Abstract
Blacks are at greater risk for lower sleep quality and higher risk for obstructive sleep apnea (OSA) than other racial groups. In this study, we summarize the development of a tailored website including visuals, key messages, and video narratives, to promote awareness about sleep apnea among community-dwelling blacks. We utilized mixed methods, including in-depth interviews, usability-testing procedures, and brief surveys (n = 9, 55% female, 100% black, average age 38.5 years). Themes from the qualitative analysis illuminated varied knowledge regarding OSA symptoms and prevalent self-reported experience with sleep disturbance and OSA symptoms (e.g., snoring). On a scale from 1 (not at all) to 5 (very high), participants provided favorable ratings of website usefulness (mean = 4.9), user friendliness (mean = 4.9) and attractiveness (mean = 4.3). Our findings suggest although tailored health communication has potential for serving as a tool for advancing health equity, usability-testing of health materials is critical to ensure that culturally and linguistically tailored messages are acceptable and actionable in the intended population.
Introduction
Obstructive sleep apnea (OSA) is a sleep disorder characterized by breathing-related disruptions from sleep (Eckert & Malhotra, 2008). Individuals with OSA are at risk for adverse health outcomes, including elevated risk for cardiovascular disease (CVD) (Strollo & Rogers, 1996). Unfortunately, black/African-American individuals (hereafter referred to as blacks) are at higher risk for OSA than other racial/ethnic groups (Adenekan et al., 2013; Ertel, Berkman, & Buxton, 2011; Pandey et al., 2013).
Epidemiological estimates suggest OSA prevalence may be as high as 30% among adult males in the United States (Peppard, Young, Palta, & Skatrud, 2000). Yet very few individuals at risk for OSA have been diagnosed (Buysse et al., 2008). OSA is associated with fragmented sleep and excessive daytime sleepiness (Johns, 1993; Kribbs et al., 1993; Slanger et al., 2016). Particularly concerning, individuals with OSA have both elevated nocturnal sympathetic nervous system activation (Somers, Dyken, Clary, & Abboud, 1995) and early morning blood pressure (Marin et al., 2012; Nieto et al., 2000; Peppard et al., 2000). OSA has been found to have strong correlations to cardiometabolic risk factors (Eckert & Malhotra, 2008; Strollo & Rogers, 1996), and individuals with OSA are at high risk for stroke (Yaggi et al., 2005).
Treatment for OSA most commonly includes behavioral and lifestyle changes as well as use of positive airway pressure (PAP) therapy (Billings et al., 2011; McEvoy et al., 2016). Adherence to recommended PAP treatment is low among individuals diagnosed with OSA (Punjabi, 2008; Young, Peppard, & Gottlieb, 2002), but is particularly low among blacks (Ayanian, Cleary, Weissman, & Epstein, 1999; Wallace et al., 2017). Particularly concerning, compared to other racial/ethnic groups, there is higher prevalence of OSA risk factors among black individuals (e.g., overweight/obese and snoring, Adenekan et al., 2013; Ertel et al., 2011; Pandey et al., 2013). Low treatment adherence coupled with higher prevalence of OSA risk factors create a need to promote awareness about OSA among blacks (Marin et al., 2012; Nieto et al., 2000; Peppard et al., 2000).
Online platforms are promising tools for health, as Internet access has increased to over 88% of US adults (Pew Research Center, 2017). Online and web-based tools, with their rich affordances and capability to deliver personalized information, thus hold the potential to improve population health (Free et al., 2013). The work was conducted as part of a current NIH-funded study titled the Tailored Approach to Sleep Health Education (TASHE), the aim of which is to develop an online website to promote awareness about OSA among blacks (Williams et al. 2016).
Developing a website to promote awareness about OSA among community-based black individuals
The draft of the of the TASHE website
The draft website was designed with two key principles: (1) message tailoring and (2) video narratives. Tailored messages are data or information (e.g., graphics and text) designed specifically for the unique knowledge, beliefs, and cultural customs of particular audiences or populations (Klausen et al., 2012; Noar, Harrington, & Aldrich, 2009; Soetens, Vandelanotte, de Vries, & Mummery, 2014). Message tailoring has been found to be effective for increasing message comprehension and persuasion in efforts to address health disparities (Freimuth & Quinn, 2004; Resnicow, Baranowski, Ahluwalia, & Braithwaite, 1998). Thus, the website was designed to address the current knowledge and attitudes, as well as communication preferences, of the intended population.
In addition to message tailoring, the website featured video narratives that present messages in the form of a story (Green, 2006; Green & Brock, 2002). Narrative is persuasive because it is a format that is easy to comprehend and immersive, thereby increasing attention to the message and encouraging attitudes and beliefs that are aligned with a health intervention goal (e.g., to promote awareness about OSA, Murphy et al., 2015). The website also made use of video narratives filmed with individuals who are representative of the intended audience sharing their experience being diagnosed with OSA and using positive airways pressure (PAP) therapy.
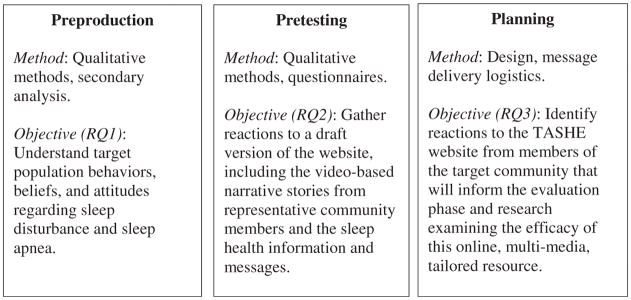
Usability testing of the website was conducted using the think aloud approach (Jääskeläinen, 2010; Mankoff et al., 2003), and procedures were guided by the three-step model offered by Atkin and Freimuth (2012) for health communication. Specifically, messages were identified using “pre-production” research to ascertain beliefs and attitudes among the intended audience (phase 1). Next, the messages and website were “pre-tested” (phase 2) to ensure appropriate cultural and linguistic tailoring, as well as general usability of the technology, in the current study. The insights obtained from the pre-production and pre-testing phases then inform the final stage “planning” stage of the intervention (phase 3, see Figure 1). In so doing, the current study sought to address three three research questions:
Figure 1.
Atkin and Freimuth (2012) three-step approach to health communication design and development.
Research Question 1: What beliefs and attitudes about OSA are common among community-dwelling blacks?
Research Question 2: What are reactions to the video narrative messages among community-dwelling blacks?
Research Question 3: How do community-dwelling blacks rate the usability of the website?
Methods
We recruited individuals who were representative of the intended user population using newspaper advertisements and posting flyers in the community. Mixed methods, including in-depth interviews and closed-ended surveys, were utilized to enhance the collection of feedback that will ensure optimization of the intervention prior to dissemination (Hawkins, Kreuter, Resnicow, Fishbein, & Dijkstra, 2008; Schmid, Rivers, Latimer, & Salovey, 2008). In addition, we utilized the think aloud usability testing protocol to collect feedback on the usability of the website (Bastien, Vallières, & Morin, 2001; Jääskeläinen, 2010; Kushniruk, Patel, & Cimino, 1997; Lundgrén-Laine & Salanterä, 2010; Mankoff et al., 2003). All participants signed a written informed consent form prior to participating in the study. The study was approved by the NYU School of Medicine Institutional Review Board.
Participants
Participants were recruited from community contexts (e.g., faith-based organizations, community centers) using posted paper flyers. Inclusion criteria for the study included self-identification as black or African-American. In addition, in order to be eligible to participate in the study, individuals needed to be at low to moderate risk for OSA (a response of 4 or greater according to a validated instrument, the Apnea Risk Evaluation System [ARES]; Westbrook et al., 2005).
Procedures
Once identified as eligible, participants were scheduled into interview slots with the informatics researcher (second author, Y.S.). Participants were first asked questions during an in-depth interview to assess their beliefs and attitudes toward OSA (RQ1). Next, individuals participated in the usability testing procedure, which involved assessing and viewing the TASHE draft website and providing reactions (RQ2) and providing feedback for the dissemination phase (RQ3). Participants were given refreshments during the interview procedure and received $50 for their participation.
In-depth interviews
The focus of the in-depth interviews was to assess sleep health and sleep apnea knowledge and beliefs, along with holistic, qualitative responses and feedback after accessing the TASHE website. Discussion followed an open-ended protocol (see Appendix). For example, to assess OSA knowledge and beliefs (RQ1), participants were asked “Tell me about your sleep generally, how good would you say your sleep is” and “Do you ever find yourself snoring, or waking up gasping for air?” Participants were asked specifically about their experience and knowledge of sleep apnea, “Do you know what sleep apnea is?” and “Have you or has anyone you know been diagnosed with sleep apnea?” Probes were used where necessary; such as “Tell me more, what are the symptoms of sleep apnea to the best of your knowledge.” Participants were also asked for feedback on how best to disseminate the intervention (RQ3).
Usability testing
The usability testing procedures in the current study followed the think aloud approach (Bastien et al., 2001; Jääskeläinen, 2010; Kushniruk et al., 1997; Lundgrén-Laine & Salanterä, 2010; Mankoff et al., 2003). The think aloud method is a procedure whereby individuals are asked to utilize the tool or intervention. While using the tool, participants are asked to verbally share their reactions and experience aloud with the interviewer (Hawkins et al., 2008; Jääskeläinen, 2010; Schmid et al., 2008). Participants are given a task to carry out in the system, and instructed to speak aloud as they navigate through the various website pages, read the content, and view the study videos, just mentioning anything that comes to mind, as it happens. Benefits of the think aloud method include capture of the user thoughts and actions in an unbiased manner as they happen. For instance, participants are instructed to vocalize their reactions as they use the website. It also tends to capture more details of the human-computer interaction than retrospective surveying, providing greater insight into usability flaws and the cognitive processes of the user (Jaspers, 2009; Jaspers, Steen, Bos, & Geenen, 2004).
Brief surveys
Following the think aloud usability testing, participants were asked to mark responses to closed-ended questions about the website. Participants marked answers on a scale from 1 (strongly disagree) to 5 (strongly agree) to questions about the website usefulness (“How useful was the website you just visited?”), usability (“How easy was the website you just visited to use”), and attractiveness (“How attractive, or nice to look at, was the…”). Finally, participants were asked to justify their responses and for their advice for the dissemination phase of the intervention.
Data analysis
Descriptive statistics were computed for all quantitative, closed-ended questionnaire responses. Qualitative data collected from the in-depth interviews and thinkaloud protocol were first transcribed (Charmaz, 2006). Next, data were analyzed using the constant comparative method to identify common themes within the specific question categories. Themes identified from participant responses were synthesized to identify prominent factors influencing perceptions on sleep health, sleep disorders, and reactions to the various intervention components. Themes identified in in-depth interviews regarding sleep health and sleep disorders as well as those identified in the pretesting phase are reported in the sections below. These were used to inform the final round of edits to the TASHE intervention before the main study was implemented.
Results
All participants were black. Nine adult men and women participated in the usability testing (N = 9). Of the study participants, 55% were female with an average age of 38.5 years and an ARES score of 4 or higher at the time of recruitment (participant mean ARES score = 4.8, s.d. = 0.7), which indicated they were at risk for OSA.
Beliefs and knowledge by OSA risk and symptoms
Table 1 displays the themes from interview responses regarding OSA beliefs and knowledge.
Table 1.
Results from the qualitative analysis of questions assessing participant knowledge and understanding of sleep, sleep apnea to assess research question 1 (n = 9).
| Theme | Supporting quotation |
|---|---|
| Varied OSA beliefs and knowledge |
|
| Personal experience with sleep disturbance |
|
| Friends and family experience sleep disturbance |
|
Knowledge about OSA ranged widely. Comments from participants demonstrate the had a wide range knowledge and beliefs. One participant demonstrated knowledge of OSA characteristics, “Yeah, or sometimes people just stop breathing, and then usually they wake up, but they might not remember that they woke up. It’s difficult. Your throat and everything gets—makes it difficult for you to breathe.” However, other participants raised questions in the interviews about OSA suggesting underlying uncertainty. For instance, as one participant asked, “When you—does that mean that—does it—do we have to be sleeping in a certain position for this to happen?”
Personal experience with sleep disturbance and sleep apnea
Another theme pertained to personal experience with sleep disturbance and OSA. Participants shared personal experiences such as one female participant describing her own snoring, “Oh, sometimes I snore. Not all the time, but he tell me—he be like, ‘You was snoring, girl. I tried to wake you up, and you was snoring your butt off.’” In addition, participants indicated sleep disturbance and OSA were common among friends and family. One participant shared a story about her sister who had severe daytime sleepiness that often impaired her driving, “That’s my sister. Cause she would be driving and stopping—I don’t know, she just go to sleep.” These quotes indicate personal experience with sleep disturbance, and also evidence that these difficulties are prevalent among close friends and family members. These quotes also, particularly in the case of sleepiness impairing safe driving, have the potential to be a significant public safety issue.
Reactions to video narratives
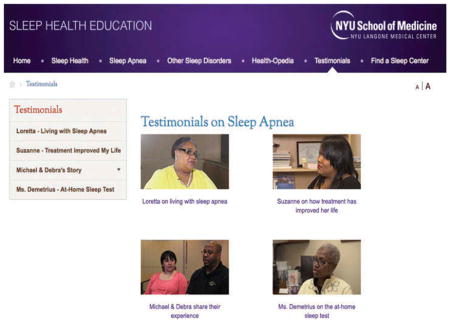
Table 2 provides a description of each video-based qualitative reactions provided to the videos after viewing. Video narrative messages were cast, filmed, and edited by a professional videographer hired for this study. There were a total of four video messages depicting black individuals sharing their personal experience with various issues relating to sleep and OSA, such as obtaining an overnight sleep recording, and using PAP treatment.
Table 2.
Overview of the four video vignettes in the online website testimonial section, and participant reactions to these four videos (n = 9).
| Message | Overview | Quotes |
|---|---|---|
| Michael and Debra | Sleep difficulty, and symptoms |
|
| Loretta | Living with sleep apnea |
|
| Suzanne | “How treatment changed my life” |
|
| Ms. Demetrius | At home sleep test option. |
|
Video 1: Michael and Debra
This video describes a story of a mixed race couple (the husband, Michael, is black and the wife, Debra, is Latina). Michael shares his experience with loud snoring. In the video the wife shares her frustration, and insists her husband receive treatment. Comments highlighted favorable aspects, including the role of the wife in prompting her husband to seek treatment, as one participant stated, “For what I’ve seen in black families, it’s always the woman [who motivates her husband to change.]” However, another individual indicated disliking the video, citing distaste that the couple was mixed race, and “yeah, the interracial couple is an issue.” The participant went on to explain this could be a barrier to the successful adoption of the advice in the video, as mixed race couples are often stigmatized in black culture.
Video 2: Loretta
This narrative features a black woman, Loretta, sharing her experience with severe snoring and daytime sleepiness, diagnosis and treatment of OSA. In this narrative, Loretta also shares her experience having an overnight sleep recording and the support she received from her family for seeking treatment. After viewing this video, one participant stated liking how the video captured the role of the grandmother in the black family, “Most black households are run by the grandmother, even if she doesn’t live there. Everything is what her general rule is. If she gets sick, we got a Big Momma thing. If Big Momma gets sick, everybody’s gonna lose it.” Another participant indicated the video provided an educational moment, “I didn’t know that when you falling asleep behind the wheel, green light, red light, whatever, it was a sign of apnea as well. That I didn’t know…. I learned something good today.”
Video 3: Suzanne
This video showcases Suzanne, a black woman, sharing her story of being diagnosed with OSA and her experience with treatment. In the video, you see Suzanne featured in a visit to her doctor. Suzanne shares her positive experience with sleep apnea treatment, and even her recent weight reduction after adhering to her doctor’s recommendations. One participant indicated liking the optimistic message about weight loss after PAP treatment, “She did lose weight, she said, ‘Well, let me try at least one thing I know I can do differently, which is add a little more activity to your life.’ I did find that fascinating with her.” Another participant indicated, in seeing the visual of the CPAP device, that it provided inspiration to take precautions to engage in healthy lifestyle practices to reduce OSA risk, “I really am willing to lose the weight because I don’t want to wear the mask.”
Video 4: Ms. Demetrius
In this video, Ms. Demetrius, a black woman, shares her OSA symptoms with her doctor and also comments on her fears about undergoing an overnight sleep recording. In the video, Ms. Demetrius and her physician share the possibilities of at home testing. One participant, who did not know about the at-home sleep test option for OSA, demonstrated her positive evaluation of the message, “You’re at home with it and they monitor everything? Wow. That’s good. That helps, your test…. That’s good you’re at home.’” Another participant comment indicated the message sparked interest in seeking an evaluation, “Seeing a sleep specialist.” See, that’s what I need to do. That’s what it’s getting me to do, like ASAP. No games.”
Usability testing
Table 3 outlines participant ratings of the online website, supporting quotations and guidance for dissemination. Participants provided high marks for usefulness of information (mean = 4.9/5.0) and indicated several reasons for their high marks, such as the educational nature of the website: “It’s very good. You give a lot of information. I really like it. I was learning a lot from it.” One participant indicated they were motivated to make healthier changes, such as seek treatment, after using the website: “I’m really motivated, yes, to do that. This was good. This is an eye opener for me. Yeah, yeah.” Another participant mentioned the videos were useful: “Definitely that and like I said, the videos make sure you have different types of people.”
Table 3.
Participant ratings and qualitative feedback on the website (n = 9).
| Category | Mean score* | Quotations |
|---|---|---|
| Useful information | 5.0 |
|
| User friendly | 4.9 |
|
| Attractive | 4.3 |
|
Ratings provided on scale from 1 (strongly disagree) to 5 (strongly agree).
Ratings for user friendliness of the TASHE website were high (mean = 4.9/5.0). Participants mentioned the website as easy to navigate: “I liked it. It was smooth. It was easy to operate. It was easy to navigate, cuz I look for that. Navigation is key.” Another participant said the information was digestible, not too much, “No, for real because there’s a lot websites that really need to—this in itself is like its own—There’s a lot of websites that I go on and I’m like, I don’t like this website, they’re doing too much, you know?”
Finally, ratings for attractiveness were moderate to high (mean = 4.3/5). Participants mentioned liking the display of content, as one male participant indicated: “It’s very easy to navigate. Everything is laid out really well. It’s not too overcrowded with too much information on one page. I like that.” Several individuals voiced discomfort about the over emphasis on blacks in the website, as one male indicated, “The only one thing I might probably say is why is it only in African-Americans? Why it is not—a lot of people have problems sleeping as well.” This was critical feedback for the production team in the final design stages, and sheds light on the fine line between tailoring and being too pointed in communicating to a particular demographic. These comments also illustrate the need for inclusiveness and generalization in message content and visuals. The production team emphasized diversity in their final design and production stages included more images of diverse individuals (as opposed to just black).
Discussion
Disparities in OSA risk represent a threat to population health (Ayanian et al., 1999; Duru et al., 2009). The current study describes the usability testing of an innovative website website designed to promote awareness about OSA among black individuals. The current study included a draft website designed to promote awareness about OSA among blacks that utilized message tailoring principles (Noar, Benac, & Harris, 2007) and video-based narrative storytelling approaches (Zebregs, van den Putte, Neijens, & de Graaf, 2014). Usability testing procedures described in the current study recruited representative participants from the intended audience to provide open-ended feedback regarding the draft website, and results were used to inform the subsequent website dissemination.
Utilizing in-depth interviews, the think aloud procedure, and brief surveys, we collected reactions to the draft TASHE intervention. The results illuminated several primary themes pertaining to sleep health and message-related reactions among black individuals, including prevalence of OSA symptoms in this population. Participant responses indicated personal experience with OSA, and prevalence of these issues among others in social circles such as friends and extended family members. Participants demonstrated moderate knowledge of OSA, such as snoring and/or paused breathing, as primary symptoms. The results also indicate that questions about symptoms and risk for OSA persist in this population, such as whether there is a connection between body mass or sleeping position as contributing factors to OSA risk.
Participants indicated that they endorsed the video-based narrative stories. Participants liked the video describing the process for OSA treatment and hearing stories about personal experience with snoring and family member support for seeking treatment. Participants also liked learning the connection between weight and sleep apnea that was explained in the video stories.
Overall ratings of the website were favorable and described the website as useful, attractive, and user-friendly. According to the think aloud protocol procedure, participants also provided qualitative assessments to support these positions. The high user ratings for the website on the dimensions of usefulness, attractiveness, and user-friendliness (e.g., 4.9/5.0) also highlights the fact that the extensive formative preparation done by the development team helped ensure the tested product was mostly very good.
Interestingly, several quotes suggest some participants were uncomfortable with the overwhelming focus on black individuals in the website messages and visuals. This finding suggests that too much tailoring of images and visuals to minority communities may jeopardize message persuasive outcomes.
The themes and results of the think aloud testing procedure in the current study results informed final website edits and changes, such as making photos and resources hyperlinked to improve navigation through the website. Overall this study found positive reactions toward the TASHE website from members of the intended audience, which informed final edits on the intervention website prior to dissemination. In addition, the reactions suggest tailoring and narrative tutorials are promising strategies for designing online health communication to address health disparities.
Limitations and strengths
Several limitations and strengths are notable. First, the small sample size and sole focus on blacks may limit generalizability. Second, the study was restricted to reactions to test messages developed as a result of an artistic team (web designers, graphic designers) and stakeholder engagement to to understand the cultural considerations and belief factors characteristic of the population. Despite those limitations, use of the think aloud procedure to elicit open-ended feedback enabled us to tailor messages in the final stages of the intervention design. This factor constitutes a major strength of this work.
Conclusion
Health communication strategies, including message tailoring and narrative storytelling, hold promise for informing community-based research efforts that seek to address health disparities. Although this is not the first study to examine message tailoring for minority populations, this is the first study to our knowledge to create tailored resources designed specifically to address OSA-related health disparity. Our results highlight the varied knowledge about OSA among blacks and offer preliminary evidence for the feasibility of an online, tailored intervention for improving awareness about OSA in this population. Participant reactions, however, also identified important areas to address prior to dissemination (e.g., revised text and language in response to participant comments and feedback). These findings reinforce the importance of tailoring when designing health communication to ensure that messages are relevant to the intended user population and is both culturally and linguistically appropriate.
Acknowledgments
Funding
This work was supported by funding from the NHLBI [grant number R25HL116378, K23HL125939, and K07AG052685].
Appendix 1
Screenshot from the video narrative page of the TASHE website.
Appendix 2. Thinkaloud in-depth interview protocol
-
Background
-
Tell me about how you use computers in your everyday life
How easily accessible are computers in your life?
-
Tell me about how you use the Internet
What do you use the Internet for?
What types of information are you interested in on the web?
Is this different based on device?
Have you used internet to get health advice? If so, how?
-
Tell me about your sleep
Tell me about your sleep generally, how good would you say your sleep is?
Tell me about sleep apnea, do you know what it is?
Do you know anyone who has sleep apnea?
What are the symptoms of sleep apnea?
Do you ever find yourself snoring, or waking up gasping for air?
-
-
Thinkaloud protocol (interviewer provides description), then participant is given a sheet of paper with a task described, and shown the site
-
Participant is shown a 2-minute video clip of a person doing a thinkaloud protocol and asked to thinkaloud, even if it feels weird at first
Recording starts (with permission)
-
-
Participant carries out the task
Interviewer guides the participant only when a task or area has been attempted and the participant requires help in order to move forward.
Interviewer guides the participant to areas not yet explored.
-
Participant is shown three short, 3-minute videos about sleep apnea, sleep apnea diagnosis, and sleep apnea treatment, asked by the interviewer:
What did you think about the videos?
What are some of the things you liked about the videos?
What are some of the things you did NOT like about the videos?
-
Participant is asked to rate the website along the following dimensions
-
On a scale from 1 (strongly disagree) to 5 (strongly agree) would you agree o disagree to the following statements:
The website is useful.
The website is user friendly.
The website is attractive.
-
Is there anything else you might suggest we do to improve the website?
Debrief and ask for further questions.
Participant is asked if he/she might want to assist with further exercises or site development, is given incentive, and leaves.
Footnotes
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/hhth.
References
- Adenekan B, Pandey A, McKenzie S, Zizi F, Casimir GJ, Jean-Louis G. Sleep in America: Role of racial/ethnic differences. Sleep Medicine Reviews. 2013;17:255–262. doi: 10.1016/j.smrv.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkin CK, Freimuth V. In Public communication campaigns. 2. Newbury Park, CA: Sage; 2012. Formative evaluation research in campaign design; pp. 125–146. [Google Scholar]
- Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. New England Journal of Medicine. 1999;341:1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Billings ME, Auckley D, Benca R, Foldvary-Schaefer N, Iber C, Redline S, … Kapur VK. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34:1653–1658. doi: 10.5665/sleep.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Hall ML, Strollo PJ, Kamarck TW, Owens J, Lee L, … Matthews KA. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. Journal of Clinical Sleep Medicine. 2008;4:563–571. [PMC free article] [PubMed] [Google Scholar]
- Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. London, UK: Sage Publications Ltd; 2006. [Google Scholar]
- Duru OK, Gerzoff RB, Selby JV, Brown AF, Ackermann RT, Karter AJ, … Mangione CM, et al. Identifying risk factors for racial disparities in diabetes outcomes: The Translating Research into Action for Diabetes (TRIAD) study. Medical Care. 2009;47:700–706. doi: 10.1097/mlr.0b013e318192609d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckert DJ, Malhotra A. Pathophysiology of adult obstructive sleep apnea. Proceedings of the American Thoracic Society. 2008;5:144–153. doi: 10.1513/pats.200707-114MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertel KA, Berkman LF, Buxton OM. Socioeconomic status, occupational characteristics, and sleep duration in African/Caribbean Immigrants and US white health care workers. Sleep. 2011;34:509–518. doi: 10.1093/sleep/34.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, … Haines A. The effectiveness of mobile-health technologies to improve health care service delivery processes: A systematic review and meta-analysis. PLoS Med. 2013;10:e1001363. doi: 10.1371/journal.pmed.1001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freimuth VS, Quinn SC. The contributions of health communication to eliminating health disparities. American Journal of Public Health. 2004;94:2053–2055. doi: 10.2105/ajph.94.12.2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M. Narratives and cancer communication. Journal of Communication. 2006;56:S163–S183. [Google Scholar]
- Green M, Brock T. In the mind’s eye: Transportation-imagery model of narrative persuasion. In: Green M, Strange JJ, Brock TC, editors. Narrative impact: Social and cognitive foundations. Mahwah, NJ: Lawrence Erlbaum Associates; 2002. pp. 315–341. [Google Scholar]
- Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Education Research. 2008;23:454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jääskeläinen R. Think-aloud protocol. Handbook of Translation Studies. 2010;1:371–374. [Google Scholar]
- Jaspers MWM. A comparison of usability methods for testing interactive health technologies: Methodological aspects and empirical evidence. International Journal of Medical Informatics. 2009;78:340–353. doi: 10.1016/j.ijmedinf.2008.10.002. [DOI] [PubMed] [Google Scholar]
- Jaspers MWM, Steen T, Bos C, Geenen M. The think aloud method: A guide to user interface design. International Journal of Medical Informatics. 2004;73:781–795. doi: 10.1016/j.ijmedinf.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Johns MW. Daytime sleepiness, snoring, and obstructive sleep apnea: The Epworth Sleepiness Scale. Chest. 1993;103:30–36. doi: 10.1378/chest.103.1.30. [DOI] [PubMed] [Google Scholar]
- Klausen SH, Mikkelsen UR, Hirth A, Wetterslev J, Kjærgaard H, Søndergaard L, Andersen LL. Design and rationale for the PREVAIL study: Effect of e-Health individually tailored encouragements to physical exercise on aerobic fitness among adolescents with congenital heart disease–A randomized clinical trial. American Heart Journal. 2012;163:549–556. doi: 10.1016/j.ahj.2012.01.021. [DOI] [PubMed] [Google Scholar]
- Kribbs NB, Pack AI, Kline LR, Getsy JE, Schuett JS, Henry JN, … Dinges DF. Effects of one night without nasal CPAP treatment on sleep and sleepiness in patients with obstructive sleep apnea. American Review of Respiratory Disease. 1993;147:1162–1168. doi: 10.1164/ajrccm/147.5.1162. [DOI] [PubMed] [Google Scholar]
- Kushniruk AW, Patel VL, Cimino JJ. Usability testing in medical informatics: Cognitive approaches to evaluation of information systems and user interfaces. Proceedings of the AMIA Annual Fall Symposium; 1997. pp. 218–222. [PMC free article] [PubMed] [Google Scholar]
- Lundgrén-Laine H, Salanterä S. Think-aloud technique and protocol analysis in clinical decision-making research. Qualitative Health Research. 2010;20:565–575. doi: 10.1177/1049732309354278. [DOI] [PubMed] [Google Scholar]
- Mankoff J, Dey AK, Hsieh G, Kientz J, Lederer S, Ames M. Heuristic evaluation of ambient displays. Proceedings of the SIGCHI conference on Human factors in computing systems; NY, USA: ACM; 2003. pp. 169–176. Retrieved from http://dl.acm.org/citation.cfm?id=642642. [Google Scholar]
- Marin JM, Agusti A, Villar I, Forner M, Nieto D, Carrizo SJ, … Jelic S. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307:2169–2176. doi: 10.1001/jama.2012.3418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X, … Anderson CS. CPAP for prevention of cardiovascular events in obstructive sleep apnea. New England Journal of Medicine. 2016;375:919–931. doi: 10.1056/NEJMoa1606599. [DOI] [PubMed] [Google Scholar]
- Murphy ST, Frank LB, Chatterjee JS, Moran MB, Zhao N, Amezola De Herrera P, Baezconde-Garbanati LA. Comparing the relative efficacy of narrative vs nonnarrative health messages in reducing health disparities using a randomized trial. American Journal of Public Health. 2015;105:2117–2123. doi: 10.2105/AJPH.2014.302332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. JAMA. 2000;283:1829–1836. doi: 10.1001/jama.283.14.1829. [DOI] [PubMed] [Google Scholar]
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin. 2007;133:673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Noar SM, Harrington NG, Aldrich RS. The role of message tailoring in the development of persuasive health communication messages. Communication Yearbook. 2009;33:73–133. [Google Scholar]
- Pandey A, Williams N, Donat M, Ceide M, Brimah P, Ogedegbe G, … Jean-Louis G. Linking sleep to hypertension: Greater risk for blacks. International Journal of Hypertension. 2013;2013 doi: 10.1155/2013/436502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. New England Journal of Medicine. 2000;342:1378–1384. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. Internet/broadband fact sheet. 2017 Jan 12; Retrieved September 6, 2017, from http://www.pewinternet.org/fact-sheet/internet-broadband/
- Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proceedings of the American Thoracic Society. 2008;5:136–143. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: Defined and demystified. Ethnicity & Disease. 1998;9:10–21. [PubMed] [Google Scholar]
- Schmid KL, Rivers SE, Latimer AE, Salovey P. Targeting or tailoring? Maximizing resources to create effective health communications. Marketing Health Services. 2008;28:32–37. [PMC free article] [PubMed] [Google Scholar]
- Slanger TE, Gross JV, Pinger A, Morfeld P, Bellinger M, Duhme A-L, … Erren TC. Person-directed, non-pharmacological interventions for sleepiness at work and sleep disturbances caused by shift work. Cochrane Database of Systematic Reviews. 2016:CD010641. doi: 10.1002/14651858.CD010641.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soetens KCM, Vandelanotte C, De Vries H, Mummery KW. Using online computer tailoring to promote physical activity: A randomized trial of text, video, and combined intervention delivery modes. Journal of Health Communication. 2014;19:1377–1392. doi: 10.1080/10810730.2014.894597. [DOI] [PubMed] [Google Scholar]
- Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. The Journal of Clinical Investigation. 1995;96:1897–1904. doi: 10.1172/JCI118235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strollo PJJ, Rogers RM. Obstructive sleep apnea. New England Journal of Medicine. 1996;334:99–104. doi: 10.1056/NEJM199601113340207. [DOI] [PubMed] [Google Scholar]
- Wallace DM, Williams NJ, Sawyer AM, Jean-Louis G, Aloia MS, Vieira DL, Wohlgemuth WK. Adherence to positive airway pressure treatment among minority populations in the US: A scoping review. Sleep Medicine Reviews. 2017;17:30010–30012. doi: 10.1016/j.smrv.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westbrook PR, Levendowski DJ, Cvetinovic M, Zavora T, Velimirovic V, Henninger D, Nicholson D. Description and validation of the apnea risk evaluation system: A novel method to diagnose sleep apnea-hypopnea in the home. CHEST Journal. 2005;128:2166–2175. doi: 10.1378/chest.128.4.2166. [DOI] [PubMed] [Google Scholar]
- Williams NJ, Robbins R, Rapoport D, Allegrante JP, Cohall A, Ogedgebe G, Jean-Louis G. Tailored approach to sleep health education (TASHE): study protocol for a web-based randomized controlled trial. Trials. 2016;17:585. doi: 10.1186/s13063-016-1701-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. New England Journal of Medicine. 2005;353:2034–2041. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea. American Journal of Respiratory and Critical Care Medicine. 2002;165:1217–1239. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- Zebregs S, Van Den Putte B, Neijens P, De Graaf A. The differential impact of statistical and narrative evidence on beliefs, attitude, and intention: A meta-analysis. Health Communication. 2014;30:282–289. doi: 10.1080/10410236.2013.842528. [DOI] [PubMed] [Google Scholar]