Abstract
Medications may lessen core symptoms of attention deficit hyperactivity disorder (ADHD), yet families continue to report stress and have a low quality of life. Primary care providers manage almost half of all children with ADHD but do not have a brief measure to assess ADHD impacts on family in the context of everyday family life. The IMPACT (Impact Measure of Parenting-Related ADHD Challenges and Treatment) 1.0 Scale was codeveloped with input from parent advisors and administered to 79 parents of children with ADHD. Exploratory factor analysis, correlations with validated instruments, and test-retest reliability were examined. Exploratory factor analysis resulted in 4 subscales (Misbehavior, Siblings, Time, School), which demonstrated moderate to high test-retest reliability. Scale domains were related to severity and change in ADHD symptoms. Significant correlations were found between IMPACT scores, adaptive functioning in the home, and ADHD-related quality of life. The IMPACT 1.0 Scale provides a novel, reliable, and valid method to assess family impact of ADHD.
Keywords: primary care, quality of life, pediatrics, measurement, patient-centered outcomes
Introduction
Raising a child with attention deficit hyperactivity disorder (ADHD) can be stressful for parents. Core symptoms related to hyperactivity, impulsivity, and/or inattention create significant functional impairments at home and school. While stimulant medications can ameliorate symptoms of ADHD, families report ongoing stress related to everyday activities and a lower quality of life compared with those raising children without ADHD.1
Primary care providers are increasingly taking on primary management of almost half of all children with the diagnosis of ADHD.2,3 ADHD guidelines developed by professional organizations4,5 emphasize the importance of accurate diagnosis and use of well-established, relevant rating instruments.
The Vanderbilt ADHD Diagnostic Rating Scale (VADRS) is used in primary care to identify not only the core symptoms of ADHD but also its impact on the child’s daily functioning.6 The items focus on academic subjects and interpersonal relationships, with global items related to “relationship with parents” and “overall school performance.” These functional items expand the understanding of the child’s ADHD symptoms from core behaviors to the impact on daily functioning. Still, families report unmet needs not captured by broad functional categories.7 While some ADHD-related quality of life measurements evaluate specific areas of stress-related functional outcomes,8,9 these instruments are used mostly in research and not for clinical purposes. Brief tools to quickly identify areas of ADHD-related stress, problems, and daily functioning challenges during assessment and/or treatment visits to tailor treatment recommendations are lacking.
This study aimed to address this gap in clinical assessment of ADHD-related family stresses and daily functioning by developing a novel instrument for use in primary care settings. We implemented 2 phases to develop a scale with relevant content and strong psychometrics. The first phase was to determine key domains of ongoing stress for families and compare these domains to existing validated measures. The first phase uncovered the need for a new measurement tool suitable for primary care, and one was created by the team. The second phase was to assess whether this tool could be implemented in actual primary care settings and to understand how the domains measured by the tool relate to ADHD symptoms.
Methods
Participants
Three family advisors participating in a larger comparative effectiveness trial examining group visit care of ADHD in primary care agreed to participate in Phase I (Content Development). Advisors were from a subset of 21 families who (1) were willing to provide consultation on an ad hoc basis to the study team throughout the larger trial, (2) had a child aged 6 to 12 years old with ADHD, and (3) were enrolled in the larger study.
Participants in Phase II (Psychometrics) were composed of families who met study criteria and enrolled in the larger trial. Families were eligible if they received care at a participating study clinic and had a 6- to 12-year-old child with ADHD. Families were excluded if the child had a diagnosis of conduct disorder, autism, or moderate to severe intellectual disability that precluded active participation in group visit discussions. Families were assigned to receive ADHD follow-up care in a group setting or with providers receiving decision support mirroring clinical care guidelines based on the clinic attended; results are reported elsewhere.10 The focus of this article is on the development and psychometrics of the measure of family stresses related to ADHD impact. Institutional review board approval was obtained prior to the initiation of study procedures. All recruited participants provided written informed consent.
Measures
Impact Measure of Parenting-Related ADHD Challenges and Treatment (IMPACT) 1.0 Scale
The IMPACT 1.0 Scale is a parent-completed questionnaire of ADHD-related family stresses and challenges comprising 12 items. Although all 12 items on the scale were identified as domains of family stress that are exacerbated by ADHD symptoms, these 12 stress domains also occur in families of children who do not have ADHD. Therefore, families are asked to complete IMPACT 1.0 Scale items based on their general experiences, without making specific judgments about how much of each domain of stress is specifically/uniquely related to ADHD. This characteristic reduces subjective attribution of stress to ADHD versus other causes and allows for IMPACT 1.0 scores to be compared across families with ADHD and other diagnoses (or no diagnosis). Parents were asked to indicate whether the child was on medication at the time of completion. The final IMPACT 1.0 Scale consisted of 4 subscales related to Misbehavior, Siblings, Time, and School (see the appendix).
Vanderbilt ADHD Diagnostic Rating Scale
The VADRS is a screening tool for ADHD based on the Diagnostic Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria and used in primary care to identify and monitor ADHD symptoms.6 Symptom-based VADRS items fall onto 2 subscales: Inattention and Hyperactivity-Impulsivity. Parents rated symptoms on a 4-point Likert-type scale with 0 = never and 3 = very often. Severity was assessed as the sum of subscale items with higher scores indicating increasing severity.
Pediatric Quality of Life (PedsQL)
The PedsQL Scale is a caregiver-completed questionnaire to measure health-related quality of life.8 The PedsQL generic core scales contain 23 items and capture physical, emotional, social, and school functioning. Higher scores indicate better quality of life. For this study, the parent versions were administered.
Home Situations Questionnaire (HSQ)
The HSQ is a parent-completed questionnaire that assesses behavioral noncompliance across situations in the home, community, and school.11 Parents rate the presence of a particular problem behavior and, when present, rate the severity. A mean severity score is obtained based on a sum. Higher scores indicate higher severity and impairment.
Procedure
Phase I: Content Development
To understand ADHD-related stresses, family advisors were led through 2 activities (the “5 Whys” and “Distillation Game”) used in design research to engage participants quickly and easily. The “5 Whys” is an iterative technique to understand cause and effect relationships to uncover the perceived root cause of a problem.12 Each answer to the question “why” becomes the basis of the next round of questioning. Participants were asked to consider, “What specific things make it a good day for you in managing your child’s ADHD,” followed by, “Why does X make a day good?” Each subsequent response generated up to 4 additional “why” questions with each response written on post-it notes. The activity was allowed to go on for approximately 20 minutes to allow for multiple rounds of questioning. All responses were examined and grouped based on similarities. Each grouping became a domain. Participants were asked to pick the 5 domains deemed most important.
The second activity, the “Distillation Game,” utilizes techniques from popular party games such as Pictionary, Charades, and Taboo to facilitate expression of concepts in the simplest terms possible, such as one word, gesture, or image.13 These viewpoints are further probed to gain better understanding. Each of the 5 domains chosen at the end of the first activity was written on an index card, and cards were dealt to participants. Participants were asked to describe the domain on the card without using the printed words on the card, while other participants tried to guess what the card said. Cards were collected, shuffled, and dealt to participants. In rounds 2 and 3, the process was repeated but participants had to draw and then use only one word or sound to denote the domain on the card. In this way, the study team was able to better understand what parents saw as key indicators within each domain. For example, drawings for “child can cooperate with siblings” and “child can take part in family functions” both featured the child sitting and concentrating. The engagement session lasted 2 hours. The IMPACT Scale was derived based on findings and described in further detail below.
Phase II: Psychometrics
The IMPACT 1.0 Scale, along with the other measures, was administered to a total of 79 parents of children with ADHD participating in a larger comparative effectiveness trial of 2 different primary care–based interventions for ADHD. All measurement tools were administered at 2 time points: Baseline (T0) and 12 months after the initiation of intervention (T1).
Data Analysis
Phase I
The discovery session was audio-recorded and transcribed. Qualitative analysis of the data was based on Ackoff’s Data-Information-Knowledge-Wisdom scheme to distinguish between 4 different levels of sense making.14 Notes, along with materials generated in session (eg, images and text), were analyzed, and themes were extracted based on importance using a blend of research design and qualitative descriptive methodologies. Keywords were written on post-it notes, displayed visually on a wall for analysis, and coded by grouping items of significance into themes and hierarchies representing patient-centered domains of importance. Two members of the study team (CM and DL) compared domains generated to those captured in validated instruments, and disagreements were handled with input from 2 additional study team members (SEW and NSB). Several of the domains of familial importance were not adequately identified with the existing measurement tools, so a separate tool was developed to be piloted within the larger study.
Phase II
Descriptive statistics were calculated for all measures used in the study. To develop subscales for the IMPACT 1.0 Scale, exploratory factor analysis (EFA) was performed using the Time 0 (pre-intervention) data to generate groups of statistically related individual items. The number of components was selected using a combination of the Eigenvalue >1 convention, scree plot, and inspection of component loadings to produce the best differentiation of clusters of items. Loadings were examined following varimax rotation, and each item was assigned to the component with which it had the highest loading. Subscale scores were then developed by adding raw scores of constituent items on each component. Internal consistency values for subscales were calculated using T1 data, and test-retest reliability of subscales was examined using correlations of T0 and T1 data. Subscale validity and utility in ADHD assessment were investigated using Pearson correlations of IMPACT 1.0 subscale scores with other validated measures (HSQ, PedsQL) for T0, T1, and change (T1-T0).
Results
Phase I
Analysis of the discovery session led to identification of gaps in the measurement of patient-centered outcomes within proposed validated tools so a new scale was constructed, the IMPACT 1.0 Scale. A heuristic model of caregiver challenges and stress related to ADHD was developed to reflect these domains (Figure 1). The most salient themes that arose reflect challenges concerning Misbehavior (in public or with others during family events, during mealtimes); School (worries about negative perceptions from teachers and receiving calls from school); Time (perception of not having enough time for self, household duties, or other children); and Siblings (fighting or verbal arguments, not wanting to be around the child with ADHD, inability to work cooperatively). Themes mapped to domains not captured in existing tools were then used as the basis for scale item development, resulting in a 12-item scale. As noted earlier, the intent of the IMPACT 1.0 Scale was not to identify family stresses uniquely related to ADHD (eg, not present for other conditions or no diagnosis) but rather to identify family stresses specifically exacerbated by ADHD, as identified in the Phase I analysis. As such, all IMPACT 1.0 Scale items are present to some degree in all families but were rated as particularly stressful by families of children with ADHD. Each item was rated on a 5-point frequency scale with 0 = not at all to 5 = every day/almost every day; the 5-point scale was chosen to differentiate between levels of mild, moderate, and severe stress (which may not be detected on a 2- or 3-point scale) while also providing a small number of response options to facilitate rapid completion by parents.
Figure 1.
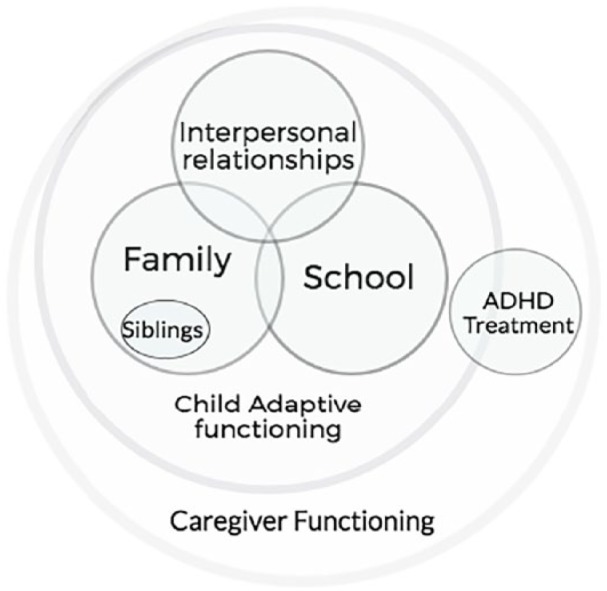
Heuristic model of caregiver challenges and stress related to attention deficit hyperactivity disorder.
Phase II
A total of 79 parents from diverse backgrounds had complete data for IMPACT items at T0. The sample characteristics are presented in Table 1. Sixty-eight subjects who had at least 9 non-missing items at T0 and T1 were included in the analysis of internal consistency and test-retest reliability. EFA of the 12 IMPACT 1.0 Scale items at T0 produced 4 factors based on Eigenvalue >1 and scree plot inspection. Varimax (orthogonal) rotation revealed a pattern of loadings supporting content for the following 4 subscales: Siblings, Misbehavior, Time, and School (Table 2). Factor analysis using Maximum Likelihood with Quartimin rotation was also explored, and similar patterns were found (data not shown). Subscale scores were created by adding raw scores for items assigned to each of the 4 factors. Internal consistency values for subscales were then calculated using T1 data, and test-retest reliabilities of subscales were examined using correlations of T0 and T1 data (see Table 2). Descriptive statistics for all measures used in the study, including the IMPACT subscale scores, are presented in Table 3.
Table 1.
Sample Characteristics (N = 79)a.
| Characteristics | Group Visit Condition (N = 46), n (%) | Individual Visit Condition (N = 33), n (%) |
|---|---|---|
| Child’s race | ||
| African American | 19 (41.3) | 28 (84.8) |
| White | 12 (26.1) | 4 (12.1) |
| Other | 15 (32.6) | 1 (3.0) |
| Child’s ethnicity | ||
| Hispanic | 17 (37.0) | 3 (9.1) |
| Child’s gender | ||
| Male | 34 (73.9) | 20 (60.6) |
| Child’s age | ||
| N (mean ± SD) | 42 (9.2 ± 1.8) | 25 (9.2 ± 2.1) |
| Total children in home | ||
| N (mean ± SD) | 37 (2.5 ± 1.3) | 31 (2.6 ± 1.3) |
| Child on medication T0 | ||
| Yes | 34 (73.9) | 28 (84.8) |
| Parent’s race | ||
| African American | 16 (34.8) | 23 (69.7) |
| White | 10 (21.7) | 7 (21.2) |
| Other | 20 (43.5) | 3 (9.1) |
| Parent’s ethnicity | ||
| Hispanic | 14 (35.9) | 3 (9.4) |
| Parent’s gender | ||
| Female | 38 (97.4) | 29 (93.5) |
| Parent’s preferred language | ||
| Spanish | 11 (23.9) | 0 (0.0) |
| Highest grade in school | ||
| High school or less | 26 (65.0) | 19 (59.4) |
| 2 year college+ | 9 (22.5) | 9 (28.1) |
| Other | 5 (12.5) | 4 (12.5) |
| Marital status | ||
| Married | 14 (35.9) | 8 (24.2) |
| Never married | 16 (41.0) | 17 (51.5) |
| Other | 9 (23.1) | 8 (24.2) |
| Health literacy (SILS) | ||
| Limited | 9 (19.6) | 3 (9.1) |
| Parent diagnosed/treated for ADHD | ||
| Yes | 3 (7.5) | 8 (24.2) |
Abbreviations: SILS, Single Item Literacy Screener; ADHD, attention deficit hyperactivity disorder.
Values may not equal 100% due to missing data.
Table 2.
Exploratory Factor Analysis (EFA) Loadings After Varimax Rotation.
| Component |
||||
|---|---|---|---|---|
| Item |
I |
II |
III |
IV |
| EFA Loadings | Siblings | Misbehavior | Time | School |
| Phone calls from school | 0.045 | 0.102 | −0.076 | 0.936 |
| Worry if teachers think negative of child | 0.078 | 0.337 | 0.467 | 0.473 |
| Misbehavior at social/family events | 0.082 | 0.790 | 0.213 | 0.228 |
| Misbehavior at meal times | 0.098 | 0.898 | 0.118 | −0.079 |
| Misbehavior in public | 0.058 | 0.877 | 0.140 | 0.155 |
| Feeling no time for other children | 0.440 | 0.363 | 0.545 | −0.070 |
| Feeling no times for yourself | 0.188 | 0.104 | 0.847 | 0.047 |
| Feeling no time for household duties | 0.158 | 0.170 | 0.877 | −0.051 |
| Physical fights with siblings | 0.831 | 0.043 | 0.207 | −0.036 |
| Verbal arguments with siblings | 0.851 | 0.0278 | 0.154 | 0.163 |
| Siblings do not want to be around child | 0.799 | 0.144 | 0.174 | −0.046 |
| Siblings cannot work together | 0.852 | 0.061 | 0.040 | 0.061 |
| Eigenvalue | 4.536 | 2.164 | 1.284 | 1.009 |
| Cronbach’s α at Time 1 | 0.858 | 0.931 | 0.849 | 0.640 |
| Mean (SD) at Time 0 | 7.3 (5.6) | 4.4 (3.4) | 4.4 (3.9) | 1.6 (1.8) |
| Mean (SD) at Time 1 | 6.8 (5.5) | 3.9 (3.6) | 3.3 (3.8) | 1.9 (2.2) |
| Test-retest correlation | 0.630*** | 0.497*** | 0.670*** | 0.639*** |
Bolded results indicate significance p<0.0001.
Table 3.
Descriptive Summary of Measures.
| T0, N = 68 | T1, N = 68 | Change (T1 − T0) | |
|---|---|---|---|
| IMPACT Sibling | |||
| Mean ± SD | 7.3 ± 5.6 | 6.9 ± 5.5 | −0.3 ± 4.7 |
| Median (Min, Max) | 7.0 (0.0, 20.0) | 6.0 (0.0, 20.0) | 0.0 (−20.0, 11.0) |
| IMPACT Misbehavior | |||
| Mean ± SD | 4.4 ± 3.4 | 3.9 ± 3.6 | −0.5 ± 3.6 |
| Median (Min, Max) | 3.0 (0.0, 12.0) | 3.0 (0.0, 12.0) | 0.0 (−9.0, 11.0) |
| IMPACT Time | |||
| Mean ± SD | 4.4 ± 3.9 | 3.3 ± 3.8 | −1.1 ± 3.2 |
| Median (Min, Max) | 3.0 (0.0, 12.0) | 1.5 (0.0, 12.0) | −0.5 (−9.0, 9.0) |
| IMPACT School | |||
| Mean ± SD | 1.6 ± 1.8 | 1.9 ± 2.2 | 0.2 ± 1.7 |
| Median (Min, Max) | 1.0 (0.0, 7.0) | 1.0 (0.0, 8.0) | 0.0 (−4.0, 7.0) |
| VADRS Hyperactive-Impulsive Symptom Severity | |||
| Mean ± SD | 15.3 ± 7.6 | 13.8 ± 7.8 | −1.5 ± 5.3 |
| Median (Min, Max) | 16.0 (1.0, 27.0) | 14.0 (0.0, 27.0) | −1.0 (−12.0, 14.0) |
| VADRS Inattentive Symptom Severity | |||
| Mean ± SD | 15.4 ± 6.0 | 14.5 ± 6.3 | −1.1 ± 5.9 |
| Median (Min, Max) | 16.0 (2.0, 26.0) | 14.0 (2.0, 27.0) | −1.5 (−15.0, 18.0) |
| VADRS Hyperactive-Impulsive Symptom Count | |||
| Mean ± SD | 5.0 ± 3.2 | 4.4 ± 3.4 | −0.5 ± 2.7 |
| Median (Min, Max) | 5.0 (0.0, 9.0) | 4.0 (0.0, 9.0) | 0.0 (−7.0, 8.0) |
| VADRS Inattentive Symptom Count | |||
| Mean ± SD | 5.1 ± 3.1 | 4.7 ± 3.1 | −0.5 ± 2.9 |
| Median (Min, Max) | 5.0 (0.0, 9.0) | 5.0 (0.0, 9.0) | 0.0 (−7.0, 7.0) |
| Parent PedsQL Physical Functioning Score | |||
| Mean ± SD | 67.8 ± 21.4 | 70.2 ± 21.1 | 2.4 ± 25.6 |
| Median (Min, Max) | 71.9 (18.8, 100.0) | 71.4 (12.5, 100.0) | 0.0 (−65.6, 78.1) |
| Parent PedsQL Emotional Health Score | |||
| Mean ± SD | 60.4 ± 20.7 | 65.7 ± 20.3 | 5.1 ± 18.0 |
| Median (Min, Max) | 60.0 (10.0, 100.0) | 65.0 (25.0, 100.0) | 10.0 (–50.0, 55.0) |
| Parent PedsQL Social Functioning Score | |||
| Mean ± SD | 62.9 ± 23.6 | 64.1 ± 24.2 | 1.5 ± 24.5 |
| Median (Min, Max) | 60.0 (0.0, 100.0) | 65.0 (0.0, 100.0) | 0.0 (−65.0, 60.0) |
| Parent PedsQL School Functioning Score | |||
| Mean ± SD | 55.1 ± 15.2 | 53.8 ± 17.0 | −1.5 ± 16.9 |
| Median (Min, Max) | 55.0 (5.0, 85.0) | 55.0 (15.0, 90.0) | −5.0 (−45.0, 45.0) |
| Parent PedsQL Psychosocial Health Summary Score | |||
| Mean ± SD | 59.4 ± 14.5 | 61.1 ± 15.5 | 1.6 ± 13.4 |
| Median (Min, Max) | 60.0 (21.7, 88.3) | 62.5 (26.7, 93.3) | 1.7 (−35.0, 23.3) |
| Parent PedsQL Total Score | |||
| Mean ± SD | 62.4 ± 14.1 | 64.3 ± 14.3 | 1.9 ± 14.5 |
| Median (Min, Max) | 63.0 (30.4, 87.0) | 65.2 (37.0, 92.4) | 1.1 (−41.3, 41.3) |
| Median (Min, Max) | 69.2 (16.7, 100.0) | 66.7 (20.0, 93.3) | −1.7 (−40.0, 50.0) |
| HSQ Total Number Problems | |||
| Mean ± SD | 8.1 ± 3.2 | 7.0 ± 3.7 | −1.1 ± 3.6 |
| Median (Min, Max) | 8.8 (0.0, 13.0) | 6.8 (0.0, 13.0) | −1.0 (−8.0, 13.0) |
| HSQ Number Problems ≥5 | |||
| Mean ± SD | 4.3 ± 3.6 | 3.4 ± 3.3 | −1.0 ± 4.1 |
| Median (Min, Max) | 4.0 (0.0, 12.0) | 2.0 (0.0, 12.0) | 0.0 (−12.0, 10.0) |
| HSQ Severity | |||
| Mean ± SD | 3.1 ± 1.9 | 2.6 ± 2.0 | −0.6 ± 2.0 |
| Median (Min, Max) | 2.8 (0.0, 6.9) | 2.1 (0.0, 8.2) | −0.6 (−4.9, 4.9) |
Abbreviations: IMPACT, Impact Measure of Parenting-Related ADHD (attention deficit hyperactivity disorder) Challenges and Treatment; Min, minimum; Max, maximum; VADRS, Vanderbilt ADHD Diagnostic Rating Scale; PedsQL, Pediatric Quality of Life; HSQ, Home Situations Questionnaire.
Subscale validity and utility in ADHD assessment were investigated using Pearson correlations of IMPACT 1.0 subscale scores with other validated measures for T0, T1, and change (T1 − T0; see Table 4). IMPACT 1.0 subscale scores correlated with VADRS scores; however, the same was not true across correlations with the PedsQL or HSQ. IMPACT 1.0 Sibling scores at Time 1 were significantly positively correlated with VADRS Hyperactivity-Impulsivity severity and HSQ severity scores but were not consistently correlated with PedsQL scores (only one positive correlation with physical functioning was found). IMPACT 1.0 Misbehavior scores at each time point were positively and significantly correlated with ADHD symptoms (VADRS Hyperactivity-Impulsivity severity and VADRS Inattention severity scores) and behavioral noncompliance in the home (HSQ Severity score) and negatively correlated with quality of life in multiple domains (PedsQL Emotional Health, Social Functioning, and School Functioning scores). IMPACT 1.0 Time scores at each time point were positively and significantly correlated with inattentive ADHD symptoms (VADRS Inattention severity) but were correlated positively with VADRS Hyperactive-Impulsive severity scores only at Time 1. Time scores were not significantly correlated with most of the PedsQL and HSQ measures, with the exception of a negative correlation at Time 0 with PedsQL Emotional Health. IMPACT 1.0 School scores were significantly positively correlated with VADRS Hyperactivity-Impulsivity severity at each time point but were not significantly correlated with most PedsQL or HSQ severity scores.
Table 4.
IMPACT 1.0 Subscales Correlations With Other Outcomes.
| I. Sibling |
II. Misbehavior |
III. Time |
IV. School |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | Change | T0 | T0 | T0 | T0 | T1 | Change | T0 | T1 | Change | |
| VADRS Hyperactive-Impulsive Symptom Severity | 0.13 | 0.263* | 0.390** | 0.582** | 0.585** | 0.407** | 0.227 | 0.385** | 0.311* | 0.393** | 0.486** | 0.382** |
| VADRS Inattentive Symptom Severity | 0.004 | 0.154 | 0.292* | 0.294* | 0.443** | 0.332** | 0.417** | 0.343** | 0.327** | 0.21 | 0.244 | 0.346** |
| VADRS Hyperactive-Impulsive Symptom Count | 0.135 | 0.24 | 0.286* | 0.536** | 0.562** | 0.276* | 0.199 | 0.423** | 0.300* | 0.423** | 0.504** | 0.376** |
| VADRS Inattentive Symptom Count | 0.039 | 0.127 | 0.205 | 0.22 | 0.373** | 0.191 | 0.354** | 0.301* | 0.259* | 0.224 | 0.172 | 0.365** |
| Parent PedsQL Physical Functioning Score | −0.001 | 0.288* | 0.048 | −0.126 | 0.12 | 0.048 | −0.102 | 0.236 | 0.165 | 0.146 | −0.022 | −0.035 |
| Parent PedsQL Emotional Health Score | −0.169 | −0.12 | −0.067 | −.307* | −.368** | −.329** | −.375** | −0.161 | −0.225 | −0.085 | −0.235 | −0.018 |
| Parent PedsQL Social Functioning Score | −0.037 | −0.073 | −0.18 | −.369** | −.354** | −.332** | −0.119 | −0.024 | 0.007 | −0.009 | −.467** | −0.123 |
| Parent PedsQL School Functioning Score | 0.069 | 0.053 | −0.161 | −.265* | −0.161 | −0.03 | −0.206 | −0.222 | −0.134 | −.263* | −0.06 | −0.07 |
| Parent PedsQL Psychosocial Health Summary Score | −0.077 | −0.072 | −0.198 | −.437** | −.407** | −.343** | −.314** | −0.158 | −0.155 | −0.137 | −.364** | −0.115 |
| Parent PedsQL Total Score | −0.052 | 0.096 | −0.084 | −.361** | −0.225 | −0.174 | −.265* | 0.011 | 0.013 | −0.014 | −.269* | −0.085 |
| HSQ Total Number Problem Items | 0.228 | 0.296* | 0.103 | 0.531** | 0.498** | 0.454** | 0.395** | 0.299* | 0.399** | 0.235 | 0.246* | 0.039 |
| HSQ Number Problems ≥5 | 0.196 | 0.399** | 0.266* | 0.549** | 0.608** | 0.442** | 0.478** | 0.366** | 0.324** | 0.166 | 0.402** | 0.105 |
| HSQ Severity | 0.222 | 0.329** | 0.172 | 0.564** | 0.577** | 0.479** | 0.490** | 0.371** | 0.383** | 0.227 | 0.370** | 0.108 |
Abbreviations: IMPACT, Impact Measure of Parenting-Related ADHD (attention deficit hyperactivity disorder) Challenges and Treatment; VADRS, Vanderbilt ADHD Diagnostic Rating Scale; PedsQL, Pediatric Quality of Life; HSQ, Home Situations Questionnaire.
Correlation significant at the .05 level (2-tailed). **Correlation significant at the .01 level (2-tailed).
Importantly, changes in all IMPACT 1.0 subscale scores mirrored changes in all VADRS subscale scores, indicating that change in the IMPACT 1.0 assessed level of family stress was sensitive to rated change in ADHD symptoms. For the Misbehavior and Time subscales, change in IMPACT 1.0 scores was significantly correlated with change in HSQ-assessed behavioral noncompliance in the home.
Discussion
The IMPACT 1.0 Scale was developed using design thinking methods to capture salient family stresses and challenges that affect well-being and daily functioning. While existing tools capture broad impairment in home and school, they may miss more nuanced everyday stresses and challenges, which are crucial for treatment decision-making, global psychological adjustment, and satisfaction with care. The IMPACT 1.0 Scale includes items to improve understanding of the extent to which ADHD interferes with children’s behavior, siblings, school, and caregiver well-being. Because ADHD is a significant public health issue affecting the child, family, and community at large, better understanding of the functional stresses in these areas is a critically important component of clinical and research evaluation.15 IMPACT item content is not specific to ADHD, but content analyses suggest that family stresses captured on IMPACT items are particularly important and relevant for understanding the effect of ADHD on the family. Hence, IMPACT-assessed family stresses may also present with less frequency among children without any mental health condition,16 allowing for comparison of families of children with ADHD to other families. The IMPACT Scale was designed for clinician use during primary care follow-up visits in conjunction with the Vanderbilt to provide a more comprehensive and salient assessment of child and family functioning going beyond focused assessment of ADHD symptoms, in order to guide understanding, communication, and decision-making. Nevertheless, further work is needed to ensure that the scale distinguishes between children with and without ADHD.
Design thinking techniques elicited both tacit and latent knowledge that ultimately allowed for the creation of the IMPACT 1.0 Scale items.17 Design thinking has roots in business and engineering and used to explore stakeholders’ experiences and co-creating solutions that match stakeholders’ needs, add value to experiences, or improve interactions with a product.18 The approach has been used increasingly in cancer care and inpatient health care service delivery.19,20 It has also been used in technologies to improve diabetes and depression self-care.21,22 Thus, the approach to co-creation of the IMPACT 1.0 Scale with families struggling with ADHD is noteworthy, increases its face validity, and can lead to conversations that are practical and family-centered.
IMPACT 1.0 subscale scores were empirically developed using EFA and showed good internal consistency (particularly considering the brevity of the subscales and that α is related to subscale length) and test-retest reliability. These findings support the constructs of misbehavior, time, school, and siblings as sources of family stress as rated by parents of children with ADHD. In support of the validity of the IMPACT 1.0 Scale, we found a positive relationship between core ADHD symptoms on the Vanderbilt and IMPACT scores, such that increased ADHD severity was related to greater family stresses in all IMPACT subscale areas. As such, IMPACT represents a way for providers to efficiently identify, address, and monitor family stresses as a part of treatment that is related to but not redundant with core ADHD symptoms. Even for children successfully treated with ADHD medication, lingering family stresses may significantly affect quality of life (consistent with the significant correlations between IMPACT 1.0 and PedsQL scores). Discussion of family stress related to ADHD can create an opportunity for providers to more holistically assess the effect of current treatment, provide critical support, and facilitate referrals to family and social services that may improve overall quality of life. For example, it is unlikely that a family will be fully satisfied with treatment if symptom ratings improve but family stress levels show little concurrent change.
In addition to scale development, core constructs were identified for understanding the family impact of ADHD, by developing subscales in consultation with parents: Misbehavior, Time, Siblings, and School. An area of ongoing concern for parents of a child with ADHD pertains to the strife between siblings. Qualitative studies have shown siblings often have negative feelings toward the child with ADHD, and these experiences are often overlooked or minimized.23 It is not uncommon for family conflict to arise between the child with ADHD and sibling(s), which can contribute to severe strain within family relationships and parental stress.24-26 The IMPACT 1.0 Sibling subscale includes 4 items to capture the unique contribution of sibling conflict and ADHD. Sibling subscale scores were related to hyperactive-impulsive symptoms and to parental perception of the child’s behavior at home. Positive responses to Sibling items may lead to tailored counseling around sibling relationships and referrals for parenting training or family therapy and may spur discussions between the child with ADHD and/or sibling(s).
Children’s behavior and functioning at school are important to monitor to ensure that ADHD does not impede academic success. Executive functioning deficits and coexisting learning disabilities increase the risk of poor educational outcomes, including poor grades and increased detention and expulsion rates.27 Children with ADHD, particularly those with coexisting oppositional or aggressive behaviors, often experience problem behaviors at school that are stressful for teachers and parents.28 The IMPACT School subscale includes 2 items: “worrying that teachers thought negatively of their child” and “receiving phone calls from school.” School subscale scores were strongly related to ADHD hyperactive-impulsive symptoms, suggesting that externalizing symptoms of ADHD are particularly salient in generating school-related stresses for the family.
The last 2 subscales of IMPACT pertain to family stress related to time commitments and to functional effects and environments of misbehavior (eg, social events, in public, and meals). Misbehavior scores were strongly related to ADHD symptoms regardless of subtype. Time scores were strongly related to ADHD Inattentive symptoms and less consistently related to hyperactive-impulsive symptoms. Scores on the Misbehavior and Time subscales were also strongly related to parental perception of child behavioral issues at home, and Misbehavior scores in particular were highly related to parental report of child psychosocial quality of life.
The cumulative effects of family stresses related to misbehavior, time, siblings, and school may put the well-being of parents at risk. Parents experience high levels of stress when caring for a child with overt behavioral problems.29-31 Parents may experience depression, feelings of isolation, and poorer health.32,33 Positive responses to any items may produce targeted discussions about the parents’ support network, opportunities for self-care, and perceptions of parenting practices.
The findings of this research must be considered in light of the methodological characteristics used and IMPACT 1.0 Scale content. As with any parent-reported tool, IMPACT scores may be influenced by rater factors including social desirability, catastrophizing, limited awareness/insight into behavior, and insufficient understanding of content. All questionnaires were completed by the same rater (parent), raising potential effects of method bias. In addition, content and wording might reflect biases and experiences of the small number of parent advisors. While a larger number of families were invited to participate, the final number was due to scheduling and logistics during the winter. A cognitive interviewing method with additional parent advisors is being done with the plan to revise (including adding or subtracting items) and retest the scale as needed. Moreover, although challenges in the IMPACT Scale are common and stressful,1,34,35 specific items may not always be applicable (eg, Sibling scale). Further research is planned to optimize the utility of the scale in primary care settings, as well as examining pediatricians’ and pediatric providers’ perceptions of this tool for use in practice. Therefore, use of the scale should be done with caution despite strong psychometric support, pending further investigation. Last, no counterbalancing measures of resilience were utilized. However, as with any screening tool in pediatrics, the clinician should use these tools as a way to discuss strengths, in addition to parental concerns with families.
Conclusion
The IMPACT 1.0 Scale allows examination of a domain of family functioning (family stress) not captured by existing tools suitable for primary care practice. It is a valid, reliable, and novel tool that can guide discussions so treatment and services can be prescribed or refined to meet the unique needs of each family. Further research will explore ways to optimize the tool for primary care, including minor changes to content and wording, as well as examination to the feasibility of its implementation as perceived by pediatric providers.
Acknowledgments
The authors wish to thank the clinical support staff, nurses, and physicians at the study clinics within Eskenazi Health and Riley Hospital for Children at Indiana University Health who supported this study. We wish to thank all the parents and children who participated in the study. We also wish to thank the Pediatric Research Network (PResNet) for their tireless efforts to reach mothers and for working closely with the clinical staff to coordinate scheduling and research. A special thanks to the following PResNet research assistants: Amy Pottenger, Elaine Cuevas, Vickie Cater, Jennifer Stanton, and Cathy Luthman (PResNet executive director). A special thanks to Gina Claxton MPH, RD, program manager of the Indiana CTSI Community Health Partnerships, for her role in helping coordinate engagement sessions and study team meetings. The study team would also like to thank Dr Scott Denne and the Indiana CTSI Pediatrics Project Development Team for their thoughtful critiques in the early stages of this project after the initial patient engagement sessions that led to the development of the IMPACT Scale.
Appendix
IMPACT 1.0 Scale: Impact Measure of Parenting-Related ADHD Challenges and Treatment
Directions: This form asks about common challenges reported by families who have a child with ADHD. When answering, think about your child with ADHD and his/her behavior over the past 4 weeks. There are no right or wrong answers. If you are unsure how to answer, give the best response you can.
Was your child on medication for ADHD over the past 4 weeks? Yes ____ No _____
| How Often, in the Past 4 Weeks Have the Following Occurred: | ||||||
|---|---|---|---|---|---|---|
| Not at All | One or 2 Times | About Once a Week | More Than Once a Week | Every Day or Almost Every Day | No Other Children in the Family | |
| 1. Caused you to receive phone calls about your child’s behavior or performance at school/childcare | ||||||
| 2. Caused you to worry that teachers/child care providers think negatively about your child with ADHD | ||||||
| 3. Misbehavior at social events and family gatherings create stress | ||||||
| 4. Misbehavior during meal times at home | ||||||
| 5. Misbehavior in public while running errands | ||||||
| 6. Feeling like you do not have enough time to give other children attention | ||||||
| 7. Feeling like you do not have enough time to relax or find time for yourself | ||||||
| 8. Feeling like you have trouble finding enough time to do household things (ie, cook dinner or clean) | ||||||
| 9. Physical fights with siblings | ||||||
| 10. Verbal arguments with siblings | ||||||
| 11. Siblings do not want to be around child with ADHD | ||||||
| 12. Siblings cannot work together to complete household tasks | ||||||
Developed by Bauer et al (2017), Indiana University School of Medicine. Email: nsbauer@iu.edu. Please contact the author prior to use of the IMPACT 1.0 Scale.
Footnotes
Author Contributions: NSB: Contributed to conception/design; contributed to analysis; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
SO: Contributed to conception/design; contributed to analysis; drafted manuscript; critically revised manuscript; gave final approval.
CM: Contributed to conception/design; contributed to analysis; drafted manuscript; critically revised manuscript; gave final approval.
DL: Contributed to conception/design; contributed to analysis; drafted manuscript; critically revised manuscript; gave final approval.
SEW: Contributed to conception/design; contributed to analysis; critically revised manuscript; gave final approval.
SMD: Contributed to conception/design; critically revised manuscript; gave final approval.
AEC: Contributed to conception/design; critically revised manuscript; gave final approval.
WGK: Contributed to conception/design; contributed to analysis; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded, in part, by R24 award (R24-HS022434-01) from the Agency for Healthcare Research and Quality (Principal Investigator: Aaron E. Carroll, MD, MS). This project was supported, in part, with support from the Indiana Clinical and Translational Sciences Institute funded, in part by Grant Number UL1TR001108 from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award. Dr Bauer is an investigator with the Implementation Research Institute (IRI) at the George Warren Brown School of Social Work, Washington University in St. Louis, MO; through an award from the National Institute of Mental Health (5R25MH08091607) and the Department of Veteran Affairs, Health Services Research & Developmental Service, Quality Enhancement Research Initiative (QUERI).
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the Ethical Standards of the Institutional and/or National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Approval for the protocol outlined in the article was approved prior to initiation of the study.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Welfare of Animals: This article does not contain any studies with animals performed by any of the authors.
ClinicalTrials.gov Registration: Comparative Effectiveness of Primary Care-based Interventions for Pediatric ADHD (NCT02105142).
ORCID iD: Nerissa S. Bauer  https://orcid.org/0000-0002-1816-3575
https://orcid.org/0000-0002-1816-3575
References
- 1. Klassen AF, Miller A, Fine S. Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Pediatrics. 2004;114:e541-e547. [DOI] [PubMed] [Google Scholar]
- 2. Williams J, Klinepeter K, Palmes G, Pulley A, Foy JM. Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics. 2004;114:601-606. [DOI] [PubMed] [Google Scholar]
- 3. Hoagwood K, Jensen PS, Feil M, Vitiello B, Bhatara VS. Medication management of stimulants in pediatric practice settings: a national perspective. J Dev Behav Pediatr. 2000;21:322-331. [DOI] [PubMed] [Google Scholar]
- 4. Subcommittee on Attention-Deficit/Hyperactivity Disorder; Steering Committee on Quality Improvement and Management; Wolraich M, et al. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007-1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. American Academy of Pediatrics; Subcommittee on Attention-Deficit/Hyperactivity Disorder and Committee on Quality Improvement. Clinical practice guideline: treatment of the school-aged child with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108:1033-1044. [DOI] [PubMed] [Google Scholar]
- 6. Wolraich ML, Lambert W, Doffing MA, Bickman L, Simmons T, Worley K. Psychometric properties of the Vanderbilt ADHD Diagnostic Parent Rating Scale in a referred population. J Pediatr Psychol. 2003;28:559-567. [DOI] [PubMed] [Google Scholar]
- 7. Sikirica V, Flood E, Dietrich CN, et al. Unmet needs associated with attention-deficit/hyperactivity disorder in eight European countries as reported by caregivers and adolescents: results from qualitative research. Patient. 2015;8:269-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Varni JW, Burwinkle TM, Seid M. The PedsQL as a pediatric patient-reported outcome: reliability and validity of the PedsQL Measurement Model in 25 000 children. Expert Rev Pharmacoecon Outcomes Res. 2005;5:705-719. [DOI] [PubMed] [Google Scholar]
- 9. Rentz AM, Matza LS, Secnik K, Swensen A, Revicki DA. Psychometric validation of the Child Health Questionnaire (CHQ) in a sample of children and adolescents with attention-deficit/hyperactivity disorder. Qual Life Res. 2005;14:719-734. [DOI] [PubMed] [Google Scholar]
- 10. Bauer NS, Sullivan PD, Szczepaniak D, et al. Attention deficit-hyperactivity disorder group visits improve parental emotional health and perceptions of child behavior. J Dev Behav Pediatr. 2018;39:461-470. [DOI] [PubMed] [Google Scholar]
- 11. Altepeter TS, Breen MJ. The Home Situations Questionnaire (HSQ) and the School Situations Questionnaire (SSQ): normative data and an evaluation of psychometric properties. J Psychoeduc Assess. 1989;7:312-322. [Google Scholar]
- 12. Manktelow J, Carlson A. 5 whys: getting quickly to the root of the problem. https://www.mindtools.com/pages/article/newTMC_5W.htm. Accessed February 21, 2019.
- 13. Brandt E, Messeter J. Facilitating collaboration through design games. Paper presented at: Proceedings of the Eighth Conference on Participatory Design: Artful Integration: Interweaving Media, Materials, and Practices—Volume 1; July 27-31, 2004; Toronto, Canada. [Google Scholar]
- 14. Ackoff R. From data to wisdom. J Appl Syst Anal. 1989;16:3-9. [Google Scholar]
- 15. Perou R, Bitsko RH, Blumberg SJ, et al. Mental health surveillance among children—United States, 2005-2011. MMWR Suppl. 2013;62(suppl 2):1-35. [PubMed] [Google Scholar]
- 16. Minuchin S. Families and Family Therapy. Cambridge, MA: Harvard University Press; 1974. [Google Scholar]
- 17. Orlowski S, Matthews B, Bidargaddi N, et al. Mental health technologies: designing with consumers. JMIR Hum Factors. 2016;3:e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Asch DA, Rosin R. Innovation as discipline, not fad. N Engl J Med. 2015;373:592-594. [DOI] [PubMed] [Google Scholar]
- 19. Patel M, Moore D, Blayney D, Milstein A. Transforming cancer care: are transdisciplinary approaches using design-thinking, engineering, and business methodologies needed to improve value in cancer care delivery? J Oncol Pract. 2014;10:e51-e54. [DOI] [PubMed] [Google Scholar]
- 20. Carmel-Gilfilen C, Portillo M. Designing with empathy: humanizing narratives for inspired healthcare experiences. HERD. 2016;9:130-146. [DOI] [PubMed] [Google Scholar]
- 21. Petersen M, Hempler NF. Development and testing of a mobile application to support diabetes self-management for people with newly diagnosed type 2 diabetes: a design thinking case study. BMC Med Inform Decis Mak. 2017;17:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yarosh S, Schueller SM. “Happiness inventors”: informing positive computing technologies through participatory design with children. J Med Internet Res. 2017;19:e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kendall J. Sibling accounts of attention deficit hyperactivity disorder (ADHD). Fam Process. 1999;38:117-136. [DOI] [PubMed] [Google Scholar]
- 24. Smith AJ, Brown RT, Bunke V, Blount RL, Christophersen E. Psychosocial adjustment and peer competence of siblings of children with attention-deficit/hyperactivity disorder. J Atten Disord. 2002;5:165-177. [DOI] [PubMed] [Google Scholar]
- 25. Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2005;90(suppl 1):i2-i7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mikami AY, Pfiffner LJ. Sibling relationships among children with ADHD. J Atten Disord. 2008;11:482-492. [DOI] [PubMed] [Google Scholar]
- 27. Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. J Pediatr Psychol. 2007;32:643-654. [DOI] [PubMed] [Google Scholar]
- 28. Greene R, Beszterczey S, Katzenstein T, Park K, Goring J. Are students with ADHD more stressful to teach? Patterns of teacher stress in an elementary school sample. J Emot Behav Disord. 2002;10:79-89. [Google Scholar]
- 29. Hinojosa MS, Hinojosa R, Fernandez-Baca D, Knapp C, Thompson LA. Parental strain, parental health, and community characteristics among children with attention deficit-hyperactivity disorder. Acad Pediatr. 2012;12:502-508. [DOI] [PubMed] [Google Scholar]
- 30. Podolski CL, Nigg JT. Parent stress and coping in relation to child ADHD severity and associated child disruptive behavior problems. J Clin Child Psychol. 2001;30:503-513. [DOI] [PubMed] [Google Scholar]
- 31. Tzang RF, Chang YC, Liu SI. The association between children’s ADHD subtype and parenting stress and parental symptoms. Int J Psychiatry Clin Pract. 2009;13:318-325. [DOI] [PubMed] [Google Scholar]
- 32. Murphy NA, Christian B, Caplin DA, Young PC. The health of caregivers for children with disabilities: caregiver perspectives. Child Care Health Dev. 2007;33:180-187. [DOI] [PubMed] [Google Scholar]
- 33. DosReis S, Barksdale CL, Sherman A, Maloney K, Charach A. Stigmatizing experiences of parents of children with a new diagnosis of ADHD. Psychiatr Serv. 2010;61:811-816. [DOI] [PubMed] [Google Scholar]
- 34. Whalen CK, Henker B, Ishikawa SS, et al. An electronic diary study of contextual triggers and ADHD: get ready, get set, get mad. J Am Acad Child Adolesc Psychiatry. 2006;45:166-174. [DOI] [PubMed] [Google Scholar]
- 35. Whalen CK, Henker B, Jamner LD, et al. Toward mapping daily challenges of living with ADHD: maternal and child perspectives using electronic diaries. J Abnorm Child Psychol. 2006;34:115-130. [DOI] [PubMed] [Google Scholar]


