Abstract
Objective
The objective of this study was to evaluate the effect of prior term birth on recurrent spontaneous preterm birth (sPTB) risk.
Study Design
Retrospective cohort study of 211 women with prior sPTB, comparing women with and without prior term births. The primary outcome was recurrent sPTB <37 weeks. Analyses stratified by gestational age of prior sPTB and adjusted for confounders using multivariable logistic regression.
Results
The overall sPTB rate was 33.7%, with no statistical difference between women with and without prior term births (28.9 vs. 37.7%, p = 0.2). Among women with prior second-trimester loss (16–236/7 weeks), those with a term birth had a decreased sPTB rate (15.4 vs. 43.2%, p = 0.02), which persisted after adjusting for age and 17-α hydroxyprogesterone caproate use. For women with prior sPTB ≥24 weeks, there was no difference in sPTB with and without prior term births (29.5 vs. 26.6%, p = 0.7). A term birth as the most recent delivery lowered, but did not eliminate, the sPTB risk (19.1 vs. 36.4%, p = 0.1).
Conclusion
Prior term birth lowers the risk of recurrent sPTB for women with prior second-trimester loss, but not for women with prior sPTB ≥24 weeks. Women with prior preterm and term births should be counseled accordingly and all sPTB prevention strategies should be recommended.
Keywords: birth order, prematurity, recurrent preterm birth, spontaneous preterm birth
Although the preterm birth (PTB) rate has declined since reaching an all-time high in 2006, prematurity continues to be the leading cause of neonatal morbidity and mortality. In 2016, PTB complicated 9.84% of pregnancies in the United States, with spontaneous PTB (sPTB) accounting for two-thirds of all PTBs.1–3
A prior sPTB is one of the most significant risk factors for sPTB with rates of recurrence ranging from 20 to 60%.4–7 In contrast, women with a prior full-term birth and no history of sPTB have only a 5 to 7% sPTB rate, which is below the national average.4,5,8 The impact that a prior full-term birth has on recurrent sPTB among women with a prior sPTB is understudied.4,5 Existing literature suggests that a prior full-term birth reduces the risk of recurrent PTB. However, these data are more than 20 years old and limited by the use of birth certificate data and the inclusion of women with both spontaneous and medically indicated PTB.
The ability to quantify the risk of recurrent sPTB for women with a prior full-term birth is important for risk assessment and patient counseling regarding preventative strategies. This is highlighted in recent literature suggesting that women with a prior full-term birth are 50% less likely to utilize 17-α hydroxyprogesterone caproate (17P), a proven interventions to reduce the risk of recurrent sPTB.9
The objective of this study, therefore, was to evaluate the effect of a prior full-term birth on the recurrence rate of sPTB in women with prior sPTB. Our hypothesis was that a prior full-term birth reduces, but does not eliminate, the risk of recurrent sPTB.
Materials and Methods
This retrospective cohort study was a secondary analysis of women evaluated in the Prematurity Prevention Program at the Hospital of the University of Pennsylvania from 2010 to 2014. The study was performed with approval by the Institutional Review Board.
The Prematurity Prevention Program was established to identify and counsel women who are at risk for sPTB. All women seen for consultation in this program were included in the original Prematurity Prevention Program cohort (n = 316). These women have their prior delivery records reviewed, when available, and a detailed history taken to understand the clinical situation surrounding the prior PTB and to confirm that it was a spontaneous and not medically indicated PTB. Each case is reviewed by maternal–fetal medicine specialists to determine whether the woman’s obstetric history qualifies her for evidence-based interventions to prevent recurrent sPTB.10,11 Standard counseling at our institution includes the recommendation for weekly 17P if the woman had a prior sPTB less than 37 weeks, as well as serial cervical length screening with cerclage recommendation for a short cervix (≤15 mm) if the prior sPTB was less than 34 weeks.10,11
Women were included in this study if they had ≥1 prior sPTB(s) of a singleton gestation between 16 and 366/7 weeks and delivered a subsequent singleton gestation at our institution during the study period. We compared the risk of recurrent sPTB < 37 weeks between those with and without prior full-term births. The primary outcome for this study was recurrent sPTB before 37 weeks’ gestation. The estimated gestational age at delivery was established by the best obstetrical estimate using last menstrual period (if known) and earliest ultrasound documenting estimated date of delivery.12 sPTB was identified based on chart review and was defined as preterm premature rupture of membranes or spontaneous labor and delivery between 16 and 366/7 weeks. Women were excluded if delivery information was not available for the subsequent pregnancy.
Our cohort of women with a prior sPTB included: (1) women with a prior spontaneous second-trimester loss defined as preterm premature rupture of membranes, preterm labor, or cervical insufficiency between 16 and 236/7 weeks in the absence of fetal demise and (2) women with a prior sPTB ≥24 weeks defined as preterm premature rupture of membranes or preterm labor and delivery between 24 and 366/7 weeks.
Women with fetal anomalies were excluded. Women were included in the study only once; if a woman had multiple pregnancies during the study time period, the earlier pregnancy was included in our analysis.
Data were collected by chart abstraction and included demographic data (race, age, body mass index, and insurance), obstetric history (parity, gestational age of all prior deliveries, details regarding prior preterm deliveries, and mode of delivery), current pregnancy data (17P use, number of prenatal visits, and medical comorbidities), and delivery data (gestational age at delivery and mode of delivery) for each woman. The use of 17P was identified based on prescription of the medication and/or documentation of administration in the prenatal chart. A woman was considered to have used 17P if she ever used the medication during the pregnancy; compliance throughout the duration of pregnancy was not assessed.
The sample size was fixed (n = 211) based on the primary study. Assuming a baseline recurrence risk of sPTB of 40%, we would have more than 80% power to detect a twofold difference in recurrent sPTB between the study groups.
All data were analyzed using Stata version 12.0 (College Station, TX). Statistical significance of p < 0.05 was used. Categorical data were compared using chi-squared tests. Parametric data were compared with Student’s t-test, with means and standard deviations reported. Nonparametric data were compared with Mann–Whitney U-tests with medians and interquartile ranges reported. Multivariable logistic regression was used to calculate odds ratios and adjust for significant confounders. Confounders were based on those identified as significant in univariate analysis with a p-value ≤0.1. Multivariable backward stepwise elimination was used to create a comprehensive model. Significant confounders identified were maternal age and 17P use.
Because of the reported differences in the recurrence risk of sPTB among women with a prior second-trimester loss versus women with a prior sPTB ≥24 weeks,4 and because of reported differences in risk based on the order of the preceding preterm and full-term births,5 tests for effect modification based on these variables were performed and found to be significant. Analyses were therefore stratified based on the gestational age of the prior sPTB (16–236/7 vs. ≥24 weeks) and based on the timing of the prior full-term birth. Exploratory analyses were performed to evaluate the impact of the number of prior preterm deliveries and recurrent sPTB.
Results
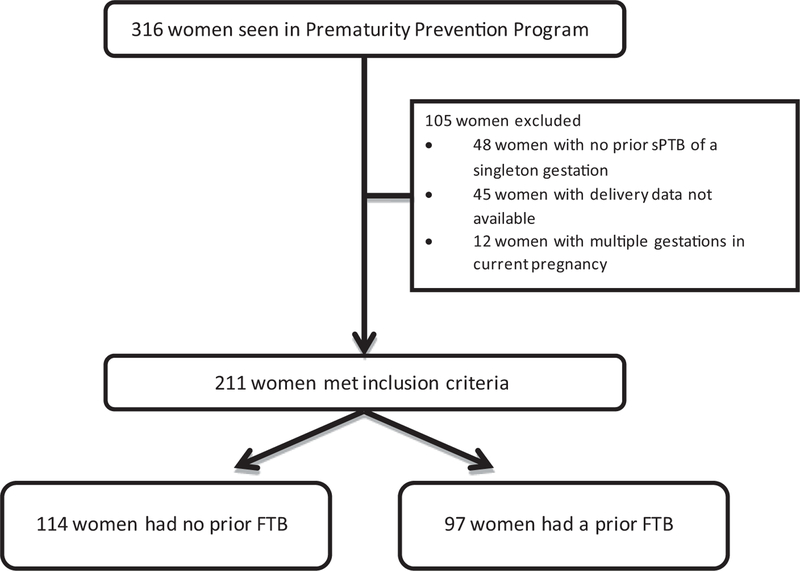
Of the 316 women who were included in the primary cohort, 211 women met inclusion criteria for this study (►Fig. 1). Of these 211 women, 97 (46%) had a prior full-term birth and 114 (54%) did not have a prior full-term birth.
Fig. 1.
Study cohort. This figure depicts the inclusion and exclusion criteria and process for selection of the study cohort. FTB, full-term birth; sPTB, spontaneous preterm birth.
►Table 1 shows the demographic information for this cohort. Women with a prior full-term birth were older and more parous than those without a prior full-term birth. More than two-thirds of women in the cohort had a history of a prior sPTB ≥24 weeks. Although all women in this cohort were eligible for and offered 17P, the rate of use was lower among women with a prior full-term birth compared to those without a full-term birth (p = 0.02). Among those eligible for cerclage, cerclage uptake was high regardless of full-term birth history.
Table 1.
Demographics
| No prior FTB (n = 114) | Prior FTB (n = 97) | p-Value | |
|---|---|---|---|
| Maternal age (y) | 26.4 (21.9–31.1) | 30.2 (26.4–34.5) | <0.01 |
| Race | |||
| Black | 93 (81.6) | 85 (87.6) | 0.4 |
| Caucasian | 13 (11.4) | 9 (9.3) | |
| Other | 8 (7.0) | 3 (3.1) | |
| Tobacco use | 10 (8.8) | 14 (14.4) | 0.3 |
| Parity | 1 (0–1) | 2 (2–3) | <0.01 |
| Number prior FTB | – | 1 (1–2) | – |
| Prior sPTB ≥24 wka | 77 (67.5) | 71 (73.2) | 0.4 |
| Prior second-trimester loss 16–236/7 wka | 50 (43.9) | 36 (37.1) | 0.3 |
| 17P use | 90 (79.0) | 60 (61.9) | 0.02 |
| Eligible for cerclage based on short CL | 38 (33.3) | 15 (15.5) | 0.01 |
| Cerclage placed (among eligible women) | 37 (97.4) | 14 (93.3) | 0.8 |
Abbreviations: CL, cervical length; FTB, full-term birth; sPTB, spontaneous preterm birth; 17P, 17-α hydroxyprogesterone caproate.
Note: p-Values by chi-square test (categorical data) and Mann–Whitney U-tests (continuous data). Categorical data are presented as n (%) and continuous data as median (IQR).
Prior sPTB ≥24 weeks and prior second-trimester loss 16–236/7 weeks not mutually exclusive.
The rate of overall PTB in the cohort was 39.8% and the rate of recurrent sPTB in the cohort was 33.7%. For the entire cohort, women with a prior full-term birth had a nonsignificant reduction in the rate of overall PTB compared with those without a prior full-term birth (34.0 vs. 44.7%, p = 0.1). There was also a nonsignificant reduction in the rate of recurrent sPTB in a subsequent pregnancy as compared with those without a prior full-term birth, even after adjusting for maternal age and 17P use (28.9 vs. 37.7%, p = 0.2, adjusted odds ratio [aOR] 0.85 [0.38–1.89]). As planned a priori, we then analyzed our results stratified by gestational age of the prior sPTB (second-trimester loss 16–236/7 weeks vs. sPTB ≥24 weeks).
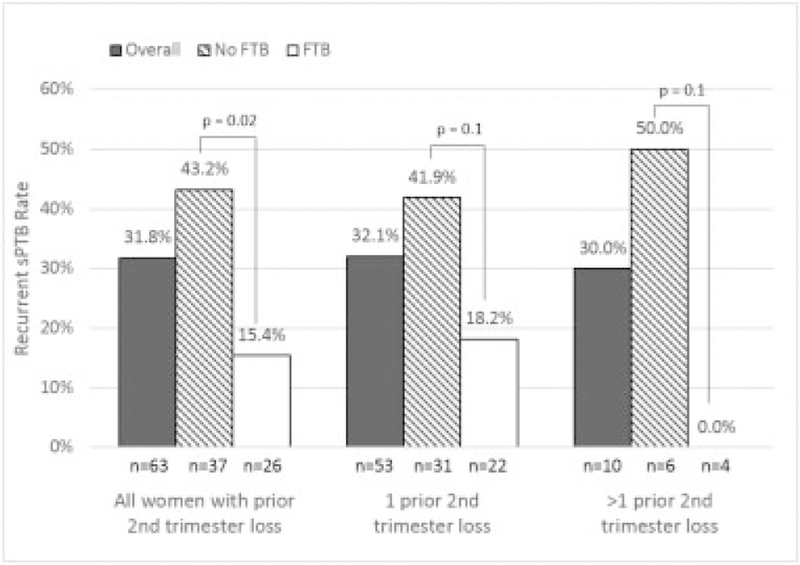
►Fig. 2 shows the recurrent sPTB rates among women with a prior second-trimester loss at 16 to 236/7 weeks (n = 63). Among all women with a history of a second-trimester loss, there was a 76% reduction in the rate of recurrent sPTB for women with a prior full-term birth compared with women without a prior full-term birth (15.4 vs. 43.2%, OR: 0.24 [0.068–0.83], p = 0.02). This reduction remained after adjusting for maternal age and 17P (aOR: 0.12 [0.017–0.875], p = 0.04). There were 10 women in the cohort who had more than one prior second-trimester loss. In exploratory analyses, we compared outcomes for women with one versus more than one prior second-trimester loss and found a nonsignificant reduction in recurrent sPTB (►Fig. 2).
Fig. 2.
Recurrent sPTB among women with prior second-trimester loss. This figure compares the recurrent sPTB rates among women with prior second-trimester loss with versus without a prior FTB, stratified by number of prior second-trimester losses. FTB, full-term birth; sPTB, spontaneous preterm birth.
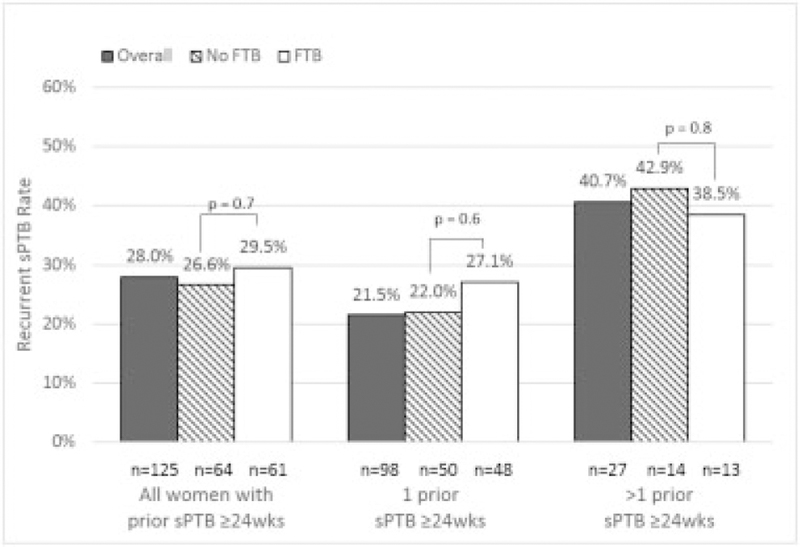
►Fig. 3 displays the recurrent sPTB rates among women with a prior sPTB ≥24 weeks (n = 125). Unlike women with a prior second-trimester loss, a prior full-term birth did not appear to be protective for the women in this group, regardless of the number of prior sPTBs. The number of prior sPTBs ≥24 weeks per woman in this subgroup ranged from 1 to 4, with 27 women having had more than one prior sPTB ≥24 weeks. While not statistically significant, women with more than one prior sPTB ≥24 weeks had a higher rate of recurrent sPTB compared with those with only one prior sPTB ≥24 weeks (40.7 vs. 21.5%, p = 0.09).
Fig. 3.
Recurrent sPTB among women with prior sPTB ≥ 24 weeks. This figure compares the recurrent sPTB rates among women with prior sPTB ≥ 24 weeks with versus without a prior FTB, stratified by number of prior sPTB ≥ 24 weeks. FTB, full-term birth; sPTB, spontaneous preterm birth.
The remaining 23 women in the cohort had both a second-trimester loss and a prior sPTB ≥24 weeks. In this group, we did not observe a statistically significant difference in the rate of recurrent sPTB between those with and without prior full-term births (60.0 vs. 76.9%, p = 0.4).
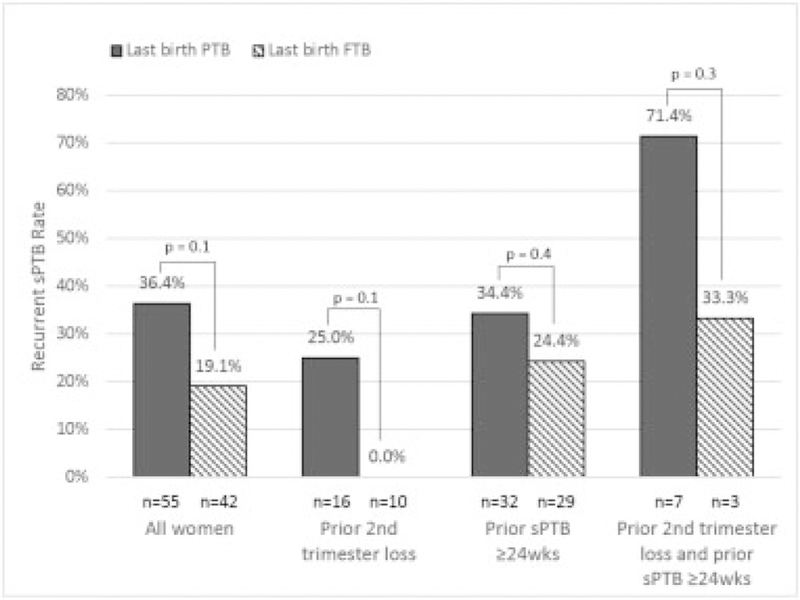
Analyses determined that birth order, specifically the timing of the prior full-term birth, impacted the outcome of recurrent sPTB. For the subset of women with a prior full-term birth (n = 97), we compared women whose most recent delivery was a full-term birth (n = 42, 43.3%) to those whose full-term birth preceded their sPTB (n = 55, 56.7%). As seen in ►Fig. 4, a full-term birth as the most recent delivery lowers, but does not eliminate, the risk of recurrent sPTB.
Fig. 4.
Recurrent sPTB by birth order in women with prior FTB. This figure displays the recurrent sPTB rates in those women who had a prior FTB, based on whether the most recent birth was a preterm birth or a FTB. The results are stratified by obstetric history. FTB, full-term birth; PTB, preterm birth; sPTB, spontaneous preterm birth.
Discussion
This study evaluates the risk of recurrent sPTB among women with prior sPTB, and assesses whether or not this risk is mitigated by a history of a prior full-term birth. Although we did not find a statistically significant difference in our primary outcome of recurrent sPTB before 37 weeks’ gestation, there was an 8.8% absolute reduction and nearly 25% relative reduction in recurrent sPTB for women with a prior full-term birth compared with those without. The study was underpowered for a difference of this magnitude, but the relative reduction in recurrent sPTB is of clinical significance and warrants further study.
Our data further suggest that a prior full-term birth has differential effects on the recurrence risk of sPTB depending on the gestational age of the prior PTB. Specifically, women with a history of a second-trimester loss and a full-term birth were 88% less likely to have a recurrent sPTB as compared with those without a prior full-term birth. That being said, the rate of sPTB in women with a history of second-trimester loss and full-term birth (15.4% in our study) is still 56% higher than the national average of 9.84%.3 This difference in risk between women with and without prior full-term births was not noted among women with a prior sPTB ≥24 weeks. Our results also suggest that birth order is an important risk modifier. Although the small sample size limits our power for definitive conclusions, we found that, for those women with a prior term birth, a full-term birth as the most recent pregnancy almost halves one’s risk of recurrent sPTB compared with having a sPTB as the most recent pregnancy.
Our study further expands upon the literature and our current knowledge of recurrent PTB risk. Edlow et al reported that a prior second-trimester loss is associated with a recurrent sPTB rate that approaches that of women with a prior sPTB ≥24 weeks.4 This is consistent with our results and lends additional support to the concept that these two groups of women should have similar clinical management strategies available to them.13 Although 37% of women with a prior second-trimester loss in the Edlowet al cohort also had a prior full-term birth, the study did not evaluate the impact of the prior full-term birth on the recurrence risk of sPTB for these women.
McManemy et al examined the recurrence risk of PTB in a third pregnancy.5 The authors concluded that a prior full-term birth reduces the risk of PTB, with the greatest reduction in those with a term delivery in the most recent pregnancy. This study, conducted from 1989 to 1997, is limited by relying on birth certificate data and including women with both spontaneous and medically indicated preterm deliveries. Our contemporary study excludes medically indicated PTB (for which the underlying pathophysiologies as well as the risk-reduction strategies are quite different) and therefore provides further insight into recurrence patterns for sPTB. As such, our results are more applicable to patient counseling. Another strength of our study was the rigorous process used to evaluate the preceding pregnancies to accurately identify women with a prior sPTB. As patients were captured through the highly specialized Prematurity Prevention Program, complete information was available related to obstetric history, birth order, and utilization of interventions to prevent recurrent sPTB. In addition, our study is unique with regard to the inclusion of women with second-trimester pregnancy loss, a group whose recurrence risk is understudied.
Our study was limited by a fixed sample size and we are therefore underpowered for some of our outcomes that appear clinically different but were not statistically significant. This highlights the importance of performing larger studies to further answer these questions. Another limitation is that our cohort was composed of a selected group of patients seen in our Prematurity Prevention Program, who were motivated to seek counseling and preventive strategies against sPTB. In addition, more than 80% of our cohort was African American, a group known to be at particularly high risk for PTB. These two factors may make our results less generalizable to other populations.
In summary, our data highlight the important concept that a prior full-term birth decreases, but does not eliminate, the risk of recurrent sPTB. Women with a prior sPTB who also have a prior full-term birth remain at high risk for recurrent sPTB. We are fortunate today to have several interventions to reduce the risk of recurrent sPTB. Nevertheless, patient acceptance of such interventions may be tied to self-perceived risk of recurrent sPTB and physician counseling regarding the likelihood of recurrence.9 It is therefore of the utmost importance to ensure that, regardless of prior full-term birth, counseling of patients with prior sPTB includes their high recurrence rates. If we are to be successful in our continued efforts to decrease the PTB rate, all therapeutic interventions available to these women should be recommended and encouraged.
Acknowledgments
Funding
This study was funded in part by a National Institute of Health career development award in Women’s Reproductive Health Research: K12-HD001265-14.
Footnotes
Conflict of Interest
None.
References
- 1.MacDorman MF, Declercq E, Zhang J. Obstetrical intervention and the singleton preterm birth rate in the United States from 1991–2006. Am J Public Health 2010;100(11):2241–2247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldenberg RL, Iams JD, Mercer BM, et al. ; NICHD MFMU Network. The preterm prediction study: the value of new vs standard risk factors in predicting early and all spontaneous preterm births. Am J Public Health 1998;88(02):233–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamilton BE, Martin JA, Osterman MJK, Driscoll AK, Roseen LM. Births: Provisional Data for 2016. Vital Statistics Rapid Release; No 2 Hyattsville, MD: National Center for Health Statistics; 2017 [Google Scholar]
- 4.Edlow AG, Srinivas SK, Elovitz MA. Second-trimester loss and subsequent pregnancy outcomes: what is the real risk? Am J Obstet Gynecol 2007;197(06):581.e1–581.e6 [DOI] [PubMed] [Google Scholar]
- 5.McManemy J, Cooke E, Amon E, Leet T. Recurrence risk for preterm delivery. Am J Obstet Gynecol 2007;196(06):576.e1–576.e6 [DOI] [PubMed] [Google Scholar]
- 6.Iams JD, Goldenberg RL, Mercer BM, et al. ; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. The Preterm Prediction Study: recurrence risk of spontaneous preterm birth. Am J Obstet Gynecol 1998;178(05): 1035–1040 [DOI] [PubMed] [Google Scholar]
- 7.Goldenberg RL, Mayberry SK, Copper RL, Dubard MB, Hauth JC. Pregnancy outcome following a second-trimester loss. Obstet Gynecol 1993;81(03):444–446 [PubMed] [Google Scholar]
- 8.Levine LD, Bogner HR, Hirshberg A, Elovitz MA, Sammel MD, Srinivas SK. Term induction of labor and subsequent preterm birth. Am J Obstet Gynecol 2014;210(04):354.e1–354.e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turitz AL, Bastek JA, Purisch SE, Elovitz MA, Levine LD. Patient characteristics associated with 17-alpha hydroxyprogesterone caproate use among a high-risk cohort. Am J Obstet Gynecol 2016;214(04):536.e1–536.e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meis PJ, Klebanoff M, Thom E, et al. ; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med 2003; 348(24):2379–2385 [DOI] [PubMed] [Google Scholar]
- 11.Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol 2009;201(04):375.e1–375.e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Method for Estimating Due Date. Committee opinion no 611: method for estimating due date. Obstet Gynecol 2014;124(04):863–866 [DOI] [PubMed] [Google Scholar]
- 13.Iams JD. Clinical practice. Prevention of preterm parturition. N Engl J Med 2014;370(03):254–261 [DOI] [PubMed] [Google Scholar]