Abstract
Objective -
To investigate women’s preferred approach to prenatal genetic testing decision making and assess concordance between preference and experience.
Methods –
We conducted a secondary analysis of data from two randomized trials conducted between 2007–2012. Survey items assessed participants’ preferred approach to decision making and whether they experienced a preference-concordant decision process. Logistic regression estimated relationships between patient characteristics and these outcomes.
Results –
56% of women preferred autonomous decision making, 39% preferred shared decision making, and 5% preferred a provider-driven approach. Only 57% experienced preference-concordant decision making. On bivariate analysis, black women, Spanish-speaking Latinas and women with less education were less likely to experience this outcome, than white, more educated women. Numeracy and preferring a provider-driven approach fully mediated observed disparities in preference-concordant decision making for most participants, except for Spanish-speaking Latinas, who were still less likely to have experienced this outcome after accounting for these factors.
Conclusion –
Numeracy, preference for provider-driven decision processes, and language barriers were key drivers of disparities in preference-concordant decision making.
Practice Implications -
Given the values-sensitive and quantitative nature of prenatal testing decisions, nuanced counseling and interventions to address language barriers, numeracy gaps, and decision-making preferences are needed to tailor counseling to patient’s backgrounds and desires.
Keywords: Shared decision making, patient participation, preferences, patient-centered communication, prenatal genetic testing decision making, concordance, disparities
1. Introduction
Shared decision making has been advocated as an ideal approach to clinical encounters in which multiple, reasonable courses of action are available and the ‘best’ choice depends, in part, on patient values and preferences [1–3]. However, numerous studies have demonstrated that patients differ in their preferences for participation in a variety of clinical decisions [4,5]. Investigations into the extent to which there is concordance between patients’ preferred approach to decision making and what actually occurs in the clinical encounter are limited [6,7].
In prenatal testing specifically, the American College of Obstetricians and Gynecologists has endorsed using a shared decision-making approach to decisions about screening and diagnostic testing [8,9]. Little is known, however, about whether women’s own preferences for decision making in this context align with the shared decision-making model, as compared to a completely autonomous or a provider-driven process, and whether they experience decision making that is concordant with this preference.
Given documented racial/ethnic and socioeconomic disparities in the understanding of prenatal testing options [10], it is necessary to investigate the decision-making experience of women from diverse sociodemographic backgrounds, including women with limited English proficiency and varying literacy and numeracy levels. In particular, health numeracy, a component of health literacy, has emerged as an important factor to consider in medical decision making, especially as it relates to the understanding of risk [11,12]. Health numeracy is “the degree to which individuals have the capacity to assess, process, interpret, communicate, and act on numerical, quantitative, graphical, biostatistical, and probabilistic health information needed to make effective health decisions [13],” and notably is distinct from education [14,15].” A growing body of work has linked numeracy to understanding the benefits of screening mammography [16], to the care of pregnant women with diabetes [17], and to preferring a more active role in decision making around cancer [18], however, there is limited data on its role in the decision-making process for prenatal genetic testing.
We sought to 1) describe women’s preferred approach to decision making, 2) explore the extent to which they experienced preference-concordant decision making, and 3) analyze associations between their sociodemographic characteristics and both their preferred approach to decision-making and whether they experienced preference-concordant decision making.
2. Methods
2.1. Data source
We conducted a secondary analysis of data from two randomized studies (Clinicaltrials.gov NCT00505596) conducted between 2007 and 2012. The studies examined the effect of a decision support tool and elimination of financial barriers to testing on prenatal test use (both diagnostic test use and testing strategy undergone) and decision making (including decision conflict and regret) among women of varying literacy and numeracy levels. Results of the first study were not published, as changes in prenatal testing guidelines and practices made the original tool obsolete; the second study was published in 2014 [19]. Because the eligibility criteria, measures and assessment schedule were common to both trials and the difference in guidelines did not impact this research question, we included data from both in the secondary analysis presented in this manuscript. In brief, inclusion criteria for the two trials included being English- or Spanish-speaking, being no more than 20 weeks gestation, and having not yet undergone any prenatal genetic screening and/or diagnostic testing in the current pregnancy. Participants from several clinical sites in the San Francisco Bay area were enrolled from 2007 – 2009 (Trial 1) and 2010–2012 (Trial 2). Institutional review board approval was obtained from all recruitment sites. Bilingual research associates interviewed participants during their enrollment visit (baseline), and again at 24–36 weeks gestation (follow-up), after the timeframe for prenatal testing had closed. The baseline interview included items related to sociodemographic characteristics, reproductive history, literacy, and numeracy. The follow-up interview included questions about preferences regarding their own and their provider’s role in the decision-making process for prenatal genetic testing, and the extent to which they and their providers were involved in that process. Interview items were the same for both trials. This secondary analysis focused on the effects of patient sociodemographic variables on prenatal testing decision preferences and processes, not on potential effects of intervention groups. Thus, data were pooled across the intervention and control groups for analyses.
2.2. Measures
2.2.1. Women’s preferred approach to decision making
The first of two outcomes focused on women’s preferred approach to decision making, which was assessed using a single question: “In deciding about prenatal testing options for your pregnancy, who do you think should decide which test(s), if any, you should have?” Response options included: 1) “Me or me and my family, alone,” 2) “Mostly me or me and my family,” 3) “Healthcare providers and me or me and my family equally,” 4) “Mostly my healthcare providers,” and 5) “My healthcare providers alone.” Based on their responses, the participants were classified into one of three preferred approach categories: Women who chose answers 1 or 2 were classified as preferring autonomous decision making; women who chose answer 3 were classified as preferring shared decision making, and women who chose answers 4 or 5 were classified as preferring provider-driven decision making.
2.2.2. Experience with preference-concordant decision making
The second outcome for this analysis was whether participants had experienced preference-concordant decision making. For this outcome, we used responses to two questions and compared them to the participants’ expressed preferred approach to decision making, outlined above. The two questions were “How involved were you in making decisions regarding prenatal testing for birth defects?” and “How involved were your healthcare providers in making decisions regarding prenatal testing for birth defects?” For both questions, the response categories were “Not at all”; “A little”; and “A lot.” Participants were then categorized as having experienced a preference-concordant decision process if their preferred approach to decision making corresponded both to their reported involvement and provider involvement (Table 1). All other combinations of decision-making preferences with patient and provider involvement responses were coded as preference discordant. If any of the three components (decision-making preference, patient involvement, provider involvement) were missing we coded the preference-concordance outcome as missing.
Table 1:
Combinations of Patient and Provider Involvement in Prenatal Testing Decisions Classified as Preference Concordant
| Patient-Reported Preferred Decision-Making Approach | |||
|---|---|---|---|
| Autonomous | Shared | Provider-Driven | |
| Patient Involvement | A lot | A lot | A little/Not at all |
| Provider Involvement | A little/Not at all | A lot | A lot |
2.2.3. Explanatory variables
Our primary variables for these analyses were selected a priori based on a theoretical understanding of the relationships between components of the decision process, reflecting the range of factors that may influence women’s decision making for prenatal genetic testing [12,20]. These consisted of sociodemographic characteristics, including a combined race, ethnicity, and language variable (with language defined by whether the woman opted to complete the interview in English or Spanish), educational attainment, parity; as well as literacy, numeracy, site of prenatal care (categorized as safety net site if it served primarily low income women versus non-safety net clinical site if it served all women), and an item about the impact of social networks on decision making. Literacy was measured using the Rapid Estimate of Adult Literacy in Medicine-Revised scale (REALM-R)[21]. Women who scored six or lower on the 8-point REALM-R scale were considered to have poor literacy. Numeracy was measured using an adapted, 5-item version of the validated Lipkus Expanded Numeracy Scale [14]. The numeracy scale was validated among a highly educated sample, and demonstrated that even at higher levels of education, individuals may still have difficulty with simple numeracy questions. Women with two or fewer correct responses on the numeracy scale were categorized as having low numeracy. To include consideration of whether social influences might underlie decision-making preferences, we asked participants whether someone other than their healthcare provider had expressed an opinion regarding their decision: “Were there any people in your life, other than your healthcare providers, who expressed an opinion regarding whether you should or should not have prenatal testing for birth defects?” Response options were “yes” or “no.” All multivariate models reported here included this set of covariates. Preliminary models also included the intervention group indicator and the trial indicator (Trial 1 and Trial 2) as covariates, but because their effects were non-significant, they were dropped from final models.
2.3. Analysis
We first calculated descriptive statistics for the entire sample and then compared the characteristics of women in each decision-making preference category (autonomous, shared, and provider-driven), using Pearson’s chi-squared tests. Bivariate and multivariate logistic regression models were fit to each of the two outcomes: the three-category, multinomial, decision-making preference outcome (autonomous, shared, and provider-driven) with ‘autonomous’ as the outcome reference category, and the binary outcome, preference-concordant decision making. In addition to the primary variables outlined above, the multivariate model for the binary preference-concordant decision making outcome also included women’s preferred approach to decision making as a covariate.
Finally, we conducted mediation analysis based on our preliminary results and an understanding of the potential mediating role of numeracy in the decision-making process, as outlined in the theoretical framework for prenatal genetic testing decision making proposed by Smith et al [12]. In the Smith et al framework they illustrate how various mediating factors, including numeracy, can influence how socioeconomic characteristics impact a women’s ability to experience an informed decision-making process. We first investigated whether the effects of patient characteristic variables (race/ethnicity/language, education, and literacy) on preference for a provider-driven decision process (versus autonomous) were mediated by low numeracy. In turn, we investigated whether the effect of numeracy on preference-concordant decision making was mediated by preferring a provider-driven decision. We used the joint significance test to establish the significance of mediated pathways. I.e., if each individual segment of a mediated pathway was significant (p<.05), then the entire mediated pathway was determined to be significant [22]. The same set of covariates described above was included in these models. All analyses were conducted with STATA version 14.1.
3. Results
3.1. Preferred approach to decision making by patient characteristics
For the first analysis, we used data from 902 participants (319 from Trial 1 and 583 from Trial 2) who had completed the decision-making preference question during their follow-up interview. Together, these women constituted a racially and ethnically diverse group representing a broad range of socioeconomic levels and varying literacy and numeracy skills (Table 2).
Table 2.
Characteristics of Study Participants by Preferred Approach to Prenatal Testing Decision Making
| Preferred Approach to Prenatal Testing Decision Making | |||||
|---|---|---|---|---|---|
| Characteristic | Total n=902, (%) | Autonomous n=510, (%) | Shared n=351, (%) | Provider-Driven n=41, (%) | P |
| Maternal Age (y) | .006 | ||||
| <35 | 644 (71.4) | 343 (67.3) | 268 (76.4) | 33 (80.5) | |
| ≥ 35 y | 258 (28.6) | 167 (32.8) | 83 (23.7) | 8 (19.5) | |
| Race, ethnicity and language | < .001 | ||||
| Latina (Spanish speaking) | 213 (23.6) | 121 (23.7) | 78 (22.2) | 14 (34.1) | |
| Latina (English speaking) | 79 (8.8) | 40 (7.8) | 35 (10.0) | 4 (9.8) | |
| Black | 146 (16.2) | 69 (13.5) | 65 (18.5) | 12 (29.3) | |
| Asian | 70 (7.8) | 32 (6.3) | 36 (10.3) | 2 (4.9) | |
| Othera | 75 (8.3) | 40 (7.8) | 30 (8.5) | 5 (12.2) | |
| White | 319 (35.4) | 208 (40.8) | 107 (30.5) | 4 (9.8) | |
| Married or living with partnerb | 694 (77.0) | 419 (82.2) | 254 (72.6) | 21 (51.2) | < .001 |
| Educational attainmentc | < .001 | ||||
| Some high school or less | 182 (20.2) | 92 (18.1) | 72 (20.5) | 18 (43.9) | |
| High school graduate | 136 (15.1) | 67 (13.2) | 57 (16.2) | 12 (29.3) | |
| Some college | 169 (18.8) | 88 (17.3) | 75 (21.4) | 6 (14.6) | |
| College graduate or more | 415 (45.9) | 262 (51.5) | 147 (41.9) | 5 (12.2) | |
| Poor literacyd | 193 (21.4) | 97 (19.0) | 76 (21.7) | 20 (48.8) | < .001 |
| Low numeracye | 311 (34.6) | 158 (31.0) | 123 (35.2) | 30 (73.2) | < .001 |
| Annual household income, $f | < .001 | ||||
| ≤ 25,000 | 303 (37.4) | 151 (32.5) | 126 (40.5) | 26 (74.3) | |
| 25,001–50,000 | 112 (13.8) | 60 (12.9) | 47 (15.1) | 5 (14.3) | |
| 50,001–100,000 | 144 (17.8) | 89 (19.1) | 53 (17.0) | 2 (5.7) | |
| >100,000 | 252 (31.1) | 165 (35.5) | 85 (27.3) | 2 (5.7) | |
| Prenatal care received at a safety net clinical site | 382 (42.3) | 193 (37.8) | 158 (45.0) | 31 (75.6) | < .001 |
| Prior birth | 470 (52.1) | 259 (50.8) | 182 (51.9) | 29 (70.7) | .048 |
| Someone other than provider expressed opinion regarding prenatal testing | 474 (52.8) | 284 (56.1) | 178 (50.7) | 12 (30.0) | .004 |
includes Native American (6), Filipina (31), Mixed (37), cannot choose (1)
missing, n=1;
missing, n=1;
missing, n=1;
missing, n=3;
missing, n=91;
These women varied in their preferred approach to prenatal testing decision making: 56% preferred autonomy, 39% desired a shared decision process, and 5% felt the provider should drive the decision (Table 2). We observed significant differences in the sociodemographic characteristics of women in each of these categories. For example, women aged 35 or older, White women, and women who were college graduates were disproportionally represented in the group preferring an autonomous decision. On the other hand, Spanish-speaking Latinas and Black women, women who had lower educational attainment, and women who had low numeracy scores were overrepresented in the group preferring a provider-driven decision.
Race/ethnicity/language, education, and type of clinical site all were significantly associated with preferring shared decision-making versus an autonomous decision process in bivariate analyses (Table 3). However, in multivariate analysis, only race/ethnicity/language persisted as being significantly associated with shared decision making; compared to White women, Asian women were significantly more likely to prefer shared decision making [adjusted odds ratio (aOR) 2.1, 95% confidence interval (CI) 1.2–3.6, P=.008]. In the bivariate models, all variables were significantly related to a preference for a provider-driven decision versus an autonomous decision-making process; however, only numeracy retained a significant effect in the multivariate analysis. Specifically, women who were less numerate were significantly more likely to report preferring a provider-driven rather than an autonomous decision (aOR 2.6, 95% CI 1.1 – 6.1, P=.032).
Table 3.
Patient Characteristics Associated with Preferred Decision-Making Approach (n=893)
| Shared compared to Autonomous | Provider-Driven compared to Autonomous | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | OR (CI 95%) | P | aORa (CI 95%) | P | OR (CI 95%) | P | aORa (CI 95%) | P |
| Race, ethnicity and language | ||||||||
| Spanish-speaking Latina | 1.3 (.9–1.8) | .229 | .72 (.41–1.3) | .27 | 6.0 (1.9–18.7) | .002 | .61 (.13–2.8) | .523 |
| English-speaking Latina | 1.7 (1.0–2.8) | .041 | 1.4 (.79 −2.4) | .27 | 5.2 (1.3–21.7) | .024 | 1.4 (.27–7.1) | .689 |
| Black | 1.8 (1.2–2.8) | .004 | 1.3 (.78– 2.2) | .30 | 9.0 (2.8–29.0) | <. 001 | 1.5 (.35– 6.5) | .576 |
| Asian | 2.2 (1.3–3.7) | .004 | 2.1 (1.2–3.6) | .008 | 3.3 (.57–18.5) | .184 | 1.3 (.19– 8.2) | .81 |
| Otherb | 1.5(.9–2.5) | .161 | 1.2 (.69–2.1) | .50 | 6.5 (1.7–25.3) | .007 | 1.8 (.37–8.7) | .471 |
| White | Reference | Reference | Reference | Reference | ||||
| Educational attainment | ||||||||
| Some high school or less | 1.4 (.96–2.0) | .077 | 1.7 (.9–3.1) | .10 | 10.3 (3.7–28.4) | <. 001 | 2.6 (.54–12.4) | .235 |
| High school graduate | 1.5 (1.0–2.3) | .045 | 1.4 (.8–2.6) | .21 | 9.4 (3.2–27.6) | <. 001 | 2.4 (.54–10.8) | .25 |
| Some college | 1.5 (1.1–2.2) | .026 | 1.5 (.9–2.3) | .11 | 3.6 (1.1–12.0) | .039 | 1.4 (.34–6.1) | .627 |
| College graduate or more | Reference | Reference | Reference | Reference | ||||
| Poor literacy | 1.2 (.8–1.7) | .333 | .81 (.55–1.2) | .31 | 4.1 (2.1–7.8) | < .001 | 1.4 (.66–3.1) | .371 |
| Low numeracy | 1.2 (.9– 1.6) | .198 | 1.0 (.71–1.5) | .90 | 6.1 (3.0–12.4) | < .001 | 2.6 (1.1– 6.1) | .032 |
| Prior birth | 1.0 (.8–1.6) | .758 | .96 (.71–1.3) | .78 | 2.3 (1.2– 4.7) | .016 | 1.6 (.73–3.5) | .238 |
| Someone other than provider expressed opinion regarding decision for prenatal testing | .80 (.61– 1.1) | .118 | .95 (.71–1.3) | .76 | .34 (.17– .67) | .002 | .70 (.33–1.5) | .362 |
| Prenatal care received at a safety net clinical site | 1.3 (1.0–1.8) | .036 | 1.3 (.82– 1.9) | .291 | 5.1 (2.4–10.6) | < .001 | 2.0 (.77– 5.2) | .154 |
OR, odds ratio; aOR, adjusted odds ratio; CI, confidence interval
multivariate model adjusted for variables included in table and selected a priori
includes includes Native American (6), Filipina (31), Mixed (37), cannot choose (1)
Bold type indicates statistical significance at P ≤ .05
3.2. Experience of preference-concordant decision making by patient characteristics and decision-making preferences
A total of 887 women provided answers to all three decision-making questions (preferred approach to decision making, own involvement, and provider involvement), which enabled us to determine whether they experienced preference-concordant decision making for prenatal genetic testing. Over half (57%) of this group was identified as having experienced a preference-concordant decision-making process. Bivariate analyses yielded several significant associations for this outcome, including race/ethnicity/language, education, poor literacy, low numeracy level, having another person express an opinion on the decision, and clinical site; however, only preference for decision-making approach and being a Spanish-speaking Latina retained significant effects in the multivariate analysis (Table 4). Specifically, compared to women who preferred an autonomous decision process, women who preferred a shared (aOR=0.42, 95% CI 0.32 – 0.57, P < .001) or a provider-driven decision process (aOR=0.21, 95% CI 0.10 – 0.45, P < .001) were significantly less likely to experience preference-concordant decision making. In addition, compared to White women, Spanish-speaking Latinas were significantly less likely to experience a preference-concordant decision process (aOR=0.40, 95% CI 0.22 – 0.73, P = .002).
Table 4.
Patient Characteristics Associated with Preference-Concordant Decision Making (n= 879)
| Experienced Preference-Concordant Decision Making | |||||
|---|---|---|---|---|---|
| Variable | n, (%) | OR (95% CI) | P | aORa (95% CI) | P |
| Preferred decision-making approach | |||||
| Shared | 157 (45.9) | .42 (.32 – .56) | < .001 | .42 (.32 – .57) | < .001 |
| Provider-driven | 10 (25.6) | .17 (.08 – .36) | < .001 | .21 (.10 – .45) | < .001 |
| Autonomous | 338 (66.8) | Reference | Reference | ||
| Race, ethnicity, and language | |||||
| Latina (Spanish speaking) | 86 (41.3) | .34 (.24 – .49) | < .001 | .40 (.22 – .73) | .002 |
| Latina (English speaking) | 45 (57) | .64 (.38–1.05) | .079 | .79 (.45 – 1.4) | .41 |
| Black | 77 (53.5) | .55 (.37–.83) | .004 | .76 (.45 – 1.3) | .31 |
| Asian | 37 (55.2) | .59 (.35–1.01) | .056 | .73 (.41–1.3) | .27 |
| Otherb | 46 (63.9) | .85 (.50–1.45) | .556 | 1.1 (.60 –1.9) | .80 |
| White | 214 (67.5) | Reference | Reference | ||
| Educational attainment | |||||
| Some high school or less | 74 (42.5) | .39 (.27 – .57) | < .001 | .88 (.47–1.7) | .69 |
| High school graduate | 70 (52.2) | .58 (.39 – .86) | .007 | 1.1 (.61–1.96) | .774 |
| Some college | 91 (54.8) | .65 (.45 – .93) | .019 | .99 (.61– 1.6) | .95 |
| College graduate or more | 269 (65.3) | Reference | Reference | ||
| Poor literacy | 89 (47.6) | .62 (.45 – .85) | .004 | .80 (.54 – 1.2) | .28 |
| Low numeracy | 150 (49.8) | .64 (.49 – .85) | .002 | 1.2 (0.85–1.8) | .28 |
| Prior birth | 258 (55.8) | .91 (.70 – 1.2) | .495 | 1.3 (.95 – 1.8) | .11 |
| Someone other than provider expressed opinion regarding decision for prenatal testing | 287 (60.9) | 1.4 (1.1 – 1.8) | .011 | 1.1 (.8 – 1.5) | .50 |
| Prenatal care received at a safety net clinical site | 171 (46.1) | .47 (.35 – .61) | < .001 | .77 (.50– 1.2) | .23 |
OR, odds ratio; aOR, adjusted odds ratio; CI, confidence interval
multivariate model adjusted for variables included in table and selected a priori
includes Native American (6), Filipina (31), Mixed (37), cannot choose (1)
Bold type indicates statistical significance at P ≤ .05
3.3. Mediation analysis elucidating pathways between patient characteristics and preference-concordant decision making
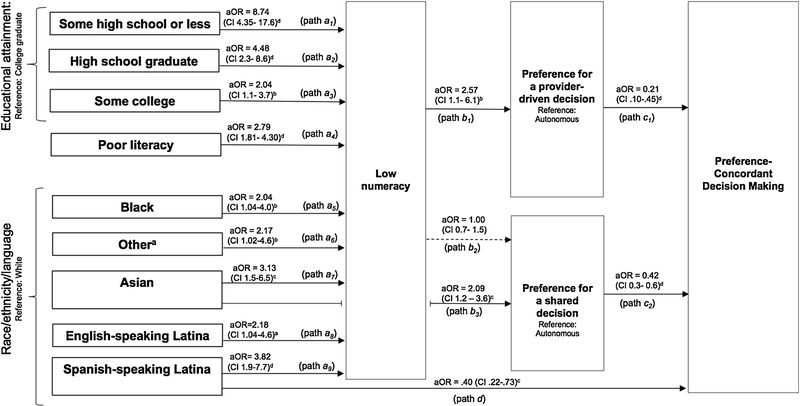
To determine whether low numeracy mediated the effects of patient characteristics (including race/ethnicity/language, education, and literacy) on preferring a provider-driven decision, we regressed the low numeracy indicator onto these characteristics (results not tabled). The results indicated significant effects of these sociodemographic indicators on numeracy (Figure 1; paths a1‒a9): (i) all race/ethnicity/language groups tended to have lower numeracy than White women: Spanish-speaking Latinas (aOR=3.8, 95% CI 1.9– 7.7 P= < .001), English-speaking Latinas (aOR=2.2, 95% CI 1.04– 4.57, P= .039), Black women (aOR=2.0, 95% CI 1.04– 4.0, P= .039), Asian women (aOR=3.1, 95% CI 1.5–6.5, P= .003), and women grouped as ‘Other’ (aOR=2.2, 95% CI 1.02– 4.6, P=.045); (ii) all women with less than a college degree had lower numeracy than college graduates: women with less than a high school education (aOR=8.7, 95% CI 4.3–17.6, P= < .001), or who had graduated from high school, but had not attended college (aOR=4.5, 95% CI 2.3– 8.6, P = < .001), and women who attained some college education, but did not graduate from college (aOR=2.0, 95% CI 1.1 – 3.7, P=.017); and (iii) women who had poor literacy had significantly higher odds of low numeracy, compared to women with adequate literacy (aOR=2.8, 95% CI 1.8 – 4.3, P= < .001).
Fig 1. Mediators of the relationship between sociodemographic characteristics and preference-concordant decision making.
A set of pathways (a1–9, b1–3, c1–2, and d) elucidate the role of low numeracy and preferring a provider-driven decision as mediators of the relationship between sociodemographic characteristics and preference-concordant decision making.
OR, odds ratio; aOR, adjusted odds ratio; CI, confidence interval
a includes Native American (6), Filipina (31), Mixed (37), cannot choose (1)
bP ≤ .05, cP ≤ .01, dP ≤ .001
dashed arrow indicates non-significant association
The significant associations between these sociodemographic characteristics and numeracy, and between numeracy and preference for a provider-driven decision (described above; Table 3), indicates that low numeracy mediated the relationships (i) between race/ethnicity/language, educational attainment, poor literacy, and (ii) preferring a provider-driven process (Figure 1; paths a1‒a9 and b1). In addition, compared to women preferring an autonomous decision process, those who preferred a provider-driven approach had significantly lower odds of experiencing preference-concordant decision making (path c1; aOR=0.21; 0.10 – 0.45). Thus, the relationship between numeracy and preference-concordant decision making was mediated by preferring a provider-driven approach (i.e., paths b1 and c1). Finally, although numeracy was not associated with preferring a shared decision versus an autonomous decision (path b2), this preference was associated with lower odds of preference-concordant decision making (path c2), and Asian women were significantly more likely to prefer shared decision making (path b3).
Looking across the entire set of analyses, the relationships between patient sociodemographic characteristics of race/ethnicity and education and experiencing preference-concordant decision making were mediated by low numeracy and preferring a provider-driven decision (versus autonomous). Among English-speaking Latinas, Black women, and women who were categorized as ‘Other’ (versus White women), as well as among women with lower educational attainment or poor literacy, low numeracy and preferring a provider-driven decision explained all the disparity in preference-concordant decision making. Among Spanish-speaking Latinas, low numeracy and preferring a provider-driven decision explained some, but not all, of the disparity (versus White women). Spanish-speaking Latinas, however, retained a significant association with the preference-concordant decision-making outcome that was independent of all mediators (aOR=0.40; 0.22–0.73; path d).
4. Discussion and Conclusion
4.1. Discussion
While shared decision making has been advocated for decisions around prenatal genetic testing, our results shed light on other decision-making approaches that some women may prefer. Just over half of the women in our study preferred an autonomous decision and 5% expressed a preference for a provider-driven decision. Importantly, a substantial proportion (43%) of the study participants did not experience preference-concordant decision making; non-White women, women who were not college graduates, and women who had low literacy were less likely to experience this outcome. Most of these sociodemographic disparities were completely mediated by numeracy and preferring a provider-driven approach (versus autonomous) through an interconnected set of pathways. For Spanish-speaking Latinas, not all the disparity was explained by these mediators; they remained significantly less likely to experience preference-concordant decision making, independent of the mediators.
Our results highlight the spectrum of decision-making approaches women may prefer, and although only 5% of women in our study preferred a provider-driven approach, it is consistent with other studies on decision making for genetic testing among breast cancer patients where 7–10% of patients preferred more provider-driven decision-making processes [23,24]. In another small study, seven out of ten women chose to delegate the decision-making process to trusted individuals such as their obstetricians for the decision on whether to undergo invasive prenatal genetic testing [25].
Our finding that disparities among Spanish-speaking Latinas persisted after adjusting for these mediators is consistent with other studies that have documented disparities among patients with limited English proficiency in the quality of care they receive [26–28]. Factors such as language and ethnicity discordance with the provider, or not utilizing medical interpreters, may have contributed to the persistent disparity for these patients [29]; however, we did not collect data on those elements.
The finding that 43% of study participants did not receive preference-concordant decision making is consistent with results from a previous systematic review [8], and suggests ample room for improvement in patient-centered counseling around prenatal genetic testing decision making, especially as past research has shown a strong association between preference-concordant decision making and satisfaction with both the decision-making process and treatment choice in other clinical contexts, including breast cancer [30–32].
One possible explanation for why women who preferred more provider input were less likely to experience a concordant decision process, or the reverse, why women who preferred an autonomous decision process were more likely to experience a concordant decision process, is that nondirective, patient-led counseling has historically been emphasized in prenatal genetic counseling because of concerns of impinging on autonomy, given the personal nature of the decision and a history of eugenics [33]. While this emphasis has recently shifted to encouraging shared decision making [34], providers may continue to be less accommodating of and responsive to preferences for decision making with more provider engagement.
Finally, although numeracy has often been conceptualized as part of health literacy, a growing body of research has documented the specific impact of numeracy on health outcomes [11,17]. Less numerate women in our study were more likely to prefer provider-driven decision making, consistent with past research in other clinical contexts [35]. Given the highly quantitative information typically included in prenatal testing counseling, our finding linking low numeracy to preference for a provider-driven decision and, in turn, lower odds of experiencing preference-concordant decision making highlights the importance of attention to individual patients’ needs for health communication to facilitate patient-centered care.
Our study has several limitations. First, while we were successful in recruiting a very diverse sample of pregnant women, all were seeking prenatal care in the San Francisco Bay Area, and agreed to participate in a study on decision making for prenatal test use. There may exist geographic regional variation in how women approach decision making for prenatal testing, and by agreeing to participate in the parent study, it is possible that they represent a group with different decision process preferences. Second, the observational design allows us to determine associations but not causation. Third, recall bias is possible because women were asked to think back to a decision process that had taken place weeks or months prior to the interview, and thus may not be an accurate assessment of what occurred. Finally, we constructed the preference-concordant decision-making variable, therefore potentially limiting its validity and generalizability.
4.2. Conclusion
In this study of women from diverse sociodemographic backgrounds and with varying literacy and numeracy levels, there was a wide range of preferences regarding approach to prenatal genetic testing decision making. Importantly, a significant proportion of women did not experience their preferred decision-making approach, with race/ethnicity and lower education being associated with not experiencing preference-concordant decision making. Women’s numeracy level, their preferred approach to decision making, and language contributed to women’s likelihood of experiencing preference-concordant decision making.
4.3. Practice Implications
Our findings have two key clinical implications. First, the range of women’s preferences for approach to prenatal genetic testing decision making underscores the importance of nuanced counseling. By eliciting women’s preferences for how they wish to approach these decisions, providers can respond to their preferences in a patient-centered manner to facilitate preference-concordant decision making. For women who prefer a provider-driven decision, for example, the provider can focus on eliciting women’s values to help inform recommendations; for women who desire an autonomous decision, the goal should be providing sufficient information to enable the patient to make an informed decision. Second, by understanding the important role of numeracy in decision-making preferences and preference-concordant decision making, tools that improve how prenatal testing information is communicated to women who are less numerate can enable decisions that align with women’s values.
Language barriers among women with limited English proficiency, coupled with low numeracy, may make this group of women particularly vulnerable to not experiencing a preference-concordant decision process. Future work can focus on understanding how providers and health systems can best meet these patients’ needs. Given the values-sensitive and quantitative nature of prenatal testing decisions, nuanced counseling approaches and interventions to address language and numeracy gaps are needed.
HIGHLIGHTS.
Over half of women did not prefer a shared decision making approach.
There were sociodemographic disparities in experiencing preference concordance.
Numeracy and preference for provider-driven approach mediated disparities.
Language barriers present challenges to preference-concordant decision making.
Acknowledgments
Role of Funding:
Funded by grants from the National Institutes of Health (R01HD49686), the March of Dimes Foundation (Social and Behavioral Sciences Research Grant 12-FY09-213), and the National Institute on Minority Health and Health Disparities of the National Institutes of Health (R25MD006832 and P60MD006902)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: none reported
References:
- [1].Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1997;44:681–92. [DOI] [PubMed] [Google Scholar]
- [2].Committee on Quality Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century Washington (DC): National Academy Press; 2001. [Google Scholar]
- [3].Sheridan SL, Harris RP, Woolf SH, Shared decision making about screening and chemoprevention. a suggested approach from the U.S. Preventive Services Task Force. Am J Prev Med 2004;26:56–66. [DOI] [PubMed] [Google Scholar]
- [4].Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med 2005;20:531–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Arora NK, McHorney CA. Patient preferences for medical decision making: who really wants to participate? Med Care 2000;38:335–41. [DOI] [PubMed] [Google Scholar]
- [6].Brom L, Hopmans W, Pasman HR, Timmermans DR, Widdershoven GA, Onwuteaka-Philipsen BD. Congruence between patients’ preferred and perceived participation in medical decision-making: a review of the literature. BMC Med Inform Decis Mak 2014;14:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Murray E, Pollack L, White M, Lo B. Clinical decision-making: patients’ preferences and experiences. Patient Educ Couns 2007;65:189–96. [DOI] [PubMed] [Google Scholar]
- [8].Prenatal diagnostic testing for genetic disorders. ACOG Practice Bulletin No. 162. American College of Obstetricians and Gynecologists. Obstet Gynecol 2016;127:108–22. [Google Scholar]
- [9].Screening for fetal aneuploidy. ACOG Practice Bulletin No. 163. American College of Obstetricians and Gynecologists. Obstet Gynecol 2016;127:123–37. [Google Scholar]
- [10].Bryant AS, Norton ME, Nakagawa S, et al. Variation in women’s understanding of prenatal testing. Obstet Gynecol 2015;125:1306–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ancker JS, Kaufman D. Rethinking health numeracy: a multidisciplinary literature review. J Am Med Inform Assoc 2007;14:713–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Smith SK, Sousa MS, Essink-Bot ML, Halliday J, Peate M, Fransen M. Socioeconomic differences in informed decisions about down syndrome screening: a systematic review and research agenda. J Health Commun 2016;21:868–907. [DOI] [PubMed] [Google Scholar]
- [13].Golbeck AL, Ahlers-Schmidt CR, Paschal AM, Dismuke SE. A definition and operational framework for health numeracy. Am J Prev Med 2005;29:375–6. [DOI] [PubMed] [Google Scholar]
- [14].Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making 2001;21:37–44. [DOI] [PubMed] [Google Scholar]
- [15].Reyna VF, Nelson WL, Han PK, Dieckmann NF. How numeracy influences risk comprehension and medical decision making. Psychol Bull 2009;135:943–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical implications of numeracy: theory and practice. Ann Behav Med 2008;35:261–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Yee LM, Niznik CM, Simon MA. Examining the role of health literacy in optimizing the care of pregnant women with diabetes. Am J Perinatol 2016;33:1242–9. [DOI] [PubMed] [Google Scholar]
- [18].Hanoch Y, Miron-Shatz T, Rolison JJ, Omer Z, Ozanne E. Shared decision making in patients at risk of cancer: the role of domain and numeracy. Health Expect 2015;18:2799–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kuppermann M, Pena S, Bishop J, et al. Effect of enhanced information, values clarification, and removal of financial barriers on use of prenatal genetic testing: a randomized controlled trial. J Amer Med Assoc 2014;312:1210–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Lawson KL, Pierson RA. Maternal decisions regarding prenatal diagnosis: rational choices or sensible decisions? J Obstet Gynaecol Can 2007;29:240–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Bass PF 3rd, Wilson JF, Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med 2003;18:1036–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 2002;7:83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Matsen CB, Lyons S, Goodman MS, Biesecker BB, Kaphingst KA. Decision role preferences for return of results from genome sequencing amongst young breast cancer patients. Patient Educ Couns 2018. [DOI] [PMC free article] [PubMed]
- [24].Helmes AW, Bowen DJ, Bengel J. Patient preferences of decision-making in the context of genetic testing for breast cancer risk. Genet Med 2002;4:150–7. [DOI] [PubMed] [Google Scholar]
- [25].Jun M, Thongpriwan V, Choi J, Sook Choi K, Anderson G. Decision-making about prenatal genetic testing among pregnant Korean-American women. Midwifery 2018;56:128–34. [DOI] [PubMed] [Google Scholar]
- [26].Ngo-Metzger Q, Sorkin DH, Phillips RS, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med 2007;2:324–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Institute of Medicine. Race, ethnicity, and language data: standardization for health care quality improvement Washington DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- [28].Sudore RL, Landefeld CS, Perez-Stable EJ, Bibbins-Domingo K, Williams BA, Schillinger D. Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Educ Couns 2009;75:398–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. J Amer Med Assoc 1999;282:583–9. [DOI] [PubMed] [Google Scholar]
- [30].Lantz PM, Janz NK, Fagerlin A, et al. Satisfaction with surgery outcomes and the decision process in a population-based sample of women with breast cancer. Health Serv Res 2005;40:745–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Vogel BA, Helmes AW, Hasenburg A. Concordance between patients’ desired and actual decision-making roles in breast cancer care. Psychooncology 2008;17:182–9. [DOI] [PubMed] [Google Scholar]
- [32].Keating NL, Guadagnoli E, Landrum MB, Borbas C, Weeks JC. Treatment decision making in early-stage breast cancer: should surgeons match patients’ desired level of involvement? J Clin Oncol 2002;20:1473–9. [DOI] [PubMed] [Google Scholar]
- [33].Hodgson J, Spriggs M. A practical account of autonomy: why genetic counseling is especially well suited to the facilitation of informed autonomous decision making. J Genet Couns 2005;14:89–97. [DOI] [PubMed] [Google Scholar]
- [34].Elwyn G, Gray J, Clarke A. Shared decision making and non-directiveness in genetic counselling. J Med Genet 2000;37:135–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Goggins KM, Wallston KA, Nwosu S, et al. Health literacy, numeracy, and other characteristics associated with hospitalized patients’ preferences for involvement in decision making. J Health Commun 2014;2:29–43. [DOI] [PMC free article] [PubMed] [Google Scholar]