Abstract
Background and Objectives:
Multidisciplinary care teams may improve health and control total cost for children with medical complexity (CMC). This paper aims to quantify the time required to perform non-reimbursed care coordination activities by a multidisciplinary care coordination program for CMC, and to estimate the direct salary costs of that time.
Methods:
From April 2013 to October 2015, program staff tracked time spent in practicably-measured non-billed care coordination efforts. Staff documented the discipline involved, the method used, and the target of the activity. Cost was estimated by multiplying the time spent by the typical salary of the type of personnel performing the activity.
Results:
Staff logged 53,148 unique non-billed care coordination activities for 208 CMC. Dietitians accounted for 26% of total time, MDs/NPs 24%, RNs 29% and social workers 21% (1.8, 2.3, 1.2, and 1.4 hours per CMC per month per full time provider, respectively). Median time spent in non-reimbursed care coordination was 2.3 hours per child per month (IQR 0.8–6.8). Enrollees required substantially greater time in their first program month than thereafter (median 6.7 vs 2.1 hours per CMC per month). Based on 2015 national salary data, the adjusted median estimated cost of the documented activities ranged from $145 to $210 per CMC per month.
Conclusions:
In this multidisciplinary model, care coordination for CMC required substantial staff time, even without accounting for all activities, particularly in the first month of program enrollment. Continued advocacy is warranted for the reimbursement of care coordination activities for CMC.
Table of Contents Summary:
This observational study estimates the time and non-reimbursed direct salary costs for care coordination in an ACO-aligned multidisciplinary program.
INTRODUCTION
Children with medical complexity (CMC) represent less than 1% of the US pediatric population yet account for as much as 33% of total healthcare spending for children1 and 40% of pediatric hospital charges.2 The intensity of services and costs required for optimal care of this vulnerable population places substantial burden on families and on healthcare systems alike.3–5 Substantial variations exist in healthcare utilization by CMC.6 High quality healthcare systems are asking how they can optimize the health and wellbeing of this vulnerable population, while limiting high-cost spending to those areas where it will produce the most health.7
One approach that has shown great promise in improving health and controlling total cost of care for CMC is to create and deploy multidisciplinary care teams. Such teams exist on a spectrum from nurse care management by a practice, to disease management by external entities8, to the more intensive multidisciplinary management that may be provided by physicians, nurse practitioners, nurse coordinators, nutritionists and social workers at centers such as children’s hospitals.9 By matching CMC in a timely fashion to those services that will provide meaningful benefit,10,11 care delivered by multidisciplinary teams increases the use of outpatient12 and surgical13 services, while reducing total hospital days13,14, and decreasing out of pocket costs to families.5 Their value exists not only in reducing the level of care required for these children: evidence suggests that they may improve child quality of life.15
Multidisciplinary teams seek to match clinical services to patient needs by practicing a high degree of care coordination, defined as a process that links children and their families with appropriate services and resources in a coordinated effort to achieve good health.16 Although care coordination programs are expected to reduce health system costs, the actual work performed by these programs can be poorly quantified and is often not reimbursed. Therefore, this paper aims to quantify non-reimbursed care coordination activities and to estimate the direct personnel costs associated with those activities, as incurred by a multidisciplinary care coordination program for CMC.
PATIENTS AND METHODS
We conducted a time study of care coordination activities performed for children and young adults with medical complexity enrolled with the University Hospitals Rainbow Center for Comprehensive Care from January 2013 through June 2015.
Setting
The UH Rainbow Center for Comprehensive Care (“the center”) is a multidisciplinary care coordination program established in 2013 and intended to address the Triple Aim17 for community-dwelling children and young adults with medical complexity in Northeast Ohio. Following the model of tertiary care-primary care partnership established by leaders in the field10, the center teams with families, primary care clinicians (PCCs), and subspecialty services to optimize care and address barriers experienced by CMC and their families. Patients may be referred to the center (a) by an inpatient service at UH Rainbow Babies and Children’s Hospital, a free-standing children’s hospital aligned with a pediatric Accountable Care Organization (ACO); (b) from the ambulatory setting by their PCC or specialist; or (c) by self-referral.
Patient Population (Tables 1 and 2):
Table 1:
Study Population: Child Characteristics
| Child Characteristics | N | % |
| Gender | ||
| male | 108 | 52% |
| female | 100 | 48% |
| Age at Enrollment | ||
| Birth to <1 year | 27 | 13% |
| 1 to <5 years | 55 | 26% |
| 5 to <11 years | 61 | 29% |
| 11 to <18 years | 40 | 19% |
| 18+ years | 25 | 12% |
| Clinical Characteristics | ||
| Number of body systems-median(range) | 208 | 4(3-6) |
| Neurodevelopmental disabilities | 131 | 63% |
| Cerebral Palsy | 98 | 47% |
| Epilepsy, seizures, or convulsions | 88 | 42% |
| Developmental delay | 14 | 7% |
| Other neurologic condition | 10 | 5% |
| Technology dependence | 162 | 78% |
| Tracheostomy | 32 | 15% |
| Respiratory support devicea | 19 | 9% |
| Feeding tube | 143 | 69% |
| Other technologyb | 49 | 24% |
| Caregiver assistance with ADLs | 194 | 93% |
| Gross Motor Function Classificationc | ||
| Level I-III | 20 | 10% |
| Level IV | 36 | 17% |
| Level V | 93 | 45% |
| Not scored | 59 | 28% |
ADLs-activities of daily living, FPL-Federal Poverty Level, PIPP/HEAP-Percentage of Income/Home Energy Assistance Plan
Respiratory support device: ventilator, CPAP or BiPAP
Other technology: central line, urinary catheter, intrathecal baclofen pump, vagal nerve stimulator, or other
Gross Motor Function Classification: Palisano et al. (1997) Dev Med Child Neurol 39:214-23
Table 2:
Study Population: Family Characteristics
| Family Characteristics | N | % |
|---|---|---|
| Primary Insurer | ||
| Medicaid Fee for Service | 153 | 74% |
| Medicaid Managed Care | 21 | 10% |
| Commercial | 26 | 13% |
| Self-Pay | 5 | 2% |
| missing | 3 | 1% |
| Household Income (%FPL) | ||
| <100% | 47 | 23% |
| 100-150% | 32 | 15% |
| 151-250% | 4 | 2% |
| >250% | 53 | 25% |
| missing | 72 | 35% |
| Social Stressors | ||
| Receive food assistance | 65 | 31% |
| PIPP/HEAP | 53 | 25% |
| Single parent household | 46 | 22% |
| Rely on public transportation | 17 | 8% |
| Receive housing assistance | 16 | 8% |
| Residence | ||
| Miles from center-median(range) | 208 | 20.9(0-135) Median(range) child-months |
| Status in Program as of 10/1/2015 | ||
| Active | 163 | 16.5(4.4-34.6) |
| Discharged | 29 | 6(0-32) |
| Deceased | 10 | 4.2(1.4-19.3) |
| Missing | 5 | |
| Overall | 208 | 14.8(0-34.6) |
ADLs-activities of daily living, FPL-Federal Poverty Level, PIPP/HEAP-Percentage of Income/Home Energy Assistance Plan
Respiratory support device: ventilator, CPAP or BiPAP
Other technology: central line, urinary catheter, intrathecal baclofen pump, vagal nerve stimulator, or other
Gross Motor Function Classification: Palisano et al. (1997) Dev Med Child Neurol 39:214-23
Children and young adults aged 0–26 years eligible for enrollment with the center experience significant neurocognitive impairment, involvement of three or more body systems, dependence on technology, and/or reliance on caregivers for instrumental activities of daily living. CMC are ineligible for the program if they are already served by a disease-specific care coordination program (e.g, sickle cell, cystic fibrosis), if they are currently exercising their hospice benefits, or if they reside in a long-term care facility. There are no restrictions to enrollment based on insurer. A total of 208 children and young adults with medical complexity were included in this study. At enrollment, these CMC were between 3 months and 26 years of age, with mean age of 8 years. Two-thirds demonstrated neurocognitive impairment. Three quarters relied on technology, including feeding tubes (69%), tracheostomies (15%), respiratory support devices including ventilators, CPAP or BiPAP (9%), and other technology including central lines, urinary catheters, intrathecal baclofen pumps, vagal nerve stimulators, etc (24%).
Care Team Structure and Function:
Center staff function as a care coordination team linking CMC and their PCC with coordinated specialty services. Staffing assumes enrollment of 75-100 patients per full time equivalent (FTE) clinician. The team consists of 0.5 FTE general pediatricians (MD), 2 FTE pediatric nurse practitioners (NP), 3 FTE registered nurse (RN) case managers, 2 FTE dietitians, 2 FTE social workers (SW), and 4 FTE medical assistants hired as Family Care Advocates (FCA), a novel role intended to facilitate home visits with center enrollees. Center MDs and NPs are available 24 hours per day, 7 days per week. On enrollment, the center team in partnership with the CMC and their family develops a comprehensive care plan considering findings from detailed medical, nutrition, and psychosocial assessments. This care plan is made available to the center team, PCCs, and specialists via electronic medical record (EMR), and is used to guide care. Center clinicians see patients for both planned and urgent visits in the clinic and are available in some situations to conduct home visits. A center NP is available for consultation to inpatient teams to enroll new patients, to participate in multidisciplinary team rounds for established patients, and to assist with hospital discharge planning. Discharge from the program may occur if families move out of the ACO region, or if they request program discharge.
Data sources
Inclusion criteria:
This analysis included all recorded observations for all 208 children and young adults who enrolled with the center from January 1, 2013 (program start) through June 1, 2015. Data collection ended October 1, 2015.
Demographics:
Center staff documented patient characteristics at the time of program enrollment into a study-specific SharePoint Enterprise (Microsoft Corporation, Redmond Washington) database housed on HIPAA-secure, hospital-based encrypted servers.
Staff time and non-reimbursed costs of care coordination:
For each care coordination activity for each CMC, the individual performing the activity documented in the central SharePoint database their discipline (MD/NP, RN, dietitian, SW, or FCA); the method of the interaction (email, telephone, chart review, video conference, or formal team review); the target of the activity (patient or his/her caregiver; outside provider not employed at the center such as durable medical equipment suppliers, home nursing agencies, county Department of Children and Family Services, specialists, therapists, PCCs, etc; or other); and the duration (in 1 minute increments) of the activity. Direct data entry by each staff member into the SharePoint database occurred as close to real-time as possible, and no later than by the end of the work day in which the activity took place. To ensure consistency amongst staff, documentation of these activities was discussed as part of monthly interdisciplinary team meetings, however, the SharePoint database was not independently audited for accuracy. Activities omitted by this design included informal conversations amongst center staff outside the team case review setting and other communication activities such as faxing records.
This study was approved by the University Hospitals Cleveland Medical Center Institutional Review Board.
Variables
Outcome variables:
The primary outcome was total time spent by center staff in care coordination activities. We estimated personnel cost by multiplying the hours in a given month spent in care coordination for a given child by the estimated hourly wage of the category of personnel performing the activity. We used estimated wages as reported by the Bureau of Labor Statistics Occupational Employment Statistics Survey, May 2015 (see Supplemental Table 5).18 We did not assess indirect costs or benefits associated with these wages. Because physician and nurse practitioner time was recorded together by center staff as a single category, hourly salary for this category was weighted to reflect program time commitments by personnel type. Additionally, any in-person activities by physicians or nurse practitioners were excluded from these analyses, as some might be in fact billable services, depending on the setting in which they occurred.
Covariates:
Child-level factors of interest included gender (male/female), age, presence of neurocognitive impairment (yes/no), insurance status, and insurance type. Family-level factors included distance of residence from center location, family socio-economic status (SES) at four levels (household income as percentage of federal poverty level: 0-100%, 101-250%, greater than 250%, or missing), number of adult caregivers in the household, and receipt of food assistance (yes/no).
Analyses
First, we described child and family level demographic characteristics for all children in the study. We next performed bivariate analyses using Pearson’s chi-square or Fisher’s exact test (when expected cell size <20) to assess relationships between categorical child- and family-level characteristics, and the Wilcoxon-Mann-Whitney test to evaluate relationships between those characteristics and care coordination effort (time and cost per child per month). After estimating total time and direct personnel cost per child per month for all non-reimbursed activities, we constructed generalized linear models for each wage category to adjust cost estimates for child gender, age at enrollment, family income, and length of time enrolled in the program, censoring observations at date of program discharge, patient death, or end of the observation period. Sensitivity analyses tested for robustness of estimates to missing data and varying model assumptions. All analyses were conducted using SAS 9.4 (SAS Institute, Cary NC).
RESULTS
Care Coordination Activities:
We recorded 53,148 care coordination activities for 205 children with medical complexity (3 enrollees contributed no activities prior to program discharge), an average of 19,327 activities per year and 21 activities per child per month. Our observations totaled 2,586 child-months, ranging between 1 and 33 months for a given child (Table 2).
While RNs and SWs accounted for a greater number of total activities, the clinical practitioners (physicians / NPs, and dieticians) accounted for a larger proportion of time spent in such activities. Overall, all team members together spent on average 4.8 hours per enrolled child per month (median 2.3, IQR 0.8-6.8) in care coordination activities (Figure 1).
Figure 1:
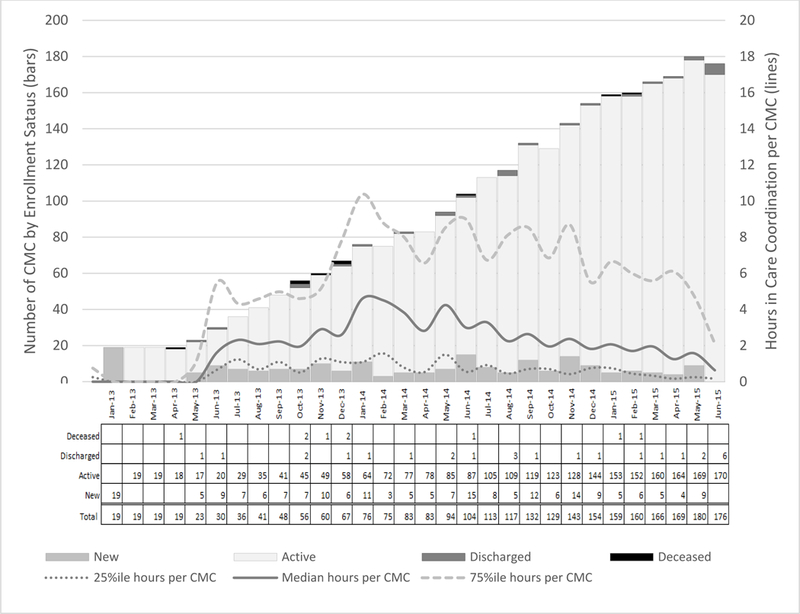
Program enrollment status and care coordination time by calendar month, January 2013 - June 2015. CMC - child with medical complexity
Twenty percent of all recorded care coordination activities consisted of communication with a primary care physician, specialist or ancillary provider outside the comprehensive care team. These communications required approximately 10 minutes each (median 7, range 0-330). Across all disciplines, an average of 61 minutes per child per month were spent in communication with other providers (median 30, range 0-846). A slightly higher (21%) proportion of these communication activities involved either the patient directly or his or her caregiver. These communications were the most time consuming, requiring median 10 minutes for each communication (range 1-330), and totaling median 48 minutes per child per month (range 0-661). The majority of care coordination activities were classified as “other”, a category that included chart review and formal case review processes, weekly team-based review of new enrollees, and updates regarding acute concerns, emergency visits, and hospitalizations of established patients within the preceding week. Across all disciplines, care team members spent median 100 minutes per child per month in these activities (range 0-4060).
The majority of recorded care coordination activities comprised telephone calls, chart review, team-based case review, and (for non-MD/NP personnel) in-person communication with patients and their families. In contrast, little time was spent in email (n=5966, median 5 minutes per activity, range 1-120) or video calls (n=122, median 5 minutes per call, range 1-90).
We found that program staff spent substantially greater time in care coordination for children in their first month of program enrollment than they did in subsequent months. In that initial month, program staff spent median 6.7 hours per child in care coordination activities (IQR 3.7-10.6). This compares with the more modest 2.2 hours per child per month (IQR 0.7-6.4) devoted in subsequent months (Figure 2).
Figure 2:
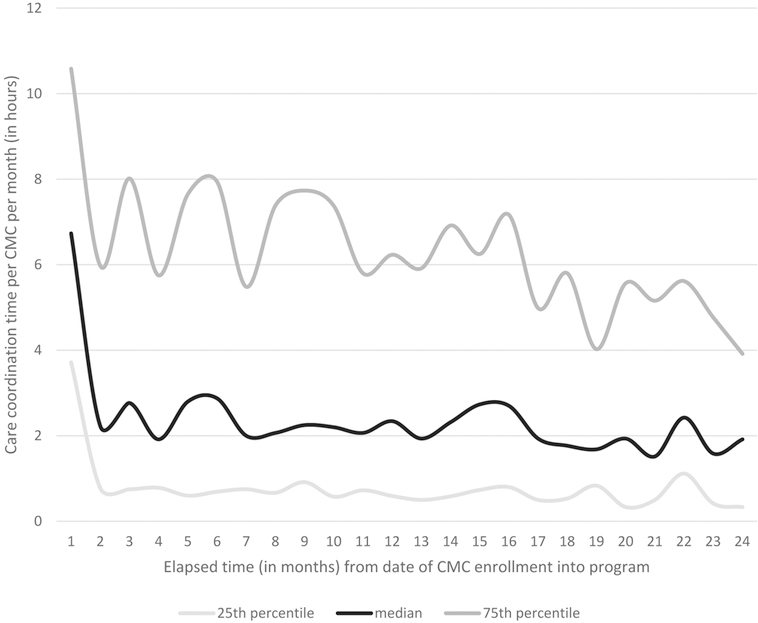
Estimated total time spent per month in non-reimbursed care coordination activities, by elapsed time in months from date of CMC enrollment into the program. CMC:child with medical complexity.
Estimates of costs:
Our second objective was to estimate personnel costs for these activities. We first estimated unadjusted personnel costs for care coordination. Assuming 25th percentile wages for all staff involved in care coordination, we found median cost per child per month to be $68 (IQR $19-$208), increasing to $98 (IQR $28-$300) if 75th percentile wages were assumed. Adjusting for family income, child gender, child age at program enrollment, and length of time with the program, we found that younger child age at enrollment was significantly associated with greater personnel costs for care coordination. In addition, compared to families with income exceeding 250 percent of the federal poverty level, those children whose families reported income at or below 100 percent of the federal poverty level were more likely to incur increased costs for care coordination. These observations were consistent across models assuming hourly personnel wages at the national 25th percentile, median, and 75th percentile, respectively. In sensitivity analyses, inclusion of presence of neurocognitive impairments or distance from home to the center did not improve model fit and were not significantly associated with personnel costs. Therefore, accounting for child age, gender, duration with program, and family income, adjusted median personnel cost per child per month was between $145 (assuming 25th percentile wages) and $210 (assuming 75th percentile wages, see Table 3).
Table 3:
Non-Reimbursed Care Coordination Activities Performed by Staff - number of activities and estimate of cumulative time spent in such activities
| Overall | Na | mean | SD | median | min | max | |
|---|---|---|---|---|---|---|---|
| Months of observation | 2586 | 10 | 7.1 | 9 | 1 | 33 | |
| Time (hours per child-month) | 2586 | 4.8 | 6.1 | 2.3 | 0 | 81.4 | |
| Activities (per child-month) | 2586 | 20.5 | 22.6 | 13 | 1 | 163 | |
| By Discipline | |||||||
| Time (hours per child-month) |
MD/NP | 1618 | 2.6 | 3.7 | 1.1 | 0 | 35.0 |
| Social work | 1865 | 1.4 | 2.3 | 0.5 | 0 | 26.0 | |
| Dietician | 1927 | 1.8 | 2.1 | 1.1 | 0 | 22.1 | |
| RN | 2127 | 1.2 | 1.6 | 0.6 | 0 | 28.7 | |
| FCA | 64 | 1.1 | 1.9 | 0.2 | 0 | 9.9 | |
| Missing | 37 | 0.2 | 0.2 | 0.1 | 0 | 1.0 | |
| Activities (number per child-month) |
MD/NP | 1618 | 7.6 | 9.1 | 4 | 1 | 78 |
| Social work | 1865 | 6.1 | 8.0 | 4 | 1 | 107 | |
| Dietician | 1927 | 7.1 | 7.2 | 5 | 1 | 79 | |
| RN | 2127 | 7.2 | 7.4 | 5 | 1 | 58 | |
| FCA | 64 | 3.3 | 3.2 | 2 | 1 | 16 | |
| Missing | 37 | 1.5 | 1 | 1 | 1 | 5 | |
| By Target | |||||||
| Time (hours per child-month) |
Provider | 1589 | 1.0 | 1.4 | 0.5 | 0 | 14.6 |
| Patient | 2088 | 1.5 | 1.8 | 0.8 | 0 | 11.0 | |
| Other | 2221 | 3.4 | 4.5 | 1.7 | 0 | 67.7 | |
| Activities (number per child-month) |
Provider | 1589 | 6.8 | 9.5 | 3 | 1 | 112 |
| Patient | 2088 | 5.3 | 5.0 | 4 | 1 | 46 | |
| Other | 2221 | 14.1 | 15.6 | 8 | 1 | 98 | |
| By Mode | |||||||
| Time (hours per child-month) |
1574 | 0.5 | 0.6 | 0.3 | 0 | 7.8 | |
| Phone | 1721 | 0.7 | 0.9 | 0.4 | 0 | 10.3 | |
| In-person | 1149 | 2.2 | 2.0 | 1.8 | 0 | 14.2 | |
| Video calls | 87 | 0.2 | 0.3 | 0.1 | 0 | 1.5 | |
| Formal Team Reviewb | 2131 | 2.9 | 4.1 | 1.4 | 0 | 69.4 | |
| Chart review | 1605 | 1.0 | 1.2 | 0.6 | 0 | 9.4 | |
| Activities (number per child-month) |
1574 | 4.6 | 5.6 | 3 | 1 | 70 | |
| Phone | 1721 | 5.2 | 6.0 | 3 | 1 | 64 | |
| In-person | 1149 | 4.6 | 4.5 | 3 | 1 | 40 | |
| Video calls | 87 | 1.4 | 1.1 | 1 | 1 | 6 | |
| Formal Team Reviewb | 2131 | 12.2 | 13.3 | 7 | 1 | 97 | |
| Chart review | 1605 | 3.5 | 3.9 | 2 | 1 | 33 | |
MD-general pediatrician, NP-pediatric nurse practitioner, RN-registered nurse, FCA - family care assistant
Total child-months of observation
Formal Team Review: weekly structured face-to-face meetings amongst members of the interdisciplinary team to discuss needs of new enrollees and address acute or emergent concerns regarding established patients in the program. This mode excludes informal or “curbside” consultations regarding a given patient.
DISCUSSION
Children with medical complexity are increasingly becoming the focus of attention nationally 4,15,19,20 both because we have much to learn about how best to manage their care and because it has become increasingly apparent that these children consume a substantial proportion of the fraction of Medicaid dollars that go to children. We found that in the context of a children’s hospital that is generally well-staffed to care for these children, care coordination activities required conservative estimate of $145 to $210 in un-reimbursed salary per child per month, not including fringe benefits, management or overhead costs. We note that our estimates are conservative, as our study design explicitly excluded important time-consuming tasks such as informal conversations amongst team members regarding a patient’s care and appointment scheduling. It is possible that over time the development of systems to support this work (for a cost) and efficiencies borne of experience or economies of scale could alter these salary costs. Nonetheless, salaries are likely to continue to constitute a significant cost to support providing coordinated care for children with medical complexity.
Care management requires work and that work consumes resources. The value from care management may be generated through improved family and patient-centered outcomes (including better health and greater satisfaction). Value may also be produced by increasing the efficiency of care: inappropriate services can be reduced, preventable complications avoided, and services may be provided in a more timely fashion. One challenge is that cost-efficient and even cost-savings programs may not benefit the provider of the care coordination services. For example, assuming 75th percentile wages for clinicians and staff, we estimate a median cost of just over $200 per CMC per month in direct salary costs to provide such services ($2400 per CMC per year); the equivalent cost of 4.2 emergency department visits (at median cost $570 per visit21), or 1 hospital day (at $2400 per day22- see Supplemental Table 6). Thus, while the global outcome may be beneficial and efficient, there are market inefficiencies that allow for perverse consequences from critical perspectives: a clinical system may provide care coordination services whose efficiency reduces future revenue, while a payer may benefit by avoiding future costs for no or minimal investment. Modern innovations, such as accountable care organizations, and a population-based value framework19 attempt to create better alignment of incentives. Whether for assessing potential costs and savings for health planning in an innovations framework or for budgeting in a more traditional framework, the field needs a better understanding of the costs and benefits of care coordination for this vulnerable and relatively expensive population. This study provides a conservative estimate of the cost component.
The time study described in this report supports planning and design. High quality and safe care for these children requires care coordination.23-26 Our finding that new enrollees require substantially greater hours for care coordination in their first month compared to the observed subsequent relative “steady state” may help similar programs to pace admissions of new enrollees. In this era of accountability, developing payment models that align accountability, costs, and benefits will be critical for such care coordination efforts to be sustained by healthcare providers.26
For its contributions, this study has important limitations. First, as an observational, uncontrolled assessment of clinical activity in a real-world setting, we have designed this study so that its biases reduce our estimate of costs. We considered only wages for time in direct services provision. We did not account for any of the additional costs required to maintain such a care program, such as program management, facility fees, and overhead. Our estimates of time and cost relied on staff logging of time spent in various activities. We speculate that when faced with pressing patient care concerns, staff may have forgone logging of those activities, further contributing to underestimation of total time expended in care coordination. Second, our program experienced substantial growth during the study period. It is therefore possible the program was over- or under-staffed to meet the actual needs of CMC at various points during the study period.
We thus interpret our estimates as a low approximation of the non-reimbursed activities provided by our program. The data are specific to the design of our program; care coordination in other settings may require more or less staff. It is also likely that costs will not remain constant over time. Further research is needed to determine whether our findings would hold in a more mature program. Finally, we have tried to make our estimates more general by using national salary estimates rather than local salaries. While this study did not assess directly outcomes in terms of the Triple Aim, it does bridge the gap in the literature by estimating costs and efforts required to perform services that others have shown to be effective.4,17,23
CONCLUSIONS
This study aims to provide valid estimates of the un-reimbursed direct salary cost of care coordination for CMC. At $145-$210 per child per month, even this conservative estimate of costs represents a substantial investment by the institution that provides healthcare. Our data may be helpful for planners seeking to develop similar programs, those considering the costing of similar programs in the accountable care context, and to inform and stimulate conversations to develop evidence-informed fixes for the fee-for-service context.
Supplementary Material
Table 4:
Estimated Direct Personnel Costs of Non-Reimbursed Care Coordination Activities, assuming 25th percentile, median, and 75th percentile hourly wages ($USD per child-month)
| Na | mean | SD | median | IQR | |
|---|---|---|---|---|---|
| Unadjusted Estimated Cost | |||||
| 25th Percentile Wage | 2586 | 150.70 | 213.46 | 68.44 | (19.05 - 207.57) |
| 50th Percentile Wage | 2586 | 184.50 | 236.00 | 82.15 | (23.02 - 253.54) |
| 75th Percentile Wage | 2586 | 217.79 | 307.45 | 98.24 | (28.02 - 300.15) |
| Adjustedb Estimated Cost | |||||
| 25th Percentile Wage | 2544 | 150.86 | 53.42 | 145.03 | (111.33 - 187.52) |
| 50th Percentile Wage | 2544 | 184.70 | 65.75 | 177.55 | (135.94 - 229.91) |
| 75th Percentile Wage | 2544 | 217.99 | 77.03 | 209.73 | (160.89 - 270.90) |
Total child-months of observation
Adjusted for family income, child age, child gender, and time since enrollment in the program, via generalized linear model with gamma distribution and log link
IQR - Interquartile Range
What’s Known on This Subject:
Children with medical complexity are relatively high cost and have better outcomes and lower costs when care coordination is successful. Various models exist but how much care is delivered beyond what is reimbursed has not been described.
What This Study Adds:
The time study described in this report provides an estimate of the minimum time spent in non-billable care coordination activities for children with medical complexity.
Acknowledgements:
The authors gratefully acknowledge Susan Connor, PhD, Nellie Coughlin, MSN, APRN, PPCNP-BC, Nicole Deutsch, MSN, APRN, PCNP-PC, Samantha Drake, RN, CPN, Katina Ferguson, LISW-S, Rebecca Loos, RN, Mary Neff, LSW, Laurel Rose, RN, CPN, Bernida Rowe, Amber Smith, LISW-S, Sarah Weiss, LISW-S, Jenna Wiltzer Karim, MS, RDN, Jodi Wolff MS, RDN, and the patients and families of the UH Rainbow Center for Comprehensive Care for their contributions to this work.
Funding Source: This study received support from Funding Opportunity Number CMS-1C1-12-0001 from Centers for Medicare and Medicaid Services, Center for Medicare and Medicaid Innovation.
Abbreviations:
- ACO
accountable care organization
- CMC
children with medical complexity
- EMR
electronic medical record
- FCA
family care advocate
- FTE
full time equivalent
- MD
physician
- NP
Nurse Practitioner
- PCC
primary care clinician
- SW
social worker
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Berry JG, Hall M, Neff J, Goodman D, Cohen E, Agrawal R, et al. Children with medical complexity and medicaid: spending and cost savings. Health Affairs. 2014;33(12):2199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simon TD, Berry J, Feudtner C, Stone BL, Sheng X, Bratton SL, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quigley L, Lacombe-Duncan A, Adams S, Hepburn CM, Cohen E. A qualitative analysis of information sharing for children with medical complexity within and across healthcare organizations. BMC Health Serv Res. 2014;14:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coller RJ, Nelson BB, Sklansky DJ, Saenz AA, Klitzner TS, Lerner CF, et al. Preventing hospitalizations in children with medical complexity: a systematic review. Pediatrics. 2014;134(6):e1628–47. [DOI] [PubMed] [Google Scholar]
- 5.Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and Costs of Healthcare Use of Children With Medical Complexity. Pediatrics. 2012;130(6):e1463–e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ralston SL, Harrison W, Wasserman J, Goodman DC. Hospital variation in healthcare utilization by children with medical complexity. Pediatrics. 2015;136(5):860–7. [DOI] [PubMed] [Google Scholar]
- 7.Porter ME. What is value in healthcare? New England Journal of Medicine. 2010;363(26):2477–81. [DOI] [PubMed] [Google Scholar]
- 8.Kleinman LC. A Vision for Disease Management. Surgical Services Management. 1995. [Google Scholar]
- 9.Mosquera RA, Avritscher EB, Samuels CL, Harris TS, Pedroza C, Evans P, et al. Effect of an enhanced medical home on serious illness and cost of care among high-risk children with chronic illness: a randomized clinical trial. JAMA. 2014;312(24):2640–8. [DOI] [PubMed] [Google Scholar]
- 10.Kleinman LC, Kosecoff J, Dubois RW, Brook RH. The medical appropriateness of tympanostomy tubes proposed for children younger than 16 years in the United States. JAMA. 1994;271(16):1250–5. [PubMed] [Google Scholar]
- 11.Kemper KJ. Medically inappropriate hospital use in a pediatric population. New England Journal of Medicine. 1988;318(16):1033–7. [DOI] [PubMed] [Google Scholar]
- 12.Casey PH, Lyle RE, Bird TM, Robbins JM, Kuo DZ, Brown C, et al. Effect of hospital-based comprehensive care clinic on health costs for Medicaid-insured medically complex children. Archives of Pediatrics & Adolescent Medicine. 2011;165(5):392–8. [DOI] [PubMed] [Google Scholar]
- 13.Berman S, Rannie M, Moore L, Elias E, Dryer LJ, Jones MD, Jr. Utilization and costs for children who have special healthcare needs and are enrolled in a hospital-based comprehensive primary care clinic. Pediatrics. 2005;115(6):e637–42. [DOI] [PubMed] [Google Scholar]
- 14.Gordon JB, Colby HH, Bartelt T, Jablonski D, Krauthoefer ML, Havens P. A tertiary care-primary care partnership model for medically complex and fragile children and youth with special healthcare needs. Archives of Pediatrics & Adolescent Medicine. 2007;161(10):937–44. [DOI] [PubMed] [Google Scholar]
- 15.Simon TD, Mahant S, Cohen E. Pediatric hospital medicine and children with medical complexity: past, present, and future. Current Problems in Pediatric and Adolescent Healthcare. 2012;42(5):113–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Council on Children with Disabilities and Medical Home Implementation Project Advisory Committee. Patient- and family-centered care coordination: a framework for integrating care for children and youth across multiple systems. Pediatrics. 2014;133(5):e1451–60. [DOI] [PubMed] [Google Scholar]
- 17.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health affairs. 2008;27(3):759–69. [DOI] [PubMed] [Google Scholar]
- 18.US Bureau of Labor Statistics. Occupational employment statistics. Available at: http://data.bls.gov/oes/search.jsp. Accessed November 2, 2015
- 19.Chen AY, Schrager SM, Mangione-Smith R. Quality measures for primary care of complex pediatric patients. Pediatrics. 2012:peds. 2011-0026. [DOI] [PubMed] [Google Scholar]
- 20.Berry JG, Agrawal RK, Cohen E, Kuo DZ. The landscape of medical care for children with medical complexity. Overland Park, KS: Children’s Hospital Association; 2013;7. [Google Scholar]
- 21.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey 2008. Available at: https://meps.ahrq.gov/mepsweb/data_stats/tables_compendia_hh_interactive. Accessed February 2, 2018. [PubMed]
- 22.Kaiser Family Foundation. Hospital adjusted expenses per inpatient day by ownership, 2015. Available at: https://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day-by-ownership/ Accessed February 2, 2018.
- 23.Berry JG, Agrawal R, Kuo DZ, Cohen E, Risko W, Hall M, et al. Characteristics of hospitalizations for patients who use a structured clinical care program for children with medical complexity. The Journal of Pediatrics. 2011;159(2):284–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gidengil C, Parast L, Burkhart Q, Brown J, Elliott MN, Lion KC, et al. Development and Implementation of the Family Experiences With Coordination of Care Survey Quality Measures. Academic Pediatrics. 2017. [DOI] [PubMed] [Google Scholar]
- 25.Hessels AJ, Agarwal M, Saiman L, Larson EL. Measuring patient safety culture in pediatric long-term care. Journal of Pediatric Rrehabilitation Medicine. 2017;10(2):81–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kleinman LC. Conceptual and technical issues regarding the use of HEDIS and HEDIS-like measures in preferred provider organizations. Medical Care Research and Review. 2001;58(4_suppl):37–57. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


