Short abstract
This case report describes the use of a three-dimensional reconstruction technique to plan the abdominal incision in order to avoid incision-related complications in a 53-year-old female patient who had had a cystic mass in the liver for 16 years and had undergone four previous surgeries. The patient presented with a recurrent cyst. The surgical team used three-dimensional reconstruction to model the liver mass, the area of abdominal wall weakness due to previous surgeries, bowel adhesions, skeletal structure and whole abdominal contour. The models were superimposed upon each other to reveal the relationship between the various features so that the optimum incision point could be selected so as to avoid the area of abdominal wall weakness, bowel adhesions and vital organs. The actual surgical incision was made based on the three-dimensional reconstruction models and the surgeon was able to avoid the area of abdominal wall weakness and bowel adhesions as planned. No incisional hernia and wound infection were observed postoperatively and the incision healed well. The three-dimensional reconstruction technique for preoperative surgical incision planning on patients with a history of multiple abdominal surgeries can minimize incision-related complications and achieve good therapeutic results.
Keywords: Three-dimensional reconstruction, repeated abdominal operations, incision planning, incision complications
Introduction
Patients with some benign liver or biliary diseases are very likely to undergo repeated abdominal surgeries during their lifetimes due to the developments in surgical technology and increasing life expectancy, and this phenomenon is expected to increase in the future.1 It is reported that as many as 10% of patients undergoing general surgeries are having repeat operations.1,2 Reoperation for some patients with a history of abdominal surgery is challenging because adhesiolysis leads to increased operation time, increased incidence of bowel injury, increased intraoperative blood loss and incidence of postoperative incisional hernia formation.3 Furthermore, postoperative mortality and healthcare costs are increased.4
With the development of computer technology, computer-assisted medicine has become a new direction in surgery. Currently, computers are being used during preoperative evaluations and to prepare a precise surgical plan, leading to safer and less invasive surgical procedures.5,6 Thus, computer-assisted surgery is able to decrease postoperative complications and risks.6 This case report describes the retrospective assessment of the application of computer-assisted incision planning in a patient that had previously undergone repeated abdominal surgeries.
Case report
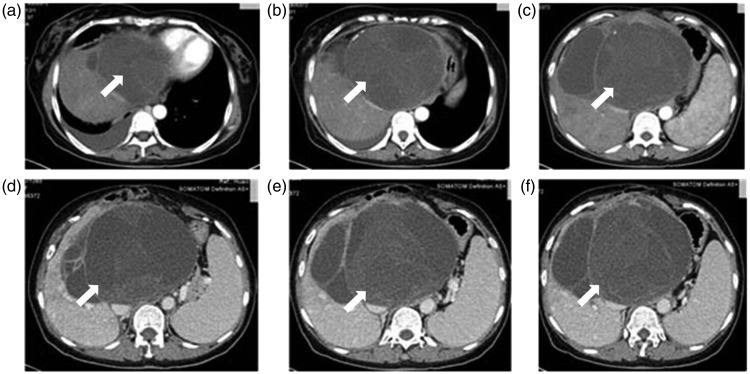
A 53-year-old female patient had been suffering from a cystic mass in the liver for 16 years and had undergone four previous surgical treatments. On 20 August 2017, the patient presented at the Department of Liver Surgery, West China Hospital, Sichuan University, Chengdu, Sichuan Province, China with abdominal distension and a recurrent cyst was diagnosed. A physical examination revealed multiple surgical scars on the abdomen and the abdominal wall associated with the scars was thin and weak. A computed tomography (CT) scan showed a multiple cystic mass in the liver that was approximately 15 × 12 cm (Figure 1). The mass was close to the abdominal wall and adhesions were suspected. The initial surgical plan was to remove the cystic mass using an open approach. Upon consideration of the special situation of the abdominal wall, the ideal incision needed to avoid the adhesive bowel, cystic wall and weak areas of the abdominal wall in order to prevent bowel injury, postoperative wound dehiscence, incisional hernia formation and other postoperative complications. Therefore, the surgical team decided to use a computer-assisted three-dimensional reconstruction technique to plan the most appropriate surgical incision in advance.
Figure 1.
A 53-year-old female patient had been suffering from a cystic mass in the liver for 16 years and had undergone four previous surgical treatments. The patient presented with abdominal distension and a recurrent cystic mass was diagnosed. Enhanced computed tomography scan images showing the cystic mass (white arrows) in the liver at different transverse levels.
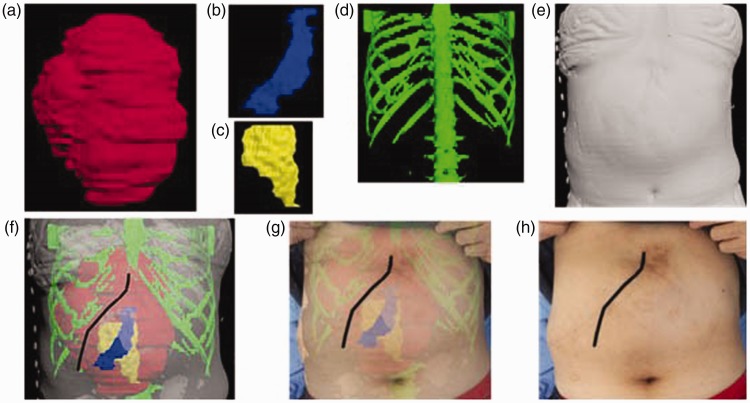
The surgical team used CT scan images of the patient to reconstruct a three-dimensional model of the cystic mass, the weak area of the abdominal wall, the bowel area close to the abdominal wall, the skeletal structure and the whole abdominal contour using Mimics software version 15.0 (Materialise, Leuven, Belgium) (Figures 2a–2e). Then all of the three-dimensional models were superimposed upon each other to reveal the relationship between the weak area of the abdominal wall, the cystic mass and the adhesive bowel, so that the incision site could be selected to avoid the abdominal wall weakness and bowel adhered to the abdominal wall (Figure 2f). Then the actual abdominal incision site was selected by overlaying the three-dimensional model images over the patient's abdominal contour image (Figures 2g–2h).
Figure 2.
A computer-assisted three-dimensional reconstruction technique was used to plan the most appropriate surgical incision in advance of the actual surgery in a 53-year-old female patient who had been diagnosed with a recurrent cystic mass. (a) Cystic mass in the liver; (b) weak area of the abdominal wall; (c) bowel adhesion to the abdominal wall; (d) skeletal reconstruction used for positioning; (e) reconstruction of the abdominal contour; (f) images of the cystic mass, weak area of the abdominal wall, bowel adhesive area, bones and contour of the abdomen were all superimposed upon each other to help with the selection of the optimal surgical incision point; (g) overlay of image F onto the patient's actual abdominal contour picture; (h) the surgical incision point that was selected for surgery. The colour version of this figure is available at: http://imr.sagepub.com.
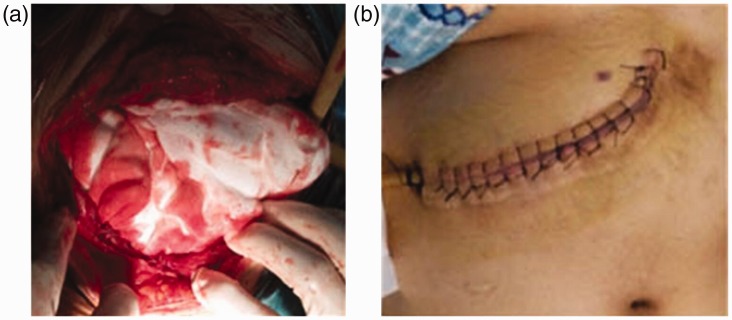
The surgical team opened the abdomen through the incision that had been planned using the computer-assisted three-dimensional models. The incision went approximately 3cm through subcutaneous and muscular tissue. Intraoperative exploration revealed some small intestine adhered to the abdominal wall. The incision just avoided the area of abdominal wall weakness and the intestinal adhesion. The incision healed well without any wound infection and no incisional hernia developed postoperatively (Figure 3).
Figure 3.
Representative photographs of the actual surgical incision (a) and the healed incision (b) in a 53-year-old female patient who had been diagnosed with a recurrent cystic mass in whom a computer-assisted three-dimensional reconstruction technique was used to plan the most appropriate surgical incision in advance of the actual surgery. The colour version of this figure is available at: http://imr.sagepub.com.
This study was approved by the ethics committee of the West China Hospital, Sichuan University, Chengdu, Sichuan Province, China. The patient provided written informed consent.
Discussion
With the development of computer-assisted surgical planning, hepatobiliary surgery has started to enter a phase of precision surgery. A precise operation is dependent upon an accurate preoperative evaluation and the development of a precise surgical plan to allow for meticulous manipulation with minimal invasion. Three-dimensional reconstruction techniques provide a powerful tool for the development of precision surgery.6,7
Repeated abdominal surgery usually leads to intra-abdominal organ adhesion, which changes the normal visceral anatomy and peritoneal cavity, so surgeons often find this a challenge especially when there is also a thin abdominal wall.8,9 How to choose a good incision point in patients with a history of repeated abdominal surgery remains a challenge for experienced surgeons. Three-dimensional reconstruction modelling was introduced to facilitate the development of individualized preoperative surgical planning. By using a three-dimensional reconstruction technique, the visceral anatomy and abdominal wall status can be evaluated in advance of the surgery and preoperative abdominal incision planning can be precisely made.
Traditional abdominal imaging is limited to two-dimensional images, which means that the surgeon has to be able to imagine the three-dimensional anatomical relationship of the abdominal organs,10–12but subjectivity and low accuracy makes it difficult to evaluate lesion invasion and to select the most appropriate surgical approach. With the development of digital medical technology, three-dimensional reconstruction techniques have been widely used in the preoperative evaluation of patients with benign and malignant hepatic tumours and intrahepatic bile duct stones, achieving good results.13,14Using three-dimensional reconstruction, the surgeon can accurately construct a three-dimensional model of the abdominal organs using a computer. It provides details of the location, size and volume of the abdominal mass and its spatial relationship with vascular structures, which allows surgeons to optimize their surgical plans and to undertake virtual surgery. In this current case, three-dimensional reconstruction was used to reconstruct the size and location of the abdominal mass in relation to the weak area of the abdominal wall on the computer in advance of the actual operation. This technique allowed for a precise surgical incision that avoided postoperative incisional hernia formation.
Although three-dimensional imaging has achieved incremental progress in precise preoperative and intraoperative surgical planning beyond conventional two-dimensional imaging, certain limitations should be pointed out.15,16 Three-dimensional imaging is based on two-dimensional imaging, thus, improved two-dimensional imaging resolution will significantly increase the accuracy of these three-dimensional models.11,17However, the current level of accuracy rendered by these three-dimensional imaging models appears to be associated with some limitations when compared with the actual tissues observed during surgery.18 Another limitation is the time used to produce a single three-dimensional model, which is approximately 3–4 hours.16,19,20 Research is constantly working on a number of initiatives that will likely improve the efficiency of three-dimensional model reconstruction.
In conclusion, this case report has described the successful surgical treatment of a female patient with multiple previous abdominal surgeries using three-dimensional imaging for preoperative surgical incision planning. The use of digital three-dimensional reconstruction technology can improve the accuracy of surgery and achieve good therapeutic results.
Declaration of conflicting interest
The authors declare that there are no conflicts of interest.
Funding
The research was funded by the Chinese Foundation for Hepatitis Prevention and Control – Tian Qing Liver Disease Research Fund Subject (no. TQGB20170067), the Scientific Research Starting Foundation for Youths of Sichuan University (no. 2015SCU11999-9), and the Science and Technology Support Program of Sichuan Province (no. 2017KZ0019).
References
- 1.Schurr P, Kohrs D, Reichelt U, et al. Repeated surgery improves survival in recurrent gastrointestinal stromal tumors: a retrospective analysis of 144 patients. Dig Surg 2009; 26: 229.–. [DOI] [PubMed] [Google Scholar]
- 2.ten Broek RP, Strik C, Issa Y, et al. Adhesiolysis-related morbidity in abdominal surgery. Ann Surg 2013; 258: 98–106. [DOI] [PubMed] [Google Scholar]
- 3.Stommel MW, Strik C, ten Broek RP, et al. Impact of adhesiolysis on outcome of colorectal surgery. Dig Surg 2016; 33: 83–93. [DOI] [PubMed] [Google Scholar]
- 4.ten Broek RP, Issa Y, van Santbrink EJ, et al. Burden of adhesions in abdominal and pelvic surgery: systematic review and met-analysis. BMJ 2013; 347: f5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Oosterom MN, van der Poel HG, Navab N, et al. Computer-assisted surgery: virtual- and augmented-reality displays for navigation during urological interventions. Curr Opin Urol 2018; 28: 205–213. [DOI] [PubMed] [Google Scholar]
- 6.Su L, Zhou XJ, Dong Q, et al. Application value of computer assisted surgery system in precision surgeries for pediatric complex liver tumors. Int J Clin Exp Med 2015; 8: 18406–18412. [PMC free article] [PubMed] [Google Scholar]
- 7.Dong J, Yang S, Zeng J, et al. Precision in liver surgery. Semin Liver Dis 2013; 33: 189–203. [DOI] [PubMed] [Google Scholar]
- 8.Kobayashi A, Morioka D, Matsumoto C, et al. Hepatocellular carcinoma incidentally detected at second hepatectomy for repeated colorectal liver metastasis in a patient with hepatitis C virus-related cirrhosis: a case report. J Med Case Rep 2016; 10: 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Treska V, Skalicky T, Liska V, et al. Repeated procedures for colorectal liver metastases. Hepatogastroenterology 2007; 54: 1775–1778. [PubMed] [Google Scholar]
- 10.Muller MA, Marincek B, Frauenfelder T. State of the art 3D imaging of abdominal organs. JBR-BTR 2007; 90: 467–474. [PubMed] [Google Scholar]
- 11.Hicks CW, Hashimoto K, Uso TD, et al. Use of 3-dimensional imaging reconstruction in the treatment of advanced intra-abdominal desmoid tumors. Surgery 2012; 151: 625–627. [DOI] [PubMed] [Google Scholar]
- 12.Wasnik AP, Mazza MB, Lalchandani UR, et al. Normal and variant abdominal anatomy on magnetic resonance imaging. Magn Reson Imaging Clin N Am 2011; 19: 521–545. [DOI] [PubMed] [Google Scholar]
- 13.Fang CH, Liu J, Fan YF, et al. Outcomes of hepatectomy for hepatolithiasis based on 3-dimensional reconstruction technique. J Am Coll Surg 2013; 217: 280–288. [DOI] [PubMed] [Google Scholar]
- 14.Fang CH, Tao HS, Yang J, et al. Impact of three-dimensional reconstruction technique in the operation planning of centrally located hepatocellular carcinoma. J Am Coll Surg 2015; 220: 28–37. [DOI] [PubMed] [Google Scholar]
- 15.Ni Q, Wang H, Liang X, et al. Successful parenchyma-sparing anatomical surgery by 3-dimensional reconstruction of hilar cholangiocarcinoma combined with anatomic variation. J Coll Physicians Surg Pak 2016; 26: S13–S15. [PubMed] [Google Scholar]
- 16.He YB, Bai L, Jiang Y, et al. Application of a three-dimensional reconstruction technique in liver autotransplantation for end-stage hepatic alveolar echinococcosis. J Gastrointest Surg 2015; 19: 1457–1465. [DOI] [PubMed] [Google Scholar]
- 17.Zhang T, Chowdhury S, Lustig M, et al. Clinical performance of contrast enhanced abdominal pediatric MRI with fast combined parallel imaging compressed sensing reconstruction. J Magn Reson Imaging 2014; 40: 13–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perica E, Sun Z. Patient-specific three-dimensional printing for pre-surgical planning in hepatocellular carcinoma treatment. Quant Imaging Med Surg 2017; 7: 668–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guan T, Fang C, Mo Z, et al. Long-term outcomes of hepatectomy for bilateral hepatolithiasis with three-dimensional reconstruction: a propensity score matching analysis. J Laparoendosc Adv Surg Tech A 2016; 26: 680–688. [DOI] [PubMed] [Google Scholar]
- 20.Li K, Tang Z, Liu GJ, et al. Three-dimensional reconstruction of paracentesis approach in transjugular intrahepatic portosystemic shunt. Anat Sci Int 2012; 87: 71–79. [DOI] [PubMed] [Google Scholar]