Abstract
Background
The American Congress of Obstetricians and Gynecologists recommends that a pelvic examination be offered to asymptomatic women after an informed discussion with their provider. While the adverse health outcomes the examination averts were not delineated, the organization stated that it helps establish open communication between patients and physicians. Recent surveys have focused on obstetrician-gynecologists’ attitudes and beliefs about the examination, but the perspectives of women have not been well characterized.
Objective
To better understand women’s beliefs about the purpose and value of routine pelvic examinations.
Study Design
We conducted structured interviews with 264 women aged 21 to 65 years who agreed to participate in a 50-minute interview about cervical cancer screening. Recruitment took place in outpatient women’s clinics at a public hospital and an academic medical center in San Francisco, California. Women were shown an illustration of a bimanual pelvic exam and asked a series of closed-ended questions: if they knew why it was performed, if it reassured them of their health and if they felt it helped establish open communication with their provider. Women were asked an open-ended question about their perception of the examination’s purpose. Multivariable logistic regression analysis was used to identify demographic predictors of responses.
Results
About half (56%) of the participants stated that they knew the examination’s purpose. The most frequently cited reason was assurance of normalcy. The majority of participants (82%) believed the examination reassured them of their health. Just under two-thirds (62%) believed that the examination helps establish open communication with their provider. In multivariate analyses, older age (45+ years) independently predicted a higher likelihood of a belief that they knew the examination’s purpose [odds ratio (OR) 2.9, 95% confidence interval (CI) 1.5–5.6] and a belief that it facilitates open communication (OR 2.1, 95%CI 1.1–3.9). Non-white race also was associated with a belief that the examination helps facilitate open communication between patients and providers (OR 1.9, 95%CI 1.1–3.1).
Conclusions
About half of the women who participated in our study reported not knowing the purpose of the pelvic examination, yet most believed it to be of some value, especially reassurance of health. To achieve shared, informed decision making, clinicians will need to better communicate to their patients the examination’s purpose.
Keywords: patient preferences, patient view, routine pelvic examination
Introduction
Standard gynecology office practice continues to evolve in response to evidence-based recommendations. Cervical cancer screening intervals have increased (1, 2), and both screening for sexually transmissible infections and provision of hormonal birth control have been uncoupled from pelvic examinations (3, 4). Thus, the purpose of the annual pelvic examination in asymptomatic women has been questioned (5, 6), and current recommendations for performing the examination are conflicting.
In 2014, a systematic review and meta-analysis focused on screening pelvic examinations found no evidence of its value in decreasing morbidity and mortality of a variety of conditions, including ovarian cancer and pelvic inflammatory disease (7). The review identified possible harms, both from the examination itself (such as pain, discomfort, anxiety) and from downstream consequences of positive testing, including unnecessary surgery. In response, the American College of Physicians (ACP) recommended against performing screening pelvic examinations in non-pregnant, asymptomatic women (8). At the same time, the American Congress of Obstetricians and Gynecologists (ACOG) reaffirmed its 2012 recommendation for annual speculum and bimanual examinations for all women aged 21 and older (9), despite acknowledging that no evidence supports or refutes the examination for asymptomatic, low-risk patients. The organization further advised that the decision regarding whether or not to perform the examination should be after a discussion between the patient and her provider. In a Practice Advisory (10,11), ACOG cited additional benefits, including an opportunity to explain anatomy, assure normalcy and answer specific questions, “thus establishing open communication between patient and physician”.
In 2015, ACOG’s Well Woman Task Force (12) stated that a pelvic examination should be offered to asymptomatic women after an informed discussion with their provider although the health benefits the examination aims to achieve were not stated. Obstetrician-gynecologists in the United States have been surveyed about their attitudes and beliefs concerning screening pelvic examinations (13) and been found to have favorable attitudes, but little is known about women’s perspectives. Our study sought to further understand women’s beliefs about the pelvic examination, including their understanding of its purpose and its perceived value.
Materials and Methods
This survey was conducted as part of a study of patient preferences for various cervical cancer screening strategies. For the main study, we aimed to recruit 450 English- or Spanish-speaking women seeking care at outpatient women’s clinics at a public hospital (Zuckerberg San Francisco General Hospital and Trauma Center) and an academic medical center in San Francisco, California [University of California, San Francisco (UCSF) Mt. Zion Hospital Women’s Clinic]. These clinics serve women with a variety of obstetrical and gynecologic conditions commonly seen in routine practice. The criteria for enrollment were being aged 21 to 65 years and speaking either English or Spanish. Study personnel identified women meeting these criteria from the clinic schedule and invited them to participate in a structured 50-minute face-to-face interview, during which preferences for the potential outcomes of cervical screening strategies were elicited. Because pelvic examinations are coupled with cervical cancer screening, we asked several questions at the end of the interview regarding the examination. Written informed consent was obtained, and participants were compensated with a $50 gift card.
We collected participant demographic characteristics included age, race, educational level, income level and number of prior births. Participants were shown an illustration of a woman in dorsal lithotomy position undergoing a speculum examination and then answered questions about cervical cancer screening. After completing the preference elicitation portion of the interview, participants were shown an illustration of a bimanual pelvic exam and asked closed-ended questions with response options of ‘yes’, ‘no’ and ‘don’t know’. They were asked “Have you ever had this examination?” and “Do you know why this examination is performed?”. Those responding ‘yes’ to the latter question were asked to explain the reasons, and the interviewer recorded these responses in free text. They were also asked: “Do you think this examination is important to reassure you of your health even if you were having no problems?”, and “Do you think this examination helps establish open communication between you and your health care provider?” as suggested by ACOG. One study investigator reviewed all free text comments and sorted them into broad categories using an iterative process. Two other investigators reviewed the draft categorizations, and a final designation was obtained through consensus.
In June 2014, the ACP issued its recommendation against pelvic examinations, providing an opportunity for our research group to address other novel and relevant questions, including the effect of two different guidelines on women’s desires to have the examination; that portion of the study is on-going. In the current report, we present results from the first 264 enrollees with a focus on answers to questions about their attitudes and beliefs concerning the examination’s purpose and value. These interviews were conducted from September 2014 to October 2015. The Committee on Human Research at UCSF and Zuckerberg San Francisco General Hospital approved the study protocol.
Our sample size was based on the precision around estimates for the preference scores; we had no formal sample size or power calculations for the analyses related to the pelvic examination questions. Multivariable logistic regression analysis was used to identify demographic predictors of responses to the closed-ended questions. We selected variables for each outcome with a P value = 0.05 for the multivariate analyses.
Results
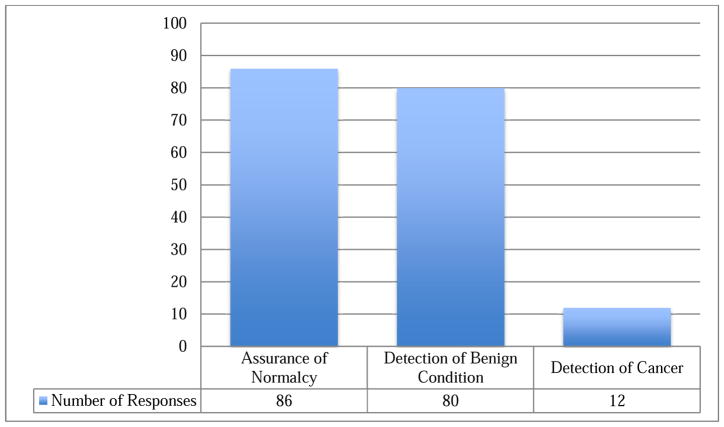
We approached 740 women, 264 (36%) of whom were ultimately interviewed. Study participants represented an urban population of mostly educated, reproductive age, and ethnically diverse women (Table 1). Participants were aged 21 to 65 years. Of the 264 women interviewed, 262 completed all questions. After viewing the illustration of a bimanual examination, 89% of the women reported having had the examination, 8% never had the examination, and 3% were unsure. Of the women stating that they knew its purpose, free text responses were grouped into the following categories: assurance of normalcy, detection of benign conditions and detection of cancerous conditions (Figure 1).
Table 1.
Characteristics of study participants (n=262)*
| Characteristic | N (%)† |
|---|---|
| Age (years) | |
| 21–29 | 79 (30) |
| 30–39 | 103 (39) |
| 40–49 | 44 (17) |
| 50–65 | 36 (14) |
| Race/ethnicity | |
| Caucasian, White or European American | 109 (42) |
| Asian or Pacific Islander | 36 (14) |
| African American or Black | 35 (13) |
| Latina, Latin American, or Hispanic | 48 (18) |
| Native American, American Indian, Alaskan Native or Indigenous Person | 1 (0) |
| Mixed | 24 (9) |
| Other | 9 (3) |
| Highest level of education completed | |
| High school | 45 (18) |
| Some college, junior college or vocational school | 70 (27) |
| College, professional or graduate school | 147 (56) |
| Yearly household income (before taxes) | |
| Under $50,000 | 111 (42) |
| $50,000 – 100,000 | 55 (21) |
| $100,001 – 200,000 | 48 (18) |
| Over $200,000 | 27 (10) |
| Missing | 21 (8) |
| Ever given birth | |
| Yes | 132 (50) |
| No | 130 (50) |
| Total | 262 (100) |
data missing for 2 participants
some percentages do not add to 100 due to rounding
Figure 1. Participant's stated beliefs about the purpose of bimanual pelvic examinations, N=263*, San Francisco 2014–2015.
*Data missing for one participant.
Of 147 women stating that they know the purpose of the pelvic examination, 86 indicated the examination was for assurance of normalcy, 80 referred to detection of benign conditions and 12 believed the examination was for cancer detection. Numbers do not add to 147 since response categories were not mutually exclusive.
Just over half (147/262, 56%) of the participants stated that they knew why the examination is performed (Table 2). In univariate analyses, predictors of answering ‘yes’ to knowing the purpose of the examination were: age 45 years or greater [odds ratio (OR) 2.7, 95% confidence interval (CI) 1.5–5.2), having at least some college education (OR 2.5, 95% CI 1.3–4.8) and ever having given birth (OR 1.7, 95% CI 1.1–2.9). Non-white race predicted a lower likelihood of stating knowledge of the examination’s purpose (OR 0.6, 95% CI 0.4–1.0).
Table 2.
Characteristics associated with knowledge and beliefs about pelvic examinations (N=262)
| Know why exam performed? | Examination important to reassure you of | Examination helps establish open | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Yes | Univariate | Multivariate | Yes | Univariate | Multivariate | Yes | Univariate | Multivariate | ||||||
| N (row%) | OR (95%CI) | P | OR (95%CI) | P | N (row%) | OR (95%CI) | P | OR (95%CI) | P | N (row%) | OR (95%CI) | P | OR (95%CI) | P | |
| Age, years | |||||||||||||||
| 20 to 44 | 102 (50.7%) | ref | ref | 157 (78%) | ref | ref | 118 (58%) | ref | ref | ||||||
| 45 to 65 | 45 (74%) | 2.7 (1.5–5.2) | .002 | 2.9 (1.5–5.6) | .001 | 56 (92%) | 3.1 (1.2–8.3) | .02 | 3.1 (1.2–8.3) | 0.02 | 45 (74%) | 2.0 (1.1–3.7) | .04 | 2.1 (1.1–3.9) | .03 |
| Race | |||||||||||||||
| White | 69 (63%) | ref | ref | 84 (77.1%) | ref | NA | 59 (54%) | ref | ref | ||||||
| Non-white | 78 (51%) | 0.6 (0.4–1.0) | .05 | 0.80 (0.5–1.4) | .43 | 129 (84%) | 1.6 (0.9–3.0) | .14 | 104 (68%) | 1.8 (1.1–3.0) | .02 | 1.9 (1.1–3.1) | .02 | ||
| Education | |||||||||||||||
| No college | 17 (38%) | ref | ref | 38 (84.4%) | ref | NA | 32 (71%) | ref | NA | ||||||
| At least some college | 130 (60%) | 2.5 (1.3–4.8) | .008 | 1.89 (0.9–3.9) | .09 | 175 (81%) | 0.8 (0.3–1.8) | .55 | 131 (60%) | 0.62 (0.3–1.3) | .18 | ||||
| Ever given birth | |||||||||||||||
| Yes | 65 (49%) | ref | ref | 112 (85%) | ref | NA | 84 (64%) | ref | NA | ||||||
| No | 82 (63%) | 1.7 (1.1–2.9) | .02 | 1.6 (0.95–2.78) | .07 | 101 (78%) | 0.6 (0.3–1.2) | .14 | 79 (61%) | 0.89 (0.5–1.5) | .63 | ||||
NA indicates not applicable; no predictors identified in univariate analyses.
Most women (213/262, 81%) reported that the examination is important to reassure them of their health. In univariate analyses, age 45 years or greater was the only significant predictor of holding this belief (OR 3.1, 95% CI 1.2–8.3). Most (163/262, 62%) participants felt that the examination helps establish open communication with their health care provider; in univariate analyses, age 45 years or greater (OR 2.0, 95% CI 1.1–3.7) and non-white race (OR 1.8, 95% CI 1.1–3.0) were predictors of responding ‘yes’.
In multivariate analyses, we found that age 45 years or greater independently predicted a higher likelihood of belief in knowing the examination’s purpose (OR 2.9, 95% CI 1.5–5.6), being reassured by the examination (OR 3.1, 95% CI 1.2–8.3) and a belief that it facilitates open communication (OR 2.1 95% CI 1.1–3.9). Our finding that non-white women were more likely than white women to say they believed the examination helps establish open communication with their providers remained significant (OR 1.9 95% CI 1.1–3.1).
Comment
About half of the women we interviewed did not know the purpose of the pelvic examination, yet most believed it to be of some value, especially in reassuring them of their health. Our observation that older women are more likely to hold favorable views about the examination suggests a generational effect reflecting long-held beliefs about its importance.
Our findings are of contemporary relevance. Over 60 million pelvic examinations were performed in the United States in 2010 (14). In a survey of 521 obstetrician-gynecologists throughout the United States, almost all reported that they would perform a bimanual examination on an asymptomatic patient at a routine visit, even in women who had previously had a hysterectomy due to fibroids and no previous dysplasia (15). About 80% of these clinicians believed the examination to be at least moderately important for adherence to standard medical practices. Over 90% believed that it was at least moderately important for reassuring women of their health; 81% of our enrollees had a similar belief, suggesting a concurrence of opinion from both patients and providers about the examination’s role in confirming normalcy.
In 2016, a systematic review commissioned by the U.S. Preventive Services Task Force (USPSTF) was published that found inadequate evidence concerning the benefits and harms of screening pelvic examinations. Potential harms include false positives leading to diagnostic workups that could include surgery (in 5% to 36% of the 1 to 8% of women with positive screening tests) (16). Their draft recommendation stated that evidence was insufficient to assess the balance of benefits and harms, thus they could not recommend for or against performing screening pelvic examinations.
Our finding that over half of women believed the examination helps establish open communication, as suggested by ACOG, should be interpreted with caution. Among the very limited number of justifications for the examination put forth by ACOG, the potential impact on open communication was important to define from the perspective of women. Thus, we chose to ask this question in a straightforward manner: “Do you think this examination helps establish open communication between you and your health care provider?” The finding that most women responded “yes” points to other potential benefits not captured in current systematic evidence reviews. That these beliefs are more prevalent among older women and non-white women suggests cultural factors that deserve further study. Alternatively, women may have responded “yes” for reasons of social desirability. The finding in the 2014 systematic review that pelvic examinations can cause pain, discomfort, anxiety is notable, though we did not ask about these aspects of the examination or other potential harms in our study. Certainly women value communication with their providers; a better understanding of other less invasive ways clinicians can foster open communication would be important.
While a major strength of our study is the enrollment of a relatively large socio-demographically diverse group of women, our participants were from a single geographical area of the United States and may not represent views of other women. We recruited women from women’s health clinics, enriching our sample with women who may have preconceived perceptions about routine examinations. Further, the questions about pelvic examinations were posed after discussions of cervical cancer screening; this temporality may have influenced participants’ responses, perhaps more favorably toward these examinations. Finally, the materials in our study showed a speculum examination but focused on the bimanual examination; inspection of external genitalia is also considered a part of a routine pelvic examination, but was not specifically mentioned. Nonetheless, we believe that our materials conveyed what most women identify as a pelvic examination.
Our study shows a lack of knowledge about the purpose of the routine pelvic examination among a substantial proportion of women recruited from two women’s clinics. With current guidelines for performing routine pelvic examinations in conflict, professional societies have a unique opportunity to clarify the precise reasoning for the examination. To achieve shared, informed decision making, clinicians will need to better communicate to their patients the examination’s purpose, including its potential benefits and harms.
Acknowledgments
This work was supported in part by a grant from the National Cancer Institute (NCI) (1R01CA169093). NCI had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
We thank study staff members Allison O’Leary, Rachel Freyre and Xochilt Borja, all employees of the University of California, San Francisco, for recruiting participants and conducting interviews. Finally, we are grateful to all of the women who participated.
Footnotes
The authors report no conflict of interest.
Presented at the 83rd annual meeting of the Pacific Coast Obstetrical and Gynecological Society September 28-October 2, 2016 in Sun Valley, Idaho
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American College of Obstetricians and Gynecologists. ACOG Practice Bulletin no. 109: Cervical cytology screening. Obstet Gynecol. 2009;114(6):1409–20. doi: 10.1097/AOG.0b013e3181c6f8a4. [DOI] [PubMed] [Google Scholar]
- 2.Moyer VA U S. Preventive Services Task Force. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;156:880–91. doi: 10.7326/0003-4819-156-12-201206190-00424. [DOI] [PubMed] [Google Scholar]
- 3.Johnson RE, Newhall WJ, Papp JR, Knapp JS, Black CM, Gift TL, et al. Screening tests to detect Chlamydia trachomatis and Neisseria gonorrhea infections-2002 MMWR Recomm. Rep. 2002;51(RR-15):1–38. [PubMed] [Google Scholar]
- 4.Stewart FH, Harper CC, Ellertson CE, Grimes DA, Sawaya GF, Trussell J. Clinical breast and pelvic examination requirements for hormonal Contraception: Current practice vs evidence. JAMA. 2001;285:2232–9. doi: 10.1001/jama.285.17.2232. [DOI] [PubMed] [Google Scholar]
- 5.Sawaya GF. Pelvic examinations in asymptomatic women: tipping a sacred cow. Arch Intern Med. 2011;171(22):2054–5. doi: 10.1001/archinternmed.2011.567. [DOI] [PubMed] [Google Scholar]
- 6.Westhoff CL, Jones HE, Guiahi M. Do new guidelines and technology make the routine pelvic exam obsolete? J Women’s Health. 2011;20:5–10. doi: 10.1089/jwh.2010.2349. [DOI] [PubMed] [Google Scholar]
- 7.Bloomfield HE, Olson A, Greer N, et al. Screening pelvic examinations in asymptomatic, average-risk adult women: an evidence report for a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2014;161(1):46–53. doi: 10.7326/M13-2881. [DOI] [PubMed] [Google Scholar]
- 8.Qaseem A, Humphrey LL, Harris R, et al. Screening pelvic examination in adult women: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2014;161(1):67–72. doi: 10.7326/M14-0701. [DOI] [PubMed] [Google Scholar]
- 9.Committee on Gynecologic Practice. Committee opinion no. 534: Well-Woman Visit. Obstet Gynecol. 2012;120:421–4. doi: 10.1097/AOG.0b013e3182680517. [DOI] [PubMed] [Google Scholar]
- 10."Healthy women do not need routine pelvic exams, influential physicians group says". [Accessed July 15, 2016];The Washington Post. 2014 Jun 30; https://www.washingtonpost.com/news/to-your-health/wp/2014/06/30/healthy-women-do-not-need-routine-pelvic-exams-influential-physicians-group-says/
- 11. [Accessed July 15, 2016];Do you really need that pelvic exam? https://www.washingtonpost.com/national/health-science/do-you-really-need-that-pelvic-exam/2015/10/12/8c79942e-3b7e-11e5-8e98-115a3cf7d7ae_story.html.
- 12.Conry JA, Brown H. Well-Woman Task Force: components of the well-woman visit. Obstet Gynecol. 2015;126(4):697–701. doi: 10.1097/AOG.0000000000001055. [DOI] [PubMed] [Google Scholar]
- 13.Henderson JT, Yu JM, Harper CC, Sawaya GF. U.S clinicians’ perspectives on less frequent routine gynecologic examinations. Prev Med. 2014;62C:49–53. doi: 10.1016/j.ypmed.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Ambulatory and Hospital Care Statistics Branch. National Ambulatory Medical Care Survey: 2010 Summary Tables. Atlanta, GA: Centers for Disease Control and Prevention; [Accessed July 15, 2016]. https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf. [Google Scholar]
- 15.Henderson JT, Harper CC, Gutin S, et al. Routine bimanual pelvic examinations: practices and beliefs of US obstetrician-gynecologists. Am J Obstet Gynecol. 2013;208(2):109e1–7. doi: 10.1016/j.ajog.2012.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guirguis-Blake JM, Henderson JT, Perdue LA, Whitlock EP. Preventive Services Task Force. Screening for Gynecologic Conditions With Pelvic Examination: A Systematic Review for the U.S. Jun, 2016. Evidence Synthesis No. 147. AHRQ Publication No. 15–05220-EF-1. [PubMed] [Google Scholar]