Significance
Growing up in urban environments is associated with risk of developing psychiatric disorders, but the underlying mechanisms are unknown. Green space can provide mental health benefits and possibly lower risk of psychiatric disorders. This nation-wide study covering >900,000 people shows that children who grew up with the lowest levels of green space had up to 55% higher risk of developing a psychiatric disorder independent from effects of other known risk factors. Stronger association between cumulated green space and risk during childhood constitutes evidence that prolonged presence of green space is important. Our findings affirm that integrating natural environments into urban planning is a promising approach to improve mental health and reduce the rising global burden of psychiatric disorders.
Keywords: geographic information systems, mental health, psychological ecosystem services, remote sensing, urban planning
Abstract
Urban residence is associated with a higher risk of some psychiatric disorders, but the underlying drivers remain unknown. There is increasing evidence that the level of exposure to natural environments impacts mental health, but few large-scale epidemiological studies have assessed the general existence and importance of such associations. Here, we investigate the prospective association between green space and mental health in the Danish population. Green space presence was assessed at the individual level using high-resolution satellite data to calculate the normalized difference vegetation index within a 210 × 210 m square around each person’s place of residence (∼1 million people) from birth to the age of 10. We show that high levels of green space presence during childhood are associated with lower risk of a wide spectrum of psychiatric disorders later in life. Risk for subsequent mental illness for those who lived with the lowest level of green space during childhood was up to 55% higher across various disorders compared with those who lived with the highest level of green space. The association remained even after adjusting for urbanization, socioeconomic factors, parental history of mental illness, and parental age. Stronger association of cumulative green space presence during childhood compared with single-year green space presence suggests that presence throughout childhood is important. Our results show that green space during childhood is associated with better mental health, supporting efforts to better integrate natural environments into urban planning and childhood life.
The number of people living in cities is increasing, and, globally, more than 50% of the human population is now city dwellers, with no sign of this trend slowing down (1). Urban living often offers good sanitation, access to health care, nutrition, and education (2), but has also been associated with adverse health effects (3, 4). In some societies, urban residents have almost 50% higher risk of developing psychiatric disorders such as anxiety and mood disorders compared with their rural counterparts (5–7), and schizophrenia risk is 200% higher for children growing up in the most urban environments (8, 9). Different hypotheses have been proposed to explain these urban−rural gradients in mental health, including selective migration (10), social stress processing (4), higher exposure to infections (8), and reduced exposure to nature (11). However, the mechanistic links are not well understood (5, 12).
Low exposure to nature, or green space, has been proposed in recent years as a potential environmental risk factor for various mental health outcomes. Exposure to green space has been suggested to lower depression (13, 14) and schizophrenia risk (15), improve children’s cognitive development (16), and reduce neural activity linked to psychiatric disorders (11, 17). Dose–response relationships from other studies show that higher doses of green space are associated with better mental health (13), and long-lasting positive effects of moving to greener areas (18) suggest causation, albeit most of these studies are small and cross-sectional. Whether the association with green space is specific or applies to a broader spectrum of psychiatric disorders and to what degree the association is independent from urbanization in general or just mirrors the urban−rural gradient are unknown. Access to green space partially depends on socioeconomic factors, such as housing prices, and the extent to which this explains associations between green space and mental illnesses is another unknown aspect.
Exposure to green space may influence mental health through both psychological and physiological pathways, as green spaces serve as settings for individual and social behavior and can mitigate negative influences of other aspects of the physical environment (19). These mechanistic pathways could vary for different psychiatric disorders, with green space as a shared risk-decreasing factor. Green space can promote mental health by supporting psychological restoration, encouraging exercise, improving social coherence, decreasing noise and air pollution affecting cognition and brain development, and improving immune functioning (19–22). Given that green space can promote mental health and quality of life in urban populations, urban planning and policy will benefit from more information on the likely generality of effects on psychiatric disorders and how those effects are realized over the life course. Here, we investigate whether green space presence during childhood is associated with the risk of developing any of a broad range of psychiatric disorders later in life, by combining nationwide population data with individual-level green space presence data. We determine the strength and shape of the association between green space and a spectrum of mental health outcomes to clarify whether dose–response relationships exist and, if this is the case, whether the associations are linear or asymptotic. We also examine whether risk of psychiatric disorders is more strongly associated with green space presence at a specific age during childhood.
We use data extracted from multiple Danish population-based registers together with high-resolution satellite images. Unlike most previous studies on green space, the current study includes all members of the national population who met our criteria for inclusion. Our study population thus includes all persons born in Denmark from 1985 to 2003 and living in Denmark on their 10th birthday for whom we have longitudinal data on mental health outcomes, socioeconomic status, and place of residence (n = 943,027). We constructed a dataset of yearly individual-level green space presence within 210 × 210 m, 330 × 330 m, 570 × 570 m, and 930 × 930 m squares around each person’s residence based on the normalized difference vegetation index (NDVI). NDVI was calculated from remotely sensed 30-m-resolution Landsat satellite images covering the entire country for the years 1985–2013. We combined these two datasets for two purposes: (i) to examine the specific contribution of green space presence during childhood to the risk of diverse, adolescent into adult psychiatric disorders, over and above the contributions of correlated risk factors including urbanization, socioeconomic factors, parental history of mental illness, and parental age; and (ii) to explore how green space is affecting mental health by estimating these associations at different ages and by determining the shape of the relationship green space has with each of the psychiatric disorders.
Results
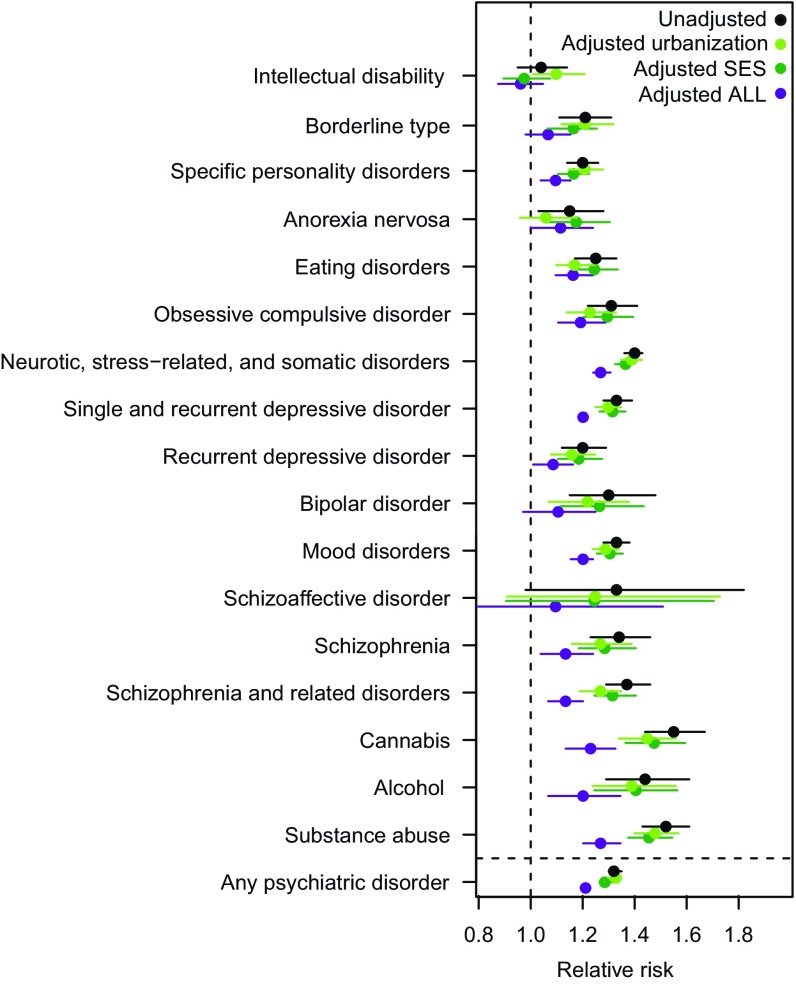
Relative risk, estimated as incidence rate ratios (IRR), was higher for persons living at the lowest NDVI compared with those living at the highest levels of NDVI for all psychiatric disorders, except intellectual disability (IRR: 1.04; 95% CI: 0.95 to 1.14) and schizoaffective disorder (IRR: 1.33; 95% CI: 0.98 to 1.82) (Fig. 1). Adjusting for urbanization, parents’ socioeconomic status, family history, parental age, municipal socioeconomic factors, and a combination of all five potential confounding factors only changed the risk estimates slightly, with no change to the overall association with NDVI, except for borderline type, anorexia, and bipolar disorder for which adjusting for all five factors made green space presence insignificant (Fig. 1 and SI Appendix, Fig. S1). Population attributable risk estimates showed that the association between NDVI and psychiatric disorder risk was, in general, comparable in magnitude to that of family history and parental age, higher than urbanization, and slightly lower than parents’ socioeconomic status (SI Appendix, Table S1). Substance abuse disorders, specific personality disorder, borderline type, and intellectual disability risk were mostly associated with parents’ socioeconomic status, while mood disorder, single and recurrent depressive disorder, and neurotic, stress-related, and somatic disorder risk were mostly associated with NDVI, although the last has an association of similar strength as parents’ socioeconomic status.
Fig. 1.
The association between childhood green space presence and the relative risk of developing a psychiatric disorder later in life. Green space presence was measured as the mean NDVI within a 210 × 210 m square around place of residence (n = 943,027). Low values of NDVI indicate sparse vegetation, and high values indicate dense vegetation. Relative risk estimates are relative to the reference level (set to the highest decile) for NDVI fitted as numeric deciles in classes of 10. Estimates above the dashed line indicate higher risk of developing a given psychiatric disorder for children living at the lowest compared with the highest values of NDVI. Three additional models were fitted to adjust for the effect of urbanization, parental socioeconomic status (SES), and the combined effect of urbanization, parental and municipal socioeconomic factors, parental history of mental illness, and parental age at birth on risk estimates. All estimates were adjusted for age, year of birth, and gender and plotted with 95% CIs.
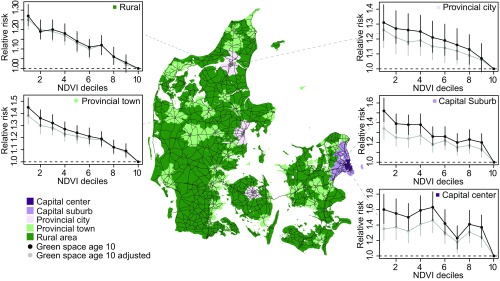
The relative risk of developing any psychiatric disorder was related to NDVI in a dose–response relationship across urbanization levels, with risk declining incrementally with higher doses of green space, although nonmonotonically for the capital center region (Fig. 2). Mean NDVI was lowest for the capital center area, but the range of NDVI values was represented across each urbanization category (SI Appendix, Table S2). The strongest association between relative risk and the lowest decile of green space presence was for the capital center region (NDVI decile 1; IRR1: 1.60; 95% CI1: 1.42 to 1.80) and the weakest association was for rural areas (IRR1: 1.27; 95% CI1: 1.22 to 1.33). Although a Cox regression model with an interaction term showed that the association with NDVI varied significantly across the different degrees of urbanization (P = 0.001, chisq = 97.8, df = 36), the general pattern of lower NDVI being associated with higher risk was similar within each degree of urbanization. Adjusting for urbanization and parents’ socioeconomic status only slightly lowered estimates.
Fig. 2.
The association between relative risk of developing any psychiatric disorder and childhood green space presence across urbanization levels. Data were split between each of the five urbanization classes (Capital center n = 56 650, Capital suburb n = 124,193, Provincial city n = 90,648, Provincial town n = 265,570, and Rural n = 376,525). NDVI was recalculated as deciles, and separate models, shown in black, were fitted within each urbanization class to determine the shape of the association between green space and mental health. Integer values on the x axis refer to decile ranges, i.e., 1 corresponds to decile 0 to 10%. An additional model, shown in grey, was fitted for each urbanization class to adjust for urbanization and parents’ socioeconomic status. Estimates of relative risk from all five models were adjusted for year of birth and gender and plotted with 95% CIs within each degree of urbanization.
We found no consistent sign of green space presence being associated with any particularly sensitive age across all disorders (SI Appendix, Fig. S2). Alcohol abuse, specific personality disorders, and borderline type diverged from the general pattern, with a tendency toward stronger protective associations occurring at age 3 y to 4 y based on the nonoverlapping confidence intervals between individual estimates. We compared the association with cumulated green space presence by fitting models with deciles of mean NDVI at the 10th birthday and as cumulated NDVI from birth to the 10th birthday. Mean and cumulated NDVI were both associated with risk in a dose–response relationship, with children living at the lowest green space presence having the highest risk of developing a psychiatric disorder (SI Appendix, Fig. S3). Risk estimates were generally higher for cumulated green space presence than presence measured at age 10 y, again suggesting an accumulating dose–response relationship. About half of all cases across all disorders were diagnosed in adulthood (age >19 y) (SI Appendix, Table S3). Splitting data between persons diagnosed in adolescence (age 13 y to 19 y) and adulthood showed a stronger association between risk of any psychiatric disorder and green space for the former (IRR1: 1.64; 95% CI1: 1.58 to 1.70) than the latter age category (IRR1: 1.43; 95% CI1: 1.35 to 1.52), with no change in the direction of the association (SI Appendix, Fig. S4). Associations mostly did not differ between the two age groups for individual disorders, with the exception of substance and cannabis abuse. Both substance and cannabis abuse showed stronger associations between risk and green space for persons diagnosed in adolescence; however, cannabis abuse diagnosed in adulthood was statistically insignificant due to low sample size in the first half of the sampling period. We found no strong difference in the association between risk and green space measured at 210 × 210 m, 330 × 330 m, 570 × 570 m, or 930 × 930 m presence zones (SI Appendix, Table S4). For both the age sensitivity and cumulated green space analysis, adjusting for urbanization and parents’ socioeconomic status only slightly lowered risk estimates.
Discussion
Our results show that high levels of childhood green space are associated with lower risk of developing any of a spectrum of adolescent into adult psychiatric disorders. Living at the lowest levels of green space compared with living at the highest levels of green space was associated with 15 to 55% higher risk, except for intellectual disability and schizoaffective disorder. The protective association remained after adjusting for other known risk factors including urbanization, socioeconomic factors, family history of mental illness, and parental age, indicating an independent association with green space. Our results are in line with previous reports of positive impacts on mental health from green space (19, 20, 23, 24). Furthermore, the association with NDVI was comparable in magnitude to or even higher than those of other known risk factors, including parents’ socioeconomic status, history of mental illness, and age.
A number of psychological and physiological mechanisms might link elements of green space to decreased risk of psychiatric disorders. Each of the hypothetical mechanisms considered below may be of greater importance for some disorders than for others. Individuals with urban upbringing have high neural activity linked to stress processing, which could lead to higher risk of psychiatric disorders in adults (4). Green space can enhance psychological restoration, can affect brain structure through positive associations with amygdala integrity, and could mitigate negative effects from the socially dense and noisy city environment that heighten stress (17, 19, 23, 24). The present study offers some evidence bearing specifically on green space as a support for psychological restoration. Previous studies have shown mental health benefits for children with better access to green space (25), with, for example, nearby nature buffering the negative impact of life stress for rural children (26). Neurotic, stress-related, and somatic disorders, as well as single and recurrent depressive disorder, had some of the highest relative risk and population attributable risk estimates associated with NDVI, which could reflect the role of green spaces as restorative environments. Strong associations for substance abuse disorders could indicate the development of better stress-processing ability with more green space, resulting in less need for self-medication later in life. Genetically vulnerable individuals could be particularly at risk from stress-triggered expression of psychiatric disorders, and gene−environment interactions should be investigated next, e.g., using polygenic risk scores or genome-wide association studies.
In our study, the relative risk of developing any psychiatric disorder was associated with green space in a dose–response relationship within all urbanization levels, showing that the association with green space presence is present after adjusting for urbanization. We found the highest relative risk for the capital center region and the lowest for rural areas, consistent with previous findings (27, 28). Higher pace of life and social stress in the most urbanized areas could create a stronger need for restorative environments such as urban green space. This finding also suggests that the highly urbanized capital center area could benefit most from additional green space as an early intervention tool in healthy city planning and development. In contrast, the nonmonotonic decrease of risk in the capital center area could indicate that capital residents residing in high-income neighborhoods receive risk-decreasing benefits from the urban environment, e.g., better schools or lower crime rates, not captured by our municipal socioeconomic adjustment and that these benefits, at some level, become more important than green space.
We found no consistent sign across all psychiatric disorders of green space presence being associated with any particularly sensitive age during childhood. NDVI at age 10 y and cumulated NDVI were both associated with risk across all psychiatric disorders in a dose–response relationship that could reflect causation. We might expect neurodevelopmental disorders such as schizophrenia to be more strongly associated with green space during the earliest years of life when brain development is most vulnerable compared with, e.g., substance abuse disorders. Schizophrenia risk peaked slightly at age 3 y, but the pattern was not stronger than for other disorders. Interestingly, substance and alcohol abuse showed slight increases in the protective association during both the earliest and latest years, suggesting that multiple pathways may influence these particular associations. Comparing associations for persons diagnosed in adolescence versus in adulthood may indicate that childhood green space is somewhat more strongly associated with developing a psychiatric disorder in adolescence. We hypothesize that, during the earliest years of childhood, pathways related to passive exposure, such as noise reduction or air pollution removal, may be important, whereas pathways related to use, such as exercise and social interactions, may become increasingly important as a child becomes more independent. Green space around children’s schools likely becomes increasingly important with age. Furthermore, parents’ actions will influence children’s visits to parks and other green spaces. The use of different high-resolution measures of green space such as vegetation height and structure should be investigated further to understand which aspects of green space affect mental health and through which mechanisms.
Risk estimates were generally higher for a measure of cumulated green space presence, compared with presence measured at age 10 y, supporting a dose–response relationship over time. Furthermore, this suggests that the protective association with green space builds up over time and that green space presence is important all through childhood. Our results are consistent with previous work showing improved mental well-being and cognitive development among children exposed to more green space (16, 25). The relation to cognitive development found by Dadvand et al. (16) was partly mediated by air pollution, and this result is supported by other studies on air pollution and psychiatric disorders (29, 30). The role of green spaces as natural filters of environmental pollution should be investigated further in relation to psychiatric disorders. Another promising hypothesis is that exposure to green space, especially biodiverse green space, and animal contact lead to better immune functioning, which has been linked to mental health (22, 31). Training the human immune systems seemingly requires prolonged exposure to microbiota during childhood (22), consistent with our finding of accumulative associations with green space presence. For neurodevelopmental disorders, such as intellectual disability and schizophrenia, poor immune functioning and consequently greater risk of infections could explain some of the association with green space.
Although we found a strong association between green space and psychiatric disorder risk, our study also has some limitations. At this point, we cannot completely dismiss that choice of residential location is somewhat affected by genetic confounding. A recent study using polygenic risk scores showed that people with higher genetic loading for schizophrenia lived in denser urban areas (32). However, another study for Denmark showed that the association between urbanicity and the risk of schizophrenia was not explained by genetic liability (33). Hence, the association between green space and mental health is unlikely to be entirely driven by genetically determined choice of residential location, but gene−environment interactions could still play a role. Selection bias from parents of higher socioeconomic status choosing to move to greener areas could also influence the results, although, for schizophrenia, selective migration has been shown to only partly explain the association in Denmark (34). Although we adjusted for municipal and parents’ socioeconomic status, our results may be influenced by unmeasured socioeconomic factors such as lower-quality green space, higher crime rates, and fewer social advantages in deprived neighborhoods.
These limitations point to several follow-up questions. First, the deviations from the general dose–response relationship warrant further studies into the epidemiology of certain psychiatric disorders such as alcohol abuse, anorexia, and intellectual disability. Second, despite the strong longitudinal design of our study, our risk estimates fundamentally only show correlations. Causation is generally hard to infer from observational studies and is difficult to prove when the etiology of psychiatric disorders is unknown (35). New knowledge from genetic and neurobiological research (e.g., refs. 17 and 36) could guide future combinations of longitudinal and experimental studies. Third, the mechanistic links between green space and psychiatric disorders remain to be identified. Using NDVI from satellite images allowed us to estimate individual-level green space presence at a fine resolution but captured no information about other aspects of natural environments such as blue space, biodiversity, the presence of animals, or quality of vegetation. Also, NDVI provides no information about the use of green space. Effects of different qualitative aspects and use of green space is important to identify a possible mechanistic link (37). Restorative environment studies assessing the positive, restoration-promoting (i.e., salutogenic) characteristics of green space in combination with the absence of risk factors such as noise and pollution are promising ways to determine whether and how natural environments provide benefits that promote mental health (38). Tracking people’s use of green space through GPS (39) or possibly through social media could provide more information about pathways related to use of green space.
Our results complement other studies showing positive associations between nature and mental health (19–21, 23, 24), while showing a consistent, protective association with individual-level childhood green space presence for many of a spectrum of psychiatric disorders after adjusting for urbanization and covering a large proportion of the population. As shown by the dose–response relationship between green space presence and psychiatric disorder risk, we found no sign of the positive association with green space reaching an upper limit. Hence, finding ways to provide high green space exposure during childhood should be encouraged in sustainable urban planning. Population attributable risk estimates suggest that green space might contribute large health benefits across the population. Future studies should address the extent to which benefits arise from passive exposure versus active use, and whether the source of benefits differs for different psychiatric disorders. Cumulated green space presence was more strongly associated with risk, and this should be considered in future studies of green space effects on mental health.
In conclusion, our data show a consistent association between higher levels of green space during childhood and a lower risk of developing any of a multitude of psychiatric disorders later in life. These findings contribute to our understanding of the urban environment as an important environmental risk factor for mental health and can guide the design of healthy city environments, as well as institutions and programs affecting childhood life, for example, school systems. Ensuring access to green space and enhancing opportunities for a diverse range of uses, especially in densifying urban environments, could be an important tool for managing and minimizing the global burden of disease increasingly dominated by psychiatric disorders. Lower access to green space could be an added risk factor for mental health among vulnerable groups of society (40, 41). Loss of human−nature interactions presents a health risk, and it can also reduce peoples’ appreciation of natural environments, creating negative feedback loops (42). In contrast, positive experiences, such as psychological restoration or social cohesion, can motivate positive ecological behaviors (43). Increasing urban nature could potentially provide mental health benefits while simultaneously protecting biodiversity and ecosystem services of natural environments.
Methods
Study Population and Assessment of Psychiatric Disorders.
Denmark is a small, relatively homogeneous country with a population of 5.8 million people and a total area of about 43,000 km2. Distances within the country are small, with most people living within 25 km of a city with >30,000 inhabitants and a psychiatric hospital or department. The Danish Civil Registration System was established in 1968 and contains a personal identification number (PIN) and information on gender, place of birth, vital status, parents’ PINs, and continuously updated information on vital status and place of residence for all Danish citizens. All national registers use the PIN, linking each individual to all other national registers, e.g., containing information on health, contextual, and socioeconomic information. The study population included all persons born in Denmark from 1985 to 2003 and who were alive and residing in Denmark at their 10th birthday (943,027 persons).
We linked all individuals from the study population and their parents and siblings with the Danish Psychiatric Central Research Register (44) to obtain information about psychiatric disorders. The Register contains information on all admissions to Danish psychiatric in-patient facilities since April 1, 1969, and, since 1995, all out-patient visits to psychiatric departments or emergency care. There are no private psychiatric in-patient facilities in Denmark, and treatment is free. From 1969 to 1993, the diagnostics system used was the Danish modification of the International Classification of Diseases (ICD-8) (45) and, from 1994 and on, the ICD-10 (46). Individuals were classified with a psychiatric disorder if they had been admitted to a psychiatric facility, received outpatient care, or visited a psychiatric emergency care unit with a diagnosis of one of 18 psychiatric disorders (SI Appendix, Table S5). The date of onset was defined as the first contact at which any of the above-defined diagnoses were applied.
Quantification of Green Space.
We calculated mean green space covering the period of 1985 to 2013 from the NDVI, obtained from 30-m-resolution remote sensing images from the Landsat archive (earthexplorer.usgs.gov/, accessed February 2, 2016). NDVI is the difference between absorbed (red) and reflected (near-infrared) light by vegetation following
where NIR is the near-infrared and RED is the red band. NDVI is a commonly used and effective measure of green space (47, 48). Low values indicate sparse vegetation, and high values indicate dense vegetation.
The Landsat archive contains satellite data of Earth acquired by six satellites over more than 40 y. Over the years, the purpose and spatial focus of the Landsat program has changed, and, as a result, the availability of the data varies. The Landsat satellites provide images of 4 to 11 bands at 30- to 120-m resolution on a 16- to 18-d revisit cycle. We aimed to obtain images from the growing season in June, July, or August with none to low cloud cover for the entire country each year. The best data coverage comes from the later years, whereas data availability of the earliest years fluctuates. For example, the satellite images from 1978 to 1983 only cover parts of Zealand and the island of Bornholm. Also, due to technical difficulties, some years in the time period are only partly covered or not covered at all (see SI Appendix, Table S6 for details of each year).
All Landsat images were atmospherically corrected and converted to Top of Atmosphere (TOA) reflectance using ENVI version 5.1 to remove atmospheric effects from water vapor and the position of the Sun. Despite our best efforts to find cloud-free images, some images were partly covered by clouds. For images with severe cloud cover (∼5 to 30%), we downloaded several images covering the same area at different dates and merged them to obtain a single complete image. Clouds were identified and masked loosely following a previously published approach (49). Clouds on images from Landsat 8 (only for year 2013) were identified and masked using the Quality Assessment band. Manual assessment revealed an acceptable match between the cloud masks and clouds on the images, although with slight imprecisions with unidentified thin clouds (hazes) and small patches of bare soil wrongly identified as clouds. Lastly, all images were processed with histogram matching using the best (low cloud cover and large land area) image for each year, and large water bodies were masked out before calculating NDVI. The NDVI maps for Denmark can be downloaded from https://bios.au.dk/en/about-bioscience/organisation/ecoinformatics-and-biodiversity/data/.
NDVI images were mosaicked into a single image for each year with bilinear interpolation. Missing values were interpolated using simple linear interpolation for cells with a minimum of three measurements across all years. The mean of the NDVI values was then calculated for quadratic areas (presence zones) of 210 × 210 m, 330 × 330 m, 570 × 570 m, and 930 × 930 m (7, 11, 19, and 31 cells, respectively) around each address for the years 1985–2013. Cumulated NDVI is the mean of mean NDVI from birth to the 10th birthday for each cohort member with at least 10 y of observations. As the Danish residence database is continuously updated, NDVI values for each residence were used for children that moved within the 10-y timespan. Unless stated otherwise, we refer to estimates from green space presence measured on the year of the 10th birthday, when children are relatively independent and likely to be exposed to surrounding green space through outdoor activities. For each presence zone, place of residence was located in the center of the quadrat. Calculating the mean of the NDVI for this large number of addresses was a challenging computational task. Therefore, we performed these computations using efficient algorithms to process large amounts of geographic data within a reasonable amount of time (50).
Statistical Analyses.
Cohort members were followed for the development of psychiatric disorders from their 10th birthday until first treatment contact for any of the psychiatric disorders, death, emigration from Denmark, or December 31, 2013, whichever came first. IRR of psychiatric disorders were estimated in time-to-event analyses using Cox regressions, using age as the underlying timescale with separate baselines for each gender (51). NDVI values were linked to each cohort member with the addresses. Mean NDVI at age 10 y was fitted as deciles for all four presence zone sizes, and cumulated NDVI was likewise fitted as deciles (cutoff values are presented in SI Appendix, Table S7). We adjusted models for potential confounding by other known risk factors identified by previous studies. Urbanization was fitted as a categorical variable with five levels: capital center, capital suburb, provincial city, provincial town, or rural area, as previously described (34). We controlled for a range of individual and socioeconomic confounding factors, including year of birth, gender, parents’ education (three levels: primary school, high school\vocational training, or higher education), parents’ income (gross income divided in quintiles and adjusted for inflation and gender differences), parents’ employment status (three levels: employed, unemployed, or outside workforce), parents’ age (seven levels: 12 y to 19 y, 20 y to 24 y, 25 y to 29 y, 30 y to 34 y, 35 y to 39 y, 40 y to 44 y, and 45 y or older), and parents’ previous diagnosis with any psychiatric disorder up to and including the child’s 10th birthday (two levels: yes or no) (52). We also controlled for differences in residential areas’ socioeconomic status at the smallest available administrative unit using the Danish municipalities. Many important political decisions are made at the municipal level, e.g., budgets for schools, parks, and early prevention action programs. Danish municipalities are also responsible for implementation of action programs and the practical management of schools and parks. We calculated a measure of socioeconomic deprivation for each municipality as the average income as defined above, the proportion of individuals with a low education level (primary school compared with high school or higher education), and the proportion of individuals outside the workforce (unemployed or outside workforce compared with employed). Estimates adjusted for each possible confounding factor separately are presented for easy comparison of each factor’s association and to avoid potential bias from overadjustment (SI Appendix, Fig. S1). The calendar year of the end of study for each cohort member was treated as a time-dependent variable to account for different hazard rates over time and categorized as 1995–2000, 2001–2005, 2006–2010, and 2011–2013. All other variables were treated as independent of time.
We performed the following sensitivity analyses to determine the best models for evaluating the association with NDVI by fitting additional Cox regressions: assessing (i) the association with different green space presence zone sizes (SI Appendix, Table S4), (ii) the potential modifying association of gender (SI Appendix, Table S8), (iii) the association with NDVI measured at different ages from birth to the 10th birthday (SI Appendix, Fig. S2), (iv) the potential modifying effect of urbanization (Figs. 1 and 2), and (v) the association with green space measured as mean cumulated NDVI from birth to the 10th birthday for each cohort member with observations for least 10 y out of 11 y (SI Appendix, Fig. S3). We calculated the population attributable risk from IRR to compare the magnitude of the associations with NDVI to other known risk factors. In the main text, unless stated otherwise, NDVI was measured within quadratic presence zones of 210 × 210 m at place of residence at the 10th birthday, as we found no strong difference in measuring green space of different presence zone sizes or when measured at other specific ages.
All data processing and statistics were performed in R (53) using packages data.table, Hmisc, landsat, lubridate, plyr, raster, rgdal, RStoolbox, sp, and survival. The only exception was the TOA conversion, performed using the ENVI software, version 5.1 (Exelis Visual Information Solutions). Data on the study population are not publicly available due to privacy protection. To request access to the data, contact P.B.M. at pbm@econ.au.dk.
Supplementary Material
Acknowledgments
We thank S. Nielsen and A. Pearcy for proofreading and comments on a previous draft of the manuscript. We thank M. Thygesen and A. Timmermann for data administrative help. This study was funded by the Stanley Medical Research Institute and the Centre for Integrated Register-based Research at Aarhus University. J.-C.S. considers this work a contribution to his VILLUM Investigator project (VILLUM FONDEN Grant 16549).
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission. T.H. is a guest editor invited by the Editorial Board.
Data deposition: The NDVI maps used to estimate green space presence are available for download at https://bios.au.dk/en/about-bioscience/organisation/ecoinformatics-and-biodiversity/data.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1807504116/-/DCSupplemental.
References
- 1.United Nations, Department of Economic and Social Affairs, Population Division 2014 World urbanization prospects: The 2014 revision, highlights (ST/ESA/SER.A/352). Available at https://esa.un.org/unpd/wup/Publications/Files/WUP2014-Highlights.pdf. Accessed February 15, 2019.
- 2.Dye C. Health and urban living. Science. 2008;319:766–769. doi: 10.1126/science.1150198. [DOI] [PubMed] [Google Scholar]
- 3.Lambert KG, Nelson RJ, Jovanovic T, Cerdá M. Brains in the city: Neurobiological effects of urbanization. Neurosci Biobehav Rev. 2015;58:107–122. doi: 10.1016/j.neubiorev.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lederbogen F, et al. City living and urban upbringing affect neural social stress processing in humans. Nature. 2011;474:498–501. doi: 10.1038/nature10190. [DOI] [PubMed] [Google Scholar]
- 5.Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr Scand. 2010;121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- 6.Vassos E, Agerbo E, Mors O, Pedersen CB. Urban-rural differences in incidence rates of psychiatric disorders in Denmark. Br J Psychiatry. 2016;208:435–440. doi: 10.1192/bjp.bp.114.161091. [DOI] [PubMed] [Google Scholar]
- 7.March D, et al. Psychosis and place. Epidemiol Rev. 2008;30:84–100. doi: 10.1093/epirev/mxn006. [DOI] [PubMed] [Google Scholar]
- 8.Mortensen PB, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med. 1999;340:603–608. doi: 10.1056/NEJM199902253400803. [DOI] [PubMed] [Google Scholar]
- 9.Vassos E, Pedersen CB, Murray RM, Collier DA, Lewis CM. Meta-analysis of the association of urbanicity with schizophrenia. Schizophr Bull. 2012;38:1118–1123. doi: 10.1093/schbul/sbs096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mortensen PB. Urban–rural differences in the risk for schizophrenia. Int J Ment Health. 2000;29:101–110. [Google Scholar]
- 11.Bratman GN, Hamilton JP, Hahn KS, Daily GC, Gross JJ. Nature experience reduces rumination and subgenual prefrontal cortex activation. Proc Natl Acad Sci USA. 2015;112:8567–8572. doi: 10.1073/pnas.1510459112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adli M, et al. Neurourbanism: Towards a new discipline. Lancet Psychiatry. 2017;4:183–185. doi: 10.1016/S2215-0366(16)30371-6. [DOI] [PubMed] [Google Scholar]
- 13.Shanahan DF, et al. Health benefits from nature experiences depend on dose. Sci Rep. 2016;6:28551. doi: 10.1038/srep28551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maas J, et al. Morbidity is related to a green living environment. J Epidemiol Community Health. 2009;63:967–973. doi: 10.1136/jech.2008.079038. [DOI] [PubMed] [Google Scholar]
- 15.Engemann K, et al. Childhood exposure to green space—A novel risk-decreasing mechanism for schizophrenia? Schizophr Res. 2018;199:142–148. doi: 10.1016/j.schres.2018.03.026. [DOI] [PubMed] [Google Scholar]
- 16.Dadvand P, et al. Green spaces and cognitive development in primary schoolchildren. Proc Natl Acad Sci USA. 2015;112:7937–7942. doi: 10.1073/pnas.1503402112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kühn S, et al. In search of features that constitute an “enriched environment” in humans: Associations between geographical properties and brain structure. Sci Rep. 2017;7:11920. doi: 10.1038/s41598-017-12046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alcock I, White MP, Wheeler BW, Fleming LE, Depledge MH. Longitudinal effects on mental health of moving to greener and less green urban areas. Environ Sci Technol. 2014;48:1247–1255. doi: 10.1021/es403688w. [DOI] [PubMed] [Google Scholar]
- 19.Hartig T, Mitchell R, de Vries S, Frumkin H. Nature and health. Annu Rev Public Health. 2014;35:207–228. doi: 10.1146/annurev-publhealth-032013-182443. [DOI] [PubMed] [Google Scholar]
- 20.James P, Banay RF, Hart JE, Laden F. A review of the health benefits of greenness. Curr Epidemiol Rep. 2015;2:131–142. doi: 10.1007/s40471-015-0043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Twohig-Bennett C, Jones A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ Res. 2018;166:628–637. doi: 10.1016/j.envres.2018.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rook GA. Regulation of the immune system by biodiversity from the natural environment: An ecosystem service essential to health. Proc Natl Acad Sci USA. 2013;110:18360–18367. doi: 10.1073/pnas.1313731110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fong KC, Hart JE, James P. A review of epidemiologic studies on greenness and health: Updated literature through 2017. Curr Environ Health Rep. 2018;5:77–87. doi: 10.1007/s40572-018-0179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van den Berg M, et al. Health benefits of green spaces in the living environment: A systematic review of epidemiological studies. Urban For Urban Green. 2015;14:806–816. [Google Scholar]
- 25.McCormick R. Does access to green space impact the mental well-being of children: A systematic review. J Pediatr Nurs. 2017;37:3–7. doi: 10.1016/j.pedn.2017.08.027. [DOI] [PubMed] [Google Scholar]
- 26.Wells NM, Evans GW. Nearby nature: A buffer of life stress among rural children. Environ Behav. 2003;35:311–330. [Google Scholar]
- 27.Sarkar C, Webster C, Gallacher J. Residential greenness and prevalence of major depressive disorders: A cross-sectional, observational, associational study of 94 879 adult UK biobank participants. Lancet Planet Health. 2018;2:e162–e173. doi: 10.1016/S2542-5196(18)30051-2. [DOI] [PubMed] [Google Scholar]
- 28.Mitchell R, Popham F. Greenspace, urbanity and health: Relationships in England. J Epidemiol Community Health. 2007;61:681–683. doi: 10.1136/jech.2006.053553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Attademo L, Bernardini F, Garinella R, Compton MT. Environmental pollution and risk of psychotic disorders: A review of the science to date. Schizophr Res. 2017;181:55–59. doi: 10.1016/j.schres.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 30.Oudin A, Bråbäck L, Åström DO, Strömgren M, Forsberg B. Association between neighbourhood air pollution concentrations and dispensed medication for psychiatric disorders in a large longitudinal cohort of Swedish children and adolescents. BMJ Open. 2016;6:e010004. doi: 10.1136/bmjopen-2015-010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Böbel TS, et al. Less immune activation following social stress in rural vs. urban participants raised with regular or no animal contact, respectively. Proc Natl Acad Sci USA. 2018;115:5259–5264. doi: 10.1073/pnas.1719866115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Colodro-Conde L, et al. Association between population density and genetic risk for schizophrenia. JAMA Psychiatry. 2018;75:901–910. doi: 10.1001/jamapsychiatry.2018.1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paksarian D, et al. The role of genetic liability in the association of urbanicity at birth and during upbringing with schizophrenia in Denmark. Psychol Med. 2018;48:305–314. doi: 10.1017/S0033291717001696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pedersen CB. Persons with schizophrenia migrate towards urban areas due to the development of their disorder or its prodromata. Schizophr Res. 2015;168:204–208. doi: 10.1016/j.schres.2015.08.028. [DOI] [PubMed] [Google Scholar]
- 35.Miller G. Mysteries of the brain. Why is mental illness so hard to treat? Science. 2012;338:32–33. doi: 10.1126/science.338.6103.32. [DOI] [PubMed] [Google Scholar]
- 36.Sekar A, et al. Schizophrenia Working Group of the Psychiatric Genomics Consortium Schizophrenia risk from complex variation of complement component 4. Nature. 2016;530:177–183. doi: 10.1038/nature16549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Markevych I, et al. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ Res. 2017;158:301–317. doi: 10.1016/j.envres.2017.06.028. [DOI] [PubMed] [Google Scholar]
- 38.von Lindern E, Lymeus F, Hartig T. The restorative environment: a complementary concept for salutogenesis studies. In: Mittelmark MB, et al., editors. The Handbook of Salutogenesis. Springer; New York: 2017. pp. 181–195. [PubMed] [Google Scholar]
- 39.Dewulf B, et al. Associations between time spent in green areas and physical activity among late middle-aged adults. Geospat Health. 2016;11:411. doi: 10.4081/gh.2016.411. [DOI] [PubMed] [Google Scholar]
- 40.Cabrera LY, Tesluk J, Chakraborti M, Matthews R, Illes J. Brain matters: From environmental ethics to environmental neuroethics. Environ Health. 2016;15:20. doi: 10.1186/s12940-016-0114-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wolch JR, Byrne J, Newell JP. Urban green space, public health, and environmental justice: The challenge of making cities ‘just green enough.’. Landsc Urban Plan. 2014;125:234–244. [Google Scholar]
- 42.Soga M, Gaston KJ. Extinction of experience: The loss of human-nature interactions. Front Ecol Environ. 2016;14:94–101. [Google Scholar]
- 43.Hartig T, Kaiser FG, Strumse E. Psychological restoration in nature as a source of motivation for ecological behaviour. Environ Conserv. 2007;34:291–299. [Google Scholar]
- 44.Mors O, Perto GP, Mortensen PB. The Danish psychiatric central research register. Scand J Public Health. 2011;39(7 Suppl):54–57. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- 45.World Health Organization . International Statistical Classification of Diseases and Related Health Problems (ICD-8) World Health Org; Geneva: 1967. [Google Scholar]
- 46.World Health Organization . The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostics Guidelines. World Health Org; Geneva: 1992. [Google Scholar]
- 47.Rhew IC, Vander Stoep A, Kearney A, Smith NL, Dunbar MD. Validation of the normalized difference vegetation index as a measure of neighborhood greenness. Ann Epidemiol. 2011;21:946–952. doi: 10.1016/j.annepidem.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lo C. Integration of landsat thematic mapper and census data for quality of life assessment. Remote Sens Environ. 1997;62:143–157. [Google Scholar]
- 49.Martinuzzi S, Gould W, González O. 2007. Creating cloud-free Landsat ETM+ data sets in tropical landscapes: Cloud and cloud-shadow removal (US Dep Agric, Portland, OR), General Technical Report IITF-GTR-32.
- 50.Arge L, Haverkort H, Tsirogiannis C. Proceedings of the 20th ACM SIGSPATIAL International Conference on Advances in Geographic Information Systems (ACM GIS) ACM Press; New York: 2012. Fast generation of multiple resolution instances of raster data sets; pp. 52–60. [Google Scholar]
- 51.Andersen PK, Gill RD. Cox ’s regression model for counting processes : A large sample study. Ann Stat. 1982;10:1100–1120. [Google Scholar]
- 52.Danmarks Statistik . IDA–En Integreret Database for Arbejdsmarkedsforskning: Hovedrapport. Denmark Stat; Copenhagen: 1991. [Google Scholar]
- 53.R Development Core Team 2013. R: A language and environment for statistical computing (R Foundation for Statistical Computing, Vienna), Version 3.5.1.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.