Abstract
Background:
Severe coal workers’ pneumoconiosis (CWP) is increasingly common, and sometimes requires lung transplantation.
Methods:
Using Organ Procurement and Transplantation Network data, we updated the trend for CWP-related lung transplants, described CWP patients who have been waitlisted but not transplanted, and characterized the primary payer of medical costs for CWP-related and other occupational lung disease transplants.
Results:
There have been at least 62 CWP-related lung transplants; 49 (79%) occurred in the last decade. The rate of these procedures has also increased. Twenty-seven patients were waitlisted but did not receive a transplant. Compared to other occupational lung diseases, transplants for CWP were more likely to be paid for by public insurance.
Conclusions:
The increase in the frequency and rate of lung transplantation for CWP is consistent with the rising prevalence of severe CWP among U.S. coal miners. Effective exposure controls and identification of early stage CWP remain essential for protecting these workers.
Keywords: coal workers’ pneumoconiosis, lung transplantation, occupational lung disease, Organ Procurement and Transplantation Network
1. INTRODUCTION
Since the first lung transplant for coal workers’ pneumoconiosis (CWP) was performed in 1996, the procedure has become increasingly common among miners with end-stage CWP, with median post-transplant survival estimated to be 3.7 years.1 The average medical cost for a bilateral lung transplant performed in the United States is $1.2 million for the period including 1 month before transplantation, through 6 months afterwards.2 The increasing trend in lung transplantation has coincided with a resurgence, since approximately 2000, of severe CWP identified among working coal miners in Appalachia,3 and with a growing literature implicating crystalline silica exposure in the rapid progression of CWP in contemporary coal miners.4–6 Subsequent reports have identified the largest documented clusters of progressive massive fibrosis, the most severe form of CWP, primarily among former coal miners who worked in the central Appalachian coalfields.7,8
Coal mine dust is the only cause of CWP, which has no cure, and can continue to progress after dust exposure ends.9 For miners with severe CWP, lung transplantation might be indicated. In light of the high medical and personal cost of lung transplantation, and the recent resurgence of progressive massive fibrosis, we re-analyzed U.S. organ transplant registry data to provide an update on the lung transplantation trend1 among patients with CWP, using an additional 2.5 years of data. We also described patients with a diagnosis of CWP who have been added to a transplant waitlist, but who have not undergone the procedure. Finally, to improve our understanding of which entities finance lung transplantation for patients with CWP and other occupational lung diseases, we assessed the primary payer of medical costs for each patient.
2. METHODS
We analyzed de-identified patient data compiled by the United Network for Organ Sharing (UNOS), which administers the Organ Procurement and Transplantation Network (OPTN), a registry of organ transplant-related events. We previously analyzed OPTN data to assess the frequency and possible misclassification of CWP and other occupational lung diseases.1,10 For the current analysis, the data included all lung transplant waitlist registrations and lung transplantations (single and bilateral) listed or performed in the United States during October 1, 1987-June 30, 2017, and we restricted analysis to adult (>18 years) recipients. Our organization determined that this activity did not involve human subjects, and thus did not require Institutional Review Board review.
Although OPTN is designed to record both numeric and free text diagnoses at patient listing and at transplantation, for some common indications, such as cystic fibrosis, only a numeric code is entered. For certain broader indications, such as occupational lung disease, the corresponding numeric code includes the phrase “other specify” to prompt entry of a specific free text diagnosis. However, querying numeric codes to then screen for more specific conditions (such as selecting patients with the occupational lung disease code, and then identifying those with a free text diagnosis specifying coal workers’ pneumoconiosis), will result in missed cases. A previous analysis we completed using OPTN data found that nearly half of lung transplant recipients with a specified free text diagnosis of an occupational lung disease (eg, CWP, silicosis, asbestosis) were not assigned an occupational lung disease numeric code.10 Thus, a substantial number of occupational disease cases would be missed if the numeric code was the only variable used for case finding. For patients who received a lung transplant, we examined the primary diagnosis specified at the time of transplant, and included those with a primary diagnosis of CWP (including those with alternate wordings, for example, “coal miner’s pneumoconiosis”), and patients with a primary diagnosis of pneumoconiosis unspecified (prior research suggests a majority of these cases are likely CWP1). We calculated the rate of lung transplantation for CWP and pneumoconiosis unspecified, relative to all adult lung transplants, during consecutive time periods, and the ratio and confidence interval for these rates. For patients who were placed on a waitlist, but who had not received a lung transplant by the end of the study period, we examined the diagnosis specified at the time of listing, and included patients with a diagnosis of CWP, and those with pneumoconiosis unspecified.
To characterize the primary payer of medical costs associated with completed and planned lung transplants for CWP patients, we identified the primary source of payment for lung transplant recipients, and the primary projected source of payment for patients on a waitlist. Additionally, we identified patients who received a lung transplant for all other occupational lung diseases combined, and compared the primary payer for these patients with those who had a diagnosis of CWP. Payment source categories included private insurance, public insurance, U.S. or state government agency, free care, and self-payment. The public insurance category included Medicaid, Medicare Fee for Service, “Medicare + Choice” (renamed “Medicare Advantage” in 2003), Medicare not specified, Department of Veteran’s Affairs, and “other government insurance.”
3. RESULTS
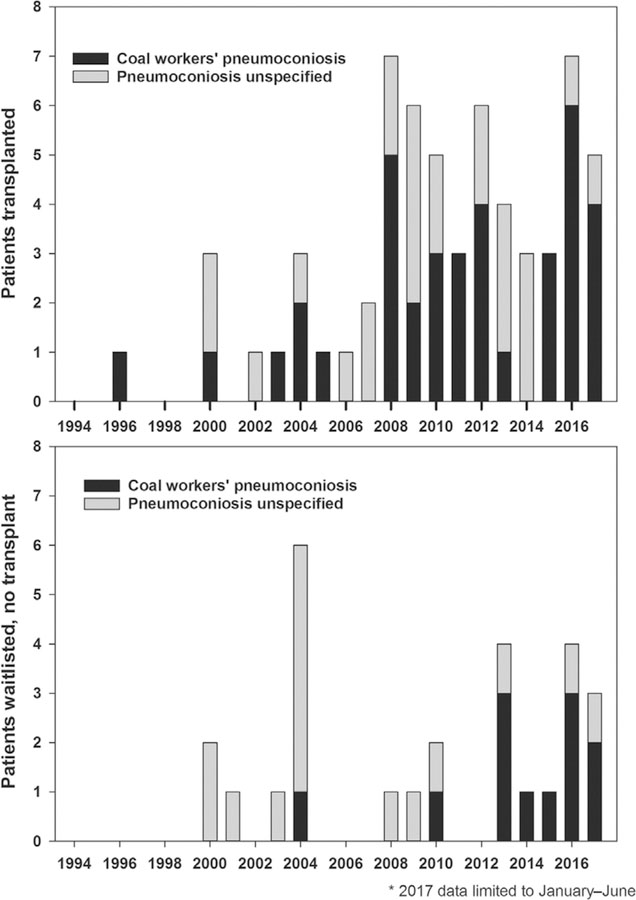
We identified 62 patients with a diagnosis of CWP (n = 37) or pneumoconiosis unspecified (n = 25; hereafter, pneumoconiosis unspecified is combined with CWP) who underwent lung transplantation during 1994–2017 (Figure 1). Each of these patients was male, mean age at transplant was 56.8 years (range: 41–69 years), and 49 (79.0%) lived in West Virginia, Kentucky, or Virginia. Approximately one-quarter (n = 15, 24.2%) of all lung transplants completed for CWP occurred during the 2.5 years since the previous report1; 49 (79.0%) have occurred during the last decade. During 2007-June 2017, lung transplants were performed for patients with CWP at a rate of 2.68 per 1000 adult transplants; during 1996–2006 the rate was 0.98 per 1000 (RR = 2.73, 95% CI: 1.42, 5.23). Since 2000, a total of 27 patients (mean age = 55.6 years, range: 42–70 years) with a diagnosis of CWP were placed on a waitlist, but had not received a lung transplant as of June 30, 2017. Of these patients, 11 died while on the waitlist, five were still waiting at the end of follow-up (mean duration = 228 days), four became not healthy enough for transplantation, two improved and transplantation was no longer necessary, and five were removed from the waitlist for an unspecified reason.
FIGURE 1.
Frequency of lung transplant in patients with a primary diagnosis at time of transplant of coal workers’ pneumoconiosis or pneumoconiosis unspecified, defined as a patient listed with a free-text diagnosis of pneumoconiosis without additional specification (top frame); frequency of lung transplant waitlist addition for patients with a diagnosis of coal workers’ pneumoconiosis or pneumoconiosis unspecified, as specified at time of waitlist addition (bottom frame), United States, January 1994-June 2017*
Among the 143 lung transplant recipients with occupational lung diseases other than CWP, 137 (95.8%) were male, mean age at transplant was 54.1 years (range: 22–72 years), and the most common states of residence were Texas (n = 17), Pennsylvania (n = 15), and Ohio (n = 11). Public insurance was more likely to be the primary payer of medical costs for patients with CWP (Table 1), compared with those with other occupational lung diseases (64.5% vs 40.7%, p = 0.002); much of this difference is accounted for by Medicare Advantage and “other government insurance.”
TABLE 1.
Primary source of payment for medical expenses associated with lung transplantation for coal workers’ pneumoconiosis and other occupational lung diseases, United States, January 1987-June 2017
| Primary source of payment | CWPa, n (%) | All other occupational lung diseaseb, n (%) |
|---|---|---|
| Public insurance | 40 (64.5)c | 57 (40.7) |
| Medicaid | 0 (0) | 3 (2.1) |
| Medicare fee for service | 6 (9.7) | 22 (15.7) |
| Medicare + choiced | 16 (25.8) | 11 (7.9) |
| Medicare, no additional detail | 2 (3.2) | 10 (7.1) |
| Dept. of Veteran’s Affairs | 1 (1.6) | 2 (1.4) |
| Other government insurance | 15 (24.2) | 9 (6.4) |
| Private insurance | 21 (33.9) | 75 (53.6) |
| U.S./State government agency | 1 (1.6) | 6 (4.3) |
| Total | 62 (100) | 140e (100) |
Includes patients with CWP and pneumoconiosis unspecified.
Includes asbestosis, berylliosis, metal pneumoconiosis, silicosis, and other occupational lung disease.
Public insurance more likely to be primary source of payment for patients with CWP compared to those with all other occupational lung diseases combined (P = 0.002).
Renamed “Medicare Advantage” in 2003.
Three patients with “all other occupational lung disease” had missing payer data.
4. DISCUSSION
During the last two decades, at least 89 U.S. men with a diagnosis of CWP have been placed on a lung transplant waitlist, and at least 62 of those have received a transplant. The rate of lung transplantation for CWP has also increased significantly in recent years. Among the 27 CWP patients who were waitlisted but had not received a transplant by the end of the study period, more than half were because they had died while waiting, or were too ill to undergo surgery. Previous registry-based studies have characterized the burden of severe CWP by highlighting lung transplant recipients,1,11 but we are unaware of any published reports describing patients who were waitlisted but have not received a transplant. These patients also have severe, end-stage disease that should be acknowledged. Five of the patients who were waitlisted but had not yet received a lung transplant were still waiting at the end of the study period, and it is possible that some of these patients have since undergone lung transplantation. Although OPTN includes some information on payer type, the relatively high proportion of CWP transplants paid for by public insurance programs—and notably “other government insurance,” which likely includes the Black Lung Disability Trust Fund (which pays for CWP claims when no responsible mine operator can be identified)—merits additional attention. We confirmed with UNOS that more specific payer information were not available in the registry data.
The primary goals of collecting and maintaining information on transplant donors and recipients are to assure best use of the limited supply of donor organs, improve post-transplant survival, and protect patient safety. As such, the OPTN registry was not designed for public health surveillance, and there are limitations to using these data for that purpose. Because patient industry and occupation data are not captured in the system, it is likely that not all patients with a designation of “pneumoconiosis unspecified” had CWP. It is also likely that the number of cases of CWP recorded in OPTN does not reflect the true number of lung transplants performed for persons with respiratory disease caused by coal mining employment. In addition to CWP and other interstitial conditions such as mixed-dust pneumoconiosis and dust-related diffuse fibrosis, exposure to coal mine dust can also cause chronic obstructive pulmonary disease (COPD) including emphysema and chronic bronchitis. Some coal miners with severe COPD caused by workplace exposure could have been assigned to this diagnosis group without occupational attribution. Silicosis was the leading indication for lung transplants among patients listed with other occupational lung diseases, and it is possible that coal miners with interstitial lung disease resulting from their employment were included in this category. However, we identified CWP cases using the most detailed diagnosis information available in the database, and the lung transplant trend reported is consistent with rising levels of CWP morbidity and black lung compensation claims.12
Coal workers’ pneumoconiosis is completely preventable and would not occur without hazardous coal mine dust exposures. Recent reports documenting high levels of CWP and progressive massive fibrosis in Appalachian coal miners demonstrate that the burden of this disease continues to increase, which will likely influence future demand for lung transplantation among coal miners.8 During 2014–2016, additional measures to reduce coal mine dust exposures, and to detect early signs of dust-related lung disease, were enacted to improve protections for all U.S. coal miners.13,14 In December 2017, a request for information was filed by the Department of Labor soliciting public comment on existing standards and regulations.15 Although it is too early to assess the health impact of these recent primary and secondary prevention measures, contemporary scientific findings demonstrate that effective dust exposure prevention remains essential for all U.S. coal miners. Ongoing health surveillance will be needed to monitor respiratory health trends over time.
ACKNOWLEDGMENTS
The authors thank Randy Nett, MD, and Brent Doney, PhD, for their thoughtful and constructive reviews of this manuscript.
FUNDING
The authors report that there was no funding source for this work that resulted in the article or the preparation of the article.
DISCLAIMER
This work was supported in part by Health Resources and Services Administration contract 234–2005-370011C. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Footnotes
ETHICS APPROVAL AND INFORMED CONSENT
The National Institute for Occupational Safety and Health determined this activity does not require institutional review board review because the data were collected for another purpose and the investigator cannot readily ascertain the identities of the individuals to whom the data pertain (16-RHD-NR01).
DISCLOSURE (AUTHORS)
The authors disclose no conflicts of interest.
DISCLOSURE BY AJIM EDITOR OF RECORD
Steven B. Markowitz declares that he has no conflicts of interest in the review and publication decision regarding this article.
Institution at which the work was performed: National Institute for Occupational Safety and Health.
REFERENCES
- 1.Blackley DJ, Halldin CN, Cummings KJ, Laney AS. Lung transplantation is increasingly common among patients with coal workers’ pneumoconiosis. Am J Ind Med 2016;59:175–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bentley TS, Phillips SJ. 2017 U.S. organ and tissue transplant cost estimates and discussion. Milliman Research Report, August 2017. (Accessed 3/13/2018, at http://www.milliman.com/insight/2017/2017-U_S_-organ-and-tissue-transplant-cost-estimates-and-discussion/.).
- 3.Blackley DJ, Halldin CN, Laney AS. Resurgence of a debilitating and entirely preventable respiratory disease among working coal miners. Am J Respir Crit Care Med 2014;190:708–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laney AS, Petsonk EL, Attfield MD. Pneumoconiosis among underground bituminous coal miners in the United States: is silicosis becoming more frequent? Occup Environ Med 2010;67:652–656. [DOI] [PubMed] [Google Scholar]
- 5.Cohen RA, Petsonk EL, Rose C, et al. Lung pathology in US coal workers with rapidly progressive pneumoconiosis implicates silica and silicates. Am J Respir Crit Care Med 2016;193:673–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laney AS, Blackley DJ, Halldin CN. Radiographic disease progression in contemporary US coal miners with progressive massive fibrosis. Occup Environ Med 2017;74:517–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blackley DJ, Crum JB, Halldin CN, Storey E, Laney AS. Resurgence of progressive massive fibrosis in coal miners—Eastern Kentucky, 2006. MMWR Morb Mortal Wkly Rep 2016;65:1385–1389. [DOI] [PubMed] [Google Scholar]
- 8.Blackley DJ, Reynolds LE, Short C, et al. Progressive massive fibrosis in coal miners from 3 clinics in Virginia. J Am Med Assoc 2018;319: 500–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petsonk EL, Rose C, Cohen R. Coal mine dust lung disease. New lessons from an old exposure. Am J Respir Crit Care Med 2013;187: 1178–1185. [DOI] [PubMed] [Google Scholar]
- 10.Blackley DJ, Halldin CN, Cohen RA, et al. Misclassification of occupational disease in lung transplant recipients. J Heart Lung Transplant 2017;36:588–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Enfield KB, Floyd S, Barker B, et al. Survival after lung transplant for coal workers’ pneumoconiosis. J Heart Lung Transplant 2012;31: 1315–1318. [DOI] [PubMed] [Google Scholar]
- 12.Claims filed under part C of the Black Lung Benefits Act, 2001–2017 (Accessed 1/12/2018, at https://www.dol.gov/owcp/dcmwc/statistics/PartCClaimsFiled.htm.).
- 13.Department of Labor. Lowering miners’ exposure to respirable coal mine dust, including continuous personal dust monitors. Fed Regist 2014:24814–24994.
- 14.Department of Health and Human Services. Specifications for medical examinations of coal miners. Fed Regist 2016:73270–73290.
- 15.Department of Labor. Regulatory Reform of Existing Standards and Regulations; Retrospective Study of Respirable Coal Mine Dust Rule. http://Reginfo.gov, 2017.