Abstract
Comorbid mental health disorders are highly common in trauma-exposed individuals with posttraumatic stress disorder (PTSD), depression, and generalized anxiety disorder (GAD) among the most common co-occurring conditions. Network models of psychopathology offer a novel method to understand how this comorbidity manifests. The present study examined the presence of symptom communities (groups of highly connected symptoms) within a network of these disorders and hub symptoms (symptoms that connect such communities). Cross-sectional data were obtained from a community sample (N = 1184) of trauma exposed adults. Network analyses identified 5 communities: 1 containing all depression and GAD symptoms and 4 for PTSD. The PTSD communities corresponded to symptoms of intrusion and avoidance, hyperarousal, dysphoria, and negative affect. These communities had varying levels of connectivity to the Depression & GAD community. Symptoms of GAD (inability to relax) and PTSD (restricted or diminished positive emotion) were identified as key hub symptoms for the network. The results suggest symptoms of depression and GAD are highly interrelated and that PTSD is heterogeneous. The comorbidity among these diagnoses is thought to stem from their overlap with negative affect.
Keywords: PTSD, GAD, Depression, Network Analysis
Exposure to traumatic events increases the risk for multiple psychiatric disorders including posttraumatic stress disorder (PTSD), depression, and generalized anxiety disorder (GAD) (Bryant et al., 2010; Kessler et al., 2005). Estimates of comorbidity rates with PTSD are as high as 91% (Bryant et al., 2010). This rate suggests there are systematic underlying processes that lead to comorbidity. A prominent model to explain comorbidity is the quadripartite model of psychopathology, which proposes that disorders are defined across two dimensions, general distress and specificity (Watson, 2009). The general distress factor represents negative affect and the specificity factor reflects differentiation from negative affect. Depression, GAD, and PTSD are all thought to have high levels of general distress which leads to elevated comorbidity. PTSD is comprised of four clusters, each of which has specificity from GAD and depression, however. Intrusion (Cluster-B) and avoidance (Cluster-C) consistently have weaker relations to symptoms of depression and GAD than Negative Alterations in Cognitions and Mood (NACM, Cluster-D) and Alterations to Arousal and Reactivity (Cluster-E) (Price et al., 2017; Price and van Stolk-Cooke, 2015; Watson, 2009).
The quadripartite model and empirical investigations of comorbidity have been examined primarily through factor analysis (Contractor et al., 2015; Grant et al., 2008; Price and van Stolk-Cooke, 2015). A limitation of factor analysis is the assumption of symptom independence – symptoms are only related via their corresponding factors. This assumption may miss important nuances in how symptoms of each diagnosis affect one another. For example, nightmares, a symptom of PTSD-Cluster B, are likely to lead to sleep difficulties, a symptom of PTSD-Cluster E, yet this path is not included in factor models. Rather, this relation is subsumed in the relation between the PTSD-B factor and the PTSD-E factor. Implied in this factor relation is that all other symptoms of cluster B and cluster E are related, which obscures the unique relation between nightmares and sleep. This set of relations may incorrectly associate other symptoms of cluster B to sleep difficulties. Models that allow for direct symptom would capture these associations, which may further elucidate specific pathways by which comorbidity occurs. According to the quadripartite model, it is expected that these relations would be among symptoms that are more strongly associated with negative affect.
An alternative conceptualization of psychopathology is to view disorders as an integrated network (Borsboom and Cramer, 2013). Networks are defined as a set of nodes (symptoms) and edges (connections between nodes). In a network model, the symptoms themselves comprise the disorder. The onset and maintenance of symptoms is determined by tracing a path through the network (McNally et al., 2015). For example, a strong physiological reaction to a trauma cue can lead to a strong emotional reaction, which can then lead to avoidance of thoughts about the trauma and avoidance of external reminders of the trauma. Comorbidity is modeled by expanding of the network to include symptoms of other disorders. Those disorders with a high rate of comorbidity would have a high edge density, defined as numerous edges between symptoms (Afzali et al., 2017). Edge density is used to identify local symptom communities. Communities are groups of nodes that have a greater set of edges to each other than to other sets of nodes in the network.
Network analyses have been applied to the diagnosis of PTSD (Armour et al., 2015; McNally et al., 2015; Stockert et al., 2018). The centrality of each symptom was the primary focus of these analyses. Centrality refers to the extent that a node is integral to the networks structure (Barrat et al., 2007). Symptoms of reactivity to trauma cues and negative trauma-related emotions consistently had high strength centrality, defined as the magnitude of the weights for all edges to a node (Armour et al., 2017; Bryant et al., 2017; Stockert et al., 2018). The centrality of these two nodes implies that PTSD may have two components. As per the quadripartite model, negative trauma related emotions is more closely aligned with the general distress factor whereas trauma cue reactivity is more closely aligned with a specific factor of fear-based symptoms. It is unclear, however, how the remaining symptoms cluster around these two central symptoms.
Only a handful of studies have examined comorbidity using networks. Afzali et al. (2017) examined a network of PTSD and depression symptoms using DSM IV criteria. The results suggested that the edge density was higher within a diagnosis than across diagnoses. The strongest edges that bridged PTSD and MDD were among the symptoms that were present in both conditions including difficulties with sleep, irritability, and difficulties with concentration. A second study examined a network of MDD and GAD symptoms (Beard et al., 2016). There was greater density within a disorder than across disorders. The most central nodes within this network were MDD-Depressed mood, GAD-Unable to relax, and GAD-Uncontrollable worry. The strongest cross disorder edges were again found in symptoms present in both conditions. These studies did not examine the community structure of the network and so it is unclear how the centrality of these nodes fit within the network structure.
Only one study examined communities with comorbid conditions. In a network of PTSD and MDD symptoms, four communities were detected. MDD was divided into two communities, one that contained primarily mood symptoms and another that contained somatic symptoms (Choi et al., 2017). PTSD was divided in two communities as well. The first included the cluster B (Intrusions) and cluster C (Avoidance) symptoms whereas the remaining symptoms formed a second community. There were several cross-community edges among negative affect symptoms and those present in both diagnoses. However, this study had several limitations that warrant further investigation such as the sample contained only men and the DSM-IV definition of PTSD was used.
Another aspect of networks that can explain comorbidity is hub symptoms. Hub symptoms are nodes with numerous edges that are of a moderate weight. Hub symptoms create indirect effects for all symptoms to which they are connected. The edges among the hub are of moderate to high weight, which means this indirect effect is likely meaningful. Hubs with edges to symptoms across disorders serve as relevant bridges along which comorbidity may occur. Hubs are determined by their weighted degree, a metric of centrality that classifies nodes according to their strength (sum of edge weights) and degree (count of edges) (Opsahl et al., 2010).
The present study explored the comorbidity of PTSD, Depression, and GAD in a trauma-exposed sample using network analysis. It was hypothesized that the symptoms of these three disorders would form a sparsely connected network. The quadripartite model guided hypotheses about the structure of the network. Depression and GAD symptoms that are thought to be heavily undergirded by the general distress factor were hypothesized to have high edge density and form their own community. The symptoms of PTSD Cluster-D (NACM) were hypothesized have the greatest edge density with depression and GAD, as this cluster is also thought to be associated with the general distress factor. NACM symptoms were hypothesized to be part of the Depression & GAD community given their theoretical association with the general distress factor. PTSD Cluster-B (Intrusions) and Cluster-C (Avoidance) were hypothesized to have a higher density of edges with each other and form their own community. These symptoms have shown greater specificity from other clusters in PTSD in prior work. Finally, symptoms of negative affect in PTSD (cluster-D) and depression were hypothesized to be hub symptoms as these are thought to most closely reflect the general distress factor.
Methods
Participants & Procedure
Participants were 1184 individuals who endorsed a traumatic event that met Criterion A for a diagnosis of PTSD (APA, 2013). Recruitment occurred via Amazon’s Mechanical Turk (MTurk), an online survey platform. Samples recruited via MTurk provide valid clinical and community data that is comparable to trauma exposed samples recruited via traditional methods (Shapiro et al., 2013; van Stolk-Cooke et al., 2018). Such samples are more demographically diverse than typical community cohorts (Buhrmester et al., 2011). Prospective participants first completed the Life Events Checklists (LEC) to determine if they endorsed a potentially traumatic event that met Criterion A. Embedded within the remaining measures were 5 validity checks to ensure participants provided valid responses (e.g., For this item, please select “5”). A valid case was defined as answering at least 3 of these responses correctly and taking more than 5 minutes to complete all surveys. This strategy increases the validity of survey data collected from MTurk (Paolacci et al., 2010; Paolacci and Chandler, 2014). Participants’ accounts were flagged once they completed the measures to prevent repeated responses. A total of N = 1669 individuals completed the measures. Of these, 351 reported a traumatic event that did not meet Criterion A and 32 did not meet the validity criteria. Of the remaining cases, 102 had missing data on the PCL-5, GAD-7, or PHQ-8 and were excluded.
Participants were M = 31.79, SD = 11.21 years of age and 56.7% of the sample identified as female. The majority of the sample was single (n = 532, 44.9%) or married (n = 359, 30.3%). The sample predominately self-identified as White (n = 709, 64.3%), White-Latino (n = 203, 18.4%), African American (n = 67, 6.7%), and Asian American (n = 86, 7.8%). Slightly less than half the sample (n = 568, 48.2%) reported making less than $20,000 per year.
Measures
Life Events Checklist-5
(LEC-5; Weathers et al., 2013): The LEC-5 is a 17-item self-report measure that assesses exposure to potentially traumatic events across one’s life span. Participants reported exposure to 16 known events, with an additional item included to assess exposure to other extraordinary stressful events. The extended version of the LEC, which asked participants to describe the worst event was used.
PTSD Checklist-5
(PCL-5; Weathers et al., 2013): The PCL-5 is a 20-item self-report measure that assesses PTSD symptoms experienced over the last month. The PCL-5 was anchored to the traumatic event specified in the LEC. Items assess severity on a 0–4 point Likert scale. The internal consistency of responses on the PCL was excellent, α = 0.95.
Patient Health Questionnaire-8
(PHQ-8; Kroenke et al., 2009): The PHQ-8 is an 8-item self-report measure that assesses depression symptoms experienced over the past two weeks on a 0–3 point Likert scale. The PHQ-8 is adapted from the PHQ-9 and removes an item on suicidal ideation. The internal consistency of responses on the PHQ-8 was excellent, α = 0.90.
Generalized Anxiety Disorder-7
(GAD-7; Spitzer et al., 2006): The GAD-7 is a 7-item self-report measure that assesses GAD symptoms experienced over the past two weeks. Ratings are made on a 0–3 point Likert scale. The reliability of responses on the GAD-7 was excellent, α = 0.92.
Data Analytic Plan
Network analyses were conducted in R (v.3.4.1) using the qgraph (Epskamp et al., 2012) and bootnet packages (Epskamp et al., 2017). The nodes were symptoms of PTSD, depression, and GAD. Symptoms that appeared in measures of multiple diagnoses were removed such that each symptom only appeared once in the network. The removed symptoms were, GAD-7 Item 5 (restlessness), PHQ-8 Item 3 (sleep difficulties), and PCL-5 Item 12 (loss of interest in pleasurable activities) and Item 19 (concentration difficulties). The network was estimated using a Gaussian Graphical Model (GGM: Constantini et al., 2015). Edges corresponded to partial correlation coefficients of a regularized regression between symptoms. The graphical LASSO (glasso) is applied to regularize the magnitude of each regression weight based on a tunable parameter λ (Friedman et al., 2008). λ is selected so that it minimizes the Extended Bayesian Information Criterion (EBIC: Chen & Chen 2008). Glasso shrinks regression weights to exactly 0, which removes the edge between two nodes. Coefficients that were > 0 were included as edges with the magnitude of the coefficient serving as the weight. The stability of the network was analyzed according to the recommendations of Epskamp et al. (2018).
Network Stability.
Networks stability refers to the confidence that the results obtained from a given network will be replicated. The stability of the network was examined with the case-dropping subset bootstrap with a correlation stability coefficient threshold of 0.5. Of interest is the proportion of cases that can be removed before the correlation between the centrality metrics of the total sample and the reduced sample falls below 0.5.
Density.
Density was defined as the number of observed edges / the number of possible edges or n x (n-1)/2 for nodes within a diagnosis and nDiagnosis 1 x n Diagnosis 2 across diagnoses. The density of connections within each symptom category was compared using a χ2 test for equal proportions with Yate’s continuity correction.
Community Detection.
The community structure of the network was evaluated using the information map algorithm (Rosvall and Bergstrom, 2008) within the igraph package (Csardi & Nepusz, 2006). Communities are determined by the amount of memory required to store the length of a path between two nodes such that the path between nodes within the same community will require less storage than the path to a node outside the community (Cover and Thomas, 2012). A second algorithm, the walktrap algorithm (Pons and Latapy, 2005), was used to confirm the presence of the communities.
Centrality.
Three metrics of network centrality were computed for each node in the network: 1) Weighted Degree, 2) Closeness, 3) Betweenness. Weighted Degree refers to a combination of the degree (number of edges) and strength (sum of the edge weights) for a given node. Weighted degree is calculated with the guidelines presented by Opshal et al. (2010). The tuning parameter, α was set to 0.5. Closeness refers to the inverse of the mean shortest path from all other nodes to a given node using the weighted degree. Betweenness refers to the inverse of the number of shortest paths between all pairs of nodes that include a given node. Closeness and Betweenness were calculated using node strength.
Results
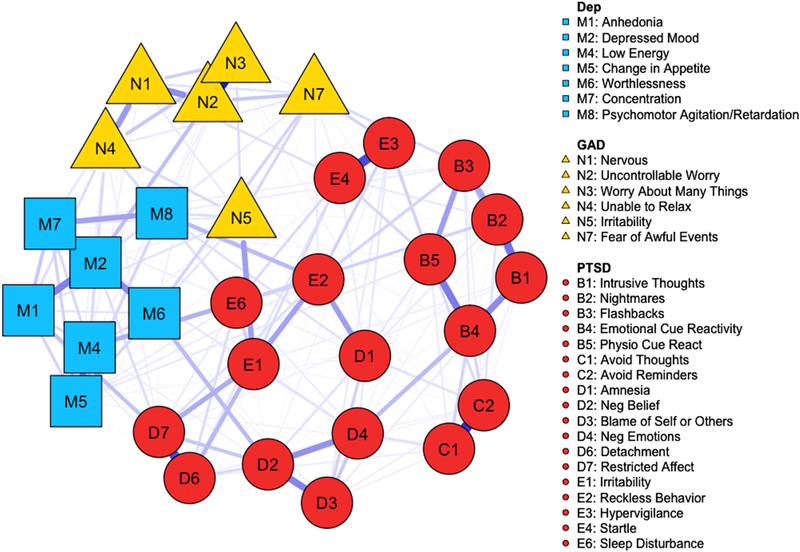
Descriptive information is presented in Table 1. A sparse network that consisted of 31 nodes and 197 edges was obtained (Figure 1). A stability analysis suggested that that network was highly stable such that a correlation of 0.5 or greater for the metrics of all centrality was maintained when more than 50% of the sample was removed (Figure S1). Overall, 42.4% of the possible edges within the network were estimated. Edge density was highest within each disorder: GAD – 86.67%; depression – 76.2%; PTSD – 57.5%. Proportional chi-square tests suggested that there were no differences in the connectivity within each diagnosis (p’s = .054 – .722). Across disorders, symptoms of PTSD and depression had 19.4% of the possible edges present and PTSD and GAD had 25.4% of the possible edges present. Depression and GAD, however, were substantially more connected with 64.3% of the possible edges present. The proportion of edges present between depression and GAD was significantly greater than that between PTSD and depression (χ2(1) = 19.24, p < .001) and PTSD and GAD (χ2 (1) = 25.92, p < .001).
Table 1.
Descriptive statistics
| Variable | Mean | Standard Deviation |
|---|---|---|
| PCL-5 | 19.97 | 17.76 |
| PHQ-8 | 6.85 | 6.85 |
| GAD-7 | 6.38 | 6.38 |
| N | % | |
| PCL-5 ≥ 33 | 275 | 23.2 |
| PHQ-8 ≥ 10 | 376 | 31.8 |
| GAD-7 ≥ 10 | 314 | 26.5 |
Note: Total sample is N = 1184. PCL-5 = PTSD Checklist for the DSM 5. PHQ-8 = Patient Health Questionnaire – 8 Items. GAD-7 = Generalized Anxiety Disorder – 7 Item screen. A score on the PCL-5 ≥ 33 indicates the likely presence of PTSD. A score on the PHQ-8 ≥ 10 indicates the presence of moderate to severe depression. A score on the GAD-7 ≥ 10 indicates the presence of moderate to severe anxiety.
Figure 1.
Diagram of the network according to DSM-5 diagnostic categories. Circles are symptoms of PTSD. Squares are symptoms of Depression. Triangles are symptoms of GAD. Edges reflect the weighted relation between nodes with color and size determined by the edge weight.
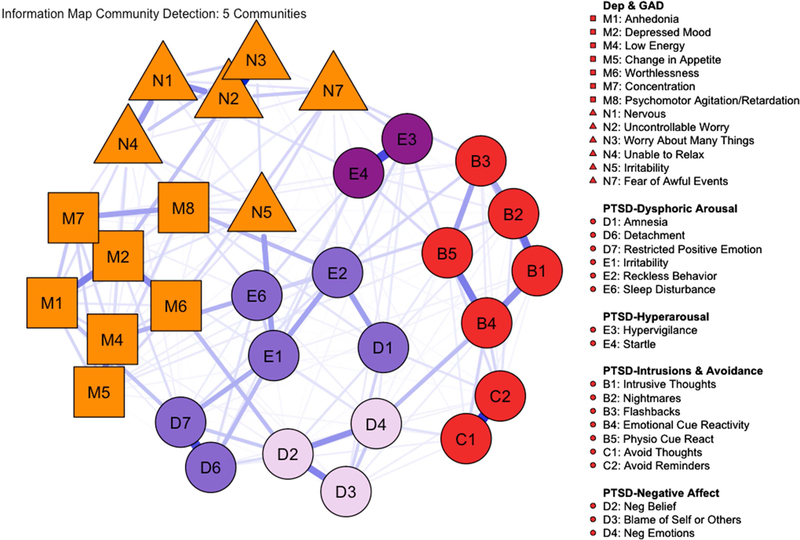
Five communities were detected (Figure 2). The largest community included all the symptoms of GAD and depression. The remaining four communities were comprised of PTSD symptoms. The first PTSD community comprised all of PTSD cluster B (Intrusions) and C (Avoidance). The next included two symptoms of cluster-E (AAR), PTSD-E3 (Hypervigilance) and PTSD-E4 (Exaggerated startle). The third PTSD community consisted of PTSD symptoms from cluster-D (NACM) centered around negative affect: PTSD-D2 (Negative beliefs about self, others, and the world), PTSD-D3 (Blame of self or others), and PTSD-D4 (Strong negative emotions). The fourth PTSD community contained symptoms from cluster D (NACM) and E (AAR) that corresponded to dysphoria and externalizing behaviors. There was considerable overlap between the communities detected in this algorithm and the walktrap algorithm (Figure S2). The density of edges across each community indicated that the PTSD community of symptoms from cluster B and C has the highest edge density (67%) with the PTSD negative affect community (Figure 3).
Figure 2.
Communities as determined by the information map community detection algorithm. Nodes of the same color are of the same community. Shapes correspond to the DSM 5 diagnoses with PTSD = circles, Depression = squares, GAD = triangles.
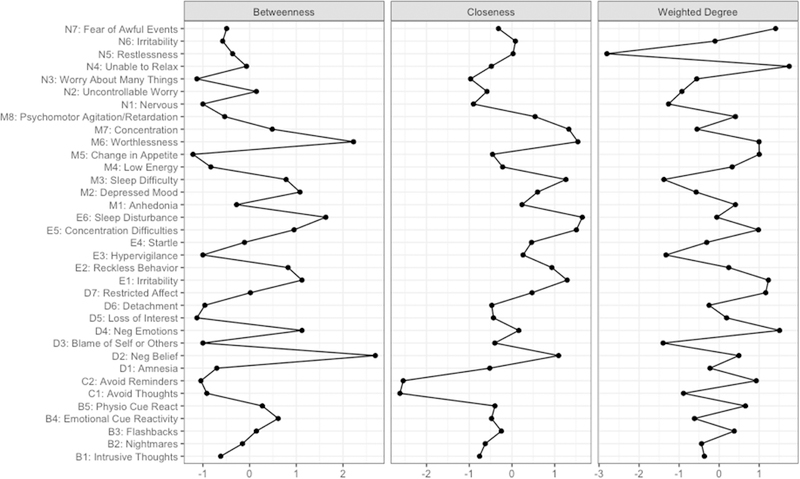
Figure 3.
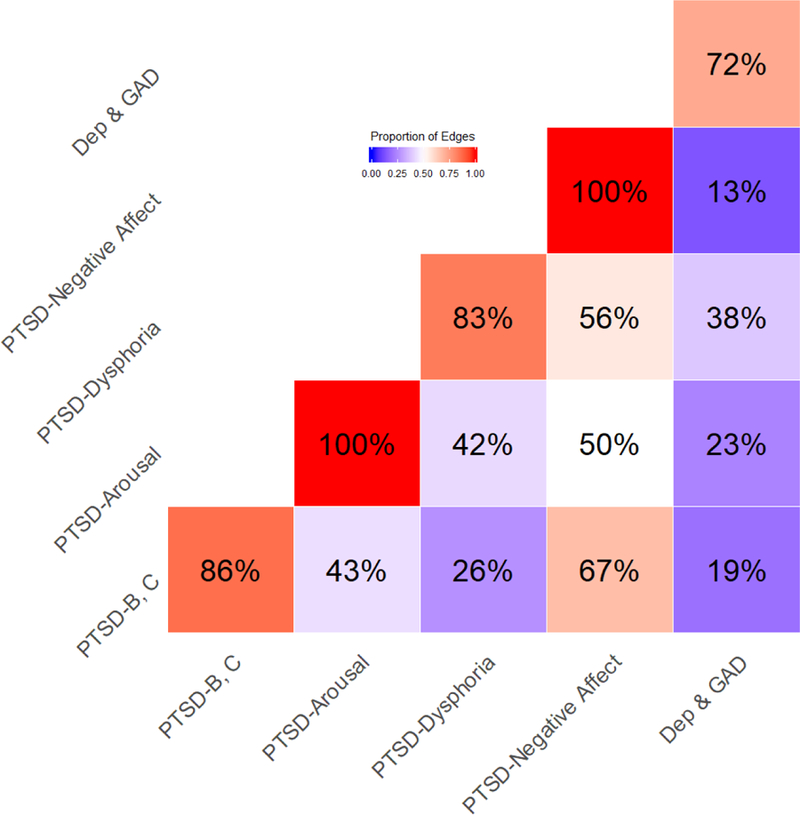
Heatmap of the proportion of edges between (off-diagonal) and within (diagonal) the communities identified by the information map community detection algorithm.
The weighted degree of all symptoms identified several hub symptoms (Figure 4, right panel). The symptom with the highest weighted degree was PTSD-D7 (Restricted or Diminished Positive Emotion). It had 16 total edges (4 to depression, 1 to GAD, 11 to PTSD). These edges suggest this symptom is a key bridge across PTSD, depression, and GAD. It also served as a local hub within the PTSD diagnosis. The symptom with the second highest weighted degree was GAD N4 (difficulty relaxing). Of GAD N4’s 16 total edges, 6 were with symptoms of depression and 6 were with symptoms of PTSD, suggesting it also served an important hub role between all three diagnoses.
Figure 4.
Centrality metrics for each node in the network. B1 – E6 correspond to the symptoms of PTSD (B = Intrusions, C = Avoidance, D = NACM, E = AAR). M1 – M 8 correspond to symptoms of Depression. N1 – N7 correspond to symptoms of GAD. X-axis are standardized (z-scores).
The betweenness and closeness centrality of negative affect symptoms were the highest in the network, consistent with the quadripartite theory that these diagnoses are comprised of significant general distress (Figure 4). Specifically, PTSD-D2 (Negative beliefs about self and the world) had the highest betweenness centrality as well as the third highest closeness centrality. PTSD-E2 (Reckless behavior) had the highest closeness centrality. MDD-D6 (Worthlessness) had the second highest betweenness centrality and highest closeness centrality.
Discussion
The results of the present study offer new insights as to how comorbidity between PTSD, depression, and GAD occurs. The network was sparsely connected and formed a single component - all symptoms were directly or indirectly connected - which is consistent with prior studies (Armour et al., 2015; Beard et al., 2016; Choi et al., 2017; McNally et al., 2015). The community structure suggests that depression and GAD are highly related such that there are numerous pathways by which the symptoms interact. It also suggests that PTSD was heterogeneous in that negative affect and externalizing symptoms were more related to depression and GAD than fear-based symptoms.
The present study was the first to evaluate communities within a network of these disorders. The community structure was largely consistent with the hypotheses that were guided by the quadripartite model of psychopathology (Watson, 2009). The symptoms of GAD and depression formed a community, which further supports their association with the underlying general distress factor. These results suggest that a symptom of depression or GAD is of comparable distance from any another symptom of depression or GAD. This limited separation of the symptoms is indicative of the high comorbidity between these conditions. The strongest cross-diagnostic edges of chronic worry ν depressed mood and depressed mood ν inability to relax edges suggest a possible process by which comorbidity may emerge. These edges were found in prior work (Beard et al., 2016). That these disorders were in the same community, however, points to the presence of numerous symptom-level pathways by which these disorders may reinforce each other. Examining these pathways in greater detail through an exploration of causal mechanisms and the underlying biological factors is a necessary next step.
PTSD was divided into four communities that did not correspond directly to the clusters as indicated by the DSM 5. As hypothesized, the symptoms of cluster B (intrusions) and cluster C (avoidance) formed a community, which represents the fear-specific symptoms of the disorder. Factor analytic work has shown that these clusters are more strongly related to each other than the other clusters of PTSD (Elhai et al., 2015; Price et al., 2017; Price and van Stolk-Cooke, 2015). Work using fear conditioning paradigms has shown that intrusions and avoidance symptoms are more strongly associated with the extinction of fear (Norrholm et al., 2011). Thus, fear conditioning may be a particularly useful model for understanding this aspect of the disorder. Within the quadripartite model, these clusters have greater specificity, which suggests that they should be separate from those symptoms who are more closely aligned with general distress. The second community included PTSD-E3 (Exaggerated startle) and PTSD-E4 (Hypervigilance). The distinction of these symptoms from the intrusions and avoidance community is conceptualized as a state of generalized reactivity to threat instead of reactivity specifically to trauma cues.
The remaining communities of PTSD were more closely aligned with negative affect. The third community reflected the negative affect core of PTSD (PTSD-D2: Negative beliefs about the self, others and the world; PTSD-D3: Blame of self or others; PTSD-D4: Strong negative emotions) (Foa, 2006). This community is consistent with findings of the 7-factor model of PTSD in which these symptoms form a factor of negative affect (Armour et al., 2015; Pietrzak et al., 2015). The remaining symptoms of cluster E (AAR) and cluster D (NACM) formed the fourth community. This community contained the most heterogeneous set of symptoms, many of which reflect externalizing symptoms and social withdrawal. These two communities are proposed to represent the onset of negative affect and its consequences. The cluster E and D community had the highest density of edges with the Depression & GAD community, which suggests that these symptoms may be a bridge for comorbidity. Indeed, this community contained PTSD-D7 (Restricted or Diminished Positive Emotion), which had the highest weighted degree in the network and was connected to several depression symptoms. These communities may be more closely aligned with the general distress factor and thus are more relevant to comorbidity than the other communities.
The hub nodes identified symptoms of restricted or diminished positive emotion as those with the greatest weighted degree in the network. Restricted or diminished positive emotion was the strongest hub in that it created indirect effects between a majority of PTSD symptoms and depression symptoms. Inability to relax was the second strongest hub. From a clinical perspective, these hubs suggest that symptoms from each disorder contribute to each condition. These two hubs were directly connected, which also suggests a primary path by which symptoms from each disorder may influence one another.
These results have implications for transdiagnostic treatments (Farchione et al., 2012). The connectedness of these disorders highlights the need for treatment strategies that are able to adequately address comorbidity. The presence of a single community for depressive and GAD symptoms suggests that treatments that target both diagnoses are likely to have improved efficacy than those that target just one. Relatedly, the community structure of PTSD also highlights the utility of a transdiagnostic approach. Distinct communities for intrusions & avoidance and negative affect suggests the need for approaches that target trauma reactivity symptoms and mood symptoms. Finally, the low density of edges across the Depression & GAD and PTSD communities suggests that addressing symptoms of depression and GAD may not address PTSD symptoms. As such, transdiagnostic treatments may benefit from being tailored towards trauma-specific symptoms.
The present study had several limitations of note. First, the data were obtained cross-sectionally, yet psychopathology networks represent dynamic processes (McNally, 2012). The directionality of the edges cannot be determined. Second, the sample was drawn from the community and had a range of trauma exposures. Although recent work has suggested that the structure of PTSD may be similar across trauma types (Contractor et al., 2018), this is a source of variability that was unaccounted for in the present study. Diagnostic instruments were not used and thus it is unclear if these results generalize to clinical populations. Third, only self-report measures were used. Relatedly, certain opposing symptoms (e.g., Depression hypersomnia or insomnia) were evaluated with a single item, which may have affected the presence of edges. Network models have been critiqued for having limited replicability across samples, especially when examining specific edges (Forbes et al., 2017). Specific edge pathways found in the current analysis should be replicated before drawing firm conclusions. Finally, the sample had relatively low ethno-racial diversity, which may limit the generalizability to specific populations.
The results of the present study demonstrate the utility of using networks to understand comorbidity. The detection of several communities helps to understand the symptoms most strongly connected to each other. The detected communities did not map onto the factor structure or diagnostic categorization of the disorders yet fit well with theoretical models of psychopathology. The hub symptoms point to the role of negative affect in connecting a range of disparate symptoms across conditions. Future work using these models should examine data from treatment outcome studies to test the hypothesis that targeting such hub symptoms is beneficial. These results also indicate that transdiagnostic treatment are likely necessary to address the integrated structure of these symptoms.
Supplementary Material
Highlights.
Symptoms of GAD and MDD were more densely connected to each other than to PTSD.
5 communities were detected. MDD and GAD symptoms formed a single community.
PTSD was divided into 4 communities that did not correspond to the DSM 5 clusters.
Inability to relax and restricted affect were hub symptoms.
Comorbidity likely occurs via indirect relations established by the hub symptoms.
Acknowledgements
This work was supported by the National Institute of Mental Health [K08-MH107661-01A1 (PI: Price)].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Afzali MH, Sunderland M, Teesson M, Carragher N, Mills K, Slade T, 2017. A network approach to the comorbidity between posttraumatic stress disorder and major depressive disorder: The role of overlapping symptoms. J. Affect. Disord 208, 490–496. 10.1016/j.jad.2016.10.037 [DOI] [PubMed] [Google Scholar]
- Armour C, Fried EI, Deserno MK, Tsai J, Pietrzak RH, 2017. A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in U.S. military veterans. J. Anxiety Disord 45, 49–59. 10.1016/j.janxdis.2016.11.008 [DOI] [PubMed] [Google Scholar]
- Armour C, Tsai J, Durham TA, Charak R, Biehn TL, Elhai JD, Pietrzak RH, 2015. Dimensional structure of DSM-5 posttraumatic stress symptoms: Support for a hybrid Anhedonia and Externalizing Behaviors model. J. Psychiatr. Res 61, 106–113. 10.1016/j.jpsychires.2014.10.012 [DOI] [PubMed] [Google Scholar]
- Barrat A, Barthélemy M, Vespignani A, 2007. The Architecture of Complex Weighted Networks: Measurements and Models, in: Large Scale Structure and Dynamics of Complex Networks, Complex Systems and Interdisciplinary Science. WORLD SCIENTIFIC, pp. 67–92. 10.1142/9789812771681_0005 [DOI]
- Beard C, Millner AJ, Forgeard MJC, Fried EI, Hsu KJ, Treadway MT, Leonard CV, Kertz SJ, Björgvinsson T, 2016. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol. Med 46, 3359–3369. 10.1017/S0033291716002300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Cramer AOJ, 2013. Network Analysis: An Integrative Approach to the Structure of Psychopathology. Annu. Rev. Clin. Psychol 9, 91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- Bryant RA, Creamer M, O’Donnell M, Forbes D, McFarlane AC, Silove D, Hadzi-Pavlovic D, 2017. Acute and Chronic Posttraumatic Stress Symptoms in the Emergence of Posttraumatic Stress Disorder: A Network Analysis. JAMA Psychiatry 74, 135–142. 10.1001/jamapsychiatry.2016.3470 [DOI] [PubMed] [Google Scholar]
- Bryant RA, O’Donnell ML, Creamer M, McFarlane AC, Clark CR, Silove D, 2010. The psychiatric sequelae of traumatic injury. Am. J. Psychiatry 167, 312–320. 10.1176/appi.ajp.2009.09050617 [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, Gosling SD, 2011. Amazon’s Mechanical Turk A New Source of Inexpensive, Yet High-Quality, Data? Perspect. Psychol. Sci 6, 3–5. 10.1177/1745691610393980 [DOI] [PubMed] [Google Scholar]
- Choi KW, Batchelder AW, Ehlinger PP, Safren SA, O’Cleirigh C, 2017. Applying network analysis to psychological comorbidity and health behavior: Depression, PTSD, and sexual risk in sexual minority men with trauma histories. J. Consult. Clin. Psychol 85, 1158–1170. 10.1037/ccp0000241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Caldas SV, Dolan M, Lagdon S, Armour C, 2018. PTSD’s factor structure and measurement invariance across subgroups with differing count of trauma types. Psychiatry Res 264, 76–84. 10.1016/j.psychres.2018.03.065 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Elhai JD, Fine TH, Tamburrino MB, Cohen G, Shirley E, Chan PK, Liberzon I, Galea S, Calabrese JR, 2015. Latent profile analyses of posttraumatic stress disorder, depression and generalized anxiety disorder symptoms in trauma-exposed soldiers. J. Psychiatr. Res 68, 19–26. 10.1016/j.jpsychires.2015.05.014 [DOI] [PubMed] [Google Scholar]
- Cover TM, Thomas JA, 2012. Elements of Information Theory John Wiley & Sons. [Google Scholar]
- Elhai JD, Contractor AA, Tamburrino M, Fine TH, Cohen G, Shirley E, Chan PK, Liberzon I, Calabrese JR, Galea S, 2015. Structural relations between DSM-5 PTSD and major depression symptoms in military soldiers. J. Affect. Disord 175, 373–378. 10.1016/j.jad.2015.01.034 [DOI] [PubMed] [Google Scholar]
- Epskamp S, Borsboom D, Fried EI, 2018. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 50, 195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, Gallagher MW, Barlow DH, 2012. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: A Randomized Controlled Trial. Behav. Ther., SPECIAL SERIES: Innovations in the Treatment of Anxiety Psychopathology 43, 666–678. 10.1016/j.beth.2012.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, 2006. Psychological Processes Related to Recovery from a Trauma and an Effective Treatment for PTSD. Ann. N. Y. Acad. Sci 821, 410–424. 10.1111/j.1749-6632.1997.tb48295.x [DOI] [PubMed] [Google Scholar]
- Forbes MK, Wright AGC, Markon KE, Krueger RF, 2017. Evidence that psychopathology symptom networks have limited replicability. J. Abnorm. Psychol 126, 969–988. 10.1037/abn0000276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J, Hastie T, Tibshirani R, 2008. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 9, 432–441. 10.1093/biostatistics/kxm045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant DM, Beck JG, Marques L, Palyo SA, Clapp JD, 2008. The structure of distress following trauma: Posttraumatic stress disorder, major depressive disorder, and generalized anxiety disorder. J. Abnorm. Psychol 117, 662–672. 10.1037/a0012591 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, Wang P, Wells KB, Zaslavsky AM, 2005. Prevalence and treatment of mental disorders, 1990 to 2003. N. Engl. J. Med 352, 2515–2523. 10.1056/NEJMsa043266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH, 2009. The PHQ-8 as a measure of current depression in the general population. J. Affect. Disord 114, 163–173. 10.1016/j.jad.2008.06.026 [DOI] [PubMed] [Google Scholar]
- McNally RJ, 2012. The Ontology of Posttraumatic Stress Disorder: Natural Kind, Social Construction, or Causal System? Clin. Psychol. Sci. Pract 19, 220–228. 10.1111/cpsp.12001 [DOI] [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno MK, Borsboom D, 2015. Mental Disorders as Causal Systems: A Network Approach to Posttraumatic Stress Disorder. Clin. Psychol. Sci 3, 836–849. 10.1177/2167702614553230 [DOI] [Google Scholar]
- Norrholm SD, Jovanovic T, Olin IW, Sands LA, Karapanou I, Bradley B, Ressler KJ, 2011. Fear Extinction in Traumatized Civilians with Posttraumatic Stress Disorder: Relation to Symptom Severity. Biol. Psychiatry, Genes and Anxiety 69, 556–563. 10.1016/j.biopsych.2010.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opsahl T, Agneessens F, Skvoretz J, 2010. Node centrality in weighted networks: Generalizing degree and shortest paths. Soc. Netw 32, 245–251. 10.1016/j.socnet.2010.03.006 [DOI] [Google Scholar]
- Paolacci G, Chandler J, 2014. Inside the Turk Understanding Mechanical Turk as a Participant Pool. Curr. Dir. Psychol. Sci 23, 184–188. 10.1177/0963721414531598 [DOI] [Google Scholar]
- Paolacci G, Chandler J, Ipeirotis PG, 2010. Running experiments on Amazon Mechanical Turk. Judgm. Decis. Mak 5, 411–419. [Google Scholar]
- Pietrzak RH, Tsai J, Armour C, Mota N, Harpaz-Rotem I, Southwick SM, 2015. Functional significance of a novel 7-factor model of DSM-5 PTSD symptoms: Results from the National Health and Resilience in Veterans Study. J. Affect. Disord 174, 522–526. 10.1016/j.jad.2014.12.007 [DOI] [PubMed] [Google Scholar]
- Pons P, Latapy M, 2005. Computing Communities in Large Networks Using Random Walks, in: Computer and Information Sciences - ISCIS 2005, Lecture Notes in Computer Science Presented at the International Symposium on Computer and Information Sciences, Springer, Berlin, Heidelberg, pp. 284–293. 10.1007/11569596_31 [DOI] [Google Scholar]
- Price M, Pallito S, Legrand AC, 2017. Heterogeneity in the Strength of the Relation Between Social Support and Post-Trauma Psychopathology. J. Psychopathol. Behav. Assess 1–10. 10.1007/s10862-017-9629-3 [DOI] [PMC free article] [PubMed]
- Price M, van Stolk-Cooke K, 2015. Examination of the interrelations between the factors of PTSD, major depression, and generalized anxiety disorder in a heterogeneous trauma-exposed sample using DSM 5 criteria. J. Affect. Disord 186, 149–155. 10.1016/j.jad.2015.06.012 [DOI] [PubMed] [Google Scholar]
- Rosvall M, Bergstrom CT, 2008. Maps of random walks on complex networks reveal community structure. Proc. Natl. Acad. Sci 105, 1118–1123. 10.1073/pnas.0706851105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro DN, Chandler J, Mueller PA, 2013. Using Mechanical Turk to study clinical populations. Clin. Psychol. Sci 2167702612469015. 10.1177/2167702612469015 [DOI]
- Spitzer RL, Kroenke K, Williams JW, Lowe B, 2006. A brief measure for assessing generalized anxiety disorder: The gad-7. Arch. Intern. Med 166, 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Stockert SHH von, Fried EI, Armour C, Pietrzak RH, 2018. Evaluating the stability of DSM-5 PTSD symptom network structure in a national sample of U.S. military veterans. J. Affect. Disord 229, 63–68. 10.1016/j.jad.2017.12.043 [DOI] [PubMed] [Google Scholar]
- van Stolk-Cooke K, Brown A, Maheux A, Parent J, Forehand R, Price M, 2018. Crowdsourcing Trauma: Psychopathology in a Trauma-Exposed Sample Recruited via Mechanical Turk. J. Trauma. Stress 31, 549–557. 10.1002/jts.22303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, 2009. Differentiating the Mood and Anxiety Disorders: A Quadripartite Model. Annu. Rev. Clin. Psychol 5, 221–247. 10.1146/annurev.clinpsy.032408.153510 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.