Abstract
Background
There are few data comparing patient reported outcomes (PROs) in randomized trials of initial antiretroviral therapy (ART). We present results from a substudy of the NEAT001/ANRS143 trial.
Methods
The randomized trial compared first-line DRV/r 800/100mg once daily plus RAL 400mg twice daily and DRV/r plus TDF/FTC 245/200mg once daily. Changes in PROs were assessed with 3 questionnaires: EuroQoL 5 domains (EQ-5D), Centre for Epidemiologic Studies Depression scale (CES-D), and HIV Treatment Satisfaction (HIVTSQ). Major Depressive Disorder (MDD) was defined as CES-d≥16. General estimating equations were used to model change over 96 weeks in PROs from baseline.
Results
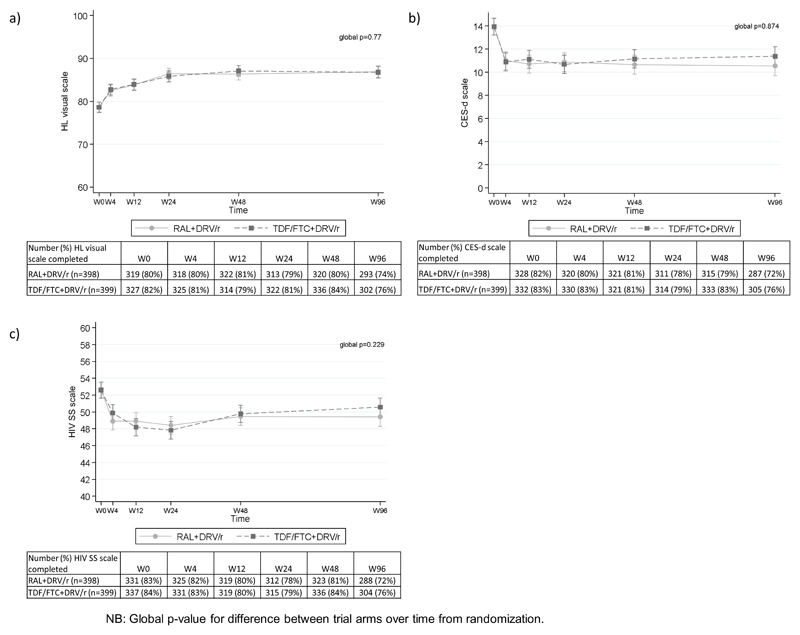
Of the 805 participants, 797(99%) contributed to the substudy. Baseline PROs data were similar for the two randomized groups. Health status improved over time with a mean increase in EQ-5D visual analogue scale of 8.0 by W96 (95%CI 6.5-9.4; p<0.001), and no statistically significant differences between groups (difference of 0.3 on VAS score (95%CI -1.7, 2.3); p=0.7, global p-value ≥0.05 for all domains over follow-up). There was no significant difference between groups on CES-D (difference of -0.1 (95%CI -1.3, 1.1); p=0.9), or MDD during follow-up, adjusted for baseline MDD (OR=0.98, 95%CI 0.82-1.18; p=0.9). RAL+DRV/r group had lower level of convenience (p=0.03) and fitted less well into patients’ lifestyle (p=0.007) than the TDF/FTC+DRV/r regimen, and was associated with lower treatment satisfaction (median score: 53 RAL+DRV/r vs 55 TDF/FTC+DRV/r (p=0.001).
Conclusion
PROs improved after starting ART, with no statistically significant difference between groups. The lower satisfaction with RAL+DRV/r may be explained by twice-daily administration.
Keywords: Quality of life, raltegravir, treatment satisfaction, EQ5D, ritonavir-boosted darunavir, health improvement
Introduction
Antiretroviral therapy (ART) has dramatically reduced mortality and morbidity at all stages of HIV infection 1,2, making an overall improvement of patients’ health status an important goal of therapy. In fact, according to most recent guidelines, one of the key treatment goals is to “prolong the quality of survival” 3. In this context, patient-reported outcomes (PROs) have been recognized as an important measure of health that deserves to be taken into account, together with the traditional efficacy and safety parameters, when measuring a patient’s health status both in research and clinical practice. Indeed, there is compelling evidence that both HIV infection and prolonged ART can impair PROs such as health-related quality of life (HRQL), fatigue, and work productivity 4. Assessment of PROs measures is of particular interest when two or more therapeutic strategies have the same clinical efficacy, as PROs are the major drivers of adherence to long-term ART 5. In fact, PROs during treatment may explain the gap that is frequently reported between efficacy rates and those reported for the effectiveness of ART in the real world practices. PROs are also important surrogates for patients’ experience with their disease and its treatment 6. Combined, these reasons make PROs important endpoints for clinical trials to identify the strategy that maximize the patient’s health status, and irreplaceable sources of important information in clinical practice 7. A large European NEAT001/ANRS143 randomized multicenter trial which compared two different ART regimens for 1st-line treatment in naïve patients showed non-inferiority based on a virological composite primary outcome at 96 weeks. There was also no difference in the frequency of serious or treatment modifying adverse events. We report the results of a specific PROs’ substudy nested within the NEAT001/ANRS143 large clinical trial.
Participants and methods
Study treatment and participants
NEAT001/ANRS143 was a randomized, open-label, non-inferiority trial conducted in 15 European countries between August 2010, and October 2013. The full study design and results have been previously reported 8. Briefly 805 naive HIV-infected adults were randomly assigned in a 1:1 ratio to receive oral treatment with 800mg darunavir and 100mg ritonavir once daily plus either 400mg raltegravir twice daily (NtRTI-sparing regimen) or tenofovir/emtricitabine in a 245mg and 200mg fixed dose combination once daily (standard regimen). Participants were offered to participate in the PROs’ substudy. Ethics committee approval was obtained for all participating centers, in accordance with the principles of the Declaration of Helsinki. All trial participants gave written informed consent. The study was registered with ClinicalTrials.gov (NCT01066962).
Data collection
Participants attended study centers at screening, baseline (randomization), weeks 2, 4, 8, 12, 18, 24, 32, 48, 64, 80, and 96, and every 12-16 weeks thereafter. Each visit included assessment of vital signs and adverse events, physical examination, and collection of blood samples for full blood cell counts and serum chemistry, liver function and immuno-virological measurements, except at W2 for the latter. Adverse events recorded during the study were grouped based on the body system as previously described 8.
Patient-reported outcomes
PROs were collected at baseline and during scheduled follow up visits at weeks 4, 12, 24, 48 and 96 through self-administered questionnaires in participants’ native languages. Four PROs questionnaires were used in this study: 1) The EuroQoL 5 domains (EQ-5D) 9, a widely used generic questionnaire for measuring health related quality of life (HRQoL), that includes two parts. The EQ-5D self-classifier asks participants to describe their health on five domains: (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) and three levels: 1 indicating “no problem,” 2 indicating “some or moderate problems,” and 3 indicating “extreme problems/impossible to do.” The EQ-VAS is a visual analogue scale that takes values between 100 (best imaginable health) and 0 (worst imaginable health) on which participants provide an overall measure of their health status; 2) The ISS-NEAT HIV Symptoms scale, a self-administered list of 38 symptoms 10, that evaluates the impact of symptoms over the last 4 weeks through a Likert five-point intensity scale rated from ‘not at all’=1 to ‘a very great deal’=5; 3) The Center for Epidemiological Studies-Depression (CES-D), that asks participants to rate how often over the past week they experienced symptoms associated with depression, with response options ranging from 0 to 3 for each item (0 = rarely or none of the time, 1 = some or little of the time, 2 = occasionally or moderately, 3 = most or all the time). Major Depressive Disorder (MDD) was defined as CES-D ≥16. In this study a short version of 10 items was used 11; 4) The HIV Treatment Satisfaction Questionnaire (HIVTSQ) measuring overall satisfaction with HIV treatment and by specific domains such as convenience, ease of use, and flexibility through a 10-item self-reported scale with a maximum possible score of 60 12.
Statistical analysis
Together with clinico-demographic parameters, the PROs at and during follow-up were compared between the 2 trial treatments using Pearson's chi-square test for categorical variables or t-tests and Wilcoxon ranksum tests for continuous variables. The two treatment groups were compared as randomized, according to the intention-to-treat principle. Generalised estimating equations (GEEs) including all participants that contributed one or more questionnaires were used to model: change over time in PROs from baseline; odds of MDD during the trial adjusted for baseline MDD; and odds of having moderate or severe problems (compared to no problems) on EQ5D domains adjusted for baseline levels. GEEs were used as the models can handle missing measurements without the need for imputation and have been shown to be a viable analysis for PROs in HIV trial data.13 Within the GEE models, potential differences between arms and visit weeks were accounted for with interaction terms. Sensitivity analyses were carried out by imputing missing values of PROs at each time point using multiple imputation with chained equations (with predictive mean matching for CES-D and EQ-VAS, and regression for HIV symptom score) and then changing the imputed values to test the assumption that the group who had missing data had systematically worse or better outcomes14. Baseline factors that were associated with change in EQ5D VAS scale over time (age, gender, country of enrolment, body mass index (BMI), mode of infection, ethnicity, HIV stage, CD4 and log10 plasma HIV RNA) were included in the GEE model. Levels of treatment satisfaction between groups were compared with chi-squared tests in participants with questionnaires at baseline and W96 and logistic regression for the % very satisfied at W96 adjusted for baseline factors. This timepoint was in line with the primary endpoint for the main trial measured once all participants had reached W96. For this PROs’ substudy, no predetermined sample size was calculated. Statistical analyses were performed using Stata v14.0.
Results
Baseline characteristics and data completeness
Of the 805 participants, 797 (99%) contributed to the substudy: 683/797 (86%) at baseline, 611 (77%) at W96, 526 (66%) at both visits. A minimum of 74% participants contributed to PRO data at each visit and >80% contributed at visits within the first 12 weeks (Figure 1A). There was no significant difference between randomized groups for completeness of data at each visit and overall (global p-value from GEE models for missingness of CES-D scale, EQ-VAS and HIV symptom scale score was 0.10, 0.41, and 0.28 respectively). Baseline characteristics and PROs of the participants contributing at baseline were not different between treatment groups (Table 1) and were similar to those of the 805 participants randomized to the main NEAT001/ANRS143 trial.
Figure 1.
Table 1. Baseline patient reported outcomes and characteristics.
| Patient Reported Outcomes | RAL + DRV/r | TDF/FTC + DRV/r |
| Median (IQR) CES-d score ; N | 12 (7, 18); 328 | 12 (7, 19); 332 |
| Major Depressive Disorder (MDD) (%) | 121/328 (37%) | 110/332 (33%) |
| Median (IQR) HIV Symptom scale ; N | 49 (43, 59); 331 | 49 (42, 59); 337 |
| Euroqol EQ5D domains (% moderate or severe problems) | ||
| Mobility | 11/335 (3%) | 11/342 (3%) |
| Self-care | 2/335 (<1%) | 5/341 (1%) |
| Usual Activities | 26/336 (8%) | 26/340 (8%) |
| Pain/Discomfort | 79/335 (24%) | 90/341 (26%) |
| Anxiety/Depression | 143/336 (43%) | 145/340 (43%) |
| Median (IQR) EQ5D VAS; N | 80 (70-90); 319 | 80 (70-90); 327 |
| Baseline characteristics for those with any baseline PRO recorded | N=340 | N=343 |
| Mean (sd) Age (years) | 38 (10) | 39 (10) |
| Male (%) | 299 (88%) | 305 (89%) |
| Mean (sd) baseline CD4 (mm3) | 328 (7) | 315 (7) |
| Mean (sd) baseline HIV RNA (log10 c/mL) | 10.9 (0.08) | 10.8 (0.08) |
| Mean (sd) BMI (kg/m2) | 23.8 (0.2) | 23.7 (0.2) |
| Mode of contamination* | ||
| Homosexual/bisexual sex | 230 (72%) | 235 (71%) |
| Heterosexual sex | 81 (25%) | 83 (25%) |
| Intravenous blood use | 7 (2%) | 10 (3%) |
| Blood or blood product receipt | 1 (<1%) | 0 (0%) |
| Other | 3 (1%) | 4 (1%) |
| Ethnic origin | ||
| White | 281 (83%) | 284 (83%) |
| Black | 43 (13%) | 36 (11%) |
| Asian | 6 (2%) | 8 (2%) |
| Other | 10 (3%) | 15 (4%) |
| HIV Stage | ||
| A | 279 (82%) | 284 (83%) |
| B | 44 (13%) | 43 (13%) |
| C | 17 (5%) | 18 (5%) |
Percentages are based only on patients with available data (RAL+DRV/r n=318, TDF-FTC+DRV/r n=329); seven patients had more than one risk factor (RAL+DRV/r n=4, TDF–FTC+DRV/r n=3). There was no evidence of differences in any baseline characteristic or PRO between the randomised arms in those that had any baseline PRO recorded.
PRO measures
There were no significant differences between randomized groups for any of the EQ-5D domains including VAS over time (Table 2 and Figure 1A). During follow-up an improvement of participant overall health status (EQ-VAS) was observed in both randomized groups, with a marked increase during the first 24 weeks of therapy (difference from baseline of 7.5 (95% CI 6.5,8.5); p<0.001), then a plateau, however there were no statistically significant differences between randomized groups at any time point (Figure 1a). A reduction of HIV symptoms scale score was observed in first 4 weeks (difference from baseline of -3 (95%CI -4,-2); p<0.001) for standard regimen), with stabilisation up to W96 and no statistically significant differences between the two randomized groups (Figure 1b). Depression/anxiety as measured on the CES-D scale also improved, as by week 4, statistically significant improvement was evidenced in both groups (difference of -3 (95% CI (-4,-2); p<0.001), with no difference between the 2 groups (Figure 1c). Sensitivity analyses showed that under the assumptions that participants with missing PROs either had systematically worse or better outcomes there were no significant differences between randomized groups for EQ-VAS, CES-D or HIV symptom scale score (Appendix Table 1). There was no evidence of a difference between groups in MDD during the 96 weeks duration of the study (OR 0.98, 95% CI 0.82,1.18). At W96, participants in the NtRTI-sparing regimen reported significantly lower median score in treatment satisfaction than participants in the standard regimen (53 (IQR 48-58) versus 55 (IQR 50-59); Kruskel-Wallis p=0.001). There were no differences between groups on satisfaction regarding general satisfaction, satisfaction with control and understanding of disease, side effects, or wish to continue current treatment (Table 3).
Table 2. Odds ratios of RAL+DRV/r vs TDF/FTC+DRV/r for having moderate or severe problems in the EQ5D domains over follow up.
| Odds Ratio of RAL + DRV/r vs TDF/FTC + DRV/r (95% CI) | ||||||
|---|---|---|---|---|---|---|
| EQ-5D Domain | W4 | W12 | W24 | W48 | W96 | Global p-value |
| Mobility (n=677) |
0.77 (0.32-1.90) |
0.52 (0.20-1.36) |
4.18 (1.12-15.66) |
2.19 (0.83-5.82) |
2.41 (0.97-5.96) |
0.05 |
| Self-care (n=677) |
1.26 (0.15-10.93) |
0.49 (0.13-1.92) |
0.71 (0.05-9.51) |
0.26 (0.03-2.63) |
0.24 (0.02-2.35) |
0.80 |
| Usual activity (n=676) |
0.99 (0.47-2.07) |
0.98 (0.45-2.11) |
0.98 (0.43-2.24) |
0.77 (0.35-1.66) |
0.75 (0.33-1.68) |
0.99 |
| Pain or discomfort (n=676) |
0.74 (0.48-1.16) |
1.13 (0.72-1.79) |
1.63 (1.01-2.64) |
0.96 (0.60-1.52) |
1.12 (0.69-1.82) |
0.26 |
| Anxiety or depression (n=676) |
1.09 (0.72-1.67) |
1.14 (0.74-1.74) |
0.87 (0.57-1.34) |
1.10 (0.71-1.69) |
1.33 (0.84-2.10) |
0.85 |
Table 3. Odds ratios of RAL+DRV/r vs TDF/FTC+DRV/r for proportion with a ‘very satisfied’ response on the HIVTSQ at W96 and impact of adjusting for potential confounders by logistic regression.
| Treatment satisfaction Question at W96 (% very satisfied (5 or 6)) |
RAL+DRV/r | TDF/FTC + DRV/r | Unadjusted OR (95% CI) for RAL vs TDF/FTC | Adjusted OR* | Other significant factors in model (OR (95%CI)) |
|---|---|---|---|---|---|
| Satisfied with current treatment | 238/268 (89%) | 269/288 (93%) | 1.78 (0.98, 3.25); p=0.06 | 1.55 (0.75, 3.19); p=0.24 | Age (1.03 (95%CI 1.0-1.08)) |
| Satisfaction with how well HIV was controlled | 250/268 (93%) | 277/287 (97%) | 1.99 (0.90, 4.40); p=0.09 | 1.99 (0.77, 5.18); p=0.16 | HIV symptom score change from baseline (0.92 (95% CI 0.89-0.96)), and EQ5D VAS change from baseline (1.03 (95%CI 1.00-1.06)), |
| Satisfied with extent of unwanted side effects | 234/267 (88%) | 250/287 (87%) | 0.95 (0.58, 1.57); p=0.85 | 0.88 (0.48, 1.60); p=0.67 | HIV symptom score change from baseline (0.96 (95%CI 0.94-0.99)) |
| Satisfaction with how demanding treatment is | 180/267 (67%) | 220/286 (77%) | 1.61 (1.11, 2.34); p=0.01 | 1.43 (0.91, 2.24); p=0.12 | HIV symptom score change from baseline (0.98 (95%CI 0.95-1.00)), age (1.03 (95%CI 1.00-1.05)) and gender (2.72 (95%CI 1.03-7.18)) |
| Convenience | 209/268 (78%) | 249/287 (87%) | 1.84 (1.18, 2.89); p=0.007 | 1.86 (0.08, 3.23); p=0.03 | HIV symptom score change from baseline (0.96 (95%CI 0.94-0.99) |
| Flexibility of treatment | 176/271 (65%) | 217/285 (76%) | 1.72 (1.19, 2.49); p=0.004 | 1.54 (0.99, 2.38); p=0.06 | CES-d score change from baseline (0.96 (95%CI 0.93-0.98)), age (1.02 (95%CI 1.00-1.05)), gender (3.44 (95%CI 1.30-9.10)) |
| Satisfaction with understanding of HIV | 232/266 (87%) | 252/287 (88%) | 1.05 (0.64, 1.74); p=0.84 | 1.08 (0.60, 1.94); p=0.78 | |
| Extent with which treatment fits into lifestyle | 203/264 (77%) | 250/287 (87%) | 2.03 (1.29, 3.17); p=0.002 | 2.12 (1.22, 3.66); p=0.007 | |
| Recommendation to a friend | 230/266 (86%) | 267/288 (93%) | 1.99 (1.13, 3.51); p=0.02 | 2.21 (1.09, 4.51); p=0.03 | |
| Continuation of treatment | 230/266 (86%) | 252/286 (88%) | 1.16 (0.70, 1.92); p=0.56 | 1.43 (0.77, 2.63); p=0.26 | EQ5D VAS score change from baseline (0.97 (95%CI 0.95-0.99)), CES-d score change from baseline (0.95 (95%CI 0.91-0.99)). |
adjusted for change from baseline in CES-d, Symptom scale and EQ5D VAS and baseline factors: age (years), and gender (transgender male to female = female, odds ratios estimated for female vs male).
PROs predictors
Age (Wald test p<0.001) and country of enrolment (overall Wald test p=0.05) were found to be independently associated with change in overall health status adjusting for the other baseline factors and baseline EQ5D VAS. Older age was associated with lower VAS score (decrease of -0.1 (95% CI -0.2,-0.05) per age year), and two countries were associated with increased VAS score (Hungary (n=6, increase of 11 (95% CI 1,21); p=0.03), and Portugal (n=21, increase of 12 (95%CI 3,21); p=0.007). The potential baseline predictors were also included in the models for change in CES-d and HIV symptoms scale adjusted for their baseline values. Age was found to be an independent predictor of change in the model for HIV symptoms scale with older age associated with an increased score (increase of 0.1 per age year (95%CI 0.03,0.2); p=0.006). Gender was found to be an independent predictor of change in CES-d score with female gender (including transgender male to female) associated with an increased CES-d score (increase of 2 (95% CI 0.1,4); p=0.04).
Multivariate analysis of treatment satisfaction
A logistic regression model was fitted for the proportion who responded with 5 or 6 (very satisfied) on each question on the HIVTSQ at W96 adjusted for treatment group, age at enrolment, gender and change from baseline in the other PRO measures (CES-d, EQ5D VAS and HIV symptom score). The proportion of participants feeling very satisfied with convenience, extent with which treatment fits into their lifestyle and who would recommend their treatment to a friend were higher in the standard regimen after adjustment (Table 3).
Discussion
Our data indicate that the majority of PRO domain scores measured with 4 different validated instruments significantly improved during 1St line antiretroviral treatment. Previous studies have shown reduction of fatigue and HIV symptoms in HIV-infected patients initiating antiretroviral therapy 15,16 but few studies have evaluated PROs in a randomized comparative study.
In our study, improvement of PROs scores started shortly after the initiation of therapy and then plateaued between 6 months and 2 years on continuous therapy, suggesting that PROs benefit was maximal when plasma virologic suppression was achieved and did not increase thereafter. For three of the PRO measures assessed, HRQoL, HIV symptoms scale and CES-D, improvement was not different between the two randomized groups either overall or any time point of follow-up. These results represent additive arguments to the hypothesis that PROs improvement is related to virologic suppression achievement rather than to a specific drug regimen. However, it is interesting to note that PROs improvement in the first weeks after treatment initiation were of similar magnitude in both randomized groups, although at W4 and W24 a significantly higher proportion of participants achieved virologic suppression on the NtRTI regimen, while at 96 weeks both regimens were virologically non-inferior 8. The underlying mechanisms to connect HIV plasma suppression with PROs improvement are yet to be elucidated 17. Some putative mechanisms may be related to the improvement of cytokine and other metabolites profile, both in peripheral blood and central nervous system, due to the viral suppression which could in turn positively impact patients’ experience 18. Viral suppression might thus improve fatigue and other PROs related to chronic HIV infection 19.
Our multivariate analysis showed an association between older age and lower health-related outcomes. Poorer PROs in older patients has been reported in many studies on HCV treatment, including the most-recent ones with highly effective and very well tolerated direct-acting antiviral regimens 20. Older age was negatively associated with physical Fatigue Impact Scale subscores in an observational study on raltegravir 19, while in a review of literature, there was no association between age and fatigue in most studies 21. HIV disease factors, such as CDC stage, CD4 and plasma HIV RNA did not influence PROs improvement, indicating that benefit of HIV therapy on quality of life was seen whatever the baseline immune-virological status of the patient, taking into account that 15 patients in our study had CD4 cell counts< 200/mm3 and only 5% CDC stage C HIV infection.
Association of worsening of depression score in women over time might be related to higher difficulty to cope with HIV disease or to higher vulnerability or perceived stigma. Most studies in an HIV-positive population have showed a higher rate of depression in women than men 22, however no longitudinal study over a 2-years period has been reported. The difference found in improved overall health status by country, as measured by EQ-VAS score, was driven by differences in Hungary and Portugal, and could be due to the small numbers enrolled in the trial in these countries as modest absolute differences from baseline in small groups can have a large impact. HIVTSQ scores for treatment convenience, fitting into lifestyle and willingness to recommend to a friend were significantly higher in participants taking the 3 pills once daily DRV/r + TDF/FTC regimen compared to 4 pills DRV/r + RAL regimen requiring twice daily intake, possibly reflecting a preference for a simplified regimens with less daily intake. A meta-analysis of randomized clinical trials has shown that lower pill burden was associated with both better adherence and virological suppression 23. However, once-daily regimens were associated with slightly better adherence, but not virological suppression, as compared with twice-daily regimens 23. Absence of differences in satisfaction with regards to side effects and HIV disease control and knowledge between randomized groups is in line with findings of the study showing non-inferiority of virological efficacy and no differences in safety over follow-up 8. In fact, even if participants were less satisfied with twice-daily regimens and less prone to recommend such a regimen, this did not translate in poorer outcome at W96. Indeed, the finding of a 2-point difference in treatment satisfaction score, although statistically significant, did not seem to have much clinical relevance since it did not appear to be associated with any adverse patient-reported or clinical outcomes. Furthermore, participants on twice-daily DRV/r + RAL regimen were equally satisfied to continue on their current regimen than those on once-daily DRV/r + TDF/FTC, probably because of perceived benefit in terms of virologic suppression and immunologic recovery.
The study limitations primarily arise from the nature of any clinical trial study which has strict enrollment criteria and close follow-up. In this context, the findings from an efficacy trial may potentially have limited generalizability to the entire HIV population. However, the design of our study was pragmatic with a wide range of enrolment criteria and similar follow-up to routine care. Additionally, some parameters which could potentially be associated with PROs were not collected during the study. These include level of education, marital status, income, and type of work. Finally, some of the PRO instruments were not systematically validated in all languages used in this study. Nevertheless, all these instruments have been systematically translated with some face-to-face and content validation. We also acknowledge that EQ5D might lack sensitivity, and may not capture subtle differences in participants’ quality of life.
In summary, this randomized-controlled trial of twice daily DRV/r + RAL versus once daily DRV/r + TDF/FTC demonstrated significant and persistent improvement of PRO scores during treatment. PROs improve rapidly after treatment initiation, with no difference between arms, reflecting probable improvement in immuno-virologic status and/or suggestive perception of disease control while on therapy. However treatment satisfaction was significantly lower with the twice-daily regimen for convenience and fitting into the participants’ lifestyles, without affecting W96 outcome. These findings provide a comprehensive approach when treating and selecting initial ART in HIV-infected participants.
Supplementary Material
Acknowledgements
We thank the NEAT001/ANRS143 study participants and their partners, families, and caregivers for participation in the study. We also thank the staff from all the centres participating in the trial.
Members of the NEAT 001/ANRS 143 Study Group
Trial Development Team (TDT)
Belgium: Nikos Dedes (Brussels); France: Geneviève Chêne, Laura Richert (Bordeaux), Clotilde Allavena, François Raffi (Nantes) and Brigitte Autran (Paris); Italy: Andrea Antinori, Raffaella Bucciardini and Stefano Vella (Rome); Poland: Andrzej Horban (Warsaw); Spain: Jose Arribas (Madrid); UK: Abdel G. Babiker, Marta Boffito, Deenan Pillay and Anton Pozniak (London).
Trial Steering Committee (TSC)
Belgium: Xavier Franquet and Siegfried Schwarze (Brussels); Denmark: Jesper Grarup (Copenhagen); France: Geneviève Chêne, Aurélie Fischer, Laura Richert, Cédrick Wallet (Bordeaux), François Raffi (Nantes), Alpha Diallo, Jean-Michel Molina, Juliette Saillard (Paris); Germany: Christiane Moecklinghoff (Janssen Pharmaceuticals; Neuss), Hans-Jürgen Stellbrink (Hamburg); Italy: Stefano Vella (Rome); Netherlands: Remko Van Leeuwen (Amsterdam); Spain: Jose Gatell (Barcelona); Sweden: Eric Sandstrom (Stockholm); Switzerland: Markus Flepp (Zurich); UK: Abdel G Babiker, Fiona Ewings, Elizabeth C. George, Fleur Hudson, and Anton Pozniak (London); USA: Gillian Pearce, Romina Quercia, Felipe Rogatto (Gilead Sciences; Foster City, CA), Randi Leavitt, and Bach-Yen Nguyen (Merck Laboratories; Whitehouse Station, NJ).
Trial Management Team (TMT)
France: Clotilde Allavena and François Raffi (Nantes); Italy: Stefano Vella (Rome); UK: Anton Pozniak (London).
CMG-EC, INSERM U897 Coordinating Unit, Bordeaux, France
Geneviève Chêne, Head of coordinating CTU, Member; Other Members : Fabien Arnault, Aurélie Fischer, Virginie Paniego, Laura Richert, Christine Schwimmer, Monique Termote, Guillaume Touzeau and Cédrick Wallet; Observers: Céline Boucherie, Delphine Jean, Felasoa Paraina, Elodie Rouch, Malika Soussi and Audrey Taieb.
MRC Clinical Trials Coordinating Unit, London, UK
Trial Statisticians: Abdel G. Babiker, Fiona Ewings, Elizabeth C. George; Other members: Wendy Dodds and Fleur Hudson; Observers: Adam Cursley, Anne Hoppe, Ischa Kummeling, Filippo Pacciarini, Nick Paton, Charlotte Russell, Kay Taylor and Denise Ward.
Centre for Health and Infectious Disease Research (CHIP), Copenhagen, Denmark
Members: Daniela Gey, Jesper Grarup, Per O. Jansson, Karoline Jensen, Mary Pearson, Birgit Riis Nielsen; Observers: Bitten Aagaard, Marius Eid, Birgitte Gram Jensen, Marie-Louise Jakobsen, Zillah Maria Joensen, Ellen Moseholm Larsen, Christiane Pahl, Birgit Riis Nielsen and Søren Stentoft Reilev.
Amsterdam Medical Center Coordinating Unit, Amsterdam, The Netherlands
Members: Desiree Lathouwers, Corry Manting and Remko Van Leeuwen; Observers: Ilse Christ.
INSERM-ANRS, Paris, France
Members: Alpha Diallo, Bienvenu Yves Mendy, Annie Metro, Juliette Saillard, Sandrine Couffin-Cadiergues.
ISS, Rome, Italy
Member: Lucia Palmisiano; Observer: Anne-Laure Knellwolf.
Local Clinical Trials Units (CTUs)
GESIDA, Madrid, Spain: Esther Aznar, Cristina Barea, Manuel Cotarelo, Herminia Esteban, Iciar Girbau, Beatriz Moyano, Miriam Ramirez, Carmen Saiz, Isabel Sanchez, Maria Yllescas; ISS, Rome, Italy: Andrea Binelli, Valentina Colasanti, Maurizio Massella, Lucia Palmisiano; University of Athens Medical School, Greece: Olga Anagnostou, Vicky Gioukari, Giota Touloumi.
Study Investigators
Austria: Brigitte Schmied (National Coordinating Investigator), Armin Rieger, Norbert Vetter; Belgium: Stephane De Wit (National Coordinating Investigator), Eric Florence, Linos Vandekerckhove; Denmark: Jan Gerstoft (National Coordinating Investigator), Lars Mathiesen; France: Christine Katlama (National Coordinating Investigator), André Cabié, Antoine Cheret, Michel Dupon, Jade Ghosn, Pierre-Marie Girard, Cécile Goujard, Yves Lévy, Jean-Michel Molina, Philippe Morlat, Didier Neau, Martine Obadia, Philippe Perré, Lionel Piroth, Jacques Reynes, Pierre Tattevin, François Raffi, Jean Marie Ragnaud, Laurence Weiss, Yazdan Yazdanpanah, Patrick Yéni, David Zucman; Germany: Georg Behrens (National Coordinating Investigator), Stefan Esser, Gerd Fätkenheuer, Christian Hoffmann, Heiko Jessen, Jürgen Rockstroh, Reinhold Schmidt, Christoph Stephan, Stefan Unger; Greece: Angelos Hatzakis (National Coordinating Investigator), George L. Daikos, Antonios Papadopoulos, Athamasios Skoutelis; Hungary: Denes Banhegyi (National Coordinating Investigator); Ireland: Paddy Mallon (National Coordinating Investigator), Fiona Mulcahy; Italy: Andrea Antinori (National Coordinating Investigator), Massimo Andreoni, Stefano Bonora, Francesco Castelli, Antonella D’Arminio Monforte, Giovanni Di Perri, Massimo Galli, Adriano Lazzarin, Francesco Mazzotta, Torti Carlo, Vincenzo Vullo; The Netherlands: Jan Prins (National Coordinating Investigator), Clemens Richter, Dominique Verhagen, Arne Van Eeden; Poland: Andrzej Horban (National Coordinating Investigator); Portugal: Manuela Doroana (National Coordinating Investigator), Francisco Antunes, Fernando Maltez, Rui Sarmento-Castro; Spain: Juan Gonzalez Garcia (National Coordinating Investigator), Jose Lopez Aldeguer, Bonaventura Clotet, Pere Domingo, Jose M. Gatell, Hernando Knobel, Manuel Marquez, Martin Pilar Miralles, Joaquin Portilla, Vicente Soriano, Maria-Jesus Tellez; Sweden: Anders Thalme (National Coordinating Investigator), Anders Blaxhult, Magnus Gisslen; UK: Alan Winston (National Coordinating Investigator), Julie Fox, Mark Gompels, Elbushra Herieka, Margaret Johnson, Clifford Leen, Anton Pozniak, Alastair Teague, Ian Williams.
Quality-of-life working group
Raffaella Bucciardini (coordinator), Nikos Dedes, Vincenzo Fragola, Elizabeth C. George (statistician), Marco Lauriola, Rita Murri, Pythia Nieuwkerk, Bruno Spire, Alain Volny-Anne, Brian West.
Footnotes
Conflicts of Interest and Source of Funding
NEAT is a project funded to the Instituto Superiore di Sanità – Rome, by the European Union under the Sixth Framework Programme, project number LSHP-CT-2006-037570. The trial was also supported by Gilead Sciences, Janssen Pharmaceuticals, and Merck Laboratories. The French National Institute for Health and Medical Research–France Recherche Nord & Sud Sida-HIV Hepatites (Inserm-ANRS) was the sponsor and a funder of the trial. Elizabeth C George was also supported by the UK Medical Research Council (grant number MC_U122886352).
François Raffi has received research funding or honoraria from, or consulted for, Abbvie, Bristol-Myers Squibb, Gilead Sciences, Janssen, MSD, and ViiV Healthcare. Bruno Spire has received honorarium fees from Gilead, MSD and Jansen-Cilag. Anton Pozniak has received research funding and honoraria from Merck, Janssen, Gilead and Viiv. Jean-Michel Molina has sat on advisory boards for Gilead, Merck, Janssen, Viiv BMS and Teva and received research funding from Gilead. Nikos Dedes has received financial support and been a board member of Gilead, Merck and Janssen. For the remaining authors no conflicts of interest were declared.
Competing interests
FR has received research funding or honoraria from, or consulted for, Abbvie, Bristol-Myers Squibb, Gilead Sciences, Janssen, MSD, and ViiV Healthcare. BS has received honorarium fees from Gilead, MSD and Jansen-Cilag. AP has received research funding and honoraria from Merck, Janssen, Gilead and Viiv. J-MM has sat on advisory boards for Gilead, Merck, Janssen, Viiv BMS and Teva and received research funding from Gilead. ND has received financial support and been a board member of Gilead, Merck and Janssen. ECG, RB, PN, MT, SV, AV-A, VF, BW, JF, BW, AH and LR declare no competing interests.
References
- 1.Palella FJ, Jr, Deloria-Knoll M, Chmiel JS, et al. Survival benefit of initiating antiretroviral therapy in HIV-infected persons in different CD4+ cell strata. Ann Intern Med. 2003;138(8):620–626. doi: 10.7326/0003-4819-138-8-200304150-00007. [DOI] [PubMed] [Google Scholar]
- 2.Group ISS, Lundgren JD, Babiker AG, et al. Initiation of Antiretroviral Therapy in Early Asymptomatic HIV Infection. N Engl J Med. 2015;373(9):795–807. doi: 10.1056/NEJMoa1506816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Services DoHaH. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents Living with HIV. 2017 [Google Scholar]
- 4.Marcellin F, Preau M, Ravaux I, Dellamonica P, Spire B, Carrieri MP. Self-reported fatigue and depressive symptoms as main indicators of the quality of life (QOL) of patients living with HIV and Hepatitis C: implications for clinical management and future research. HIV Clin Trials. 2007;8(5):320–327. doi: 10.1310/hct0805-320. [DOI] [PubMed] [Google Scholar]
- 5.Campo RE, Cohen C, Grimm K, Shangguan T, Maa J, Seekins D. Switch from protease inhibitor- to efavirenz-based antiretroviral therapy improves quality of life, treatment satisfaction and adherence with low rates of virological failure in virologically suppressed patients. Int J STD AIDS. 2010;21(3):166–171. doi: 10.1258/ijsa.2009.008487. [DOI] [PubMed] [Google Scholar]
- 6.Marcellin F, Carrieri MP, Spire B. Choice of therapeutic strategies in the context of HIV infection: key role of patient-reported outcomes. Expert Rev Anti Infect Ther. 2012;10(4):403–406. doi: 10.1586/eri.12.27. [DOI] [PubMed] [Google Scholar]
- 7.Kozak MS, Mugavero MJ, Ye J, et al. Patient reported outcomes in routine care: advancing data capture for HIV cohort research. Clin Infect Dis. 2012;54(1):141–147. doi: 10.1093/cid/cir727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raffi F, Babiker AG, Richert L, et al. Ritonavir-boosted darunavir combined with raltegravir or tenofovir-emtricitabine in antiretroviral-naive adults infected with HIV-1: 96 week results from the NEAT001/ANRS143 randomised non-inferiority trial. Lancet. 2014;384(9958):1942–1951. doi: 10.1016/S0140-6736(14)61170-3. [DOI] [PubMed] [Google Scholar]
- 9.Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 10.Bucciardini R, Pugliese K, Francisci D, et al. Validation of a self-reported HIV symptoms list: the ISS-HIV symptoms scale. AIDS Res Ther. 2016;13:18. doi: 10.1186/s12981-016-0102-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 12.Woodcock A, Bradley C. Validation of the revised 10-item HIV Treatment Satisfaction Questionnaire status version and new change version. Value Health. 2006;9(5):320–333. doi: 10.1111/j.1524-4733.2006.00121.x. [DOI] [PubMed] [Google Scholar]
- 13.Fairclough DL, Thijs H, Huang IC, Finnern HW, Wu AW. Handling missing quality of life data in HIV clinical trials: what is practical? Qual Life Res. 2008;17(1):61–73. doi: 10.1007/s11136-007-9284-3. [DOI] [PubMed] [Google Scholar]
- 14.White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ. 2011;342:d40. doi: 10.1136/bmj.d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edelman EJ, Gordon K, Rodriguez-Barradas MC, Justice AC, Vacs Project T. Patient-reported symptoms on the antiretroviral regimen efavirenz/emtricitabine/tenofovir. AIDS Patient Care STDS. 2012;26(6):312–319. doi: 10.1089/apc.2012.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nglazi MD, West SJ, Dave JA, Levitt NS, Lambert EV. Quality of life in individuals living with HIV/AIDS attending a public sector antiretroviral service in Cape Town, South Africa. BMC Public Health. 2014;14:676. doi: 10.1186/1471-2458-14-676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Winston A, Stohr W, Antinori A, et al. Changes in Cognitive Function Over 96 Weeks in Naive Patients Randomized to Darunavir-Ritonavir Plus Either Raltegravir or Tenofovir-Emtricitabine: A Substudy of the NEAT001/ANRS143 Trial. J Acquir Immune Defic Syndr. 2017;74(2):185–192. doi: 10.1097/QAI.0000000000001189. [DOI] [PubMed] [Google Scholar]
- 18.Hong S, Banks WA. Role of the immune system in HIV-associated neuroinflammation and neurocognitive implications. Brain Behav Immun. 2015;45:1–12. doi: 10.1016/j.bbi.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spire B, Nait-Ighil L, Pugliese P, et al. Quality of life improvement in HIV-1 patients treated with raltegravir in a real-life observational study: RACING. HIV Clin Trials. 2017;18(1):1–16. doi: 10.1080/15284336.2016.1251030. [DOI] [PubMed] [Google Scholar]
- 20.Younossi ZM, Stepanova M, Charlton M, et al. Patient-reported outcomes with sofosbuvir and velpatasvir with or without ribavirin for hepatitis C virus-related decompensated cirrhosis: an exploratory analysis from the randomised, open-label ASTRAL-4 phase 3 trial. Lancet Gastroenterol Hepatol. 2016;1(2):122–132. doi: 10.1016/S2468-1253(16)30009-7. [DOI] [PubMed] [Google Scholar]
- 21.Jong E, Oudhoff LA, Epskamp C, et al. Predictors and treatment strategies of HIV-related fatigue in the combined antiretroviral therapy era. AIDS. 2010;24(10):1387–1405. doi: 10.1097/QAD.0b013e328339d004. [DOI] [PubMed] [Google Scholar]
- 22.Nanni MG, Caruso R, Mitchell AJ, Meggiolaro E, Grassi L. Depression in HIV infected patients: a review. Curr Psychiatry Rep. 2015;17(1):530. doi: 10.1007/s11920-014-0530-4. [DOI] [PubMed] [Google Scholar]
- 23.Nachega JB, Parienti JJ, Uthman OA, et al. Lower pill burden and once-daily antiretroviral treatment regimens for HIV infection: A meta-analysis of randomized controlled trials. Clin Infect Dis. 2014;58(9):1297–1307. doi: 10.1093/cid/ciu046. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.