Abstract
Yellow nail syndrome (YNS) is a rare clinical syndrome characterized by a triad of yellow thick nail, lymphedema and respiratory diseases. We experienced 2 cases of YNS with diffuse panbronchiolitis (DPB)-like pulmonary manifestation. Since YNS might be hidden to those who have been diagnosed with DPB, physicians should be alert to recognize nail signs of YNS in case of DPB refractory to macrolide therapy. We hereby review previous case reports of YNS and discuss its pulmonary manifestations.
Keywords: yellow nail syndrome, diffuse panbronchiolitis, tree-in-bud sign
Introduction
Yellow nail syndrome (YNS) is a rare clinical syndrome characterized by a triad of yellow thick nail, lymphedema and respiratory diseases, which was initially described by Samman and White in 1964 (1). The diagnosis of YNS remains essentially clinical in nature and is usually established by the classical triad. However, the complete triad is present only in 27-60 percent of the patients (2), therefore the presence of two features may be judged to be sufficient for diagnosis (3).
Various kinds of pulmonary manifestations of YNS are documented in the literature. Maldonado et al. evaluated 41 consecutive YNS cases and reported various pulmonary manifestations including pleural effusion (46%), bronchiectasis (44%), chronic sinusitis (41%) and recurrent pneumonia (22%) (3). Woodfield et al. also demonstrated that YNS patients with bronchiectasis presented with septal thickening (32%), consolidation (21%), pleural effusions (20%) and focal tree-in-bud appearances (4). However there are no case reports of YNS with diffuse panbronchiolitis (DPB)-like pulmonary manifestation.
We report our experience of two YNS patients that presented with DPB-like pulmonary manifestation with reviews of the literature.
Case Reports
[Case 1]
An 80-year-old woman with dyspnea, cough with moderate amounts of white-yellow sputum and chronic sinusitis with an onset of 20 years ago had been diagnosed with diffuse panbronchiolitis 14 years ago as computed tomography (CT) showed centrilobular nodules and bronchiolectasis (Fig. 1a), and her blood human leukocyte antigen (HLA) typing revealed B54 antigen. Her sputum culture revealed pseudomonas aeruginosa while mycobacterial culture of sputum was negative. Although oral erythromycin, 400 mg/day, was started, her dyspnea, CT findings (Fig. 1b) and airflow obstruction progressively worsened; the force expiratory volume in one second (FEV1) fell 85% of predicted to 73% of predicted for 9 years. Then long-term oxygen therapy (LTOT) was introduced one year ago for respiratory failure. The patient presented to our emergency room department with a 2-day history of fever and increasing sputum and was admitted to our hospital with a working diagnosis of bacterial pneumonia. Physical examination demonstrated a fast pitting edema in bilateral lower extremities and the presence of thickened and yellowish nails involving all fingers and toe nails (Fig. 2), whose potassium hydroxide smear was negative for fungus infection and which grew slowly as she had not cut her nails for 5 months. Chest CT revealed consolidation in the right lower lobe and bilateral pleural effusion. Sputum culture on admission was positive for pseudomonas aeruginosa; therefore she was diagnosed with bacterial pneumonia. Although her general condition improved after treatment with antibiotics, fast pitting edema of the lower extremities and pleural effusion didn't improve. We considered that these clinical features were caused by lymph edema thus reached a diagnosis of YNS.
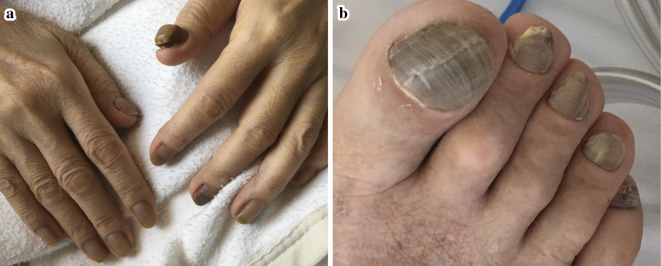
Figure 1.
Chest CT. (a) (Before macrolide therapy) Ill-defined centrilobular nodules in subpleural region, often extending to small branching linear areas of attenuation (tree-in-bud pattern). (b) (10 years after initiation of macrolide therapy) centrilobular nodules worsened and bronchiectasis are demonstrated.
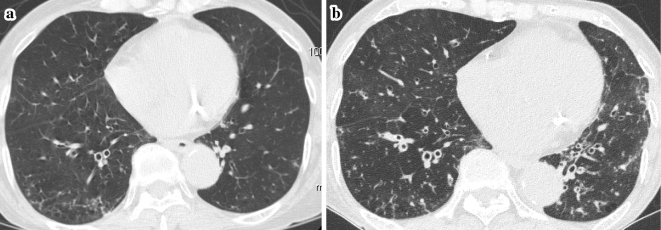
Figure 2.
The nails of both extremities (a, b). They turned yellow-black and thickened; especially the nail of left thumb was like a small stone.
[Case 2]
A 79-year-old woman with sinusitis and 20-year history of rheumatoid arthritis (RA) had been treated with prednisolone, celecoxib and methotrexate, never treated with bucillamine or D-penicillamine before. She was referred to our outpatient clinic because of chest CT findings which showed centrilobular nodules 4 years ago (Fig. 3a). Her sputum culture revealed pseudomonas aeruginosa while mycobacterial culture of sputum was negative. She was treated for chronic lower respiratory tract infection associated with RA with erythromycin 400 mg/day, however, the symptoms and radiological findings progressively worsened (Fig. 3b). Four years after starting long-term erythromycin, we noticed that her nail turned yellow with thickening (Fig. 4) and bilateral symmetric fast pitting edema in her lower extremities, leading to the diagnosis of YNS.
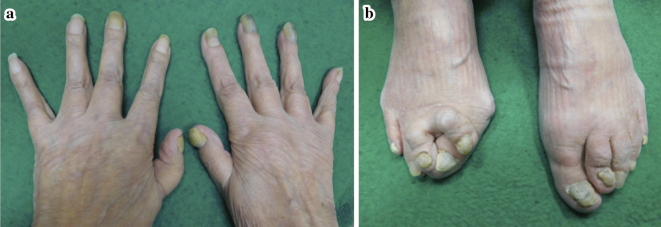
Figure 3.
Chest CT. (a) (Before macrolide therapy). Centrilobular nodules and curve-linear opacities in subpleural region of lower lobe. (b) (3 years after initiation of macrolide therapy) centrilobule nodules worsened with traction bronchiectasis and mucoid impaction of the bronchi.
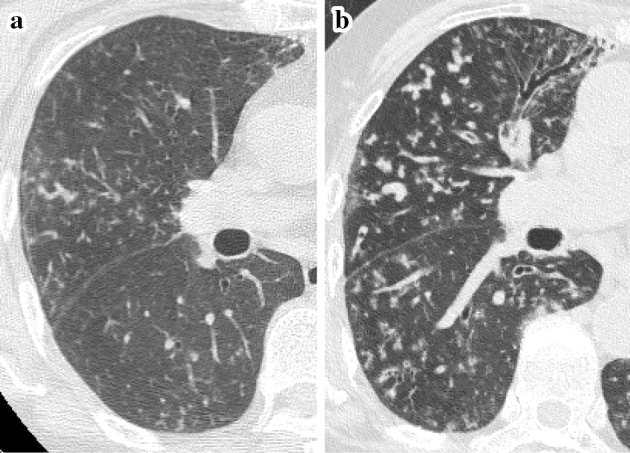
Figure 4.
The nails of both extremities (a, b). They turned yellow and thickened.
Discussion
We experienced two YNS patients with DPB-like pulmonary manifestations which were refractory to macrolide therapy; one case was associated with rheumatoid arthritis.
Although the etiology of YNS is poorly understood, disorder of lymphatic drainage is thought to be involved in the pathogenesis of YNS (5, 6), which is often evoked to explain lymphedema, pleural effusion, slow growth of nail or nail discoloration (2). However it is difficult to explain the pulmonary parenchymal manifestations, which are diverse including bronchiectasis and localized parenchymal infiltrates (3).
Woodfield et al. demonstrated that YNS patients showed symmetrical predominantly lower lobe bronchiectasis, with significantly less upper and middle lobe disease, and increased mucus plugging compared with matched idiopathic bronchiectasis patients (4). This suggests that pulmonary manifestations in YNS is caused by a disorder of delayed clearance due to abnormal lymphatic function, where gravity influences lower lobe disease development (3, 4). This lymphatic disorder may cause recurrent bronchitis or bronchiolitis, leading to bronchiectasis, which accounts for the tree-in-bud appearances in YNS patients in previous reports (4). On the other hand, small nodules in DPB patients representing bronchioles filled with secretions are getting dilated to proximal bronchi in ascending, which may be useful in differential diagnosis of DPB.
YNS has been associated with a variety of underlying diseases including connective tissue disease, malignancy, immunodeficiency states, drugs (D-penicillamine, gold and bucillamin), focal infection, such as nail candidiasis or tinea unguium, and several endocrine disorders such as diabetes mellitus and thyroid dysfunction (3, 7-9). When YNS is suspected, it is essential to confirm the presence of slow growth of nail and to rule out congestive heart failure and fungal infection based on fungal cultures or microscopic visualization of the fungal forms.
On the other hand, DPB is an idiopathic inflammatory disease, well recognized in Japan, characteristically presenting with bilateral, diffuse centrilobular nodular shadows with pulmonary hyperinflation and bronchiectasis on HRCT (10). Both DPB and YNS are typically associated with productive cough and chronic sinusitis, but DPB improves dramatically with the use of macrolide antibiotics whereas no effective treatment has been established for YNS (11). If patients suspected of DPB are refractory to macrolide therapy, we should consider other possible differential diagnosis, such as YNS. Moreover primary ciliary dyskinesia must be ruled out by electron microscopy though we didn't perform it in our cases.
Since YNS might be hidden to those who have been diagnosed with diseases such as DPB or bronchiolitis associated with RA, physicians should be alert to recognize nail signs of YNS, so that further investigations can be performed to confirm or exclude the presence of the triad features (7). The accumulation of cases may lead to elucidation of pathogenesis in the future.
In conclusion, we hereby provided first report of cases of YNS with pulmonary manifestations resembling DPB. More case detection and further evaluation is required for better understanding of YNS.
These preliminary cases were reported at the meeting for presentation of clinical reports of the Japanese Society of Internal Medicine, Tokyo, Japan, December 2017.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Samman PD, White WF. The “yellow nail” syndrome. Br J Dermatol 76: 153-157, 1964. [DOI] [PubMed] [Google Scholar]
- 2.Woodfield GE, Loebinger MR, Wilson R. Yellow nail syndrome: a review. Orphanet J Rare Dis 12: 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maldonado F, Tazelaar HD, Wang CW, Ryu JH. Yellow nail syndrome: analysis of 41 consecutive patients. Chest 134: 375-381, 2008. [DOI] [PubMed] [Google Scholar]
- 4.Woodfield G, Nisbet M, Jacob J, et al. Bronchiectasis in yellow nail syndrome. Respirology 22: 101-107, 2017. [DOI] [PubMed] [Google Scholar]
- 5.Bourcier T, Baudrimont M, Borderie V, Mayaud C, Laroche L. Conjunctival changes associated with yellow nail syndrome. Br J Ophthalmol 86: 930, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marks R, Ellis JP. Yellow nails. Arch Dermatol 102: 619-623, 1970. [DOI] [PubMed] [Google Scholar]
- 7.Noor NM, Basavaraju K, Sharpstone D. Yellow nail syndrome in rheumatoid arthritis: an aetiology beyond thiol drugs. Oxford Med Case Reports 3: 37-40, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta S, Samra D, Yel L, Agrawal S. T and B cell deficiency associated with yellow nail syndrome. Scand J Immunol 75: 329-335, 2012. [DOI] [PubMed] [Google Scholar]
- 9.Maldonado F, Ryu JH. Yellow nail syndrome. Curr Opin Pulm Med 15: 371-375, 2009. [DOI] [PubMed] [Google Scholar]
- 10.Poletti V, Casoni G, Chilosi M, Zompatori M. Diffuse panbronchiolitis. Eur Respir J 28: 862-871, 2006. [DOI] [PubMed] [Google Scholar]
- 11.Kudoh S, Keicho N. Diffuse panbronchiolitis. Clin Chest Med 33: 297-305, 2012. [DOI] [PubMed] [Google Scholar]