scholar]
- Espy KA, Sheffield TD, Wiebe SA, Clark CAC, & Moehr MJ (2011). Executive control and dimensions of problem behaviors in preschool children. Journal of Child Psychology and Psychiatry, 52(1), 33–46. doi: 10.1111/j.1469-7610.2010.02265.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fair DA, Dosenbach NUF, Church JA, Cohen AL, Brahmbhatt S, Miezin FM,… Schlaggar BL (2007). Development of distinct control networks through segregation and integration. Proceedings of the National Academy of Sciences of the United States of America, 104(33), 13507–13512. doi: 10.1073/pnas.0705843104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo LC, & Matthews KA (2003). Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin, 129(1), 10–51. doi: 10.1037/0033-2909.129.1.10 [DOI] [PubMed] [Google Scholar]
- Giancola PR, & Mezzich AC (2003). Executive functioning, temperament, and drug use involvement in adolescent females with a substance use disorder. Journal of Child Psychology and Psychiatry, 44(6), 857–866. doi: 10.1111/1469-7610.00170 [DOI] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, & Kenworthy L (2015). Brief Rating Inventory of Executive Function, Second Edition (BRIEF-2) WPS Publishing. [Google Scholar]
- Guyer AE, Monk CS, McClure-Tone EB, Nelson EE, Roberson-Nay R, Adler AD, & … Ernst M (2008). A developmental examination of amygdala response to facial expressions. Journal of Cognitive Neuroscience, 20(9), 1565–1582. doi: 10.1162/jocn.2008.20114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackman DA, Gallop R, Evans GW, & Farah MJ (2015). Socioeconomic status and executive function: Developmental trajectories and mediation. Developmental Science, 18(5), 686–702. doi: 10.1111/desc.12246 [DOI] [PubMed] [Google Scholar]
- Hall PA, & Marteau TM (2014). Executive function in the context of chronic disease prevention: Theory, research and practice. Preventive Medicine, 68, 44–50. doi: 10.1016/j.ypmed.2014.07.008 [DOI] [PubMed] [Google Scholar]
- Hare TA, Tottenham N, Galvan A, Voss HU, Glover GH, & Casey BJ (2008). Biological substrates of emotional reactivity and regulation in adolescence during an emotional go-nogo task. Biological Psychiatry, 63(10), 927–934. doi: 10.1016/j.biopsych.2008.03.015015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillman CH, Pontifex MB, Castelli DM, Khan NA, Raine LB, Scudder MR, … Kamijo K (2014). Effects of the FITKids randomized controlled trial on executive control and brain function. Pediatrics, 134(4), e1063–e1071. doi: 10.1542/peds.2013-3219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes J, Gathercole SE, & Dunning DL (2009). Adaptive training leads to sustained enhancement of poor working memory in children. Developmental Science, 12(4), F9–F15. doi: 10.1111/j.1467-7687.2009.00848.x [DOI] [PubMed] [Google Scholar]
- Jaworska N, & MacQueen G (2015). Adolescence as a unique developmental period. Journal of Psychiatry and Neuroscience, 40(5), 291–293. doi: 10.1503/jpn.150268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kertz SJ, Belden AC, Tillman R, & Luby J (2016). Cognitive control deficits in shifting and inhibition in preschool age children are associated with increased depression and anxiety over 7.5 years of development. Journal of Abnormal Child Psychology, 44(6), 1185–1196. doi: 10.1007/s10802-015-0101-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana A, Romer D, Betancourt LM, Brodsky NL, Giannetta JM, & Hurt H (2013). Working memory ability predicts trajectories of early alcohol use in adolescents: The mediational role of impulsivity. Addiction, 108(3), 506–515. doi: 10.1111/add.12001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koster EW, De Lissnyder E, Derakshan N, & De Raedt R (2011). Understanding depressive rumination from a cognitive science perspective: The impaired disengagement hypothesis. Clinical Psychology Review, 31(1), 138–145. doi: 10.1016/j.cpr.2010.08.005 [DOI] [PubMed] [Google Scholar]
- Lake AA, Adamson AJ, Craigie AM, Rugg-Gunn AJ, & Mathers JC (2009). Tracking of dietary intake and factors associated with dietary change from early adolescence to adulthood: The ASH30 study. Obesity Facts, 2(3), 157–165. doi: 10.1159/000219819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K, Bull R, & Ho RM (2013). Developmental changes in executive functioning. Child Development, 84(6), 1933–1953. doi: 10.1111/cdev.12096 [DOI] [PubMed] [Google Scholar]
- Lenroot RK, Schmitt JE, Ordaz SJ, Wallace GL, Neale MC, Lerch JP, & … Giedd JN (2009). Differences in genetic and environmental influences on the human cerebral cortex associated with development during childhood and adolescence. Human Brain Mapping, 30(1), 163–174. doi: 10.1002/hbm.20494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luna B, Garver KE, Urban TA, Lazar NA, & Sweeney JA (2004). Maturation of cognitive processes from late childhood to adulthood. Child Development, 75(5), 1357– 1372. doi: 10.1111/j.1467-8624.2004.00745.x [DOI] [PubMed] [Google Scholar]
- Luna B, Padmanabhan A, & O’Hearn K (2010). What has fMRI told us about the development of cognitive control through adolescence? Brain and Cognition, 72(1), 101– 113. doi: 10.1016/j.bandc.2009.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luna B, Marek S, Larsen B, Tervo-Clemmens B, & Chahal R (2015). An integrative model of the maturation of cognitive control. Annual Review of Neuroscience, 38, 151– 170. doi: 10.1146/annurev-neuro-071714-034054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin AA, & Davidson TL (2014). Human cognitive function and the obesogenic environment. Physiology & Behavior, 136, 185–193. doi: 10.1016/j.physbeh.2014.02.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElhaney K, Allen J, Stephenson J, & Hare A (2009). Attachment and autonomy during adolescence. In Lerner RM, & Steinberg L (Eds.), Handbook of adolescent psychology, Vol. 1: Individual bases of adolescent development (3rd ed., pp. 358–403). Hoboken, NJ: John Wiley. [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. doi: 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2018). Monitoring the Future national survey results on drug use, 1975–2017: Volume I, Secondary school students Ann Arbor, MI: Institute for Social Research, The University of Michigan. [Google Scholar]
- Moriguchi Y, & Hiraki K (2009). Neural origin of cognitive shifting in young children. PNAS Proceedings of the National Academy of Sciences of the United States of America, 106(14), 6017–6021. doi: 10.1073/pnas.0809747106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton JB (2010). Understanding genetic, neurophysiological, and experiential influences on the development of executive functioning: The need for developmental models. Wiley Interdisciplinary Reviews: Cognitive Science, 1(5), 709–723. doi: 10.1002/wcs.87 [DOI] [PubMed] [Google Scholar]
- Nelson JM, Choi HJ, Clark CA, James TD, Fang H, Wiebe SA, & Espy KA (2015). Sociodemographic risk and early environmental factors that contribute to resilience in executive control: A factor mixture model of 3-year-olds. Child Neuropsychology, 21(3), 354–378. doi: 10.1080/09297049.2014.910300 [DOI] [PubMed] [Google Scholar]
- Nelson TD, James TD, Hankey M, Nelson JM, Lundahl A, & Espy KA (2017). Early executive control and risk for overweight and obesity in elementary school. Child Neuropsychology, 23(8), 994–1002. doi: 10.1080/09297049.2016.1183606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson TD, Kidwell KM, Hankey M, Nelson JM, & Espy KA (2016). Preschool executive control and sleep problems in early adolescence. Behavioral Sleep Medicine Advance online publication. doi: 10.1080/15402002.2016.1228650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson TD, Kidwell KM, Nelson JM, Tomaso CC, Hankey M, & Espy KA (2018). Preschool executive control and internalizing symptoms in elementary school. Journal of Abnormal Child Psychology doi: 10.1007/s10802-017-0395-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT, Wong MM, Martel MM, Jester JM, Puttler LI, Glass JM, & … Zucker RA (2006). Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 45(4), 468–475. doi: 10.1097/01.chi.0000199028.76452.a9 [DOI] [PubMed] [Google Scholar]
- Nixon SJ (2013). Executive functioning among young people in relation to alcohol use. Current Opinion in Psychiatry, 26(4), 305–309. doi: 10.1097/YCO.0b013e328361ea3c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters M, Janssen T, Monshouwer K, Boendermaker W, Pronk T, Wiers R, & Vollebergh W (2015). Weaknesses in executive functioning predict the initiating of adolescents’ alcohol use. Developmental Cognitive Neuroscience, 16, 139–146. doi: 10.1016/j.dcn.2015.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pentz MA, & Riggs NR (2013). Longitudinal relationships of executive cognitive function and parent influence to child substance use and physical activity. Prevention Science, 14(3), 229–237. doi: 10.1007/s11121-012-0312-3 [DOI] [PubMed] [Google Scholar]
- Pieper JR, & Laugero KD (2013). Preschool children with lower executive functioning may be more vulnerable to emotion-based eating in the absence of hunger. Appetite, 62, 103– 109. doi: 10.1016/j.appet.2012.11.020 [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, & Dodge KA (2008). Understanding peer influence in children and adolescents New York, NY: The Guilford Press. [Google Scholar]
- Riggs N, Chou CP, Spruijt-Metz D, & Pentz MA (2010). Executive cognitive function as a correlate and predictor of child food intake and physical activity. Child Neuropsychology, 16(3), 279–292. doi: 10.1080/09297041003601488 [DOI] [PubMed] [Google Scholar]
- Rose SA, Feldman JF, & Jankowski JJ (2011). Modeling a cascade of effects: The role of speed and executive functioning in preterm/full-term differences in academic achievement. Developmental Science, 14(5), 1161–1175. doi: 10.1111/j.1467-7687.2011.01068.x [DOI] [PubMed] [Google Scholar]
- Sarsour K, Sheridan M, Jutte D, Nuru-Jeter A, Hinshaw S, & Boyce WT (2011). Family socioeconomic status and child executive functions: The roles of language, home environment, and single parenthood. Journal of the International Neuropsychological Society, 17(1), 120–132. doi: 10.1017/S1355617710001335 [DOI] [PubMed] [Google Scholar]
- Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, & Patton GC (2012). Adolescence: A foundation for future health. Lancet, 379(9826): 1630–1640. doi: 10.1016/S0140-6736(12)60072-5 [DOI] [PubMed] [Google Scholar]
- Selemon LD (2013). A role for synaptic plasticity in the adolescent development of executive function. Translational Psychiatry, 3, e238. doi: 10.1038/tp.2013.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith WC, Anderson E, Salinas D, Horvatek R, & Baker DP (2015). A meta-analysis of education effects on chronic disease: The causal dynamics of the Population Education Transition Curve. Social Science & Medicine, 127, 29–40. doi: 10.1016/j.socscimed.2014.10.027 [DOI] [PubMed] [Google Scholar]
- Smith E, Hay P, Campbell L, & Trollor JN (2011). A review of the association between obesity and cognitive function across the lifespan: Implications for novel approaches to prevention and treatment. Obesity Reviews, 12(9), 740–755. doi: 10.1111/j.1467-789X.2011.00920.x [DOI] [PubMed] [Google Scholar]
- Snyder HR (2013). Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: A meta-analysis and review. Psychological Bulletin, 139(1), 81–132. doi: 10.1037/a00287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP, & Silveri MM (Eds.) (2016). The Adolescent Brain [Special issue]. Neuroscience & Biobehavioral Reviews, 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamm L, Nakonezny PA, & Hughes CW (2014). An open trial of a metacognitive executive function training for young children with ADHD. Journal of Attention Disorders, 18(6), 551–559. doi: 10.1177/1087054712445782 [DOI] [PubMed] [Google Scholar]
- Tan CC, & Holub SC (2011). Children’s self-regulation in eating: Associations with inhibitory control and parents’ feeding behavior. Journal of Pediatric Psychology, 36(3), 340–345. doi: 10.1093/jpepsy/jsq089 [DOI] [PubMed] [Google Scholar]
- Van der Ven SH, Kroesbergen EH, Boom J, & Leseman PP (2012). The development of executive functions and early mathematics: A dynamic relationship. The British Journal of Educational Psychology, 82, 100–119. doi: 10.1111/j.2044-8279.2011.02035.x [DOI] [PubMed] [Google Scholar]
- van den Berg L, Pieterse K, Malik JA, Luman M, van Dijk KW, Oosterlaan J, & Delemarre-van de Waal HA (2011). Association between impulsivity, reward responsiveness and body mass index in children. International Journal of Obesity, 35(10), 1301–1307. doi: 10.1038/ijo.2011.116 [DOI] [PubMed] [Google Scholar]
- Wiebe SA, Sheffield TD, Nelson JM, Clark CAC, Chevalier N, & Espy KA (2011). The structure of executive function in 3-year-olds. Journal of Experimental Child Psychology, 108(3), 436–452. doi: 10.1016/j.jecp.2010.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilens TE, Martelon M, Fried R, Petty C, Bateman C, & Biederman J (2011). Do executive function deficits predict later substance use disorders among adolescents and young adults? Journal of The American Academy of Child and Adolescent Psychiatry, 50(2), 141–149. doi: 10.1016/j.jaac.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, & Pennington BF (2005). Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry, 57(11), 1336–1346. doi: 10.1016/j.biopsych.2005.02.006 [DOI] [PubMed] [Google Scholar]
- Zelazo PD, & Bauer PJ (2013). National Institutes of Health Toolbox Cognition Battery (NIH Toolbox CB): Validation for children between 3 and 15 years. Monographs of the Society for Research in Child Development, 78(4), 1–172. [DOI] [PubMed] [Google Scholar]
- Zelazo PD, & Carlson SM (2012). Hot and cool executive function in childhood and adolescence: Development and plasticity. Child Development Perspectives, 6(4), 354–360. doi: 10.1111/j.1750-8606.2012.00246 [DOI] [Google Scholar]


