Abstract
Background
Corticosteroid (CS) injections have been proven to be effective in ameliorating symptoms of plantar fasciitis. Shock-wave (SW) therapy is another common treatment of plantar fasciitis, and several meta-analyses have documented its advantages when compared to placebo treatment. Despite this, few studies have focused on comparing the use of CS and SW in the treatment of plantar fasciitis. The purpose of this meta-analysis is to assess whether SW is superior to CS in managing plantar fasciitis, both in terms of ameliorating pain as well as improving functionality.
Methods
A systematic search of the literature was conducted to identify relevant articles that were published in Pubmed, Medline, Embase, the Cochrane Library, SpringerLink, Clinical Trials.gov and OVID from the databases’ inception to July 2018. All studies comparing the efficacy of SW and CS in terms of pain levels and functionality improvement were included. Data on the two primary outcomes were collected and analyzed using the Review Manager 5.3.
Results
Six studies were included in the current meta-analysis. A significant difference in VAS score (MD = − 0.96, Cl − 1.28 to − 0.63, P < 0.00001, I2 = 96%) was noted between the SW group and the CS group. No significant difference was seen in the Mayo CSS or FFI or HFI or 100 Scoring System score at the 3 months follow-up (Chi2 = 0.62, I2 = 0%, P > 0.05).
Conclusions
The clinical relevance of the present study is that both SW and CS were effective and successful in relieving pain and improving self-reported function in the treatment of plantar fasciitis at 3 months. Although inter-group differences were not significant, the VAS score was better improved in the SW group, highlighting that shock-wave therapy may be a better alternative for the management of chronic plantar fasciitis.
Keywords: Plantar fasciitis, Shock-wave, Corticosteroid, Intra-articular
Introduction
Plantar fasciitis is a major cause of heel pain, which is often seen in middle aged and elderly people and is responsible for a reduction in quality of life [1]. Treatment modalities that have been used in plantar fasciitis include orthoses [2, 3], stretching [4, 5], taping [6], extracorporeal shock-wave therapy [7, 8], laser therapy [9], percutaneous injection [10] and drug medication [11]. Corticosteroid (CS) injections have been proven to be effective in achieving beneficial effects for this disorder [12, 13], but there exist limitations. Studies [14, 15] have reported different durations of pain relief due to use of different injection sites, as well as side effects such as heel pad atrophy and rupture of the plantar fascia [15]. Shock-wave (SW) therapy is another common treatment of plantar fasciitis, and several meta-analyses have documented its advantages over placebo treatment [16, 17]. However, the therapeutic response to SW therapy depends on the intensity, pulse cycle and SW modality [16]. Although both methods are useful for plantar fasciitis, few studies have focused on comparing the use of CS and SW in the treatment of the condition and which treatment is superior, if either, is still uncertain. The purpose of this meta-analysis is to assess whether SW is superior in managing plantar fasciitis, both in terms of ameliorating pain as well as improving functionality.
Materials and methods
Search strategy
The databases searched were Pubmed, Medline, Embase, the Cochrane Library, SpringerLink, Clinical Trials.gov and OVID from inception to May 2018. The following search terms were used: plantar fasciitis or PF; Shock-wave or SW; Corticosteroid or CS; intra-articular injection or IA injection.
Data selection
Inclusion eligibility was independently performed by two investigators who screened the title and abstracts of all articles. Disagreements were resolved with discussion between the authors. A third researcher was the adjudicator when the two investigators did not reach agreement. The inclusion criteria were: (1) studies were designed as RCTs; (2) participants were at least 18 years old; (3) studies compared SW with CS; (4) articles were written in the English language.
Data extraction
Two authors independently extracted the following data from each eligible study: study design, type of study population, age, number of participants and interventions. Any discrepancies in data extraction were resolved by a third investigator.
Quality and risk of bias assessments
The modified Jadad scale was used to assess the methodological quality of each study. A score of ≥ 4 indicated high quality. The Cochrane Handbook for Reviews of Interventions (Revman Version 5.3) was used to assess the risk of bias. Two independent authors subjectively reviewed all articles and assigned a value of “high”, “low” or “unclear” based on the following items: selection bias; performance bias; detection bias; attrition bias; reporting bias and other bias. Any disagreements were resolved with discussion to reach a consensus. If a consensus could not be reached a third investigator was consulted.
Statistical analysis
RevMan software was used to analyze the numerical data extracted from the included studies. For binary data, the risk ratios (RR) and 95% confidence intervals (CI) were assessed (ɑ = 0.05 for the inspection standards). For continuous data, means and standard deviations (SD) were pooled to a weighted mean difference (WMD) and a 95% confidence internal (CI) in the meta-analysis. Heterogeneity was tested using the I2 statistic. Studies with an I2 statistic of 25–50% were considered to have low heterogeneity, those with an I2 statistic of 50–75% were considered to have moderate heterogeneity and those with an I2 statistic > 75% were considered to have high heterogeneity. When the I2 statistic was > 50%, sensitivity analyses were performed to identify any potential sources of heterogeneity. Statistical significance was indicated by a p value < 0.05. And the analysis was done using fixed effects which adds more statistical power to the analysis.
Results
Description of studies and demographic characteristics
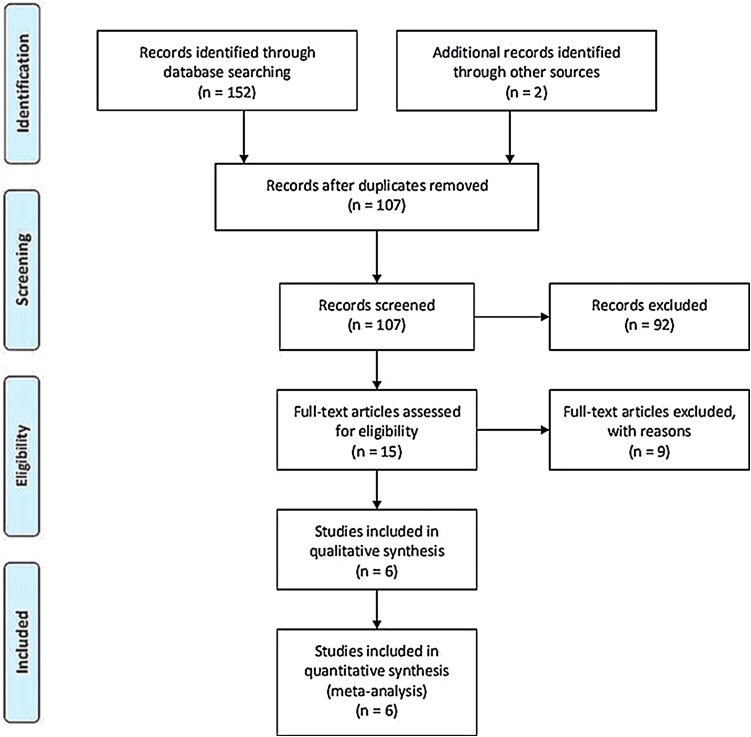
A total of 154 articles were identified as potentially relevant studies (Fig. 1). Following screening of titles and abstracts (n = 92) and removal of duplicates (n = 47) resulted in a total of 15 full publications. The 15 full manuscripts were assessed and a further 9 trials were excluded, leaving 6 trials eligible to be included in the meta-analysis. The demographic characteristics are summarized in Tables 1 and 2. All trials compared the effect of the SW group versus the CS group.
Fig. 1.
Flow chart outlining the process of study identification, inclusion and exclusion
Table 1.
Characteristics of included studies
| Study | Year | Country | Patients (n) | Age (Y) | Average disease duration, month (week) | PF thickness (mm) | Study design | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SW | CS | SW | CS | SW | CS | SW | CS | ||||
| Lai | 2018 | Taiwan, China | 47 | 50 | 54.53 ± 8.62 | 54.58 ± 8.63 | 7.94 ± 2.92 | 8.06 ± 2.87 | 0.37 ± 0.07 | 0.38 ± 0.06 | RCT |
| Sehriban | 2017 | Turkey | 36 | 36 | 50.22 ± 8.29 | 47.86 ± 7.90 | 8 | 9 | 4.75 | 4.7 | RCT |
| Mark | 2005 | Australia | 61 | 64 | 38.6 | 39.9 | 12.7 | 14.6 | NC | NC | RCT |
| Nayera | 2012 | Egypt | 30 | 30 | 34.27 ± 7.19 | 34.23 ± 6.67 | NC | NC | 5.94 ± 0.54 | 5.96 ± 0.46 | RCT |
| Istemi | 2010 | Turkey | 27 | 33 | 42.9 ± 7.08 | 44.7 ± 9.20 | 37.7 ± 8.6 | 39.4 ± 10.2 | NC | NC | RCT |
| Fariba | 2016 | Iran | 20 | 20 | 41.45 ± 8.05 | 42.85 ± 8.62 | 8.5 ± 4.53 | 10.4 ± 5.53 | NC | NC | RCT |
Table 2.
Characteristics of the six trials selected showing general information
| Study | Year | Treatment cycle | Treatment schedule | Assessment methods | Adverse event | Follow-up, month | |
|---|---|---|---|---|---|---|---|
| SW | CS | ||||||
| Lai | 2018 | 2 | The stable energy level 6 (0.29 mJ/mm2) was kept for 25 min to achieve total 1500 shock | 20 mg triamcinolone acetonite with 2 ml 2% xylocaine were injected into the marker | PFT, VAS, 100-point scoring | NC | 3 |
| Sehriban | 2017 | 3 | A 15-mm head with 2000 shockwave at each session at 10-Hz frequency with an energy flux density per shock of 0.16 mJ/mm2 | Single 1-mL dose of betamethasone sodium plus 0.5 mL of prilocaine | VAS, PFT, HTI, FFI | NC | 6 |
| Mark | 2005 | 3 | 3 applications of 1000 pulses of an energy flux density of 0.08/mm2 | One milliliter betamethasone (5.7 mg) and 2 mL of lignocaine 1% were injected |
VAS, TT scoring | NC | 12 |
| Nayera | 2012 | 2 | Energy intensity applied ranged from 14 to 17 kV, 2 Hz, 1000–1500 pulses, same technique is repeated after two weeks | Injection of 2 mL of 4 mg/mL twice (betamethasone diproprionate and betamethasone sodium phosphate, 0.5% zylocaine hydrochloride) | Mayo CSS PFT |
NC | 6 |
| Istemi | 2010 | 1 | A single application of 3,000 shockwaves Using an electrohydraulic shockwave generator |
A 2-mL syringe filled with 0.5 mL of combined betamethasone dipropionate (6.43 mg/mL) andbetamethasone sodium phosphate (2.63 mg/mL) |
VAS, HTI | Pain (n = 4), no infection |
3 |
| Fariba E | 2016 | 5 | 2000 shockwaves/session of 0.2 mJ/mm2, all subjects received 5 sessions of ESWT at 3-day intervals | Injection of 5 ml once a week, 3 times in total | VAS, FFI | NC | 2 |
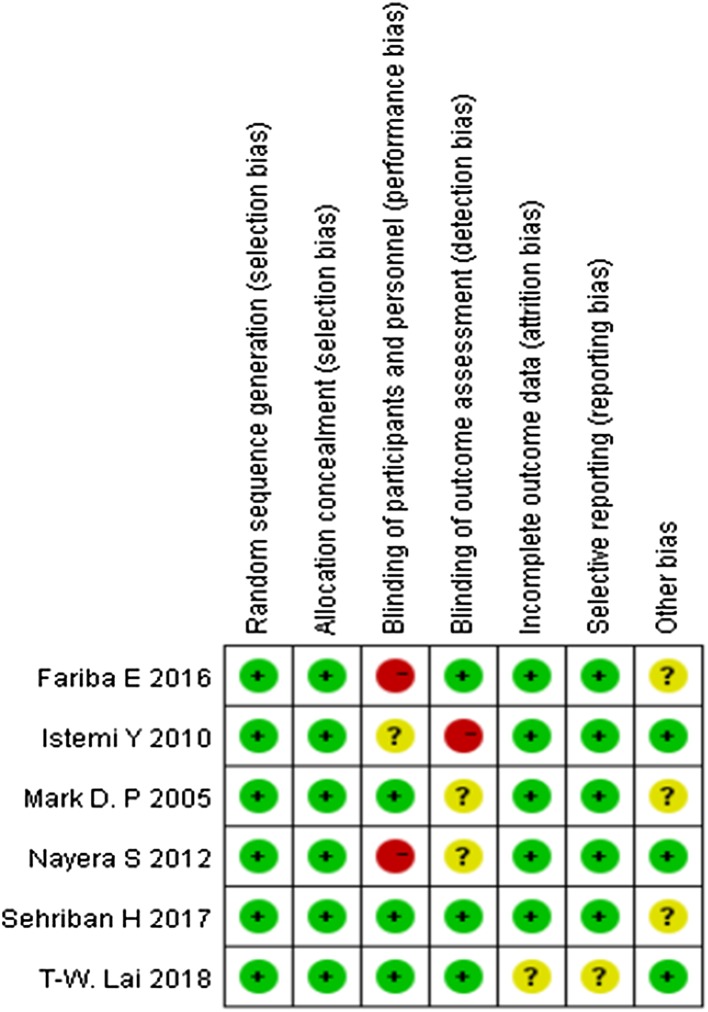
Risk of bias in included studies
Assessment of the risk of bias is presented in Fig. 2. All trials included were randomized trial designs [18–23]. Three trials [20–22] did not describe the methods of allocation concealment. Blinding of participants and personnel (performance bias) was unclear and incomplete outcome data (attrition bias) was high risk in one trial [20]. One trial [18] had patients lost to follow-up.
Fig. 2.
Risk of bias summary
Shock-wave versus corticosteroid
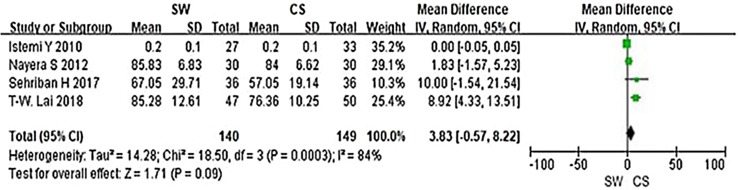
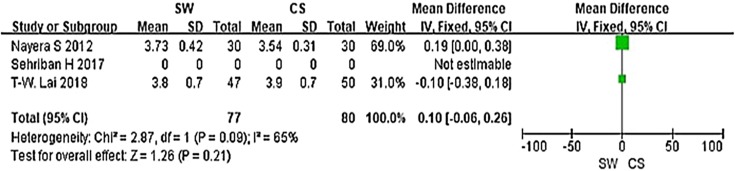
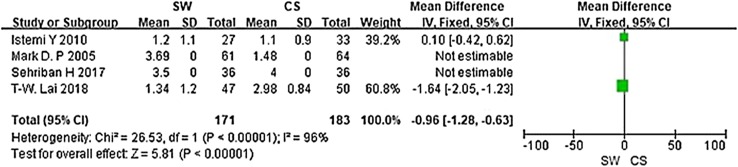
From the six studies comparing SW with CS, four used the Mayo CSS, FFI, HFI and 100 Scoring System score (both including pain and functional subscales) 3 months after accepting treatment. SW was not found to be superior to CS when calculating the pooled effect size of Mayo CSS, FFI, HFI, and 100 Scoring System score from the follow-up at 3 months (Fig. 3; SMD = 3.83, P = 0.09, I2 = 84%). A sensitivity analysis failed to determine any one or two trials that might be causing the statistical heterogeneity. Further analysis of the different changes 3 months after accepting treatment in PFT was performed and is shown in Fig. 4 (MD = 0.10, P = 0.21, I2 = 65%). No significant heterogeneity was observed in this analysis. In addition, trial outcomes assessed by the VAS score were also analyzed, and the result is displayed in Fig. 5 (MD = − 0.96, P < 0.00001, I2 = 96%). A significant difference in VAS score was noted between the SW group and the CS group.
Fig. 3.
Forest plot of Mayo CSS, FFI, HFI and 100 Scoring System score in the SW group compared with the CS group from the 3-month follow-up
Fig. 4.
Forest plot of PFT in the SW group compared with the CS group from the 3-month follow-up
Fig. 5.
Forest plot of VAS score in the SW group compared with the CS group from the 3-month follow-up
Discussion
Shock-wave therapy has been used in the treatment of calcified tendonitis of the rotator cuff, nonunion of bone, chronic tennis elbow, and painful heel syndrome [24–27]. The efficacy of SW was controversial in previous studies. The success rates range from 40 to 80% [28–31], and the results are affected by symptom duration [32]. In this meta-analysis, which synthesizes the efficacy of SW on the basis of comparison with CS, SW displayed similar efficacy to CS in improving self-reported function and better effect on relieving pain in the treatment of plantar fasciitis at 3 months.
To our knowledge, this is the first meta-analysis looking at randomized controlled trails comparing the efficacy of SW and CS, and prior to this analysis the outcome of CS and SW as primary treatments of plantar fasciitis remained elusive. In 2012, Saber et al. [21] performed a randomized controlled trial, which showed SW was as useful as CS for relieving symptoms of plantar fasciitis. However, Porter et al. [23] revealed that corticosteroid injection was more efficacious and cost-effective than SW in the treatment of plantar fasciopathy. In our meta-analysis, we found no significant difference in Mayo CSS, FFI, HFI or 100 Scoring System score. A moderately better outcome was, however, seen in the SW group in terms of symptom and pain control in these scoring systems. This difference was not, however, statistically significant (p > 0.05). In addition, a significant difference in VAS score was noted between the SW group and the CS group (MD = − 0.96, P < 0.00001, I2 = 96%), which encouraged us to believe that SW is more effective in relieving pain for the treatment of plantar fasciitis.
Previous studies had investigated the relationship of PFT and clinical symptoms. Thickening of the plantar fascia insertion more than 4 mm is considered abnormal and more than 5 mm is suggestive of plantar fasciopathy [33, 34]. As such, it can be inferred that PFT can be treated as an observational index for the comparative research. In our meta-analysis, we observed the different changes in PFT after accepting 3 months treatment and we found no significant difference between the two groups.
Many researchers [35–37] had pointed out that SW was effective in short- and mid-term follow-up in terms of relieving pain and improving functionality, but its efficacy in long-term should be established, especially for the recurrence of plantar fasciitis. Malliaropoulos [36] et al. conducted a retrospective study concerning recurrence rate of plantar fasciitis in 2016, which showed that three key factors for recurrence: female sex, pretreatment pain duration, and the number of SW sessions received. Wang Ching-Jen et al. [37] observed long-term (12 months) results of 79 patients (85 heels) received 1500 impulses of shockwaves at 16 kV to the affected heel in a single session, and the recurrence rate was relative low (11%, 9/81 heels), they also regarded that recalcitrant plantar fasciitis could be caused by plantar fascia thickening and loss of normal tissue elasticity. Therefore if a patient presents with advanced symptoms then they may be less receptive to conservative management. CS as another treatment for plantar fasciitis had some advantages to be recommended, but a Cochrane review concluded that whilst valuable in the short term, the effects of injection therapy are not maintained beyond 6 months [38]. Furthermore, Jolanta et al. [39] had compared the efficacy between ultrasound and shock-wave therapy among 47 patients of plantar fasciitis, which showed that the shock-wave therapy would be a better option for pain relief, as with fewer treatments, the cost of therapy is lower. And the researchers suggested that a complex prophylaxis programme needed be implemented, patients should be encouraged to fight with obesity, and the key to combine theory with practice is to teach patients responsibility and integrate the therapy with everyday life. Thus, we can regard that SW combined with health education would be a better choice for patients compared with ultrasound wave therapy.
Just like other meta-analyses, our study is not devoid of limitations. First, in the SW group, the outcomes may be highly dependent on machine-type (electrohydraulic, electromagnetic, and piezoelectric systems) and treatment protocols [25, 30, 40]. The energy levels are categorized into high (> 0.60 mJ/mm2), medium (0.28–0.59 mJ/mm2), and low (0.08–0.27 mJ/mm2) [41]. In the CS group, outcome may be influenced by the injection dosage, timing, and interval. However, in this meta-analysis, the machine type and energy levels of SW, as well as the injection dosage, timing, and interval were nonuniform among the different trials. Second, the current meta-analysis focuses only on papers published in the English language. Inclusion of studies reported in other languages may influence heterogeneity and affect the current results. In addition, the variance of populations, disease duration, and outcome scores contributed to a high level of heterogeneity and diverse clinical outcomes. In this study, we focus on the shock-wave therapy and corticosteroids therapy for the treatment of Plantar Fasciitis. So we did not look at an untreated control group. All these inconsistencies complicated data synthesis and increased the risk of incorrect results. Furthermore, the follow-up time was not consistent across studies. Further rigorously designed RCTs with larger sample sizes are necessary to better confirm the efficacy of SW.
Conclusion
The clinical relevance of the present study is that both SW and CS were effective and successful in relieving pain and improving self-reported function in the treatment of plantar fasciitis at 3 months post treatment. Although inter-group differences were not significant, the VAS score showed higher improvement in the SW group, thus shock-wave therapy appears to be a better alternative for the management of chronic plantar fasciitis. Further studies are needed to compare the efficacy of SW and CS on long-term follow-up patients.
Acknowledgements
This work was accomplished with the help of the library of Huazhong University of Science and Technology.
Abbreviations
- PFT
Plantar fascia thickness
- VAS
Visual Analogue Scale
- HTI
Heel tenderness index
- TT
Tenderness threshold
- FFI
Foot function index
- CSS
Clinical scoring system
- RCT
Randomized controlled trial
- NC
Not clear
Author contributions
YX and QW participated in the design of the study; YL and QW carried out data curation; JL and HX performed the statistical analysis; JL and QW carried out investigation; BM and JL carried out project administration; YL and WZ operated software; YL carried out supervision; LH and QW carried out validation; YX and BM conceived the study, and participated in its design and coordination and helped to draft the manuscript; GL. YX and AP participated in the sequence alignment and drafted the manuscript. All authors read and approved the final manuscript.
Funding
No external funding was received for the initiation or completion of this study.
Conflict of interest
All the authors responsible for this work declare no conflict of interest.
Availability of data and materials
Please contact author for data requests.
Contributor Information
Yuan Xiong, Email: xiongyuanmed@163.com.
Qipeng Wu, Email: 364258104@qq.com.
Bobin Mi, Email: mi19882@163.com.
Wu Zhou, Email: 494260189@qq.com.
Yi Liu, Email: liuyizsy@qq.com.
Jing Liu, Email: 907732140@qq.com.
Hang Xue, Email: 15871393021@163.com.
Liangcong Hu, Email: huliangcongtj@hust.edu.cn.
Adriana C. Panayi, Email: apanayi@bwh.harvard.edu
Guohui Liu, Email: liuguohui@medmail.com.cn.
References
- 1.Genc H, Saracoglu M, Nacir B, et al. Long-term ultrasonographic follow-up of plantar fasciitis patients treated with steroid injection. Joint Bone Spine. 2005;72(1):61–65. doi: 10.1016/j.jbspin.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Gross MT, Byers JM, Krafft JL, et al. The impact of custom semirigid foot orthotics on pain and disability for individuals with plantar fasciitis. J Orthop Sports Phys Ther. 2002;32(4):149–157. doi: 10.2519/jospt.2002.32.4.149. [DOI] [PubMed] [Google Scholar]
- 3.Lynch DM, Goforth WP, Martin JE, et al. Conservative treatment of plantar fasciitis. A prospective study. J Am Podiatr Med Assoc. 1998;88(8):375–380. doi: 10.7547/87507315-88-8-375. [DOI] [PubMed] [Google Scholar]
- 4.Powell M, Post WR, Keener J, et al. Effective treatment of chronic plantar fasciitis with dorsiflexion night splints: a crossover prospective randomized outcome study. Foot Ankle Int. 1998;19(1):10–18. doi: 10.1177/107110079801900103. [DOI] [PubMed] [Google Scholar]
- 5.DiGiovanni BF, Nawoczenski DA, Lintal ME, et al. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A(7):1270–1277. doi: 10.2106/00004623-200307000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Landorf KB, Radford JA, Keenan AM, et al. Effectiveness of low-Dye taping for the short-term management of plantar fasciitis. J Am Podiatr Med Assoc. 2005;95(6):525–530. doi: 10.7547/0950525. [DOI] [PubMed] [Google Scholar]
- 7.Böddeker R, Schäfer H, Haake M. Extracorporeal shockwave therapy (ESWT) in the treatment of plantar fasciitis—a biometrical review. Clin Rheumatol. 2001;20(5):324–330. doi: 10.1007/PL00011207. [DOI] [PubMed] [Google Scholar]
- 8.Buchbinder R, Ptasznik R, Gordon J, et al. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. JAMA. 2002;288(11):1364–1372. doi: 10.1001/jama.288.11.1364. [DOI] [PubMed] [Google Scholar]
- 9.Basford JR, Malanga GA, Krause DA, et al. A randomized controlled evaluation of low-intensity laser therapy: plantar fasciitis. Arch Phys Med Rehabil. 1998;79(3):249–254. doi: 10.1016/S0003-9993(98)90002-8. [DOI] [PubMed] [Google Scholar]
- 10.Kamel M, Kotob H. High frequency ultrasonographic findings in plantar fasciitis and assessment of local steroid injection. J Rheumatol. 2000;27(9):2139–2141. [PubMed] [Google Scholar]
- 11.Probe RA, Baca M, Adams R, Preece C. Night splint treatment for plantar fasciitis. A prospective randomized study. Clin Orthop Relat Res. 1999;368:190–195. doi: 10.1097/00003086-199911000-00023. [DOI] [PubMed] [Google Scholar]
- 12.Ball EMA, McKeeman HMA, Patterson C, et al. Steroid injection for inferior heel pain: a randomised controlled trial. Ann Rheum Dis. 2013;72(6):996–1002. doi: 10.1136/annrheumdis-2012-201508. [DOI] [PubMed] [Google Scholar]
- 13.Li Z, Xia C, Yu A, et al. Ultrasound- versus palpation-guided injection of corticosteroid for plantar fasciitis: a meta-analysis. PLoS One. 2014;9(3):e92671. doi: 10.1371/journal.pone.0092671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brinks A, Koes BW, Volkers ACW, et al. Adverse effects of extra-articular corticosteroid injections: a systematic review. BMC Musculoskelet Disord. 2010;11:206. doi: 10.1186/1471-2474-11-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee HS, Choi YR, Kim SW, et al. Risk factors affecting chronic rupture of the plantar fascia. Foot Ankle Int. 2014;35(3):258–263. doi: 10.1177/1071100713514564. [DOI] [PubMed] [Google Scholar]
- 16.Chang KV, Chen SY, Chen WS, et al. Comparative effectiveness of focused shock wave therapy of different intensity levels and radial shock wave therapy for treating plantar fasciitis: a systematic review and network meta-analysis. Arch Phys Med Rehabil. 2012;93(7):1259–1268. doi: 10.1016/j.apmr.2012.02.023. [DOI] [PubMed] [Google Scholar]
- 17.Yin MC, Ye J, Yao M, et al. Is extracorporeal shock wave therapy clinical efficacy for relief of chronic, recalcitrant plantar fasciitis? A systematic review and meta-analysis of randomized placebo or active-treatment controlled trials. Arch Phys Med Rehabil. 2014;95(8):1585–1593. doi: 10.1016/j.apmr.2014.01.033. [DOI] [PubMed] [Google Scholar]
- 18.Lai TW, Ma HL, Lee MS, et al. Ultrasonography and clinical outcome comparison of extracorporeal shock wave therapy and corticosteroid injections for chronic plantar fasciitis: a randomized controlled trial. J Musculoskelet Neuronal Interact. 2018;18(1):47–54. [PMC free article] [PubMed] [Google Scholar]
- 19.Hocaoglu S, Vurdem UE, Cebicci MA, et al. Comparative effectiveness of radial extracorporeal shockwave therapy and ultrasound-guided local corticosteroid injection treatment for plantar fasciitis. J Am Podiatr Med Assoc. 2017;107(3):192–199. doi: 10.7547/14-114. [DOI] [PubMed] [Google Scholar]
- 20.Eslamian F, Shakouri SK, Jahanjoo F, et al. Extra corporeal shock wave therapy versus local corticosteroid injection in the treatment of chronic plantar fasciitis, a single blinded randomized clinical trial. Pain Med. 2016;17(9):1722–1731. doi: 10.1093/pm/pnw113. [DOI] [PubMed] [Google Scholar]
- 21.Sabera N. Ultrasound guided local steroid injection versus extracorporeal shockwave therapy in the treatment of plantar fasciitis. Alex J Med. 2012;48:8. [Google Scholar]
- 22.Yucel I, Ozturan KE, Demiraran Y, et al. Comparison of high-dose extracorporeal shockwave therapy and intralesional corticosteroid injection in the treatment of plantar fasciitis. J Am Podiatr Med Assoc. 2010;100(2):105–110. doi: 10.7547/1000105. [DOI] [PubMed] [Google Scholar]
- 23.Porter MD, Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport Med. 2005;15(3):119–124. doi: 10.1097/01.jsm.0000164039.91787.dc. [DOI] [PubMed] [Google Scholar]
- 24.Hammer DS, Adam F, Kreutz A, et al. Extracorporeal shock wave therapy (ESWT) in patients with chronic proximal plantar fasciitis: a 2-year follow-up. Foot Ankle Int. 2003;24(11):823–828. doi: 10.1177/107110070302401103. [DOI] [PubMed] [Google Scholar]
- 25.Speed CA, Richards C, Nichols D, et al. Extracorporeal shock-wave therapy for tendonitis of the rotator cuff. A double-blind, randomised, controlled trial. J Bone Joint Surg Br. 2002;84(4):509–512. doi: 10.1302/0301-620X.84B4.12318. [DOI] [PubMed] [Google Scholar]
- 26.Durst HB, Blatter G, Kuster MS. Osteonecrosis of the humeral head after extracorporeal shock-wave lithotripsy. J Bone Joint Surg Br. 2002;84(5):744–746. doi: 10.1302/0301-620X.84B5.12282. [DOI] [PubMed] [Google Scholar]
- 27.Maier M, Milz S, Tischer T, et al. Influence of extracorporeal shock-wave application on normal bone in an animal model in vivo. Scintigraphy, MRI and histopathology. J Bone Joint Surg Br. 2002;84(4):592–599. doi: 10.1302/0301-620X.84B4.11621. [DOI] [PubMed] [Google Scholar]
- 28.Rompe JD, Kirkpatrick CJ, Küllmer K, et al. Doserelated effects of shock waves on rabbit tendo Achillis. A sonographic and histological study. J Bone Joint Surg Br. 1998;80(3):546–552. doi: 10.1302/0301-620X.80B3.8434. [DOI] [PubMed] [Google Scholar]
- 29.Haake M, Buch M, Schoellner C, et al. Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial. BMJ. 2003;327(7406):75. doi: 10.1136/bmj.327.7406.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ogden J, Alvarez RG. Plantar fasciopathy and orthotripsy: the effect of prior cortisone injection. Foot Ankle Int. 2005;26(3):231–233. doi: 10.1177/107110070502600308. [DOI] [PubMed] [Google Scholar]
- 31.Costa M, Donell S. Low-energy extracorporeal shock-wave treatment (ESWT) for tendinitis of the supraspinatus. J Bone Joint Surg Br. 2002;84(4):619–620. doi: 10.1302/0301-620X.84B4.0840619b. [DOI] [PubMed] [Google Scholar]
- 32.Riddle DL, Pulisic M, Sparrow K. Impact of demographic and impairment-related variables on disability associated with plantar fasciitis. Foot Ankle Int. 2004;25(5):311–317. doi: 10.1177/107110070402500506. [DOI] [PubMed] [Google Scholar]
- 33.Hammer DS, Adam F, Kreutz A, Rupp S, Kohn D, Seil R. Ultrasonographic evaluation at 6-month follow-up of plantar fasciitis after extracorporeal shock wave therapy. Arch Orthop Trauma Surg. 2005;125(1):6–9. doi: 10.1007/s00402-003-0591-z. [DOI] [PubMed] [Google Scholar]
- 34.Karabay N, Toros T, Hurel C. Ultrasonographic evaluation in plantar fasciitis. J Foot Ankle Surg. 2007;46(6):442–446. doi: 10.1053/j.jfas.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 35.Akşahin E, Doğruyol D, Yüksel HY, et al. The comparison of the effect of corticosteroids and platelet-rich plasma (PRP) for the treatment of plantar fasciitis. Arch Orthop Trauma Surg. 2012;132(6):781–785. doi: 10.1007/s00402-012-1488-5. [DOI] [PubMed] [Google Scholar]
- 36.Malliaropoulos N, Crate G, Meke M, et al. Success and recurrence rate after radial extracorporeal shock wave therapy for plantar fasciopathy: a retrospective study. Biomed Res Int. 2016;2016:9415827. doi: 10.1155/2016/9415827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang CJ, Wang FS, Yang KD, et al. Long-term results of extracorporeal shockwave treatment for plantar fasciitis. Am J Sports Med. 2006;34(4):592–596. doi: 10.1177/0363546505281811. [DOI] [PubMed] [Google Scholar]
- 38.Crawford F, Thomson C. Interventions for treating plantar heel pain. Cochrane Database Syst Rev. 2003 doi: 10.1002/14651858.CD000416. [DOI] [PubMed] [Google Scholar]
- 39.Krukowska J, Wrona J, Sienkiewicz M, et al. A comparative analysis of analgesic efficacy of ultrasound and shock wave therapy in the treatment of patients with inflammation of the attachment of the plantar fascia in the course of calcaneal spurs. Arch Orthop Trauma Surg. 2016;136:1289–1296. doi: 10.1007/s00402-016-2503-z. [DOI] [PubMed] [Google Scholar]
- 40.Speed CA, Nichols D, Wies J, et al. Extracorporeal shock wave therapy for plantar fasciitis. A double blind randomised controlled trial. J Orthop Res. 2003;21(5):937–940. doi: 10.1016/S0736-0266(03)00048-2. [DOI] [PubMed] [Google Scholar]
- 41.Speed CA. Extracorporeal shock-wave therapy in the management of chronic soft-tissue conditions. J Bone Joint Sur Br 200486(2):165–171 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Please contact author for data requests.